Abstract
Background
Noncommunicable diseases (NCDs) are one of the major global health challenges in developed countries and are rapidly increasing globally. Perception of self-efficacy is important for complex activities and long-term changes in health behavior. This study aimed to determine whether self-efficacy mediates the effect of individual beliefs (perceived severity, susceptibility, benefits and barriers) among informal settlement residents’ health behavior in relation to the prevention and management of NCDs.
Methods
A cross-sectional survey was conducted using a closed-ended questionnaire among informal settlement residents in Diepsloot, Johannesburg. The proposed model was tested using structural equation modeling (AMOS software).
Results
A total of 2,277 participants were interviewed during this survey, consisting of 1,236 (54.3%) females, with the majority of them aged between 20 and 29 years. All constructs in the questionnaire had a good reliability with a Cronbach’s alpha of >0.7. Perceived benefits and perceived barriers were the strongest predictors of self-efficacy, with the highest beta values of 0.14 and 0.15, respectively. Once associated with perceived self-efficacy, the direct effect of perceived susceptibility and perceived benefits on health behavior was statistically nonsignificant (P=0.0894 and P=0.2839, respectively). Perceived benefits and perceived susceptibility were totally mediated by self-efficacy. The indirect effects of perceived severity and perceived barriers (through self-efficacy) on health behavior were significant. Thus, perceived severity and perceived barriers were partially mediated by self-efficacy.
Conclusion
Perceived susceptibility and perceived benefits did not affect health behavior unless associated with self-efficacy. In contrast, individual perception of the seriousness of NCDs and perceived barriers might still have a direct influence on health behavior even if the person does not feel able to prevent NCDs. However, this influence would be more significant when perceived severity and perceived barriers of NCDs are associated with self-efficacy.
Keywords: perceptions, Diepsloot township, health belief model, noncommunicable diseases, perceived susceptibility, perceived barriers
Background
NCDs have been recognized as the leading causes of morbidity and mortality worldwide, although their underlying risk factors are largely preventable.1–4 Adopting positive health behaviors and accessing preventive health care services can reduce morbidity and mortality from NCDs.5 Self-efficacy, in relation to health behavior, is an individual’s ability to change behavior, which is fundamental in reducing the incidence of NCDs and improving the health outcomes.6–8 Perception of self-efficacy is important for complex activities and long-term changes in health behavior, an aspect considered critical in NCD prevention and management.3,9 Self-efficacy is an indicator for predicting important health outcomes such as hospital admissions and health-related quality of life.9 The effects of lifestyle changes on the outcome of NCDs have shown to be consistent across various studies.10 Monitoring health-risk behaviors of communities and their participation in access to health care services provides information that is critical in designing behavior change interventions.5 People’s self-perception of their ability to function normally poses as an important mediating factor of health behaviors.9 Some studies indicate that NCD self-management programs can initiate positive behavioral and lifestyle changes and influence an improvement in the health of community members.11 Similarly, action control and self-monitoring, in particular, has been shown to be a very efficacious behavior change technique to initiate health behavior.12 However, knowledge, awareness and action control may not effectively change individual health behavior. This is an indication that behavior change modification through addressing determinants such as social influence, attitude, self-efficacy and intention might be necessary.13
Evidence-based solutions for changing health behaviors exist. However, problems such as feasibility, sustainability and dissemination limit the impact of evidence-based solutions on advocacy, social mobilization and behavioral and social changes among individuals.14 One study has shown that perceptions of illness influence the way patients cope and self-manage the illness. Knowledge of perception of illness may inform health care providers about the psychosocial responses of patients and may be a crucial component of good clinical practice.15
The HBM was tested for diabetes,16 HIV,17,18 cancer,19 dietary practices20 and other diseases.21,22 Despite that the HBM has been used for NCDs, the mediating role of selfefficacy has not been tested. Various studies have been conducted on the HBM.19,23–27 However, there is limited literature on the role of perceived self-efficacy as a mediator of perceived susceptibility, severity, barriers and benefits in influencing health behaviors in Johannesburg, South Africa. The predictive strength of individual beliefs regarding NCD- related health behavior has also not been investigated in the context of the prevention and management of NCDs.
In this study, perceived susceptibility is defined as an individual’s own perception of the likelihood of experiencing a condition that would adversely affect their health. Perceived severity is defined as a person’s interpretation of the degree of intensity of a disease. This means that the extent to which the person considers that the disease may make great demands on them and affect their interpretation of obstacles that could prevent or control advancement, access or progress. Perceived benefits have been defined as actions taken to prevent disease or deal with an illness. Perceived barriers are characteristics of a treatment or preventive measure that may be seen as inconvenient, expensive, unpleasant, painful or upsetting. Perceived self-efficacy in the context of this study is the individual confidence to prevent NCDs.19,23–27
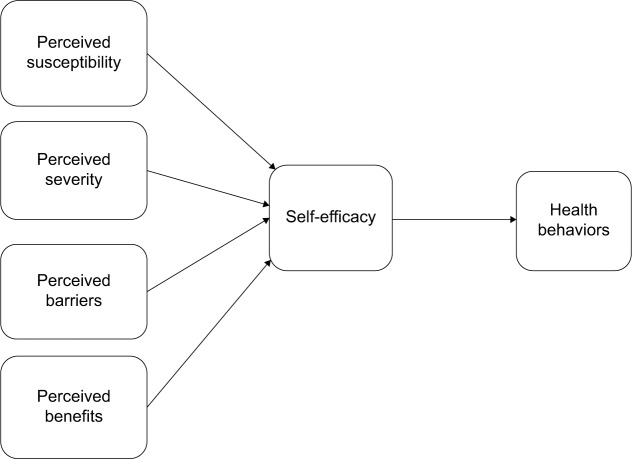
Urbanization in Johannesburg, South Africa, is a catalyst for the rapid development of informal settlements.28 The informal settlement residents are faced with limited access to health information on healthy lifestyle and health care services. Their living conditions are worsened by undue circumstances such as unemployment and poverty levels, making it difficult to practice good health behavior. As such, there is an increasing trend in the prevalence of NCDs among this population.3 In addition, there is limited literature on research conducted in informal settlements that relate to NCDs in Johannesburg, South Africa. Therefore, this study aimed to determine whether self-efficacy mediates the effect of individual beliefs (perceived susceptibility, severity, barriers and benefits) on informal settlement residents’ health behavior in relation to the prevention and management of NCDs using a conceptual model as illustrated in Figure 1. For the purposes of this study, we used a multiple behavior index in measuring health behavior.
