Abstract
Background and Objectives:
Dehydration is a common complication after ileostomy creation and is the most frequent reason for postoperative readmission to the hospital. We sought to determine the clinical and economic impact of an outpatient intervention to decrease readmissions for dehydration after ileostomy creation.
Methods:
All new ileostomates from 09/2011 through 10/2012 at the University of Florida were enrolled to receive an ileostomy education and management protocol and a daily telephone call for 3 weeks after discharge. Counseling and medication adjustments were provided, with a satisfaction survey at the end. Outcomes of these patients were compared to those in a historical control cohort. A cost analysis was conducted to calculate the savings to the hospital.
Results:
Thirty-eight patients were enrolled. All patients required telephone counseling, and the mean satisfaction score rating was 4.69, on a scale of 1 to 5. The readmission rate for dehydration within 30 days of discharge decreased significantly from 65% before intervention to 16% (5/32 patients) after intervention (P = .002). The length of readmission hospital stay decreased from a mean of 4.2 days before the introduction of the intervention to 3 days after. Cost analysis revealed that the actual total hospital cost of dehydration-specific readmission decreased from $88,858 to $25,037, a saving of $63,821.
Conclusion:
A standardized ileostomy pathway with comprehensive patient education and outpatient telephone follow-up is cost effective, has a positive influence on patient satisfaction, and reduces dehydration-related readmission rates.
Keywords: Dehydration, Ileostomy, Readmission
INTRODUCTION
Ileostomy creation is a commonly performed operation in colorectal surgery. A frequently encountered complication is postoperative dehydration because of high ostomy output,1,2 which is the most common indication for postoperative readmission in this cohort. Historical readmission rates for patients after index ileostomies range from 10 to 30%,3 with dehydration being the predominant cause in as many as 44%.2,4 Nationally, fast-track protocols and cost reduction efforts have resulted in a decreasing hospital length of stay after colorectal procedures. However, concern remains regarding early discharge leading to an increased readmission rate and potentially greater morbidity in the readmitted patient. Hospital readmission within 30 days after surgery is receiving increased attention as a costly and possibly preventable postoperative complication and is closely scrutinized as an outcome measure and indicator for quality. The Affordable Care Act has led to intensification of financial pressures on health care systems with increased attention to avoiding such preventable complications due to their effects on reimbursement and hospital finances.
Literature addressing protocols to help decrease readmissions after ileostomies is sparse.2,5 The effectiveness of such protocols has been demonstrated in single-institution case series, but we sought to study the economic impact of such a protocol. We wanted to determine whether a simple patient-centered outpatient intervention at a tertiary care referral center would mitigate readmissions for dehydration and have a positive economic impact relative to the cost to the hospital of this complication. In addition, an anonymous patient satisfaction survey was completed to assess the response of patients to the intervention.
MATERIALS AND METHODS
After obtaining the approval of the University of Florida Institutional Review Board, all patients who had an index ileostomy created from September 2011 through October 2012 by 1 of the 3 surgeons from the Colorectal Surgery Service at University of Florida and who consented for participation were enrolled in this prospective study. Exclusion criteria included any unrelated condition that would interfere with oral intake (such as dysphagia or esophagitis) or inability to document intake and output or to participate responsibly in the study (dementia and nursing home residency). Primary outcome measures were dehydration-related readmission rates after the index procedure and total costs for the readmission; secondary outcome measures were patient satisfaction, the length of hospital stay on readmission, the severity of dehydration on readmission, and response to treatment.
