Abstract
Background:
Nigeria has a high population density but a weak health-care system. To improve the quality of care, 3 organizations carried out a quality improvement pilot intervention at the primary health-care level in selected rural areas.
Objective:
To assess the change in quality of care in primary health-care facilities in rural Nigeria following the provision of technical governance support and to document the successes and challenges encountered.
Method:
A total of 6 states were selected across the 6 geopolitical zones of the country. However, assessments were carried out in 40 facilities in only 5 states. Selection was based on location, coverage, and minimum services offered. The facilities were divided randomly into 2 groups. The treatment group received quality-of-care assessment, continuous feedback, and improvement support, whereas the control group received quality assessment and no other support. Data were collected using the SafeCare Healthcare Standards and managed on the SafeCare Data Management System—AfriDB. Eight core areas were assessed at baseline and end line, and compliance to quality health-care standards was compared.
Result:
Outcomes from 40 facilities were accepted and analyzed. Overall scores increased in the treatment facilities compared to the control facilities, with strong evidence of improvement (t = 5.28, P = .0004) and 11% average improvement, but no clear pattern of improvement emerged in the control group.
Conclusion:
The study demonstrated governance support and active community involvement offered potential for quality improvement in primary health-care facilities.
Keywords: health care, quality, primary health care, governance
Introduction
Nigeria, with a population of 170 million, is one of the most populous nations but weak in health-care standards.1 Despite extensive investments, the country still has insufficient health-care delivery infrastructures, poor quality health-care services, and unevenly distributed human resource capacity.2 These are reflected in its health-care quality ranking of 187 of 200 countries3 and listing among countries with some of the worst health indicators in the world.1,4,5
The country has an estimated 23 640 health facilities, and 85.5% of these are primary health-care facilities.6 Although these facilities serve the majority of the population, they are unable to provide basic and cost-effective services, especially in rural areas.7-9 This poor performance is attributed to various factors including poorly equipped health facilities, insufficient staff, lack of clearly defined roles and responsibilities, inadequate political commitment, and poor accountability.1,10,11
Quality improvement at primary health-care facilities is critical, however, efforts to address the quality of care as a contributory factor to the country’s poor health outcomes receive less attention.12 Clinical governance, the systematic approach to maintaining and improving the quality of patient care within a health system, needs to be at the core of every effort aimed at improving any health care.13 To ensure quality of care, facilities are required to have structures and processes according to the Donabedian model.14
To improve the quality of care in Nigeria’s primary health-care facilities, 3 organizations: Saving One Million Lives Initiative, Subsidy Reinvestment and Empowerment Programme on Maternal and Child Health (SURE-P MCH), and PharmAccess Foundation, collaborated to implement a pilot health-care quality improvement project in primary health-care facilities in rural communities.
PharmAccess Foundation, a Dutch group of organizations, is dedicated to making quality health care accessible in Africa. To achieve this, a set of quality standards and improvement methodology called SafeCare was established.15 SafeCare introduces international health-care standards to health facilities using a stepwise approach.
SafeCare places particular emphasis on processes, while not ignoring the need to improve inputs. This provides an opportunity to achieve the results despite resource constraints.16 Given the lack of data and a proper quality accreditation body in Nigeria, the project provided opportunities to define a clear pathway from assessment of care to improvement, by focusing on health-care delivery processes and patient safety.
This article aims to show how improvement in quality of health-care could be achieved through continuous governance support, local capacity building, and quality assessments, as well as to identify barriers to low-cost quality improvement at the primary health-care level in rural areas. It complements alternative efforts to evaluate this program.17
Methods
Forty-eight facilities from 6 states were randomly selected, 1 from each geopolitical zone in Nigeria. This approach ensured all parts of the country were represented. The states selected were Anambra, Bauchi, Cross River, Ekiti, Kebbi, and Niger States. However, all facilities in Bauchi State were dropped at the baseline phase due to data management issues, as a result of armed conflict in the region. Thus, the assessment was carried out in 5 states.
