Abstract
To determine the efficacy and safety of Trabectome surgery on patients with steroid response, ranging from ocular hypertension refractory to maximal medical therapy to the development of steroid-induced glaucoma.
A nonrandomized, nonblinded, retrospective study of 20 subjects with steroid response was conducted. All 20 eyes underwent Trabectome surgery alone. Nine subjects had steroid response with unremarkable visual field, 3 had mild steroid-induced glaucoma, and 8 had advanced steroid-induced glaucoma. Outcome measures included intraocular pressure (IOP), number of glaucoma medications, need for secondary glaucoma surgery, and steroid regimen. Mann–Whitney U test was used to compare postoperative IOP and number of medications to preoperative IOP and number of medications. Kaplan–Meier was used for survival analysis, and success was defined as: IOP reduced by 20% or more on any 2 consecutive visits after 3 months; IOP ≤21 mm Hg on any 2 consecutive visits after 3 months; and no secondary glaucoma surgery.
The average preoperative IOP was 33.8 ± 6.9 mm Hg and average preoperative glaucoma medication usage was 3.85 ± 0.75 medications. At 12 months, the IOP was reduced to 15.00 ± 3.46 mm Hg (P = 0.03) and glaucoma medication was reduced to 2.3 ± 1.4 (P < 0.01). The survival rate at 12 months was 93%. At 12 months, 10 patients were continued on their preoperative steroid treatments, 5 were on tapered steroid treatments, and 5 had ceased steroid treatments entirely. One patient required secondary glaucoma surgery (glaucoma drainage device). No other complications were noted.
The Trabectome procedure is safe and highly effective for steroid-response glaucoma, even in the context of continued steroid treatment.
Keywords: glaucoma, steroid-response ocular hypertension, trabeculotomy ab interno (Trabectome)
1. Introduction
Steroid response is characterized by a secondary ocular hypertension associated with corticosteroid administration, which may result in development of secondary open-angle glaucoma. Thought to be related to decreased aqueous outflow facility at the trabecular meshwork (TM),[1–16] steroid-induced open-angle glaucoma (SIOAG) occurs more often in those who are genetically susceptible[5–7,17–20] or have clinical risk factors.[5,6,16] Reported routes of corticosteroid administration that may induce steroid response include topical eyedrops,[21,22] topical cutaneous ointments, periocular injection, intraocular injection,[23–27] inhalational spray,[5,28,29] intranasal spray,[30] and oral/systemic.[5,23,29,31–35] Standard treatment options include: trabeculectomy, aqueous shunt implantation, and cyclodestructive procedures.[5–6,16]
Trabeculotomy ab interno (Trabectome) is a conjunctiva-sparing glaucoma surgery that enters the anterior chamber via a clear corneal incision and ablates the TM circumferentially to facilitate direct aqueous outflow through Schlemm canal and into the collector channels.[36–41] This procedure has been previously shown to reduce preoperative intraocular pressure (IOP) by 40% in open-angle glaucoma patients.[36] To our knowledge, the authors are the first to evaluate the outcome of primary Trabectome in patients with steroid-response ocular hypertension (SROH) or SIOAG.
2. Materials and methods
2.1. Patients and consent
Institutional Review Board (IRB) and Ethics Committee approval was obtained from the University of California, Irvine, and from Gifu Red Cross Hospital before data analysis. All patients reviewed and signed a detailed informed consent form before participating in the study. Retrospective review of charts from 2008 to 2015 comprised of patient data from 2 sites: 14 eyes of 14 patients from a single-site academic practice at the University of California, Irvine, USA, and 6 eyes of 6 patients from a single-site community practice at Gifu Cross Hospital, Gifu, Japan, for a total of 20 eyes of 20 patients. Surgeries at Irvine were performed by 1 surgeon (SM), and at Gifu were performed by 1 surgeon (MM). Perioperatively, 2% pilocarpine was administered, along with topical antibiotic and topical anesthetic, with surgery being performed under monitored anesthesia care. Postoperatively, patients were prescribed 2% pilocarpine for 6 to 8 weeks as tolerated and loteprednol etabonate 0.5% ophthalmic suspension 4 times a day tapered over 6 to 8 weeks.
All patients had primary surgery Trabectome[36,40,42] (Neomedix Inc, Tustin, CA) alone and all patients had surgery unilaterally. Briefly, via direct gonioscopic view with the patient's head tilted 15 degrees away from the surgeon, the disposable Trabectome handpiece entered a 1.7-mm clear corneal incision and utilized microbipolar electrocautery to ablate a 90 to 120-degree arc of TM under continuous irrigation (to avoid heat-related damage of adjacent tissue) and aspiration (to remove tissue debris) from the same handpiece. A power setting of 0.7 to 0.8 W was used with a peristaltic aspiration rate of up to 10 mL/min. The anterior chamber was maintained intraoperatively with dispersive 2% hydroxypropyl methylcellulose viscoelastic (OcuCoat, Bausch & Lomb, Rochester, NY), continuous irrigation, and placement of 10–0 vicryl suture in all cases at the main wound. Before tying of clear corneal suture, a disposable Simcoe irrigation/aspiration handpiece was used for coaxial removal of any remaining tissue debris or viscoelastic to minimize aqueous outflow resistance.
2.2. Inclusion criteria
Inclusion criteria included subjects with open angles in the nasal quadrant on gonioscopy (Shaffer III–IV), subjects with documented SROH related to corticosteroid administration or SIOAG with documented visual field progression on static automated perimetry, subjects with clear corneas allowing adequate gonioscopic assessment, and subjects with follow-up for at least 12 months after surgery. All patients included underwent Trabectome surgery alone without any other simultaneous procedures.
