Abstract
Background
The Affordable Care Act requires hospices to report quality measures across a range of processes and practices. Yet uncertainties exist regarding the impact of hospice preferred practices on patient outcomes.
Objective
Assess the impact of six hospice preferred practices and hospice organizational characteristics on hospital utilization and death using the first national data on hospice preferred practices.
Design
Longitudinal cohort study (2008–2011) of Medicare beneficiaries (N=149,814) newly enrolled in a national random sample of hospices (N=577) from the National Hospice Survey (84% response rate) and followed until death.
Outcome Measures
The proportion of patients at each hospice admitted to the hospital, emergency department (ED), and intensive care unit (ICU), and who died in the hospital after hospice enrollment.
Results
Hospices that reported assessing patient preferences for site of death at admission had lower odds of being in the highest quartile for hospital death (AOR=0.36, 95% CI 0.14, 0.93) and ED visits (AOR=0.27, 95%CI 0.10–0.76). Hospices that reported more frequently monitoring symptoms had lower odds of being in the highest quartile for ICU stays (AOR=0.48, 95%CI 0.24–0.94). In adjusted analyses, a higher proportion of patients at for-profit compared with nonprofit hospices experienced a hospital admission (15.3% versus 10.9%, P<0.001), ED visit (21.8% versus 15.6%, P<0.001), and ICU stay (5.1% versus 3.0%, P<0.001).
Conclusions
Hospitalization of patients following hospice enrollment varies substantially across hospices. Two of the six preferred practices examined were associated with hospitalization rates and for-profit hospices had persistently high hospitalization rates regardless of preferred practice implementation.
INTRODUCTION
The Affordable Care Act required the Secretary of Health and Human Services to establish quality reporting measures for hospice programs in the U.S. Under this Hospice Quality Reporting Program, all Medicare certified hospices are required to report quality measures related to pain and symptom screening and assessment, and the elicitation of patient preferences and spiritual or existential concerns in order to avoid a reduction of their annual payment update. The initiation of hospice quality reporting and the linking of reporting to reimbursement provides an incentive to improve the quality of care provided to the 1.65 million individuals1 who receive hospice care each year, a group that has dramatically increased in both size and diversity in the past decade.2
Recent evidence regarding hospice quality3 has used measures derived from the work of the National Quality Forum, which endorsed a set of preferred practices for palliative and hospice care quality aimed at improving palliative and hospice care across the Institute of Medicine’s six dimensions of quality—safe, effective, timely, patient centered, efficient, and equitable.4 This evidence3 suggests that the implementation of hospice preferred practices such as the frequency of pain and symptom monitoring, existence of an on-call physician both evenings and weekends, and the timing of the assessment of patient preferences for care varied significantly by hospice characteristics. Specifically, our prior work using data from the National Hospice Survey found that the range of reported implementation of individual preferred practices among hospices was 45% to 97%.3 In adjusted analyses, larger hospices (100 or more patients per day) were significantly more likely than smaller hospices to report having implemented preferred practices, and, similarly, chain-affiliated hospices were significantly more likely than free-standing hospices to report having implemented preferred practices.3 What is missing from our prior work but is essential to building the evidence base for quality-based performance measurement is the link between specific hospice practices and patient and family outcomes at the end of life.
Accordingly, we sought to examine the associations between preferred hospice practices and hospitalization following hospice enrollment. Using data from the National Hospice Survey, we measured the reported use of hospice practices recommended by the National Quality Forum and the National Consensus Project and similar to those now utilized by the Hospice Quality Reporting Program. We measured outcomes using Medicare claims data from hospice enrollment to death for all patients cared for by the hospices in our survey. In doing so, we report the first national data on the link between hospice practices and outcomes for patients receiving hospice care. In addition, we report the association between hospice characteristics (including ownership, size and region) and these outcomes given the increasing body of evidence regarding variation in outcomes across hospice provider types.3, 5–12 Given that hospices have been required to report the Hospice Quality Reporting Program measures since July 2014, it is imperative to understand how these practices may relate to the care of patients at the end of life.
METHODS
Study Design and Sample
We conducted a longitudinal study using data for hospices that responded to our previously completed National Hospice Survey, linked to Medicare claims data for beneficiaries newly enrolled in responding hospices during the survey period September 2008 to November 2009 (N=213,495). A total of 577 (98%) hospices in our survey were linked to Medicare claims data for beneficiaries; for 14 hospices, Medicare claims were unavailable, primarily because the hospice had merged/closed during the survey period. We excluded patients younger than age 66 (N=15,003) to ensure that individuals were eligible for Medicare in the year prior to hospice enrollment so that we could access data on comorbidities as possible confounding variables. We excluded patients not eligible for both Medicare Parts A and B (N=2,111) or who were enrolled in a managed care organization (N=46,567); eligibility for Medicare Part B is important for establishing outpatient claims and diagnoses for more accurate assessment of comorbidities,13 as has been done in previous research.6, 14–16 Medicare managed care enrollees were not included because their claims and utilization data are not available in Medicare claims data. After our exclusion criteria were applied, our final sample was comprised of 149,814 individuals cared for by 577 hospices.
National Hospice Survey Instrument and Claims Based Measures
As reported elsewhere,3, 11, 17 the National Hospice Survey was a national random sample of hospices surveyed between September 2008 and November 2009. We chose the random sample of hospices from the Medicare Provider of Services files, which include all hospices that participate in the Medicare program. We have completed surveys from 591 hospices, representing an 84% response rate, and representing approximately 20% of all Medicare certified hospices in the U.S. operating in 2009.
