Abstract
Recent observational studies have reported controversial results for the association between different anthropometric indices of obesity and severity of atherosclerosis. The aim of the current study is to determine the associations between anthropometric indices with severity of atherosclerosis in adult population in north of Iran.
The cross-sectional study was performed on 610 participants, who were admitted to a hospital for elective angiographyin Rasht, Iran, Anthropometric indices, including waist circumference (WC), waist-to-height ratio (WHtR), conicity index (CI), body mass index (BMI), and hematological factors, were measured using the standard methods. According to angiography reports, severity of atherosclerosis was determined.
Sixty-two percent of participants had moderate to severe atherosclerosis. According to BMI, 44% were overweight and 25.8% were obese. Based on WHtR and WC, 90%, and 57% were obese, respectively. The prevalence of moderate to severe atherosclerosis in centrally obese women was significantly higher than in centrally nonobese women (52% vs 28% P = 0.02). According to multivariate adjustment analysis, age, sex, systolic blood pressure, hemoglobin A1c, uric acid, and triglyceride were independently associated with severity of atherosclerosis. BMI, WC, CI, and WHtR had no significant association with severity of atherosclerosis.
Our findings showed that anthropometric indices reflective of general and abdominal obesity were not independently related to the severity of atherosclerosis in adults, in northern Iran.
Keywords: atherosclerosis, body mass index, conicity index, Iran, waist-circumference, waist-to-height ratio
1. Introduction
Atherosclerosis, the principal cause of coronary artery disease (CAD), is a complex phenomenon, which can be described as an excessive fibro-fatty, proliferative, inflammatory response to damage of the artery wall and involving several cell types.[1,2] CAD is the leading cause of death worldwide.[3] The prevalence of cardiovascular disease varies geographically and culturally. Its incidence varies from culture to culture and country to country.[1,4] Iran possibly has a higher burden relative to other countries in this region.[4] Many risk factors have been identified for CAD. Obesity, which refers to the excessive accumulation of body fat, has been identified as a potential cardiovascular risk factor for a long time.[5,6] Obesity often leads to a negative effect on health and numerous studies have shown that it increases morbidity and mortality.[7,8]
It is estimated that by 2030 up to 57.8% of adults in the world would suffer from being overweight or obese.[9] Findings of a national study emphasizes high prevalence of obesity among population who live in different regions of Iran.[9] Body mass index (BMI) is a technique that is used to classify general body weight, widely.[10] Studies have shown that central body fat distribution has more atherogenic properties than peripheral fat distribution.[11] To measure central obesity, various indices have been suggested; waist circumference (WC), and waist-to-height ratio (WHtR) are regarded as the most popular indices. Abdominal volume index (AVI) and conicity index (CI) have also been introduced recently.[12] Studies confirm that ethnicity and geographic area can influence the association between anthropometrics index and CAD. Based on recent studies, the same anthropometric obesity measures cannot be used across all ethnic groups and also, ethnicity should be incorporated into cardiovascular assessment.[13,14]
Recent observational studies have reported differential relationships between the different anthropometric indices of obesity and risk for cardiovascular disease. However, it remains undetermined whether anthropometric indices of obesity are also associated with severity of atherosclerosis and which anthropometric obesity measures are more strongly associated with atherosclerosis in different ethnic groups or geographic area.
A coronary angiogram is a diagnostic image and validated biomarker of the anatomic extent of atherosclerotic disease which uses dye and special X-rays to show the inside of coronary arteries and severity of atherosclerosis. Because of the effect of ethnicity and geographic area on the association between anthropometric measures and cardiovascular disease, it is necessary to examine the associations between anthropometric indices reflective of general and abdominal obesity with severity of atherosclerosis in adult population in the north of Islamic Republic of Iran, a geographic area that has the high prevalence of obesity and CAD.
