Abstract
Objective
To determine the interrelationships during early pregnancy of complement-activation fragments Bb, C3a and sC5b-9, and angiogenesis-related factors placental growth factor (PiGF), soluble fms-like tyrosine kinase-1 (sFlt-1) and soluble endoglin (sEng), and their associations with pre-eclampsia.
Design
Prospective cohort study.
Setting
Denver complement study (June 2005–June 2008).
Population
A total of 668 pregnant women with singleton gestations, recruited between 10 and 15 weeks of gestation.
Methods
Using univariable and multivariable logistic regression analysis, concentrations of complement-activation fragments and angiogenesis-related factors were compared between 10 and 15 weeks of gestation in women who subsequently did or did not develop pre-eclampsia. Interrelationships between these variables were tested using the non-parametric Spearman rank correlation coefficient.
Main outcome measure
Pre-eclampsia. The association of complement-activation fragments and angiogenesis-related factors with obesity was also examined.
Results
The mean (±SD) levels of complement Bb in early pregnancy among women who did and did not develop pre-eclampsia were 0.84 (±0.26) µg/ml and 0.69 (±0.2) µg/ml, respectively (P = 0.001). Concentrations of PiGF were significantly (P = 0.01) lower (31 ± 12 pg/ml) in early pregnancy in the pre-eclamptic group of women, as compared with the normotensive group (39 ± 32 pg/ml). The adjusted odds ratio (AOR) of Bb and PiGF were 2.1 (CI = 1.4–3.1, P < 0.0003) and 0.2 (CI = 0.07–0.7, P = 0.01), respectively. There was no significant difference in the levels of C3a, sC5b-9, sFlt-1 and sEng in early pregnancy among women who developed pre-eclampsia, compared with women who remained normotensive during pregnancy. Higher levels of Bb (P = 0.0001) and C3a (P = 0.03), and lower levels of sFlt-1 (P = 0.0002) and sEng (P = 0.0001) were found among women with obesity, compared with non-obese controls. No meaningful relationships were found between the complement-activation fragments and the angiogenesis-related factors.
Conclusions
In this cohort during early pregnancy, increased concentrations of complement-activation factor Bb and lower concentrations of PiGF were associated with the development of pre-eclampsia later in pregnancy.
Keywords: Angiogenesis-related factors, complement-activating factors, obesity, pre-eclampsia
Introduction
Pre-eclampsia is an important hypertensive condition of pregnancy, and causes considerable maternal, fetal and neonatal morbidity and mortality.1 In the last decade many researchers have demonstrated that pre-eclampsia is characterised by an imbalance in placental-derived angiogenesis-related factors, notably placental growth factor (PiGF), soluble fms-like tyrosine kinase-1 [sFlt-1 (also known as VEGF receptor 1)] and soluble endoglin (sEng). Prospective clinical studies have shown that lower levels of the pro-angiogenic factor PiGF, and higher levels of the anti-angiogenic factors sFlt-1 and sEng, are found in the serum of women who subsequently develop pre-eclampsia several weeks before the clinically apparent onset of this hypertensive disease of pregnancy.2–4
The syndrome of pre-eclampsia is also associated with dysregulation of the immune system.5,6 Indeed, in recent times our group has shown a significant link between inflammation related to complement activation in early human pregnancy with the development of pre-eclampsia later in pregnancy.7 Evidence from murine studies also suggests an important role for complement activation in intrauterine fetal death and intrauterine growth restriction (IUGR).8,9 As described in detail elsewhere,10–13 the complement system is a cascade of over 30 plasma proteins, found in the blood and on the surface of cells, that acts to destroy microbial pathogens, as well as remove immune complexes, apoptotic cells and the products of inflammation. The complement system has thus a key role in early pregnancy,14 a time of intense tissue and vascular remodelling.15 In brief, there are three complement pathways: the classical, lectin and alternative pathways.10,16,17 These pathways converge to generate enzymes called C3 convertases, which cleave the third component of the complement system into C3b and C3a. C3b is a major effector molecule of the complement system, and acts by binding to the surface of foreign cells and opsonising the cells for phagocytosis. Factors B, D and properdin initiate the activation of C3b primarily through the alternative pathway initiation complex. The activation product Bb is derived from factor B. C3b can also be triggered from engagement of the classical or lectin pathways, with augmentation through an alternative pathway amplification loop. C3a mainly has anaphylatoxin and chemotactic functions. Elevated circulating levels of Bb and C3a are indicative of the activation of the complement pathway, either systemically or locally. The functions of the complement system are mediated by these and other complement-activation fragments (e.g. C3b, C3d, C5a and C5b-9, the membrane attack complex).
The interrelationship between complement activation and the generation of angiogenesis-related factors in humans is unknown, although a causal link has been suggested in an animal model of pregnancy loss.18 The primary objective of this current study was to determine whether altered levels of complement-activation fragments (Bb, C3a and sC5b-9) and angiogenesis-related factors (PiGF, sFlt-1 and sEng) at 10–15 weeks of gestation contribute to the development of pre-eclampsia, and if these biomarkers are related to one another. The second objective of this project was to explore further whether levels of these biomarkers are different among women with and without obesity, as suggested by our previous study.7 These studies were completed using archived samples from women who participated in the Denver complement study.