We developed the National Hospice Survey instrument after a comprehensive review of published guidelines from the National Quality Forum and the National Consensus Project and included preferred practices that were specific to hospice care and that were measurable at the level of the hospice agency. Given that the guidelines were relatively new at the time of our survey development, they at times lacked specific operational metrics for defining high quality practices. In these instances, we operationalized these measures to enable their assessment. For example, the National Consensus Project guideline 2.1 calls for “regular, ongoing assessment of pain [and] nonpain symptoms…”18 Our National Hospice Survey measure is whether or not a hospice measures pain at least every few days and symptoms at least every few days. Questions relating to the frequency with which hospices monitor pain and symptoms are specific to patients receiving hospice in a home rather than an inpatient hospice setting, given that more than 93% of hospice patient care days are provided in a home setting.19 The survey instrument consisted predominantly of closed-ended items and was pre-tested with 16 hospices to assess the clarity and comprehensiveness of survey questions using cognitive interviews with pre-test respondents. In this analysis we included preferred practices (Table 1) reported by hospices that we hypothesized to be related to the following hospital utilization-based outcomes: hospitalization, emergency department (ED) visits, intensive care unit (ICU) admissions, and hospital death. In addition, we evaluated hospitalizations and ED visits within the first 2 weeks after hospice enrollment as these outcomes are more proximal to the hospice admission procedures.
Table 1.
National Hospice Survey Preferred Practice Measures
| National Hospice Survey Question | Response | |
|---|---|---|
| 1. | Does your hospice have a physician on-call 24 hours per day, 7 days per week to provide clinical advice to family caregivers? Response: yes, no | Yes 82% |
| 2. | How often does your hospice staff monitor pain for patients who are receiving hospice in the home? Response: daily, every few days, weekly, less often | Daily/Every few days 87% |
| 3. | How often does your hospice staff monitor each of the following symptoms (anxiety, constipation, delirium, depression, dyspnea, fatigue, nausea) for patients who are receiving hospice in the home? Response: daily, every few days, weekly, less often | Daily/Every few days 71% |
| 4. | How often are patient goals of care included in discussions of patients’ plans of care? (Check all that apply) Response: at initial admission, when clinical conditions change, on a routine schedule, not discussed | At initial admission 80% |
| 5. | How often are family preferences for care included in discussions of patients’ plans of care? (Check all that apply) Response: at initial admission, when clinical conditions change, on a routine schedule, not discussed | At initial admission 83% |
| 6. | How often are patient preferences for place of death included in discussions of patients’ plans of care? (Check all that apply) Response: at initial admission, when clinical conditions change, on a routine schedule, not discussed | At initial admission 83% |
The survey also included questions regarding descriptive characteristics of hospices including: ownership (for-profit, nonprofit, government/other), whether the hospice was part of a chain of hospices, size (number of patients per day in the past 12 months), proportion of patients served in the nursing home, and the census region of the hospice.
We used Medicare hospice claims data to obtain patient demographic and clinical characteristics including age (categorized as 65–69, 70–74, 75–79, 80–84, and >=85 years), gender, race/ethnicity (white, black, other), and primary diagnosis based on International Classification of Diseases, Ninth Revision (ICD-9) codes. We obtained information regarding the number of chronic conditions by examining all Medicare hospital inpatient and outpatient claims for each individual for the 12 months prior to their hospice enrollment. We measured hospice length of stay for each patient using the Medicare hospice claims data.
We also used Medicare claims data to measure the following utilization based outcomes from the time of a beneficiary’s hospice enrollment to his/her death: one or more hospitalizations, one or more ED visits, ICU admission, and hospital death.
Statistical Analysis
Our prior work estimated the proportion of hospices that reported having implemented each of the preferred practices shown in Table 1.3 Using the patient-level Medicare claims data, we estimated the characteristics of each hospice’s patient population as follows: average age, percent female, percent white race, percent with cancer as primary diagnosis, percent with a mental disorder as primary diagnosis, average number of chronic conditions, and median length of hospice stay. We estimated the proportion of each hospice’s patients who experienced the following utilization-based outcomes from the time of their hospice enrollment to their death: one or more hospitalizations, one or more ED visits, ICU admission, and hospital death. We evaluated the distribution of these outcomes across hospices and identified hospices in the top quartile for each outcome.
We used multivariable logistic regression models at the level of the hospice to estimate the adjusted associations between a hospice being in the top quartile of the distribution for a utilization-based outcome and each hospice preferred practice, controlling for hospice organizational characteristics (ownership, chain affiliation, size, urban location and region) and patient population characteristics (average age, percent female, percent white race, percent with a primary diagnosis of cancer, percent with a primary diagnosis of a mental disorder, percent of patients cared for in a nursing home, average number of chronic conditions, and median length of hospice stay). To determine the impact of hospice preferred practices during the initial 2 weeks following enrollment, we re-estimated the multivariable logistic regression model evaluating the hospitalization and ED outcomes after limiting the timeframe to the first 2 weeks after hospice enrollment.
We used multivariable linear regression models at the level of the hospice to estimate the adjusted associations between the existence of hospice preferred practices and the proportion of patients hospitalized, admitted to the ED, admitted to the ICU, or who died in the hospital, controlling for hospice organizational and patient population characteristics. We used the margins post-estimation command to estimate the adjusted proportions of each hospitalization outcome by hospice organizational and patient population characteristics. We performed analyses using SAS software, version 9.3 (SAS Institute, Cary, North Carolina) and Stata software, version 13.