Figure 1.
Proposed conceptual model of individual health beliefs, self-efficacy and health behavior in informal settlement residents.
In order to test the mediating effect of self-efficacy, the following four hypotheses were considered:
H1: Self-efficacy is mediating the effect of perceived susceptibility on health behavior.
H2: Self-efficacy is mediating the effect of perceived severity on health behavior.
H3: Self-efficacy is mediating the effect of perceived barriers on health behavior.
H4: Self-efficacy is mediating the effect of perceived benefits on health behavior.
Methods
Study design
A cross-sectional survey was conducted over a period of 6 days in the month of August 2014. The study targeted individuals who voluntarily participated in the Health Services Campaign. Individuals participating in these campaigns were offered the following health services for free: blood pressure checks, BMI assessment, TB screening, health education and HCT. Individuals with signs and symptoms of particular ailments were referred to health facilities for further clinical assessment within their catchment area. Systematic random sampling was done in which every seventh person who had a BMI assessment was invited to participate in the study.
Study setting
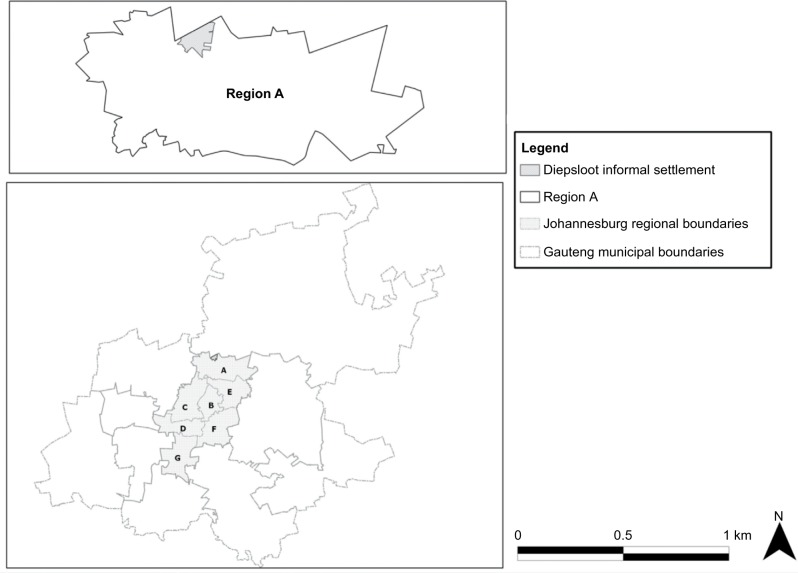
The study was conducted in a township located in Diepsloot, Region A, north of Johannesburg, as shown in Figure 2. In <20 years, Diepsloot has grown into a bustling neighborhood covering ~5 km2 with a population of >160,000.29 Diepsloot was established in 1994 as a relocation area for informally settled households from Zevenfontein. The Diepsloot region, a township where the study was conducted, has an estimated population size of 38,275.30 The informal settlements are overcrowded by inhabitants and numerous local shops referred to as “spaza shops” that sell lowly priced and mostly unhealthy foods.3
Figure 2.
Map shows the position of Diepsloot township (in gray) that is in Region A in the City of Johannesburg.
Data collection
Data were collected using a closed-ended questionnaire loaded onto an electronic data collection system using personal tablet computers. Thirty-one trained fieldworkers interviewed study participants and completed the questionnaire. During the Health Services Campaign, banners were displayed around the testing station explaining what NCDs are with a focus on ischemic heart disease, lung cancer, COPD and type II diabetes mellitus. Pamphlets on NCDs and HIV were also distributed. A public address system that continuously played music with an intermittent discussion on ischemic heart disease, lung cancer, COPD and type II diabetes mellitus exposed study participants to NCDs and their implications. This was considered as enough cues for people to understand what an NCD is and respond accordingly depending on their understanding of NCDs when asked to participate in our study.
Measures
The measures used for data collection were categorized into sociodemographics, anthropometric measurements, perceived susceptibility, perceived severity, perceived benefits, perceived barriers, health behavior and self-efficacy. Sociodemographic characteristics included participant’s marital status (single, married, divorced, cohabitating and widowed), ethnicity (black and nonblack), type of dwelling (formal housing and informal housing), employment status (unemployed and employed), nationality (non-South African and South African), age (20–29, 30–39, 40–49, 50–59 and ≥60 years) and highest education (below high school, high school and posthigh school qualifications, including certificate, diploma and degrees).
Perceived susceptibility, perceived severity, perceived benefits, perceived barriers; health behavior and self-efficacy regarding NCDs were collected using closed-ended questions. The participants rated each question on a Likert scale of 1–5 ranging from strongly disagree to strongly agree, respectively. The lists of items under each construct are listed in Table 1.
Table 1.
