Supplemental Digital Content is available in the text
Keywords: Chinese, diabetic complications, T2DM, weight loss
Abstract
Our goal was to investigate the relationship between weight loss before a diagnosis of type 2 diabetes mellitus (T2DM) and diabetic complications among hospitalized patients with T2DM.
We conducted a cross-sectional study and evaluated 347 and 642 hospitalized patients with T2DM who experienced and did not experienced weight loss before T2DM diagnosis, respectively. We used propensity score matching to reduce the confounding bias between the groups. In addition, a logistic regression analysis of the matched data was performed to evaluate the risk of diabetic complications.
A total of 339 patients who experienced weight loss were matched to 339 patients who did not experience weight loss. After adjusting for age, gender, origin, occupation, smoking history, alcohol use, and duration of diabetes, the logistic regression analysis showed that compared with patients who did not experience weight loss, patients who lost ≤5 kg had a higher risk of diabetic nephropathy (DN) (odds ratio [OR]: 2.05, 95% confidence interval [CI]: 1.35–3.10) and diabetic retinopathy (OR: 1.79, 95% CI: 1.11–2.87). However, we did not observe a dose–response relationship in terms of weight loss.
We found that weight loss before a diagnosis of T2DM might serve as a risk factor for DN and diabetic retinopathy. Our findings demonstrate that we should strengthen the management and prevention of complications in patients who experience weight loss of ≤5 kg prior to a T2DM diagnosis, particularly those who are centrally obese.
1. Introduction
The prevalence of diabetes mellitus (DM) has increased rapidly over the past 2 decades.[1,2] In 2015, a total of 415 million adults worldwide had diabetes, and by 2040, this figure is expected to increase to 642 million.[3] China has the most patients with DM (92.4 million) of any country in the world.[4] As a result, DM has caused more than 10 million disability-adjusted life years and was the 8th major cause of death in China in 2012; thus, DM represents a major public health problem in China.[5] Type 2 diabetes mellitus (T2DM) is the most common type of DM in China, and a substantial proportion of patients with T2DM are at risk for diabetic complications.[6] Diabetic complications are linked with disability and even death in patients with T2DM and thus constitute the main disease burden of T2DM. Therefore, identifying patients at a high risk of developing complications is important.
To the best of our knowledge, clinical trials have generally focused on the association between diabetic complications and blood pressure and the levels of blood glucose and blood lipids. Furthermore, previous studies on weight loss have typically studied the benefits of intrusive body weight control for the control of diabetes complications.[7,8] Along with increased drinking, eating, and urinating, weight loss in the absence of intentional dieting, diuretic therapy or exercise prior to the diagnosis of T2DM is generally identified as a symptom of T2DM[9]; however, few studies have investigated the relationship between weight loss prior to the T2DM diagnosis and diabetic complications.
Thus, we designed an observational study to investigate the relationship between weight loss prior to the T2DM diagnosis and diabetic complications in hospitalized patients with T2DM, which is the population with the highest proportion of diabetic complications. To increase the comparability between the 2 groups (patients who experience and who do not experience weight loss before the diagnosis of T2DM) and to reduce the influence of confounding factors, we used propensity score matching (PSM).[10]
2. Design and methods
2.1. Study sample
We used clinical data from the Department of Nephrology and Endocrinology at the PLA 148th Hospital. Among the 1025 inpatients (recruited from January 2010 to December 2012), we excluded 25 type 1 DM inpatients and 11 latent autoimmune diabetes in adult inpatients and therefore recruited a total of 989 (507 men and 482 women) participants in this study.
Based on the inclusion criteria, the included participants were inpatients of the Department of Nephrology and Endocrinology at the PLA 148th Hospital from January 2010 to December 2012 who were diagnosed with T2DM, had no history of cancer and tumors, were not pregnant, and agreed to participate in this study. The exclusion criteria were the following: non-Chinese nationality, pregnant women, a history of cancer and tumors, and lack of consent to participate in this study.
We collected information regarding the participant's gender, age, occupation, region, alcohol consumption, smoking history, diabetes duration, weight loss, and diabetes complications status (acute and chronic complications).