2. Material and method
This cross-sectional study was performed on 610 participants, age 20 to 75 years, who were admitted to a tertiary hospital in Rasht (center of Guilan province in the north of Iran) because they were chosen for elective angiography, between December 22, 2015 and April 20, 2016. The patients who were diagnosed with renal or inflammatory diseases such as rheumatoid arthritis were excluded from the study. All participants gave informed consent for the study, which was approved by the Ethics Committee of Guilan University of Medical Sciences. Trained health care providers measured blood pressure. Both systolic and diastolic blood pressure levels were measured using a gauge of the right arm and after 15 minutes rest with a mercury sphygmomanometer in a sitting position. Systolic blood pressure level more than 140 mm Hg and diastolic blood pressure level more than 90 mm Hg were considered hypertension.
2.1. Anthropometric indices
To measure central obesity, WC, WHtR, and CI, and to measure general obesity, BMI were regarded. Trained health care providers measured anthropometric data, including weight, height, WC. Before weight measurement, calibration of weighing scales was performed with 5-kg weights. Moreover, the removal of excess clothes and shoes was recommended to assure accurate measurements.
BMI was calculated as weight (in kilogram) divided by height squared (in m2). A BMI 25 or more is defined as overweight while a BMI 30 or more is characterized as obese.
WC was determined, in duplicate, at the midpoint between the lowest costal ridge and the upper border of the iliac crest. WC was done with a nonstretchable and accurately calibrated scale with 0.5-cm precision. In the event of a>2-cm discrepancy, then a third measurement was performed and the average of the 2 nearest values was reported as WC. In men, a cutoff point of 102 cm, and in women, a cutoff point of 88 cm were considered for WC. Height was measured while the participants were standing against a wall with their heels and buttocks in contact with the wall. WHtR and CI were calculated using formulas. Cutoff point of 0.5 was considered for WHtR,[15] and 1.25 was considered for CI.[16]
WHtR = waist (cm)/height (cm)
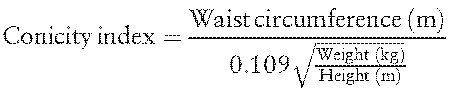 |
2.2. Coronary angiography
Coronary angiography was performed via femoral approach. Angiograms were analyzed by 2 cardiologists. Severity of atherosclerosis was estimated visually.
Angiograms with no visible atherosclerotic changes in the coronary arteries were considered normal. Stenosis that reduced the lumen diameter up to 50%, 50% to 70%, and more than 70% respectively was defined as mild, moderate, and severe stenosis.
The presence of stenosis in 1, 2, or 3 of major coronary arteries (left main, right coronary artery, left anterior descending, circumflex) was respectively considered evidence of single, 2, or 3-vessel coronary artery disease.
2.3. Blood measurements
A venous blood sample was drawn from each participant following 12-hour fasting to assess fasting blood sugar (FBS), hemoglobin A1c (HbA1c), triglycerides (TG), high-density lipoprotein cholesterol (HDLC), low-density lipoprotein cholesterol (LDL-C), total cholesterol, uric acid, and creatinine.
2.4. Statistical analyses
Continues and categorical data were described as mean (standard deviation) or frequency (percent), respectively. In this study, we categorized subjects into 2 groups including normal to mild and moderate to severe atherosclerosis. The 2 groups were compared using t test or χ2 test. Multivariate logistic regression model was used to estimate adjusted odds ratio with 95% confidence interval for anthropometric indices. Those variables with a P value less than 0.1 entered the multivariate adjusted model. The model goodness of fit was assessed using area under the ROC curve and Hosmer–Lemeshow statistic. All analyses were performed using Stata 13.
3. Result
A total of 610 healthy individuals were included in the study. The mean age of participants was 58.2 years (SD = 9.1) and more than half of them (55%) were men. Of total, 381 subjects (62%) had moderate to severe atherosclerosis. The frequencies of 1, 2, and 3-vessel CAD were 24%, 20%, and 26% respectively.