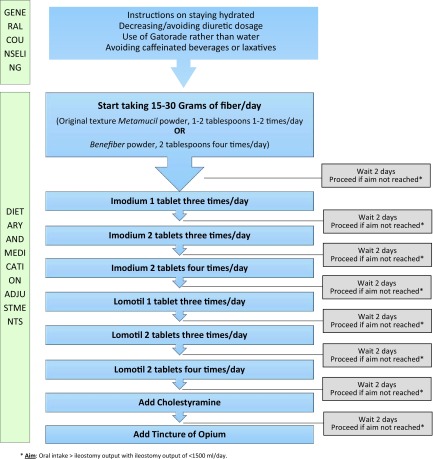
All patients received standard ileostomy education by ostomy-trained nurses while still admitted in the postoperative period and home health care after discharge. The quality of information provided was intentionally not changed during the course of the study. This included furnishing the patients with a ledger to record intake, output, and weight daily. Patients were also educated on the signs and symptoms of dehydration, including presence of dizziness, dry mouth, ostomy output consistency, and urine amount and color. In addition to these measurements, all patients were contacted with a daily telephone call from a healthcare provider (a physician, advanced registered nurse practitioner [ARNP], or registered nurse) for the first 21 days of the postoperative period. The questions asked mirrored those of the ostomy teaching (Table 1). The answers to these questions were recorded, and appropriate patient counseling was conducted regarding intake and output and avoiding dehydration. In addition, medication adjustments for patients with a volume deficit or high ostomy output (>1500 mL/day) were made in consultation with a physician or an ARNP daily. The protocol used for telephone counseling and dietary/medication adjustments is outlined in Figure 1. An anonymous satisfaction survey was also administered at the end to assess patient experience and perception of this intervention (scale 1–5; 5, excellent and 1, poor). The validated score of patient satisfaction (Table 2) was adapted from the dehydration portion of the European Organisation for Research and Treatment of Cancer In-Patient Satisfaction 32-item survey (EORTC IN-PATSAT32).6
Table 1.
Provider-Administered Questionnaire
|
Figure 1.
Outpatient phone call protocol to help reduce ileostomy output.
Table 2.
Patient Satisfaction Survey
During the study, how would you rate the healthcare provider who called you in terms of*:
|
Scale of 1–5, with 1 being poor and 5 being excellent.
The outcomes of the patients included in the study were compared with a historical control cohort of patients who had undergone ileostomy by the same physicians at University of Florida Health during the immediately preceding period. Patients in the 13-month period before (08/2010 through 09/2011) and after (09/2011 through 10/2012) the intervention were compared in their 30-day readmission specifically from dehydration secondary to high ileostomy output. Patients who fulfilled the exclusion criteria; those who were readmitted solely for other reasons, such as deep surgical site infection; and those who were readmitted after undergoing ileostomy creation by another service or hospital who were not a part of this protocol were not included. These criteria were set in an attempt to get a true sense of the efficacy of the outpatient protocol in reducing readmissions specifically from ostomy-related dehydration and to exclude confounding factors. The 2 groups were compared in their baseline characteristics and outcome variables to determine the degree of dehydration at readmission, subsequent length of hospital stay, and hospital costs.
Costs were defined as the U.S. dollar amount of resources used to provide all aspects of patient care. The cost of readmission, provided by institutional data, was determined by calculating the total actual hospital costs including both direct and indirect costs. Direct and indirect costs were not separated for this analysis because of limitations of our database. Direct costs were calculated from effort studies by job class, supply studies and invoices, and contract reviews, which were adjusted to reflect the actual incurred expense. Indirect costs were allocated based on multiple-allocation methods, such as human resource costs allocated based on full-time equivalents, utilities, and environmental services allocated based on weighted square footage and accounting allocated by relative total of charges and expenses. A stepdown method was used to allocate indirect costs to direct cost centers (for example, the finance department utility costs were allocated to the finance department before its total costs were allocated to the hospitalization and other direct cost centers). A cost analysis was performed to estimate the cost of applying this intervention, which was deducted from the savings from decreased dehydration-related complications during the study period and compared to the cost of similar complications in the preceding period, to determine the true implications of this intervention. Cost savings specifically as a result of the intervention were calculated for the University of Florida during the study period, along with future implications.
Student's t test, χ2, and Fisher's exact test were used for statistical analyses (SPSS Statistics for Windows, ver. 21.0, 2012; IBM Corp., Armonk, New York, USA).