This study excluded subjects who underwent Trabectome combined with any other procedure, including phacoemulsification, subjects whose visual acuity was less than hand motions, subjects with media opacities that prevented a baseline gonioscopic view, subjects with angle closure or with significant peripheral anterior synechiae, subjects with a history of uveitis, aphakia, or evidence of neovascularization within the anterior segment, and subjects who had an inability to follow-up.
2.3. Outcomes
Outcomes included percent IOP reduction, number of patients who attained IOP of 21 mm Hg or less, and reduction in number of medications needed to control IOP. Postoperative complications, including hyphema greater than expected, were also recorded. Failure was defined as having uncontrolled IOP requiring additional glaucoma surgery, or less than 20% reduction in IOP from preoperative levels, or IOP greater than 21 mm Hg on 2 consecutive visits postoperatively. Kaplan–Meier survival analysis was performed to monitor success and failure rates.
3. Results
Patient preoperative information was recorded as shown in Tables 1 and 2. Mean age was 60.7 years with a standard deviation (SD) of 18.9 and range of 31 to 89 years. Sex was distributed with 12 male and 8 female patients. Race, preoperative Snellen visual acuity, visual field status, cup-to-disc ratio, lens status, Shaffer grade on gonioscopy, and route and duration of corticosteroid administration were recorded. Visual field status was recorded according to Hoddap–Parrish–Anderson criteria, primarily using mean deviation (MD) to classify patients as normal/full, mild (MD no worse than −6.00 dB), moderate (MD ranging from −6.01 to −12.00 dB), and advanced (MD ranging from −12.01 to −20.00 dB). The duration of steroid use before surgery was variable for each patient, and ranged from a minimum of 1 month to a maximum of 8 months.
Table 1.
Patient preoperative profile.
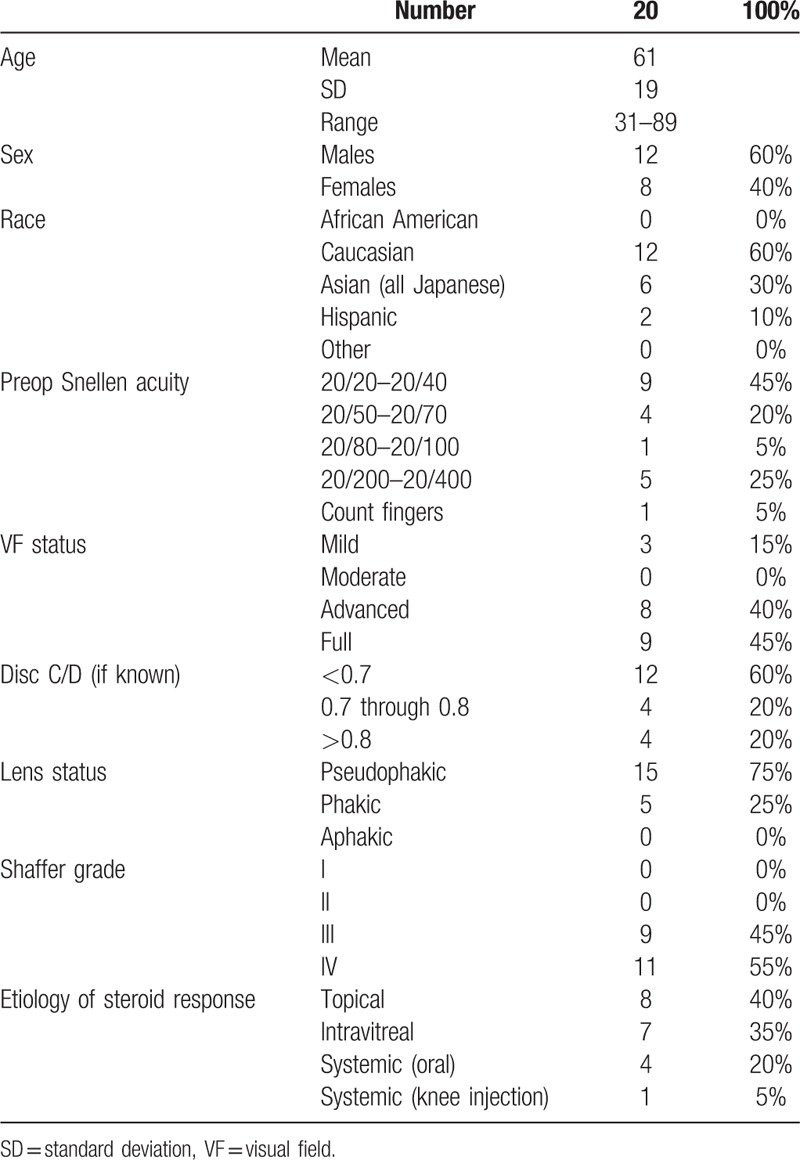
Table 2.
Cases classified by route of corticosteroid administered.