Facility selection was based on the ward-level coverage of 10 000 to 30 000 population per rural community, provision of basic maternal and child health services, high burden of maternal and child deaths, and intervention support from government through the SURE-P MCH program only.
The pilot project took place between October 2013 and March 2015 with 9 months of facility engagement. The duration included facility selection, data analysis, and final report development.
The selected facilities were split randomly into 2 equal treatment arms: “treatment A” facilities receiving full intervention and “treatment B” receiving minimal intervention (Table 1). For this study, treatment B facilities served as the control group.
Table 1.
Summary of the Intervention Given to the Groups.
| Intervention | Treatment A (24 Facilities) | Treatment B (24 Control Facilities) |
|---|---|---|
| Baseline assessment and feedback | Yes | Yes |
| Facility-specific quality improvement plan | Yes | No |
| Continuous improvement support and hands-on facilitation including trainings and documentation reviews | Yes | No |
| Additional support (weekly visits) by local facilitators | Yes | No |
| End of program assessment and feedback | Yes | Yes |
Data Resources and Management
Resource materials and tools used for the study were adopted from the SafeCare Healthcare Standards, and all data collected were managed on the SafeCare Data Management System—AfriDB.
The SafeCare standards covered a full range of management functions, clinical, clinical support, and ancillary services. Each service element contained a set of criteria that were assessed to ascertain compliance level. Compliance by the primary health centres (PHC) were graded on a scale of 1 to 100, with scoring categories as follows:
fully compliant—80% and above compliance,
partially compliant—40% to 80% compliance,
not compliant—no compliance to any significant degree, and
not applicable—does not provide service or level of service.
Scores were automatically generated by the management system and could not be influenced by facilitators.
Project Field Facilitators
A pair of quality assessors (QAs) conducted the baseline and end line assessments using the SafeCare’s Healthcare Standards. Fifteen quality improvement field officers (QIFOs) were responsible for providing continuous support to the facilities through regular facility visits. To build local capacity, 2 quality facilitators assisted the SafeCare team baseline assessments in Kebbi State as the distance between facilities in those states were wide.
In each facility, 1 quality lead (QL) was selected from the staff to ensure that facility responsibilities in respect to quality improvement were carried out in both treatment and control facilities.
Technical Assistance Capacity Building
A 3-day introductory training on SafeCare Methodology and Quality Improvement activities was held for all QAs, QIFOs, and QLs. Two mentoring sessions were also conducted for the QAs to increase their capacity to conduct assessments using the SafeCare approach.
Four-day refresher training for QAs and QIFOs was held 6 months after. The training included giving feedback to facility representatives, emphasizing the role of advocacy and meetings, and specific quality management topics and activities.
Finally, a 1-day workshop for 20 local government representatives and treatment A facility managers was held midway through the project to discuss inadequate governance support, stakeholder roles, and government impact on health-care quality.
Data Collection Approach
Required data were collected from observation of service activities in the facility, facility managers, and documentation reviews through a mixed-method approach. Quantitative data were collected for patient attendance, commodity supply, and utilization and observation checklists, whereas qualitative data were gathered through feedback sessions and interviews with facility staff.
The pair of SafeCare assessors conducted the quality baseline assessments between November 2013 and February 2014 and the end line assessments after 9 months. The end line was assessed by a different team. Pairing of assessors and using different teams at baseline and end line was a SafeCare model for peer review, triangulation, consistency, and reduction in result subjectivity.
Data collected were uploaded onto the data management system AfriDB 2.0, which ran an initial quality check, and afterward, a final quality check was done by an independent reviewer in the SafeCare team to ensure accuracy.
Quality Improvement Plans
After the baseline assessment, commonalities in governance structure, infrastructure, technology, and processes were documented and prioritized. Facility-specific standardized quality improvement plans, with priority areas for improvement and persons responsible, were developed and used only in treatment A facilities as part of the study intervention.