RESULTS
Study Population
Our sample of Medicare beneficiaries was composed of 149,814 patients who were newly enrolled with one of the 577 hospices that responded to the National Hospice Survey (Table 2). The majority of our sample was older than 80 years, female, and white. Approximately one-third of the sample had a primary diagnosis of cancer, one-fifth had a primary diagnosis of a disease of the circulatory system and almost all individuals had more than one chronic condition. The median length of hospice stay for this cohort was 16 days and the interquartile range was 4 to 77 days. The demographic and clinical characteristics of our sample of hospice users as well as the characteristics of the sampled hospice providers are consistent with those of the overall population of Medicare beneficiaries using hospice and Medicare certified hospice providers.2, 20–21
Table 2.
Characteristics of Sampled Hospices and Hospice Patients
| Patients (N=149,814) | |
| Age | No. (%) |
| 65–69 | 10,401 (7) |
| 70–74 | 16,292 (11) |
| 75–79 | 22,682 (15) |
| 80–84 | 31,280 (21) |
| ≥85 | 69,159 (46) |
| Gender | |
| Female | 88,960 (59) |
| Male | 60,854 (41) |
| Race | |
| White | 133,966 (89) |
| Black | 11,072 (7) |
| Other | 4,776 (4) |
| Primary Diagnosis | |
| Neoplasms | 48,904 (33) |
| Mental disorders | 12,702 (8) |
| Diseases of the nervous system and sense organs | 11,617 (8) |
| Diseases of the circulatory system | 28,587 (19) |
| Diseases of the respiratory system | 13,869 (9) |
| Symptoms, signs, and ill-defined conditions | 24,220 (16) |
| Other | 9,915 (7) |
| Hospices (N=577) | |
| No. (%) | |
| Hospice Ownership | |
| For-profit | 273 (47) |
| Nonprofit | 281 (49) |
| Government/other | 23 (4) |
| Hospice Size: (Avg. number patients per day) | |
| <20 | 154 (27) |
| 20–49 | 153 (27) |
| 50–99 | 148 (26) |
| ≥100 | 122 (21) |
| Hospice is a member of a chain | 138 (24) |
| Location | |
| Urban | 397 (69) |
| Suburban/Rural | 180 (31) |
| Region | |
| New England | 28 (5) |
| Middle Atlantic | 39 (7) |
| Eastern North Central | 91 (16) |
| Western North Central | 69 (12) |
| South Atlantic | 92 (16) |
| Eastern South Central | 59 (10) |
| Western South Central | 100 (17) |
| Mountain | 48 (8) |
| Pacific | 51 (9) |
The sample of hospices from the National Hospice Survey has been described elsewhere.3, 11, 17 Approximately half were for-profit, one-quarter were part of a chain of hospices, two-thirds were located in an urban area, and approximately half had fewer than 50 patients per day on average (Table 2). The average proportion of patients per day cared for in their place of residence was 94.6 percent (standard deviation 15.1) including 25.3 percent (standard deviation 21.8) in a nursing home.
Variation among Hospice Providers in Hospitalization-Based Outcomes
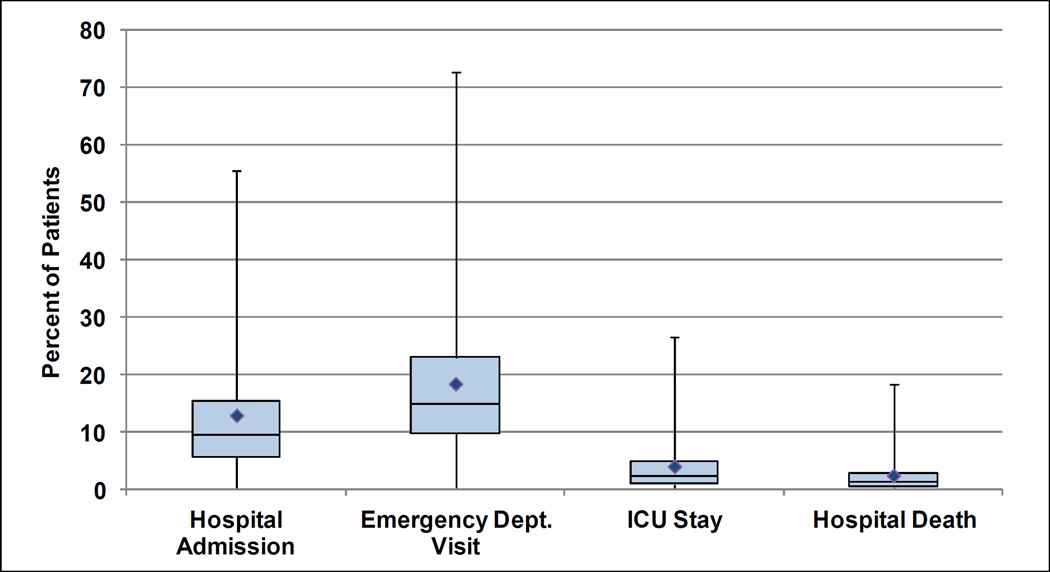
The variation in outcomes among hospice providers is shown in Figure 1. The average proportion of patients at each hospice who were admitted to the hospital was 12.8% (standard deviation (SD) 11.6%), and ranged from 0% of patients at some hospices to 55.6% (the 99th percentile) at other hospices. The average proportion of patients with ED visits was 18.3% (SD 13.0%), and ranged from 0% of patients at some hospices to 72.7% (the 99th percentile) at other hospices. For ICU stays and hospital death, the proportions were smaller. The average proportion of patients at each hospice who spent time in the ICU was 3.9% (SD 5.2%), and ranged from 0% of patients at some hospices to 26.6% (the 99th percentile) at other hospices and the average proportion of patients at each hospice who died in the hospital was 2.3% (SD 3.5%) ranging from 0% of patients to 18.2% (the 99th percentile) of patients.