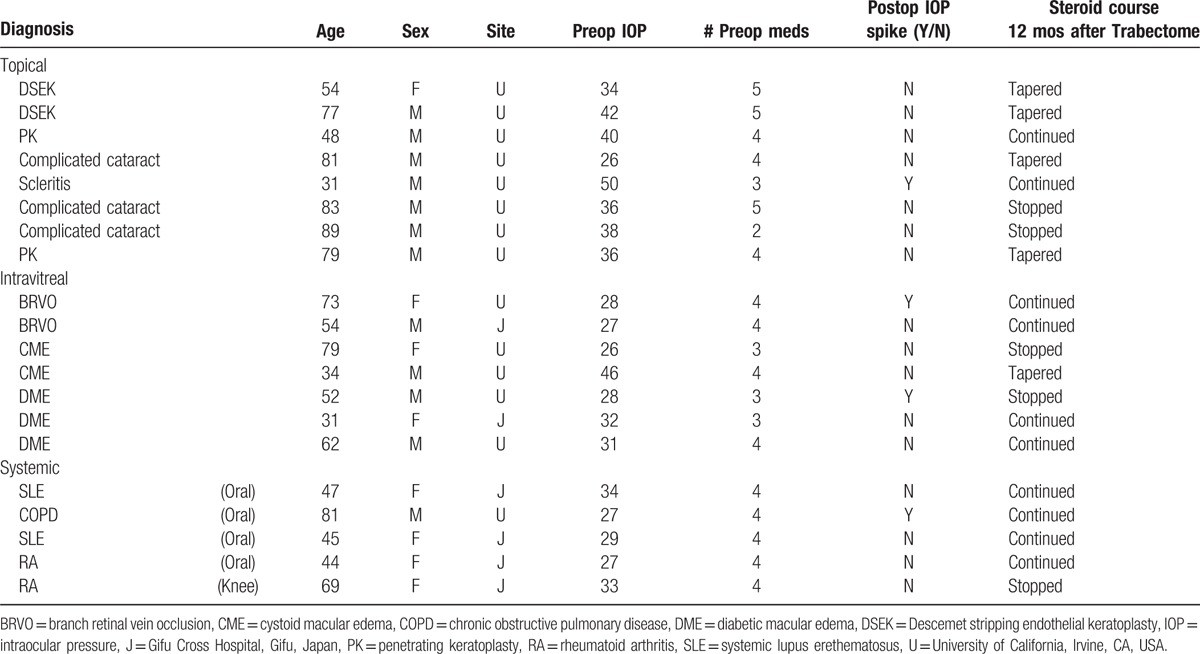
The average preoperative IOP was 33.8 ± 6.9 mm Hg. At 12 months, the IOP was reduced to 15.00 ± 3.46 mm Hg (P = 0.03), with a mean 55.6% reduction in IOP. Figure 1 graphically depicts the trend in IOP. Average preoperative glaucoma medication usage was 3.85 ± 0.75 medications, and at 12 months, the mean number of glaucoma medication was reduced to 2.3 ± 1.4 (P < 0.01), as shown in Fig. 2. At 12 months, 10 patients were continued on their preoperative steroid treatments, 5 were on tapered steroid treatments, and 5 had ceased steroid treatments entirely. visual acuity at postoperative month 3 remained unchanged for 17 patients, improved for 2 patients, and decreased for 1 patient.
Figure 1.
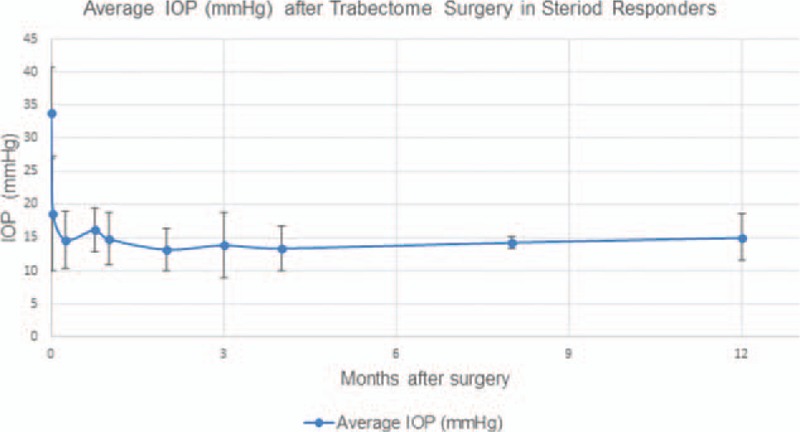
Mean intraocular pressure (IOP) throughout study. A graphical representation of mean IOP from sample size during length of study.
Figure 2.
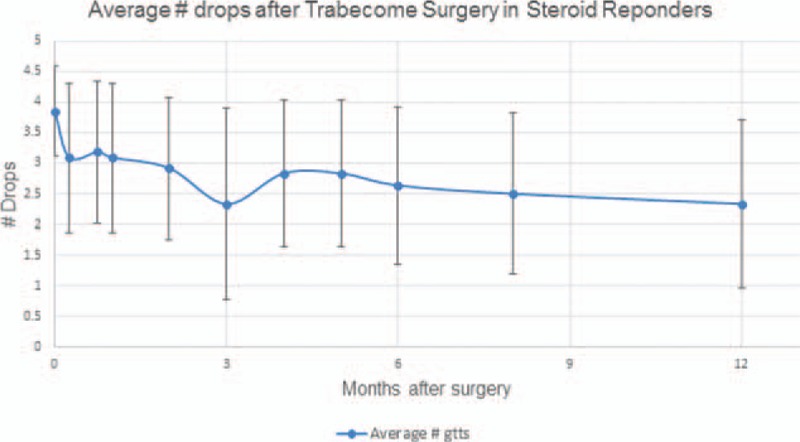
Mean number of medications throughout study. A graphical representation of mean number of medications from sample size during length of study.
In total, 1 patient needed secondary surgery to maintain IOP control. This patient had persistent hyphema with IOP over 35, despite maximal tolerated medical therapy 2 weeks after surgery (mechanism partially due to heme reflux after surgery, and partially due to patient-induced accidental eye trauma that occurred outside of surgery, during the postoperative period) and subsequently underwent implantation of glaucoma drainage device with scleral patch graft. The Kaplan–Meier survival curve for the length of time of the sample size was examined (Fig. 3).
Figure 3.