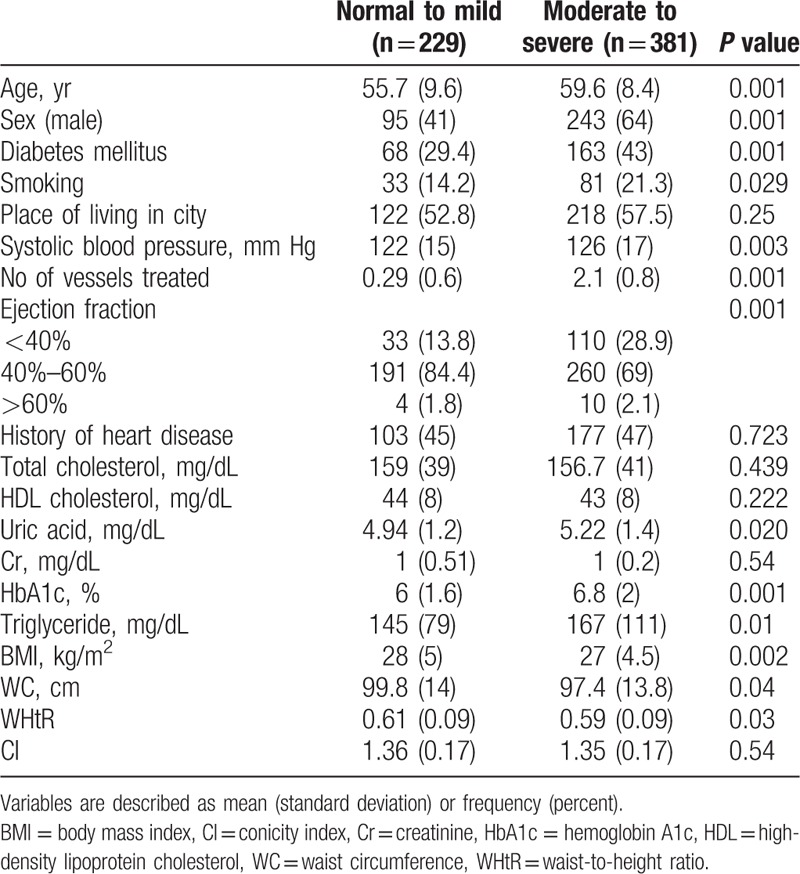
According to BMI, 267 subjects (44%) were overweight (BMI between 25 and 30) and 157 subjects (25.8%) were obese (BMI ≥30). Five hundred forty-eight subjects (90%) were obese based on WHtR and 348 subjects (57%) were obese based on WC. The mean of CI was 1.35 (SD = 0.17). Table 1 shows description of anthropometric indices according to sex. The mean of all anthropometric measures in women is significantly higher than in men. The distribution of participant characteristics, cardiovascular disease risk factors, and anthropometric indices according to severity of atherosclerosis is shown in Table 2. Participants with moderate to severe atherosclerosis were older, more likely to be men, had higher diabetes mellitus, smoking status, systolic blood pressure, total serum cholesterol, and uric acid level and lower HDL cholesterol level. In contrast, subjects with normal to mild atherosclerosis had significantly higher BMI and WC.
Table 1.
Anthropometric indices of participants according to sex.
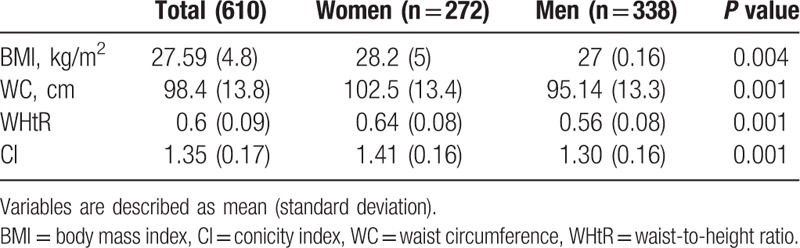
Table 2.
Participant's characteristics, cardiovascular risk factors, and anthropometric indices according to severity of atherosclerosis.