Figure 1. Variation Among Hospices in the Proportion of Patients with Each Hospital Utilization-Based Outcome.
This figure is a box-plot describing the distribution of the proportion of patients with each hospital-based outcome among the hospices in our sample. The bottom and top of the box represent the first and third quartiles of the distribution and the band inside the box is the second quartile or median. The diamond represents the mean. The ends of the lines represent the first and ninety-ninth percentile values of the distribution.
The average proportion of patients across hospices with hospitalizations in the first 2 weeks following hospice enrollment was as follows: hospital admission 2.2% (SD 3.5%) and ED visits 3.9% (SD 4.4%).
Hospice Preferred Practices
In multivariable models, two of the six hospice preferred practices examined were statistically significantly associated with hospitalization outcomes (Table 3). Hospices that reported assessing patient preferences for site of death were less likely to be in the highest quartile for the proportion of patients who die in the hospital (OR=0.36, 95% CI 0.14, 0.93) and the proportion of patients who visit the ED (OR=0.27, 95%CI 0.10, 0.76). In addition, hospices that reported monitoring symptoms at least every few days were less likely to be in the highest quartile for the proportion of patients admitted to the ICU (OR=0.48, 95% CI 0.24, 0.94) than hospices that monitored symptoms less frequently. The unadjusted and adjusted proportions of patients hospitalized did not significantly differ across hospices with and without the measured preferred practices (not shown).
Table 3.
Adjusted Association Between Reported Hospice Preferred Practices and Hospital Utilization-Based Outcomesa
| Hospital Admission |
Emergency Dept. Visit |
Intensive Care Unit Stay |
Hospital Death |
|
|---|---|---|---|---|
| Adjusted Odds Ratio (95%CI) | ||||
| Preferred Practices | ||||
| Physician on-call 24/7 | 0.86 (0.39–1.89) | 1.21 (0.52–2.79) | 1.04 (0.48–2.26) | 1.05 (0.49–2.23) |
| Monitor pain at least every few days | 1.09 (0.36–3.35) | 0.93 (0.29–2.95) | 2.03 (0.77–5.38) | 2.44 (0.92–6.50) |
| Monitor symptoms at least every few days | 1.17 (0.52–2.64) | 1.27 (0.56–2.90) | 0.48 (0.24–0.94)† | 0.61 (0.30–1.21) |
| Patient goals of care assessed at admission | 2.01 (0.68–5.96) | 1.52 (0.52–4.44) | 0.58 (0.22–1.56) | 1.14 (0.43–3.00) |
| Family preferences for care assessed at admission | 0.96 (0.27–3.50) | 1.82 (0.48–6.86) | 2.39 (0.71–8.10) | 1.88 (0.58–6.12) |
| Patient preferences for site of death assessed at admission | 0.47 (0.17–1.29) | 0.27 (0.10–0.76)† | 0.47 (0.18–1.24) | 0.36 (0.14–0.93)† |
| Patient Population Characteristics | ||||
| Average age | 0.87 (0.78–0.98)† | 0.90 (0.81–1.00) | 0.96 (0.87–1.06) | 0.99 (0.90–1.10) |
| Percent female | 0.98 (0.94–1.01) | 0.96 (0.92–0.99)† | 0.96 (0.93–1.00)† | 0.98 (0.95–1.01) |
| Percent white race | 0.97 (0.95–0.99)* | 0.97 (0.95–1.00)† | 0.98 (0.96–1.00)† | 0.97 (0.95–0.99)* |
| Percent with cancer as primary diagnosis | 0.98 (0.95–1.01) | 0.95 (0.92–0.98)* | 0.99 (0.96–1.02) | 0.98 (0.95–1.00) |
| Percent with mental disorder as primary diagnosis | 0.97 (0.93–1.02) | 0.98 (0.94–1.03) | 1.00 (0.96–1.04) | 0.96 (0.93–1.00) |
| Average number of chronic conditions | 1.31 (0.82–2.09) | 1.22 (0.78–1.97) | 1.45 (0.94–2.22) | 1.08 (0.72–1.64) |
| Percent of patients in nursing home | 0.99 (0.98–1.01) | 0.99 (0.98–1.01) | 0.98 (0.97–1.00)† | 0.99 (0.97–1.00)† |
| Median patient length of stay | 1.06 (1.04–1.07)* | 1.05 (1.03–1.07)* | 1.03 (1.02–1.04)* | 1.02 (1.01–1.03)* |
| Hospice Characteristics | ||||
| For-profit hospice ownership | 2.77 (1.33–5.76)* | 2.58 (1.22–5.45)† | 2.56 (1.30–5.03)* | 1.74 (0.91–3.34) |
| Hospice is a member of a chain | 0.76 (0.38–1.51) | 0.60 (0.30–1.20) | 0.97 (0.52–1.83) | 0.95 (0.51–1.78) |
| Hospice size (patients per day) | ||||
| <20 | Reference | Reference | Reference | Reference |
| 20–49 | 1.17 (0.53–2.58) | 1.12 (0.49–2.55) | 2.27 (1.05–4.89)† | 1.53 (0.75–3.14) |
| 50–99 | 1.02 (0.44–2.38) | 1.01 (0.43–2.40) | 1.63 (0.72–3.69) | 0.84 (0.38–1.85) |
| ≥100 | 0.55 (0.20–1.53) | 0.65 (0.23–1.83) | 1.39 (0.54–3.56) | 0.75 (0.30–1.86) |
| Urban location | 0.48 (0.25–0.94)† | 0.56 (0.28–1.10) | 0.63 (0.33–1.19) | 0.41 (0.23–0.76)* |
| Region | ||||
| South Atlantic | Reference | Reference | Reference | Reference |
| New England/Middle Atlantic | 0.52 (0.16–1.70) | 0.54 (0.15–1.96) | 0.28 (0.07–1.03) | 0.34 (0.10–1.11) |
| North Central | 0.16 (0.06–0.46)* | 0.20 (0.07–0.59)* | 0.34 (0.14–0.84)† | 0.12 (0.04–0.34)* |
| South Central | 1.18 (0.54–2.55) | 1.36 (0.61–3.04) | 1.20 (0.58–2.47) | 1.24 (0.62–2.47) |
| Mountain/Pacific | 0.32 (0.12–0.86)† | 0.42 (0.16–1.14) | 0.55 (0.23–1.31) | 0.51 (0.22–1.19) |
The dependent variable for each multivariable logistic regression model is the hospice being in the highest quartile of the distribution for the outcome.