Methods
This prospective study (June 2005–June 2008) was approved by the Colorado Multiple Institutional Review Board. Some of the study subjects have been described in previous publications.7,19 Women were recruited from the University of Colorado Hospital prenatal clinics, and two affiliated sites. Women were referred to the study’s research assistant by the prenatal intake nurse. Informed consent was obtained and additional plasma (for complement-activation fragments) and serum (for angiogenic factors) samples were obtained with the routine prenatal tests. Data were gathered on the maternal medical and obstetrical history. The women were followed throughout pregnancy. At or shortly after delivery, outcome data were collected and the gestational age at blood draw at the recruitment visit was verified using results from ultrasound examinations obtained during the pregnancy.
Study exclusions
We excluded records from the complete complement study data set (n = 1287), in the following order: women who were lost to follow-up (n = 49), a repeat delivery during the study period (n = 6), pregnancies complicated by an intrauterine fetal loss (mostly miscarriage, n = 51), multiple gestation (n = 42) or gestational hypertension (n = 49). The reason for excluding the cases of gestational hypertension was to avoid misclassification of the outcome, because of the uncertainty in whether gestational hypertension is a separate entity from pre-eclampsia or a mild version of pre-eclampsia.20 An a priori decision was made to concentrate the analysis on women who had blood taken between 10 and 15 weeks of gestation to: (a) reflect the major time of uteroplacental vascular remodelling,15 and (b) reduce the potential confounding effect of gestational age at blood draw. For this reason, women enrolled at a gestational age of <10 weeks or >15 weeks of gestation (n = 375) were excluded from the analysis. Women with a missing plasma or serum sample (because of a deviation from the study protocol at the initial blood draw) were also removed from the analysis (n = 51). Following exclusions, 668 women remained in the data set.
Study outcomes
At delivery, outcome data were collected by the perinatal database staff and entered into the complement study data set. A secondary review of each completed maternal record was conducted by one investigator (AML) before the participant’s sample was assayed. A random selection of the records of women with pre-eclampsia was also reviewed by a single Maternal–Fetal Medicine specialist (blinded to the results of the assay), to verify the classification of the outcome. Outcomes of women who delivered outside of the University of Colorado Hospital (UCH) (n = 387) were obtained from a detailed questionnaire, completed within 2 weeks of the estimated date of delivery (by phone interview or by mail), and by review of the medical records, with the participant’s consent. The main outcome of the study was pre-eclampsia classically defined as gestational hypertension and proteinuria. Gestational hypertension was defined as a systolic blood pressure of >140 mmHg, or a diastolic blood pressure of >90 mmHg, on at least two occasions at least 6 hours apart after 20 weeks of gestation, in women known to be normotensive before pregnancy, and before 20 weeks of gestation. Pre-eclampsia was defined as: (i) gestational hypertension with proteinuria (300 mg + per 24-hour period, or at least 1 + on the dipstick), or (ii) in the absence of proteinuria gestational hypertension with cerebral symptoms, epigastric or right upper quadrant pain, with nausea or vomiting, or thrombocytopenia and abnormal liver function tests.21 Preeclampsia was classified in subjects without knowledge of the levels of biomarker-related exposure. IUGR was defined as a birth percentile of less than the tenth percentile, using the Colorado Intrauterine Growth Charts.22
Primary and secondary exposures
Complement activation fragments (Bb, C3a and sC5b-9) and angiogenesis-related factors (sFlt-1, PiGF and sEng) were the primary exposures examined. Maternal risk factors were: age (over 35 versus <35 years), race/ethnicity (Non-hispanic white, Hispanic White, African American, Asian and other), cigarette smoking at conception (yes versus no) and gestational age at blood draw. A maternal history of medical disease (yes versus no) was a composite of pre-existing maternal hypertension, type-1 diabetes or systemic lupus erythematosus. Maternal prepregnant body mass index (BMI) (kg/m2) was examined as a dichotomous (obese versus non-obese) variable. Obesity was defined as a BMI ≥ 30 kg/m2.
Complement and angiogenic-factor assays
Each plasma sample was processed within an average time of 11 minutes from phlebotomy, and aliquots were placed in a freezer at −80°C. At the time of the assay an aliquot of plasma was thawed. The complement activation fragments Bb and sC5b-9 were measured using a quantitative sandwich enzyme-linked immunosorbent assay (ELISA) (Quidel, San Diego, CA, USA). The kit numbers for the Quidel Bb and sC5b-9 kits were A007 and A020, respectively. The Pharmingen OptEIATM ELISA was used to measure C3a. The interassay coefficients of variation were as follows: Bb (Quidel) = 5.4%, C3a (OptEIA) = 12.1% and sC5b-9 (Quidel) = 6.9%. The intra-assay coefficients of variation were: Bb (Quidel) = 3.9%, C3a (OptEIA) = 5.5% and sC5b-9 (Quidel) = 12.1%. The assays for sFlt-1, PiGF and endoglin were performed from a thawed serum sample using commercial ELISA kits from R&D Systems (Minneapolis, MN, USA) according to the manufacturer’s instructions. Assays for the three markers employed a similar quantitative sandwich enzyme immunoassay technique. The inter-assay coefficients of variation for sFlt-1, PiGF and endoglin in our laboratory were 9.9%, 6.7% and 7.2%, respectively. All samples were run in duplicate. The individuals performing all study assays were blinded to the participant’s pregnancy outcome.