2.2. Measurement
T2DM was defined according to the American Diabetes Association criteria. Diabetic complications comprise acute and chronic complications, and the acute complications included diabetic ketoacidosis, hyperglycemia hyperosmolar state, and diabetes lactic acidosis.[9] The chronic diabetic complications included cardiovascular and cerebrovascular diseases (diagnosed after T2DM), diabetic nephropathy (DN), diabetic retinopathy, diabetic peripheral neuropathy, and diabetic lower limb angiopathy. All diabetic complications were diagnosed by 2 physicians according to the diagnostic criteria provided by the Chinese Diabetes Society.
Weight loss was defined as a decrease of at least 5% body weight within 6 months before the diagnosis of T2DM in the absence of intentional dieting and diuretic therapies. This information was collected by the primary nurse, and to ensure the accuracy of the information, the weight loss was confirmed with the patients and their relatives. Central obesity was defined as a waist circumference >90 cm for men or >80 cm for women.[11] In addition, we used 5 kg as the threshold for weight loss because previous studies showed that a weight loss of at least 5 kg was the standard value defining significant weight loss in patients with obesity[12] and weight loss >5 kg during the course of 1 year is an independent risk factor for 6-month mortality of nursing home residents. Furthermore, we included continuous loss of weight (kg) in the logistic analysis to determine the odds ratios [ORs] of weight loss (kg).
2.3. Statistical analysis
SPSS version 19.0 (Serial No. 5076595) was used for the data analyses. The significance level for all tests was set to a 2-tailed α value of 0.05. The differences in means and proportions were evaluated using Student t test and Chi-squared tests, respectively. Logistic regression models were used to identify the risk of weight loss (grouped and continuous).
PSM[13] was used for matching between the weight-loss group and the no-weight-loss groups. Gender, age, origin, occupation, smoking history, alcohol use, and duration of T2DM were included as covariates. We used nearest-neighbor matching to match former smokers to current smokers at a 1:1 ratio with a caliper width of 0.02.[14]
2.4. Ethical considerations
The Committee for Medical Ethics of the Chinese PLA General Hospital examined and approved our study. Before completing the questionnaire, each involved participant signed an informed consent form.
3. Results
A total of 989 (507 men and 482 women) inpatients were included in our study prior to PSM. The average age of the participants was 56.8 ± 11.6 years (range: 14–93 years). The average ages of the patients in the weight-loss and no-weight-loss groups were 54.7 ± 11.3 years (19–93 years) and 58.0 ± 11.6 years (14–87 years), respectively. The general characteristics (age, gender, origin, occupation, smoking history, and alcohol use) of the participants are shown in Table 1. Compared with the patients in the weight-loss group, those in the no-weight-loss group were older, included a higher proportion of females, experienced a longer duration of T2DM and had a lower fasting blood glucose (FBG) level.
Table 1.
Demographic characteristics of the participants according to weight loss before and after PSM.
