Abstract
Objective
The paper examines direct and moderating effects of age on coping preferences for psychological distress among a sample of trauma exposed adults to inform treatment approaches for this population.
Methods
Using data from a community survey of trauma exposed urban-dwelling adults (n = 181), direct and moderating effects of coping preferences on the relationship between age and psychological distress were examined using hierarchical linear regression.
Results
Direct effects with distress were supported for age, gender, and coping preferences of avoidance and positive reframing. No direct effects with problem-focused coping were present, however, a significant interaction resulted with the relationship between age and level of reported distress.
Discussion
Problem-focused coping may provide a buffering effect on experiences with distress for older trauma exposed adults. Findings highlight the benefits of directive and action oriented approaches to care for aging adults. Implications for future intervention research and clinical considerations for treating trauma over the life course are discussed.
Keywords: trauma, coping, psychological distress, aging
Introduction
Limited definitive research exists on coping preferences with trauma related distress as a person ages with many studies presenting inconsistent findings and less of a focus on civilian populations making implications for the general population difficult (Böttche, Kuwert, & Kneavelsrud, 2012; Cook & Niederehe, 2007; Ogle, Rubin, Bernsten, & Siegler, 2013; Tracy, Morgenstern, Zivin, Aiello, & Galea, 2014). This is an important area of research given that in public healthcare settings up to 90% of clients report experiencing some form of trauma (SAMSHA, 2015). Commonly this exposure is associated with the increased risk of posttraumatic stress disorder (PTSD; Breslau, Peterson, Poisson, Schultz, & Lucia, 2004), depression, and other forms of psychological distress (Breslau et al., 2004; Cook, Dinnen, & O'Donnell, 2011; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). Trauma responses differ from those of younger individuals with variations in emotional adjustments to traumatic events, types of support to manage distress, and impact on physical health and mortality rates (Lohr, Palmer, Eidt, et al., 2015; Weiner, Monin, Mota, & Pietrzak, 2016). Trauma exposed older adults in public care systems are often less likely than younger populations to seek out and receive care when in need, extending disparities in initiation and use of mental health services for individuals as they age especially among minority older adults (Durai et al., 2011). The experiences of multiple stressful life events over the life course creates increased risk of cumulative distress impacting life satisfaction and psychological well-being as one ages if unresolved (Krause, 2004).
When examining types of experienced traumatic events, there are noted age related differences with younger populations reporting higher rates of violent crime and sexual assaults and older adults reporting events associated with sudden loss or sustained injuries (Hatch & Dohrenwend, 2007; Krause, 2004). Though traumatic events are reported to occur more frequently earlier in life, the experiences may exert lasting effects on coping strategies and impair quality of life with age (Bernick, Grinberg, Holynaty, & Rodgers, 2001). There is limited understanding of how coping with trauma exposure may differ when accounting for age related developmental needs (Tracy et al., 2014). Further, older adults are commonly underrepresented in community surveys examining consequences of traumatic events leaving a need to add to this area of research in the field of traumatic stress (Cook & Niederehe, 2007; Ogle et al., 2013)
Aging and Experiences with Trauma
Disparities in functional outcomes, access to services, and support resources for older adults are commonly associated with complicated adjustments to lifetime experiences including traumatic life-events (Krause, Shaw, & Cairney, 2004). Variations in the presentation of symptoms associated with traumatic stress in older adults can reduce screening for and connection to social, educational, and healthcare resources; increasing risk of burden in managing complicated age related care needs (Cook et al., 2011). These include late-life adjustments to changing health conditions, reduced socioeconomic status due to retirement or changes in employment status, stressful life events such as losses of loved ones, and functional declines (Kessler et al., 2005; Krause, 2004; Tanner, Martinez, & Harris, 2014). There is an inevitable interconnectedness of traumatic experiences over the life course that influences how older adults adjust to managing these psychosocial and health related needs as they age (Dulin & Passmore, 2010). A study by Ogle, Rubin & Siegler (2013) reported that individuals who experienced their most distressing trauma early in life reported increased rates of traumatic events over their life course, creating more reported mental health needs associated with posttraumatic stress, depression, anxiety, and decreased functioning into advanced age. This is especially significant given that depression and anxiety affect approximately 2-million older adults annually in the U.S., and highly associated with disease, disability, and mortality (Kessler et al., 1995; Tanner et al., 2014). For older adult trauma survivors, these recurrent experiences with trauma are also compounded by higher rates of co-morbidities of functional difficulties and chronic disease for this age group. Commonly these mental health needs are masked or overridden by acute health demands leading to high rates of service use associated with difficulties in coping and self-care (Cook & Niederehe, 2007). Such competing demands do not allow for either need to be adequately managed and requires simultaneous treatment to avoid persistent and unresolved distress (Chung, Berger, Jones, & Rudd, 2008; Krause et al., 2004).
Coping and Trauma
Treatment decisions and coping methods among trauma exposed populations are commonly related to one’s self-perceived need, stigma around formal mental health services, and contextual factors of support and previous experiences with approaches to self-care (Davis, Ressler, Schwartz, Stephens, & Bradley, 2008). The method of coping with a traumatic event may account for the resilience or alternatively exacerbate the mental health difficulties faced by individuals as they age. The emotional outcome of coping with a traumatic event may also be determined by characteristics of the event, personal attributes, cognitive appraisal of harm, and applied coping style (Böttche et al., 2012; Lazarus & Folkman, 1984).
