Supplemental Digital Content is available in the text.
Key Words: end of life, health care cost, health insurance, regional variation, palliative care, Switzerland
Abstract
Background:
Health care spending increases sharply at the end of life. Little is known about variation of cost of end of life care between regions and the drivers of such variation. We studied small-area patterns of cost of care in the last year of life in Switzerland.
Methods:
We used mandatory health insurance claims data of individuals who died between 2008 and 2010 to derive cost of care. We used multilevel regression models to estimate differences in costs across 564 regions of place of residence, nested within 71 hospital service areas. We examined to what extent variation was explained by characteristics of individuals and regions, including measures of health care supply.
Results:
The study population consisted of 113,277 individuals. The mean cost of care during last year of life was 32.5k (thousand) Swiss Francs per person (SD=33.2k). Cost differed substantially between regions after adjustment for patient age, sex, and cause of death. Variance was reduced by 52%–95% when we added individual and regional characteristics, with a strong effect of language region. Measures of supply of care did not show associations with costs. Remaining between and within hospital service area variations were most pronounced for older females and least for younger individuals.
Conclusions:
In Switzerland, small-area analysis revealed variation of cost of care during the last year of life according to linguistic regions and unexplained regional differences for older women. Cultural factors contribute to the delivery and utilization of health care during the last months of life and should be considered by policy makers.
Two factors characterize the Swiss health care system: high performance and high cost. Health care expenditures (HCE) accounted for 11.4% of the gross domestic product in 2012.1 Although advances in medicine contribute to raising health care costs, HCE are unevenly distributed across the life span and end of life (EOL) is often associated with sharp increases in spending on health in an aging poplation.2,3 A significant proportion of health care costs can be attributed to the care of EOL patients.4
Differences in the use of health care between providers and regions have been widely documented.5 However, documenting variation and identifying its causes is a nontrivial exercise.6 Not all variation is bad or unwarranted and its systematic, routine documentation at the local level is the first step in addressing inefficiency of resource allocation and overuse or underuse of services.5–8 Variation in intensity and cost of EOL care (EOLC) can be of particular importance in tracking regional differences in practice patterns.9,10
None of the previous Swiss EOLC studies11–16 has investigated small-area variation in costs despite the importance of understanding local practice patterns, identifying unwarranted variation, and informing policy makers and clinicians.5,7,9,10,17 Previous work in the United Kingdom and the United States either has not reported small-area variation in EOLC costs,18–20 or has used selected geographical locations19,21 or reported variation at the level of hospital referral regions.9,10 Such regions, however, similarly as cantons or language regions that are often conveniently used in Swiss health services research, are heterogenous in terms of population size and composition, do not reflect areas where care is actually delivered and may therefore be ill-suited for regional analyses.5,22–24 Furthermore, analytical approaches used by previous studies have largely failed to take into account the multilevel nature of data.25
We studied regional variation in cost of care during the last 12 months of life in Switzerland. We constructed a nationally representative dataset of cost of care and modelled small-area variation in cost. We identified individual and regional contextual factors and described how they shaped variation in cost. We hypothesized the existence of significant spatial variation in costs which is largely explained by individual and regional factors, including measures of health care supply.
METHODS
Study Design
This was a retrospective study based on routinely collected, Swiss health insurance claims data.
Study Setting
Switzerland is a small European federal republic of 26 cantons, situated among the Alps, the Swiss Plateau, and the Jura Mountains. The Swiss health care system is chiefly financed by mandatory health insurance (MHI) and out-of-pocket payments.1 The basic MHI package is compulsory for each Swiss resident and covers all essential benefits deemed medically and cost-appropriate that are related to illness and pregnancy26 (Text 1, SDC, Supplemental Digital Content 1, http://links.lww.com/MLR/B255).
Data Sources
We used anonymized MHI claims processed by 6 large companies that insure approximately 40% of the population (Table 1, SDC, Supplemental Digital Content 1, http://links.lww.com/MLR/B255). We included all individuals with MHI who died during a 3-year period between January 1, 2008 and December 31, 2010. Information on sex, age, date of birth and death, and place of residence were available. The Swiss Federal Statistical Office’s (SFSO) database of causes of death was probabilistically linked to insurance records to derive information on cause of death, nationality, civil status, and religion (Table 2, SDC, Supplemental Digital Content 1, http://links.lww.com/MLR/B255). On the basis of SFSO data, we also assessed representativeness of the study population. Characteristics of communities, supply of health care together with population denominator were derived from available sources.
Analytical Regions
We used 705 MedStat regions—the smallest delivery unit of health statistics—which SFSO constructs by aggregating postcodes to assure population threshold of approximately 10,000 residents. We further aggregated these into 564 custom regions (hereinafter referred to as regions) that best approximated SFSO’s boundaries of Swiss administrative communities and allowed linkage to other datasets. In total, 71 utilization-based hospital service areas (HSA) were created from discharge data of all Swiss hospitals in 2010 using methodology described elsewhere22 (Fig. 1, SDC, Supplemental Digital Content 1, http://links.lww.com/MLR/B255).
