Abstract
Purpose:
The purpose of this study was to compare medical residents and practicing physicians in primary care specialties regarding their knowledge and beliefs about electronic cigarettes (e-cigarettes). We wanted to ascertain whether years removed from medical school had an effect on screening practices, recommendations given to patients, and the types of informational sources utilized.
Methods:
A statewide sample of Florida primary care medical residents (n = 61) and practicing physicians (n = 53) completed either an online or paper survey, measuring patient screening and physician recommendations, beliefs, and knowledge related to e-cigarettes. χ2 tests of association and linear and logistic regression models were used to assess the differences within- and between-participant groups.
Results:
Practicing physicians were more likely than medical residents to believe e-cigarettes lower cancer risk in patients who use them as an alternative to cigarettes (P = .0003). Medical residents were more likely to receive information about e-cigarettes from colleagues (P = .0001). No statistically significant differences were observed related to e-cigarette knowledge or patient recommendations.
Conclusions:
Practicing primary care physicians are accepting both the benefits and costs associated with e-cigarettes, while medical residents in primary care are more reticent. Targeted education concerning the potential health risks and benefits associated with the use of e-cigarettes needs to be included in the current medical education curriculum and medical provider training to improve provider confidence in discussing issues surrounding the use of this product.
Keywords: primary care, smoking, medical education, electronic cigarettes, clinical guidelines
Introduction
Electronic cigarette (e-cigarette) usage has increased significantly since their introduction in 2003. From 2009 to 2013, adult usage increased from 0.6% to 15%.1 Among adolescents, current, from 2011 to 2015, e-cigarette use has increased from 1.5% to 16%.2 Despite their popularity, research on these relatively new devices is in the beginning stages and the available literature has mixed findings. Some research indicates e-cigarettes are less harmful than traditional cigarettes,3,4 can be a successful harm reduction strategy,5,6 and have potential to be an effective cessation aid.7,8 Others have found that these devices contain harmful substances such as glycerol, polyene glycol, and tobacco-specific nitrosamines,9–11 and that users may be at risk for adverse health effects.12,13 In addition to health risks, there are concerns that e-cigarette use normalizes smoking behaviors and could lead to smoking uptake among nonsmokers.14,15
Electronic-cigarettes are often part of the clinical encounter,16–19 yet conflicting research and uncertainty surrounding their health effects renders it unclear how physicians should proceed in counseling patients about e-cigarette use. The established evidence-based guideline for treating tobacco dependency is for physicians to provide brief cessation counseling to all tobacco users.20 This physician-delivered tobacco dependence treatment is typically followed by most physicians21,22 and is effective in impacting patient smoking cessation.20,23 However, research indicates that physicians are less likely to provide this brief intervention to patients using e-cigarettes, and furthermore, a majority of physicians report discomfort talking to their patients about e-cigarettes due to the limited knowledge.17,24
Although the research addressing e-cigarettes is increasing, there is insufficient evidence as to harms or benefits to inform practice guidelines, and little work on how providers are counseling their patients concerning the use of e-cigarettes in the absence of guidelines. Therefore, the purpose of this pilot study was to compare physicians starting their careers (medical residents [MRs]), to practicing physicians (PPs), focusing on those in the primary care specialties regarding their knowledge and beliefs about e-cigarettes, and inclusion of e-cigarettes in their tobacco screening. We wanted to test whether years removed from medical school had an effect on screening practices, recommendations given to patients, and the types of informational sources utilized.
Methods
Participants
Study participants were physicians, specifically MRs and PPs, affiliated with a College of Medicine (COM). The MRs were recruited from 4 COM-affiliated primary care residency programs: family medicine, internal medicine, obstetrics/gynecology, and pediatrics. The PPs were recruited from the COM Summer Clinical Practicum (SCP) community faculty. The SCP faculty host rising second-year medical students in their practice for a 3-consecutive week summer preceptorship.
Measures
A 20-item survey was developed to address participant knowledge, behaviors, and beliefs about asking and advising their patients about e-cigarettes. We also gathered demographic variables including age, gender, race/ethnicity, county of practice, and year of graduation from medical school. Study questions were piloted with COM faculty and fourth-year medical students and subsequently revised. The survey was constructed and administered via Qualtrics.
