Abstract
Background
Childhood maltreatment is an important risk factor for problems with alcohol and other drugs such as cannabis. Although this link has been well established, the mechanisms in this association require further study. High levels of impulsivity and difficulties with emotion regulation are often associated with childhood maltreatment. Negative urgency – an emotion-based facet of impulsivity – is a strong predictor of substance use problems and may be a particularly relevant facet of impulsivity in the link between childhood maltreatment and alcohol and cannabis outcomes. However, few studies have examined the specific mediational pathway from childhood maltreatment to alcohol and cannabis problems through negative urgency.
Objectives
We tested the hypothesis that the associations between history of childhood maltreatment and current alcohol and cannabis problems would be mediated by negative urgency, but not other facets of impulsivity.
Methods
Participants (N=232), who were in late adolescence (mean age=19.75), completed self-report measures of different facets of impulsivity, past childhood maltreatment, and current alcohol and cannabis use and problems.
Results
In analyses including several facets of impulsivity as simultaneous mediators, negative urgency was the only facet to mediate the associations of childhood maltreatment severity with alcohol and cannabis problems.
Conclusions
These findings provide support for negative urgency as a unique mediator of the association between childhood maltreatment and both alcohol and cannabis problems, suggesting that future work on mechanisms in this association should focus on mood-based impulsivity.
1. Introduction
Substance-related problems pose a significant burden to society. Alcohol and cannabis are two of the most widely used substances, making them an important focus of research on substance-related problems. The developmental period spanning late adolescence and young adulthood coincides with the highest observed rates of alcohol and drug use (Substance Use and Mental Health Services Administration, 2013), and problematic substance use (i.e., heavy use that is associated with negative consequences) during this developmental period has been widely documented (Hingson, Heeren, Winter, & Wechsler, 2005). Increasingly, problems with alcohol and other drugs have been conceptualized as developmental phenomena (Brown et al., 2008; Masten, Faden, Zucker, & Spear, 2008). According to this framework, distal factors such as childhood family environment play a crucial role in the later development of substance problems (Faulkner, Goldstein, & Wekerle, 2014; Zucker, Donovan, Masten, Mattson, & Moss, 2008).
Childhood maltreatment, which encompasses abuse (emotional, physical, and sexual) and neglect (emotional and physical), is a potent risk factor for the development of problems with alcohol and drugs (Annerbäck, Sahlqvist, Svedin, Wingren, & Gustafsson, 2012; Goldstein et al., 2013; Rogosch, Oshri, & Cicchetti, 2010; Schwandt, Heilig, Hommer, George, & Ramchandani, 2013). Retrospective reports from adults with substance use problems suggest that they are more likely than the general population to have experienced childhood maltreatment (Dube et al., 2003; Fetzner, McMillan, Sareen, & Asmundson, 2011; Schwandt et al., 2013). Among adolescents and young adults, a history of childhood maltreatment has been linked to heavy episodic drinking and alcohol use disorders in large, nationally representative studies (Goldstein et al., 2013; Shin, Edwards, & Heeren, 2009). Further, self-reports of traumatic experiences and sexual victimization prior to college entry have been prospectively linked with increased risk for alcohol and other substance-related problems during the first year of college (Griffin, Wardell, & Read, 2013; Read et al., 2012). Although less research has focused specifically on cannabis, there is also evidence that childhood maltreatment is associated with cannabis problems throughout adolescence (Rogosch et al., 2010).
While there is a great deal of evidence that childhood maltreatment is an important risk factor for problems with alcohol and other drugs such as cannabis, the mechanisms that may account for these associations are in need of further investigation (see Pollak, 2005). Some research suggests that impulsivity may be relevant in the link between childhood maltreatment and substance outcomes, given that impulsivity is associated with both a history of childhood maltreatment (Gagnon, Daelman, McDuff, & Kocka, 2013; Sujan, Humphreys, Ray, & Lee, 2014) and risk for problems with alcohol and drugs (de Wit, 2009; Verdejo-García, Lawrence, & Clark, 2008). Research suggests that impulsivity is a multifaceted construct, and distinguishing among facets of impulsivity has been shown to have utility in clarifying the role of impulsivity in risky behavior (Smith et al., 2007). Whiteside and Lynam (2001) conducted a factor analysis on commonly used measures of impulsivity and identified four separable facets: (i) lack of perseverance (difficulty staying focused), (ii) lack of premeditation (acting without forethought), (iii) sensation seeking (seeking new and exciting experiences) and (iv) negative urgency (acting rashly in response to negative emotions). More recently, a positive emotion variant of urgency, known as positive urgency, has also been identified (Cyders et al., 2007). Numerous studies support the discriminant validity of these impulsivity facets (Cyders & Smith, 2007; Smith et al., 2007; Whiteside, Lynam, Miller, & Reynolds, 2005). In particular, these five facets of impulsivity have been found to relate differentially to alcohol use and alcohol problems outcomes (for review, see Coskunpinar, Dir, & Cyders, 2013). Thus, investigation of the unique, specific contribution of each of these facets to substance use and other risky behavior is generally recommended (Smith et al., 2007; Whiteside et al., 2005).