Quality Improvement Facilitation Process
This phase was implemented in treatment A facilities only, as it was the main intervention of the study. Each treatment A facility was visited 6 times, and during these visits, the facility manager and his team of nurse/midwives and community health extension workers received training on health-care and management structure, mission statement, floor plan and organogram drafting, managing patient records, and quality-of-care topics on hand hygiene, housekeeping, sterilization, waste management, storage facilities, stock management, and patients’ rights. The team selected from each facility was instructed on how to train other facility staff.
Ethical Approval
The study was based on the analysis of data collected at the primary health-care facilities without any patient identifier information and also existing in public domain. All states were informed of the study and gave their consent.
Results
Five states were included in the study, and hence, 40 facilities were assessed. The average scores at baseline and end line were 36% and 48%, respectively, compared to 36% and 35% for the control facilities. All treatment A facilities increased in overall scores at end line ranging from 5% to 23% (Figure 1). However, the control facilities showed no clear improvement with irregular patterns from 3% increase to slight decline in performance (Figure 2).
Figure 1.
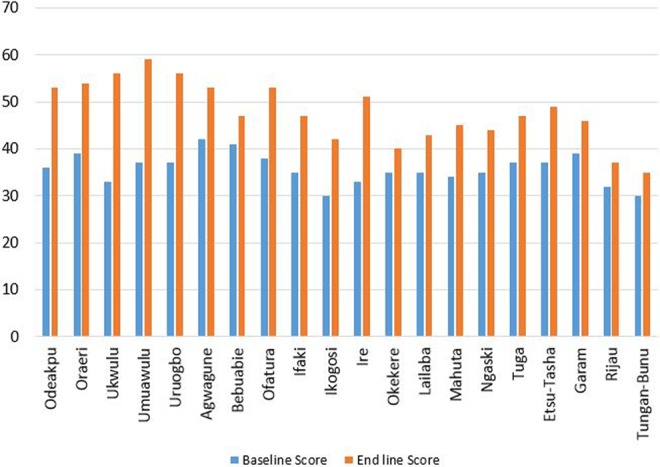
Overall scores for treatment A facilities.
Figure 2.
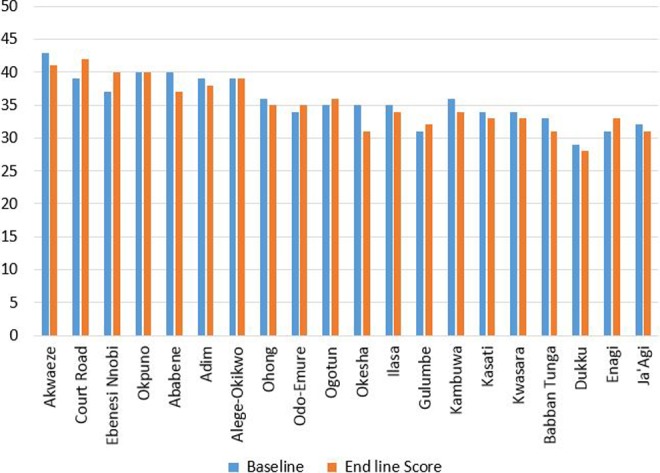
Overall scores for treatment B control facilities.
All service elements at treatment A facilities, except laboratory services, showed improvement at end line with an 11% average increase between the overall baseline and end line scores (Table 2). The χ2 analysis was conducted for each service element (Table 2) and showed 5 of the 11 elements to be statiscally significant. A 2 paired t test was also conducted between the overall baseline and end line scores and resulted in strong significant evidence of t = 5.28, P = .0004.
Table 2.