Data Collection
Both participant groups were invited to participate in the study via an e-mail, which contained a direct link to the online survey. The survey link was accompanied by a letter of support from either the senior associate dean for Medical Education and Academic Affairs (MR group) or the SCP director (PP group). The MRs completing the survey received a US$50 Amazon gift card. There was no monetary incentive for the PPs. The initial response rate for the online survey was low for the PPs. To boost the PPs response rate, an identical paper survey was mailed to their practice address, with a self-addressed/self-stamped envelope and pencil. Follow-up e-mails were sent to all participants at 3 weeks and 6 weeks after the initial invitation. Data were collected from December 2014 to September 2015. The study was approved by the Florida State University institutional review board.
Statistical Analyses
First, we checked responses to ensure that reported answers fell within the intended range. Responses that were outside the range instructed were considered as missing. For example, responses who answered that their self-reported knowledge was 0 were considered missing because they failed to follow instructions to input a number between 1 and 10, inclusive. Statistical analyses were performed using Statistical Analysis Software (SAS) version 9.4 for Windows. Due to the large number (133) of tests of interest, we adopted a Bonferroni adjustment of the 5% significance level.
Comparisons include tests of associations between outcomes and demographics between- and within-participant groups. Outcomes were assessed by age, gender, or the number of years lapsed since medical school graduation. χ2 tests of association were used to assess relationships between binary outcomes and participant group. Putative associations between Likert-coded questions and participant group were examined using χ2 tests of ordinal association with modified ridit scores. To investigate a potential association between self-rated knowledge and participant group, we fit a simple linear regression model and checked the P value of the coefficient of the slope.
Results
Of the 116 MRs invited to participate in the study, 61 completed the online survey yielding a response rate of 53%. Of the 91 PPs invited to participate, 19 responded to the electronic survey and 34 completed the paper survey, with a response rate of 58% for a total of 53 responses. The demographic breakdown of the respondents is provided in Table 1.
Table 1.
Demographic Characteristics of Respondents.
| Demographic characteristics | Total, n (%) | Medical Residents, n (%) | Physicians, n (%) |
|---|---|---|---|
| Gender | |||
| Male | 64 (56%) | 27 (44%) | 37 (70%) |
| Female | 50 (44%) | 34 (56%) | 16 (30%) |
| Age | |||
| <35 | 57 (50%) | 52 (85%) | 5 (9%) |
| 36-50 | 23 (20%) | 9 (15%) | 14 (26%) |
| 50+ | 34 (30%) | 0 (0%) | 34 (64%) |
| Race | |||
| Black/African American Hispanic | 2 (2%) | 1 (2%) | 1 (2%) |
| Black/African American non-Hispanic | 13 (11%) | 10 (16%) | 3 (6%) |
| White Hispanic | 17 (15%) | 9 (15%) | 8 (15%) |
| White non-Hispanic | 61 (54%) | 26 (43%) | 35 (66%) |
| Other | 17 (15%) | 15 (25%) | 2 (4%) |
| Missing | 4 (4%) | 0 (0%) | 4 (7%) |
| Medical school graduation year | |||
| 1960-1969 | 1 (1%) | 0 (0%) | 1 (2%) |
| 1970-1979 | 8 (7%) | 0 (0%) | 8 (15%) |
| 1980-1989 | 22 (19%) | 0 (0%) | 22 (42%) |
| 1990-1999 | 12 (11%) | 1 (2%) | 11 (21%) |
| 2000-2009 | 19 (17%) | 13 (21%) | 6 (11%) |
| 2010-2014 | 50 (44%) | 47 (77%) | 3 (6%) |
| Missing | 2 (2%) | 0 (0%) | 2 (4%) |
Two significant differences in responses between MRs and PPs were evident. First, PPs were more likely than MRs to agree that e-cigarettes lower cancer risk in patients who use them as an alternative to cigarettes, while MRs were more likely to be unsure or disagree (P =.0003; Table 2). Second, a higher proportion of MRs than PPs reported receiving information regarding e-cigarettes from their colleagues (P = .0001; Figure 1). The MRs and PPs did not differ significantly on the remaining survey questions. No significant within-participant group associations between responses and demographics were found at the Bonferroni-adjusted 5% significance level.
Table 2.