Items within constructs in the questionnaire
| Item codes | Questionnaire constructs |
|---|---|
| Psusceptibility | Perceived susceptibility |
| Psus1 | Being obese/overweight will lead me to get chronic diseases |
| Psus2 | My family medical history makes it likely to get chronic diseases |
| Psus3 | Smoking makes it likely to get chronic diseases |
| Psus4 | Unhealthy eating habits can make me get chronic diseases |
| Psus5 | Physical inactivity can make me get chronic diseases |
| Pseverity | Perceived severity |
| Psev1 | Having a chronic disease will have major effects on my life and family |
| Psev2 | Having a chronic disease will have major effects on my work and income |
| Psev3 | Having a chronic disease will cripple me |
| Psev4 | Having a chronic disease will change my outlook |
| Psev5 | Thought of having chronic diseases scares me |
| Pbenefits | Perceived benefits |
| Pbenefi | Not having a chronic disease is beneficial |
| Pbenef2 | Physical activities prevent chronic diseases |
| Pbenef3 | Healthy lifestyle prevents chronic diseases |
| Pbenef4 | Managing weight prevents chronic diseases |
| Pbenef5 | Not smoking prevents chronic diseases |
| Pbenef6 | Regular health checks will detect chronic diseases early |
| Pbenef7 | Regular health checks are beneficial |
| Pbarriers | Perceived barriers |
| Pbari | Very little that can be done to prevent chronic diseases |
| Pbar2 | No treatment will be effective in curing chronic diseases |
| Pbar3 | Healthy foods are expensive |
| Pbar4 | Health check-ups are expensive |
| Pbar5 | Preparing healthy foods is time-consuming |
| Pbar6 | Health check-ups are time-consuming |
| Pbar7 | It is embarrassing to go for health checks |
| Hbehavior | Health behavior |
| HBI | I eat a well-balanced diet |
| HB2 | I always follow medical orders to benefit my health |
| HB3 | I frequently make efforts to improve my health |
| HB4 | I exercise regularly at least three times per week |
| HB5 | I avoid fatty foods |
| HB6 | I eat small portion meals |
| Sefficacy | Self-efficacy |
| SEI | I am confident about how to prevent chronic diseases |
| SE2 | I am actively working on a healthy lifestyle to prevent chronic diseases |
| SE3 | I attend health assessments to prevent chronic diseases |
| SE4 | I have information on how to prevent chronic diseases |
Statistical analysis
Statistical analysis was performed using SPSS for Windows, Version 22 (SPSS; Chicago, IL, USA) for descriptive analysis. Further analysis for SEM was performed using Analysis of Moment Structure Version 22 (AMOS: ADC, Chicago, IL, USA).
A correlation matrix was generated using the PPMCC sometimes called “Pearson’s r” to determine the correlation coefficient of each variable. A presence of variables with very strong relationships (Rxy >0.80) results in singular covariance matrices. Multicollinearity between indicator variables is prevented by SEM solution. Many reasons motivated the choice of the SEM technique. Contrary to first-generation statistical tools such as regression, SEM enables researchers to answer a set of interrelated research questions in a single, systematic and comprehensive way. This can be done by modeling the relationships among multiple independent and dependent constructs simultaneously.31–35 This capability for simultaneous analysis differs greatly from most of the first-generation regression models, such as linear regression, LOGIT, analysis of variance and multivariate analysis of variance.
These models analyze only one layer of linkages between independent and dependent variables at a time.36–38 The combined analysis of the measurement and the SEM enables measurement errors of the observed variables to be analyzed as an integral part of the model. Factor analysis could also be combined in one operation with hypotheses testing. The result is a more rigorous analysis of the proposed research model and is a better methodological assessment tool.39
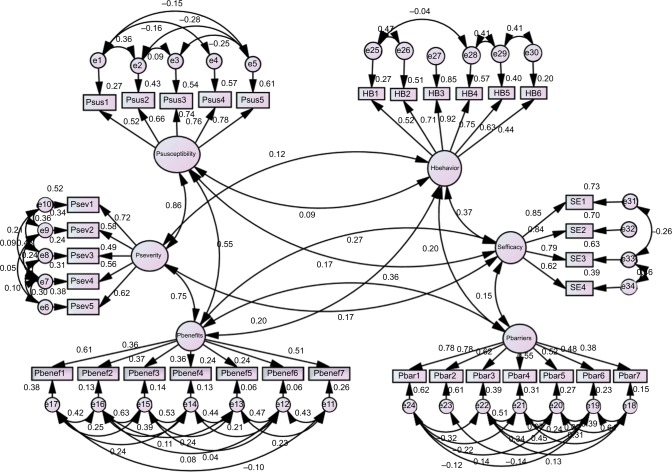
A confirmatory factor analysis (Figure 3) was conducted through a measurement model to determine the underlining components of the various factors involved in the proposed model (Figure 1). The next step of the SEM consisted of designing and testing the structural model (Figure 4). Evaluation of both the measurement and structural models also involved the use of fit indices. The chi-square statistics provided a test of the null hypothesis, ensuring that the theoretical model fits the data. Indices used to demonstrate the model goodness of fit were RMSEA, AGFI and CFI. A CFI value close to 0.9 and RMSEA value close to 0.07 indicated acceptable fit of the model.
Figure 3.
Measurement model.
Notes: Psusceptibility, perceived susceptibility; Psus I, being obese/overweight will lead me to get chronic diseases; Psus2, my family medical history makes it likely to get chronic diseases; Psus3, smoking makes it likely to get chronic diseases; Psus4, unhealthy eating habits can make me get chronic diseases; Psus5, physical inactivity can make me get chronic diseases; Pseverity, perceived severity; Psev I, having a chronic disease will have major effects on my life and family; Psev2, having a chronic disease will have major effects on my work and income; Psev3, having a chronic disease will cripple me; Psev4, having a chronic disease will change my outlook; Psev5, thought of having chronic diseases scares me; Pbenefits, perceived benefits; Pbenefl, not having a chronic disease is beneficial; Pbenef2, physical activities prevent chronic diseases; Pbenef3, healthy lifestyle prevents chronic diseases; Pbenef4, managing weight prevents chronic diseases; Pbenef5, not smoking prevents chronic diseases; Pbenef6, regular health checks will detect chronic diseases early; Pbenef7, regular health checks are beneficial; Pbarriers, perceived barriers; Pbar1, very little that can be done to prevent chronic diseases; Pbar2, no treatment will be effective in curing chronic diseases; Pbar3, healthy foods are expensive; Pbar4, health check-ups are expensive; Pbar5, preparing healthy foods is time-consuming; Pbar6, health check-ups are time-consuming; Pbar7, it is embarrassing to go for health checks; Hbehavior, health behavior; HBI, I eat a well-balanced diet; HB2, I always follow medical orders to benefit my health; HB3, I frequently make efforts to improve my health; HB4, I exercise regularly at least three times per week; HB5, I avoid fatty foods; HB6, I eat small portion meals; Sefficacy, self-efficacy; SEI, I am confident about how to prevent chronic diseases; SE2, I am actively working on a healthy lifestyle to prevent chronic diseases; SE3, I attend health assessments to prevent chronic diseases; SE4, I have information on how to prevent chronic diseases.