Association between severity of atherosclerosis and central obesity based on WC was different in 2 sexes. The prevalence of moderate to severe atherosclerosis in centrally obese women was significantly higher than in centrally nonobese women (52% vs 28% P = 0.02). But there was no significant difference in frequency of moderate to severe atherosclerosis and central or general obesity in men (Fig. 1).
Figure 1.
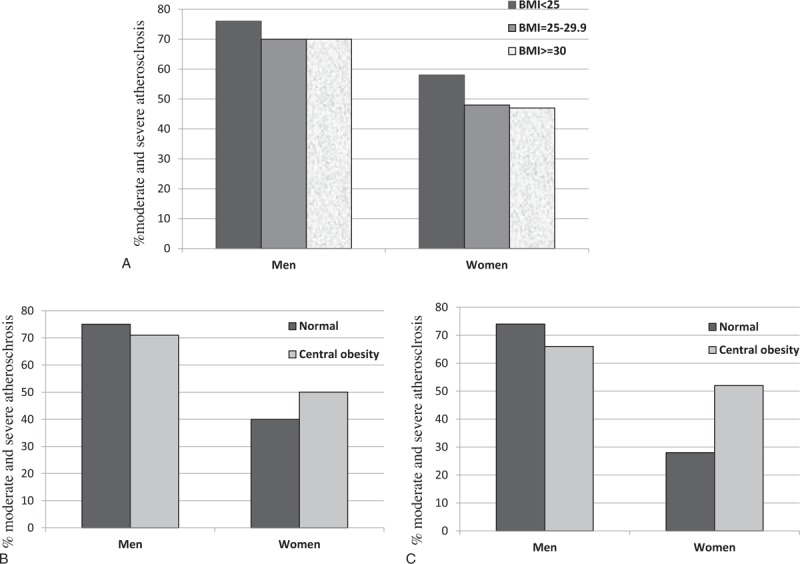
Comparison of the frequency of moderate to severe atherosclerosis based on categories of to body mass index (A), waist to height ratio (B), and waist circumference (C) in 2 sexes.
The results of multivariate adjustment model separately adjusted for each of obesity measures are shown in Fig. 2A–D. The models correctly classified 70% of patients. The area under the ROC curve for the model classifying patients to moderate and severe atherosclerosis was 0.75. Age, sex, and HbA1c were independently associated with severity of atherosclerosis. The odds of moderate to severe atherosclerosis in men was about 4 times more than in women and also significantly increased with age and HbA1c level. In multivariate adjusted analysis, the obesity status based on BMI, WC, CI, and WHtR had no significant association with severity of atherosclerosis.
Figure 2.
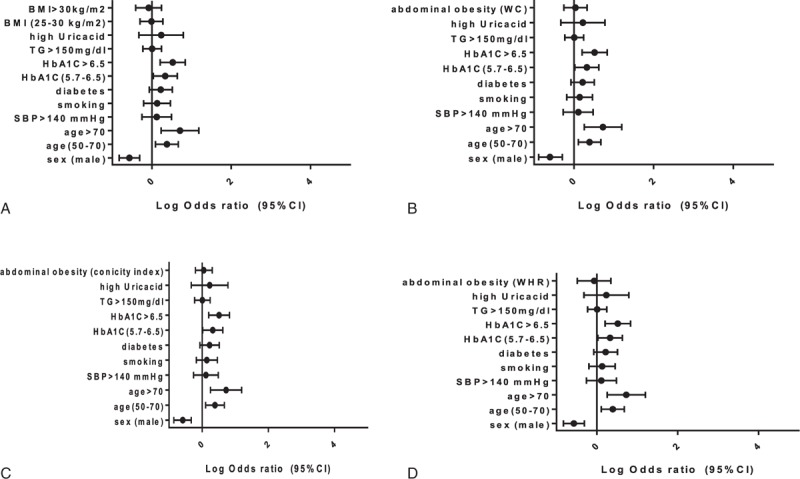
Association of obesity measures based on BMI (A), WC (B), CI (C), and WHtR (D) with moderate to severe atherosclerosis adjusted for covariates. Abdominal obesity based on CI >1.25, abdominal obesity based on WC>102 in men and >88 in women, abdominal obesity based on WHtR >0.5, high uric acid >7.5 in women and >8.5 in men. BMI = body mass index, CI = conicity index, SBP = systolic blood pressure, TG = triglyceride, WC = waist circumference, WHtR = waist-to-height ratio.