Study Population and Measures
We aggregated age into 5-year bands. Civil status was categorized as single, married, widowed, or divorced; nationality was recorded as Swiss or foreigner (including missing values); and religion was recorded as Protestant, Catholic, no affiliation, and other/unknown. Primary causes of death, coded according to the 10th revision of the International Statistical Classification of Diseases and Related Health Problems, were aggregated into 16 categories: breast cancer (women only, C50), prostate cancer (men, C61), colorectal cancer (C18–C21), lung cancer (C33–C34), other cancers (remaining C codes), heart failure27 (I50, I11.0, I13.0, I13.2, J81), stroke16 (I60–I69), coronary heart disease16 (I20–I25), other cardiovascular diseases (remaining I codes), chronic obstructive pulmonary disease28 (J40–J44, J47), other respiratory diseases (remaining I codes), dementia and Alzheimer’s29 (G30, G31.0, G31.82, G23.1, F00, F01, F02, F03, F05.1), other mental and behavioral disorders (remaining F codes), other diseases of the nervous system (remaining G codes), external causes (V00–V99, W00–W99, X00–X99, and Y00–Y99), and other.
Characteristics of regions of residence included level of urbanization (urban, periurban, rural) and language (German, French, Italian), both deriving from SFSO’s classification of communities; and quintiles of median area-based socioeconomic position (Swiss-SEP) index30 (Fig. 1, SDC, Supplemental Digital Content 1, http://links.lww.com/MLR/B255). Ambulatory care supply was measured by density of physicians per 10,000 inhabitants (regional level); acute care, as number of utilized hospital beds per 10,000 inhabitants (HSA level), and nonacute care as number of nursing home beds per 10,000 inhabitants 65 years and older (HSA level; all supply measures in quintiles).
Analyses
We used all reimbursed claims from the last 12 months of life to derive the overall cost of care for each person. We calculated frequencies and described cost [mean (SD), median, 25th and 75th percentiles] across characteristics and regions. We used individual-level data to fit multilevel regression models; regions of place of residence were nested within HSAs and the inverse hyperbolic sine31 transformed cost was the main outcome. In sensitivity analyses we used the last 3 months of life to derive costs.
Guided by previous Swiss EOLC studies,11,12,15,32 we assessed interaction of sex and a binary age indicator (19–65 y olds vs. those above 65 y) with remaining variables. We considered 4 models of increasing complexity: model 1, unadjusted; model 2, adjusted for age and cause of death; model 3, additionally adjusted for civil status, nationality, religion, level of urbanization, Swiss-SEP, and 3 supply measures; model 4, additionally adjusted for language region.
To quantify the degree to which individual and regional characteristics accounted for the observed regional cost variation, we compared variance estimates of regional cost variation across a sequence of models. We report the percentage of reduction in variance achieved in more complex models in comparison with the simplest model which included neither individual nor region or HSA-specific characteristics. Finally, based on the region-specific and HSA-specific coefficients we calculated for each region the ratio by which costs were higher or lower when compared with the national mean (cost ratios). Data management and analyses were performed in Stata version 14 (StataCorp LP, College Station, TX).
Ethics
Ethical approval was obtained from the Ethics Committee of the Canton of Bern.
RESULTS
Study Population