Coping strategies are characterized as dynamic responses to specific situations, where an effort is made to reduce or avoid the effects of a stressor. This can be done by regulating the distress (emotion-focused coping) or by self-managing the problem causing the distress through information seeking or action oriented tasks (problem-focused coping; Carver, Scheier, & Weintraub, 1989; Chung, Werrett, Easthope, & Farmer, 2004; Lazarus & Folkman, 1984). Both emotion-focused coping strategies and problem-focused coping strategies involve attempts to change the external source of stress and are often considered to be functional or adaptive for maintaining well-being (e.g. Carver et al., 1989; Lazarus, 2007). One type of emotion-focused coping is positive reframing, a method that supports cognitive reorganization of the perceived event in order to find the good in an experienced stressor (Jensen, Thorensen, & Dyb, 2015; Littleton, Horsley, John, & Nelson, 2007). Problem-focused coping may include seeking emotional or instrumental support from others to address the stress (Lazarus & Folkman, 1991; Littleton et al., 2007). In problem-focused coping direct steps are taken to decrease or eliminate stressors or their effects. Less adaptive approaches to coping include avoidance and negative coping strategies. Avoidance coping supports disengaging from emotions and thoughts associated with the trauma (Folkman & Moskowitz, 2004) whereas negative coping supports the idea of giving up efforts to address a stressor due to inability to cope (Ghafoori, Barragan, Tohidian, & Palinkas, 2012).
There is contradictory research on coping strategies commonly employed by trauma exposed individuals as they age (Clapp & Beck, 2012). Avoidance coping is reported as the most commonly utilized coping strategy with increased age, especially when compounded with health issues, however, the effectiveness of avoidance coping is questionable (Littleton et al., 2007). The strategy supports deterring reoccurring thoughts associated with trauma experiences and related symptoms of psychological distress rather than effectively processing the experience (Chung et al., 2004). Other research supports that compared to younger populations, older individuals employ more adaptive and directive approaches to managing distress such as in problem-focused coping strategies (Krause et al., 2004). In regards to mental health outcomes, some literature suggests that older individuals who use emotion-focused coping strategies may experience a high level of emotional distress especially when compounded with managing chronic health conditions (Chung et al., 2008). Alternately, research exists that suggests those who use problem-focused strategies are more likely to experience a reduction of PTSD and positive outcomes (Bryant, Marosszeky, Crooks, Bauley, & Gurka, 2000). Studies on coping with traumatic events have found problem-solving strategies that support action oriented efforts that may reduce symptoms of pain and distress and facilitate adjustment (Jensen et al., 2015).
Overall there is inconsistent research that captures an understanding of constructs that contribute to age related differences in managing distress related to trauma with ranges from no differentiation to the discussion of significant impacts for older adults as they age (Böttche et al., 2012; Chung et al., 2004; Clapp & Beck, 2012; Lohr et al., 2015). Knowledge is needed to disentangle the experiences of lifetime trauma for older adults and the effects of age on coping preferences for psychological distress. Understanding the role of coping over the life course can inform care approaches that optimize quality of life for trauma survivors as they age. Profiling risk factors for poor mental health outcomes can also assist practitioners in improving screening, outreach, and treatment models of trauma informed care for those managing cumulative distress associated with age (Ghafoori, Barragan, & Palinkas, 2014b; Roberts, Gilman, Breslau, & Koenan, 2011). Further, this understanding extends patient-centered care strategies, making treatment models more relevant to age related developmental needs and congruent with individual treatment preferences (Ghafoori, Fisher, Koresteleva, & Hong, 2014c; Krause, 2004).
The purpose of the study is to clarify inconsistencies in the coping literature to determine if reported variations in coping preferences increase vulnerability for psychological distress among trauma exposed adults and older adults. The study aims are to: 1) Examine associations between age, coping preferences, and severity of psychological distress in trauma exposed urban dwelling adults. 2) Assess direct and moderating effects of coping preference on the relationship between age and severity of psychological distress in an age diverse adult sample. Based on findings from previous empirical literature, the current study hypothesizes that trauma exposed urban dwelling young and middle aged to older adults will present with differential risk factors for psychological distress due to variations in reported coping preferences.
Methods
Study Design and Data Collection
The study is a secondary data analysis from a cross-sectional community-based research study examining treatment barriers for low-income, urban dwelling, trauma exposed adults (Ghafoori et al., 2012). The study was approved by the California State University, Long Beach Institutional Review Board. Participants were recruited for the primary study from community health and mental health clinics in southern California. All participants were seeking either medical or mental health care. Participants were recruited prior to receiving any type of medical or mental health treatment and received a $10.00 non-cash incentive for participation. All recruitment was conducted by trained research assistants who screened clinic clients for voluntary interest in participation using a structured series of questions to assess meeting of inclusion criteria that included: English speaking; 18-years and older; self-reported having witnessed, experienced, or been confronted with any lifetime traumatic event that involved actual or threatened death or serious injury or threat to physical integrity of others to which the individual responded to intense fear, helplessness, or horror based on Criteria A1 and A2 for PTSD of the Diagnostic and Statistical Manual of Mental Disorders (4th edition; DSM-IV; American Psychiatric Association, 1994). Individuals who presented with psychosis, suicidal or homicidal thoughts, history of suicide or psychiatric hospitalizations in the past year, or substance abuse use in the past 24-hours did not qualify to participate in the study. A total of 215 people were screened for participation and 181 individuals met all study eligibility criteria and consented to participate.