Treatment A Facilities—Average Safe Care Quality Elements Score.
| Safe Care Quality Service Elements | Baseline Score (%) | End Line Score (%) | Percentage Difference | χ2 Test |
|---|---|---|---|---|
| Management and leadership | 40 | 55 | 15 | 0.034 |
| Human resource management | 49 | 51 | 2 | 0.778 |
| Inpatient care | 35 | 56 | 21 | 0.003 |
| Laboratory services | 52 | 52 | 0 | 1.000 |
| Stock management | 28 | 42 | 14 | 0.038 |
| Facility management | 38 | 46 | 8 | 0.252 |
| Patient rights and access to care | 38 | 58 | 20 | 0.005 |
| Risk management | 29 | 35 | 6 | 0.363 |
| Management of information | 30 | 38 | 8 | 0.232 |
| Primary health care (malaria management, maternal and child health care) | 38 | 51 | 13 | 0.064 |
| Support services (cleaning services and security) | 19 | 38 | 19 | 0.003 |
| Mean | 36 | 47.45 | 11.45 |
The average means at baseline and end line were 35.75 and 47.25 for the treatment group and 35.6 and 35.16 for the control group, respectively (Figures 1 and 2). The mean difference in overall score between the 2 groups was 11.95. There was a statistically significant difference between the scores of the intervention (treatment) and the control groups over the period for implemented interventions, F (1,38) = 79.81, P = .0001, partial η2 = 0.667. This implies that increased technical assistance improved health-care quality. Hence, measuring the impact of technical assistance on quality improvement by comparing facilities that received a “full intervention” (assessments, reports, and technical assistance) with those that did not, we can conclude based on the findings that facilities that received technical assistance had better quality improvements.
At end line, the highest scoring service elements for treatment A facilities were patient rights and access to care (58%; P = .005), inpatient care (56%; P = .003), and management and leadership (55%; P = .034), whereas the lowest scoring service elements were management of information (38%; P = .232), risk management (35%; P = .363), and laboratory service with no change in scores (P = 1). Although support services had a low score (38%), it however showed significant improvement (P = .003), and contrariwise, despite the high score recorded for human resource management (58%), the change was insignificant (P = .778).
Discussions
This pilot study demonstrated that quality improvements can be made at the primary health-care level if given significant technical support and managed effectively. High scores at end line did not necessarily translate to significant improvements, and this was because the baseline in some cases had been high as well. However, the intervention proved statistically significant for management and leadership, inpatient care, stock management, and patient rights and access to care.
Measurable improvements in the treatment A facilities had 2 key success factors: community support and staff responsiveness to capacity building and technical support provided. Every facility had a Ward Development Committee (WDC), a team of community leaders. But despite the fact WDCs existed in all states, only WDCs in Anambra State were functional and offered support to the facility in various forms inclusive of recruiting cleaning and security staff.
The capacity of the facility managers was observed to impact overall outcomes. Facilities with supportive and committed facility managers recorded higher improvements, as was the case in the Anambra State treatment A facilities that were managed by registered nurses (Figure 3). However, facilities with only 1 or 2 self-driven personnel achieved little without the facility manager’s support. Overall, the responsiveness of the WDCs and staff was attributed as major success factors.
Figure 3.
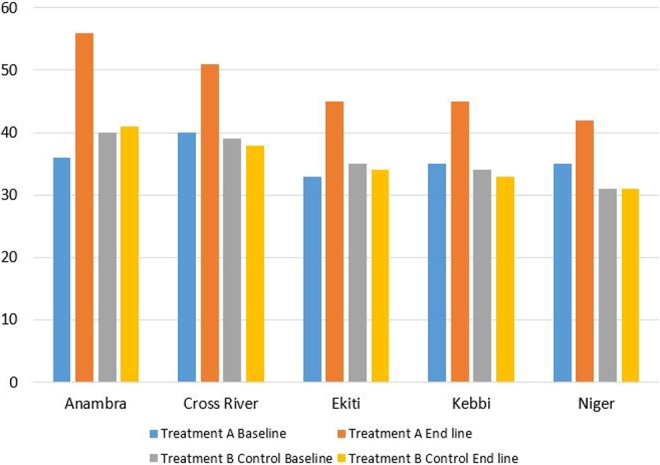
Overall scores for treatment A and treatment B control facilities at end line by state.