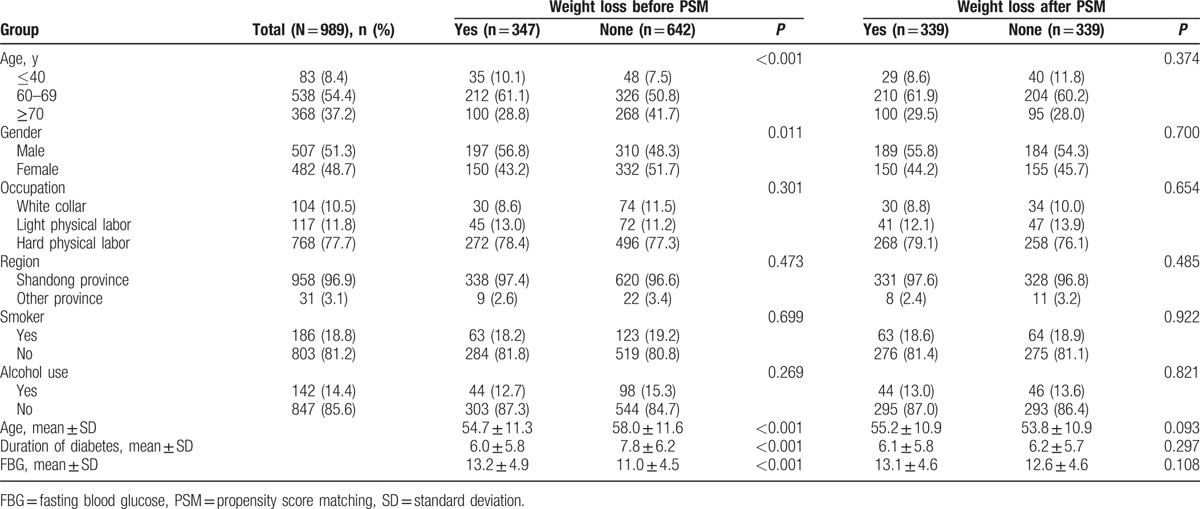
After PSM, a total of 392 participant pairs were matched, and the weight-loss and no-weight-loss groups were balanced in terms of age, gender, duration of diabetes, and FBG (Table 1).
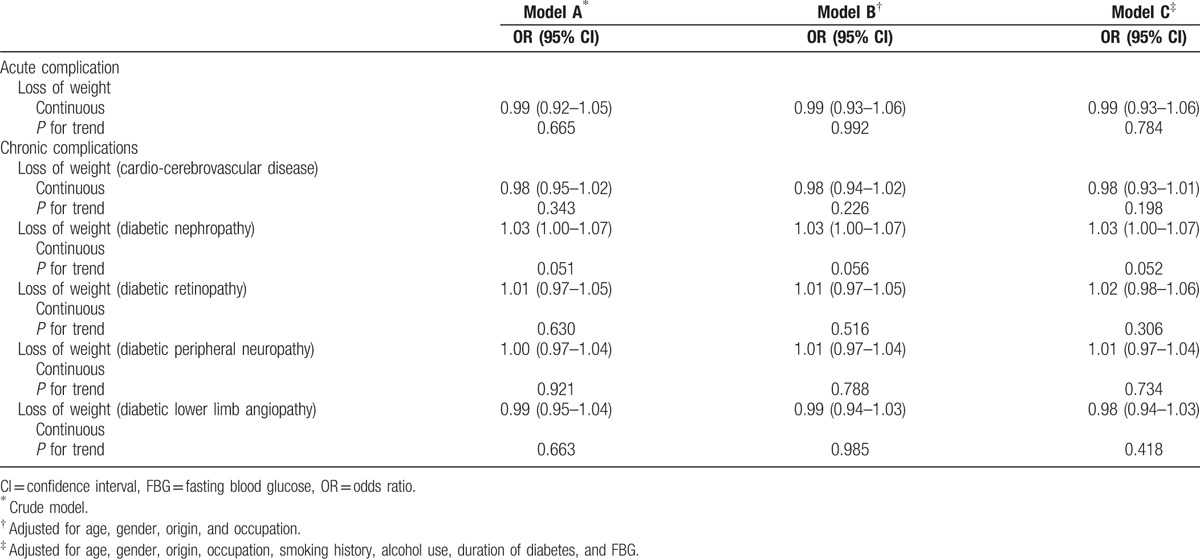
After adjusting for age, gender, origin, occupation, smoking history, alcohol use, duration of diabetes, and FBG, the logistic regression analysis revealed that compared with the no-weight-loss group, the group of patients who experienced a weight loss of ≤5 kg had a higher risk of DN (OR: 2.05, 95% confidence interval [CI]: 1.35–3.10) and diabetic retinopathy (OR: 1.79, 95% CI: 1.11–2.87); however, we did not observe a dose–response relationship based on the weight loss (Table 2). Furthermore, we included continuous loss of weight (kg) in the logistic analysis to determine the ORs of weight loss (continuous, kg) and obtained similar but not significant results (Table 3).
Table 2.
OR (95% CI) of diabetic complications according to weight loss among participants.