Figure 4.
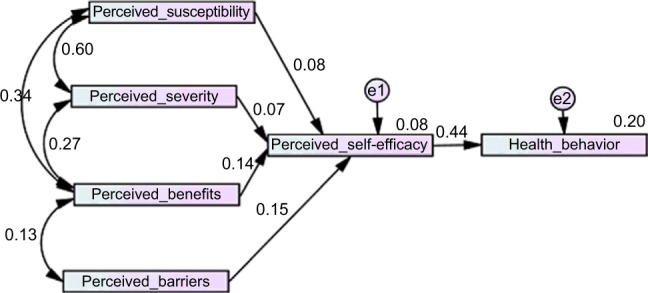
Structural model.
AMOS also allowed the use of modification indices to improve the model fit chi-square by drawing a correlation function between the identified variables. All the hypothesized paths in the conceptual model (Figure 1) were tested and included in the structural model. The correlation coefficients (r) appearing on the measurement model and Cronbach’s alpha coefficients of the constructs were generated by SPSS v 22.
Ethics approval
The ethics approval for this study was obtained from Monash University Human Research Ethics Committee, approval no: CF14/2803 - 2014001558. Verbal informed consent was obtained at the time of data collection, and the data remained anonymous.
Results
Descriptive statistics
A total of 2,277 participants were interviewed during this survey consisting of 1,236 (54.3%) females. The majority of the survey participants were single, black, lived in a shack, unemployed, South African, aged 20–29 years with no matric qualification and earned <R1,000 per month. Marital status (P=0.046), employment status (P<0.001), nationality (P=0.010), age groups (P<0.001), highest academic qualification (P<0.001) and monthly income (P<0.001) had a statistically significant variation between male and female respondents as listed in Table 2.
Table 2.
Distribu participantstion of baseline characteristics of study
| Characteristics | Female (n= 1,236), n (%) |
Male (n= 1,041), n (%) |
P-value |
|---|---|---|---|
| Marital status | 0.046 | ||
| Cohabitating | 6 (0.5) | 0 (0.0) | |
| Divorced | 12 (1.0) | 15 (1.4) | |
| Married | 312 (25.2) | 231 (22.2) | |
| Single | 900 (72.8) | 792 (76.1) | |
| Widowed | 6 (0.5) | 3 (0.3) | |
| Ethnicity | 0.302 | ||
| Black | 1,224 (99.0) | 1,026 (98.6) | |
| Nonblack | 12 (1.0) | 15 (1.4) | |
| Type of dwelling | 0.881 | ||
| Formal house | 231 (18.7) | 192 (18.4) | |
| Informal house | 1,005 (81.3) | 849 (81.6) | |
| Employment status | <0.001 | ||
| Employed | 102 (8.3) | 189 (18.2) | |
| Unemployed | 1,134 (91.7) | 852 (81.8) | |
| Nationality | 0.010 | ||
| Non-South African | 180 (14.6) | 114 (11.0) | |
| South African | 1,056 (85.4) | 927 (89.0) | |
| Age groups | <0.001 | ||
| 20–29 years | 654 (52.9) | 426 (40.9) | |
| 30–39 years | 360 (29.1) | 414 (39.8) | |
| 40–49 years | 171 (13.8) | 129 (12.4) | |
| >49 years | 51 (4.1) | 72 (7.0) | |
| Highest education | <0.001 | ||
| Certificate | 60 (4.9) | 21 (2.0) | |
| Degree | 24 (1.9) | 15 (1.4) | |
| Diploma | 39 (3.2) | 42 (4.0) | |
| Matric | 477 (38.6) | 315 (30.3) | |
| No matric | 636 (51.5) | 648 (62.3) | |
| Monthly income | <0.001 | ||
| <R1,000 | 1,134 (91.7) | 852 (81.8) | |
| R1,000–4,999 | 84 (6.8) | 156 (15.0) | |
| >R4,999 | 18 (1.5) | 33 (3.2) |
All constructs had good reliability as listed in Table 3 because Cronbach’s alpha coefficient was >0.7. This means that the internal consistencies of all constructs of the proposed model were >70%.
Table 3.
Reliability of the constructs
| Constructs | Number of items | Cronbach’s alpha |
|---|---|---|
| Perceived susceptibility | 5 | 0.812 |
| Perceived severity | 5 | 0.836 |
| Perceived benefits | 7 | 0.778 |
| Perceived barriers | 7 | 0.864 |
| Perceived self-efficacy | 4 | 0.784 |
| Health behavior | 6 | 0.842 |
Structural equation modeling
Measurement model
Initially, the hypothesized model was generated from the predicted paths among observed and latent variables predicted from literature and by a qualitative data collection method (Figure 1). The measurement model indicated that there is no confounding effect between the independent and dependent variables.
The measurement model in Figure 2 indicated the overall good factor loading of the items in the five constructs measuring perceived susceptibility, severity, self-efficacy and barriers. However, the items “managing weight prevents chronic diseases” (Pbenef4) and “not smoking prevents chronic diseases” (Pbenef5) had a low factor loading of <0.3 in the construct measuring perceived benefit.
The model also indicates the overall good correlations among constructs (r<0.5). However, there is a strong correlation between perceived susceptibility and perceived severity (r=0.86) and between perceived severity and perceived benefit (r=0.75). This could imply that these factors are overlapping or they could be measuring the same thing. Therefore, further studies could redesign these two factors.
The keys for variable names in the above mentioned measurement model are listed in Table 1. Although RMSEA (0.081) is slightly above the threshold of 0.07, the overall measurement model indicates an acceptable model fit with GFI (0.852), AGFI (0.810), TLI (0.806) and CFI (0.840).31–35 The constructs involved in the model are interrelated, and the items used to measure these constructs are appropriate. After assessing the validity of the measurement tools, the next session explored the relationships hypothesized by the proposed conceptual model.
Structural model
The structural model was useful to test the hypotheses formulated in the proposed model. The regression coefficients (single arrows) as well as the correlation coefficients (doubled arrows) are shown in Figure 4.
The chi-square of the measurement model is 159.545 (P≤0.001) at three degrees of freedom. The indices GFI (0.977), AGFI (0.921), TLI (0.825) and CFI (0.930) indicate a good model fit with indices >0.90. However, RMSEA =0.106 is slightly above the threshold of 0.07.