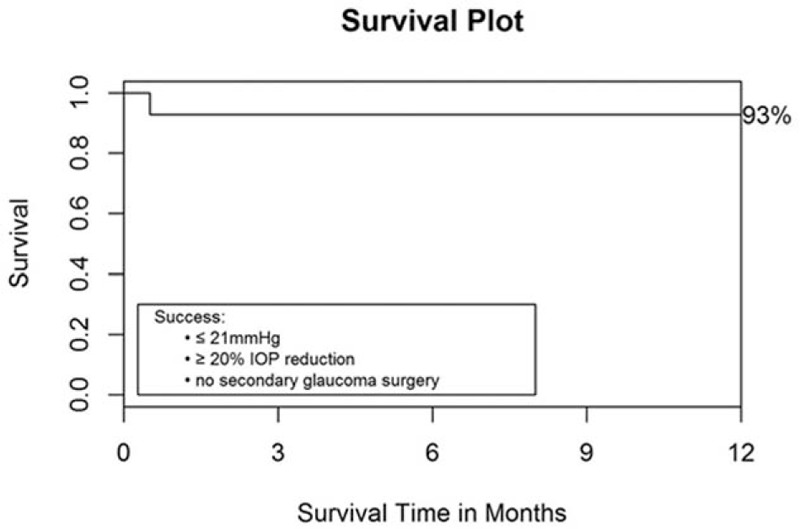
Kaplan–Meier survival curve for 1-year follow-up. Survival analysis plot with time point of failure; legend includes the criteria used to define success in this study.
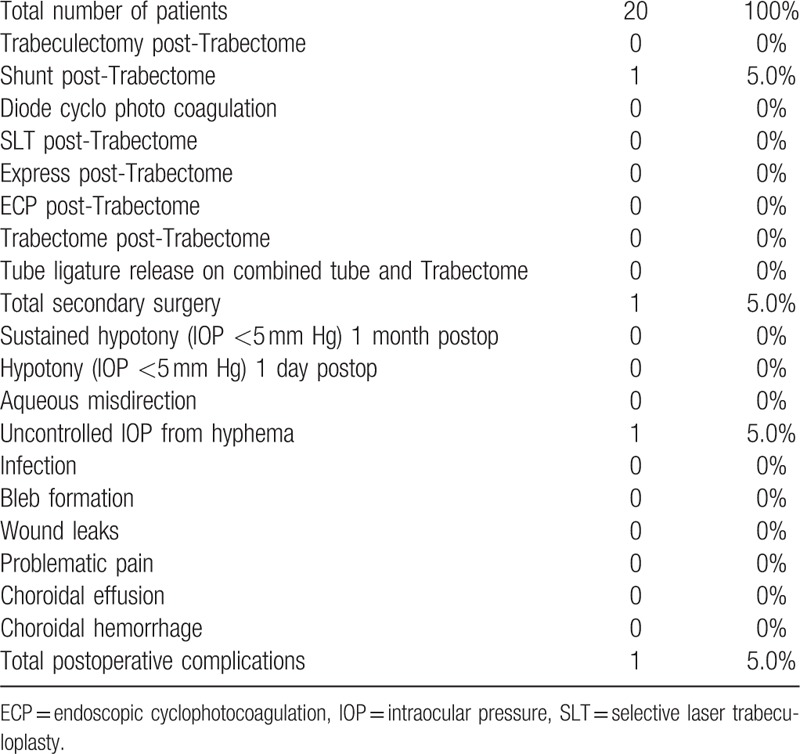
The safety of this procedure, based on postoperative outcomes such as number of patients requiring secondary glaucoma surgery and number of complications are tabulated in Table 3. There were no intraoperative complications in any of the surgeries. Postoperatively, transient IOP spikes occurred in 4 of 20 patients (20%), as shown in Table 2.
Table 3.
Postoperative observations.
4. Discussion
Prior studies have evaluated the outcomes of Trabectome in open-angle glaucoma patients such as primary open-angle glaucoma[36,43–46] and secondary-open angle glaucoma such as pseudoexfoliation.[45–48] However, the utility of the Trabectome in patients with open-angle glaucoma secondary to corticosteroid has not been studied. Thought to occur more commonly in those who are genetically predisposed,[5–7,17–20] elevation in IOP as a response to steroid administration has a complex mechanism that is not fully elucidated. It is thought that once corticosteroid molecules bind to intracellular receptor complexes, alterations in gene expression[7,9,16,20,49] have downstream effects on apoptosis and ultrastructural sites at the TM that ultimately lead to reduced aqueous outflow from increased aqueous resistance, trabeculocyte dysfunction,[50] myocilin protein expression that alters cytoskeleton architecture,[1–6] extracellular matrix (ECM) accumulation at juxtacanalicular tissue that narrows trabecular spaces,[2,10,51] changes in cytokine mileu,[13] changes in enzymatic regulation of TM structure,[52] and impaired phagocytic activity.[10,15] Given that ECM has been demonstrated to have complex interaction on electron microscopy with glycosaminoglycans, hyaluronic acid, collagen, elastin, and glycoproteins in juxtacanalicular tissue of healthy human eyes,[14] the ultrastructural network that results in thickened trabecular beams from glucocorticoid exposure is extremely intricate[10,11] and has been confirmed to be different than that of primary open-angle glaucoma on histology.[11] Steroid-induced changes may also occur at the level of the inner wall of Schlemm canal, specifically at the subendothelial region where fine fibrillar material is deposited.[16] In addition, physical obstruction at the angle by corticosteroid crystal residues has been hypothesized as a contributing mechanism.[24]
With the Trabectome, ablation of the TM conceptually reduces resistance to aqueous outflow by opening a direct pathway for aqueous to flow from the anterior chamber into Schlemm canal and collector channels. Histopathology in autopsy eyes have revealed targeted removal of TM and inner wall of Schlemm canal with preservation of the outer wall of Schlemm canal.[40] By direct elimination of the site of pathology in this particular glaucoma subtype, the authors were interested to see if the Trabectome procedure would effectively normalize IOP while minimizing risk for complications in patients with steroid response.
It has been reported that the amount of IOP elevation response to steroid is directly related to the potency of anti-inflammatory effect, concentration, frequency, and duration, of the steroid administered. With increasing numbers of corneal transplantation and intravitreal injections being performed worldwide, this complication is increasing in frequency, and therefore the development of treatments safer than standard tube shunts or trabeculectomy are essential.
