Abstract
Renocutaneous fistulae may occur as a result of chronic infection, especially in the setting of calculous disease.1 Spontaneous renocutaneous is rare.2 Usually nephrocutanous fistula developed in patient with previous renal surgery, trauma, tumors, and chronic urinary tract infection with abscess formation. We report a case of spontaneous nephrocutaneous fistula. A 37-year-old women previously well presented to ER department with purulent discharge and a palpable mass on the left lumbar area. CT scan with IV contrast fistulous tract seen within the subcutaneous plane in Left lumbar region tracking towards retroperitoneal space, and in continuity with of left kidney. The patient underwent ‘Left nephrectomy with excision of fistulous tract’ after long course of antibiotics.
Keywords: Calculus disease, Spontaneous, Renocutaneous, Nephrocutaneous, Fistula, Xanthogranulomatous pyelonephritis
Introduction
Spontaneous renal fistula to adjacent organs is a common phenomenon, however the spontaneous communication between kidney and skin is rare and few cases are described in the literature.3, 4, 5 The occurrence of spontaneous fistulas in patients without surgical history is rare.5 All cases reported in the literature are associated with chronic urinary tract infection and nephrolithiasis. Often the associated renal unit is poorly functioning, and thus definitive treatment is provided by nephrectomy.1
Case report
A 37-year-old woman previously well presented to ER department with purulent discharge and a palpable mass on the left lumbar area. Intermittent purulent pus-like drainage had persisted for the previous 6 months. Although he had general malaise and febrile sensation during that time, proper management had not been applied. She suffered from spikes of fever treated with oral antibiotics. There were no notable medical history including diabetes mellitus, urolithiasis and other comorbidities. She denied any history of indwelling urinary catheter or of the patient undergoing a urinary tract procedure with instrumentation.
Physical examination revealed febrile patient. Left flank mass extending from upper quadrant to back with discharging sinus from lumbar area (Fig. 1).
Figure 1.

Discharging sinus on left lumber area.
Laboratory investigation shows normal kidney function, elevated WBC with left shift urine analysis was free. Patient admitted to hospital. She was given broad spectrum antibiotics and scheduled for CT abdomen and pelvis IV contrast with delayed images.
A computed tomography scan of the abdomen and pelvis revealed a diffusely enlarged destructed left kidney with multiple stones and nephrocutaneous fistula communicating between skin and kidney (Fig. 2). And other kidney appears normal. After long course of antibiotics, no significant response noted. She still has spikes of fever. So she counseled for left open nephrectomy with fistulatomy.
Figure 2.
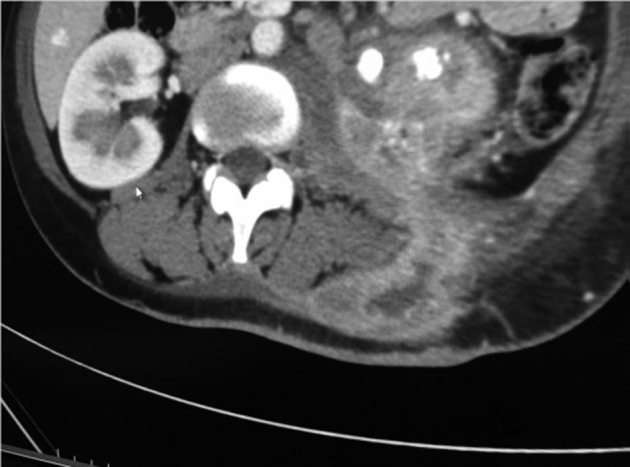
Fistula between kidney and skin through muscle plane.
Total nephrectomy and fistulectomy was successfully performed through a conventional laparotomy. Aortic injury during surgery was repaired immediately. Drain was inserted through fistula tract to back. After surgery, she suffered from mild left pleural effusion with atelectasis treated conservatively.
