Abstract
Long noncoding RNAs (lncRNAs) are emerging as having multiple roles in cancer progression. However, roles of lncRNAs in chemotherapy for colorectal cancer (CRC) remain unclear. This study investigated the biological functions of lncRNA PANDAR in CRC cells treated with curcumin chemotherapy. Herein, we identified that PANDAR expression was not notably differential in CRC tissues compared with the corresponding normal tissues. Consistently, in vitro experiments revealed that knockdown of PANDAR could not change the proliferation, apoptosis, or senescence of CRC cells. Further analyses showed that low-dose curcumin could induce senescence in CRC cells without affecting cell apoptosis. Moreover, expression of PANDAR was increased in curcumin-treated CRC cells. Furthermore, silencing PANDAR in curcumin-treated cells increased apoptosis and greatly attenuated senescence possibly by stimulating the expression of PUMA. Together, these findings indicate that knockdown of lncRNA PANDAR switches curcumin-induced senescence to apoptosis, which may be potentially valuable in CRC therapy.
Keywords: colorectal cancer, long noncoding RNA, PANDAR, curcumin, chemotherapy
Introduction
Colorectal cancer (CRC) has become the third most common cancer and the fourth most common cause of cancer-related mortality globally.1 To improve overall survival, adjuvant chemotherapy has been the cornerstone of therapy for all patients with stage III/IV and high-risk stage II colon cancer.1,2 Curcumin is a phytochemical reported to inhibit various vital pathways in cancer cells, rending curcumin a chemopreventive and antimetastatic agent clinically.3–5 Numerous studies have demonstrated that curcumin could inhibit the growth of CRC cells mainly by inducing apoptosis.6,7 While recently, researchers found that curcumin at a low dose of 10 μM, at which the inhibition of cell proliferation was started to be detectable, could exert its antitumor activity via induction of senescence in CRC cells.8,9 Since the reports that curcumin at a concentration higher than 10 μM was cytotoxic to human cells building the vasculature,10 the effects of a modest dose of curcumin on CRC cells should be further studied.
Recently, large-scale researches have shown that long noncoding RNAs (lncRNAs) are nonprotein-coding transcripts that surpass 200 nucleotides in length, whose aberrant expression is associated with different cancer types.11 Thousands of lncRNAs are found to be differentially expressed in tumors using next-generation sequencing and tissue microarray technologies. Meanwhile, various dysregulated lncRNAs have been linked to malignant transformation through affecting cellular homeostasis, including survival, proliferation, migration, or genomic stability.11–16 LncRNA PANDAR (promoter of CDKN1A antisense DNA damage-activated RNA) is located at 6p21.2 and has been firstly reported by Hung et al.17 They found that doxorubicin could upregulate the expression of PANDAR in human fibroblasts, and elevated PANDAR then inhibited the activation of pro-apoptotic genes (FAS, NOXA, and PUMA) through binging the transcription factor NF-YA.17 While in the research of Puvvula et al, they demonstrated that the expression of PANDAR was stimulated when the human fibroblasts were induced senescence, and PANDAR depletion could decrease the senescence percentage through releasing NF-YA and stimulating the expression of NF-YA-E2F-coregulated genes (CCNB1, CDC25C, and CDK1).18 These multiple biological functions of PANDAR promoted us to explore whether similar processes exist in CRC cells under the gene stress induced by curcumin.
In our study, we firstly explored the role of PANDAR in colorectal carcinogenesis. However, we could not identify remarkable expression difference of PANDAR between CRC tissues and paired adjacent normal tissues, which was not consistent with the report of Lu et al.19 Moreover, knockdown of PANDAR could not significantly affect the proliferation of CRC DLD-1 cells. Then, we demonstrated that low-dose curcumin (5 μM) could induce senescence without apoptosis response. Meanwhile, the expression of PANDAR was upregulated in DLD-1 cells treated with curcumin at this senescence-inducing concentration. Considering the findings of Hung et al,17 we hypothesized that the elevated expression of PANDAR could attenuate curcumin-induced apoptosis. Surprisingly, our results indicated that silencing PANDAR not only increased apoptosis but also attenuated senescence in DLD-1 cells treated with curcumin, which corresponded with the result of Puvvula et al.18 Furthermore, we detected the expression of the downstream genes described above between the curcumin-treated group and the curcumin combined with silencing PANDAR group. As a result, we identified that PANDAR could be induced by low-dose curcumin and the silencing of PANDAR might switch senescence to apoptosis partly by stimulating the expression of PUMA (p53-upregulated modulator of apoptosis).
Materials and methods
Patients and cell lines
Twenty-three pairs of samples (including 23 CRC samples and normal adjacent tissues) from CRC patients were obtained from the Second Affiliated Hospital, Nanjing Medical University. No anticancer treatments of these patients had been conducted before the surgery. All patients provided written informed consent for the use of the tissue samples used in this research. Our study was approved by the Research Ethics Committee of Nanjing Medical University, People’s Republic of China.
