Abstract
Context:
Health care environments have been changing rapidly, and one of the changes is to emphasize patient satisfaction. However, most studies assume that all patients integrate their health care attribute reactions in the same way to arrive at their satisfaction.
Objective:
The objective of this study is to investigate how patients’ experience of pain influences their attribute reaction integration process and their overall rating of the hospital.
Design:
Patient satisfaction data were collected using a mailed questionnaire. Multiple linear regression analyses with a dichotomous (yes/no) pain variable and its interaction effects with nursing care, physician care, staff care, and hospital room were conducted with control variables.
Main Outcome Measures:
The pain variable was statistically significant and also revealed interaction effects with the physician care and the staff care variables in the model. Patients who needed medicine for pain showed lower overall rating of the hospitals than patients who did not need medicine.
Results:
The statistically significant interaction effects indicate that for patients who needed medicine for pain, staff care becomes more important and physician care becomes less important compared to patients who do not need medicine for pain. All 4 attributes (nursing care, physician care, staff care, and hospital room) are not equally influential.
Conclusion:
Implementing policies and procedures related to these interaction effects would lead to the most efficient and effective improvement outcomes. These findings suggest that future policies should be modified to enhance nursing and staff care to provide more direct care for patients with pain.
Keywords: quality improvement, managerial epidemiology, pain management, patient centeredness, practice management
Introduction
The US health care system is a dynamic entity with many complex aspects and many different stakeholders. The health care expenditures have been increasing, and consequently, there have been many cost-containment measures. Despite these efforts, the quality of health care needs to be improved. The quality of care can be defined differently, but one of the common measures of health care quality consistently includes patient satisfaction.
As health care environments have been changing rapidly in recent years, there has been a greater emphasis on the importance of measuring patient satisfaction. This concern has been accelerated by the advent of the Affordable Care Act that mandated a tie between reimbursement and patient satisfaction. A higher patient satisfaction level leads to a higher reimbursement rates. Earlier patient satisfaction studies examined patients’ characteristics such as age, gender, race, and education.1 Although these studies were informative in demonstrating sociodemographic and socioeconomic disparities in patient satisfaction, it is not possible to develop an intervention program to change these variables. Other studies aimed at improving the psychometric properties of the patient satisfaction surveys.2,3 These studies focused on the validity and the reliability of the patient satisfaction surveys and contributed to the development of the Consumer Assessment of Healthcare Providers and Systems (CAHPS). Recent patient satisfaction studies analyzed how patients combine their attribute reactions to arrive at their overall satisfaction.4,5 Most patient satisfaction studies assume that all patients integrate their health care attribute reactions in the same way to arrive at their satisfaction. There are only a few studies that address the need to analyze subgroups of patients.6 Surprisingly, one of the clinical areas that has had limited investigation is noninstitutionalized patients who have chronic pain. Further, very few studies have examined satisfaction with the hospital stay among patients with pain, and most have been done with such patients in an outpatient setting. One exception was a study by Kroenke et al who examined the extent to which self-reported physical symptoms (which included pain as one of several variables combined into a symptom severity index) among 2126 hospital medical patients were associated with satisfaction with care.7 Patient satisfaction with care was associated with symptom severity score at discharge and degree of symptomatic improvement that occurred during hospitalization.