The initial dataset consisted of 119,613 individuals. We excluded 620 (0.5%) individuals below 19 years, 172 (0.1%) individuals who lived abroad, and 364 (0.3%) whose address was missing. The remaining population was probabilistically linked to 2008–2010 mortality data with 95.6% success rate; 5180 unlinked individuals were similar to the linked ones (Table 2, SDC, Supplemental Digital Content 1, http://links.lww.com/MLR/B255) and were excluded. The study population covered 61.3% of deaths in Switzerland between 2008 and 2010. The sex, age, nationality, civil status, level of urbanization, language region, Swiss-SEP and, most importantly, cause of death distributions were almost identical to overall mortality in that time period (Table 3, SDC, Supplemental Digital Content 1, http://links.lww.com/MLR/B255).
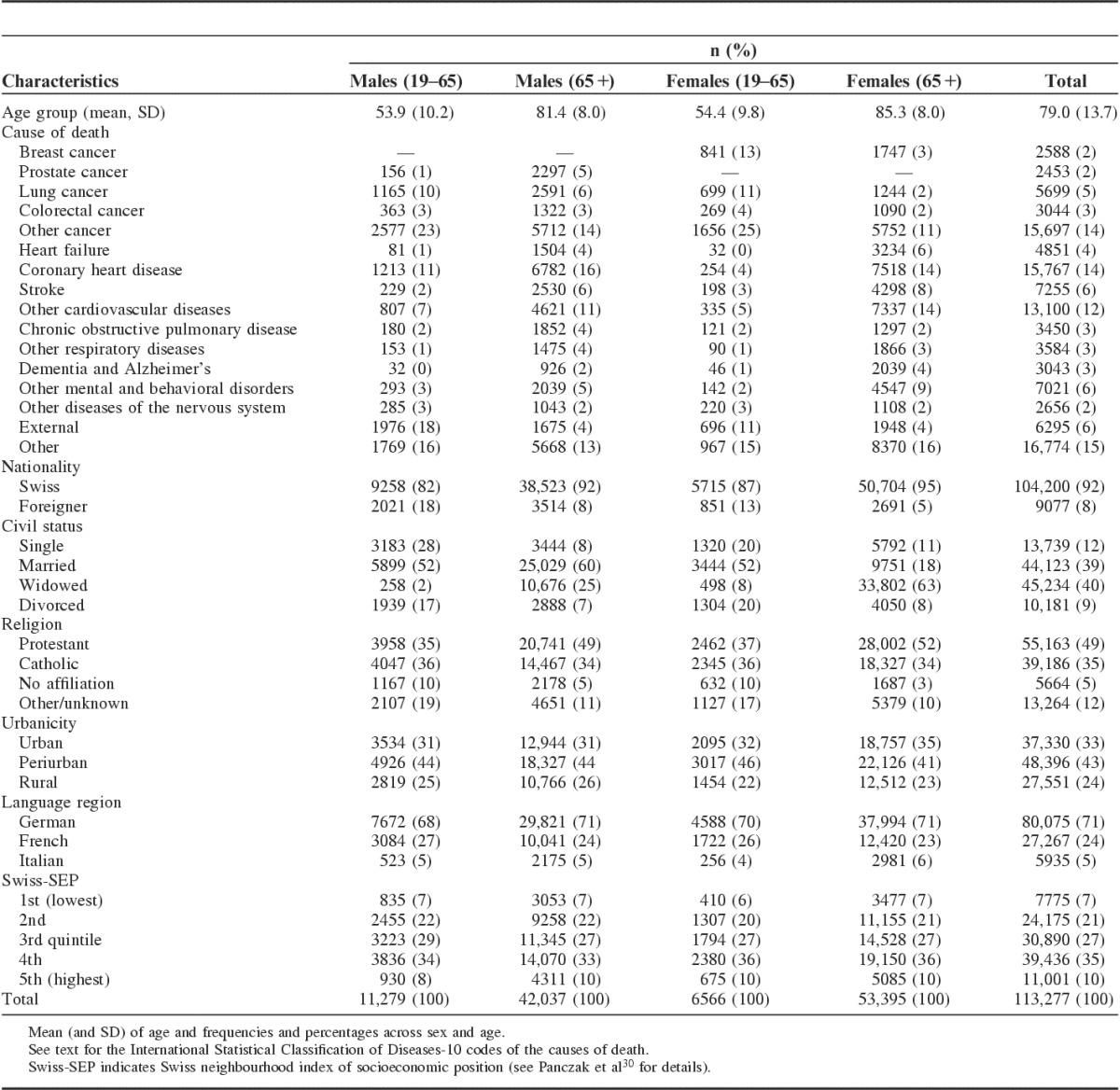
The final study population consisted of 113,277 individuals (Table 1). As expected, women were older at the time of death and main causes of death were cardiovascular diseases and cancers. Younger individuals were more likely to die of external causes than older persons. Study participants were mostly Swiss (92%), and either married (39%) or widowed (40%) at the time of death. The distribution across age and sex groups of religious affiliation, level of urbanization, and neighborhood SEP was similar.
TABLE 1.
Characteristics of the Study Population
Costs by Individual and Regional Characteristics
The mean cost of care during the last 12 months of life was 32.5k (thousand; SD, 33.2k) Swiss Francs (CHF; 1 CHF=0.90 Euro=1.01 US Dollar, as of May 19, 2016) (Table 4, SDC, Supplemental Digital Content 1, http://links.lww.com/MLR/B255). For both sexes, spending first tended to increase with age, and then decrease among the oldest age groups. Cancer deaths, especially colorectal, breast, and prostate cancers among younger individuals, were associated with the highest costs, followed by diseases of the nervous system and respiratory diseases. Coronary heart disease, external causes and, among younger individuals, mental and behavioral diseases generated, on average, lower costs. Costs tended to be higher among foreigners, married persons, and those resident in Latin-speaking parts of Switzerland, and areas of higher SEP. Costs were slightly lower in areas with a higher density of nursing home beds and lower density of hospital beds. Analyses of median cost showed similar trends (Table 5, SDC, Supplemental Digital Content 1, http://links.lww.com/MLR/B255).
Geographical Variation in Costs
There was a 7-fold variation in mean crude costs between regions (Fig. 1). We found evidence of interactions of sex and age with other variables (Table 6, SDC, Supplemental Digital Content 1, http://links.lww.com/MLR/B255). We thus used separate models for younger (aged 19–65) and older (66 and above) men and women. Sequentially including more individual and regional characteristics in the models gradually reduced cost variance at the HSA level (Fig. 2, SDC, Supplemental Digital Content 1, http://links.lww.com/MLR/B255). Model 2, which included only age and cause of death, reduced HSA-level variance by 46% for younger men and 21% for women, with smaller reductions achieved for older individuals (12% and 4%, respectively). In addition, including further individual and regional characteristics and health care supply measures resulted in a small additional reduction of cost variability at the HSA level (model 3). In contrast, also including language region resulted in a substantial reduction of HSA-level cost variability (model 4): compared with model 1 without any individual or regional characteristics, HSA-level variance was decreased by 95% for young males, 87% for females, 73% for older males, and 51% for females.
FIGURE 1.
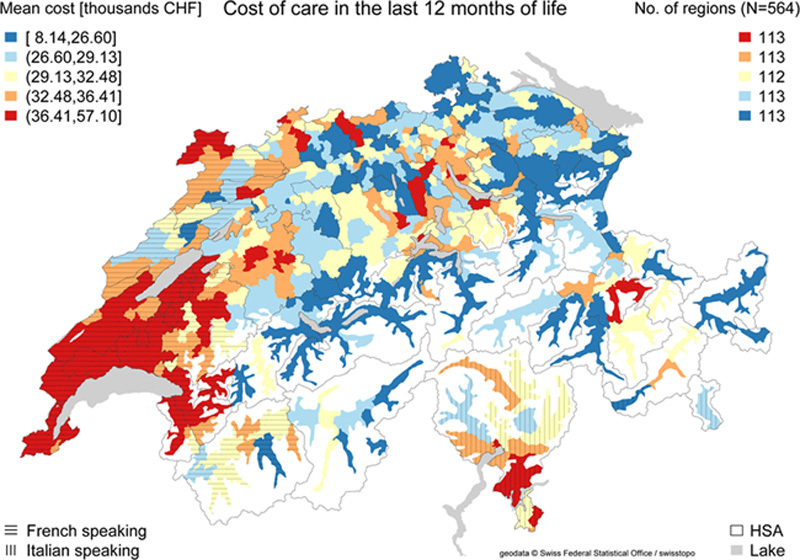
Mean cost [in 1000s Swiss Francs (CHF)] of care in the last 12 months of life among 113,277 individuals across 564 regions of place of residence, Switzerland 2008–2010. HSA indicates hospital service area.