Penetrating keratoplasty (PKP) is 1 such procedure in which prolonged steroids are implemented as part of routine postsurgical care. Postkeratoplasty glaucoma (PKG) is a well-known phenomenon that can occur in up to one-third of patients,[53] and is the second leading cause for graft failure.[54] In 1 study that implemented PKP in treating patients with Fuch and Keratoconus, postoperative steroid-induced IOP elevation was noted to be 60% and 73%, respectively.[55] In Descemet stripping endothelial keratoplasty (DSEK), postoperative IOP elevation was noted in 28% of patients, with steroid-induced IOP elevation as the leading cause, with an incidence as high as 18%.[56] IOP elevation has been noted in steroid injections and implants, with 32% to 51% developing ocular hypertension after 4 mg intravitreal triamcinolone injection,[27,56] and 79% with 2.1 mg fluocinolone implant. In 1s study, up to 45% of fluocinolone implants required surgical intervention to control IOP.[56] Our study, in which 20% of participants examined had steroid response after undergoing corneal transplantation, may suggest that Trabectome is of particular relevance in treating patients with corneal transplantation and steroid response that is refractory to medical management.
Other surgical approaches to treating steroid-induced glaucoma have been studied to a limited degree. Selective laser trabeculoplasty (SLT) was able to achieve lowering of IOP after intravitreal steroid administration; however, in multiple studies, this decrease was gradual, reaching therapeutic levels after 3 to 6 months.[57–59] In some refractory cases, filtration surgery was required to adequately control IOP. Given the risk of delayed IOP-lowering effect, some authors believe that SLT should be reserved for those patients who do not require immediate IOP lowering.[60] In Trabectome, the average IOP at the 1-week postoperative examination was 14.6 ± 4.2 mm Hg, which was maintained for 12 months (Fig. 2).
Trabeculectomy has been a long-standing surgical standard in the treatment of steroid-induced glaucoma.[61] In 1 multicenter Japanese study that examined trabeculectomy in steroid responders, 96% were able to achieve pressures <21 mm Hg at 1 year, with or without ocular hypotensive medications.[61] However, these results come with high complication rates, requiring extensive postoperative care. In the aforementioned study of trabeculectomy on steroid responders, 23.9% had complications with trabeculectomy. Our series of Trabectome, while a smaller study with a multiethnic patient cohort, had a complication rate of 5%. In the trabeculectomy versus tube (TVT) study,[60] trabeculectomy had a complication rate of 37%. Although trabeculectomy may be comparable to Trabectome in terms of its IOP-lowering ability, trabeculectomy is an external filtration surgery that requires a bleb and carries a high risk of early and late complications such as hypotony, shallow chambers, choroidal effusions, blebitis, and endophthalmitis. In contrast, Trabectome is conjunctiva-sparing and has a very low complication rate. This may be of particular importance in certain contexts, for example, in the context of PKP, where performing a trabeculectomy with disruption of the limbal conjunctiva may compromise the success of corneal transplantation,[62] and similarly in the context of trabeculectomy, where performing a PKP may increase the rate of bleb failure.[63]
Another standard surgical treatment for steroid-induced IOP elevation is tube shunt implantation. Extensive short and long-term complications exist for this procedure as well, but most importantly, tube shunts greatly increase the risk of corneal graft failure,[64–67] even when implanted in the ciliary sulcus or pars plana.[68,69]
A dose-dependent effect of corticosteroids on IOP is found to occur more acutely and more often in children than in adults.[16] Moreover, the diagnosis and management of steroid response in children is much more challenging due to limited cooperation in the pediatric age group.[70] With the increased difficulty in management, and also the lifelong burden of tube erosion, corneal decompensation, and endophthalmitis in traditional glaucoma surgery, Trabectome may offer a safer alternative for already challenging cases of uncontrolled SROH in the pediatric population.
5. Limitations and conclusions
The authors acknowledge limitations to the study. The design of this 2-center interventional case series is retrospective with the limitations inherent to these types of studies. Although the study was conducted at 2 sites with 2 patient populations, this fact further supports that Trabectome is a safe and effective procedure across different ethnic demographics as the procedure does not rely on variations in postoperative conjunctival wound healing. This effectiveness across different ethnic populations is also supported by other studies.[71] Additionally, several different disease states and routes of administration were represented in our sample. Future investigations with larger studies represented on these individual causes for steroid-induced glaucoma would help to better identify particular groups that respond better or worse to this intervention.
Trabectome is a safe and highly effective treatment for steroid-response glaucoma targeting the main site of pathology in this condition, resulting in the normalization of IOP, while also minimizing the risks often seen in our current standard glaucoma surgeries. This procedure is particularly appealing in settings where continued long-term administration of steroid is to be expected, such as in corneal transplantation, in which our current glaucoma treatments have been shown to increase the risk of graft failure. Trabectome may also be appealing in cases of pediatric steroid response, in which diagnosis and management are particularly challenging, and traditional glaucoma surgeries are prohibitive as they carry a lifelong potential for complications.
Footnotes
Abbreviations: DSEK = Descemet stripping endothelial keratoplasty, ECM = extracellular matrix, IOP = intraocular pressure, PKG = postkeratoplasty glaucoma, PKP = penetrating keratoplasty, SD = standard deviation, SIOAG = steroid-induced open-angle glaucoma, SLT = selective laser trabeculoplasty, SROH = steroid-response ocular hypertension, TM = trabecular meshwork, Trabectome = trabeculotomy ab interno, TVT = trabeculectomy versus tube.
Funding disclosure: Supported in part by a Department Developmental Grant from Research to Prevent Blindness. The authors have no financial interest or proprietary interest to disclose.