Importantly, among these five facets of impulsivity, negative urgency is the most consistent predictor of alcohol problems (Coskunpinar et al., 2013). Consistent with the finding that negative urgency is uniquely associated with coping motives for drinking (Adams, Kaiser, Lynam, Charnigo, & Milich, 2012; Settles, Cyders, & Smith, 2010), the robust association between negative urgency and alcohol problems may reflect a tendency for individuals who drink in response to negative mood to drink in riskier ways and to lack other forms of adaptive coping strategies (e.g., Merrill & Read, 2010; Smith et al., 2007). As a result, even when level of alcohol consumption is held constant across individuals, those who drink in response to negative mood are likely to experience more negative consequences and alcohol problems. Indeed, several studies have found that negative urgency predicts unique variance in alcohol-related problems after controlling for levels of alcohol use (Curcio & George, 2011; Magid & Colder, 2007; Martens, Pedersen, Smith, Stewart, & O’Brien, 2011). In addition, negative urgency has also been shown to be predictive of cannabis use (Kaiser, Milich, Lynam, & Charnigo, 2012; Robinson, Ladd, & Anderson, 2014), although the relationship between negative urgency and cannabis problems has received less attention.
Further, negative urgency is a potentially relevant construct for understanding the association between childhood maltreatment and impulsivity. For example, maltreated children and adolescents show heightened arousal to negative emotions (Cicchetti & Curtis, 2005) (Cicchetti & Curtis, 2005), as well as impulsive behavior in emotional contexts (Maughan & Cicchetti, 2002). Perhaps the emotional dysregulation and impulsive behavior patterns that are characteristic of individuals with a history of childhood maltreatment make them more likely to act rashly in response to negative emotions, which is the hallmark of negative urgency. Some support for this notion comes from a recent study which found that childhood maltreatment was correlated with higher scores on negative urgency (Gagnon et al., 2013), although a separate study did not find support for this association (Sujan et al., 2014). Thus, more research on the association between childhood maltreatment and negative urgency is needed.
Given that childhood maltreatment appears to be related to higher levels of negative urgency, and negative urgency is a risk factor for problematic substance use, it follows that negative urgency could be an important mediator in the link between childhood maltreatment and substance problems in late adolescence. Conceptually, negative urgency is particularly relevant among different facets of impulsivity, given that impulsive, dysregulated behavior in response to negative emotions may occur with greater likelihood among individuals with a history of childhood maltreatment. This study aimed to examine negative urgency as a unique mediator of the association between childhood maltreatment and substance use problems while accounting for the concurrent mediational role of other impulsivity facets. We hypothesized that negative urgency (but not other facets of impulsivity) would mediate the link between childhood maltreatment and alcohol and cannabis problems. We also expected this indirect association to be significant even after controlling for heavy drinking frequency when analyzing alcohol problems and frequency of cannabis use when analyzing cannabis problems.
2. Method
2.1 Participants
Participants recruited in late adolescence (N=232; n=122 women) completed a baseline assessment as part of a screening procedure for an experimental study. Mean age was 19.75 years (SD=1.06; Range=18–25), 97% (n = 226) were age 21 or younger, and 91% (n=212) were legal drinking age (i.e., age 19 in Ontario, Canada). Seventy-four percent (n=171) were full-time students. Participants selected one or more of the following categories to describe their ethnic/racial background: Caucasian (n=138; 59%), Asian (n=29; 13%), East Indian (n=16, 7%), Hispanic/Latino (n=20; 9%), Black/African American (n=30; 13%), Native North American (n=8; 3%), Pacific Islander (n=2; 1%), and other (n=30; 13%). Participants reported a mean of 19.12 (SD=12.86) drinking days in the past 90 days, with an average of 5.12 (SD=2.32) drinks per drinking day and 11.71 (SD=11.58) heavy drinking episodes (defined as 4+ drinks for women/5+ drinks for men). Seventy-two percent of the participants reported using cannabis during the past 90 days (n=167). Those participants who had used cannabis within the past 90 days reported a mean 25.29 (SD=34.14) days of use.
2.2 Recruitment and Procedure
Recruitment consisted primarily of Internet advertisements on public and University websites targeting social drinkers in the Greater Toronto Area. Due to the aims of the larger study, the primary eligibility criteria included at least one heavy drinking episode in the past 30 days, no past alcohol treatment or current desire/attempts to reduce drinking, and no contraindications for alcohol use. Cannabis users were not specifically targeted. These criteria were evaluated in a telephone screen; eligible participants completed an in-person assessment, from which the current data are derived. The assessment involved both self-report measures administered via computer, and a Timeline Follow Back assessment of alcohol and cannabis use conducted by a trained interviewer. Participants were paid $40 for completing the assessment.
2.3 Measures
Childhood Trauma Questionnaire (CTQ; Bernstein & Fink, 1998; Bernstein et al., 2003)
The CTQ is a self-report questionnaire that measures 5 categories of childhood maltreatment: Emotional abuse (e.g., “Family said hurtful things”), physical abuse (e.g., “Hit hard enough to leave bruises”), sexual abuse (e.g., “Was touched sexually”), emotional neglect (e.g., “Felt loved”; reversed scored), and physical neglect (e.g., “Didn’t get enough to eat”). Each category contains 5 items, and participants indicate the frequency with which they experienced each item on a 5 point scale. Cutoff scores are provided to indicate the presence or absence of each type of maltreatment, and the magnitude of the score reflects severity of the exposure. Summing across all of the items provides an index of overall maltreatment severity (Bernstein & Fink, 1998). Research supports the reliability and validity of the CTQ, with studies showing that retrospective self-reports of childhood maltreatment assessed with the CTQ correlate highly with corroborating information from therapists and other documented reports (Bernstein et al., 2003; Everson et al., 2008). Cronbach’s α in this sample was .90.