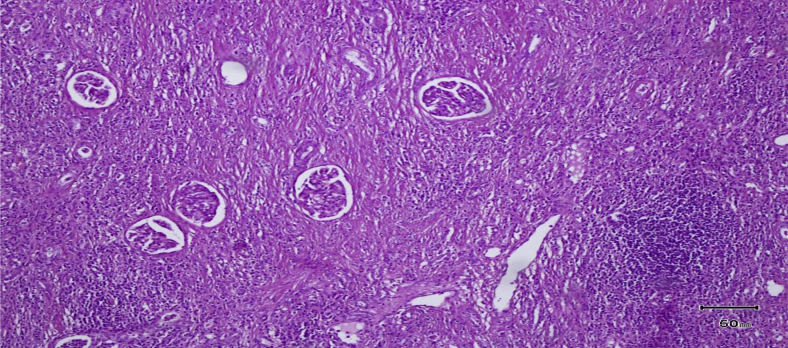
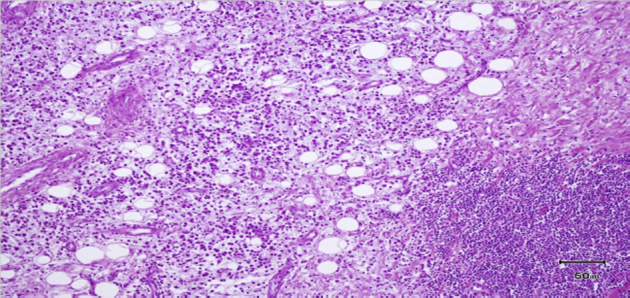
On histopathological examination, chronic granulomatous inflammation with diffuse infiltration of lipid-laden histiocytes was noted, no malignancy founded (Figure 3, Figure 4). The patient was clinically asymptomatic at 12 months of follow-up period. Culture from biopsy has been reported to be E. coli.
Figure 3.
Inflamatory reaction with lipid laden histiocytes infiltration.
Figure 4.
Severe inflammatory reaction involving all kidney.
Discussion
Urinary fistulae have been reported between the kidneys and skin due to a number of causes, including infection, trauma, and stone disease. Infectious causes include xanthogranulomatous pyelonephritis, TB, and renal abscess. Cutaneous fistulae from the urinary tract may arise from the kidney, ureter, bladder, or urethra. Renocutaneous fistulae may occur as a result of chronic infection, especially in the setting of calculous disease. Such abscesses can be derive from organs that are adjacent to the kidney, as well as from the kidney itself, by extension of urinary infection to the adjacent tissues, either by contiguity or by lymphatic route. In other occasions, abscesses can originate from an urinoma that arise as a result of external or surgical trauma on the kidney, promoting loss of continuity between them and the surrounding tissues.4 Currently, the occurrence of renal and perirenal abscesses is rare, except patients with diabetes, with neoplasias or immunodepression in general. Fistulas can develop between the kidney and skin; whenever it occurs, it typically involves patients with a past history of renal surgery.3 The majority of fistulas present as spontaneous drainage through the lumbar region following those points with lowest resistance, such as the lumbar triangle (Petit) and the lumbar quadrilateral (Grynfeld), establishing a fistulous pathway that communicates the perirenal tissues and collecting system with the external environment.2 The association with infectious renal stones is frequent and has occurred in all cases described in the literature.3, 4, 5 The patient in this case had renal calculi in the involved kidney. Therapeutic approaches must be based on the renal function and on the patient's ability to tolerate the surgical procedure, and can include total nephrectomy, partial nephrectomy or isolated antibiotic therapy.5 In the present case, persistent of infection despite long course of antibiotics guide us to perform surgery with total removal of kidney and use of fistula tract as drain to drain pus inside retropertonial area.
Conclusion
Fistula formation due to distal obstruction typically treated with relieve of obstruction. However, in severe cases long standing infection with obstruction cause permanent damage to renal unit, with also present of possibility of presence of malignancy. So it may be necessarily to perform radical treatment to cure patient. Due to few number of cases further study need to evaluate those patients.
Conflict of interest
This case report was done in the division of urology for academic purposes and was not funded by any external fund, the submission has no commercial interests, and the authors of this case report are not linked to any external agencies.
Footnotes
Statement of Originality: The material printed in this case report has not been previously submitted for another journal, and to the best of my knowledge contains no material previously published or written by another person except where due acknowledgement is made in the case report itself.
References
- 1.Rovner ES. Urinary Tract Fistulae. In: Wein AJ, Kavoussi LR, Novick AC, et al., Editors. Campbell-Walsh Urology. 10th ed: Saunders, an imprint of Elsevier Inc.; 2012. 77, P. 2261.
- 2.Bryniak S.R. Primary spontaneous renocutaneous fistula. Urology. 1983;21:516–517. doi: 10.1016/0090-4295(83)90056-0. [DOI] [PubMed] [Google Scholar]
- 3.Sarmiento R.C., Blasco C.F., Herrera F.F. Spontaneous nephrocutaneous fistula. Report of a case and review of the literature. Arch Esp Urol. 1990;43:411–413. [PubMed] [Google Scholar]
- 4.Singer A.J. Spontaneous nephrocutaneous fistula. Urology. 2002;60:1109–1110. doi: 10.1016/s0090-4295(02)01972-6. [DOI] [PubMed] [Google Scholar]
- 5.Haney P.T., Bihrle R., Kopecky K.K. Percutaneous management of a nephrocutaneous fistula due to a pyelocaliceal diverticular calculus. J Urol. 1992;148(3 Pt. 2):1105–1107. doi: 10.1016/s0022-5347(17)36832-5. [DOI] [PubMed] [Google Scholar]