The authors report no conflicts of interest.
References
- [1].Wordinger RJ, Clark AF. Effects of glucocorticoids on the trabecular meshwork: towards a better understanding of glaucoma. Prog Retin Eye Res 1999;18:629–67. [DOI] [PubMed] [Google Scholar]
- [2].Clark AF, Wordinger RJ. The role of steroids in outflow resistance. Exp Eye Res 2009;88:752–9. [DOI] [PubMed] [Google Scholar]
- [3].Kumar S, Shah S, Deutsch ER, et al. Triamcinolone acetonide decreases outflow facility in C57BL/6 mouse eyes. Invest Ophthalmol Vis Sci 2013;54:1280–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Jain A, Liu X, Wordinger RJ, et al. Effects of thailanstatins on glucocorticoid response in trabecular meshwork and steroid-induced glaucoma. Invest Ophthalmol Vis Sci 2013;54:3137–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Razeghinejad MR, Katz LJ. Steroid-induced iatrogenic glaucoma. Ophthalmic Res 2012;47:66–80. [DOI] [PubMed] [Google Scholar]
- [6].Jones R, 3rd, Rhee DJ. Corticosteroid-induced ocular hypertension and glaucoma: a brief review and update of the literature. Curr Opin Ophthalmol 2006;17:163–7. [DOI] [PubMed] [Google Scholar]
- [7].Polansky JR, Fauss DJ, Zimmerman CC. Regulation of TIGR/MYOC gene expression in human trabecular meshwork cells. Eye 2000;14:503–14. [DOI] [PubMed] [Google Scholar]
- [8].Johnson D, Gottanka J, Flugel C, et al. Ultrastructural changes in the trabecular meshwork of human eye streated with corticosteroids. Arch Ophthalmol 1997;115:375–83. [DOI] [PubMed] [Google Scholar]
- [9].Pfeffer BA, DeWitt CA, Salvador-Silva M, et al. Reduced myocilin expression in cultured monkey trabecular meshwork cells induced by a selective glucocorticoid receptor agonist: comparison with steroids. Invest Ophthalmol Vis Sci 2010;51:437–46. [DOI] [PubMed] [Google Scholar]
- [10].Rohen JW, Linner E, Witmer R. Electron microscopic studies on the trabecular meshwork in two cases of corticosteroid-glaucoma. Exp Eye Res 1973;17:19–31. [DOI] [PubMed] [Google Scholar]
- [11].Johnson DH, Bradley JM, Acott TS. The effect of dexamethasone on glycosaminoglycans of human trabecular meshwork in perfusion organ culture. Invest Ophthalmol Vis Sci 1990;31:2568–71. [PubMed] [Google Scholar]
- [12].Steely HT, Bowder SL, Julian MB, et al. The effects of dexamethasone on fibronectin expression in cultured human trabecular meshwork cells. Invest Ophthalmol Vis Sci 1992;33:2242–50. [PubMed] [Google Scholar]
- [13].Hogg P, Calthorpe M, Batterbury M, et al. Aqueous humor stimulates the migration of human trabecular meshwork cells in vitro. Invest Ophthalmol Vis Sci 2000;41:1091–8. [PubMed] [Google Scholar]
- [14].Ueda J, Wentz-Hunter K, Yue BY. Distribution of myocilin and extracellular matrix components in the juxtacanalicular tissue of human eyes. Invest Ophthalmol Vis Sci 2002;43:1068–76. [PubMed] [Google Scholar]
- [15].Bill A. The drainage of aqueous humor. Invest Ophthalmol 1975;14:1–3. [PubMed] [Google Scholar]
- [16].Avraham Cohen (2011). Steroid Induced Glaucoma, Glaucoma - Basic and Clinical Concepts, Dr Shimon Rumelt (Ed.), InTech, DOI: 10.5772/25069. Available from: http://www.intechopen.com/books/glaucoma-basic-and-clinical-concepts/steroidinduced-glaucoma. [Google Scholar]
- [17].Urban RC, Jr, Dreyer EB. Corticosteroid-induced glaucoma. Int Ophthalmol Clin 1993;33:135–9. [DOI] [PubMed] [Google Scholar]
- [18].Mookherjee S, Acharya M, Banerjee D, et al. Molecular basis for involvement of CYP1B1 in MYOC upregulation and its potential implication in glaucoma pathogenesis. PLoS One 2012;7:e45077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Marcus MW, Muskens RP, Ramdas WD, et al. Corticosteroids and open-angle glaucoma in the elderly: a population-based cohort study. Drugs Aging 2012;29:963–70. [DOI] [PubMed] [Google Scholar]
- [20].Zhang X, Clark AF, Yorio T. FK 506-binding protein 51 regulates nuclear transport of the glucocorticoid receptor beta and glucocorticoid responsiveness. Invest Ophthalmol Vis Sci 2008;49:1037–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ozeki N, Yuki I, Shiba D, et al. Intraocular pressure elevation after Descemet's stripping endothelial keratoplasty. Jpn J Ophthalmol 2012;56:307–11. [DOI] [PubMed] [Google Scholar]
- [22].Vajaranant TS, Price MO, Price FW, et al. Visual acuity and intraocular pressure after Descemet's stripping endothelial keratoplasty in eyes with and without pre-existing glaucoma. Ophthalmology 2009. 1644–50. 116. [DOI] [PubMed] [Google Scholar]
- [23].Friedman DS, Holbrook JT, Ansari H, et al. Risk of elevated intraocular pressure and glaucoma in patients with uveitis: results of the multicenter uveitis steroid treatment trial. Ophthalmology 2013;120:1571–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Singh IP, Ahmad SI, Yeh D, et al. Early rapid rise in intraocular pressure after intravitreal triamcinolone acetonide injection. Am J Ophthalmol 2004;138:286–7. [DOI] [PubMed] [Google Scholar]