Statistical analysis
The data were analysed in SAS 9.2 (SAS Institute, Cary, NC, USA). Univariable analysis was used to generate descriptive statistics for the cohort. Measures of the complement activation fragments and angiogenic factors were examined as continuous variables. Associations for categorical variables were tested using the chi-square or Fisher’s exact test (P < 0.05). Differences in means of continuous variables were tested using the Wilcoxon rank-sum test. Means for continuous variables are reported in the tables, but non-parametric methods were performed to test for differences in association. Multivariable logistic regression analysis was used to determine the odds ratio of the biomarkers for pre-eclampsia adjusted for other covariates (see above). The adjusted odds ratios (AORs) were calculated for every 1-SD change in levels of the biomarker. Correlations between the biomarkers were tested using correlation analysis and scatter plots with the non-parametric Spearman correlation coefficient, as a measure of association.
Results
Thirty-one (4.65%) women developed pre-eclampsia. Ten women had a preterm (<37 weeks of gestation) onset of preeclampsia, and three women had pre-eclampsia in association with IUGR. Eighty-three (12.4%) women were categorised as obese by pre-pregnancy BMI. The general characteristics of this cohort are shown in Table 1 (column 1).
Table 1.
Distribution of complement-activation fragments, angiogenesis-related factors* and other maternal risk factors in the cohort, and among women with and without pre-eclampsia later in pregnancy
| Cohort (n = 668) | Pre-eclampsia | P**** | ||
|---|---|---|---|---|
| Yes (n = 31) | No (n = 637) | |||
| Bb** (µg/ml) | 0.70 ± 0.2 | 0.84 ± 0.26 | 0.69 ± 0.2 | 0.001 |
| C3a** (ng/L) | 746 ± 473 | 813 ± 437 | 742 ± 474 | 0.2 |
| sC5b-9** (ng/ml) | 228 ± 134 | 234 ± 235 | 227 ± 127 | 0.2 |
| PiGF** (pg/ml) | 39 ± 32 | 31 ± 12 | 39 ± 32 | 0.01 |
| sFlt-1** (pg/ml) | 1316 ± 527 | 1374 ± 639 | 1313 ± 521 | 0.5 |
| sEng** (ng/ml) | 7.3 ± 2.2 | 7.5 ± 2.4 | 7.3 ± 2 | 0.9 |
| Maternal age ≥ 35 years | 312 (47) | 14 (45) | 298 (47) | 0.9 |
| Nulliparity | 274 (41) | 19 (61) | 255 (40) | 0.02 |
| Maternal race | ||||
| Non-hispanic white | 443 (66) | 15 (48) | 428 (67) | 0.13 |
| Hispanic white | 157 (24) | 12 (39) | 145 (23) | |
| African American | 33 (5) | 2 (6.5) | 31 (4.9) | |
| Asian or other | 35 (5.2) | 2 (6.5) | 33 (5.2) | |
| BMI ≥ 30 (obese) | 83 (12.4) | 10 (32) | 73 (11) | 0.0006 |
| Cigarette smoking at conception | 36 (5.4) | 4 (13) | 32 (5) | 0.06 |
| Pre-existing maternal medical disease*** | 23 (3.4) | 7 (23) | 16 (2.5) | <0.0001 |
| Gestational age blood draw (weeks) | 12 ± 1 | 12 ± 1 | 12 ± 1 | 0.8 |
Values shown are n (%) except where otherwise stated.
PiGF, placental growth factor; sFlt-1, soluble fms-like tyrosine kinase-1; sEng, soluble endoglin.
Blood drawn between 10 and 15 weeks of gestation.
Mean levels ± SD.
Chronic hypertension, diabetes and autoimmune disease.
By Wilcoxon’s two-sample test. Means for continuous variables are reported in the tables, but non-parametric methods were performed to test for differences in association.
The association of complement-activation fragments, angiogenesis-related factors and other maternal risk factors with pre-eclampsia is also shown in Table 1. In samples obtained between 10 and 15 weeks of gestation, women who developed pre-eclampsia later in pregnancy had significantly higher levels of complement Bb and lower levels of PiGF, as compared with women who did not develop pre-eclampsia. There was no significant difference in the levels of C3a, sC5b-9, sFlt-1 and sEng among women who developed pre-eclampsia compared with women who remained normotensive during pregnancy. In the multivariable logistic regression analysis the AORs of these covariates were calculated for every 1-SD change in levels of the biomarkers. The AORs for Bb and PiGF were 2.1 (CI = 1.4–3.1, P < 0.0003) and 0.2 (CI = 0.07–0.7, P = 0.01), respectively.