According to Figure 2, one unit increase in an individual’s perceived susceptibility, severity, benefits and barriers to NCD would lead to an increase in an individual’s perceived self-efficacy by 0.08, 0.07, 0.14 and 0.15 units, respectively. A unit increase in self-efficacy would lead to an increase of 0.44 units in behavior change. Perceived benefits and perceived barriers were the strongest predictors of self-efficacy because they had the highest beta values of 0.14 and 0.15, respectively.
As previously stated (on the measurement model), the overall level of correlation among the constructs was good (<0.5) except for perceived severity and susceptibility (r=0.6).
The mediating role of self-efficacy on the effect of individual beliefs (perceived susceptibility, severity, barriers and benefits) among informal settlement residents’ health behavior was tested in the model, and the results are listed in Table 4. When testing the mediating role self-efficacy of perceived susceptibility on health behavior, results indicated that perceived susceptibility had both a significant indirect effect and a nonsignificant direct effect on health behavior, which means that the indirect effect of perceived susceptibility on health behavior was totally mediated by self-efficacy. In other words, the belief that NCDs constitute a risk could only lead to health behavior if the individual was confident that they would able to prevent NCDs. It also means that the perception of NCD risks did influence the individual confidence in preventing NCDs, which in turn led to a change in health behavior. This conclusion was supported by the fact that the bootstrap interval (0.070; 0.129) of the indirect effect of perceived susceptibility (0.099) on health behavior through perceived self-efficacy did not contain the number zero. In addition, the direct effect of perceived susceptibility on health behavior became nonsignificant (P=0.89) when associated with perceived self-efficacy. From this study, perceived susceptibility was ineffective in influencing health behavior without factoring in self-efficacy.
Table 4.
Mediating role of self-efficacy from the other individual beliefs to health behavior measured using standardized correlation coefficients
| Hypothesis | Indirect effect | P-value of indirect effects | Direct effect | P-value of direct effects | Bootstrap interval of the indirect effect | Total effects | Type of mediation |
|---|---|---|---|---|---|---|---|
| H1:Self-efficacy is mediating the effect of perceived susceptibility on health behavior | 0.099 | <0.001 | 0.041 | 0.089 (nonsignificant) | (0.070; 0.129) | 0.141 | Total |
| H2: Self-efficacy is mediating the effect of perceived severity on health behavior | 0.106 | <0.001 | 0.104 | <0.001 (significant) | (0.074; 0.145) | 0.210 | Partial |
| H3: Self-efficacy is mediating the effect of perceived barriers on health behavior | 0.053 | <0.001 | 0.168 | <0.001 (significant) | (0.039; 0.068) | 0.221 | Partial |
| H4: Self-efficacy is mediating the effect of perceived benefits on health behavior | 0.102 | <0.001 | 0.024 | 0.263 (nonsignificant) | (0.079; 0.132) | 0.126 | Total |
Perceived benefits were totally mediated by self-efficacy with a bootstrap interval of (0.079; 0.132), showing a significant indirect effect of perceived benefit (0.102) on health behavior through perceived self-efficacy. In addition, the direct effect of perceived benefit on health behavior became statistically nonsignificant (P=0.263) when associated with perceived self-efficacy. In other words, the perceived gain in adopting health behavior could only lead to action if people felt confident enough to be able to perform the health behavior. In addition, seeing the usefulness of preventing NCDs did not affect health behavior directly. However, it impacted on self-efficacy, which in turn affected the behavior.
The effect of perceived barriers on health behavior was partially mediated by self-efficacy, which meant that the challenges people experienced while trying to prevent NCDs did affect individual health behavior. However, this effect strongly depended on their level of confidence to be able to prevent and manage NCDs. This was supported by a bootstrap interval (0.039; 0.068) of the indirect effect of perceived barriers (0.053) on health behavior through perceived selfefficacy. In addition, the direct effect of perceived barriers on health behavior is still significant (P<0.001) when associated with self-efficacy. We, therefore, concluded that perceived barriers could still have a direct influence on health behavior without self-efficacy; however, this effect (0.168) would be smaller compared to when perceived barrier is associated with self-efficacy (0.221).
Perceived severity was partially mediated by self-efficacy with a bootstrap interval of (0.074; 0.145), showing the indirect effect of perceived severity (0.106) on health behavior through perceived self-efficacy. In addition, the direct effect of perceived severity on health behavior was still significant (P<0.001) when associated with self-efficacy. We concluded that the individual perception of the seriousness of NCDs could still have a direct influence on health behavior even if the person did not feel able to prevent NCDs. However, such effect (0.104) would be more significant when perceived severity of NCDs was associated with self-efficacy (0.210).
Discussion
Previous studies have indicated that health behavior and health behavior change are some of the complex phenomena in behavioral sciences.40,41 This study aimed to investigate whether self-efficacy could mediate the effect of individual beliefs (perceived severity, susceptibility, benefits and barriers) about their health behavior in relation to NCD prevention and management intervention at the community level.
In this study, the results showed that self-efficacy was found to be a partial mediator of perceived severity and perceived barriers on health behavior. These findings built on previous studies in which good health behavior was found to be positively associated with perceived disease severity.42 In addition, perceived susceptibility and perceived benefit were totally mediated by self-efficacy. This is contrary to other studies where good health behavior was found to be negatively associated with perceived susceptibility.42
Although self-efficacy was shown to be a mediator between perceived severity, barriers and benefits in this study, this must not be misconstrued to mean that individuals with a high self-efficacy will automatically behave in accordance with their level of self-efficacy as it relates to NCD and health behavior. This, as indicated earlier, is a complex phenomenon, and self-efficacy alone cannot always be a reliable predictor or mediator of good health behavior.43
In summary, data from this study suggested that perceived susceptibility and benefits did not affect behavior change unless they are associated with self-efficacy. The combination of perceived susceptibility and perceived benefits was totally mediated by self-efficacy as mapped in the HBM.