After adjusting for age and cause of death (model 2), the highest cost ratios were observed in the western (French-speaking) parts of the country (regions around cities of Lausanne and Geneva), in canton Ticino (Italian-speaking), and in the large German-speaking cities (Basel, Bern, Zurich) (Figs. 2, 3, left columns; Fig. 3, SDC, Supplemental Digital Content 1, http://links.lww.com/MLR/B255 shows unadjusted estimates). Higher costs among older individuals were also present in parts of cantons Graubünden and Valais. In contrast, costs were lower in the valleys of the Alps and in central and north-western Switzerland. These differences remained in model 3 when adjusting for individual, regional, and care supply covariates (Fig. 4, SDC, Supplemental Digital Content 1, http://links.lww.com/MLR/B255) but were attenuated when also adjusting for language region (Figs. 2, 3, right columns). The largest spatial variation remained among older women and the smallest among young individuals. Higher costs, mainly among older individuals, were still present in and around large cities (Basel, Bern, Zurich) and in parts of Canton Vaud. A belt of lower costs stretched, in the north, from the cantons of Neuchatel to the canton of Thurgau (with the exception of Basel), and in the south along the Alps and the western part of Valais (particularly for older women). Importantly, regional level estimates of cost ratios varied within HSAs with neighboring regional estimates of both high and low cost ratios in cantons Bern, Geneva, and Zurich.
FIGURE 2.
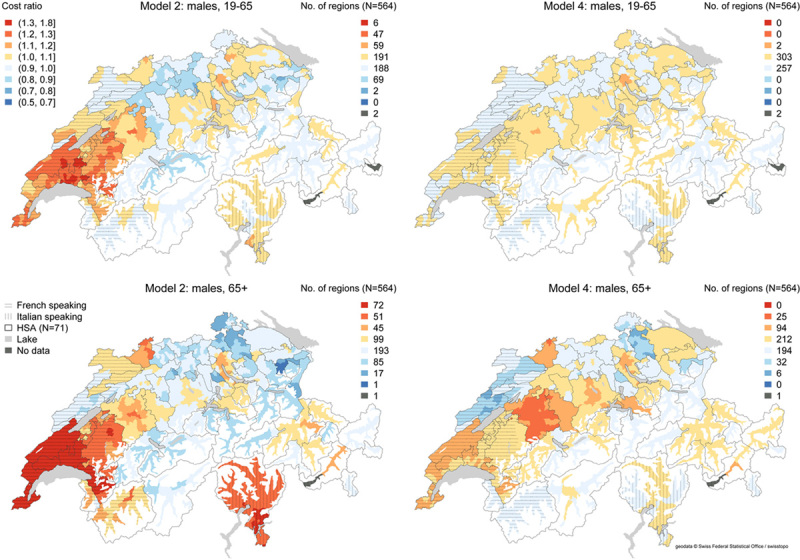
Spatial distribution of cost ratios adjusted for age and cause of death (model 2, left column) and fully adjusted (right column) for males. Regional values derived from exponentiated random effects across 564 regions of place of residence, nested within 71 hospital service areas (HSAs). Cost ratio represents the ratio by which regional costs are higher or lower when compared with the national mean; for instance, coefficient of 1.2 indicates 1.2 times (or 20%) higher cost.
FIGURE 3.
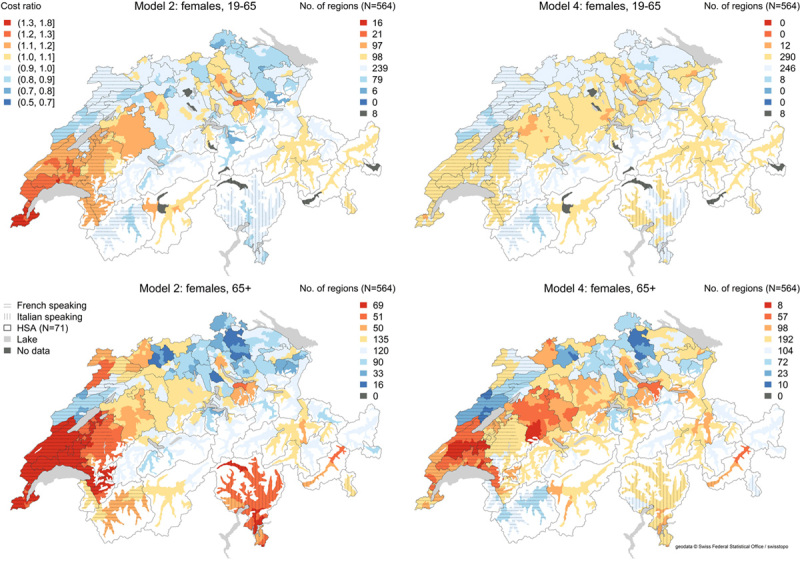
Spatial distribution of cost ratios adjusted for age and cause of death (model 2, left column) and fully adjusted (right column) for females. Regional values derived from exponentiated random effects across 564 regions of place of residence, nested within 71 hospital service area (HSAs). Cost ratio represents the ratio by which regional costs are higher or lower when compared with the national mean; for instance, coefficient of 1.2 indicates 1.2 times (or 20%) higher cost.