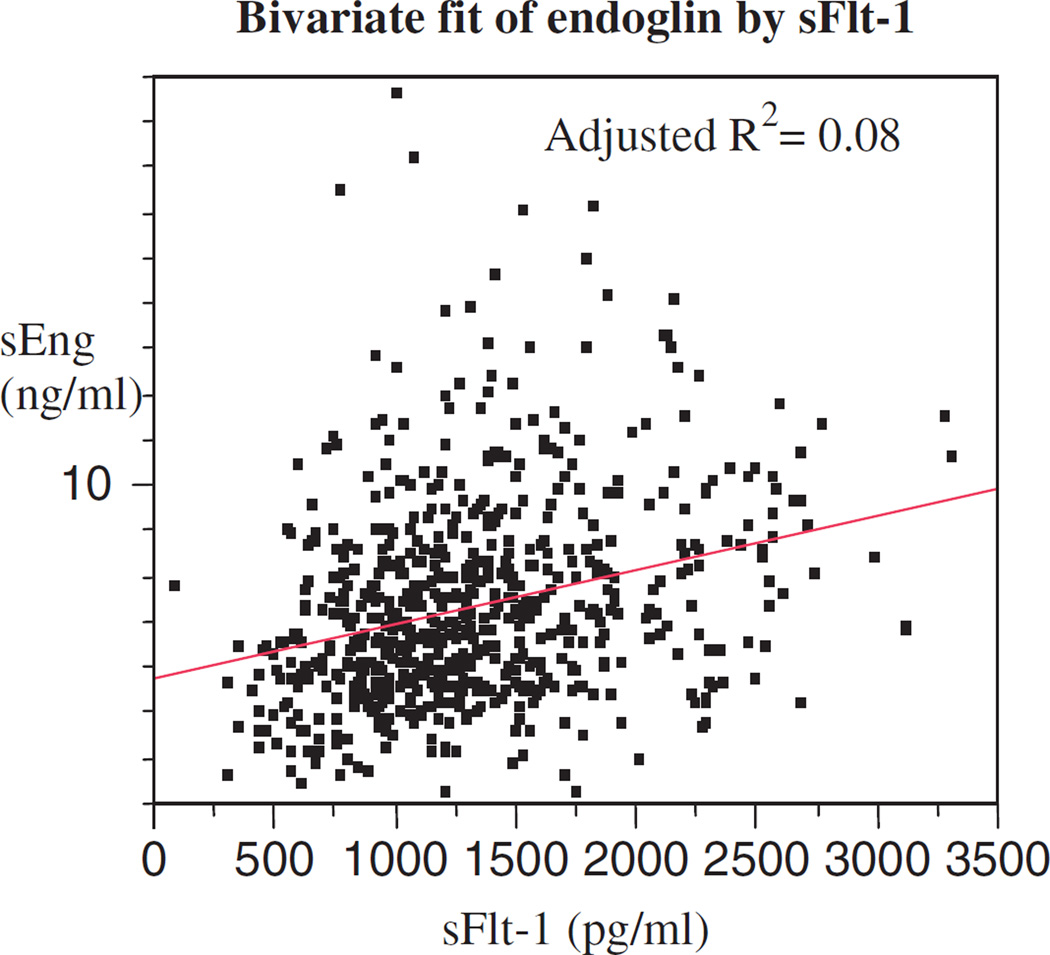
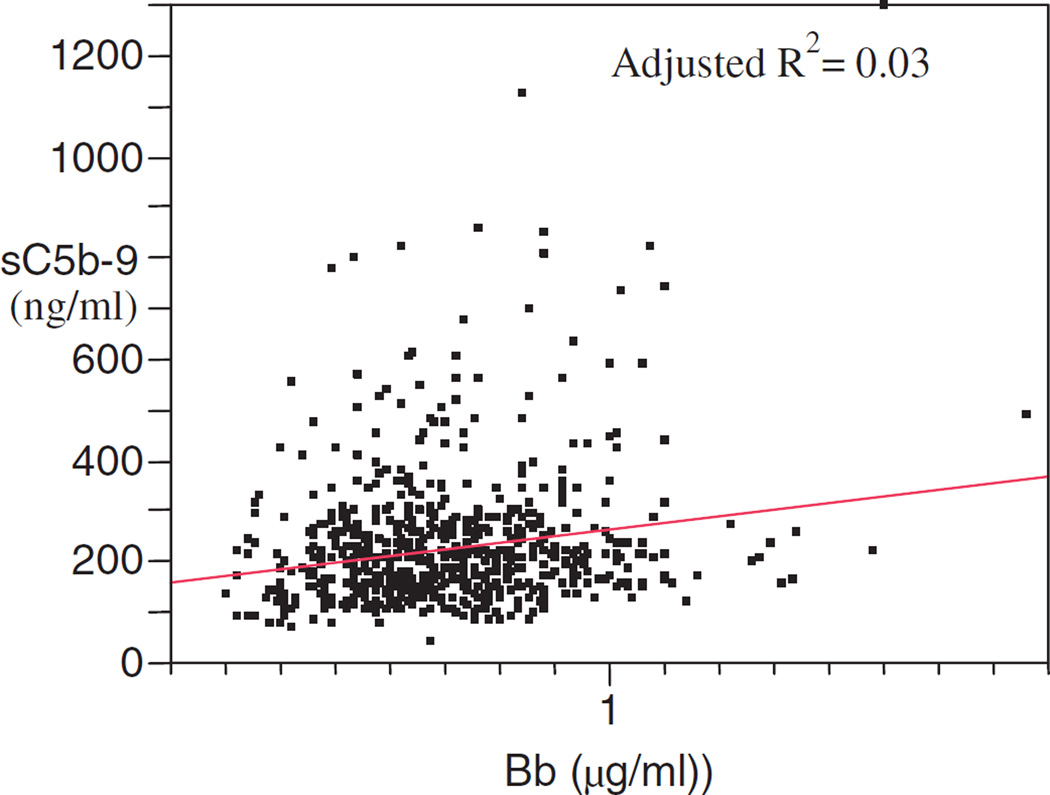
The correlations between the paired complement activation fragments and angiogenic factors were examined as continuous variables, and are shown in Table 2. Although several were significant at the 0.05 level, the highest Spearman’s rank correlation coefficient was only 0.3 for the correlation of sFlt-1 with sEng (Figure 1). Among the complement-activation fragments, the highest correlation was between Bb and sC5b-9 (Figure 2; Table 2).