UPPS-P Impulsivity Scales (Lynam, Smith, Cyders, Fischer, & Whiteside, 2007)
The UPPS-P measures five facets of impulsivity. This questionnaire contains the four impulsivity facets originally described in Whiteside and Lynam (2001) – negative urgency (12 items; α=.87; e.g., “When I feel bad, I will often do things I later regret in order to make myself feel better now”), sensation seeking (12 items; α=.84; e.g., “I generally seek new and exciting experiences and sensations”), lack of perseverance (10 items; α=.81; e.g., “I generally like to see things through to the end” [reverse scored]), and lack of premeditation (11 items; α=.86; e.g., “I don’t like to start a project until I know exactly how to proceed” [reverse scored]) – along with the more recent addition of the positive urgency scale (14 items; α=.92; e.g., “When I am in a great mood, I tend to get into situations that could cause me problems; Cyders et al., 2007). Participants rated the degree to which each item was descriptive of them on a 4 point scale. Because the scales do not contain the same number of items, we scored each scale by taking the average of the items so that mean scores would be directly comparable across scales. The reliability and validity of the UPPS-P has been demonstrated (Cyders et al., 2007; Smith et al., 2007).
Timeline Follow Back (Sobell & Sobell, 1992)
We derived estimates of alcohol and cannabis use with the Timeline Follow Back, a structured calendar assessment of recent substance use. The number of heavy drinking episodes was calculated as the number of days within the last 90 days on which the participant consumed 4+ drinks for women or 5+ drinks for men. Cannabis use frequency was calculated as the total number of days on which the participant reported any cannabis use.
Rutgers Alcohol Problems Index (RAPI; White & Labouvie, 1989)
Alcohol-related problems were assessed with the RAPI, a widely used measures of drinking problems for adolescents and young adults. Participants rated the frequency with which they experienced 23 indicators of alcohol-related problems (e.g., tolerance/withdrawal symptoms, academic problems, social/interpersonal consequences) on a scale from 0=Never to 4=More than 10 times. Cronbach’s α in this sample was .90.
Marijuana Problem Scale (MPS; Stephens, Roffman, & Curtin, 2000)
The MPS was used to measure the frequency of negative marijuana/cannabis consequences. Participants rated the severity with which they experienced 19 indicators of cannabis problems (e.g., financial problems, work/academic problems, social/interpersonal consequences) on a scale from 0=No Problem to 2=Serious Problems. Cronbach’s α in this sample was .89.
2.4 Data Analysis Plan
We first examined the distributional properties of the variables. Extreme univariate outliers – defined as values greater than 3.29 SD above the mean and clearly disconnected from the distribution (Tabachnick & Fidell, 2007) – were observed on the childhood maltreatment (4 outliers), alcohol problems (2 outliers), heavy drinking frequency (1 outlier), and cannabis problems (1 outlier) variables. These observations were recoded to one unit greater than the next most extreme value to reduce their influence (Tabachnick & Fidell, 2007). Descriptive analyses were performed to examine the characteristics of the sample.
To examine the hypothesized unique indirect associations from childhood maltreatment to alcohol and cannabis problems via negative urgency, we conducted mediation analyses using the SPSS PROCESS macro (Hayes, 2013). Separate models were specified for the outcomes of alcohol problems and cannabis problems. All participants were included in both models regardless of cannabis use status in order to facilitate comparisons across models. In both models, severity of childhood maltreatment was specified as the independent variable, and the five impulsivity facets were specified as simultaneous mediators in order to isolate the unique mediated pathway through negative urgency. Also, given that negative urgency has been shown to predict alcohol problems over and above levels of alcohol use, we conducted our analyses both with and without substance use (number of heavy drinking days and number of cannabis use days, respectively) included as a covariate. All variables were transformed into z-scores to obtain standardized estimates for coefficients.
Bootstrapping was used to derive 95% confidence intervals for the indirect associations between childhood maltreatment and the outcome variable (alcohol or cannabis problems) via the impulsivity facets. Because the five impulsivity scales were all included within the same model, the estimates of the indirect associations via negative urgency represented specific, unique indirect associations, accounting for the shared variance between negative urgency and the other facets of impulsivity.
3. Results
3.1 Descriptive Analyses
Endorsement of childhood maltreatment was relatively common in the current sample. More than half (n=134; 58%) of participants met the cutoff for at least one form of childhood maltreatment. Table 1 presents the means, standard deviations, and simple bivariate associations among the study variables. CTQ total score showed positive correlations with alcohol problems, cannabis problems, and the impulsivity domains of positive urgency, negative urgency, and lack of perseverance. Most of the impulsivity facets were significantly correlated with alcohol and cannabis problems. Importantly, several of the impulsivity scales were moderately intercorrelated, highlighting the importance of accounting for this shared variance when testing our mediation hypotheses.
Table 1.