Over 100 million Americans have chronic pain each year.8 Pain is defined as a sharp or a dull feeling triggered in the nervous system. The feeling may be sporadic or persistent. Although pain can be successfully controlled, it continues to be a significant problem for a large number of hospital patients, and the experience of pain detrimentally affects the patients’ well-being. The costs of unrelieved pain include extended hospital stays, higher rates of rehospitalization, decreased earning potential of patients due to inability to work, and decreased overall health. Pain costs approximately US$635 billion annually in medical treatment and lost productivity.8 In fact, pain medications are the second most prescribed class of drugs (after cardiac–renal drugs).9
With patients commonly experiencing pain, increased attention is needed for how to effectively manage pain symptoms to improve the patients’ health and satisfaction with care. Patients with pain tend to report lower overall levels of health in comparison to their counterparts without pain.10 Because patients experience pain differently, it is difficult to develop a routine procedure to improve patient satisfaction. However, interdisciplinary teams working together to alleviate pain can enhance patient care. Physical symptoms that lead to substantial morbidity are associated with decreased satisfaction with care.7 Physical symptoms such as chronic pain can lower the patient’s experience within a medical clinic due to worsened emotional and mental status.11 A few studies have found that particular attributes, that is, nursing staff, physician care, and room and staff care excluding nursing, of a hospital are associated with patient satisfaction. For instance, a caring nursing staff enhances patient satisfaction.12 Hospitals can improve their patients’ satisfaction by dedicating appropriate staff resources to improve pain management. Indeed, the patient–provider relationship can positively affect the patient’s experience.13 Another study conducted by Bhakta and Marco found that there was a significant association between patient satisfaction and a reduction in pain among adults in an emergency department.14
These studies suggest the role of pain and the importance of pain care on patient satisfaction. However, to date, there has been no study that analyzes how patients with pain combine their attribute reactions differently from patients without pain. The influential levels of certain attributes on patient satisfaction may be different between patients with pain and patients without pain. This study investigates these possible different combining processes for patients with pain and without pain to arrive at their overall satisfaction.
Theoretical and Conceptual Framework
After patients are discharged from a hospital, they often receive a patient satisfaction survey to complete regarding their experiences during their hospitalization. Data from these surveys can provide important insights into hospital managers to identify mechanisms to improve the quality of care delivered to patients. Certainly, some experiences (aspects) are positive, whereas others may be less positive or even negative. The question is “How do they arrive at their overall satisfaction given these multiple experiences?” Arguably, one of the most well-known customer satisfaction theories that is relevant to this patient satisfaction study is the Fishbein model.15 This model would explain that patients combine salient attribute reactions (experiences) to arrive at their overall satisfaction. Each attribute has a different weight (influential level), and thus, an attribute with a larger weight influences more than an attribute with a smaller weight on overall satisfaction. In addition, a good performance of an attribute can compensate for a weak performance of another attribute. The Fishbein model would suggest that to achieve maximum improvement in overall satisfaction, we should improve an attribute with a larger weight.
Pain in this study is measured with 1 question, “Did you need medicine for pain?” It is presumed that if patients need medicine for pain, they have pain. For analyses, it is possible to split the patient satisfaction data into 2 data sets: one with patients having pain and the other with patients having no pain and analyze them separately. However, this method would substantially limit the sample size and would make it difficult to examine statistically how patients with pain combine their attribute reactions differently from patients without pain. Thus, this study utilizes the entire sample. By capitalizing on the entire sample, it is possible to explore the interaction effects between attribute reactions and pain on overall patient satisfaction (overall rating) by creating a product term of each attribute reaction (nursing care × presence of pain, physician care × presence of pain, staff care × presence of pain, and room × presence of pain) and pain.
Methods
Data Source
This study utilized patient satisfaction data collected from 70 hospitals representing a large, national, private, not-for-profit hospital system. The data were collected as part of the public reporting of patient experience data known as the Consumer Assessment of Healthcare Providers and Systems, Hospital version (HCAHPS), a well-established and widely respected used instrument. The Agency for Healthcare Research and Quality (AHRQ) in the Department of Health and Human Services developed HCAHPS. The AHRQ had RAND Corporation, Harvard Medical School, and American Institutes for Research to carry out a rigorous, scientific process to develop and validate the HCAHPS instrument, and the results (psychometric properties including validity and reliability, credibility, usefulness, etc) have been confirmed and published elsewhere.16,17 The 70 hospitals are largely located in the midwest, southeast, south, northwest, and northeast and represent a range of hospitals in size, services, and geography. Critical access, community, and tertiary hospitals are represented in the data set. Data were collected through a multiwave mailed survey. Patients discharged from one of the hospitals were randomly selected and received the HCAHPS survey (generally within a week) in the mail and responded directly to the survey vendor. The survey vendor compiled the raw data and sent a data set to the health system’s central office. The average overall response rate was 40%. This high response rate was achieved through the multiwave survey technique. This study utilized the data collected between July 1, 2011, and June 30, 2012, and analyzed patients who are aged 18 years and older.