Table 2.
Nonparametric Spearman correlation coefficients for the relationship between complement-activation fragments and angiogenesis-related factors
| Variable | By variable | Spearman | P |
|---|---|---|---|
| sEng | C3a | −0.0189 | 0.6257 |
| PiGF | C3a | −0.0224 | 0.5628 |
| PiGF | sEng | −0.0169 | 0.6627 |
| sC5b-9 | C3a | −0.0465 | 0.2296 |
| sC5b-9 | sEng | 0.1095 | 0.0046 |
| sC5b-9 | PiGF | 0.0688 | 0.0758 |
| sFlt-1 | C3a | −0.0164 | 0.6719 |
| sFlt-1 | sEng | 0.3051 | <0.0001 |
| sFlt-1 | PiGF | 0.1747 | <0.0001 |
| sFlt-1 | sC5b-9 | 0.1075 | 0.0054 |
| Bb | C3a | 0.0892 | 0.0212 |
| Bb | sEng | 0.0822 | 0.0336 |
| Bb | sC5b-9 | 0.1516 | <0.0001 |
| Bb | sFlt-1 | 0.0248 | 0.5215 |
Figure 1.
Bivariate fit of endoglin by sFlt-1.
Figure 2.
Bivariate fit of sC5b-9 by Bb.
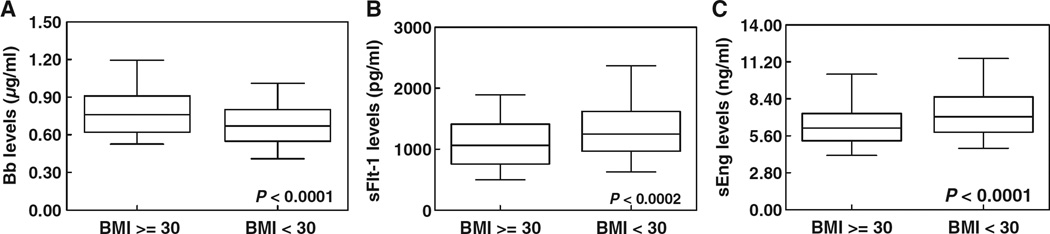
The significantly higher levels of Bb in obese compared with non-obese women are shown in Figure 3A. Women who were obese also had significantly higher levels of C3a (P < 0.03). There was no significant difference in the levels of sC5b-9 between obese and non-obese women. Significantly lower levels of the anti-angiogenic factors sFlt-1 (P < 0.0002; Figure 3B) and sEng (P < 0.0001; Figure 3C) were found in obese women compared with non-obese women. There was no significant difference in the levels of PiGF between the cases and controls. This relationship remained significant when the analysis was restricted to normotensive controls for Bb (P = 0.0005), sFlt-1 (P = 0.002) and sEng (P = 0.0003), and became non-significant for C3a.
Figure 3.
Distribution of Bb (A), sFlt-1 (B) and sEng (C) among obese (n = 85) and non-obese (n = 585) women. Upper and lower ends of the boxes are the 75th and 25th percentiles, respectively. The difference between the upper and lower lines is the interquartile range. The lines across the middles of the boxes are the medians. The upper and lower lines extending from the box are ±1.5*(interquartile range).
Discussion and conclusion
We have found that the complement-activation fragment Bb in maternal plasma at 10–15 weeks of gestation is a significant risk factor for pre-eclampsia, following adjustment for the effects of angiogenesis-related factors, other complement-activation fragments and maternal characteristics, including obesity. Using continuous data at this gestational age range the correlations and the scatterplots between the complement-activation fragments and the angiogenesis-related factors indicate that although there are some significant correlations they are not very strong, and are driven more by the size of the sample than by the consistency of a linear pattern in the data (Table 2). These data do provide evidence of a relationship between angiogenic and complement factors, but more study is needed to determine the effect of this preliminary relationship on clinical outcomes.