Means, standard deviations, and correlations among variables in the model.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | M | SD | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Sex (1=male; 2=female) | 1 | - | - | ||||||||||
| 2. Heavy Drinking Frequency | −.057 | 1 | 11.47 | 10.43 | |||||||||
| 3. Cannabis Use Frequency | −.075 | .250** | 1 | 18.20 | 31.10 | ||||||||
| 4. Positive Urgency | −.170* | .132* | .176** | 1 | 1.92 | 0.61 | |||||||
| 5. Negative Urgency | .043 | .142* | .256** | .689** | 1 | 2.34 | 0.59 | ||||||
| 6. Sensation Seeking | −.285** | .100 | .127 | .234** | .028 | 1 | 3.04 | 0.56 | |||||
| 7. Lack of Premeditation | .132* | .174** | .080 | .107 | .178** | .174** | 1 | 2.00 | 0.50 | ||||
| 8. Lack of Perseverance | .101 | .103 | .144* | .115 | .261** | −.181** | .344** | 1 | 2.07 | 0.47 | |||
| 9. Alcohol Problems | −.068 | .407** | .176** | .425** | .491** | .105 | .129* | .151* | 1 | 10.72 | 9.42 | ||
| 10. Cannabis Problems | −.083 | .202** | .527** | .222** | .299** | .134* | .066 | .144* | .396** | 1 | 3.12 | 4.33 | |
| 11. Childhood Maltreatment | .003 | −.064 | .047 | .372** | .254** | .049 | −.039 | .148* | .284** | .132* | 1 | 35.16 | 9.87 |
p < .05
p < .01
3.2 Mediation Models
Alcohol Problems
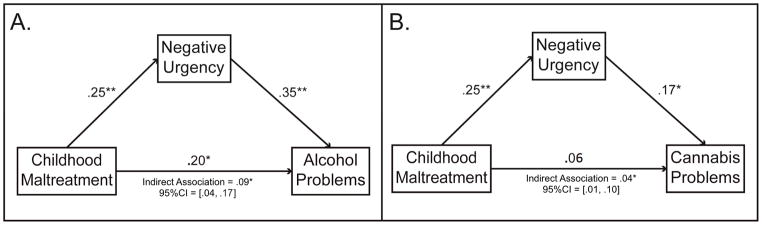
Figure 1 shows the results for the specific indirect association from childhood maltreat to alcohol problems via negative urgency, and Tables 2 and 3 contain the full set of parameter estimates for this model. Childhood maltreatment was a significant predictor of negative urgency, lack of perseverance, and positive urgency. When frequency of heavy drinking was not included as a covariate, only negative urgency and childhood maltreatment were significant, unique predictors of alcohol problems. When heavy drinking frequency was added as a covariate, it accounted for a significant portion of the variance in alcohol problems; still, both negative urgency and childhood maltreatment predicted unique variance in alcohol problems over and above heavy drinking frequency (see Table 2). Together the impulsivity facets and heavy drinking frequency accounted for approximately 40% of the variance in alcohol problems.
Figure 1.
Indirect associations between childhood maltreatment and both alcohol problems (panel A) and cannabis problems (panel B) mediated via negative urgency. In both models, the other four UPPS-P impulsivity scales were included as simultaneous mediators; however, these paths are not depicted in the figure (see Tables 2/3 for estimates). In both models, substance use (i.e., heavy drinking frequency or cannabis use frequency) was included as a covariate. Standardized regression coefficients are shown. * p < .05, ** p <.01, *** p < .001.
Table 2.
Direct associations from multiple mediation analyses examining associations of child maltreatment with alcohol problems and cannabis problems through UPPS-P facets of impulsivity
| Direct path from childhood maltreatment to each mediator | Direct paths from each mediator to alcohol problems | Direct paths from each mediator to cannabis problems | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||
| Independent Variable | Mediators | β | SE | p | R2 | Mediators | β | SE | p | ΔR2 | β | SE | p | ΔR2 |
| Childhood Maltreatment | Negative Urgency | .25** | .06 | <.001 | .065 | Negative Urgency | .35** | .08 | <.001 | .059 | .17* | .08 | .04 | .013 |
| Lack of Premeditation | −.04 | .07 | .56 | .002 | Lack of Premeditation | .01 | .06 | .97 | <.001 | −.03 | .06 | .63 | .001 | |
| Lack of Perseverance | .15* | .06 | .03 | .022 | Lack of Perseverance | −.01 | .06 | .89 | <.001 | .05 | .06 | .42 | .002 | |
| Sensation Seeking | .05 | .07 | .46 | .002 | Sensation Seeking | .03 | .06 | .54 | <.001 | .09 | .06 | .16 | .006 | |
| Positive Urgency | .37** | .06 | <.001 | .138 | Positive Urgency | .05 | .08 | .49 | .001 | −.02 | .08 | .78 | <.001 | |
| Childhood Maltreatment | .20** | .06 | <.001 | .031 | .06 | .06 | .30 | .003 | ||||||
| Alcohol/Cannabis Use | .36** | .05 | <.001 | .121 | .47** | .06 | <.001 | .199 | ||||||
Note. SE=standard error. The direct effect of childhood maltreatment on the mediators was the same in both the alcohol and the cannabis model. Substance use frequency was included as a covariate in both the alcohol and cannabis models. ΔR2 = increment in R2 when variable is added to model, representing proportion of variance in outcome that is uniquely predicted by that variable.
p<.05,
p<.01.
Table 3.
Indirect association estimates and confidence intervals for the UPPS-P facets included in the multiple mediation analyses of childhood maltreatment and alcohol problems, and childhood maltreatment and cannabis problems.
| Indirect Associations with Alcohol Problems | Indirect Associations with Cannabis Problems | ||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Independent Variable | Mediator | Coefficient | Boot SE | 95% Bias-corrected confidence interval | Coefficient | Boot SE | 95% Bias-corrected confidence interval |
| Childhood Maltreatment | Negative Urgency | .090* | .033 | .040, .168 | .043* | .021 | .012, .100 |
| Lack of Premeditation | −.001 | .004 | −.010, .008 | .001 | .005 | −.005, .016 | |
| Lack of Perseverance | −.001 | .009 | −.021, .017 | .008 | .010 | −.007, .032 | |
| Sensation Seeking | .002 | .005 | −.005, .017 | .004 | .008 | −.054, .031 | |
| Positive Urgency | .020 | .032 | −.044, .080 | −.009 | .031 | −.068, .052 | |
Based on 1,000 bootstrapped samples.
95% confidence interval does not contain zero.