The association between obesity and other covariates was assessed using logistic regression analysis. Regarding obesity status based on CI>1.25 and WC≥102 in men and ≥88 in women, only the sex of participants was a significant predictor. For obesity status based on BMI ≥30 kg/m2, both sex and age were significant predictors in that the women were more likely to be obese and the odds of obesity based on BMI was significantly decreased with age.
4. Discussion
In the present study, the odds of moderate to severe atherosclerosis in men was about 5 times more than in women. We found that BMI, WHtR, WC, and CI were not independently related to the severity of atherosclerosis in healthy adults, in Rasht, northern Iran. Conversely, age, sex, systolic blood pressure, HbA1c, uric acid, and triglyceride were independently associated with severity of atherosclerosis. The association between WC and severity of atherosclerosis in our study was dependent on sex. In women, WC was significantly related to the severity of atherosclerosis. However the significant association disappeared after multivariate adjustment of other risk factors.
Some results of our research are in agreement with previous studies. The results of a cross-sectional study on 120 subjects who underwent coronary angiography showed anthropometric measurements can be used as practical tools for assessment of metabolic risk in overweight or obese subjects but not as markers of atherosclerosis.[17] In a study by Rallidis et al,[18] WC was not an independent predictor of carotid plaques after adjustment for cardiovascular risk factors in healthy individuals. A long-term community-based epidemiologic study showed that no specific differences in artery thickness were found between metabolic risk groups in normal weight and obese adults classified by BMI and WC. Their results implied that assessment of metabolic risk, regardless of a person's BMI or WC, can provide valuable information concerning atherosclerosis status.[19]
Data from 1691 participants enrolled in the Coronary Artery Risk Development in Young Adults Study aged 40 years or more showed that in middle-aged adults, longitudinal changes in BMI had the little independent influence on changes in 10-year atherosclerotic cardiovascular disease risk scores as its effect may be largely mediated through risk factors already accounted for in the risk score.[20] WHtR indices could differ among sex and age groups because whole-body fat distribution and WC change considerably with age and also height differs among generations.[21] Two previous studies, in the United States and China, reported that the association between WHtR and cardiovascular disease was stronger among younger adults as compared with elderly adults.[22,23]
Conversely, many studies had shown a positive association between some obesity indices and atherosclerosis;examples are positive association of BMI and WC with subclinical atherosclerosis in Pokharel et al study,[24] and association of WHtR with increased risk for coronary artery calcification progression in Oh et al study.[25]
Previous evidence showed that sex, race, ethnicity, and geographic area can influence the association between anthropometrics index and CAD and confirm that the same anthropometric obesity measure cannot be used across all ethnic groups.[13,19,26,27] The low rate of smoking in Iranian people, especially in women, and the Islamic ban on alcohol consumption can explain that body fat distribution in the study population may be less dependent on the environmental factors. No association between anthropometric indices of obesity and coronary atherosclerosis in our study may be related to ethnicity and racial influences. However, these findings need to be confirmed in larger population based studies.
The present data indicated that based on all obesity indices, women in Rasht were more likely to be obese than men. In a previous study in Rasht by Maddah et al,[28] girls were more likely to be overweight and obese than boys. It has been reported that there is less social pressure for conforming to an ideal body image in Iran.[28,29] Iran as an Islamic country is socially different from Western countries. Such differences can be seen in the dressing style of women in public and limited outdoor sport for women. Such a social environment might have made Iranian women less concerned about thinness and dieting.[29] More studies are needed to address this hypothesis. This study suffers from some limitations. The cross-sectional design of study prohibits temporal assessment between obesity and severity of atherosclerosis. In our study, we could not assess nonalcoholic fatty liver disease as a consequence of the metabolic syndrome, in which abdominal adiposity plays a key role. In addition, there may be residual confounding from unmeasured confounders such as economic status.