Measures
Demographic characteristics were measured using a history form that included self-reported age at time of interview, gender, ethnic identity (African-American, Non-Hispanic White, Hispanic, Asian-Pacific Islander, Native American, or Other), marital status (dichotomized to reflect options of married or living as married vs. single/never married, separated or divorced, widowed), and highest level of education achieved (some high school or less, high school degree, associate’s degree or higher). Income was omitted from the regression analysis as the construct presented with no variance with the majority reporting income levels below poverty level. Ethnic identity was collapsed in the primary analysis to Non-Hispanic Whites compared to minorities that included those who identified as Hispanic, African-American, Asian-Pacific Islander, and Other. The decision to dichotomize the variable was made to best maximize power of available data given the overall small sample size, and the decision was supported through preliminary analysis that showed no bivariate relationships with individual ethnic identity categories and the outcome variable of psychological distress or hypothesized moderator of coping preference by type.
Coping preferences
Participants completed a 4-item questionnaire that examined self-reported approaches to coping with stressful life events. The questions asked participants, “Please indicate using the following scale what you generally do or how you feel when you experience challenges or stressful events”. Response options were based on a 4-item likert scale that ranged from “not at all”, “a little but”, “medium amount”, and “a lot” on when used the described coping technique. The questions for coping assessed: problem-focused coping, “I concentrate my efforts on doing something about it”; avoidance coping, “I turn to other activities, such as sleep, work, or using substances to take my mind off things; positive reframing coping, “I look for something good in what happened”, and negative coping, “I give up the attempt to get what I want”. The measure was not designed to be homogeneous but rather representative of diverse approaches to coping supported by previous studies examining coping behavior associated with trauma (Böttche et al., 2012; Ghafoori et al., 2012; Krause, 2004).
Psychological distress
The outcome variable of psychological distress was measured with the Brief Symptom Inventory Global Severity Index (BSI-GSI; Derogatis, 2001). The scale is a self-report measure that assesses experiences with nine dimensions of psychological distress and three global indices of distress in the previous 2-weeks. Scores were computed through converting the raw scores into t-scores based on normative data from community samples (Derogatis. 2001; Ghafoori et al., 2012). The BSI-GSI showed strong reliability with the sample, alpha = .87.
Analysis
Analysis was done using SPSS software (v.22; IBM Corp, 2013). All descriptive analysis, as well as cleaning of data and constructing variables that included examination of outliers and missing data analysis, was done initially. Mean, standard deviation, and percentages are presented to describe characteristics of the study sample (Table 1). Bivariate analysis was done to study initial relationships among variables and to inform the assessment of the necessary assumptions that must be met to conduct the regression and moderating analyses.
Table 1.
Summary of sample characteristics of low-income urban dwelling trauma exposed adults (n=181)
| Variable (range) | %/ Mean (SD) | Pearson r Psychological Distress (BSI-GIS) |
|---|---|---|
| Age (18–75 years) | 43.3 (12.3) | .145 * |
| Gender: Female | 33.7% | .215** |
| Married or married like relationship | 12.7% | −.026 |
| Ethnic Identity | ||
| Non-Hispanic White | 29.8% | .062 |
| African-American | 44.8% | −.057 |
| Hispanic | 19.3% | −.025 |
| Asian-Pacific Islander | 1.7% | .056 |
| Other – Race/Ethnicity | 4.4% | .014 |
| Education level | .021 | |
| Some high school or less | 26.5% | |
| High school graduate or equivalent | 45.3% | |
| Associates degree or higher | 28.2% | |
| Coping – Problem-focused | 96.1% | −.032 |
| Coping - Avoidance | 86.7% | .140 |
| Coping – Positive reframe | 90.1% | −.190** |
| Coping – Negative | 51.4% | −.002 |
| Brief Symptom Inventory (BSI-GIS): Psychological Distress |
59.5 (11.2) |
p≤ .05;
p≤ .01;
p≤ .001
In order to assess the proposed analytical model, a hierarchical linear regression was performed using Maximum Likelihood Estimation to examine direct effects and indirect effects of the probability of distribution of psychological distress given each independent variable. Three models were examined. Model one examined direct effects of demographic characteristics. Model two assessed associations with coping preferences controlling for demographics. The third analytical model examined the moderating effects of age and individual coping preferences on the level of expressed psychological distress for the sample controlling for demographics and the individual coping preferences. To assess model fit, the Adjusted R squared statistics were reviewed but interpreted cautiously as it is not a reliable statistic in model fit assessment in this case given the sample size (Borooah, 2002).
Moderation Analysis
A moderation model was examined to estimate the interaction effect of each coping preference construct with age to assess the association with level of psychological distress as measured by the BSI-GIS. Interaction terms were created for age with each coping preference by type. Age was kept as a continuous level variable in order to maximize use of all available data (Cohen & Cohen, 1983) and was mean-centered prior to creating the interaction term with a dichotomized individual coping preference variable to address the potential for multicollinearity (Holmbeck, 1997). Coping preferences were dichotomized to reflect comparison of those reported not using each type of coping versus those who reported “a little” “medium amount” to “all the time” and used in the interactions term with age to increase interpretability of the moderation effect on psychological distress. Post-hoc interpretation of significant interactions are presented by plotting the intercepts and slopes of the regression lines for varying degrees of reported use for significant moderating effects with coping preference. This allows for the assessment of change in the relationship between age on reported psychological distress (Holmbeck, 1997).