We next examined the confidence intervals for the indirect associations (see Table 3). Consistent with our hypotheses, the indirect association between childhood maltreatment and alcohol problems via negative urgency was statistically significant, whereas the indirect associations from childhood maltreatment to alcohol problems via the other impulsivity scales were not significant. The significance of the indirect associations did not change depending on whether or not frequency of heavy drinking was included as a covariate.1
Cannabis Problems
Tables 2 and 3 also show the results of the mediation model predicting cannabis problems (note that the paths from childhood maltreatment to the impulsivity scales were redundant with those in the alcohol problems model). Consistent with the alcohol problems model, when frequency of marijuana use was not included, negative urgency was a significant, unique predictor of cannabis problems. However, sensation seeking also predicted unique variance in cannabis problems, β=.16, SE=.07, p=.02, whereas childhood maltreatment did not have a significant direct association with cannabis problems (unlike in the alcohol problems model). Further, when frequency of cannabis use was included in the model, the unique association between sensation seeking and cannabis problems was no longer statistically significant (see Table 2). Still, the unique association between negative urgency and cannabis problems remained statistically significant over and above frequency of cannabis use (see Table 2). The impulsivity facets and cannabis use frequency accounted for approximately 32% of the variance in cannabis problems.
When we examined the confidence intervals for the indirect associations (see Table 3), we again found that the specific indirect association between childhood maltreatment and cannabis problems via negative urgency was statistically significant whereas the other indirect associations were not. This indirect pathway through negative urgency is shown in Figure 1. As with the alcohol problems model, the significance of the indirect associations did not depend on whether cannabis use frequency was included as a covariate.
4. Discussion
This study examined the indirect associations between childhood maltreatment and problems with alcohol and cannabis via specific facets of impulsivity. Consistent with our hypotheses, we found that negative urgency was a unique mediator of the relationship between childhood maltreatment and both alcohol and cannabis problems. These results suggest that, among facets of impulsivity, negative urgency appears to have a particularly important role in the pathway between childhood maltreatment and problems with alcohol and cannabis, highlighting potential avenues for interventions.
A strength of this study was the examination of negative urgency in conjunction with several other facets of impulsivity in simultaneous mediation analyses. This is an important consideration given the shared variance among the various impulsivity facets observed in our own sample and other samples (Whiteside & Lynam, 2001). Of note, we found that negative urgency uniquely mediated the relationship between childhood maltreatment and problems with alcohol and cannabis. Although positive urgency emerged as a significant mediator of the relationship between childhood maltreatment and alcohol problems in supplementary analyses that did not account for the shared variance among the impulsivity facets, the fact that this association was not significant when the other facets were included in the model indicates that the mediating role of positive urgency appears to be better accounted for by its overlap with negative urgency. Thus, the current analyses help to clarify the role of different facets of impulsivity in the association between childhood maltreatment and substance problems, suggesting that rash action in the context of negative mood is a particularly relevant mediator.
The finding that negative urgency was a unique mediator of the association between childhood maltreatment and alcohol problems is consistent with research linking childhood maltreatment with deficits in emotion regulation (Maughan & Cicchetti, 2002), as well as studies showing that negative urgency is among the impulsivity facets most strongly related to alcohol problems (e.g., Cyders, Flory, Rainer, & Smith, 2009; see Coskunpinar et al., 2013, for a review). Further, relative to alcohol problems, fewer studies have examined the relationship between specific facets of impulsivity and cannabis problems. Although we found that sensation seeking was also an independent predictor of cannabis problems when frequency of cannabis use was not included as a covariate, only negative urgency remained a significant predictor of cannabis problems when controlling for cannabis use. Our study also provides initial evidence that childhood maltreatment has an indirect influence on cannabis problems through negative urgency. This finding underscores the importance of assessing problems across a range of substances among late adolescents with a history of childhood maltreatment, and future research should extend the present investigation to substances other than alcohol and cannabis.
Furthermore, that the indirect association between childhood maltreatment and cannabis use and problems remained significant even when controlling for frequency of use indicates that the role of negative urgency in the link between childhood maltreatment and substance problems cannot simply be explained by more frequent use of substances. This finding is consistent with the literature on drinking in the context of negative mood (Cooper, Frone, Russell, & Mudar, 1995; Merrill & Read, 2010), as well as previous studies that have reported a unique association between negative urgency and alcohol problems over and above frequency of use (e.g., Magid & Colder, 2007; Martens et al., 2010; Curcio & George, 2011). These findings indicate that individuals high on negative urgency are more likely to engage in riskier drinking practices and may have more general deficits in coping strategies (e.g., Merrill & Read, 2010; Smith et al., 2007). The present study extends these findings by showing that a similar process may operate in the association between negative urgency and cannabis problems. Thus, the role that negative urgency plays in the link between childhood maltreatment and alcohol and cannabis problems may be to increase the likelihood of engaging in riskier substance use in the context of negative emotions.
With respect to the associations between childhood maltreatment and each facet of impulsivity, our finding that childhood maltreatment was associated with negative urgency, positive urgency, and lack of perseverance is somewhat consistent with previous literature. Only a few studies have investigated the relationship between childhood maltreatment and these facets of impulsivity (Gagnon et al., 2013; Sujan et al., 2014). Our findings were generally consistent with these prior studies; however, the present study found an association between childhood maltreatment and positive urgency, whereas the Sujan et al. study did not. One potential explanation for this discrepancy is that Sujan et al. used a two-item assessment of childhood maltreatment while the present study used a comprehensive, validated measure of childhood maltreatment (i.e., the CTQ). Thus, more research is needed to further clarify the link between childhood maltreatment and the various facets of impulsivity.