Comparison of Medical Residents’ and Practicing Physicians’ Beliefs Regarding e-Cigarettes.
| Medical Residents (%) | Practicing Physicians (%) | P Value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree | Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree | ||
| E-cigarettes are safer/less harmful than traditional cigarettes | 2 | 38 | 36 | 15 | 10 | 8 | 23 | 30 | 34 | 6 | .2905 |
| E-cigarettes are helpful as a harm reduction strategy and/or cessation aid | 2 | 41 | 43 | 11 | 3 | 4 | 30 | 23 | 32 | 11 | .0265 |
| E-cigarettes are FDA approved as a cessation aid | 5 | 28 | 39 | 28 | 0 | 2 | 4 | 13 | 43 | 38 | .1268 |
| E-cigarettes contain some chemicals that may cause long-term health effects | 26 | 51 | 21 | 2 | 0 | 30 | 51 | 15 | 4 | 0 | .5769 |
| E-cigarettes encourage smoking initiation in those who have never smoked | 18 | 26 | 33 | 20 | 3 | 25 | 43 | 30 | 2 | 0 | .0060 |
| E-cigarettes encourage continuation among smokers who might otherwise quit | 15 | 26 | 48 | 11 | 0 | 6 | 32 | 28 | 26 | 8 | .0512 |
| E-cigarettes counter the effectiveness of smoke-free policies | 0 | 17 | 38 | 25 | 18 | 17 | 43 | 28 | 11 | 0 | .4608 |
| E-cigarettes can lower cancer risk in patients who use them as an alternative to cigarettes | 2 | 21 | 43 | 23 | 11 | 17 | 45 | 13 | 21 | 4 | .0003a |
Abbreviations: E-cigarettes, electronic cigarettes; FDA, Food and Drug Administration.
aAverage level of agreement to the statement is significantly different between medical residents and practicing physicians at the Bonferroni-adjusted 5% significance level.
Figure 1.
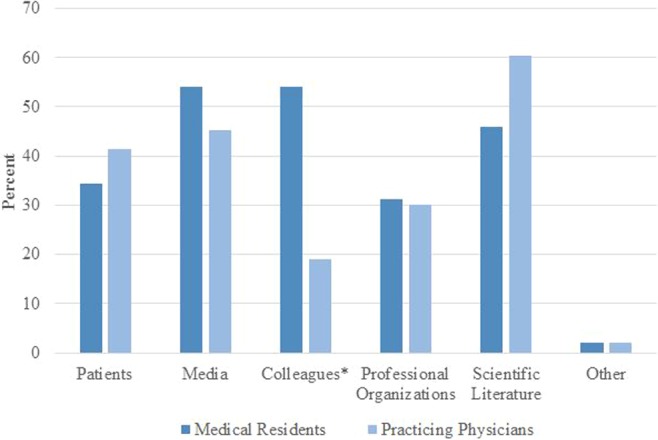
Medical residents versus practicing physicians: From what source(s) do they retrieve information regarding e-cigarettes? *Significant at the Bonferroni-adjusted 5% significance level. P = .0001. E-cigarettes indicates electronic cigarettes.
A small number of results seem potentially important but were not significant based on our stringent standard. First, knowledge was linearly related to practitioner group with a low P value (.0008). The MRs reported average knowledge ratings 1.4 points lower than their PP counterparts. Additionally, PPs were more likely than MRs to view e-cigarettes as a gateway drug or excuse not to quit with a low P value (.0060).
Discussion
This pilot study attempted to find differences in knowledge, attitude, and practices relating to e-cigarettes, between 2 groups of primary care physicians, one pursuing their residency training and the other in practice. There were few statistically significant differences within physician group or between the 2 groups. The PPs were significantly more likely to view e-cigarettes in terms of their harm reduction for cancer, while MRs were unsure or disagreed. Similarly, prior research indicates that physicians who have been in practice longer are more likely to have a harm reduction orientation to e-cigarettes.18
The fact that MRs were significantly more likely to identify their colleagues as source for information relating to e-cigarettes than the PPs may be related to both the limited and conflicting formal evidence and/or the potential use of e-cigarettes by colleagues, friends, and even themselves. The highest prevalence of e-cigarette use is among those 18 to 34 years of age, the group to which many residents currently belong.1 Finally, our findings differ slightly from previous research that found only a small minority of physicians received information on e-cigarettes from professional sources and colleagues.24
Knowledge of e-cigarettes did not achieve significance but suggests a possible difference between the groups, with MR’s knowledge being lower than that of PPs. A resident may feel less secure in making a judgment particularly under ambiguous circumstances and where there is no unanimity of opinion. This theory is supported by previous findings that comfort in discussing e-cigarettes increased with age, as older physicians tend to be more comfortable discussing risk-related topics with patients due to more years of clinical experience.24
Although not statistically significant, PPs were more likely than MRs to believe that e-cigarettes “encourage smoking initiation in those who have never smoked and encourage continuation among smokers who might otherwise quit.” This finding is supported by recent literature that indicates e-cigarette use is increasing among those who have never smoked cigarettes,25–28 and that nonsmokers who use e-cigarettes are likely to transition to cigarette smoking and dual or multiple product use.27,29–33 Therefore, physicians who believe e-cigarettes encourage smoking initiation and/or continuation may be more likely to intervene with patients who use e-cigarettes by encouraging them to use interventions proven to be effective.