RESULTS
From September 2011 through October 2012, 38 patients (17 men and 21 women) with new ileostomies were enrolled in the study. Thirty-two completed the study, and 6 withdrew or could not be contacted consistently, despite multiple attempts over the week after discharge and were dropped from the study. Of those patients, 15 received an ileostomy for ulcerative colitis: 11 for neoplasm requiring resection, and 6 for other reasons.
All patients (100%) who completed the study required telephone counseling with regard to their intake and output and techniques of avoiding dehydration, whereas a majority (29 patients, 91%) required medication adjustments to help achieve a positive fluid balance. Twenty-five (78% of the total) completed the modified EORTC IN-PATSAT32 patient satisfaction survey at the end of the study. The average score was 4.69 (95% CI: 4.51–4.66), on a scale of 1–5, indicating excellent patient satisfaction regarding the education and outpatient support provided in the postoperative period (Table 3). Of note, all patients gave the information provided to them over the phone regarding their treatment a grade of 5.
Table 3.
Patient Satisfaction Survey Results
| Item | Score* |
|---|---|
| Their knowledge of your illness and expertise in that area | 4.7 |
| The treatment and medical follow-up they provided | 5.0 |
| The attention they paid to your physical problems | 4.8 |
| Their willingness to listen to all of your concerns | 4.8 |
| The interest they showed in you personally | 4.6 |
| The comfort and support they gave you | 4.5 |
| The information they gave you about your illness | 4.3 |
| The information they gave you about your laboratory results | 4.2 |
| The information they gave you about your treatment | 5.0 |
| The frequency and duration of the phone calls | 4.9 |
| The time they devoted to you during the phone calls | 4.8 |
Scale of 1–5, with 1 being poor and 5 being excellent.
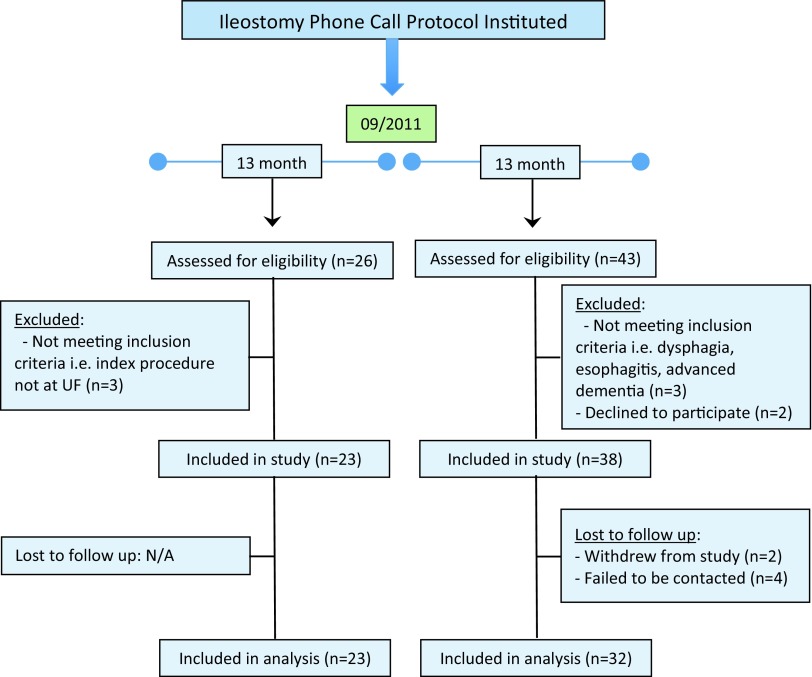
A comparison of patients with 30-day dehydration-specific readmissions after undergoing an ileostomy at University of Florida Health in the 13-month period before (08/2010–09/2011) and after (09/2011–10/2012) the intervention was made (Figure 2). Comparison of their baseline characteristics including the underlying diagnosis for which an ileostomy was created, and comorbidities did not show a significant difference in the 2 groups (Table 4).
Figure 2.