Our finding that negative urgency mediates the association between childhood maltreatment and later alcohol and cannabis problems has potential clinical implications, highlighting specific avenues for interventions. For example, treatment focusing on strategies for coping with negative mood may be effective among late adolescents with a history of childhood maltreatment. There is also evidence that personality-targeted prevention programs for alcohol misuse can be effective (Conrod et al., 2013). Further, recent research on the neural basis of individual differences in negative urgency implicates the amygdala and orbitofrontal cortex (Cyders et al., 2014). Alterations in these brain regions have also been identified in individuals with a history of maltreatment (Hanson et al., 2010; Whittle et al., 2013). Focusing childhood maltreatment research on well-defined and extensively researched constructs like negative urgency is a potentially promising strategy for elucidating the brain-based mechanisms linking childhood maltreatment with drug and alcohol problems later in life, which could provide further insight into potential avenues for interventions.
There are some limitations of the current study that must be acknowledged. The first is that the data were cross-sectional; as a result, the temporal associations among the variables in our models cannot be established. Indeed, it is not possible to determine whether childhood maltreatment preceded the development of negative urgency and substance problems, or whether current substance problems may have instead affected the recall and reporting of childhood maltreatment and responses on measures of impulsivity. Moreover, the reliance on retrospective reports of childhood maltreatment is a limitation given that many years may have passed for some of the reported experiences. Future studies employing longitudinal designs will be necessary to address these issues directly.
A related issue is that third variable explanations cannot be ruled out. For example, traits such as impulsivity and substance use problems are heritable, and in part reflect a diathesis to externalizing behaviors more broadly (Krueger, Markon, Patrick, Benning, & Kramer, 2007). Therefore, the relationships among childhood maltreatment exposure, negative urgency, and substance problems may be partly attributable to gene-environment correlation, rather than a causal process per se. Another potential limitation of the present investigation is that our sample consisted mostly of undergraduate students who generally did not report significant metal health problems. Previous research has demonstrated that many adolescents who have problems with alcohol have comorbid psychiatric conditions (Goldstein et al., 2013). As a result, it is unclear whether our results would be generalizable to clinical or treatment-seeking samples.
Despite these limitations, the results of this investigation demonstrate that negative urgency is an important construct for understanding the link between childhood maltreatment and problems with alcohol and cannabis in late adolescence. By examining pathways through multiple impulsivity facets simultaneously, this study also provides evidence that negative urgency is particularly relevant as a mediator relative to other forms of impulsivity. Future studies should examine childhood maltreatment, negative urgency, and cannabis and alcohol problems in a longitudinal design to elucidate the direction of associations among these variables.
Highlights.
We examine indirect paths from childhood maltreatment to substance problems via impulsivity facets.
Negative urgency is a unique mediator of the association between childhood maltreatment and alcohol and cannabis problems.
Other facets of impulsivity are not unique mediators of these associations.
Footnotes
In order to determine whether controlling for the shared variance among the impulsivity facets had an impact on the results of the mediation analyses, we conducted supplementary analyses in which the mediating role of each impulsivity facet was examined in a separate model, so that estimates were not adjusted for shared variance with the other impulsivity facets. The results for negative urgency were not notably different in this analysis. The only observed difference was that positive urgency emerged as a significant predictor of alcohol problems, β=.30, SE=.06, p<.001, and the indirect association from childhood maltreatment to alcohol problems via positive urgency was also significant, β=.11, 95%CI [.06, .19]. A similar set of supplementary analyses predicting cannabis problems showed that there were no differences in the mediating effects of the impulsivity facets when they were examined in separate models.
Contributors
The study was conceived by CH. Data were analyzed by NS and JW. The manuscript was prepared by JW and NS. All authors contributed to and approved the final manuscript.
Conflict of Interest
The authors declare that they have no conflict of interest.
Author Disclosures
Role of Funding Sources
This research was supported by grants from the Canadian Institutes of Health Research (260418, 288905, 307742), ABMRF/The Foundation for Alcohol Research, and the Ontario Mental Health Foundation to Christian S. Hendershot. During the preparation of this manuscript, Jeffrey D. Wardell was supported by a postdoctoral fellowship from the Canadian Institutes of Health Research (MFE-140817), and Nicole M. Strang was supported by a postdoctoral fellowship from Intersections of Mental Health Perspectives in Addictions Training Research (IMPART).