Limitations
This article describes the results of a pilot study, intended to fine-tune a survey instrument, a survey strategy, and seek some initial information about these physician groups. As a pilot study, our results have several limitations. Our sample size was small, as were some cell sizes for the outcomes. We therefore have very low statistical power to detect true effects. Our study focused on primary care physicians affiliated with a single COM, thus limiting generalizability. Prior research suggests that primary care physicians are both more knowledgeable about e-cigarettes and more likely to implement the clinical practice guidelines compared to other physician specialties.17,24,34,35 Therefore, it is likely that other physician populations may exhibit different behavior. In addition, the survey did not include a question about the subject’s own use of e-cigarettes, a behavior that can color one’s views of the product. Finally, MRs who completed the survey received an Amazon gift card, which may introduce an indeterminate response bias.
Conclusion
Extensive research on e-cigarettes remains ongoing as the overall adverse and long-term health effects of these devices remain uncertain. The Food and Drug Administration recently extended its authority to regulate e-cigrettes.36 However, until authoritative clinical guidelines are set, physicians, especially those in primary care specialties, will encounter questions about e-cigarettes from patients and others. This pilot study suggests that practicing primary care physicians are accepting both the potential benefits and costs associated with e-cigarettes, while primary care MRs are more reticent. We believe that these preliminary results suggest an important area of inquiry, specifically, how providers counsel patients concerning the use of e-cigarettes, whether and how that counsel changes with patient demographics, and where they are receiving their patient education information. We suggest using this information to augment current medical education curriculum and medical provider training to improve provider confidence in discussing issues surrounding the use of these devices. This information is important from the perspective of the future physician as a provider of information and counsel, as well as of the physician as a scientist to be aware of the controversy surrounding e-cigarettes.
Author Biographies
Karen W. Geletko is a research faculty in the Department of Biomedical Sciences and Social Medicine at Florida State University College of Medicine. She specializes in planning and conducting research projects in the intersecting areas of medicine and public health, and tobacco prevention and cessation, and develops model programs for training physicians and other health professionals to treat tobacco dependency.
Karen Myers is an assistant professor in the Department of Family Medicine and Rural Health at Florida State University College of Medicine. She serves as an instructor for first- and second-year medical students and coordinates the involvement of local physicians who serve as preceptors for first- and second-year students.
Naomi Brownstein is an assistant professor in the Department of Biomedical Sciences and Social Medicine at Florida State University College of Medicine. As a biostatistician, she aids in statistical analysis and grant proposal development, in addition to teaching biostatistics courses.
Breanna Jameson is a second year medical student at Florida State University College of Medicine and holds both a bachelor’s and master’s degree in biomedical sciences. She plans to deliver patient-centered health care in an underserved community.
Daniel Lopez is a first year medical student at Florida State University College of Medicine and holds bachelor’s degrees in biomedical sciences and public health. He aspires to practice patient-centered care in a pediatric population of need.
Alaine Sharpe is a third year medical student at Florida State University College of Medicine and holds a bachelor’s degree in biology and a master’s degree in chemistry. She hopes to practice medicine in underserved populations of need.
Gail R. Bellamy is a professor in the Department of Biomedical Sciences and Social Medicine and the Director of the Florida Blue Center for Rural Health Research and Policy at Florida State University College of Medicine. She promotes and develops programmatic collaborations in support of healthy rural communities, and works to improve rural health educational efforts by providing a rural perspective for research and programmatic efforts.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research and/or authorship of this article: Funding for this research was supported by the Florida State University Council on Research and Creativity (CRC) Planning Grant.