CONSORT diagram detailing inclusion/exclusion of patients in pre- and postintervention groups.
Table 4.
Comparison of Baseline Characteristics of Pre- and Postintervention Groups
| Preintervention | Postintervention | P | |
|---|---|---|---|
| Mean age (years) | 55 | 55 | .70 |
| Sex (M/F) | 6/9 | 1/4 | .28 |
| Body mass index (mean) | 24 | 26 | .23 |
| ASA class (mean) | 3 | 3 | .08 |
| Postoperative admission day* (mean) | 18.3 | 18.4 | .54 |
Postoperative day that the patient was readmitted for dehydration relative to the day of the ileostomy creation.
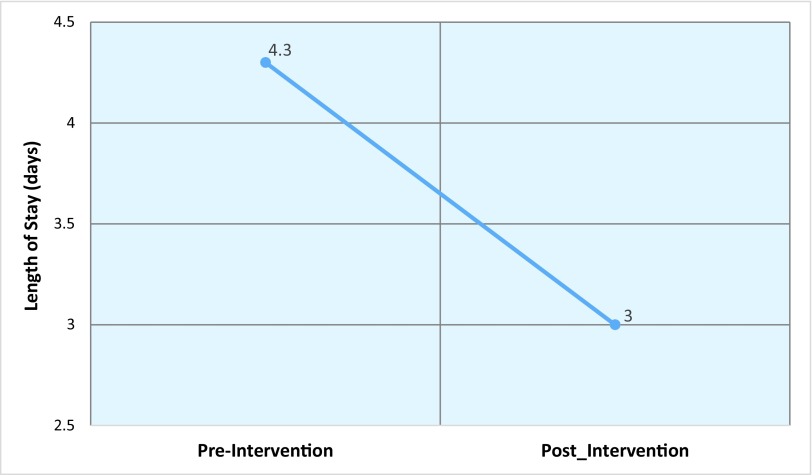
The readmission rate for dehydration within 30 days of discharge from the index procedure decreased significantly, from 65% (15/23 patients) before the intervention to 16% (5/32 patients) after the intervention (P = .002). None of the 6 patients who were dropped from the study arm was readmitted as far as we could ascertain. However, there was no significant difference in the severity of dehydration at readmission in the 2 groups, as determined by the serum blood urea nitrogen (BUN) and creatinine on readmission. Even though, after intervention, readmitted patients received significantly less intravenous fluids during the first 24 hours of their hospital stay, the difference in their urine output during the same period was not significant, although there was a trend toward higher output (1390 vs 970 mL) with less resuscitation (2000 vs 2270 mL) in the postintervention group. The length of hospital stay for the readmitted patients decreased from a mean of 4.2 days before the introduction of the study protocol to a mean of 3 days after its introduction (Figure 3). A detailed comparison of these outcomes in the 2 groups is shown in Table 5. No grade II–V complications on the Clavien-Dindo scale were noted in either group. Only 1 patient in the preintervention group had self-limited bleeding from the ostomy that did not require intervention or lead to a readmission.
Figure 3.
Comparison of length of stay in the pre- and postintervention groups.
Table 5.
Quality Metric Outcome Comparison of Pre- and Postintervention Groups
| Item | Preintervention | Postintervention | P |
|---|---|---|---|
| (n = 23) | (n = 32) | ||
| All ileostomy patients | |||
| Thirty-day readmission rate (%) | 65% | 16 | .004 |
| Total cost for readmission | $88,858 | $25,037 | .0001 |
| Readmission population | |||
| Serum BUN on readmission | 20 | 34 | .24 |
| Serum creatinine on readmission | 1.1 | 1.9 | .36 |
| Amount of IV fluids administered during day 1 of readmission (mL) | 2270 | 2000 | .007 |
| Urine output during day 1 of readmission | 970 | 1390 | .38 |
| Length of hospital stay (mean days) | 4.2 | 3 | .23 |
Data in bold indicate significant differences (P < .05.).