In conclusion, this study showed that anthropometric indices reflective of general and abdominal obesity were not independently related to the severity of atherosclerosis in healthy adults in Rasht, northern Iran.
Acknowledgments
The authors are grateful to the patients who participated in the study. The study was supported by Guilan university of Medical Sciences, Rasht, Iran.
Footnotes
Abbreviations: AVI = abdominal volume index, BMI = body mass index, CAD = coronary artery disease, CI = conicity index, FBS = fasting blood sugar, HbA1c = hemoglobin A1c, HDLC = high-density lipoprotein cholesterol, LDL-C = low-density lipoprotein cholesterol, TG = triglycerides, WC = waist circumference, WHtR = waist-to-height ratio.
The authors declare that they have followed the protocols of their work center on the publication of patient data and declare that no patient data appear in this article.
AS and MM-R conceptualized the study. Hospital coordination and analyzation of angiograms were performed by Mahboobeh Golipour and MN. RR collected the data. Data were analyzed by MS. MM-R wrote the manuscript and AS performed critical revision of the manuscript for important intellectual content. All authors read and approved the final manuscript.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
The authors have no conflicts of interest to disclose.
References
- [1].Motamed N, Perumal D, Zamani F, et al. Conicity index and waist-to-hip ratio are superior obesity indices in predicting 10-year cardiovascular risk among men and women. Clin Cardiol 2015;38:527–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Mahdavi-Roshan M, Zahedmehr A, Mohammad-Zadeh A, et al. Effect of garlic powder tablet on carotid intima-media thickness in patients with coronary artery disease: a preliminary randomized controlled trial. Nutr Health 2013;22:143–55. [DOI] [PubMed] [Google Scholar]
- [3].Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2013;380:2197–223. [DOI] [PubMed] [Google Scholar]
- [4].Talaei M, Sarrafzadegan N, Sadeghi M, et al. Incidence of cardiovascular diseases in an Iranian population: the Isfahan Cohort Study. Arch Iran Med 2013;16:138–44. [PubMed] [Google Scholar]
- [5].Sallis JF, Floyd MF, Rodríguez DA, et al. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation 2012;125:729–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Reaven GM. Insulin resistance: the link between obesity and cardiovascular disease. Med Clin North Am 2011;95:875–92. [DOI] [PubMed] [Google Scholar]
- [7].Arjmand G, Shidfar F, Nojoomi MM, et al. Anthropometric indices and their relationship with coronary artery diseases. Health Scope 2015;4: [Google Scholar]
- [8].Duncan M, Griffith M, Rutter H, et al. Certification of obesity as a cause of death in England 1979–2006. Eur J Public Health 2010;20:671–5. [DOI] [PubMed] [Google Scholar]
- [9].Esmaili H, Bahreynian M, Qorbani M, et al. Prevalence of general and abdominal obesity in a nationally representative sample of iranian children and adolescents: the CASPIAN-IV study. Iran J Pediatr 2015;25:e401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Su TT, Amiri M, Hairi FM, et al. Body composition indices and predicted cardiovascular disease risk profile among urban dwellers in Malaysia. BioMed Res Int 2015;2015: 174821. doi: 10.1155/2015/174821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Janiszewski PM, Janssen I, Ross R. Does waist circumference predict diabetes and cardiovascular disease beyond commonly evaluated cardiometabolic risk factors? Diabetes Care 2007;30:3105–9. [DOI] [PubMed] [Google Scholar]
- [12].Nyamdorj R. BMI compared with central obesity indicators in relation to diabetes and hypertension in Asians. Obesity 2008;16:1622–35. [DOI] [PubMed] [Google Scholar]