References
- 1. Regan AK, Promoff G, Dube SR, Arrazola R. Electronic nicotine delivery systems: adult use and awareness of the ‘e-cigarette’ in the USA. Tob Control. 2013;22(1):19–23. [DOI] [PubMed] [Google Scholar]
- 2. Singh T, Arrazola RA, Corey CG, et al. ; Centers for Disease Control and Prevention. Tobacco Use Among Middle and High School Students—United States, 2011–2015. MMWR Morb Mortal Wkly Rep. 2016;65(14):361–367. http://www.cdc.gov/mmwr/volumes/65/wr/mm6514a1.htm?s_cid=mm6514a1_w. Accessed June 2016. [DOI] [PubMed] [Google Scholar]
- 3. Farsalinos KE, Yannovits N, Sarri T, Voudris V, Poulas K. Protocol proposal for, and evaluation of, consistency in nicotine delivery from the liquid to the aerosol of electronic cigarettes atomizers: regulatory implications. Addiction. 2016;111(6):1069–1076. [DOI] [PubMed] [Google Scholar]
- 4. McAuley TR, Hopke PK, Zhao J, Babaian S. Comparison of the effects of e-cigarette vapor and cigarette smoke on indoor air quality. Inhal Toxicol. 2012;24(12):850–857. [DOI] [PubMed] [Google Scholar]
- 5. Cahn Z, Siegel M. Electronic cigarettes as a harm reduction strategy for tobacco control: a step forward or a repeat of past mistakes? J Public Health Policy. 2010;32(1):16–31. [DOI] [PubMed] [Google Scholar]
- 6. Polosa R, Caponnetto P, Morjaria JB, Papale G, Campagna D, Russo C. Effect of an electronic nicotine delivery device (e-cigarette) on smoking reduction and cessation: a prospective 6-month pilot study. BMC Public Health. 2011;11:786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bullen C, Howe C, Laugesen M, et al. Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet. 2013;382(9905):1629–1637. [DOI] [PubMed] [Google Scholar]
- 8. Eissenberg T. Electronic nicotine delivery devices: ineffective nicotine delivery and craving suppression after acute administration. Tob Control. 2010;19(1):87–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Foulds J, Veldheer S, Berg A. Electronic cigarettes (e-cigs): views of aficionados and clinical/public health perspectives. Int J Clin Pract. 2011;65(10):1037–1042. [DOI] [PubMed] [Google Scholar]
- 10. Pellegrino RM, Tinghino B, Mangiaracina G, et al. Electronic cigarettes: an evaluation of exposure to chemicals and fine particulate matter (PM). Ann Ig. 2012;24(4):279–288. [PubMed] [Google Scholar]
- 11. United States Food and Drug Administration. FDA warns of health risks posed by e-cigarettes; 2009. http://www.fda.gov/downloads/ForConsumers/ConsumerUpdates/UCM173430.pdf. Accessed March 2016. Updated August 2016.