Measures
The dependent variable in this study is measured by a single item that measures the overall rating of the hospital, ranging from 0 being the worst hospital possible to 10 being the best hospital possible. Patients’ experience can be assessed using the 4 key independent variables—“nursing care,” “physician care,” “staff care,” and “hospital room.” Each of these 4 independent variables is considered to be a construct and is created with multiple survey items with a 4-point Likert-type scale (always: 4, usually: 3, sometimes: 2, and never: 1) that measures the same construct. Specifically, each of the 4 independent variables (composite indexes) was calculated as an arithmetic mean of the items in the same construct. A representative item for the nursing care is as follows: “How often did nurses treat you with courtesy and respect?” The pain variable is a dichotomous item asking whether a patient needed medicine for pain (1 = yes and 0 = no). The interaction effects were analyzed by creating a product term for each independent variable as follows: nursing care × presence of pain, physician care × presence of pain, staff care × presence of pain, and room × presence of pain. Control variables include gender, age, educational attainment, and race. The age variable is an ordinal scale such as 25 to 29, 30 to 24, … 90 years or older. The educational attainment variable is also an ordinal scale such as complete the eighth grade or less, complete some high school but did not graduate, graduate from high school or earn a general educational development (GED), complete some college or earn a 2-year degree, graduate from a 4-year college, and complete more than 4-year college degree. The race variable is a dichotomous dummy variable for each race, and white is used as the reference racial group.
Analysis
This study analyzed how patients with pain combined their attribute reactions differently from patients without pain while controlling for their gender, age, educational attainment, and race. The different combining processes of patients with and without pain were assessed with the significance levels of the coefficients of the product terms. The general multiple regression model used in this study is shown together with the interaction effects and the control variables as follows:
where Y is the dependent variable, a is the intercept, b is a coefficient, X is an attribute reaction, P is the pain variable, and e is the error term. The first 2 terms of the right-hand side of the equation together with the error term are always used in a linear regression model, and the third term is an interaction effect. If the coefficient of the interaction effect is statistically significant, there is a difference between patients with and without pain for that attribute when they combine their attribute reactions. Throughout this study, an α = .05 is used to test the significance level.
Results
There were 36 528 cases for the analysis, of which 13 020 cases were male patients and 22 431 cases were female patients. Regarding race, white patients accounted for most of the cases, 31 001 (84.9%), followed by African American 4856 (13.3%), Asian 432 (1.2%), American Indian/Alaskan Native 217 (0.6%), and Native Hawaiian/Pacific Islander 22 (0.1%). As for pain, 10 269 (28.1%) patients were without pain and 26 259 (71.9%) patients were with pain, indicating there are many more patients with pain than patients without pain.
The age and educational attainment variables were both measured at the ordinal level. There are more patients in the age-groups of 55 to 59 years (3337 cases, 9.1%), 60 to 64 years (3787 cases, 10.4%), 65 to 69 years (4139 cases, 11.3%), and 70 to 74 years (3821 cases, 10.5%). The educational attainment variable shows 2 adjacent large groups “graduate from high school or earn a GED” (11 441 cases, 31.3%) and “complete some college or earn a 2-year degree” (11 104 cases, 30.4%).
The descriptive results for the survey items and composite indexes together with the descriptions of all survey items are shown in the Table 1. All survey items in the nursing care, physician care, staff care, and room attributes show positive patient responses ranging from 3.03 to 3.85, with a score of “4” indicating the strongest level of rating. Among the 4 attributes (composite indexes), nursing care shows the highest of 3.7604 (in Table 1, it shows 3.76), followed by physician care (3.7598), staff care (3.59), and room (3.55). The dependent variable of “overall rating of the hospital” has a mean of 9.00 (range: 0-10, with 10 representing the best possible score) and a standard deviation of 1.553. Note that the number of cases (N) for any composite indexes is always larger than the number of cases for any item in the same attribute because the composite index score was computed as long as patients responded to at least 1 item in the attribute.
Table 1.