The estimates of the covariates changed little between models 2 and 4 (Tables 7–10, SDC, Supplemental Digital Content 1, http://links.lww.com/MLR/B255). The fully adjusted model 4 (Fig. 4; Table 10, SDC, Supplemental Digital Content 1, http://links.lww.com/MLR/B255) showed wide variation of cost across covariates. Adjusting for age, cause of death had the strongest associations. We found moderate effects of increased cost among individuals from French-speaking and Italian-speaking parts of Switzerland. Health care supply measures had little effect. Sensitivity analyses based on the last 3 months showed similar results (Table 11, Fig. 5, SDC, Supplemental Digital Content 1, http://links.lww.com/MLR/B255).
FIGURE 4.
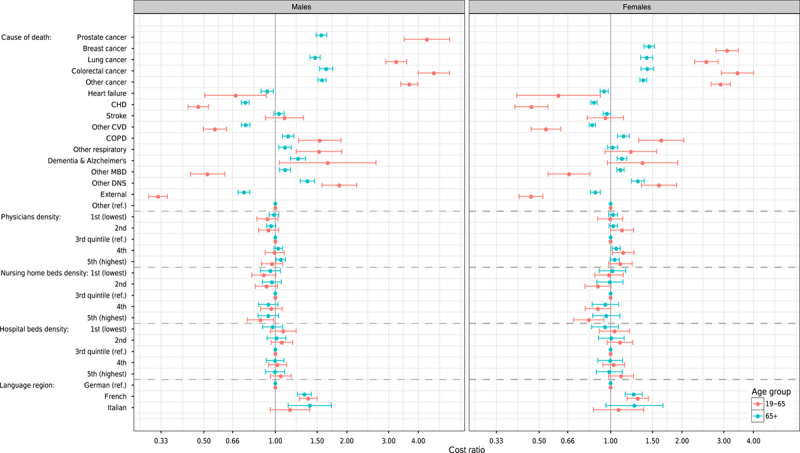
Association of cost of care in the last 12 months of life across selected covariates of model 4 (fully adjusted) across sex and age strata. Estimates additionally adjusted for age, civil status, nationality, religion, Swiss-SEP30 index, and level of urbanization. Exponentiated coefficients of regressing inverse hyperbolic sine31 transformed overall cost of care during the last 12 months of life representing cost ratios across analyzed variables. Cost ratio represents the ratio by which costs in specific category are higher or lower when compared with the national mean; for instance, coefficient of 1.2 indicates 1.2 times (or 20%) higher cost. All density of supply measures divided into quintiles of spatial units. CHD indicates coronary heart disease; CVD, cardiovascular disease; COPD, chronic obstructive pulmonary disease; DNS, diseases of the nervous system; MBD, mental and behavioral disorders; ref., reference category. See main text for International Statistical Classification of Diseases-10 codes of the causes of death. See Tables 7–10, Supplemental Digital Content 1, http://links.lww.com/MLR/B255 for exact estimates of coefficients across all covariates.
DISCUSSION
Main Findings
Studying geographical variation in cost of care in the last 12 months of life in Switzerland and assessing associations of costs with individual, regional, and health care supply factors, we found cause of death and age of the decedent to be the most important determinants at the individual level. We found that costs varied substantially between regions and these differences were only partly explained by confounders. Measures of care supply showed no associations with costs. When we included language region, the spatial variation was reduced substantially, but especially for elderly women, relevant differences between small regions remained.
Strengths
Our study was based on a large and comprehensive dataset of EOLC. Coverage and representativeness of the data allowed us to analyze, for the first time, regional variation in the cost of care during the last months of life. Earlier Swiss studies have used language regions11,16 or cantons12–14 to study regional variation in place of death and intensity of EOLC. But as this study demonstrated, cantons are heterogenous. Unlike other insurance-based studies from Switzerland,11,13,15 we included cause of death information and sociodemographic characteristics recorded on the death certificate. By using MHI claims data, we were able to cover the full range of care providers and include costs from ambulatory, inpatient, and nonacute settings. We evaluated influence of supply measures using utilization-based areas, which are better suited for this purpose than administrative units.7,22,23
Relation to Other Studies
Our findings of HCE during the last 12 months of life are comparable with previous Swiss studies. Von Wyl et al15 estimated the median cost to be 30.3k CHF for individuals aged 65 and above during the last 12 months of life, whereas the cost of the last 6 months of life for the general population determined by Reich et al11 was 17.7k CHF. These costs are considerably higher than the mean annual HCE among the general population in Switzerland, which is about 3.5k CHF33; and 6.7k CHF per year for persons aged 65 and above.32 Similar differences between the general and EOL populations have been reported in the United States.34 Both the Swiss and the American data reinforce the large economic burden EOLC places on the health care system.