References
- Adams ZW, Kaiser AJ, Lynam DR, Charnigo RJ, Milich R. Drinking motives as mediators of the impulsivity-substance use relation: Pathways for negative urgency, lack of premeditation, and sensation seeking. Addictive behaviors. 2012;37:848–855. doi: 10.1016/j.addbeh.2012.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annerbäck EM, Sahlqvist L, Svedin CG, Wingren G, Gustafsson P. Child physical abuse and concurrence of other types of child abuse in Sweden—Associations with health and risk behaviors. Child Abuse & Neglect. 2012;36:585–595. doi: 10.1016/j.chiabu.2012.05.006. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L. Childhood trauma questionnaire: A retrospective self-report manual. San Antonio, TX: The Psychological Corporation; 1998. [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, … Desmond D. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect. 2003;27:169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Brown SA, McGue M, Maggs J, Schulenberg J, Hingson R, Swartzwelder S, … Sher K. A developmental perspective on alcohol and youths 16 to 20 years of age. Pediatrics. 2008;121(Supplement 4):S290–S310. doi: 10.1542/peds.2007-2243D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Curtis W. An event-related potential study of the processing of affective facial expressions in young children who experienced maltreatment during the first year of life. Devopmental Psychopathology. 2005;17:641–677. doi: 10.1017/S0954579405050315. [DOI] [PubMed] [Google Scholar]
- Conrod PJ, O’Leary-Barrett M, Newton N, Topper L, Castellanos-Ryan N, Mackie C, Girard A. Effectiveness of a selective, personality-targeted prevention program for adolescent alcohol use and misuse: A cluster randomized controlled trial. JAMA psychiatry. 2013;70:334–342. doi: 10.1001/jamapsychiatry.2013.651. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology. 1995;69:990–1005. doi: 10.1037//0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Coskunpinar A, Dir AL, Cyders MA. Multidimensionality in impulsivity and alcohol use: A meta-analysis using the UPPS model of impulsivity. Alcoholism: Clinical and Experimental Research. 2013;37:1441–1450. doi: 10.1111/acer.12131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curcio AL, George AM. Selected impulsivity facets with alcohol use/problems: The mediating role of drinking motives. Addictive behaviors. 2011;36:959–964. doi: 10.1016/j.addbeh.2011.05.007. [DOI] [PubMed] [Google Scholar]
- Cyders MA, Dzemidzic M, Eiler WJ, Coskunpinar A, Karyadi KA, Kareken DA. Negative urgency mediates the relationship between amygdala and orbitofrontal cortex activation to negative emotional stimuli and general risk-taking. Cerebral Cortex. 2014 doi: 10.1093/cercor/bhu123. Available online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA, Flory K, Rainer S, Smith GT. The role of personality dispositions to risky behavior in predicting first-year college drinking. Addiction. 2009;104:193–202. doi: 10.1111/j.1360-0443.2008.02434.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA, Smith GT. Mood-based rash action and its components: Positive and negative urgency. Personality and Individual Differences. 2007;43(4):839–850. [Google Scholar]
- Cyders MA, Smith GT, Spillane NS, Fischer S, Annus AM, Peterson C. Integration of impulsivity and positive mood to predict risky behavior: Development and validation of a measure of positive urgency. Psychological Assessment. 2007;19:107–118. doi: 10.1037/1040-3590.19.1.107. [DOI] [PubMed] [Google Scholar]
- de Wit H. Impulsivity as a determinant and consequence of drug use: A review of underlying processes. Addiction Biology. 2009;14:22–31. doi: 10.1111/j.1369-1600.2008.00129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: The adverse childhood experiences study. Pediatrics. 2003;111:564–572. doi: 10.1542/peds.111.3.564. [DOI] [PubMed] [Google Scholar]
- Everson MD, Smith JB, Hussey JM, English D, Litrownik AJ, Dubowitz H, … Runyan DK. Concordance between adolescent reports of childhood abuse and child protective service determinations in an at-risk sample of young adolescents. Child Maltreatment. 2008;13:14–26. doi: 10.1177/1077559507307837. [DOI] [PubMed] [Google Scholar]
- Faulkner B, Goldstein AL, Wekerle C. Pathways from childhood maltreatment to emerging adulthood investigating trauma-mediated substance use and dating violence outcomes among child protective services–involved youth. Child Maltreatment. 2014 doi: 10.1177/1077559514551944. Available online ahead of print. [DOI] [PubMed] [Google Scholar]
- Fetzner MG, McMillan KA, Sareen J, Asmundson GJ. What is the association between traumatic life events and alcohol abuse/dependence in people with and without PTSD? Findings from a nationally representative sample. Depression and Anxiety. 2011;28:632–638. doi: 10.1002/da.20852. [DOI] [PubMed] [Google Scholar]
- Gagnon J, Daelman S, McDuff P, Kocka A. UPPS dimensions of impulsivity: Relationships with cognitive distortions and childhood maltreatment. Journal of Individual Differences. 2013;34:48–55. [Google Scholar]
- Goldstein AL, Henriksen CA, Davidov DM, Kimber M, Pitre NY, Afifi TO. Childhood maltreatment, alcohol use disorders, and treatment utilization in a national sample of emerging adults. Journal of Studies on Alcohol and Drugs. 2013;74:185–194. doi: 10.15288/jsad.2013.74.185. [DOI] [PubMed] [Google Scholar]
- Griffin MJ, Wardell JD, Read JP. Recent sexual victimization and drinking behavior in newly matriculated college students: A latent growth analysis. Psychology of Addictive Behaviors. 2013;27:966–973. doi: 10.1037/a0031831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson JL, Chung MK, Avants BB, Shirtcliff EA, Gee JC, Davidson RJ, Pollak SD. Early stress is associated with alterations in the orbitofrontal cortex: A tensor-based morphometry investigation of brain structure and behavioral risk. The Journal of Neuroscience. 2010;30:7466–7472. doi: 10.1523/JNEUROSCI.0859-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Press; 2013. [Google Scholar]
- Hingson RW, Heeren T, Winter M, Wechsler H. Magnitude of alcohol-related mortality and morbidity among US college students ages 18–24: Changes from 1998 to 2001. Annual Review of Public Health. 2005;26:259–279. doi: 10.1146/annurev.publhealth.26.021304.144652. [DOI] [PubMed] [Google Scholar]