In agreement with the existing literature on early pregnancy,23–27 we found that low levels of PiGF at 10–15 weeks of gestation predict the subsequent development of pre-eclampsia. However, we found no significant link between sFlt-1 or sEng and pre-eclampsia during this gestational period, in keeping with the results from other authors.3,23–25,28 It would appear that women who develop pre-eclampsia begin to show higher levels of sFlt-1 and sEng only well into the second trimester of pregnancy.2,3,28 In contrast, elevations of Bb occur much earlier.
Our data relating to women that were obese at the start of their pregnancy were especially informative. Obese pregnant women in our study had an elevated risk of pre-eclampsia (Table 1), and their levels of Bb were higher than the levels of non-obese women (Figure 3A), confirming our earlier findings.7 Our results are in agreement with the findings of other authors who have shown that the placenta develops an exaggerated inflammatory response because of obesity. This is characterised by the accumulation of macrophages and the increased expression of pro-inflammatory cytokines.29 The link between the complement system and obesity has been suggested by other researchers, who have shown that adipose tissue is a major source of factor D (adipsin) and other components of the alternative pathway of complement activation (C3, factor B and C3a).30 Furthermore, Zhang et al.31 have shown that expression of components of the complement pathways are dysregulated in obesity and insulin resistance in vivo in several rodent models of obesity, as well as in studies of human insulin resistance. There are also historic links between the activation of the alternative complement pathway by C3 nephritic factor and lipodystrophy.32–34 Bb may be a potential biomarker of an obesity-related chronic inflammatory response.
Significantly lower levels of the anti-angiogenic factors sFlt-1 and sEng were found in obese pregnant women compared with non-obese controls (Figures 3B,C). We do not have an explanation for this interaction. Other authors have described similar interactions of anti-angiogenic factors with other maternal risk factors.35 Expansion of the vascular bed in adipose tissue in obese women may contribute to an imbalance of angiogenesis-related factors. Suwaki et al.36 reported that among 27 women with pre-eclampsia, sFlt-1 levels were significantly lower in the overweight group compared with the normal weight group. However, in contrast to the results of our study, there was no significant difference in the levels of sFlt-1 in obese and non-obese subjects in their normotensive control group. This may reflect different characteristics of the study groups, and also a larger number of controls in our study. Our results suggest an imbalance of angiogenesis-related factors, driven by levels of maternal BMI.
This prospective study was characterised by the careful collection of maternal risk factors, pregnancy outcomes, low attrition (3.8%), and the meticulous collection and handling of samples. The chief limitation of the study was the relatively small number of women with pre-eclampsia. The low number of events leads to questions about the overall stability of the multivariable logistic regression model, which should be assessed in future larger studies. This also restricted our ability to analyse preterm, severe and mild preeclampsia, and the risk of the biomarkers for pre-eclampsia across strata of BMI, and it may have affected our ability to find an association between complement and angiogenic factors. However, it may also be true that these two groups of markers influence outcomes by two entirely different mechanisms, and are indeed unrelated. The other limitation is the limited time period from which samples were taken during pregnancy. We also acknowledge that there was considerable overlap in the Bb and PiGF concentrations between subjects with and without pre-eclampsia, and in the Bb, sFlt-1 and sEng concentrations in obese and non-obese women. At this stage it appears that complement Bb is not yet a clinically useful marker7,19,37 for pre-eclampsia. However, in proposed larger longitudinal studies we hope to see if the results of this study can be replicated, and if the clinical utility of the test improves with data from the second half of pregnancy, either alone or in combination with other biomarkers or maternal risk factors. In spite of the limitations of this study, we conclude that the innate immune system is triggered in early pregnancy to activate complement factors, and that this activation contributes to the syndrome of pre-eclampsia. Mechanistically, we have shown that inflammation in early pregnancy is a significant risk factor for pre-eclampsia, perhaps independently of angiogenesis-related factors.
Acknowledgments
We thank the women who participated in the Denver complement study, the administrative, medical and nursing staff at the University of Colorado Hospital, Platte River and Metro Community Practice Network clinics, the professional research assistants (Trisha VanHecke, Leslie Meyers, Mariana Villarreal, Jocelyn Phipers, Sarah Crowley and Janice Scott) associated with the study, Joseph Piccoli for programming help, Cynthia Marschner for coordination of the complement assays, Mark Parish for performing the angiogenic assays, Dr Virginia Winn for reviewing cases of pre-eclampsia and Dr Henry Galan for facilitating the use of the perinatal database.
Funding
This research was supported by grants to AML from the American Heart Association (0865481G), the Center for Women’s Health Research and the List Family Foundation, University of Colorado Denver, and the NICHD (K23 HD049684). VMH is supported by NIH R01 AI 55007 and JES is supported by NIH R01 AR49772. RJL is supported by the intramural research programme of the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Footnotes
Disclosure of interests
The authors have nothing to disclose.
Contribution to authorship
AML designed and oversaw the study, conducted the data analysis, obtained the funding and wrote the manuscript; JRM provided statistical consultation; PCG provided consultation on the interpretation of complement results; RJL contributed his expertise in the area of angiogenesis-related factors; RSG contributed his expertise in maternal–fetal medicine. VMH and JES contributed their expertise in the area of complement research, and VMH served as mentor to AML on her NICHD K23 grant.
Details of ethics approval
The Colorado Multiple Institutional Review Board approved the study (COMIRB protocol number 07-0960).