Three CRC cell lines DLD-1, SW620, and HCT116 were obtained from the Cell Bank of the Chinese Academy of Medical Sciences (Shanghai, People’s Republic of China). Cells were cultured in Roswell Park Memorial Institute (RPMI) 1640 or Dulbecco’s Modified Eagle’s Medium (DMEM) (Hyclone, Logan, UT, USA) supplemented with 10% fetal bovine serum (Thermo Fisher Scientific, Waltham, MA, USA) at 37°C in a 5% CO2 incubator.
Quantitative real-time polymerase chain reaction (qRT-PCR)
Total RNA was extracted from CRC tumor tissues, matched adjacent normal tissues, and CRC cells using TRIzol reagent (Thermo Fisher Scientific) according to the manufacturer’s protocol. RNA was reverse transcribed to cDNA by using a reverse transcription kit (Takara Biotechnology, Dalian, People’s Republic of China). Then, qRT-PCR was performed using an ABI7300 system and the SYBR Green PCR Master Mix (Takara Biotechnology). The qRT-PCR results were normalized to glyceraldehyde-3-phosphate dehydrogenase. Primers used for target amplification are listed in Table 1. All qPCR data were calculated and expressed using the 2−∆∆Ct method and then converted to fold changes.
Table 1.
Primers for real-time polymerase chain reaction analysis
| Gene name | Forward | Reverse |
|---|---|---|
| GAPDH | 5′-AGCCACATCGCTCAGACAC-3′ | 5′-GCCCAATACGACCAAATCC-3′ |
| PANDAR | 5′-TGCACACATTTAACCCGAAG-3′ | 5′-CCCCAAAGCTACATCTATGACA-3′ |
| FAS | 5′-GCTGGGCATCTGGACCCTCCTACCT-3′ | 5′-CAGTCACTTGGGCATTAACACTT-3′ |
| NOXA | 5′-AGCAGAGCTGGAAGTCGAGTGTG-3′ | 5′-TGATGCAGTCAGGTTCCTGAGC-3′ |
| PUMA | 5′-ACGACCTCAACGCACAGTACGAG-3′ | 5′-TAATTGGGCTCCATCTCGGG-3′ |
| CCNB1 | 5′-AATAAGGCGAAGATCAACATGGC-3′ | 5′-TTTGTTACCAATGTCCCCAAGAG-3′ |
| CDC25C | 5′-TCTACGGAACTCTTCTCATCCAC-3′ | 5′-TCCAGGAGCAGGTTTAACATTTT-3′ |
| CDK1 | 5′-AAATGTGTGTAGGTCTCAC-3′ | 5′-ATGATTTAAGCCAACTCAAA-3′ |
Curcumin and treatment
Curcumin was purchased from Sigma-Aldrich (St Louis, MO, USA) and dissolved as a 10-mM stock solution in dimethylsulfoxide (DMSO). For every experiment, the stock solution was diluted in culture medium immediately to obtain the appropriate concentration. The control groups received DMSO diluted accordingly (final DMSO concentration was 0.1% in all groups). To induce senescence, cells were cultured in the presence of curcumin for 24 h as described before.8
Cell transfection
DLD-1 was selected to perform following experiments as lncRNA-PANDAR expression levels in DLD-1 cells were the highest among all cell lines. RNA interference was performed by using synthetic small interfering RNA (siRNA) duplexes. Three siRNA duplexes (siRNA1: 5′-AAUGUGUGCACGUAACAGAUU-3′, siRNA2: 5′-GGGCAUGUUUUCACAGAGGUU-3′, and siRNA3: 5′-GAGAUUUGCAGCAGACACAUU-3′) targeting the PANDAR RNA sequences and a negative control (si-NC) were synthesized by Guangzhou RiboBio Company (Guangzhou, People’s Republic of China). All cells were cultured in six-well plates and transfected using Lipo-fectamine 2000 (Thermo Fisher Scientific) following the manufacturer’s instructions. After 48 h of transfection, the cells were harvested for further experiments.
Cell proliferation assay
The viability of DLD-1 cells was assessed using the Cell Counting Kit-8 (CCK-8; Dojindo, Kumamoto, Japan) at 24, 48, and 72 h after transfection or curcumin treatment. The absorbance was measured at 450 nm. As for the colony formation assay, a total of 500 cells were seeded in six-well plates to allow colony formation for 2 weeks. The colonies were fixed with methanol and stained with Giemsa for 20 min, and the visible colonies were manually counted.