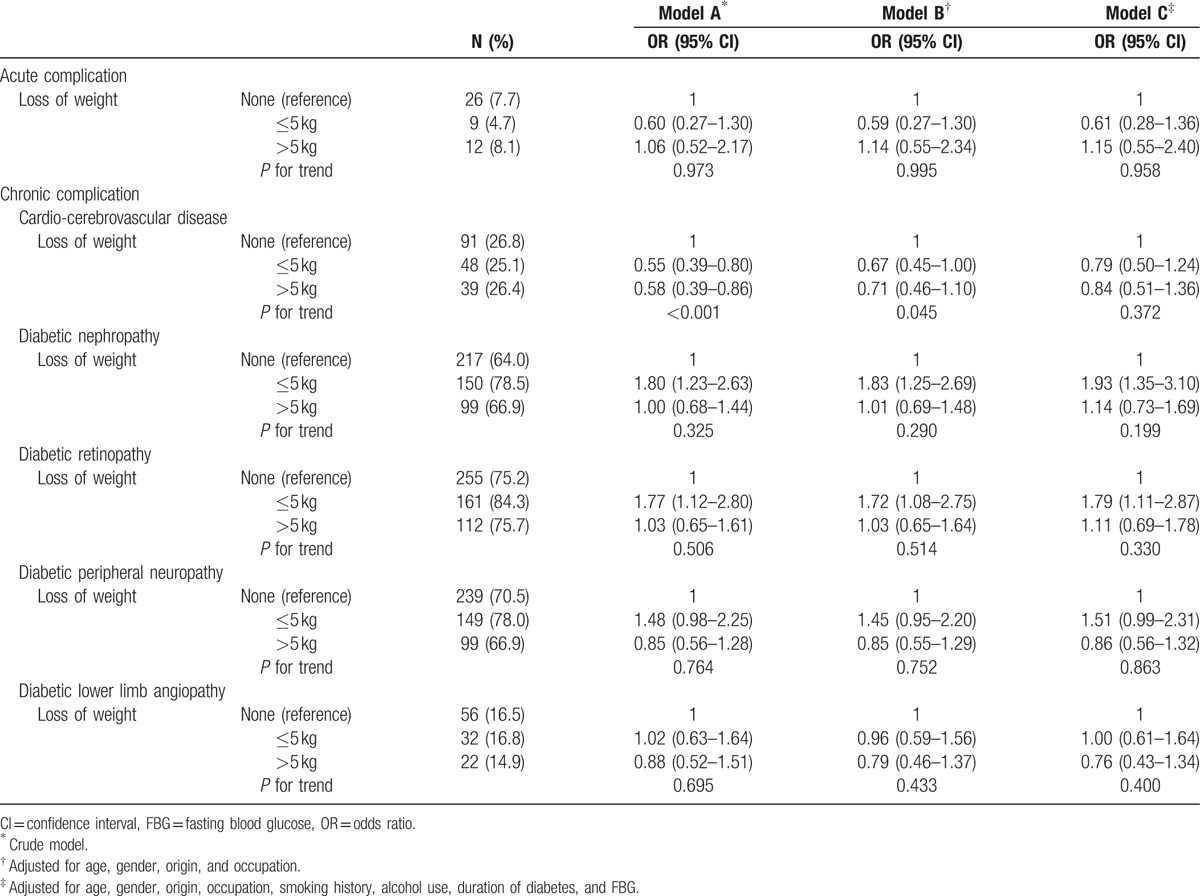
Table 3.
OR (95% CI) of diabetic complications for loss of weight in participants (continuous variable).