Descriptive Statistics of Survey Items and Composite Indexes.
| N | Mean | SD | Description | |
|---|---|---|---|---|
| Nursing care | ||||
| 1 | 36 284 | 3.84 | 0.468 | How often did nurses treat you with courtesy and respect? |
| 2 | 36 336 | 3.74 | 0.570 | How often did nurses listen carefully to you? |
| 3 | 36 276 | 3.70 | 0.613 | During this hospital stay, how often did nurses explain things in a way you could understand? |
| CI | 36 523 | 3.76 | 0.456 | Composite index (mean of the 3 items) |
| Physician care | ||||
| 4 | 36 170 | 3.85 | 0.476 | How often did doctors treat you with courtesy and respect? |
| 5 | 36 137 | 3.74 | 0.602 | How often did doctors listen carefully to you? |
| 6 | 36 185 | 3.70 | 0.630 | How often did doctors explain things in a way you could understand? |
| CI | 36 408 | 3.76 | 0.500 | Composite index (mean of the 3 items) |
| Room | ||||
| 7 | 35 833 | 3.59 | 0.743 | How often were your room and bathroom kept clean? |
| 8 | 36 217 | 3.52 | 0.757 | How often was the area around your room quiet at night? |
| CI | 36 469 | 3.55 | 0.594 | Composite index (mean of the 2 items) |
| Staff | ||||
| 9 | 26 170 | 3.77 | 0.548 | How often did the hospital staff do everything they could to help you with your pain? |
| 10 | 18 042 | 3.68 | 0.716 | Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? |
| 11 | 17 714 | 3.03 | 1.171 | Before giving you any new medicine, how often did hospital staff describe side effects in a way you could understand? |
| CI | 30 687 | 3.59 | 0.666 | Composite index (mean of the 3 items) |
| Dependent variable | ||||
| 36 294 | 9.00 | 1.553 | Overall rating of the hospital (0-10) | |
Abbreviations: SD, standard deviation; CI, Composite Index.
The results of the multiple linear regression analyses are shown in Table 2. Table 2 shows the parameter estimates, standard errors, and P values for the 4 attributes (nursing care, physician care, staff care, and room), pain, interaction effects, and control variables. The model accounted for 51.2% of the variance. All 4 attribute variables were statistically significant at the .05 level and positively related to the dependent variable (overall rating of the hospital). Among the 4 attributes, nursing care shows the strongest influence (1.223), followed by physician care (0.731), room (0.433), and staff care (0.193). The pain variable is statistically significant and is inversely associated, indicating that patients with pain were less satisfied with their hospital experience than their counterparts without pain.
Table 2.
Parameter Estimates of Attributes and Control Variables.a
| Independent Variables | Parameter Estimate | Standard Error | P |
|---|---|---|---|
| Intercept | −0.614 | 0.170 | .000 |
| Nursing care | 1.223 | 0.049 | .000 |
| Physician care | 0.731 | 0.038 | .000 |
| Staff care | 0.193 | 0.022 | .000 |
| Room | 0.433 | 0.030 | .000 |
| Pain | −0.940 | 0.180 | .000 |
| Nursing care × pain | 0.097 | 0.052 | .062 |
| Physician care × pain | −0.182 | 0.041 | .000 |
| Staff care × pain | 0.317 | 0.026 | .000 |
| Room × pain | 0.012 | 0.033 | .713 |
| African American | 0.009 | 0.019 | .644 |
| Asian | −0.239 | 0.057 | .000 |
| Native Hawaiian/Pacific Islander | 0.058 | 0.244 | .811 |
| American Indian/Alaskan Native | 0.210 | 0.081 | .010 |
| Gender: female | 0.060 | 0.013 | .000 |
| Age | 0.026 | 0.002 | .000 |
| Educational attainment | −0.050 | 0.005 | .000 |
aN = 36 528, R 2 = .512. Gender: male is a reference group. Race: white is a reference group.
Among the 4 interaction effect variables, 2 variables (physician and staff attributes) were statistically significant and, thus, demonstrated interaction effects. More specifically, the interaction effect of physician care × pain variable was negatively related, indicating patients with pain put less emphasis on physician care than patients without pain. Conversely, the interaction effect of staff care × pain was positively related, indicating patients with pain put more emphasis on staff care than patients without pain. The 2 other interaction variables were not statistically significant.