The findings in this study have important implications because they inform researchers, communities and policy makers that a broad range of factors related to self-efficacy may influence NCD education programs. It would also affect lifestyle modification among the informal settlement inhabitants in South Africa. In addition, the results of this study emphasize the importance of considering the unique social and cultural context of adults in these informal settlements. The goal of tailoring interventions to young men and females separately when addressing NCDs to improve self-efficacy is a central concept in popular information processing models used in health communication, including social cognitive theory,44 the HBM,24,45 protection motivation theory,46,47 the extended parallel process model48,49 and the theory of planned behavior.50,51
This study also affirmed that self-efficacy also plays a major role in the maintenance of health behaviors as documented across diverse health domains including exercise,52,53 sexual activity,54 diet55 and cardiovascular disease prevention.56–59 Another study also reviewed the role of self-efficacy in cigarette smoking, weight control, contraception, alcohol abuse and exercise behaviors.60 Individuals with comparatively higher levels of self-efficacy were more likely to sustain their healthy behaviors, probably because they tended to construe obstacles as challenges to be overcome.61 In an effort to increase individual self-efficacy, there is a need to establish interventions that promote health education on lifestyle changes, good dietary practices and exercise. The importance of regular health checks must be highlighted in the health education activities.
Limitations of the study
The authors have identified several limitations to this study. First, the cross-sectional survey adopted in this study did not provide a cause and effect relationship between variables. The second limitation is that a cross-sectional survey was done at a single point in time, which limited the possibility of varied findings. Third, self-reported information in public venues could lead to over reporting and under reporting of socially desirable and unacceptable behaviors, respectively.62,63 Although self-reporting of individual perceptions provides an imperfect estimate of health behaviors, it is still the most common method of health behavior measurement.64 These findings are also drawn from a special group and hence are not generalizable to the entire population; they need to be interpreted in the context of informal settlement residents.
Although anecdotal data from recruiters suggested that refusal was minimal, our sampling process did not allow us to access the refusal rates, while recruitment of respondents’ postservice provision was not captured. Interviewing the respondents who had refused could have given a different picture of the study population. These methods diverge from many of the current, traditional methods for changing health practices. Recommendations for incorporating the enhancement of self-efficacy into health behavior change programs are made in light of the study findings.
Conclusion
Using SEM, this study indicated that overall effect of perceived susceptibility and perceived benefits was totally mediated by self-efficacy. This suggested that the perception of NCD risks could have an influence on individual confidence in preventing NCDs, which in turn could lead to good health behavior. In addition, the perceived benefits of adopting health behavior could only lead to action if people felt confident enough to practice good health behavior. It was also found that perceived severity and perceived barriers still had a significant impact on health behavior even when they were not associated with self-efficacy. This study provided a clear indication to inform researchers, communities and policy makers that a broad range of factors related to selfefficacy could influence NCD education programs as well as lifestyle modifications among the informal settlement inhabitants in South Africa.
Acknowledgments
The Independent Development Trust covered the funding for this study for field staff. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the article.
Abbreviations
- AGFI
adjusted goodness-of-fit index
- BMI
body mass index
- COPD
chronic obstructive pulmonary disease
- CFI
comparative fit index
- GFI
goodness of fit index
- HBM
health belief model
- HCT
HIV counseling and testing
- HIV
human immunodeficiency virus
- NCDs
noncommunicable diseases
- PPMCC
Pearson product-moment correlation coefficient
- RMSEA
root mean square error of approximation
- SEM
structural equation modeling
- TB
tuberculosis
- TLI
Tucker-Lewis index
Footnotes
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work. PSN is the guarantor of this article.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.World Health Organization Our cities, our health, our future-Acting on social determinants for health equity in urban settings. Cent Heal Dev. 2008:1–180. [Google Scholar]
- 2.Department of National Health: South Africa . Strategic Plan for the Prevention and Control of Non-Communicable Diseases 2013–17. Pretoria, South Africa: Department of National Health; 2013. [Google Scholar]
- 3.Tshuma N. Perceptions of risk of non-communicable diseases associated with overweight and obesity among individuals living in Diepsloot informal settlements, Johannesburg, South Africa. South Am J Public Heal. 2014;2(4):629–665. [Google Scholar]
- 4.Puoanei T, Tsolekilei L, Sanders D, Parker W. Chronic non-communicable diseases. South Afr Med Res Counc. 2008:73–88. [Google Scholar]
- 5.Xu F, Mawokomatanda T, Flegel D, et al. Surveillance for certain health behaviors among states and selected local areas - Behavioral Risk Factor Surveillance System, United States, 2011. MMWR Surveill Summ. 2014;63(9):1–149. [PubMed] [Google Scholar]
- 6.Silva-Matos C, Beran D. Non-communicable diseases in Mozambique: risk factors, burden, response and outcomes to date. Global Health. 2012;8:37. doi: 10.1186/1744-8603-8-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bachani D, Srivastava R. Burden of NCDs, policies and programme for prevention and control of NCDs in India. Indian J Community Med. 2011;36(Suppl 1):7. doi: 10.4103/0970-0218.94703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fleig L, Pomp S, Schwarzer R, Lippke S. Promoting exercise maintenance: how interventions with booster sessions improve long-term rehabilitation outcomes. Rehabil Psychol. 2013;58(4):323–333. doi: 10.1037/a0033885. [DOI] [PubMed] [Google Scholar]