Results
The sample included in the analysis reflected participants who consented to participate in the study and completed the questionnaire in full (n = 181). Descriptive statistics (see Table 1) reflect an average age of the sample as 43.7 (SD = 12.3) with a range from 18–75 years. The majority of the sample was male and reported low-incomes with annual household incomes of under $14,999. The ethnic breakdown of the sample was comprised of 29.8% non-Hispanic Whites and 70.2% of individuals from ethnic-minority backgrounds, represented predominately by African-Americans at 44.8% and Hispanics at 19.3%. The sample reported to be predominately single which included those who were divorced or widowed and most with a high school diploma (45.3%). Across the coping preferences, problem-focused was most commonly reported as used to manage stressful events (96.1%) with negative coping the least (51.4%). The BSI-GSI scoring reflects a sample meeting threshold levels of clinically significant range for symptomatic distress (M = 59.5, SD = 11.2), which for the general population estimates for the BSI-GSI are reported as a score of greater than 63 (Derogatis, 2001).
In reviewing bivariate relationships (see Table 1) higher age (Pearson r = .145, p ≤ .05) and females in the sample (Pearson r = .215, p ≤ .01) were associated with increased psychological distress. Of the coping preferences, only positive reframing coping was associated with lower levels of experienced psychological distress (Pearson r = −.190, p ≤ .01).
Direct Effects and Moderating Analysis
Analysis of direct effects in the full model (Model 3; see Table 2) with psychological distress were supported for increasing age (t = 2.28, p = .023, β = 1.077), gender (female; t = 3.63, p = .000, β = .265), and coping preferences of avoidance (t = 3.26, p = .001, β = .227) and positive reframing coping (t = −.2.45, p = .015, β = −.183). Participants in the sample who used positive reframing coping reported lower levels of psychological distress. Those though who reported use of avoidance coping experienced higher psychological distress. There were no direct effects with negative coping or problem-focused coping preferences. In reviewing the interaction terms of coping preferences and age, there was no significant moderations effect with avoidance, positive reframing, or negative coping. However, a significant interaction effect resulted for age and problem-focused coping preferences on level of reported psychological distress (t = −2.76, p = .006, β = −1.05). Middle aged to older individuals reported lower levels of distress when using problem-focused coping than those who reported using this coping style to a lesser degree. The R squared value for the three tested models showed the highest in the final moderation model with 16.4% of the variance accounted for when controlling for the direct effects of demographic characteristics and individual coping preferences.
Table 2.
Results of regression analysis examining the direct and moderating effects of coping preferences on the relationship between age and psychological distress for low-income urban-dwelling trauma exposed adults (n=181)
| Model 1 Standardized Estimates |
Model 2 Standardized Estimates |
Model 3 Standardized Estimates |
|
|---|---|---|---|
| Age | .196** | .214** | 1.077* |
| Female | .266*** | .231** | .265*** |
| Education | −.026 | −.013 | −.010 |
| Married or living as married |
−.052 | −.069 | −.088 |
| Minority Status | −.079 | −.089 | −.084 |
| Coping – Problem- focused |
−.077 | −.114 | |
| Coping - Avoidance | .222** | .227*** | |
| Coping – Positive reframe |
− 0.177* | −.183* | |
| Coping – Negative | −.025 | −.031 | |
| Coping – Problem- focused × Age |
−1.05** | ||
| Coping - Avoidance × Age |
.222 | ||
| Coping – Positive reframe × Age |
−.006 | ||
| Coping – Negative × Age |
−.054 | ||
| Adjusted R2 | 0.065 | .141 | .164 |
p≤ .05;
p≤ .01;
p≤ .001
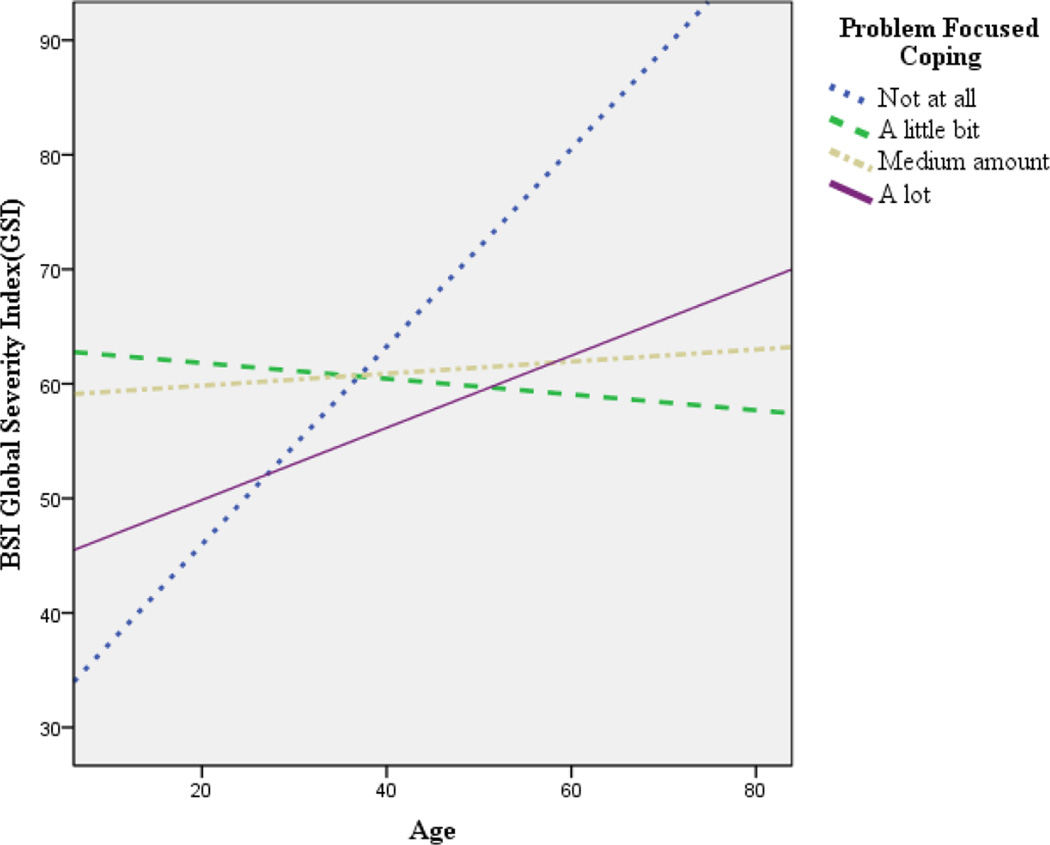
Post-hoc analysis examined the intercepts and slopes of the regression lines for values representing varying reported degrees of use of problem-focused coping values (Figure 1). Plotting the interaction terms for the association of problem-focused coping substantiated moderating effects of the coping style on service use when accounting for age, especially for those who reported more frequent use of this approach. The relationship between increased age and increased psychological distress strengthened when use of problem-focused coping decreased. Though there was limited variance in the distribution of responses of those who reported not using problem-focused therapy within the sample, the trend illustrated in the post-hoc analysis supports the assertion that variations in psychological distress resulted for those with increasing age who asserted using incrementally higher degrees of problem-focused coping.
Figure 1.
Moderation effect of degree of use of problem-focused coping on the relationship between age and experienced psychological distress
Discussion