References
- 1.Ilekis JV, Reddy UM, Roberts JM. Preeclampsia – a pressing problem: an executive summary of a National Institute of Child Health and Human Development workshop. Reprod Sci. 2007;14:508–523. doi: 10.1177/1933719107306232. [DOI] [PubMed] [Google Scholar]
- 2.Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, et al. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med. 2004;350:672–683. doi: 10.1056/NEJMoa031884. [DOI] [PubMed] [Google Scholar]
- 3.Levine RJ, Lam C, Qian C, Yu KF, Maynard SE, Sachs BP, et al. Soluble endoglin and other circulating antiangiogenic factors in preeclampsia. N Engl J Med. 2006;355:992–1005. doi: 10.1056/NEJMoa055352. [DOI] [PubMed] [Google Scholar]
- 4.Maynard S, Epstein FH, Karumanchi SA. Preeclampsia and angiogenic imbalance. Annu Rev Med. 2008;59:61–78. doi: 10.1146/annurev.med.59.110106.214058. [DOI] [PubMed] [Google Scholar]
- 5.Dekker G, Robillard PY. Pre-eclampsia: is the immune maladaptation hypothesis still standing? An epidemiological update. J Reprod Immunol. 2007;76:8–16. doi: 10.1016/j.jri.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 6.Parham P. NK cells and trophoblasts: partners in pregnancy. J Exp Med. 2004;200:951–955. doi: 10.1084/jem.20041783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lynch AM, Murphy JR, Byers T, Gibbs RS, Neville MC, Giclas PC, et al. Alternative complement pathway activation fragment Bb in early pregnancy as a predictor of preeclampsia. Am J Obstet Gynecol. 2008;198:3851–3859. doi: 10.1016/j.ajog.2007.10.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holers VM, Girardi G, Mo L, Guthridge JM, Molina H, Pierangeli SS, et al. Complement C3 activation is required for antiphospholipid antibody-induced fetal loss. J Exp Med. 2002;195:211–220. doi: 10.1084/jem.200116116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salmon JE, Girardi G, Holers VM. Complement activation as a mediator of antiphospholipid antibody induced pregnancy loss and thrombosis. Ann Rheum Dis. 2002;61:ii46–ii50. doi: 10.1136/ard.61.suppl_2.ii46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holers VM, Thurman JM. The alternative pathway of complement in disease: opportunities for therapeutic targeting. Mol Immunol. 2004;41:147–152. doi: 10.1016/j.molimm.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 11.Markiewski MM, Lambris JD. The role of complement in inflammatory diseases from behind the scenes into the spotlight. Am J Pathol. 2007;171:715–727. doi: 10.2353/ajpath.2007.070166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walport MJ. Complement. First of two parts. N Engl J Med. 2001;344:1058–1066. doi: 10.1056/NEJM200104053441406. [DOI] [PubMed] [Google Scholar]
- 13.Walport MJ. Complement. Second of two parts. N Engl J Med. 2001;344:1140–1144. doi: 10.1056/NEJM200104123441506. [DOI] [PubMed] [Google Scholar]
- 14.Morgan BP, Holmes CH. Immunology of reproduction: protecting the placenta. Curr Biol. 2000;10:R381–R383. doi: 10.1016/s0960-9822(00)00476-0. [DOI] [PubMed] [Google Scholar]
- 15.Pijnenborg R, Vercruysse L, Hanssens M. Fetal–maternal conflict, trophoblast invasion, preeclampsia, and the red queen. Hypertens Pregnancy. 2008;27:183–196. doi: 10.1080/10641950701826711. [DOI] [PubMed] [Google Scholar]
- 16.Holers VM. The spectrum of complement alternative pathway- mediated diseases. Immunol Rev. 2008;223:300–316. doi: 10.1111/j.1600-065X.2008.00641.x. [DOI] [PubMed] [Google Scholar]
- 17.Sjoberg AP, Trouw LA, Blom AM. Complement activation and inhibition: a delicate balance. Trends Immunol. 2009;30:83–90. doi: 10.1016/j.it.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 18.Girardi G, Yarilin D, Thurman JM, Holers VM, Salmon JE. Complement activation induces dysregulation of angiogenic factors and causes fetal rejection and growth restriction. J Exp Med. 2006;203:2165–2175. doi: 10.1084/jem.20061022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lynch AM, Gibbs RS, Murphy JR, Byers T, Neville MC, Giclas PC, et al. Complement activation fragment Bb in early pregnancy and spontaneous preterm birth. Am J Obstet Gynecol. 2008;199:354e1–354e8. doi: 10.1016/j.ajog.2008.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Villar J, Carroli G, Wojdyla D, Abalos E, Giordano D, Ba’aqeel H, et al. Preeclampsia, gestational hypertension and intrauterine growth restriction, related or independent conditions? Am J Obstet Gynecol. 2006;194:921–931. doi: 10.1016/j.ajog.2005.10.813. [DOI] [PubMed] [Google Scholar]