- 9.Frei A, Svarin A, Steurer-Stey C, Puhan MA. Self-efficacy instruments for patients with chronic diseases suffer from methodological limitations - a systematic review. Health Qual Life Outcomes. 2009;7:86. doi: 10.1186/1477-7525-7-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Richardson CR, Faulkner G, McDevitt J, Skrinar GS, Hutchinson DS, Piette JD. Integrating physical activity into mental health services for persons with serious mental illness. Psychiatr Serv. 2005;56(3):324–331. doi: 10.1176/appi.ps.56.3.324. [DOI] [PubMed] [Google Scholar]
- 11.Harvey IS, Janke M. Qualitative exploration of rural focus group members’ participation in the Chronic Disease Self-Management Program, USA. Rural Remote Health. 2014;14(3):2886. [PubMed] [Google Scholar]
- 12.Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a metaregression. Health Psychol. 2009;28(6):690. doi: 10.1037/a0016136. [DOI] [PubMed] [Google Scholar]
- 13.Huis A, van Achterberg T, de Bruin M, Grol R, Schoonhoven L, Hulscher M. A systematic review of hand hygiene improvement strategies: a behavioural approach. Implement Sci. 2012;7:92. doi: 10.1186/1748-5908-7-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mann DM, Quintiliani LM, Reddy S, Kitos NR, Weng M. Dietary approaches to stop hypertension: lessons learned from a case study on the development of an mHealth Behavior Change System. JMIR Mhealth Uhealth. 2014;2(4):e41. doi: 10.2196/mhealth.3307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaptein AA, Klok T, Moss-Morris R, Brand PLP. Illness perceptions: impact on self-management and control in asthma. Curr Opin Allergy Clin Immunol. 2010;10(3):194–199. doi: 10.1097/ACI.0b013e32833950c1. [DOI] [PubMed] [Google Scholar]
- 16.Becker MH, Janz NK. The health belief model applied to understanding diabetes regimen compliance. Diabetes Educ. 1985;11(1):41–47. [Google Scholar]
- 17.Kabiru CW, Beguy D, Crichton J, Zulu EM. HIV/AIDS among youth in urban informal (slum) settlements in Kenya: what are the correlates of and motivations for HIV testing? BMC Public Health. 2011;11:685. doi: 10.1186/1471-2458-11-685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gatta A, Thupayagale-Tshweneagae G. Knowledge of, and attitudes towards, voluntary HIV counselling and testing services amongst adolescent high school students in Addis Ababa, Ethiopia. Curationis. 2012;35(1):E1–E8. doi: 10.4102/curationis.v35i1.103. [DOI] [PubMed] [Google Scholar]
- 19.Guvenc G, Akyuz A, Açikel CH. Health belief model scale for cervical cancer and Pap Smear Test: psychometric testing. J Adv Nurs. 2011;67(2):428–437. doi: 10.1111/j.1365-2648.2010.05450.x. [DOI] [PubMed] [Google Scholar]
- 20.Deshpande S, Basil MD, Basil DZ. Factors influencing healthy eating habits among college students: an application of the health belief model. Health Mark Q. 2009;26(2):145–164. doi: 10.1080/07359680802619834. [DOI] [PubMed] [Google Scholar]
- 21.Shojaeizadeh D, Sadeghi R, Tarrahi MJ, Lashgarara B. The effect of educational intervention on prevention of osteoporosis through health belief model (HBM) in volunteers of Khorramabad city’s Health Centers in 2010–2011. Ann Biol Res. 2012;3(1):300–307. [Google Scholar]
- 22.Chen M-F, Wang R-H, Schneider JK, et al. Using the health belief model to understand caregiver factors influencing childhood influenza vaccinations. J Community Health Nurs. 2011;28(1):29–40. doi: 10.1080/07370016.2011.539087. [DOI] [PubMed] [Google Scholar]
- 23.Rosenstock IM. The health belief model and preventive health behavior. Health Educ Monogr. 1974;2:354–386. [Google Scholar]
- 24.Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 25.Stretcher V, Rosenstock IM. The health belief model. In: Glanz K, Lewis FM, Rimer BK, editors. Health Behavior and Health Education: Theory, Research and Practice. San Francisco, CA: John Wiley and Sons, Inc; 1997. pp. 31–36. [Google Scholar]
- 26.Champion VL, Skinner CS. The health belief model. In: Glanz K, Lewis FM, Rimer BK, editors. Health Behavior and Health Education: Theory, Research and Practice. 4th ed. San Francisco, CA: John Wiley and Sons, Inc; 2008. pp. 45–65. [Google Scholar]
- 27.Carpenter CJ. A meta-analysis of the effectiveness of health belief model variables in predicting behavior. Health Commun. 2010;25(8):661–669. doi: 10.1080/10410236.2010.521906. [DOI] [PubMed] [Google Scholar]
- 28.De Wet T, Patel L, Korth M, Forrester C. Johannesburg Poverty and Livelihoods Study. Johannesburg: Centre for Social Development in Africa, University of Johannesburg; 2008. [Google Scholar]
- 29.Johannesburg Development Agency Diepsloot: Readyfor Development. 2013. [Accessed March 7, 2015]. Available from: http://www.urbanlandmark.org.za/downloads/diepsloot_brochure.pdf.
- 30.Ayala A, Geurts E, Ahmad P, et al. Urbanising Africa: The City Centre Revisited. Rotterdam: IHS; 2010. pp. 1–80. Number 26. [Google Scholar]
- 31.Cheah WL, Wan WM, Manan A, Zabidihussin Z. A structural equation model of the determinants of malnutrition among children in rural Kelantan, Malaysia. Rural Remote Health. 2010;10(1):1248. [PubMed] [Google Scholar]
- 32.Hooper D, Coughlan J, Mullen M. Structural equation modeling: guidelines for determining model fit. Electron J Bus Res Methods. 2008;6:53–60. [Google Scholar]
- 33.Anderson JC, Gerbing DW. Structural equation modeling in practice: a review and recommended two-step approach. Psychol Bull. 1988;103(3):411–23. [Google Scholar]
- 34.Hair JF, Ringle CM, Sarstedt M. PLS-SEM: indeed a silver bullet. J Mark Theory Pract. 2011;19(2):139–152. [Google Scholar]
- 35.Anderson JC, Anderson JC, Gerbing DW, Gerbing DW. Structural equation modeling in practice: a review and recommended two-step approach. Psychol Bull. 1988;103(3):411–423. [Google Scholar]