P<0.05;
P<0.01
Hospice Characteristics
For-profit hospice ownership was significantly associated with three of the four hospitalization-based outcomes (Table 3). In adjusted analyses, for-profit hospices had more than twice the odds of being in the highest quartile for hospitalizations, ED visits, and ICU stays. In addition, both the unadjusted and adjusted proportions of patients experiencing a hospital admission, ED visit and ICU stay were higher at for-profit compared with nonprofit hospices (Table 4).
Table 4.
Unadjusted and Adjusted Proportion of Hospital Admission, Emergency Department Visits, Intensive Care Unit Stays, and Hospital Death by Hospice Characteristics
| Proportion with Hospital Admission |
Proportion with Emergency Dept. Visit |
Proportion with Intensive Care Unit Stay |
Proportion with Hospital Death |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | |||||||||
| Hospice Characteristics | ||||||||||||||||
| Hospice Ownership | ||||||||||||||||
| For-profit | 18.1 | 15.3 | 24.7 | 21.8 | 5.9 | 5.1 | 3.2 | 2.6 | ||||||||
| Nonprofit | 8.1 | * | 10.9 | * | 12.7 | * | 15.6 | * | 2.1 | * | 3.0 | * | 1.5 | * | 2.1 | |
| Chain Affiliation | ||||||||||||||||
| Chain | 13.8 | 11.7 | 19.7 | 17.0 | 4.5 | 3.6 | 2.3 | 2.0 | ||||||||
| Non-chain | 12.5 | 13.5 | 17.9 | 19.1 | † | 3.7 | 4.1 | 2.3 | 2.5 | |||||||
| Hospice size (patients per day) | ||||||||||||||||
| <20 (reference) | 14.1 | 13.6 | 19.9 | 19.5 | 3.9 | 3.9 | 2.9 | 2.6 | ||||||||
| 20–49 | 13.3 | 13.2 | 18.4 | 18.2 | 4.1 | 4.0 | 2.6 | 2.6 | ||||||||
| 50–99 | 13.4 | 13.0 | 18.9 | 18.5 | 4.0 | 3.9 | 2.1 | 2.1 | ||||||||
| >=100 | 10.0 | * | 12.1 | 15.7 | † | 18.2 | 3.5 | 4.2 | 1.6 | * | 2.2 | |||||
| Location | ||||||||||||||||
| Urban | 12.7 | 12.5 | 18.2 | 18.1 | 4.0 | 4.0 | 2.2 | 2.2 | ||||||||
| Suburban/Rural | 13.2 | 14.3 | † | 18.6 | 19.7 | 3.7 | 4.1 | 2.6 | 2.8 | |||||||
| Region | ||||||||||||||||
| South Atlantic (reference) | 16.1 | 14.4 | 22.5 | 20.9 | 5.3 | 4.8 | 3.0 | 2.6 | ||||||||
| New Engl/Middle | ||||||||||||||||
| Atlantic | 8.8 | * | 13.3 | 12.8 | * | 18.4 | 2.4 | * | 4.1 | 1.6 | * | 2.8 | * | |||
| North Central | 7.9 | * | 10.9 | * | 13.1 | * | 16.3 | * | 2.0 | * | 3.3 | † | 1.0 | * | 1.6 | |
| South Central | 19.3 | † | 15.8 | 25.0 | 21.3 | 6.0 | 4.7 | 3.8 | 3.1 | |||||||
| Mountain/Pacific | 10.2 | * | 10.4 | * | 16.0 | * | 15.8 | * | 3.4 | * | 3.2 | † | 2.0 | † | 1.9 | |
P<0.05;
P<0.01
The adjusted proportion of each outcome was calculated including the following covariables: the existence of hospice preferred practices (physician on-call 24/7, monitoring of pain at least every few days, monitoring of symptoms at least every few days, patient goals of care assessed at admission, family preferences for care assessed at admission, and patient preferences for site of death assessed at admission), characteristics of the hospice’s patient population (average age, percent female, percent white race, percent with cancer as primary diagnosis, percent with mental disorder as primary diagnosis, average number of chronic conditions percent of patients in the nursing home, and median length of hospice stay) and characteristics of the hospice (ownership, chain affiliation, size, urban location and region).