At baseline, malaria diagnosis was primarily based on the patient history of symptoms, without supporting laboratory investigation, leading to high records of malaria treatment errors. This was linked to the fact that only 30% of primary health-care facilities had either standing orders or guidelines for the management of malaria, indicating lack of adequate drug administration, guiding procedures, and monitoring. The guidelines were made available at all treatment A facilities and led to improvements in malaria management.
Despite observed improvements, deficiencies existed in the security of patients and staff, infection control, waste management, occupational health, and fire safety. This was because they were capital intensive and beyond the capacity of the facilities to improve by itself.
Contextual Relevance of Study
The most important and consequential level of care, the primary health care, is left to the weakest tier of government—the Local Government Authority (LGA).18 These LGAs lack adequate funding, manpower, and effective reporting lines, resulting in poor coordination and integration between levels of care and a weak and disorganized health system with varying outcomes based on the local situation,16-19 as observed in this study. Unless efforts to improve quality assurance are supported by a national policy framework, only scattered examples of quality excellence without comprehensive improvement will be exhibited.20
On a superficial level, the study showed facilities cannot be stimulated to improve or sustain improvements without external support due to resource constraints. However, the degree to which facilities imbibe a quality improvement culture depends on the presence of a regulatory environment that promotes this culture and patient–community engagement.19,21 These 2 factors were largely missing in this pilot, therefore, the study only speculated on the effect of their presence.
Limitations
Variance in data collection resulted in dropping all facilities in Bauchi State during the baseline assessment stage because of security issues in the state. In addition, a period of 9 months may not be sufficient to effectively observe sustained quality improvements but can provide information sufficient to demonstrate what is needed to improve quality of care at the primary care level in rural areas.
Conclusion
Overall, the pilot phase of the project met its objectives having demonstrated the potential of quality improvement in primary health-care facilities in rural Nigeria.
Despite the success within the short duration, we suggest that quality improvement needs to be a continuous cycle and requires an investment in people, processes, infrastructure, equipment, and materials, as well as periodic evaluations and feedback for sustainable improvement.
The main challenge for the SafeCare methodology, as for any quality improvement program or institution, is its long-term sustainability. Thus, we recommend a shift in focus toward building more local capacity to ensure local ownership and lower costs.
Lessons learnt from this pilot study showed that increased community engagement, as well as government support in the establishment of structures and processes, is required for improving quality of health care eventually leading to strengthening the health system.
Author Biographies
Ugo Okoli is a fellow of the Faculty of Public Health Medicine, UK. She is currently working as a Consultant in Public Health, National Primary Health Care Development Agency- SURE P MCH, Nigeria, Abuja.
Eze-Ajoku Ezinne MD, MPH (Harvard School of Public Health), is currently working towards a PhD in Public Health at John Hopkins University, Baltimore, MD, USA.
Oludipe Modupe MBBS, is the SafeCare Country Director based in Lagos, Nigeria.
Spieker Nicole PhD is the Program Director PharmAccess Foundation based in Amsterdam, the Netherlands. She is responsible for SafeCare Initiatives.
Ekezie Winifred MPH, is working towards a PhD in Epidemiology and Public Health from the University of Nottingham, UK. She also worked for SURE P MCH, Abuja, Nigeria.
Ohiri Kelechi, MB BS, MPH (Harvard School of Public Health), SM, is currently the Head of Health Strategy and Delivery Foundation and worked as part of the Save One Million Lives Initiative, Abuja, Nigeria.
Footnotes
Authors’ Note: The program concept was developed by the World Bank and SURE P MCH/SOML team inclusive of David K Evans, Felipe Alexander Dunsch, Ezinne Eze-Ajoku and Mario Macis. Furthermore, we would like to also thank the following for their contribution: Dr Muhammad A Pate, Dr Kelechi Ohiri, Dr Sidi Ali Mohammed, Dr Tokunbo Oshin, Dr Muntaqa Umar-Sadiq and Dr Asumah Anire.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. National Population Commission (NPC) [Nigeria], ICF International. Nigeria Demographic and Health Survey 2013. NPC and ICF International. 2014; Available from: https://www.dhsprogram.com/pubs/pdf/FR293/FR293.pdf. Accessed July 30, 2016.