- 36.Miles J. A framework for power analysis using a structural equation modelling procedure. BMC Med Res Methodol. 2003;3:27. doi: 10.1186/1471-2288-3-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wouters E, Heunis C, van Rensburg D, Meulemans H. Physical and emotional health outcomes after 12 months of public-sector antiretroviral treatment in the Free State Province of South Africa: a longitudinal study using structural equation modelling. BMC Public Health. 2009;9:103–111. doi: 10.1186/1471-2458-9-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gefen D, Straub D, Boudreau M. Structural equation modeling and regression: guidelines for research practice. Commun Assoc Inf Syst. 2000;4(7):1–78. [Google Scholar]
- 39.Byrne BM. Structural Equation Modeling With AMOS: Basic Concepts, Applications, and Programming, Second Edition. Routledge; 2013. [Accessed September 11, 2015]. webpage on the Internet. Available from: https://books.google.com/books?hl=en&lr=&id=0cHbAAAAQBAJ&pgis=1. [Google Scholar]
- 40.Briscoe C, Aboud F. Behaviour change communication targeting four health behaviours in developing countries: a review of change techniques. Soc Sci Med. 2012;75(4):612–621. doi: 10.1016/j.socscimed.2012.03.016. [DOI] [PubMed] [Google Scholar]
- 41.Chidrawi HC, Greeff M, Temane QM. Health behaviour change of people living with HIV after a comprehensive community-based HIV stigma reduction intervention in North-West Province in South Africa. SAHARA-J. 2014;11(1):222–232. doi: 10.1080/17290376.2014.985700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zomer TP, Erasmus V, van Empelen P, et al. Sociocognitive determinants of observed and self-reported compliance to hand hygiene guidelines in child day care centers. Am J Infect Control. 2013;41(10):862–867. doi: 10.1016/j.ajic.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 43.Jenner EA, Fletcher BC, Watson P, Jones FA, Miller L, Scott GM. Discrepancy between self-reported and observed hand hygiene behaviour in healthcare professionals. J Hosp Infect. 2006;63(4):418–422. doi: 10.1016/j.jhin.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 44.Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 45.Rosenstock IM. The health belief model: origins and correlates. Health Educ Monogr. 1974;2(4):336–353. doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- 46.Rogers RW. A protection motivation theory of fear appeals and attitude Changel. J Psychol. 1975;91(1):93–114. doi: 10.1080/00223980.1975.9915803. [DOI] [PubMed] [Google Scholar]
- 47.Rogers RW. Cognitive and physiological processes in attitude change: a revised theory of protection motivation. In: Cacioppo J, Petty R, editors. Soc Psychophysiol. New York: Guilford Press; 1983. pp. 153–176. [Google Scholar]
- 48.Witte K. Putting the fear back into fear appeals: the extended parallel process model. Commun Monogr. 1992;59(4):329–349. [Google Scholar]
- 49.Witte K. Fear as motivator, fear as inhibitor: using the extended parallel process model to explain fear appeal successes and failures. In: Andersen PA, Guerrero LK, editors. The Handbook of Communication and Emotion: Research, Theory, Applications, and Contexts. San Diego, CA: Academic Press; 1998. pp. 423–450. [Google Scholar]
- 50.Ajzen I. From intentions to actions: a theory of planned behavior. In: Kuhl J, Beckmann J, editors. Action-Control: From Cognition to Behavior. Heidelberg: Springer; 1985. pp. 11–39. [Google Scholar]
- 51.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. [Google Scholar]
- 52.Fuchs R. Causal models of physical exercise participation: testing the predictive power of the construct “pressure to change. J Appl Soc Psychol. 1996;26(21):1931–1960. [Google Scholar]
- 53.Rimal RN, Lapinski MK, Cook RJ, Real K. Moving toward a theory of normative influences: {How} perceived benefits and similarity moderate the impact of descriptive norms on behaviors. J Health Commun. 2005;10(5):433–450. doi: 10.1080/10810730591009880. [DOI] [PubMed] [Google Scholar]
- 54.Galavotti C, Cabral RJ, Lansky A, Grimley DM, Riley GE, Prochaska JO. Validation of measures of condom and other contraceptive use among women at high risk for HIV infection and unintended pregnancy. Health Psychol. 1995;14(6):570–578. doi: 10.1037//0278-6133.14.6.570. [DOI] [PubMed] [Google Scholar]
- 55.Rimal RN. Closing the knowledge - behavior gap in health promotion: the mediating role of self-efficacy. Health Commun. 2000;12(3):219–238. doi: 10.1207/S15327027HC1203_01. [DOI] [PubMed] [Google Scholar]
- 56.Estruch R, Ros E, Salas-Salvadó J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368:1279–1290. doi: 10.1056/NEJMc1806491. [DOI] [PubMed] [Google Scholar]
- 57.Balaguer Vintró I. Prevention of cardiovascular disease. Rev Clin Esp. 1987;180(1):38–42. [PubMed] [Google Scholar]
- 58.Capewell S, Graham H. Will cardiovascular disease prevention widen health inequalities? PLoS Med. 2010;7(8):e1000320. doi: 10.1371/journal.pmed.1000320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fleury J. The application of motivational theory to cardiovascular risk reduction. Image J Nurs Sch. 1992;24(3):229–239. doi: 10.1111/j.1547-5069.1992.tb00723.x. [DOI] [PubMed] [Google Scholar]
- 60.Strecher VJ, McEvoy DeVellis B, Becker MH, Rosenstock IM. The role of self-efficacy in achieving health behavior change. Health Educ Behav. 1986;13(1):73–92. doi: 10.1177/109019818601300108. [DOI] [PubMed] [Google Scholar]
- 61.Maibach E, Murphy DA. Self-efficacy in health promotion research and practice: conceptualization and measurement. Health Educ Res. 1995;10(1):37–50. [Google Scholar]
- 62.Chimoyi L, Tshuma N, Muloongo K, Setswe G, Sarfo B, Nyasulu PS. HIV-related knowledge, perceptions, attitudes, and utilisation of HIV counselling and testing: a venue-based intercept commuter population survey in the inner city of Johannesburg, South Africa. Glob Health Action. 2015;8:26950. doi: 10.3402/gha.v8.26950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tshuma N, Muloongo K, Chimoyi L, Setswe G, Sarfo B, Nyasulu P. Potential barriers to rapid testing for human immunodeficiency virus among a commuter population in Johannesburg, South Africa. HIV AIDS (Auckl) 2014;7:11–19. doi: 10.2147/HIV.S71920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Glasgow RE, Ory MG, Klesges LM, Cifuentes M, Fernald DH, Green LA. Practical and relevant self-report measures of patient health behaviors for primary care research. Ann Fam Med. 2005;3(1):73–81. doi: 10.1370/afm.261. [DOI] [PMC free article] [PubMed] [Google Scholar]