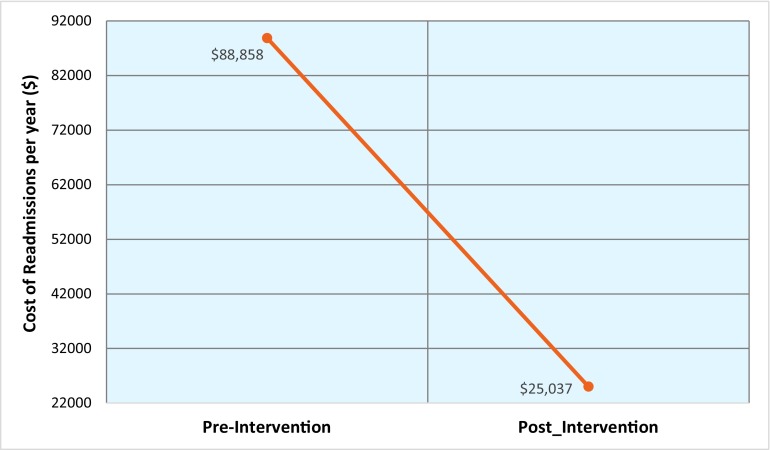
To obtain a complete picture for cost analysis, the cost of this intervention was calculated (Table 6). We had no costs for administering the telephone questionnaire during this study, but cost estimation was conducted for potential widespread clinical use. The required level of knowledge to administer the questionnaire may be equated to that of a nurse practitioner with an experienced clinician available for consultation. The average wage of a nurse practitioner in Florida according to the 2011 National Nurse Practitioner Compensation Survey is $87,653 per annum with 2000 working hours per year. The time needed to administer the questionnaire, given current clinical volume, is ∼15 minutes per day. With an hourly wage of $44 per hour, this brings the approximate cost of the intervention to $2030 per annum (excluding assumptions for overtime and benefits). The implementation of the intervention was associated with a decrease of 49% in the dehydration-specific readmission rate, which in turn led to a significant decrease in total actual cost for readmission from $73,858 to $25,037 (P < .0001; Figure 4). Further, when patients were readmitted, the length of stay was a mean of 3 days versus 4.2 days before the protocol, resulting in an additional cost savings of $15,000/annum (assuming hospital costs of $2,500/day). During the study period, this calculation resulted in a total saving of $63,821 to the University of Florida after the intervention. When the cost for implementing this intervention in the future ($2,030/annum) is deducted from the average expected cost reduction ($63,821/annum), the overall future savings for the University of Florida amounts to $61,791 per annum, if resources are used to administer the intervention. However, the above calculation does not account for the ripple effect of an “opportunity cost”—that is, the potential gain by the upstream choice of an alternative patient admitted in the freed hospital beds. Assuming that the bed is occupied by a similar patient, it would result in $6,000–$10,900 opportunity cost per bed freed, increasing the overall cost saving to the University to between $123,505 and $173,905 per annum.
Table 6.
Cost Analysis for the Intervention
| Cost Analysis | Cost/Annum | Overall Cost Savings |
|---|---|---|
| Cost reduction | $63,821 | |
| Decrease in readmissions by 49% | $48,821 |  |
| One-day decrease in hospital stay for readmissions | $15,000 | |
| Cost of administering future questionnaire through nurse practitioners | $2,030* | $61,791 |
| Opportunity cost gain (potential gain by the upstream choice of an alternative in the freed hospital beds) | $112,114 |  |
| Total cost savings | $173,905** |
Assumes an average wage of a nurse practitioner in Florida of $87,653 per annum with 2000 working hours/year and ∼15 minutes/day necessary to complete the questionnaire.
Obtained by adding the overall actual cost savings from the protocol to the opportunity cost gain.
Figure 4.
Comparison of total actual costs in the pre- and postintervention groups.