We found evidence for large geographic variation in cost, yet were unable to completely explain its causes. Similarly as in the United States, the cause of death, sex, and age played an important role in determining costs on the individual level,8,20 but these variables did not explain the substantial spatial variation in costs, particularly among older females. Nevertheless, the effect of language region suggests that regional differences in volume and type of care could be factors. We know the differences across Swiss cantons in overall cost of care,35,36 overall number of hospitalizations,5,37 and intensity of EOLC of cancer patients.12–14 Language region was also associated with treatment intensity in ambulatory settings.38 These findings overlap with ours: costs were higher in many regions of French-speaking and Italian-speaking Switzerland. More people died in the hospital than at home or in a nursing home in French-speaking and Italian-speaking cantons, and as hospital deaths tend to cost more this may be a partial explanation.11,14,16 Doctors’ EOL decisions also vary across cultural regions. Fischer and colleagues demonstrated, for instance, that French-speaking physicians were more likely to manage pain and symptoms aggressively, but were less willing than their German-speaking colleagues to comply with patients’ wishes of minimal or no treatment.39 We found no association of costs with urbanization, but after adjustment we found increased EOL costs in and around the biggest cities. This has been reported earlier using Scottish data in which it was suggested that differences in case-mix and clinical practice increase cost in large urban centers.18 In addition, in Switzerland, deaths at home, which are associated with lower cost, are more common in rural areas, which might explain part of this pattern.11
Health care supply was not associated with costs and did not influence geographic variation. Density of physicians was associated with EOLC intensity in the United States9,10 as were intensity and cost of general health care in Switzerland in earlier studies.17,35,38 However, these studies used data aggregated over large regions7 or lacked adjustment for individual-level characteristics,8,20 which might have influenced their results. Similarly, hospital bed density was not associated with cost of care, which resembles previous results from Switzerland,40 but not from the United States.9,10,41,42 Again, these studies used relatively large spatial units that could have partly masked regional variation.7 It is also important to point out that the Swiss health care system can be regarded as a fee-for-service system in which suppliers may respond quickly to meet high demand, thus making the effect of supply measures weaker than that in studies from other countries. Alternatively, our results may indicate that the mechanisms of supply-induced care do not operate in EOLC in Switzerland.
Implications
Previous studies tracked variation in EOLC cost in Switzerland across place of death11 and across time.15 This study adds regional analyses, which can be used to involve stakeholders and guide future EOLC studies in Switzerland. Geographical variation in prevailing type of EOLC, the coverage and strength of palliative care institutions, or family and social support may be important determinants of cost. High EOLC cost might not only indicate potential waste of resources, but also potential overuse of costly hospital-based services instead of appropriate palliative care.21 Moreover, past EOLC spending in a region might be used as an exposure in studies tracking variation in other areas of health care.9
Supply of care did not seem to play a role; however, we did identify significant variation that may indicate underuse or overuse of services. But if regions that spend more offer better quality of care and have higher patient satisfaction, the rest of the country should follow suit. If future research finds that this is not the case, then the areas highlighted by our findings should become the focus of regionally tailored interventions. Finally, regional findings may point to different patient preferences between regions. If meeting these preferences, independent of medical needs, is considered a valid social goal,42 then substantial variation in cost of care in the last months of life in Switzerland will persist.
The results of this study align with previous findings and point to the importance of assessing utilization and spending patterns at the local level.7 Large spatial units could be heterogenous and too crude for planning policies. In addition, we found that cost of care was associated with language region; countries with culturally diverse populations and regions should consider these findings in future studies. Finally, our methodology and findings could contribute to understanding HCE in countries with similar health care organization and demographics in which the extent of variation has been documented, but the studies of its determinants are still scarce.
Limitations
Studies based on health insurance claims contain limited patient-level information. Quality or appropriateness of care are also difficult to measure from administrative data. We supplemented this data by linking to other sources, but important aspects of cost determinants may not be included; for instance, we could not include measures of illness severity,43 patient and family preferences,42,44 functional status,3 presence of relative nearby,45 or place of death.16 Second, overall cost is only one possible outcome in analyses of EOLC,43,46,47 so our ongoing analyses will aim at disaggregating costs across providers and exploring alternative measures of intensity of care. Third, focusing on the last 12 months of life is an arbitrary choice and can only be considered a proxy for EOLC, as it might include unrelated costs.48 However, it is also one of the most frequently used timeframes and facilitates comparability with other studies. A retrospective design efficiently identifies dying patients so we could construct large representative datasets. Our study does not suffer from inaccurate prognostication of survival and incomplete enrolment of patients. Langton et al47 describe 2 retrospective and prospective cancer EOLC studies with comparable results.49,50 Our sensitivity analyses indicated that shorter timeframe of 3 months provided similar results. Fourth, relying only on MHI claims could cause us to underestimate overall cost. Our estimates do not include costs covered by supplementary insurance, claims paid directly by patients, or costs not delivered to insurers.11,32 About 50% of inpatient costs are subsidized by cantons and MHI pays only about 18% of costs of nursing home stays (mainly for medical treatments).15 Our sensitivity analyses showed that while monetary cost understandably increases when we use cost corrected for cantonal subsidies of hospital care and differences in tariffs for reimbursement of ambulatory care (TARMED),2 the direction and strength of the associations were unaffected (Table 12, Fig. 6, SDC, Supplemental Digital Content 1, http://links.lww.com/MLR/B255).
CONCLUSIONS
MHI claims data show that in Switzerland HCE in the last months of life vary strongly across regions, particularly among older individuals. The effect of language region might indicate that the organization of EOLC differs between cultural regions. However, supply of care does not seem to play a major role. In light of the 2012 Swiss-wide changes to a new inpatient reimbursement system, this study provides a baseline for tracking the effects of these changes on EOLC. Future Swiss and international studies should take into account cultural factors of delivery and utilization of health care.
Supplementary Material
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website, www.lww-medicalcare.com.