With reference to the control variables, a few of them were statistically significant and deserve some mention. For the race variables, only Asian and American Indian/Alaskan Native are statistically significant. Asians are less likely and American Indians/Alaskan Natives are more likely than whites to rate their overall hospital stay as favorable. The gender variable is statistically significant, and female patients tend to rate their overall hospital stay more positively than male patients. Age is statistically significant and positively related, indicating older patients are more positive than younger patients on their overall hospital stay. Educational attainment is statistically significant and is negatively related, indicating patients with more education are less positive than patients with less education on their overall hospital stay.
Discussion
The purpose of this study was to investigate how patients with pain combine their attribute reactions differently from patients without pain. First, this study found that patients with pain had a lower overall rating of the hospital than patients without pain. This difference is statistically significant, and the magnitude of −0.94 is quite large. This finding is consistent with previous studies.10,14 This study also showed that the pain variable interacted with physician care and staff care but not with nursing care and room. Patients with pain put more emphasis on staff care than patients without pain. However, patients with pain put less emphasis on physician care than patients without pain.
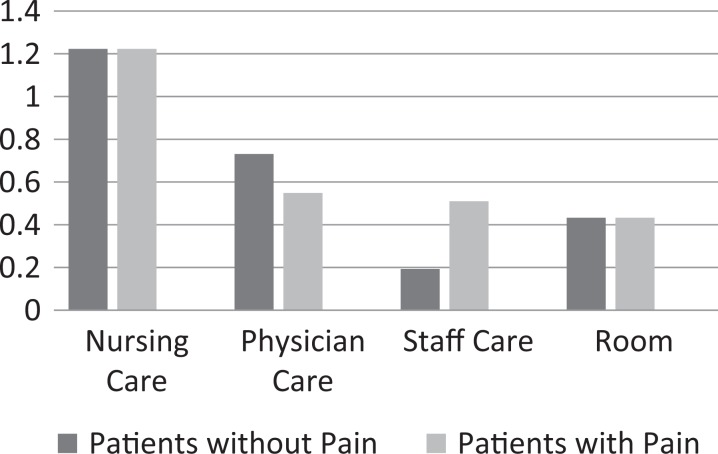
For patients without pain, the influential order of the 4 attributes is nursing care, physician care, room, and staff care, whereas for patients with pain, the influential order is nursing care, physician care, staff care, and room. There seems to be a minor difference between patients with and without pain. However, when the influential levels are quantified as seen in Figure 1, it is clear that patients with pain and patients without pain are different. This quantification was performed by considering the parameter estimates of the significant interaction effects with the corresponding attributes. Note that a group of patients without pain is a reference group. For patients without pain, nursing care (1.223) is the most influential, followed by physician care (0.731), room (0.433), and staff care (0.193), and their influential levels go down almost consistently. However, for patients with pain, statistically significant interaction terms must be considered when evaluating the effects of these 4 attributes. Although nursing care (1.223) is still the most influential, other attributes have similar influential levels: physician care (0.731-0.182 = 0.549), staff care (0.193 + 0.317 = 0.510), and room (0.433). For patients with pain, staff care becomes more influential and physician care becomes less influential compared to patients without pain, and thus, the influential levels of physician care and staff care are now close. These changes are noteworthy when hospitals treat patients with pain and patients without pain.
Figure 1.
Influential levels of the 4 attributes for patients with and without pain.
Why, then, do patients with pain put more emphasis on staff care and put less emphasis on physician care than patients without pain? One possible explanation is that patients see the staff as the individuals who can provide them more comfort during the pain experience. Patients may also see that the staff would prevent the pain by how they treat patients during the test or other routine activities. The shift with physicians suggests that patients do not see the physician—the dispenser of pain medication—as being critical to their situation. This may be because there is a tendency to go only so far with pain medication because of the risk of dependency. So, the physician is important to their care but important to a lesser degree in dealing with their pain. Patients with pain may see the staff as their supporters who would be always with patients during their stay at a hospital.