DISCUSSION
In this study, an ileostomy pathway with comprehensive postoperative patient education with aggressive outpatient telephone follow-up has been shown to be effective, as an easily administered, cost-effective intervention with high patient satisfaction scores that resulted in a significant reduction in dehydration-related readmission rates, a decrease in mean length of stay for readmissions, and a significant cost reduction. Very few studies have shown the utility of protocols to help decrease readmissions after ileostomies2,5; our study demonstrates the positive economic impact of such a protocol.
The colon and rectal surgery service at University of Florida was initiated in July 2008. Analysis of outcomes from January 2008 to June 2011 demonstrated that our service was a potential outlier in the area of readmission for dehydration compared to other services. This prompted us to look into ways to reduce dehydration-related readmissions. We instituted an institutional review board–approved study to evaluate the efficacy and cost effectiveness of a more intensive outpatient telephone follow-up in an attempt to achieve that goal. Subsequently, all patients who completed the study required counseling that included behavioral modification with regard to their intake and output during the telephone follow-ups; 90% of the patients received medication adjustments. This prospective educational and support program was scored very positively (4.6/5) by patients on a validated satisfaction survey. Comparison of outcomes for the 13-month period before and after initiation of the study showed a significant reduction in dehydration-related readmission rates (49% reduction), which was associated with an actual cost saving of $48,821 over the study period. When coupled with a decrease in mean length of stay for readmissions from 4.2 days before the intervention to 3 days after its institution, the total cost saving was estimated at $63,821. These cost savings were compounded ($123,505–$173,905 per annum), when the implications of downstream opportunity cost per vacated bed were added to the equation.
Although most of the cost savings were caused by a decrease in unplanned readmissions within 30 days of discharge after surgery ($48,821), substantial savings were also attributed to a decrease in the length of hospital stay upon readmission ($15,000). This decrease in length of stay was potentially a result of better education of patients after the index procedure and being readmitted with less severe dehydration after the intervention. The difference in the degree of dehydration on readmission, as calculated by the patient's BUN and creatinine, was, although not significant statistically but may be clinically and financially significant, as indicated by the better response in urine output with a significantly lesser volume of resuscitation, leading to earlier discharge. Similarly, a trend toward lower ostomy output upon readmission was seen after the intervention, which resulted in a lower mean cost for readmission per patient, with the cost decreasing from $5500 per readmission before the intervention to $5000 after the intervention.
Potential drawbacks to our study include the low number of patients enrolled because it was a single-center trial. More patients could have been included in the study by extending the period beyond October 2012, but it was intentionally ended in October 2012, to obtain an analogous cohort for historical comparison. Moreover, we had instituted several measures after October 2012, such as a change in the service structure and implementation of enhanced recovery after surgery, which would confound the results. The positive results may have been more pronounced and significant in a high-volume center. Furthermore, because this was not a randomized controlled trial, there was the potential for inherent bias. Randomization would further decrease the number of patients in our study arm and is being pursued in a multicenter study. In addition, we were unable to stratify our cost analysis into direct and indirect costs or fixed and variable costs. For example, we did not measure societal costs, because of loss of productivity as a result of ongoing health problems or readmission. Incorporation of these indirect costs, which are difficult to quantify, would further increase the cost savings noted in our study. The cost analysis included some calculated assumptions, but in a diverse health care system, relying on actual costs does not provide a complete picture. However, even if the assumptions of opportunity cost were discounted, the protocol still led to significant cost savings. Also, we chose to look at 30 days of readmissions, but when the period was extended to 90 days, the results did not change significantly. Only 1 patient was readmitted again before the 90-day period ended, and that patient was already considered a readmission within 30 days. In addition, our readmission rate cause by postileostomy dehydration of 65% before the intervention was higher than the reported national average from that time period (44%).2,4 Possible causes for those rates include a relatively new division of colorectal surgery with less than ideal emphasis on patient education and relatively delayed follow-up after discharge. These were addressed before the initiation of the study, but continued and delayed benefits may have confounded the results, as is the case with any real-time ongoing quality improvement project. However, our readmission rate of 16% after initiation of the study is better or on par with other high-volume centers.2,7,8 In addition, the design of the study made it possible to rule out participating patients who presented for postsurgical readmission to hospitals outside of our tertiary care system.