- [13].Goh LG, Dhaliwal SS, Welborn TA, et al. Ethnicity and the association between anthropometric indices of obesity and cardiovascular risk in women: a cross-sectional study. BMJ open 2014;4:e004702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Dhaliwal SS, Welborn TA. Measurement error and ethnic comparisons of measures of abdominal obesity. Prev Med 2009;49:148–52. [DOI] [PubMed] [Google Scholar]
- [15].Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0 5 could be a suitable global boundary value. Nutr Res Rev 2010;23:247–69. [DOI] [PubMed] [Google Scholar]
- [16].Shidfar F, Alborzi F, Salehi M, et al. Association of waist circumference, body mass index and conicity index with cardiovascular risk factors in postmenopausal women. Cardiovasc J Afr 2012;23:442–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Maddaloni E, Cavallari I, De Pascalis M, et al. Relation of body circumferences to cardiometabolic disease in overweight-obese subjects. Am J Cardiol 2016;118:822–7. [DOI] [PubMed] [Google Scholar]
- [18].Rallidis LS, Baroutsi K, Zolindaki M, et al. Visceral adipose tissue is a better predictor of subclinical carotid atherosclerosis compared with waist circumference. Ultrasound Med Biol 2014;40:1083–8. [DOI] [PubMed] [Google Scholar]
- [19].Camhi SM, Katzmarzyk PT, Broyles ST, et al. Subclinical atherosclerosis and metabolic risk: role of body mass index and waist circumference. Metab Syndr Relat Disord 2011;9:119–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Appiah D, Schreiner PJ, Durant RW, et al. Relation of longitudinal changes in body mass index with atherosclerotic cardiovascular disease risk scores in middle-aged black and white adults: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Ann Epidemiol 2016;26:521–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Tatsumi Y, Watanabe M, Kokubo Y, et al. Effect of age on the association between waist-to-height ratio and incidence of cardiovascular disease: the Suita study. J Epidemiol 2013;23:351–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Gelber RP, Gaziano JM, Orav EJ, et al. Measures of obesity and cardiovascular risk among men and women. J Am Coll Cardiol 2008;52:605–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Zhang X, Shu XO, Gao YT, et al. Anthropometric predictors of coronary heart disease in Chinese women. Int J Obes Relat Metab Disord 2004;28:734–40. [DOI] [PubMed] [Google Scholar]
- [24].Pokharel Y, Basra S, Lincoln AE, et al. Association of body mass index and waist circumference with subclinical atherosclerosis in retired NFL players. South Med J 2014;107:633–9. [DOI] [PubMed] [Google Scholar]
- [25].Oh HG, Nallamshetty S, Rhee EJ. Increased risk of progression of coronary artery calcification in male subjects with high baseline waist-to-height ratio: the Kangbuk Samsung health study. Diabetes Metab J 2016;40:54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Chen Y, Copeland WK, Vedanthan R, et al. Association between body mass index and cardiovascular disease mortality in east Asians and south Asians: pooled analysis of prospective data from the Asia Cohort Consortium. BMJ 2013;347:347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Li S, Chen W, Srinivasan SR, et al. Race (black–white) and gender divergences in the relationship of childhood cardiovascular risk factors to carotid artery intima–media thickness in adulthood: the Bogalusa heart study. Atherosclerosis 2007;194:421–5. [DOI] [PubMed] [Google Scholar]
- [28].Maddah M, Nikooyeh B. Factors associated with overweight in children in Rasht, Iran: gender, maternal education, skipping breakfast and parental obesity. Public Health Nutr 2010;13:196–200. [DOI] [PubMed] [Google Scholar]
- [29].Maddah M, Eshraghian MR, Djazayery A, et al. Association of body mass index with educational level in Iranian men and women. Eur J Clin Nutr 2003;57:819–23. [DOI] [PubMed] [Google Scholar]