ACKNOWLEDGMENTS
The authors are extremely grateful to the insurance companies that were part of the study—CSS, Groupe Mutuel, Helsana, Sanitas, SWICA, and Visana. They provided us with the data used in the study and offered helpful comments at the stage of data management. The authors also express their gratitude to the Swiss Medical Association (FMH) for providing data on number of Swiss physicians. Original idea, obtaining funding, and data and exploratory analyses were undertaken by André Busato, who deceased on November 12, 2013. The authors thank Kali Tal and Christopher Ritter for their editorial contributions and Greg Werbin for his helpful comments.
Footnotes
Supported by funds from Swiss National Science Foundation (grant number 406740_1393333) and by the joint grant of Swiss Medical Association (FMH), Konferenz der Kantonalen Ärztegesellschaften (KKA) and NewIndex AG.
Preliminary version of findings shown in this manuscript were presented at the 2014 Wennberg International Collaborative meeting in London, UK; GEOMED 2015 Conference in Florence, Italy; and Swiss Public Health Conference 2015, Geneva, Switzerland.
The authors declare no conflict of interest.
REFERENCES
- 1.Biller-Andorno N, Zeltner T. Individual responsibility and community solidarity—The Swiss Health Care System. N Engl J Med. 2015;373:2193–2197. [DOI] [PubMed] [Google Scholar]
- 2.Organisation for Economic Cooperation and Development. OECD Reviews of Health Systems: Switzerland, 2011.
- 3.Rosella LC, Fitzpatrick T, Wodchis WP, et al. High-cost health care users in Ontario, Canada: demographic, socio-economic, and health status characteristics. BMC Health Serv Res. 2014;14:532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Felder S, Meier M, Schmitt H. Health care expenditure in the last months of life. J Health Econ. 2000;19:679–695. [DOI] [PubMed] [Google Scholar]
- 5.Organisation for Economic Cooperation and Development. Geographic variations in health care: what do we know and what can be done to improve health system preformance? OECD Health Policy Studies. 2014.
- 6.Corallo AN, Croxford R, Goodman DC, et al. A systematic review of medical practice variation in OECD countries. Health Policy. 2014;114:5–14. [DOI] [PubMed] [Google Scholar]
- 7.Zhang Y, Baik SH, Fendrick AM, et al. Comparing local and regional variation in health care spending. N Engl J Med. 2012;367:1724–1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zuckerman S, Waidmann T, Berenson R, et al. Clarifying sources of geographic differences in Medicare spending. N Engl J Med. 2010;363:54–62. [DOI] [PubMed] [Google Scholar]
- 9.Fisher E, Wennberg D, Stukel T. The implications of regional variations in medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138:273–311. [DOI] [PubMed] [Google Scholar]
- 10.Fisher E, Wennberg D, Stukel T. The implications of regional variations in spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003;138:288–298. [DOI] [PubMed] [Google Scholar]
- 11.Reich O, Signorell A, Busato A. Place of death and health care utilization for people in the last 6 months of life in Switzerland: a retrospective analysis using administrative data. BMC Health Serv Res. 2013;13:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matter-Walstra KW, Achermann R, Rapold R, et al. Delivery of health care at the end of life in cancer patients of four Swiss cantons: a retrospective database study (SAKK 89/09). BMC Cancer. 2014;14:306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matter-Walstra KW, Achermann R, Rapold R, et al. Cancer-related therapies at the end of life in hospitalized cancer patients from four Swiss cantons: SAKK 89/09. Oncology. 2015;88:18–27. [DOI] [PubMed] [Google Scholar]
- 14.Matter-Walstra KW, Achermann R, Rapold R, et al. Days spent in acute care hospitals at the end of life of cancer patients in four Swiss cantons: a retrospective database study (SAKK 89/09). Eur J Cancer Care (Engl). 2016. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 15.von Wyl V, Telser H, Weber A, et al. Cost trajectories from the final life year reveal intensity of end-of-life care and can help to guide palliative care interventions. BMJ Support Palliat Care. 2015. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 16.Hedinger D, Braun J, Zellweger U, et al. Moving to and dying in a nursing home depends not only on health—an analysis of socio-demographic determinants of place of death in Switzerland. PLoS One. 2014;9:e113236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Camenzind P. Explaining regional variations in health care utilization between Swiss cantons using panel econometric models. BMC. Health Serv Res. 2012;12:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Geue C, Wu O, Leyland A, et al. Geographic variation of inpatient care costs at the end of life. Age Ageing. 2016;1(i):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guadagnolo BA, Liao K-P, Giordano SH, et al. Variation in intensity and costs of care by payer and race for patients dying of cancer in Texas: an analysis of registry-linked medicaid, medicare, and dually eligible claims data. Med Care. 2015;53:591–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reschovsky JD, Hadley J, Romano PS. Geographic variation in fee-for-service medicare beneficiaries’ medical costs is largely explained by disease burden. Med Care Res Rev. 2013;70:542–563. [DOI] [PubMed] [Google Scholar]