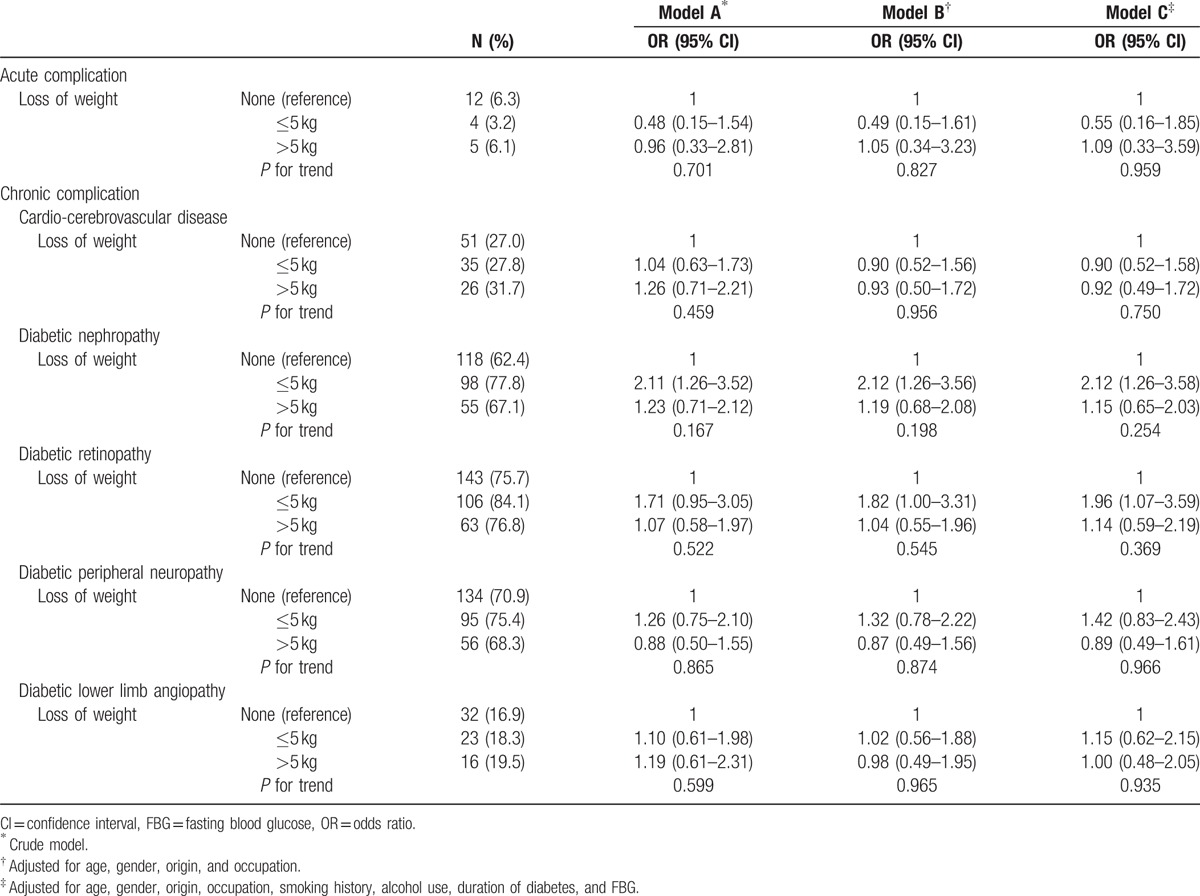
As shown in Table 4, among centrally obese participants, the weight-loss group (≤5 kg) was found to have a higher risk of DN (OR: 2.12, 95% CI: 1.26–3.58) and diabetic retinopathy (OR: 1.96, 95% CI: 1.07–3.59) after adjusting for age, gender, origin, occupation, smoking history, alcohol use, duration of diabetes, and FBG (Table 4). Among nonobese participants, this relationship was not significant (Supplementary Table S1).
Table 4.
OR (95% CI) of diabetic complications according to weight loss among obese participants.
4. Discussion
Weight loss without intentional dieting, diuretic therapy, or excise before a diagnosis of T2DM is a classic symptom of T2DM, although few studies have focused on the relationship between weight loss before a T2DM diagnosis and diabetic complications. Thus, we designed this study to observe this relationship among patients with T2DM in the PLA 148th Hospital. To the best of our knowledge, this study constitutes the first investigation of this association. The major strength of our study was the comprehensive control of and adjustment for a wide range of potential confounders using PSM. The similar results between the matched groups demonstrate the robustness of the results. Moreover, because weight loss prior to the T2DM diagnosis occurred before the onset of diabetic complications, the problem of reverse causality, one of the major limitations of cross-sectional studies, was not a major concern in our study.