The findings reflect a significant association of age and coping preferences with degree of psychological distress, supporting the primary study hypothesis. Specifically, the use of problem-focused coping buffered the experience of psychological distress with increasing age of the sample. Direct effects for coping with distress was most strongly supported for avoidance coping style, with participants who reported avoidance coping also reporting higher levels of psychological distress. This finding is consistent with the literature on avoidance coping that indicates positive short-term effects but lower long-term benefit in managing trauma related distress (Chung et al., 2004). Positive reframing coping, an emotion-focused coping strategy, was also significantly associated with distress, however, yielded lower distress for the sample when implored. This finding is consistent with research that suggests cognitive restructuring is helpful in providing a proactive approach to processing a traumatic event (Littleton et al., 2007). Neither avoidance nor positive reframing coping maintained significance when accounting for age.
Problem-focused coping emerged as a significant moderator only when accounting for age. Trauma exposed adults in the sample presented with differential risk factors for psychological distress based on the reported level of use of problem-focused coping with increasing age. However, younger aged adults maintained lower levels of distress without using problem-focused coping. This finding is consistent with literature that suggests problem-focused coping is most endorsed by older trauma exposed populations (Compas, Connor-Smith, Saltzman, & Thomsen, 2001). In addition, in the wider mental health literature, age has been found to be positively correlated with problem-focused coping (Siu, Spector, Cooper, & Donald, 2001). The results are consistent with life span models of human development and control (e.g. Hertel, Rauschenbach, Thielgen, & Krumm, 2015) where older adults often apply more active coping strategies when faced with distressing situations. It is possible that older adults are more likely to utilize problem-focused coping strategies to enhance a sense of adjustment to traumatic stressors and higher perceived control; both are associated with reduced stress and improved recovery after a traumatic event (Jensen et al., 2015). Additional research is necessary to further understand these relationships and the role of problem-focused coping for older adults who have experienced traumatic events.
The current study adds to the existing literature by highlighting that females and older adults in this sample exhibited increased distress associated with a traumatic event. This finding is consistent with the literature on risk factors for mental health difficulties after traumatic stress exposure, considering some studies have found that females and older adults have increased risk for PTSD and other trauma related disorders (Cherry, Sampson, Nezat, Cacamo, Marks, & Galea, 2015; Galea, Nandi, & Vlahov, 2005;). Females and specifically older women are commonly reported as having higher rates of mental health service use and tendency to seek out support for mental health needs compared to males (Kessler et al., 2005). An understanding that females who have life experiences with trauma may have compounded health, mental health, and service needs in managing associated distress with age is important when working with this population (Cook et al., 2011).
Limited studies exist that capture a consistent understanding of factors that contribute to age related differences in managing distress related to trauma (Clapp & Beck, 2012). There are noted differences between younger and older adult populations in rates of service use to manage distress and coping preferences with younger populations using less proactive approaches than older adults (Krause, 2004). However trauma exposed older adults present with greater levels of impaired physical functioning impairing quality of life at a higher degree as they age (Krause et al., 2004). In trauma exposed populations, these complications may influence service use, competing health demands, and cumulative stress, which creates a burden on managing mental health needs that increase with age (Krause et al., 2004; Ogle et al., 2013). Our findings reinforce previous research with older adults indicating interventions using modalities such as problem solving, emotion-focused, and behavioral activation approaches that are effective with this population (Clap & Beck, 2012). Such methods assist by offering a present oriented approach to emotional management, active engagement in daily activities, and active methods to overcome barriers to care. The current study highlights the need for service providers to consider problem-focused coping strategies for trauma-exposed older adults since these strategies may be appropriate and in-line with the developmental needs of this population. In doing so, positive outcomes are more likely to be sustainable and used as distress emerges over the life course.