Other measured hospice characteristics were not consistently significantly associated with the hospitalization-based outcomes (Table 3). Notable exceptions were hospice urban location which was associated with lower odds of being in the highest quartile for hospital admissions and hospital death and regional variation finding that hospices in the North Central region had lower odds of being in the highest quartile for hospitalization, ED visits, ICU stays and hospital death than hospices in the South Atlantic region. The unadjusted and adjusted proportions of patients hospitalized yielded similar results for urban location and region (Table 4). Urban hospices had significantly lower proportions of patients hospitalized and visiting the ED compared with surburban/rural hospices. By region, hospices in the North Central and Mountain/Pacific regions had the lowest adjusted proportions of hospital admissions and ED visits of their patients.
DISCUSSION
We found that two of the six examined hospice preferred practices were associated with significantly lower hospitalization of patients following hospice enrollment. Specifically, hospices that reported assessing patient preferences for site of death at admission were less likely to be in the highest quartile for hospital death and ED use and hospices that reported monitoring symptoms more frequently were less likely to be in the highest quartile for ICU stays for their patient population. The other four examined preferred practices were not associated with hospitalization based outcomes. In addition, we found that despite preferred practice implementation, there was significant variation across hospices in hospitalization rates including higher hospitalization rates at for-profit hospices, and hospices in suburban or rural areas.
This magnitude of hospice level variation in outcomes is critical to understand as we move forward with quality reporting requirements and quality-based reimbursement measures. Our results suggest that although some preferred practices are moderately related to utilization based outcomes, it is the organization of the hospice itself in terms of ownership, and location that likely drive policies and decisions regarding hospitalization. This is consistent with our prior work3 which finds that some of these same characteristics explain variation in the implementation of preferred practices. Our current findings suggest that factors such as financial incentives relating to the hospitalization of hospice patients play out differently across hospice provider types and dominate the impact of preferred practices on outcomes. Specifically, the consistent positive association between for-profit ownership and hospitalization after accounting for variation in patient population characteristics (including length of hospice stay, case mix, and the proportion cared for in a nursing home) suggests that the hospitalization of individuals who had enrolled with hospice may be a means of shifting costs of care from the hospice organization to Medicare. Further research evaluating this issue is needed.
Our results are consistent with mounting evidence that factors beyond patient acuity and clinical characteristics affect healthcare utilization at the end of life.22–24 Treatment intensity at the end of life, as measured by hospitalizations, ICU use, and site of death, has significantly increased been 2000 and 2009.25 Despite the fact that use of hospice has been found to reduce these measures of treatment intensity,26–27 our results demonstrate fairly high rates of hospitalization and ED use within a subset of hospices in our sample even after controlling for patient population characteristics including primary diagnosis, number of comorbidities, and length of hospice stay. Although we identify specific hospice practices that may reduce hospitalizations, greater understanding of the hospitalization decision from the patient’s perspective, the family’s perspective and the hospice’s perspective is needed.
There are several limitations to our study. One limitation of this analysis is that the National Hospice Survey data regarding preferred practices were self-reported by hospices and thus may over or under estimate the true prevalence of preferred practices. Second, neither the National Hospice Survey data nor the Medicare hospice claims data include information regarding the frequency with which clinical care processes were received by patients. We also do not know the content of patient and family preferences for care and thus the congruence of hospitalization outcomes with care preferences, however, we would expect such preferences for or against hospitalization to be fairly evenly distributed across hospices. Similarly, we do not have data on other important patient and family outcomes such as satisfaction with care, pain and other symptoms, and quality of life. In addition, the National Quality Forum guidelines were relatively new at the time of our survey development and, in some cases, lacked specific operational metrics for defining high quality practices. A strength of our study, however, is that we operationalized and then measured these preferred practices and established a baseline for future assessments of hospices’ implementation of preferred practices. It is possible that hospice preferred practices changed during the follow-up period, however, although our entire follow-up period ended in 2011, the median number of days in hospice for this cohort was only 16, with an inter-quartile range of 4 to 77 days. Ninety percent of patients had died within 240 days. Therefore, for the vast majority of patients, outcomes were assessed within 8 months of our quality assessment. Given that our study is observational, another limitation is that there may be unmeasured confounders, however, we have included a fairly comprehensive set of both hospice and patient population characteristics in our multivariable models. Finally, our results are not generalizable to the approximately 7% of hospices in the U.S. that do not participate in the Medicare program,1 hospice users who are not Medicare beneficiaries, and hospice users who are enrolled in managed care organizations.
Numerous studies indicate that the majority of individuals in the U.S prefer not to have intensive hospital-based care when they die28–29 and would prefer to die at home.30–32 Individuals who die at home have been found to have greater quality of life and fewer unmet needs compared with those who die in the hospital.33–34 Transitions to the hospital at the end of life can lead to aggressive interventions, medical errors, and adverse reactions for patients.35–36 Even caregivers of individuals who die at home with hospice have been found to have improved outcomes compared with caregivers of those who die in the ICU.25 We found that some practices – namely assessing patient preferences for site of death at hospice admission and more frequent symptom monitoring – reduce hospitalizations and thus may be important to implement for the 17% and 29%, respectively, of hospices who may not already engage in these practices. Policy levers including monitoring, licensure, or payment reform linked to the implementation of these types of hospice practices may provide incentives for greater implementation. Our results also highlight the need to better understand the practices of for-profit hospices where the pattern of high hospitalization of patients is persistent, regardless of preferred practice implementation. The substantial hospice level variation in hospitalization-based outcomes identified in this study underscores the need to better understand the drivers of inter-hospice variation, to develop quality measures based on these determinants, and to create incentives for high performance on quality measures to improve the experiences of patients and families at the end of life.