Ileostomy pathways including restriction of oral hypotonic fluids, use of isotonic solutions, antidiarrheal/antisecretory medications, and adequate caloric nutritional support have been proposed to help prevent dehydration after ileostomy and reduce unplanned readmissions.9–11 Such pathways are currently in use by select institutions. Nagle et al5 from Beth Israel Deaconess Medical Center (Boston, Massachusetts, USA) used a comprehensive ileostomy pathway to decrease their overall readmission rates, and other centers, such as the University of Cincinnati, have adopted the same pathway.2 This pathway includes educating the patient about signs of dehydration, telephone calls by nurses, supplies given to the patient, and avoidance of certain medications (eg, diuretics), to prevent dehydration, with a focus toward enabling patients to take ownership of the ostomy. The protocols practiced included patient visits to nurse practitioners between postoperative days 7 and 10 to review intake/output, diet, medications, and hydration status. Outcome data after the use of these ileostomy pathways are very limited because of recent implementation, with only Beth Israel Deaconess Medical Center showing an actual reduction in readmissions from 35.4 to 21.4%, after the use of the protocol, of which dehydration-related readmissions were reduced from 15.5 to 0%5; however, no cost effectiveness data were provided. Moreover, a goal of no dehydration-related readmissions after ileostomy creation would be too expensive and difficult to achieve in the long term. Our protocol was different in the sense that it was telephone based without the need for additional clinic visits with providers, it elicited higher patient satisfaction, and it was less time consuming, which would equate to cost savings at the expense of a slightly higher readmission rate.
The ideal interval and duration of contacting patients after surgery is difficult to ascertain. Most of the patients (60%) required daily counseling and adjustments of medications, and the rest (40%) needed a medication adjustment every 2–3 days. The adjustments were more intensive in the period immediately after discharge and the majority of the patients (80%) were able to achieve a positive net fluid balance within 6 days of discharge. Based on this statistic, we suggest early identification of high-risk patients who should be contacted every day, whereas the rest could be contacted every other day, with an option to have them call if any problems arise. In an ideal setting, the ability to get patients into an outpatient infusion center for placement of a peripherally inserted central line, with intravenous fluid replacement after early identification during the phone encounters would further decrease the readmission rate. Access to such an outpatient unit was attempted but was not feasible during this study. In an ideal world, the inpatient cost savings would translate into an investment in the outpatient setting, to help better transitional care of the patients in the postoperative period; however, the independence of our inpatient and outpatient financial structures made this a nonviable option. In this age of outcome reporting, addressing this need is paramount, but ideally an approach should be developed that does not compromise patient satisfaction and health care costs.
We have shown efficacy of implementation of an easily administered, cost-effective intervention with high patient satisfaction scores that resulted in a significant (49%) reduction in dehydration-related readmission rates, a decrease from 4.2 to 3 days in mean length of stay for readmissions and a total cost saving estimated between $123,505 and $173,905 per annum. These results are a direct consequence of decreasing unplanned readmissions secondary to dehydration after ileostomy formation by implementing aggressive outpatient follow-up and management. Adoption of such a pathway is crucial in this era of emphasis on cost savings, with contiguous assessment of quality and outcome measures.
The cost savings calculated in this study are likely to be magnified in a larger center with higher clinical volumes in a metropolitan location, because the hospital cost savings of $2500 per day assumed in this study for our tertiary care teaching hospital in a rural setting would probably be amplified in that scenario. Prospective evaluation is needed in a larger patient population.
CONCLUSION
We have shown the efficacy of implementation of an easily administered, cost-effective intervention with high patient satisfaction scores that resulted in a significant (49%) reduction in dehydration-related readmission rates, a decrease in mean length of stay for readmission from 4.2 to 3 days, and a total cost saving estimated between $123,505 and $173,905 per annum. These results are a direct consequence of decreasing unplanned readmissions secondary to dehydration after ileostomy formation by emphasizing aggressive outpatient follow-up and management. Adoption of such a pathway is crucial in this era of cost savings with contiguous assessment of quality and outcome measures. The cost savings calculated in this study are likely to be magnified in larger more urban settings. This possibility should be further evaluated prospectively in a larger patient population.