- Kaiser AJ, Milich R, Lynam DR, Charnigo RJ. Negative urgency, distress tolerance, and substance abuse among college students. Addictive Behaviors. 2012;37:1075–1083. doi: 10.1016/j.addbeh.2012.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Benning SD, Kramer MD. Linking antisocial behavior, substance use, and personality: An integrative quantitative model of the adult externalizing spectrum. Journal of Abnormal Psychology. 2007;116:645–666. doi: 10.1037/0021-843X.116.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynam DR, Smith G, Cyders M, Fischer S, Whiteside S. The UPPS-P: A multidimensional measure of risk for impulsive behavior. Unpublished technical report 2007 [Google Scholar]
- Magid V, Colder CR. The UPPS impulsive behavior scale: Factor structure and associations with college drinking. Personality and Individual Differences. 2007;43:1927–1937. [Google Scholar]
- Martens MP, Pedersen ER, Smith AE, Stewart SH, O’Brien K. Predictors of alcohol-related outcomes in college athletes: The roles of trait urgency and drinking motives. Addictive Behaviors. 2011;36:456–464. doi: 10.1016/j.addbeh.2010.12.025. [DOI] [PubMed] [Google Scholar]
- Masten AS, Faden VB, Zucker RA, Spear LP. Underage drinking: A developmental framework. Pediatrics. 2008;121(Supplement 4):S235–S251. doi: 10.1542/peds.2007-2243A. [DOI] [PubMed] [Google Scholar]
- Maughan A, Cicchetti D. Impact of child maltreatment and interadult violence on children’s emotion regulation abilities and socioemotional adjustment. Child Development. 2002;73:1525–1542. doi: 10.1111/1467-8624.00488. [DOI] [PubMed] [Google Scholar]
- Merrill JE, Read JP. Motivational pathways to unique types of alcohol consequences. Psychology of Addictive Behaviors. 2010;24:705–711. doi: 10.1037/a0020135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollak SD. Early adversity and mechanisms of plasticity: Integrating affective neuroscience with developmental approaches to psychopathology. Developmental Psychopathology. 2005;17:735–752. doi: 10.1017/S0954579405050352. [DOI] [PubMed] [Google Scholar]
- Read JP, Colder CR, Merrill JE, Ouimette P, White J, Swartout A. Trauma and posttraumatic stress symptoms predict alcohol and other drug consequence trajectories in the first year of college. Journal of Consulting and Clinical Psychology. 2012;80:426–439. doi: 10.1037/a0028210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson JM, Ladd BO, Anderson KG. When you see it, let it be: Urgency, mindfulness and adolescent substance use. Addictive Behaviors. 2014;39:1038–1041. doi: 10.1016/j.addbeh.2014.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogosch FA, Oshri A, Cicchetti D. From child maltreatment to adolescent cannabis abuse and dependence: A developmental cascade model. Devopmental Psychopathology. 2010;22:883–897. doi: 10.1017/S0954579410000520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwandt ML, Heilig M, Hommer DW, George DT, Ramchandani VA. Childhood trauma exposure and alcohol dependence severity in adulthood: Mediation by emotional abuse severity and neuroticism. Alcoholism: Clinical and Experimental Research. 2013;37:984–992. doi: 10.1111/acer.12053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Settles RF, Cyders M, Smith GT. Longitudinal validation of the acquired preparedness model of drinking risk. Psychology of Addictive Behaviors. 2010;24:198–208. doi: 10.1037/a0017631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin SH, Edwards EM, Heeren T. Child abuse and neglect: Relations to adolescent binge drinking in the national longitudinal study of Adolescent Health (AddHealth) study. Addictive Behaviors. 2009;34:277–280. doi: 10.1016/j.addbeh.2008.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith GT, Fischer S, Cyders MA, Annus AM, Spillane NS, McCarthy DM. On the validity and utility of discriminating among impulsivity-like traits. Assessment. 2007;14:155–170. doi: 10.1177/1073191106295527. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring alcohol consumption: Psychosocial and biochemical methods. Totowa, NJ US: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Stephens RS, Roffman RA, Curtin L. Comparison of extended versus brief treatments for marijuana use. Journal of Consulting and Clinical Psychology. 2000;68:898–908. [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Summary of national findings. Rockville, MD: 2014. NSDUH series H-48, HHS publication no. (SMA) 14-4863. [PubMed] [Google Scholar]
- Sujan AC, Humphreys KL, Ray LA, Lee SS. Differential association of child abuse with self-reported versus laboratory-based impulsivity and risk-taking in young adulthood. Child Maltreatment. 2014;19:145–155. doi: 10.1177/1077559514543827. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 5. Boston, MA: Allyn & Bacon/Pearson Education; 2007. [Google Scholar]
- Verdejo-García A, Lawrence AJ, Clark L. Impulsivity as a vulnerability marker for substance-use disorders: review of findings from high-risk research, problem gamblers and genetic association studies. Neuroscience & Biobehavioral Reviews. 2008;32:777–810. doi: 10.1016/j.neubiorev.2007.11.003. [DOI] [PubMed] [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol and Drugs. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR. The Five Factor Model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences. 2001;30:669–689. [Google Scholar]
- Whiteside SP, Lynam DR, Miller JD, Reynolds SK. Validation of the UPPS impulsive behaviour scale: A four-factor model of impulsivity. European Journal of Personality. 2005;19:559–574. [Google Scholar]
- Whittle S, Dennison M, Vijayakumar N, Simmons JG, Yücel M, Lubman DI, … Allen NB. Childhood maltreatment and psychopathology affect brain development during adolescence. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52:940–952. doi: 10.1016/j.jaac.2013.06.007. [DOI] [PubMed] [Google Scholar]
- Zucker RA, Donovan JE, Masten AS, Mattson ME, Moss HB. Early developmental processes and the continuity of risk for underage drinking and problem drinking. Pediatrics. 2008;121(Supplement 4):S252–S272. doi: 10.1542/peds.2007-2243B. [DOI] [PMC free article] [PubMed] [Google Scholar]