Limitations
This study utilized a well-established and validated patient satisfaction survey instrument and collected a large patient satisfaction data set from 70 geographically dispersed hospitals nationwide, with a very large sample size. Our study found some very informative, novel findings that contribute to a void in the literature. Despite the strengths of our study, there are some limitations that deserve mention. First, this is a cross-sectional study where independent and dependent variables were collected at the same time. This type of study design can establish an association but not a cause–effect relationship. This study used the Fishbein model as the guiding theory for this study. However, an intervention study where an attribute is improved would clearly establish a cause–effect relationship. Second, the sample size of this study was large, and data were randomly collected. The data came from 70 hospitals nationwide. However, the sampling frame did not include all 50 states and was limited to Midwest, Southwest, South, Northwest, and Northeast of the United States. Thus, there may be some generalizability issue to other parts of the United States. Future studies are encouraged in those other areas to confirm the results of this study. Third, the study was able to control for some key patient-level demographic variables (age, race, gender, and educational attainment) and self-report presence of pain. However, the data made available limited us from controlling for other patient-level clinical variables such as comorbidities, self-rated physical health status, and mental health status. Fourth, pain is a complex psychosensory phenomenon, and different patients expect differently. Subgroup analyses of patients with different levels of pain, duration, and cultural backgrounds would help us understand this complex phenomenon. Lastly, there was no information on the facility-level characteristics of the hospitals. Future research should control for a wider range of patient-level and facility-level factors.
Conclusion
This study found that patients with pain are different from patients without pain. First, patients with pain rate their overall hospital stay lower than patients without pain. This study utilized 4 types of control variables (race, gender, age, and educational attainment), and thus, regardless of racial background, gender, age, and educational attainment, patients with pain rate their overall hospital stay lower than patients without pain. Second, nursing care is most influential regardless of pain. However, other attributes influence differently depending on the presence of pain. Physician care is clearly the second most influential attribute among patients without pain, but for patients with pain, the influence level of physician care decreases. Since staff care increases its influential level for patients with pain, the influential levels of physician care and staff care are about the same for patients with pain. Many patient satisfaction studies agree that patients regard nursing care more influential than physician care on their overall satisfaction in hospital settings,5 and this study adds additional evidence to this body of literature. This study also found that staff care gains its influential level among patients with pain. Considering the number of patients with pain, it is critical to improve staff care. In this data set, 71.9% of patients have pain, more than super majority. It is suggested that hospital management needs to pay attention to nursing care and staff care to increase their patient overall rating of their hospital. These outcomes are informative and constructive for hospital managers since they supervise nurses and staff members. Due to this responsibility, hospital managers can be an impetus to provide guidelines and policies to improve communication and care delivery through staff and nurses, which in turn, could benefit the patients during their hospital stay. To combat lower satisfaction among patients experiencing pain, health care managers can utilize a variety of tools to improve the care delivered. DuPree et al found that patient satisfaction can be improved through the use of Six Sigma tools.18 This indicates the potential for systematic and systemic changes to positively improve the patient satisfaction despite their pain status, and it is apparent that systematic efforts can improve patient satisfaction with pain management.19 These efforts can most drastically improve the patient satisfaction.
Author Biographies
Koichiro Otani, PhD, is an Associate Professor at the Department of Health Policy and Management, College of Public Health, University of Georgia. He received his PhD from Saint Louis University.
Neale R. Chumbler, PhD, is a Professor and Dean, at the College of Health and Human Services, Western Kentucky University. He received his PhD from Case Western Reserve University.
Patrick A. Herrmann, PhD, FACHE is a Director at the Experience Research and Metrics, Ascension Health. He received his PhD from the University of Notre Dame.