Contributor Information
Ahsan Raza, Ahsan Raza, MD, Department of Surgery, University of Florida, P. O. Box 100109, Gainesville, Florida, USA..
Emina Huang, Department of Surgery, Cleveland Clinic, Cleveland, Ohio, USA..
Lindsey Goldstein, Ahsan Raza, MD, Department of Surgery, University of Florida, P. O. Box 100109, Gainesville, Florida, USA..
Steven J. Hughes, Ahsan Raza, MD, Department of Surgery, University of Florida, P. O. Box 100109, Gainesville, Florida, USA..
Sanda A. Tan, Ahsan Raza, MD, Department of Surgery, University of Florida, P. O. Box 100109, Gainesville, Florida, USA..
References:
- 1. Roland M, Campbell S. Successes and failures of pay for performance in the United Kingdom. N Engl J Med. 2014;370:1944–1949. [DOI] [PubMed] [Google Scholar]
- 2. Paquette IM, Solan P, Rafferty JF, Ferguson MA, Davis BR. Readmission for dehydration or renal failure after ileostomy creation. Dis Colon Rectum. 2013;56:974–979. [DOI] [PubMed] [Google Scholar]
- 3. Tyler JA, Fox JP, Dharmarajan S, et al. Acute health care resource utilization for ileostomy patients is higher than expected. Dis Colon Rectum. 2014;57:1412–1420. [DOI] [PubMed] [Google Scholar]
- 4. Messaris E, Sehgal R, Deiling S, et al. Dehydration is the most common indication for readmission after diverting ileostomy creation. Dis Colon Rectum. 2012;55:175–180. [DOI] [PubMed] [Google Scholar]
- 5. Nagle D, Pare T, Keenan E, Marcet K, Tizio S, Poylin V. Ileostomy pathway virtually eliminates readmissions for dehydration in new ostomates. Dis Colon Rectum. 2012;55:1266–1272. [DOI] [PubMed] [Google Scholar]
- 6. Brédart A, Bottomley A, Blazeby JM, et al. European Organisation for Research and Treatment of Cancer Quality of Life Group and Quality of Life Unit: an international prospective study of the EORTC cancer in-patient satisfaction with care measure (EORTC IN-PATSAT32). Eur J Cancer. 2005;41:2120–2131. [DOI] [PubMed] [Google Scholar]
- 7. Datta I, Buie WD, Maclean AR, Heine JA. Hospital readmission rates after ileal pouch-anal anastomosis. Dis Colon Rectum. 2009;52:55–58. [DOI] [PubMed] [Google Scholar]
- 8. Chun LJ, Haigh PI, Tam MS, Abbas MA. Defunctioning loop ileostomy for pelvic anastomoses: predictors of morbidity and nonclosure. Dis Colon Rectum. 2012;55:167–174. [DOI] [PubMed] [Google Scholar]
- 9. Garcia-Botello SA, Garcia-Armengol J, Garcia-Granero E, et al. A prospective audit of the complications of loop ileostomy construction and takedown. Dig Surg. 2004;21:440–446. [DOI] [PubMed] [Google Scholar]
- 10. Okamoto T, Kusunoki M, Kusuhara K, Yamamura T, Utsunomiya J. Water and electrolyte balance after ileal J pouch anal anastomosis in ulcerative colitis and familial adenomatous polyposis. Int J Colorectal Dis. 1995;10:33–38. [DOI] [PubMed] [Google Scholar]
- 11. Tsao SK, Baker M, Nightingale JM. High-output stoma after small-bowel resections for Crohn's disease. Nat Clin Pract Gastroenterol Hepatol. 2005;2:604–608. [DOI] [PubMed] [Google Scholar]