- 21.Sibai B, Dekker G, Kupferminc M. Pre-eclampsia. Lancet. 2005;365:785–799. doi: 10.1016/S0140-6736(05)17987-2. [DOI] [PubMed] [Google Scholar]
- 22.Lubchenco LO, Hansman C, Boyd E. Intrauterine growth in length and head circumference as estimated from live births at gestational ages from 26 to 42 weeks. Pediatrics. 1966;37:403–408. [PubMed] [Google Scholar]
- 23.Smith GC, Crossley JA, Aitken DA, Jenkins N, Lyall F, Cameron AD, et al. Circulating angiogenic factors in early pregnancy and the risk of preeclampsia, intrauterine growth restriction, spontaneous preterm birth, and stillbirth. Obstet Gynecol. 2007;109:1316–1324. doi: 10.1097/01.AOG.0000265804.09161.0d. [DOI] [PubMed] [Google Scholar]
- 24.Thadhani R, Mutter WP, Wolf M, Levine RJ, Taylor RN, Sukhatme VP, et al. First trimester placental growth factor and soluble fms-like tyrosine kinase 1 and risk for preeclampsia. J Clin Endocrinol Metab. 2004;89:770–775. doi: 10.1210/jc.2003-031244. [DOI] [PubMed] [Google Scholar]
- 25.Romero R, Nien JK, Espinoza J, Todem D, Fu W, Chung H, et al. A longitudinal study of angiogenic (placental growth factor) and anti-angiogenic (soluble endoglin and soluble vascular endothelial growth factor receptor-1) factors in normal pregnancy and patients destined to develop preeclampsia and deliver a small for gestational age neonate. J Matern Fetal Neonatal Med. 2008;21:9–23. doi: 10.1080/14767050701830480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Taylor RN, Grimwood J, Taylor RS, McMaster MT, Fisher SJ, North RA. Longitudinal serum concentrations of placental growth factor: evidence for abnormal placental angiogenesis in pathologic pregnancies. Am J Obstet Gynecol. 2003;188:177–182. doi: 10.1067/mob.2003.111. [DOI] [PubMed] [Google Scholar]
- 27.Tidwell SC, Ho HN, Chiu WH, Torry RJ, Torry DS. Low maternal serum levels of placenta growth factor as an antecedent of clinical preeclampsia. Am J Obstet Gynecol. 2001;184:1267–1272. doi: 10.1067/mob.2001.113129. [DOI] [PubMed] [Google Scholar]
- 28.Rana S, Karumanchi SA, Levine RJ, Venkatesha S, Rauh-Hain JA, Tamez H, et al. Sequential changes in antiangiogenic factors in early pregnancy and risk of developing preeclampsia. Hypertension. 2007;50:137–142. doi: 10.1161/HYPERTENSIONAHA.107.087700. [DOI] [PubMed] [Google Scholar]
- 29.Challier JC, Basu S, Bintein T, Minium J, Hotmire K, Catalano PM, et al. Obesity in pregnancy stimulates macrophage accumulation and inflammation in the placenta. Placenta. 2008;29:274–281. doi: 10.1016/j.placenta.2007.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Choy LN, Rosen BS, Spiegelman BM. Adipsin and an endogenous pathway of complement from adipose cells. J Biol Chem. 1992;267:12736–12741. [PubMed] [Google Scholar]
- 31.Zhang J, Wright W, Bernlohr DA, Cushman SW, Chen X. Alterations of the classic pathway of complement in adipose tissue of obesity and insulin resistance. Am J Physiol Endocrinol Metab. 2007;292:E1433–E1440. doi: 10.1152/ajpendo.00664.2006. [DOI] [PubMed] [Google Scholar]
- 32.Walker UA, Kirschfink M, Peter HH. Improvement of acquired partial lipodystrophy with rosiglitazone despite ongoing complement activation. Rheumatology (Oxford) 2003;42:393–394. doi: 10.1093/rheumatology/keg076. [DOI] [PubMed] [Google Scholar]
- 33.Pattrick M, Luckett J, Yue L, Stover C. Dual role of complement in adipose tissue. Mol Immunol. 2009;46:755–760. doi: 10.1016/j.molimm.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 34.Savage DB, Semple RK, Clatworthy MR, Lyons PA, Morgan BP, Cochran EK, et al. Complement abnormalities in acquired lipodystrophy revisited. J Clin Endocrinol Metab. 2009;94:10–16. doi: 10.1210/jc.2008-1703. [DOI] [PubMed] [Google Scholar]
- 35.Jeyabalan A, Powers RW, Durica AR, Harger GF, Roberts JM, Ness RB. Cigarette smoke exposure and angiogenic factors in pregnancy and preeclampsia. Am J Hypertens. 2008;21:943–947. doi: 10.1038/ajh.2008.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Suwaki N, Masuyama H, Nakatsukasa H, Masumoto A, Sumida Y, Takamoto N, et al. Hypoadiponectinemia and circulating angiogenic factors in overweight patients complicated with pre-eclampsia. Am J Obstet Gynecol. 2006;195:1687–1692. doi: 10.1016/j.ajog.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 37.Silver RM. Immune activation early in pregnancy: trouble down the road? Am J Obstet Gynecol. 2008;199:327–328. doi: 10.1016/j.ajog.2008.06.053. [DOI] [PubMed] [Google Scholar]