After matching, we observed a significant association between an involuntary weight loss ≤5 kg before the diagnosis of T2DM and diabetic complications (DN and diabetic retinopathy). Previous studies have generally focused on the association between weight loss after a T2DM diagnosis (usually with an intervention, such as diet control, physical exercise, and even weight reduction surgery) and the developmental tendency of T2DM.[7,8] This intervention weight loss with lifestyle change is beneficial for controlling the patient's blood glucose and blood lipids[15,16]; furthermore, postdiagnosis weight loss might impact the patient's psychological state and therefore improve their health-related quality of life.[17] Regarding diabetic complications, the effect of intervention weight loss is confused or null; a cohort study showed weight loss due to gastric banding has no unfavorable effect on kidney function and retinopathy and no effect on the prevention of arterial hypertension or cardiovascular disease.[18] A meta-analysis on glycemic control and weight loss in patients with T2DM showed that exercise training reduces hemoglobin A1c by an amount that should decrease the risk of diabetic complications, but no significant effect on weight loss was found.[19] Different from intervention weight loss, we focused on weight lost without lifestyle changes or other interventions before the diagnosis of T2DM. This type of weight loss is usually identified as a symptom of T2DM, and in our study, we found that it might also be a risk factor for the development of diabetic complications (i.e., DN and diabetic retinopathy). Prediagnosis weight loss might be caused by osmotic diuresis under high blood glucose conditions. Moreover, compared with patients who do not experience weight loss, patients who experience weight loss may have a higher blood glucose when diagnosed with T2DM, which likely places a heavier burden on the kidney and microvascular system and thereby predisposes these individuals to a higher risk of developing DN and diabetic retinopathy. However, we did not observe a dose–response relationship with weight loss, which might reveal that the effect of weight loss on diabetic complications is not linear or that the mechanism differs when the amount of weight lost is >5 kg.
Our study further showed that among centrally obese patients, the weight-loss group had a higher risk of developing DN and diabetic retinopathy, but this risk was not significant among patients without central obesity. Indeed, studies have linked obesity with increased circulating hormone levels (including estrogens, androgens, insulin, and IGF-I), and central obesity is the manifestation of impaired glucose tolerance and insulin resistance.[20,21] Thus, the effect of weight loss in patients with T2DM with central obesity might be more significant.
This study had several limitations. Because the weight-loss information was based on recall, recall bias cannot be fully ruled out; however, the information was confirmed with patients and their relatives to ensure accuracy. Second, our sample might not be completely representative of patients with T2DM in China because our hospital is one of the best hospitals in Zibo and the inpatients at our hospital show a higher frequency of diabetic complications; however, the representativeness of our sample should not substantially affect the internal validity of the study. Finally, we could not examine the hazard ratio of weight loss with diabetic complications due to the lack of detailed information on the onset time of diabetic complications.
In summary, our study provides the first examination of the association of weight loss prior to a diagnosis of T2DM with diabetic complications among T2DM inpatients. We increased the comparability of the weight-loss and no-weight-loss groups using the PSM method and found that weight loss before a diagnosis of T2DM might be a risk factor for DN and diabetic retinopathy development; however, further cohort studies should be conducted to verify this causal relationship. Our findings further demonstrate that we should strengthen the management and prevention of complications in patients with weight loss ≤5 kg before their T2DM diagnosis, particularly those with central obesity.
Supplementary Material
Acknowledgments
The authors would like to thank Lei Xu, Qian Li, Wei Jia, Xinli Cai, Lihui Liu, Ying Zhang, Jinjuan Zhao, and Xinai Yan from the PLA 148th Hospital for their assistance with this research study. The authors also thank Kate S. of American Journal Experts for the help provided with the preparation of this manuscript.