This study has limitations that warrant cautious interpretation of the results. Findings from our current sample of treatment seeking trauma survivors may not be generalizable to other populations. The current study utilized a cross-sectional design that does not allow for causal assignment. Participants in the current study were also selected based on a purposeful rather than random sampling method, which could result in a non-representative sample and selection bias. The sample was comprised of individuals who were seeking services from community clinics providing health and mental health services however the stage of data collection was prior to participants receiving any type of treatment from the recruitment sites. This though can limit the generalizability of the findings to help-seeking groups (Ghafoori et al. 2014b). Since most individuals in the study reported very low income levels, we could also not assess the role of poverty for the sample. Relating to measurement, self-report measures were used instead of structured interviews to assess psychological distress; therefore, the external validity of our results is limited. Additionally, the coping measure used in the current study has no psychometrics and was not used as a homogenous scale for coping but rather provided a review of individual coping styles. With that, it may not have represented the complexity of the experience of managing trauma related stressors. Limitations in the variance of the distribution of the problem –focused coping variable also presents constraints to the presented research; however, it provides a basis to investigate further how incremental variations in coping with traumatic events impact functional outcomes for individuals as they age. A future prospective study with a larger sample size may further elucidate the relationship between age, coping preferences, and psychological distress. A strength of the current research is that our findings add to the literature on individual level factors and the role of coping as a possible moderator in the relationship between age and psychological distress.
Conclusion
Understanding factors that influence mental health outcomes and coping over the life course can inform approaches to care that optimize quality of life for trauma survivors as they age. Mental health treatment that considers the complex relationships among risk factors, coping, and psychological distress found in the current study are recommended. For example, interventions that incorporate both emotion-focused coping strategies and problem-focused strategies may be appropriate for low-income, culturally diverse trauma survivors, with a particular focus on problem-focused strategies for middle aged and older adults. Profiling risk factors for maladaptive coping strategies and outcomes can assist practitioners in improving screening for experiences with complex trauma, outreach, and treatment models of trauma informed care for those managing cumulative distress associated with trauma (Ghafoori et al., 2014b; Roberts et al., 2011). Further, this can inform patient-centered care strategies that make treatment models more relevant to aging populations and congruent with individual treatment preferences (Ghafoori et al., 2014c; Krause, 2004). Future research would benefit from examining specific factors that promote positive coping for trauma exposed individuals as they age. Specifically, understanding how contextual factors, such as support resources and service system structures, can foster increased rates of mental health service use for trauma exposed older adults given the persistent low rate of use by this population. Additional questions that can inform outreach, screening, and intervention development include: How do symptom profiles related to expressed traumatization change for individuals as they age? What points of intervention would support modes to counteract the differential rates of distress as individuals enter middle to older adulthood? This knowledge will not only highlight risk factors for poorer outcomes in this population and help target interventions but also support treatment approaches tailored to address the unique health, social, and mental health needs of trauma exposed individuals as they age.
Acknowledgments
Support was provided by NIH grant 1P20MD003942-01 and the NIH Health Disparities Loan Repayment Program. The authors acknowledge the assistance of Dennis Fisher, Kristin Powers, Alina Sgattoni, Lawrence Alexander III, Chelsea Edgecumbe, and Olga Korosteleva in the parent study protocol development.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Bernick L, Grinberg A, Holynaty L, Rodgers M. Caring for survivors of the Holocaust. The Canadian Nurse. 2001;97(3):25. [PubMed] [Google Scholar]
- Borooah VK. Logit and Probit: Ordered and multinomial models. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- Böttche M, Kuwert P, Knaevelsrud C. Posttraumatic stress disorder in older adults: An overview of characteristics and treatment approaches. International Journal of Geriatric Psychiatry. 2012;27(3):230–239. doi: 10.1002/gps.2725. http://dx.doi.org/10.1002/gps.2725. [DOI] [PubMed] [Google Scholar]