- [25].Im L, Allingham RR, Singh I, et al. A prospective study of early intraocular pressure changes after a single intravitreal triamcinolone injection. J Glaucoma 2008;17:128–32. [DOI] [PubMed] [Google Scholar]
- [26].Kramar M, Vu L, Whitson JT, et al. The effect of intravitreal triamcinolone on intraocular pressure. Curr Med Res Opin 2007;23:1253–8. [DOI] [PubMed] [Google Scholar]
- [27].Jonas JB, Kreissig I, Degenring R. Intraocular pressure after intravitreal injection of triamcinolone acetonide. Br J Ophthalmol 2003;87:24–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Bui CM, Chen H, Shyr Y, et al. Discontinuing nasal steroids might lower intraocular pressure in glaucoma. J Allergy Clin Immunol 2005;116:1042–7. [DOI] [PubMed] [Google Scholar]
- [29].Mitchell P, Cumming RJ, Mackey DA. Inhaled corticosteroids, family history, and risk of glaucoma. Ophthalmology 1999;106:2301–6. [DOI] [PubMed] [Google Scholar]
- [30].Bergmann J, Witmer MT, Slonim CB. The relationship of intranasal steroids to intraocular pressure. Curr Allergy Asthma Rep 2009;9:311–5. [DOI] [PubMed] [Google Scholar]
- [31].Tripathi RC, Kirschner BS, Kipp M, et al. Corticosteroid treatment for inflammatory bowel disease in pediatric patients increases intraocular pressure. Gastroenterology 1992;102:1957–61. [DOI] [PubMed] [Google Scholar]
- [32].Schwartz B. The response of ocular pressure to corticosteroids. Int Ophthalmol Clin 1966;6:929–89. [DOI] [PubMed] [Google Scholar]
- [33].Lindholm B, Linner E, Tengroth B. Effects of long-term systemic steroids on cataract formation and on aqueous humour dynamics. Acta Ophthalmol 1965;43:120–7. [Google Scholar]
- [34].Mandapati JS, Metta AK. Intraocular pressure variation in patients on long term corticosteroids. Indian Dermatol Online J 2011;2:67–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Ng PC, Lee CH, Tam BS, et al. Transient increase in intraocular pressure during a dose-tapering regime of systemic dexamethasone in pre-term infants. Ophthalmology 2008;115:e7–14. [DOI] [PubMed] [Google Scholar]
- [36].Minckler DS, Baerveldt G, Alfaro MR, et al. Clinical results with the Trabectome for treatment of open-angle glaucoma. Ophthalmology 2005;112:962–7. [DOI] [PubMed] [Google Scholar]
- [37].Mosaed S, Dustin L, Minckler DS. Comparative outcomes between newer and older surgeries for glaucoma. Trans Am Ophthalmol Soc 2009;107:127–35. [PMC free article] [PubMed] [Google Scholar]
- [38].Minckler D, Baerveldt G, Ramirez MA, et al. Clinical results with the Trabectome: a novel surgical device for treatment of open-angle glaucoma. Trans Am Ophthalmol Soc 2006;104:40–50. [PMC free article] [PubMed] [Google Scholar]
- [39].Minckler D, Mosaed S, Dustin L, et al. Trabectome (trabeculectomy-internal approach): additional experience and extended follow-up. Trans Am Ophthalmol Soc 2008;106:149–59. [PMC free article] [PubMed] [Google Scholar]
- [40].Francis BA, See RF, Rao NA, et al. Ab interno trabeculectomy: development of a novel device (Trabectome) and surgery for open-angle glaucoma. J Glaucoma 2006;15:68–73. [DOI] [PubMed] [Google Scholar]
- [41].Minckler DS, Hill RA. Use of novel devices for control of intraocular pressure. Exp Eye Res 2009;88:792–8. [DOI] [PubMed] [Google Scholar]
- [42].Maeda M, Watanabe M, Ichikawa K. Evaluation of Trabectome in open-angle glaucoma. J Glaucoma 2013;22:205–8. [DOI] [PubMed] [Google Scholar]
- [43].Francis BA, Minckler DS, Dustin L, et al. Combined cataract extraction and trabeculotomy by the internal approach for coexisting cataract and open-angle glaucoma: initial results. J Cataract Refract Surg 2008;34:1096–103. [DOI] [PubMed] [Google Scholar]
- [44].Augustinus CJ, Zeyen T. The effect of phacoemulsification and combined phaco/glaucoma procedures on the intraocular pressure in open-angle glaucoma. A review of the literature. Bull Soc Belge Ophthalmol 2012. 51–66. [PubMed] [Google Scholar]
- [45].Jordan JF, Wecker T, van Oterendorp C, et al. Trabectome surgery for primary and secondary open angle glaucomas. Graefes Arch Clin Exp Ophthalmol 2013;251:2753–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Ahuja Y, Ma Khin Pyi S, Malihi M, et al. Clinical results of ab interno trabeculotomy using the Trabectome for open-angle glaucoma: the mayo clinic series in Rochester, Minnesota. Am J Ophthalmol 2013;156:927–35. [DOI] [PubMed] [Google Scholar]
- [47].Ting JL, Damji KF, Stiles MC. Trabectome Study Group Ab interno trabeculectomy: outcomes in exfoliation versus primary open-angle glaucoma. J Cataract Refract Surg 2012;38:315–23. [DOI] [PubMed] [Google Scholar]
- [48].Jea SY, Francis BA, Vakili G, et al. Ab interno trabeculectomy versus trabeculectomy for open-angle glaucoma. Ophthalmology 2012;119:36–42. [DOI] [PubMed] [Google Scholar]