Richard S. Kurz, PhD, is a Professor and Dean at the School of Public Health, the University of North Texas, Health Science Center. He received his PhD from the University of North Carolina at Chapel Hill.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Dansky KH, Brannon D. Discriminant analysis: a technique for adding value to patient satisfaction surveys. Hosp Health Serv Admin. 1996;41(4):503–513. [PubMed] [Google Scholar]
- 2. Marshall GN, Morales LS, Elliott M, Spritzer K, Hays RD. Confirmatory factor analysis of the Consumer Assessment of Health Plans Study (CAHPS) 1.0 Core Survey. Psychol Assess. 2001;13(2):216–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zaslavsky AM, Beaulieu ND, Landon BE, Cleary PD. Dimensions of consumer-assessed quality of Medicare managed-care health plans. Med Care. 2000;38(2):162–174. [DOI] [PubMed] [Google Scholar]
- 4. Otani K, Herrmann PA, Kurz RS. Improving patient satisfaction in hospital care settings. Health Serv Manag Res. 2011;24(4):163–169. [DOI] [PubMed] [Google Scholar]
- 5. Otani K, Waterman B, Faulkner KM, Boslaugh S, Dunagan WC. How patient reactions to hospital care attributes affect the evaluation of overall quality of care, willingness to recommend, and willingness to return. J Healthc Manag. 2010;55(1):25–38. [PubMed] [Google Scholar]
- 6. Otani K, Harris LE. Different integration processes of patient satisfaction among four groups. Health Care Manag Rev. 2004;29(3):188–195. [DOI] [PubMed] [Google Scholar]
- 7. Kroenke K, Stump T, Clark DO, Callahan CM, McDonald CJ. Symptoms in hospitalized patients: outcome and satisfaction with care. Am J Med. 1999;107(5):425–431. [DOI] [PubMed] [Google Scholar]
- 8. Institute of Medicine. Relieving pain in America: a blueprint for transforming prevention, care, education, and research. Washington, DC: 2011. Web site http://www.iom.edu/∼/media/Files/Report%20Files/2011/Relieving-Pain-in-America-A-Blueprint-for-Transforming-Prevention-Care-Education-Research/Pain%20Research%202011%20Report%20Brief.pdf. Accessed February 15, 2014. Updated October 22, 2015. [PubMed] [Google Scholar]
- 9. Kroenke K, Krebs E, Wu J, et al. Stepped Care to Optimize Pain Care Effectiveness (SCOPE) trial study design and sample characteristics. Contemporary Clinical Trials. 2013;34(2):270–281. [DOI] [PubMed] [Google Scholar]
- 10. Kroenke K. Patients presenting with somatic complaints: epidemiology, psychiatric comorbidity and management. Int J Meth Psychiatr Res. 2003;12:34–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kroenke K, Bair MJ, Damush TM, et al. Optimized antidepressant therapy and pain self-management in primary care patients with depression and musculoskeletal pain: a randomized controlled trial. JAMA. 2009;301(20):2099–2110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Larrabee JH, Ostrow CL, Withrow ML, Janney MA, Hobbs GR, Jr, Burant C. Predictors of patient satisfaction with inpatient hospital nursing care. Res Nurs Health. 2004;27(4):254–268. [DOI] [PubMed] [Google Scholar]
- 13. Dawson R, Spross JA, Jablonski ES, Hoyer DR, Sellers DE, Solomon MZ. Probing the paradox of patients’ satisfaction with inadequate pain management. J Pain Symptom Manag. 2002;23(3):211–220. [DOI] [PubMed] [Google Scholar]
- 14. Bhakta H, Marco CA. Pain management: association with patient satisfaction among emergency department patients. Am J Emerg Med. 2014;46(4):456–464. [DOI] [PubMed] [Google Scholar]
- 15. Fishbein M, Ajzen I. Belief Attitude, Intention and Behavior: An Introduction to Theory and Research. Manila, Philippines: Addison-Wesley Publishing; 1975. [Google Scholar]
- 16. Goldstein E, Farquhar M, Crofton C, Darby C, Garfinkel S. Measuring hospital care from the patients’ perspective: an overview of the CAHPS hospital survey development process. Health Serv Res. 2005;40(6 pt 2):1977–1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. O’Malley AJ, Zaslavsky AM, Hays RD, Hepner KA, Keller S, Cleary PD. Exploratory factor analysis of the CAHPS hospital pilot survey responses across and within medical, surgical, and obstetric services. Health Serv Res. 2005;40(6 pt 2):2078–2095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. DuPree E, Martin L, Anderson R, et al. Improving patient satisfaction with pain management using Six Sigma tools. Jt Comm J Qual Patient Saf. 2009;35(7):343–350. [DOI] [PubMed] [Google Scholar]
- 19. Comley AL, DeMeyer E. Assessing patient satisfaction with pain management through a continuous quality improvement effort. J Pain Symptom Manag. 2001;21(1):27–40. [DOI] [PubMed] [Google Scholar]