Acknowledgments
Funding/Support: This study was supported by the National Institute of Nursing Research 5R01NR013499 (Aldridge); the National Cancer Institute 1R01CA116398-01A2 (Bradley) and the John D. Thompson Foundation (Bradley).
Footnotes
Presentations: The results of this study were reported at the AcademyHealth Annual Research Meeting in June as part of a panel, “The Evolution of Medicare’s Hospice Benefit: Implications for Service Use, Quality Measurement, and Payment Reform” and at the American Academy of Hospice and Palliative Medicine’s Annual Research Meeting in February 2015.
Contributor Information
Melissa D. Aldridge, Department of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai, One Gustave L. Levy Place, Box 1070, New York, NY 10029 and Geriatrics Research, Education and Clinical Center, James J. Peters Veterans Affairs Medical Center, Bronx, NY.
Andrew J. Epstein, Perelman School of Medicine, University of Pennsylvania 423 Guardian Dr, 1001 Blockley Hall, Philadelphia, PA 19104.
Abraham A. Brody, New York University College of Nursing, 726 Broadway, Room 1075, New York, NY 10003 and Geriatrics Research, Education and Clinical Center, James J. Peters Veterans Affairs Medical Center, Bronx, NY
Eric J. Lee, Department of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai, One Gustave L. Levy Place, Box 1070, New York, NY 10029
Emily Cherlin, Department of Epidemiology and Public Health, Yale School of Public Health, 2 Church Street South, Suite 409, New Haven, CT 06520.
Elizabeth H. Bradley, Department of Epidemiology and Public Health, Yale School of Public Health, 55 Hillhouse, New Haven, CT 06520
REFERENCES
- 1.National Hospice and Palliative Care Organization. NHPCO Facts and Figures: Hospice Care in America. [Accessed November 2013];2013 Available at: http://www.nhpco.org/sites/default/files/public/Statistics_Research/2013_Facts_Figures.pdf. [Google Scholar]
- 2.Aldridge MD, Canavan M, Cherlin E, Bradley EH. Has Hospice Use Changed? 2000–2010 Utilization Patterns. Med Care. 2015 Jan;53(1):95–101. doi: 10.1097/MLR.0000000000000256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carlson MD, Barry C, Schlesinger M, et al. Quality of palliative care at US hospices: results of a national survey. Med Care. 2011 Sep;49(9):803–809. doi: 10.1097/MLR.0b013e31822395b2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Quality Forum. A National Framework and Preferred Practices for Palliative and Hospice Care Quality. Washington, DC: 2006. [Google Scholar]
- 5.Carlson MD, Gallo WT, Bradley EH. Ownership status and patterns of care in hospice: results from the National Home and Hospice Care Survey. Med Care. 2004 May;42(5):432–438. doi: 10.1097/01.mlr.0000124246.86156.54. [DOI] [PubMed] [Google Scholar]
- 6.Carlson MD, Herrin J, Du Q, et al. Hospice characteristics and the disenrollment of patients with cancer. Health Serv Res. 2009 Dec;44(6):2004–2021. doi: 10.1111/j.1475-6773.2009.01002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carlson MD, Morrison RS, Holford TR, Bradley EH. Hospice care: what services do patients and their families receive? Health Serv Res. 2007 Aug;42(4):1672–1690. doi: 10.1111/j.1475-6773.2006.00685.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cherlin EJ, Carlson MD, Herrin J, et al. Interdisciplinary staffing patterns: do for-profit and nonprofit hospices differ? J Palliat Med. 2010 Apr;13(4):389–394. doi: 10.1089/jpm.2009.0306. [DOI] [PubMed] [Google Scholar]
- 9.Wachterman MW, Marcantonio ER, Davis RB, McCarthy EP. Association of hospice agency profit status with patient diagnosis, location of care, and length of stay. JAMA. 2011 Feb 2;305(5):472–479. doi: 10.1001/jama.2011.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Teno JM, Plotzke M, Gozalo P, Mor V. A National Study of Live Discharges from Hospice. J Palliat Med. 2014 Aug 7; doi: 10.1089/jpm.2013.0595. [DOI] [PubMed] [Google Scholar]
- 11.Aldridge MD, Schlesinger M, Barry CL, et al. National hospice survey results: for-profit status, community engagement, and service. JAMA Intern Med. 2014 Apr 1;174(4):500–506. doi: 10.1001/jamainternmed.2014.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lorenz KA, Ettner SL, Rosenfeld KE, Carlisle DM, Leake B, Asch SM. Cash and compassion: profit status and the delivery of hospice services. J Palliat Med. 2002 Aug;5(4):507–514. doi: 10.1089/109662102760269742. [DOI] [PubMed] [Google Scholar]
- 13.Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000 Dec;53(12):1258–1267. doi: 10.1016/s0895-4356(00)00256-0. [DOI] [PubMed] [Google Scholar]
- 14.Earle CC, Neville BA, Landrum MB, Ayanian JZ, Block SD, Weeks JC. Trends in the aggressiveness of cancer care near the end of life. J Clin Oncol. 2004 Jan 15;22(2):315–321. doi: 10.1200/JCO.2004.08.136. [DOI] [PubMed] [Google Scholar]