- 21.Kaplan RM. Variation between end-of-life health care costs in Los Angeles and San Diego: why are they so different? J Palliat Med. 2011;14:215–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Klauss G, Staub L, Widmer M, et al. Hospital service areas—a new tool for health care planning in Switzerland. BMC Health Serv Res. 2005;5:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goodman DC, Mick SS, Bott D, et al. Primary care service areas: a new tool for the evaluation of primary care services. Health Serv Res. 2003;38(1p1):287–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jackson AL, Davies Ca, Leyland AH. Do differences in the administrative structure of populations confound comparisons of geographic health inequalities? BMC Med Res Methodol. 2010;10:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krumholz HM, Brindis RG, Brush JE, et al. Standards for statistical models used for public reporting of health outcomes: an American Heart Association Scientific Statement from the Quality of Care and Outcomes Research Interdisciplinary Writing Group. Circulation. 2006;113:456–462. [DOI] [PubMed] [Google Scholar]
- 26.Thomson S, Busse R, Crivelli L, et al. Statutory health insurance competition in Europe: a four-country comparison. Health Policy. 2013;109:209–225. [DOI] [PubMed] [Google Scholar]
- 27.Pivodic L, Pardon K, Morin L, et al. Place of death in the population dying from diseases indicative of palliative care need: a cross-national population-level study in 14 countries. J Epidemiol Community Health. 2015;70:17–24. [DOI] [PubMed] [Google Scholar]
- 28.López-Campos JL, Ruiz-Ramos M, Soriano JB. Mortality trends in chronic obstructive pulmonary disease in Europe, 1994-2010: a joinpoint regression analysis. Lancet Respir Med. 2014;2:54–62. [DOI] [PubMed] [Google Scholar]
- 29.Teipel S, Fritze T, Ovari A, et al. Regional pattern of dementia and prevalence of hearing impairment in Germany. J Am Geriatr Soc. 2015;63:1527–1533. [DOI] [PubMed] [Google Scholar]
- 30.Panczak R, Galobardes B, Voorpostel M, et al. A Swiss neighbourhood index of socioeconomic position: development and association with mortality. J Epidemiol Community Health. 2012;66:1129–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Burbidge JB, Magee L, Robb AL. Alternative transformations to handle extreme values of the dependent variable. J Am Stat Assoc. 1988;83:123–127. [Google Scholar]
- 32.Bähler C, Huber CA, Brüngger B, et al. Multimorbidity, health care utilization and costs in an elderly community-dwelling population: a claims data based observational study. BMC Health Serv Res. 2015;15:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huber CA, Schneeweiss S, Signorell A, et al. Improved prediction of medical expenditures and health care utilization using an updated chronic disease score and claims data. J Clin Epidemiol. 2013;66:1118–1127. [DOI] [PubMed] [Google Scholar]
- 34.Lunney JR, Lynn J, Hogan C. Profiles of older medicare decedents. J Am Geriatr Soc. 2002;50:1108–1112. [DOI] [PubMed] [Google Scholar]
- 35.Schleiniger R. Health care cost in Switzerland: quantity- or price-driven? Health Policy. 2014;117:83–89. [DOI] [PubMed] [Google Scholar]
- 36.Reich O, Weins C, Schusterschitz C, et al. Exploring the disparities of regional health care expenditures in Switzerland: some empirical evidence. Eur J Health Econ. 2012;13:193–202. [DOI] [PubMed] [Google Scholar]
- 37.Pellegrini S, Kohler D, Otto S. Variations géographiques dans les soins de santé. La situation en Suisse [Geographical variations in health care. The situation in Switzerland] (Obsan Dossier 42). Neuchâtel; 2014. Available at: http://www.obsan.admin.ch/sites/defaul//files/publications/2015/obsan_dossier_42.pdf. Accessed August 12, 2016.
- 38.Busato A, Künzi B. Primary care physician supply and other key determinants of health care utilisation: the case of Switzerland. BMC Health Serv Res. 2008;8:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fischer S, Bosshard G, Faisst K, et al. Swiss doctors’ attitudes towards end-of-life decisions and their determinants: a comparison of three language regions. Swiss Med Wkly. 2006;136:370–376. [DOI] [PubMed] [Google Scholar]
- 40.Crivelli L, Filippini M, Mosca I. Federalism and regional health care expenditures: an empirical analysis for the Swiss cantons. Health Econ. 2006;15:535–541. [DOI] [PubMed] [Google Scholar]
- 41.Pritchard RS, Fisher ES, Teno JM, et al. Influence of patient preferences and local health system characteristics on the place of death. J Am Geriatr Soc. 1998;46:1242–1250. [DOI] [PubMed] [Google Scholar]
- 42.Baker L, Bundorf K, Kessler D. Patients’ preferences explain a small but significant share of regional variation in medicare spending. Health Aff. 2014;33:957–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Neuberg GW. The cost of end-of-life care: a new efficiency measure falls short of AHA/ACC standards. Circ Cardiovasc Qual Outcomes. 2009;2:127–133. [DOI] [PubMed] [Google Scholar]
- 44.Kelley AS, Morrison RS, Wenger NS, et al. Determinants of treatment intensity for patients with serious illness: a new conceptual framework. J Palliat Med. 2010;13:807–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kelley AS, Ettner SL, Morrison RS, et al. Determinants of medical expenditures in the last 6 months of life. Ann Intern Med. 2011;154:235–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Luta X, Maessen M, Egger M, et al. Measuring intensity of end of life care: a systematic review. PLoS One. 2015;10:e0123764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Langton JM, Blanch B, Drew AK, et al. Retrospective studies of end-of-life resource utilization and costs in cancer care using health administrative data: a systematic review. Palliat Med. 2014;28:10. [DOI] [PubMed] [Google Scholar]
- 48.Bach PB, Schrag D, Begg CB. Resurrecting treatment histories of dead patients. A study design that should be laid to rest. JAMA. 2004;292:2765–2770. [DOI] [PubMed] [Google Scholar]
- 49.Setoguchi S, Earle CC, Glynn R, et al. Comparison of prospective and retrospective indicators of the quality of end-of-life cancer care. J Clin Oncol. 2008;26:5671–5678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pyenson B, Connor S, Fitch K, et al. Medicare cost in matched hospice and non-hospice cohorts. J Pain Symptom Manage. 2004;28:200–210. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website, www.lww-medicalcare.com.