- 12. Vardavas CI, Anagnostopoulos N, Kougias M, Evangelopoulou V, Connolly GN, Behrakis PK. Short-term pulmonary effects of using an electronic cigarette: impact on respiratory flow resistance, impedance, and exhaled nitric oxide. Chest. 2012;141(6):1400–1406. [DOI] [PubMed] [Google Scholar]
- 13. Barrington-Trimis JL, Samet JM, McConnell R. Flavorings in electronic cigarettes: an unrecognized respiratory health hazard? JAMA. 2014;312(23):2493–2494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fairchild AL, Bayer R, Colgrove J. The renormalization of smoking? E-cigarettes and the tobacco “endgame”. N Engl J Med. 2014;370(4):293–295. [DOI] [PubMed] [Google Scholar]
- 15. Wills TA, Knight R, Williams RJ, Pagano I, Sargent JD. Risk factors for exclusive e-cigarette use and dual e-cigarette use and tobacco use in adolescents. Pediatrics. 2015;135(1):e43–e51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kandra KL, Ranney LM, Lee JGL, Goldstein AO. Physicians’ attitudes and use of e-cigarettes as cessation devices, North Carolina, 2013. PLoS ONE. 2014;9(7):e103462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pepper JK, Gilkey MB, Brewer NT. Physicians’ counseling of adolescents regarding e-cigarette use. J Adolesc Health. 2015;57(6):580–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Steinberg MB, Giovenco DP, Delnevo CD. Patient-physician communication regarding electronic cigarettes. Prev Med Rep. 2015;2:96–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Berg CJ, Haardoerfer R, Escoffery C, Zheng P, Kegler M. Cigarette users’ interest in using or switching to electronic nicotine delivery systems or smokeless tobacco for harm reduction, cessation, or novelty: a cross-sectional survey of US adults. Nicotine Tob Res. 2014;17(2):245–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fiore M, Jaén CR, Baker TB, et al. Treating tobacco use and dependence: 2008 update US Public Health Service Clinical Practice Guideline. US Department of Health and Human Services, Public Health Service; http://www.ncbi.nlm.nih.gov/pubmed/11203101. Updated 2016. Accessed March 2016. [Google Scholar]
- 21. Kruger J, O’Halloran A, Rosenthal A. Assessment of compliance with US Public Health Service clinical practice guideline for tobacco by primary care physicians. Harm Reduct J. 2015;12:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tong EK, Strouse R, Hall J, Kovac M, Schroeder SA. National survey of US health professionals’ smoking prevalence, cessation practices, and beliefs. Nicotine Tob Res. 2010;12(7):724–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stead LF, Buitrago D, Preciado N, Sanchez G, Hartmann-Boyce J, Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2013;(5):CD000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pepper JK, McRee AL, Gilkey MB. Healthcare providers’ beliefs and attitudes about electronic cigarettes and preventive counseling for adolescent patients. J Adolesc Health. 2014;54(6):678–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Huang LL, Kowitt SD, Sutfin EL, Patel T, Ranney LM, Goldstein AO. Electronic cigarette use among high school students and its association with cigarette use and smoking cessation, North Carolina youth tobacco surveys, 2011 and 2013. Prev Chronic Dis. 2016;13:E103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Collaco JM, Drummond MB, McGrath-Morrow SA. Electronic cigarette use and exposure in the pediatric population. JAMA Pediatr. 2015;169(2):177–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bunnell RE, Agaku IT, Arrazola RA, et al. Intentions to smoke cigarettes among never-smoking US middle and high school electronic cigarette users: National Youth Tobacco Survey, 2011-2013. Nicotine Tob Res. 2015;17(2):228–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Dutra LM, Glantz SA. Electronic cigarettes and conventional cigarette use among US adolescents: a cross-sectional study. JAMA Pediatr. 2014;168(7):610–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wills TA, Knight R, Sargent JD, Gibbons FX, Pagano I, Williams RJ. Longitudinal study of e-cigarette use and onset of cigarette smoking among high school students in Hawaii [Published online January 25, 2016]. Tob Control. 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Barnett TE, Soule EK, Forrest JR, Porter L, Tomar SL. Adolescent electronic cigarette use: associations with conventional cigarette and hookah smoking. Am J Prev Med. 2015;49(2):199–206. [DOI] [PubMed] [Google Scholar]
- 31. Barrington-Trimis JL, Urman R, Berhane K, et al. E-cigarettes and future cigarette use. Pediatrics. 2016;138(1):pii:e20160379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Leventhal AM, Strong DR, Kirkpatrick MG, et al. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA. 2015;314(7):700–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Primack BA, Soneji S, Stoolmiller M, Fine MJ, Sargent JD. Progression to traditional cigarette smoking after electronic cigarette use among us adolescents and young adults. JAMA Pediatr. 2015;169(11):1018–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Carson KV, Verbiest ME, Crone MR, et al. Training health professionals in smoking cessation. Cochrane Database Syst Rev. 2012;(5):CD000214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Victor JC, Brewster JM, Ferrence R, Ashley MJ, Cohen JE, Selby P. Tobacco-related medical education and physician interventions with parents who smoke: survey of Canadian family physicians and pediatricians. Can Fam Physician. 2010;56(2):157–163. [PMC free article] [PubMed] [Google Scholar]
- 36. United States Food and Drug Administration. Extending authorities to all tobacco products, including e-cigarettes, cigars, and hookah. Tobacco Products; 2016. http://www.fda.gov/TobaccoProducts/Labeling/ucm388395.htm.