- Breslau N, Peterson E, Poisson L, Schultz L, Lucia V. Estimating post-traumatic stress disorder in the community: Lifetime perspective and the impact of typical traumatic events. Psychological Medicine. 2004;34(5):889–898. doi: 10.1017/s0033291703001612. http://dx.doi.org/10.1017/S0033291703001612. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Marosszeky JE, Crooks J, Baguley I, Gurka J. Coping style and post-traumatic stress disorder following severe traumatic brain injury. Brain Injury. 2000;14(2):175–180. doi: 10.1080/026990500120826. http://dx.doi.org/10.1080/026990500120826. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. Journal of Personality and Social Psychology. 1989;56(2):267. doi: 10.1037//0022-3514.56.2.267. http://dx.doi.org/10.1037/0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Cherry KE, Sampson L, Nezat PF, Cacamo A, Marks LD, Galea S. Long-term psychological outcomes in older adults after disaster: relationships to religiosity and social support. Aging & Mental Health. 2015;19(5):430–443. doi: 10.1080/13607863.2014.941325. http://dx.doi.org/10.1080/13607863.2014.941325. [DOI] [PubMed] [Google Scholar]
- Chung M, Berger Z, Jones R, Rudd H. Posttraumatic stress and co-morbidity following myocardial infarction among older patients: The role of coping. Aging and Mental Health. 2008;12(1):124–133. doi: 10.1080/13607860701366152. http://dx.doi.org/10.1080/13607860701366152. [DOI] [PubMed] [Google Scholar]
- Chung MC, Werrett J, Easthope Y, Farmer S. Coping with Post-Traumatic Stress: Young, middle-aged and elderly comparisons. International Journal of Geriatric Psychiatry. 2004;19(4):333–343. doi: 10.1002/gps.1095. http://dx.doi.org/10.1002/gps.1095. [DOI] [PubMed] [Google Scholar]
- Clapp JD, Beck JG. Treatment of PTSD in older adults: Do cognitive-behavioral interventions remain viable? Cognitive and Behavioral Practice. 2012;19(1):126–135. doi: 10.1016/j.cbpra.2010.10.002. http://dx.doi.org/10.1016/j.cbpra.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum; 1983. [Google Scholar]
- Compas BE, Connor-Smith JK, Saltzman H, Thomsen AH, Wadsworth ME. Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychological Bulletin. 2001;127(1):87–127. http://dx.doi.org/10.1037//0033-2909.127.1.87. [PubMed] [Google Scholar]
- Cook JM, Dinnen S, O'Donnell C. Older women survivors of physical and sexual violence: A systematic review of the quantitative literature. Journal of Women's Health. 2011;20(7):1075–1081. doi: 10.1089/jwh.2010.2279. http://dx.doi.org/10.1089/jwh.2010.2279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook JM, Niederehe G. Trauma in older adults. In: Friedman MJ, Keane TM, Resick PA, editors. Handbook of PTSD: Science and practice. New York, NY: Guilford Press; 2007. pp. 252–276. [Google Scholar]
- Davis RG, Ressler KJ, Schwartz AC, Stephens KJ, Bradley RG. Treatment barriers for low-income, urban African Americans with undiagnosed posttraumatic stress disorder. Journal of Traumatic Stress. 2008;21(2):218–222. doi: 10.1002/jts.20313. http://dx.doi.org/10.1002/jts.20313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR. BSI 18, Brief Symptom Inventory 18: Administration, scoring and procedures manual. Minneapolis, MN: NCS Pearson; 2001. [Google Scholar]
- Dulin PL, Passmore T. Avoidance of potentially traumatic stimuli mediates the relationship between accumulated lifetime trauma and late-life depression and anxiety. Journal of Traumatic Stress. 2010;23(2):296–299. doi: 10.1002/jts.20512. http://dx.doi.org/10.1002/jts.20512. [DOI] [PubMed] [Google Scholar]
- Durai UNB, Chopra MP, Coakley E, Llorente MD, Kirchner JE, Cook JM, Levkoff SE. Exposure to trauma and posttraumatic stress disorder symptoms in older veterans attending primary care: Comorbid conditions and self-rated health status. Journal of the American Geriatrics Society. 2011;59(6):1087–1092. doi: 10.1111/j.1532-5415.2011.03407.x. http://dx.doi.org/10.1111/j.1532-5415.2011.03407.x. [DOI] [PubMed] [Google Scholar]
- Folkman S, Moskowitz JT. Coping: pitfalls and promise. Annual Review of Psychology. 2004;55(1):745–774. doi: 10.1146/annurev.psych.55.090902.141456. http://dx.doi.org/10.1146/annurev.psych.55.090902.141456. [DOI] [PubMed] [Google Scholar]
- Galea S, Nandi A, Vlahov D. The epidemiology of post-traumatic stress disorder after disasters. Epidemiological Review. 2005;27:78–91. doi: 10.1093/epirev/mxi003. http://dx.doi.org/10.1093/epirev/mxi003. [DOI] [PubMed] [Google Scholar]
- Ghafoori B, Barragan B, Tohidian N, Palinkas L. Racial and ethnic differences in symptom severity of PTSD, GAD, and depression in trauma-exposed, urban, treatment-seeking adults. Journal of Traumatic Stress. 2012;25(1):106–110. doi: 10.1002/jts.21663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghafoori B, Barragan B, Palinkas L. Mental health service use after trauma exposure: A mixed methods study. The Journal of Nervous and Mental Disease. 2014;202(3):239. doi: 10.1097/NMD.0000000000000108. http://dx.doi.org/10.1097/NMD.0000000000000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghafoori B, Fisher DG, Koresteleva O, Hong M. Factors associated with mental health service use in urban, impoverished, trauma-exposed adults. Psychological Services. 2014;11(4):451–459. doi: 10.1037/a0036954. http://dx.doi.org/10.1037/a0036954. [DOI] [PubMed] [Google Scholar]
- Hatch S, Dohrenwend B. Distribution of traumatic and other stressful life events by race/ethnicity, gender, SES and age: A review of the research. American Journal of Community Psychology. 2007;40(3–4):313–332. doi: 10.1007/s10464-007-9134-z. http://dx.doi.org/10.1007/s10464-007-9134-z. [DOI] [PubMed] [Google Scholar]