- 2. Olakunde BO. Public healthcare financing in Nigeria: which way forward? Ann Niger Med. 2012;6(1):4–10. [Google Scholar]
- 3. World Health Organization. World Health Report 2000. Health Systems - Improving Performance. Geneva: WHO; 2000. Available from: http://www.who.int/whr/2000/en/whr00_en.pdf?ua=1. Accessed July 30, 2016. [Google Scholar]
- 4. Okonofua FE, Abejide A, Makanjuola RA. Maternal mortality in Ile-Ife Nigeria: a study of risk factors. Stud Fam Plann. 1992;23(5):319–324. [PubMed] [Google Scholar]
- 5. Okafor CB, Rizzuto RR. Women’s and healthcare providers views of maternal practices and services in rural Nigeria. Stud Fam Plann. 1994;25(6 pt 1):353–361. [PubMed] [Google Scholar]
- 6. Federal Ministry of Health Nigeria. National Strategic Health Development Plan (NSHDP) 2010-2015, Federal Ministry of Health. 2010.
- 7. Adeniyi J, Ejembi CL, Igbineosun P, Mohammed D. The status of primary healthcare in Nigeria: report of a needs assessment survey National Primary Healthcare Development Agency; 2001. [Google Scholar]
- 8. Hodges A. Children’s and women’s right in Nigeria, wake-up call: situation assessment and analysis 2001 National Planning Commission and UNICEF; 2001:2–10. [Google Scholar]
- 9. Adindu A. Assessing and assuring quality of healthcare in Africa. Afr J of Med Sci. 2010;3(1):31–36. [Google Scholar]
- 10. Nnebue CC, Ebenebe UE, Adogu POU, et al. Adequacy of resources for provision of maternal health services at the primary healthcare level in Nnewi, Nigeria. Niger Med J. 2014;55(3):235–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Olumide EA, Obionu CN, Mako IV. An assessment of quality of primary healthcare in Nigeria. Report of a survey commissioned by the National Primary Healthcare Development Agency (NPHCDA) NPHCDA; 2000. [Google Scholar]
- 12. Aigbiremolen AO, Abejegah C, Eboreime E, Alenoghena I. Primary healthcare in Nigeria: strategies and constraints in implementation. Int J of Comm Research. 2014;3(3):74–79. [Google Scholar]
- 13. Scally G, Donaldson LJ. Clinical governance and the drive for quality improvement in the new NHS in England. BMJ. 1998;317(7150):61–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Donabedian A. The quality of care: how can it be assessed? JAMA. 1988;121(11):1145–1150. [PubMed] [Google Scholar]
- 15. Pharm Access Foundation, Safe Care Basic Healthcare Standards. 2000. Available at: http://www.safe-care.org/. Accessed July 30, 2016.
- 16. Adeyemo DO. Local government and healthcare delivery in Nigeria: a case study. J Hum Ecol. 2005;18(2):149–160. [Google Scholar]
- 17. Dunsch FA, Evans DK, Eze-Ajoku E, Macis M. Management Consulting and Quality Health Care: Evidence from a Field Experiment in Nigeria. SSRN Working Paper. 2015. [Google Scholar]
- 18. Abimbola S. How to improve the quality of primary healthcare in Nigeria. The BMJ Bloggs. 2012. [Google Scholar]
- 19. Abdulraheem IS, Olapipo AR, Amodu MO. Primary healthcare services in Nigeria: critical issues and strategies for enhancing the use by the rural communities. J Public Health Epidemiol. 2012;4(1):5–13. [Google Scholar]
- 20. Reenrink I, Sauerborn R. Quality of primary healthcare in developing countries: recent experiences & future directions. Int J Qual Healthcare. 1996;8(2):131–139. [DOI] [PubMed] [Google Scholar]
- 21. Abdulraheem IS. Experience and perspectives of quality of healthcare in Nigerian rural community: an exploratory study. Niger Med Pract. 2006;50(2):48–53. [Google Scholar]