Footnotes
Abbreviations: CI = confidence interval, DM = diabetes mellitus, DN = diabetic nephropathy, FBG = fasting blood glucose, OR = odds ratio, PSM = propensity score matching, T2DM = type 2 diabetes mellitus.
SY and SW have contributed equally to this work.
The authors have no funding and conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Guariguata L, Whiting DR, Hambleton I, et al. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract 2014;103:137–49. [DOI] [PubMed] [Google Scholar]
- [2].World Health Organization. Global Status Report on Noncommunicable Diseases 2014. World Health Organization; 2014; http://www.who.int/nmh/publications/ncd-status-report-2014/en (accessed May 19, 2016). [Google Scholar]
- [3].International Diabetes Federation. IDF Diabetes Atlas. 7th ed. International Diabetes Federation; 2015; http://www.diabetesatlas.org/ (accessed May 19, 2016). [Google Scholar]
- [4].Yang W, Lu J, Weng J, et al. Prevalence of diabetes among men and women in China. N Engl J Med 2010;362:1090–101. [DOI] [PubMed] [Google Scholar]
- [5].World Health Organization. Health Statistics and Information Systems, Estimates for 2000–2012. World Health Organization: 2016; http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html# Accessed May 2016. [Google Scholar]
- [6].Zhang L, Feng Y, List J, et al. Dapagliflozin treatment in patients with different stages of type 2 diabetes mellitus: effects on glycaemic control and body weight. Diabetes Obes Metab 2010;12:510–6. [DOI] [PubMed] [Google Scholar]
- [7].Douglas IJ, Krishnan B, Batterham RL, et al. Bariatric surgery in the United Kingdom: a cohort study of weight loss and clinical outcomes in routine clinical care. Rev Enferm 2015;12:S9–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Miller CK, Nagaraja HN, Weinhold KR. Early weight-loss success identifies nonresponders after a lifestyle intervention in a worksite diabetes prevention trial. J Acad Nutr Diet 2015;115:1464–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Chinese Diabetes Society. Guidelines for prevention and treatment of type 2 diabetes mellitus in China. Chin J Diabetes 2012;20:S1–37. [Google Scholar]
- [10].Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika 1983;70:41–55. [Google Scholar]
- [11].Xiao J, Xing X, Lu J, et al. Prevalence and associated factors of microalbuminuria in Chinese individuals without diabetes: cross-sectional study. BMJ Open 2013;3:e003325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Ho AK, Bartels CM, Thorpe CT, et al. Achieving weight loss and hypertension control among obese adults: a US multidisciplinary group practice observational study. Am J Hypertens 2016;29:984–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Thoemmes F. Propensity score matching in SPSS. Eprint Arxiv; 2012. arXiv:1201.6385 [stat.AP]. [Google Scholar]
- [14].Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat 2011;10:150–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Pedersen SD, Kang J, Kline GA. Portion control plate for weight loss in obese patients with type 2 diabetes mellitus: a controlled clinical trial. Arch Intern Med 2007;167:1277–83. [DOI] [PubMed] [Google Scholar]
- [16].Wei X, Barnsley J, Zakus D, et al. Evaluation of a diabetes management program in China demonstrated association of improved continuity of care with clinical outcomes. J Clin Epidemiol 2008;61:932–9. [DOI] [PubMed] [Google Scholar]
- [17].Williamson DA, Rejeski J, Lang W, et al. Impact of a weight management program on health-related quality of life in overweight adults with type 2 diabetes. Arch Intern Med 2009;169:163–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Zakaria AS, Rossetti L, Cristina M, et al. Effects of gastric banding on glucose tolerance, cardiovascular and renal function, and diabetic complications: a 13-year study of the morbidly obese. Surg Obes Relat Dis 2016;12:587–95. [DOI] [PubMed] [Google Scholar]
- [19].Boule NG, Haddad E, Kenny GP, et al. Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta-analysis of controlled clinical trials. JAMA 2001;286:1218–27. [DOI] [PubMed] [Google Scholar]
- [20].Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet 2005;365:1415–28. [DOI] [PubMed] [Google Scholar]
- [21].Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009;120:1640–5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