- Hertel G, Rauschenbach C, Thielgen MM, Krumm S. Are older workers more active copers? Longitudinal effects of age-contingent coping on strain at work. Journal of Organizational Behavior. 2015;36:514–537. http://dx.doi.org/10.1002/job.1995. [Google Scholar]
- Holmbeck GN. Toward terminological, conceptual, and statistical clarity in the study of mediators and moderators: Examples from the child-clinical and pediatric psychology literatures. Journal of Consulting and Clinical Psychology. 1997;65(4):599. doi: 10.1037//0022-006x.65.4.599. http://dx.doi.org/10.1037/0022-006X.65.4.599. [DOI] [PubMed] [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp; Released 2013. [Google Scholar]
- Jensen TK, Thorensen S, Dyb G. Coping responses in the midst of terror: The July 22 terror attack at Utøya Island in Norway. Health and Disability. 2015;56:45–62. doi: 10.1111/sjop.12182. http://dx.doi.org/10.1111/sjop.12182. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Demler O, Frank RG, Olfson M, Pincus HA, Walters EE, Zaslavsky AM. Prevalence and treatment of mental disorders, 1990 to 2003. New England Journal of Medicine. 2005;352(24):2515–2523. doi: 10.1056/NEJMsa043266. http://dx.doi.org/10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. http://dx.doi.org/10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Krause N. Lifetime trauma, emotional support, and life satisfaction among older adults. The Gerontologist. 2004;44(5):615–623. doi: 10.1093/geront/44.5.615. http://dx.doi.org/10.1093/geront/44.5.615. [DOI] [PubMed] [Google Scholar]
- Krause N, Shaw BA, Cairney J. A descriptive epidemiology of lifetime trauma and the physical health status of older adults. Psychology and Aging. 2004;19(4):637–648. doi: 10.1037/0882-7974.19.4.637. http://dx.doi.org/10.1037/0882-7974.19.4.637. [DOI] [PubMed] [Google Scholar]
- Lazarus RS. Stress and emotion: A new synthesis. In: Monat A, Lazarus RS, Reevy G, editors. The Praeger Handbook on Stress and Coping. Vol. 1. New York, NY, US: Springer; 2007. pp. 33–51. [Google Scholar]
- Lazarus RS, Folkman S. Stress appraisal and coping. New York: 1984. Springer ed. [Google Scholar]
- Lazarus RS, Folkman S. The Concept of Coping. In: Lazarus AMRS, editor. Stress and coping: An anthology. 3rd. New York, NY, US: Columbia University Press; 1991. pp. 189–206. [Google Scholar]
- Littleton H, Horsley S, John S, Nelson DV. Trauma coping strategies and psychological distress: A meta-analysis. Journal of Traumatic Stress. 2007;20(6):977–988. doi: 10.1002/jts.20276. http://dx.doi.org/10.1002/jts.20276. [DOI] [PubMed] [Google Scholar]
- Lohr JB, Palmer BW, Eidt CA, Aailaboyina S, Mausbach BT, Wolkowitz OM, Jeste DV. Is post-traumatic stress disorder associated with premature senescence? A review of the literature. The American Journal of Geriatric Psychiatry. 2015;23(7):709–725. doi: 10.1016/j.jagp.2015.04.001. http://dx.doi.org/10.1016/j.jagp.2015.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogle CM, Rubin DC, Berntsen D, Siegler IC. The frequency and impact of exposure to potentially traumatic events over the life course. Clinical Psychological Science. 2013;1(4):426–434. doi: 10.1177/2167702613485076. http://dx.doi.org/10.1177/2167702613485076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogle CM, Rubin DC, Siegler IC. The impact of the developmental timing of trauma exposure on PTSD symptoms and psychosocial functioning among older adults. Developmental Psychology. 2013;49(11):2191–2200. doi: 10.1037/a0031985. http://dx.doi.org/10.1037/a0031985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts AL, Gilman SE, Breslau J, Breslau N, Koenen KC. Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological Medicine. 2011;41(1):71–83. doi: 10.1017/S0033291710000401. http://dx.doi.org/10.1017/S0033291710000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siu O, Spector PE, Cooper CL, Donald I. Age differences in coping and locus of control: A study of managerial stress in Hong Kong. Psychology and Aging. 2001;16:707–710. doi: 10.1037//0882-7974.16.4.707. http://dx.doi.org/10.1037/0882-7974.16.4.707. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Service Administration (SAMSHA. Trauma and Violence. 2015 Retrieved from SAMSHA, http://www.samhsa.gov/trauma-violence.
- Tanner EK, Martinez IL, Harris M. Examining functional and social determinants of depression in community-dwelling older adults: Implications for practice. Geriatric Nursing. 2014;35(3):236–240. doi: 10.1016/j.gerinurse.2014.04.006. http://dx.doi.org/10.1016/j.gerinurse.2014.04.006. [DOI] [PubMed] [Google Scholar]
- Tracy M, Morgenstern H, Zivin K, Aiello A, Galea S. Traumatic event exposure and depression severity over time: results from a prospective cohort study in an urban area. Social Psychiatry and Psychiatric Epidemiology. 2014;49(11):1769–1782. doi: 10.1007/s00127-014-0884-2. http://dx.doi.org/10.1007/s00127-014-0884-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner MR, Monin JK, Mota N, Pietrzak RH. Age Differences in the association of social support and mental health in male U.S. Veterans: Results from the national health and resilience in veterans study. The American Journal of Geriatric Psychiatry. 2016 doi: 10.1016/j.jagp.2015.11.007. in press http://dx.doi.org/10.1016/j.jagp.2015.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]