- 15.Legler A, Bradley EH, Carlson MD. The Effect of Comorbidity Burden on Health Care Utilization for Patients with Cancer Using Hospice. J Palliat Med. 2011 May 6; doi: 10.1089/jpm.2010.0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carlson MD, Herrin J, Du Q, et al. Impact of hospice disenrollment on health care use and medicare expenditures for patients with cancer. J Clin Oncol. 2010 Oct 1;28(28):4371–4375. doi: 10.1200/JCO.2009.26.1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aldridge Carlson MD, Barry CL, Cherlin EJ, McCorkle R, Bradley EH. Hospices' enrollment policies may contribute to underuse of hospice care in the United States. Health Aff (Millwood) 2012 Dec;31(12):2690–2698. doi: 10.1377/hlthaff.2012.0286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Consensus Project. National Consensus Project for Quality Palliative Care: NQF Framework. 2011 http://www.nationalconsensusproject.org/NQF_Framework.asp. [Google Scholar]
- 19.National Hospice and Palliative Care Organization. NHPCO Facts and Figures: Hospice Care in America. [Accessed November 2015];2015 Available at: http://www.nhpco.org/sites/default/files/public/Statistics_Research/2015_Facts_Figures.pdf. [Google Scholar]
- 20.National Hospice and Palliative Care Organization. NHPCO Facts and Figures: Hospice Care in America. [Accessed November 2013];2012 Available at: http://www.nhpco.org/sites/default/files/public/Statistics_Research/2012_Facts_Figures.pdf. [Google Scholar]
- 21.MedPac. Report to the Congress: Medicare Payment Policy: Chapter 12: Hospice Services. 2015 [Google Scholar]
- 22.Ohta B, Kronenfeld JJ. Intensity of acute care services at the end of life: nonclinical determinants of treatment variation in an older adult population. J Palliat Med. 2011 Jun;14(6):722–728. doi: 10.1089/jpm.2010.0360. [DOI] [PubMed] [Google Scholar]
- 23.Barnato AE, Cohen ED, Mistovich KA, Chang CC. Hospital end-of-life treatment intensity among cancer and non-cancer cohorts. J Pain Symptom Manage. 2015 Mar;49(3):521–529. e521–e525. doi: 10.1016/j.jpainsymman.2014.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kelley AS. Treatment intensity at end of life--time to act on the evidence. Lancet. 2011 Oct 15;378(9800):1364–1365. doi: 10.1016/S0140-6736(11)61420-7. [DOI] [PubMed] [Google Scholar]
- 25.Teno JM, Gozalo PL, Bynum JP, et al. Change in end-of-life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013 Feb 6;309(5):470–477. doi: 10.1001/jama.2012.207624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wennberg JE, Fisher ES, Stukel TA, Skinner JS, Sharp SM, Bronner KK. Use of hospitals, physician visits, and hospice care during last six months of life among cohorts loyal to highly respected hospitals in the United States. Bmj. 2004 Mar 13;328(7440):607. doi: 10.1136/bmj.328.7440.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kelley AS, Deb P, Du Q, Aldridge Carlson MD, Morrison RS. Hospice enrollment saves money for Medicare and improves care quality across a number of different lengths-of-stay. Health Aff (Millwood) 2013 Mar;32(3):552–561. doi: 10.1377/hlthaff.2012.0851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Field MJ, Cassel CK, editors. Approaching Death: Improving Care at the End of Life. Washington, DC: National Academy Press; 1997. [PubMed] [Google Scholar]
- 29.Barnato AE, Herndon MB, Anthony DL, et al. Are regional variations in end-of-life care intensity explained by patient preferences?: A Study of the US Medicare Population. Med Care. 2007 May;45(5):386–393. doi: 10.1097/01.mlr.0000255248.79308.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gallup GH., Jr Spiritual beliefs and the dying process: a report on a national survey. Conducted for the Nathan Cummings Foundation and the Fetzer Institute. 1997 [Google Scholar]
- 31.Higginson IJ, Sen-Gupta GJ. Place of care in advanced cancer: a qualitative systematic literature review of patient preferences. J Palliat Med. 2000 Fall;3(3):287–300. doi: 10.1089/jpm.2000.3.287. [DOI] [PubMed] [Google Scholar]
- 32.Bruera E, Russell N, Sweeney C, Fisch M, Palmer JL. Place of death and its predictors for local patients registered at a comprehensive cancer center. J Clin Oncol. 2002 Apr 15;20(8):2127–2133. doi: 10.1200/JCO.2002.08.138. [DOI] [PubMed] [Google Scholar]
- 33.Wright AA, Keating NL, Balboni TA, Matulonis UA, Block SD, Prigerson HG. Place of death: correlations with quality of life of patients with cancer and predictors of bereaved caregivers' mental health. J Clin Oncol. 2010 Oct 10;28(29):4457–4464. doi: 10.1200/JCO.2009.26.3863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Teno JM, Clarridge BR, Casey V, et al. Family perspectives on end-of-life care at the last place of care. Jama. 2004 Jan 7;291(1):88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 35.Mitchell SL, Teno JM, Kiely DK, et al. The clinical course of advanced dementia. N Engl J Med. 2009 Oct 15;361(16):1529–1538. doi: 10.1056/NEJMoa0902234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gozalo P, Teno JM, Mitchell SL, et al. End-of-life transitions among nursing home residents with cognitive issues. N Engl J Med. 2011 Sep 29;365(13):1212–1221. doi: 10.1056/NEJMsa1100347. [DOI] [PMC free article] [PubMed] [Google Scholar]