- [49].Clark AF, Steely HT, Dickerson JE, Jr, et al. Glucocorticoid induction of the glaucoma gene MYOC in human and monkey trabecular meshwork cells and tissues. Invest Ophthalmol Vis Sci 2001;42:1769–80. [PubMed] [Google Scholar]
- [50].Kulkarni A, Barton K. Shaarawy TM, Sherwood MB, Crowston JG, Hitchings RA. Uveitic glaucoma. Glaucoma. China:Saunders Ltd; 2009. 393–407. [Google Scholar]
- [51].Snyder RW, Stamer WD, Kramer TR, et al. Corticosteroid treatment and trabecular meshwork proteases in cell and organ culture supernatants. Exp Eye Res 1993;57:461–8. [DOI] [PubMed] [Google Scholar]
- [52].El-Shabrawi Y, Eckhardt M, Berghold A, et al. Synthesis pattern of matrix metalloproteinases (MMPs) and inhibitors (TIMPs) in human explant organ cultures after treatment with latanoprost and dexamethasone. Eye 2000;14:375–83. [DOI] [PubMed] [Google Scholar]
- [53].Ayyala RS. Penetrating keratoplasty and glaucoma. Surv Ophthalmol 2000;45:91–105. [DOI] [PubMed] [Google Scholar]
- [54].Wilson SE, Kaufman HE. Graft failure after penetrating keratoplasty. Surv Ophthalmol 1990;34:325–56. [DOI] [PubMed] [Google Scholar]
- [55].Erdurmus M, Cohen EJ, Yildiz EH, et al. Steroid-induced intraocular pressure elevation or glaucoma after penetrating keratoplasty in patients with keratoconus or Fuchs dystrophy. Cornea 2009;28:759–64. [DOI] [PubMed] [Google Scholar]
- [56].Maier AK, Klamann MK, Torun N, et al. Intraocular pressure elevation and post-DSEK glaucoma after Descemet's stripping endothelial keratoplasty. Graefes Arch Clin Exp Ophthalmol 2013;251:1191–8. [DOI] [PubMed] [Google Scholar]
- [57].Yuki K, Inoue M, Shiba D, et al. Selective laser trabeculoplasty for elevated intraocular pressure following subtenon injection of triamcinolone acetonide. Clin Ophthalmol 2010;26:247–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Rubin B, Taglienti A, Rothman RF, et al. The effect of selective laser trabeculoplasty on intraocular pressure in patients with intravitreal steroid-induced elevated intraocular pressure. J Glaucoma 2008;17:287–92. [DOI] [PubMed] [Google Scholar]
- [59].Tokuda N, Inoue J, Yamazaki I, et al. Department of Ophthalmology, St Marianna University School of Medicine. Japan. Nippon Ganka Gakkai Zasshi 2012;116:751–7. [PubMed] [Google Scholar]
- [60].Gedde SJ, Herndon LW, Brandt JD, et al. Postoperative complications in the Tube Versus Trabeculectomy (TVT) study during five years of follow-up. Am J Ophthalmol 2012;153:804–14. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Iwao K, Inatani M, Tanihara H. Japanese Steroid-Induced Glaucoma Multicenter Study Group. Success rates of trabeculotomy for steroid-induced glaucoma: a comparative, multicenter, retrospective cohort study. Am J Ophthalmol 2011;151:1047–56. e1. [DOI] [PubMed] [Google Scholar]
- [62].Iverson SM, Spierer O, Papachristou GC, et al. Comparison of primary graft survival following penetrating keratoplasty and Descemet's stripping endothelial keratoplasty in eyes with prior trabeculectomy. Br J Ophthalmol 2015;99:1477–82. [DOI] [PubMed] [Google Scholar]
- [63].Ishioka M, Shimazaki J, Yamagami J, et al. Trabeculectomy with mitomycin C for postkeratoplasty glaucoma. Br J Ophthalmol 2000;84:714–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Kwon YH, Greenlee EC. Graft failure: III. Glaucoma escalation after penetrating keratoplasty. Int Ophthalmol 2008;28:191–207. [DOI] [PubMed] [Google Scholar]
- [65].Alvarenga LS, Mannis MJ, Brandt JD, et al. The long-term results of keratoplasty in eyes with a glaucoma drainage device. Am J Ophthalmol 2004;138:200–5. [DOI] [PubMed] [Google Scholar]
- [66].Kwon YH, Taylor JM, Hong S, et al. Long-term results of eyes with penetrating keratoplasty and glaucoma drainage tube implant. Ophthalmology 2001;108:272–8. [DOI] [PubMed] [Google Scholar]
- [67].Rapuano CJ, Schmidt CM, Cohen EJ, et al. Results of alloplastic tube shunt procedures before, during, or after penetrating keratoplasty. Cornea 1995;14:26–32. [PubMed] [Google Scholar]
- [68].Arroyave CP, Scott IU, Fantes FE, et al. Corneal graft survival and intraocular pressure control after penetrating keratoplasty and glaucoma drainage device implantation. Ophthalmology 2001;108:1978–85. [DOI] [PubMed] [Google Scholar]
- [69].Sidoti PA1, Mosny AY, Ritterband DC, et al. Pars plana tube insertion of glaucoma drainage implants and penetrating keratoplasty in patients with coexisting glaucoma and corneal disease. Ophthalmology 2001;108:1050–8. [DOI] [PubMed] [Google Scholar]
- [70].Cingu AK, Cinar Y, Turkcu FM, et al. Evaluation of retinal nerve fiber layer thickness in vernal keratoconjunctivitis patients under long-term topical corticosteroid therapy. Cutan Ocul Toxicol 2014;33:184–8. [DOI] [PubMed] [Google Scholar]
- [71].Lee JW, Yick DW, Tsang S, et al. Efficacy and safety of trabectome surgery in Chinese open-angle glaucoma. Medicine (Baltimore) 2016;95:e3212. [DOI] [PMC free article] [PubMed] [Google Scholar]