Senescence-associated β-galactosidase staining
Senescence-associated β-galactosidase (SA-β-Gal) was detected using SA-β-Gal staining kit (Beyotime, Beijing, People’s Republic of China) according to the manufacturer’s instructions. Briefly, cells were rinsed with phosphate-buffered saline (PBS) and immersed in SA-β-Gal fixing solution for 15 min at room temperature. After removing the fixative solution, cells were washed with PBS three times and stained with working solution at 37°C overnight. The percent of SA-β-Gal-positive cells was calculated by counting stained and total cells, and images were taken using a microscope at 200× magnification.
Apoptosis analysis by flow cytometry
For the cell apoptosis assay, the cells were stained with fluorescein isothiocyanate-Annexin V and propidium iodide in the dark according to the manufacturer’s instructions. Then, the cells were detected by flow cytometry (FACScan; BD Biosciences, San Jose, CA, USA) and the CellQuest software program (BD Biosciences) and were discriminated into dead cells, viable cells, early apoptotic cells, and late apoptotic cells.
Western blotting
DLD-1 cells were lysed with RIPA lysis buffer (Beyotime). Protein extracts (40 μg) were separated by 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis and then transferred to polyvinylidene difluoride membranes. After blocking in 5% nonfat milk for 1 h, the membranes were incubated with anti-PUMA antibody at 4°C overnight, and β-action antibody was used as a control. Both antibodies were purchased from Bioworld Technology (Atlanta, GA, USA). Sequentially, the membranes were incubated with the secondary antibody, and the proteins were visualized with enhanced chemiluminescence. Protein expression was quantified by densitometric analysis.
Statistical analysis
All statistical analyses were performed by Student’s t-test on Statistical Package for the Social Sciences (SPSS) software (version 18.0; SPSS, Inc., Chicago, IL, USA). A P-value of <0.05 was statistically significant. The data were reported as mean ± SD. All experiments were performed at least three times.
Results
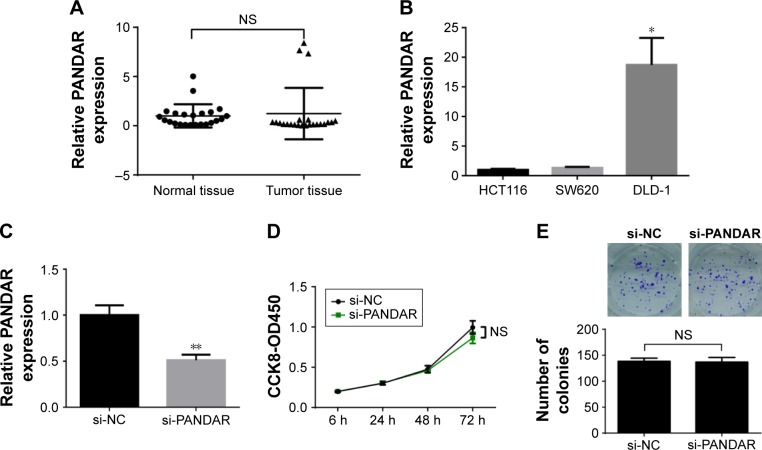
Expression of PANDAR is undifferentiated in CRC and has no obvious effect on CRC cell proliferation
To investigate the expression pattern of PANDAR in CRC, 23 paired human CRC tissues and the matched tumor adjacent normal tissues were analyzed by qRT-PCR. Compared with the normal tissues, the expression level of PAN-DAR was undifferentiated in the CRC tissues (P=0.7255; Figure 1A). Then, attempts were made to determine the effects of PANDAR on CRC cells. First, the expression level of PANDAR was detected in CRC cell lines, HCT116, SW620, and DLD-1. PANDAR expression was found to be significantly higher in DLD-1 compared with other CRC cell lines (P<0.05; Figure 1B). Then, siRNA against PANDAR was transfected into DLD-1 cells and demonstrated significant silencing capacity (P<0.01; Figure 1C). However, the CCK-8 assays were performed to find that the proliferation of DLD-1 cells transfected with si-PANDAR was not significantly changed compared with the control group (P≥0.05; Figure 1D). Consistently, the colony formation assays revealed that silencing PANDAR did not alter the clonogenic survival in DLD-1 cells (P≥0.05; Figure 1E). These results suggested that PANDAR probably could not affect the viability of CRC cells.
Figure 1.
LncRNA PANDAR is undifferentiated in human colorectal cancer (CRC) tissues and does not affect cancer cell growth in vitro.
Notes: (A) PANDAR expression was undifferentiated in CRC tissues in 23 CRC patients by qRT-PCR. (B) The relative expression level of PANDAR in CRC cell lines was detected by qRT-PCR. (C) DLD-1 cells were transfected with PANDAR siRNA and control siRNA. (D) CCK8 assay was performed to determine the proliferation of DLD-1 cells. (E) Colony-forming growth assay was performed to determine the proliferation of DLD-1 cells. The colonies were counted and captured. The experiments were repeated at least three times. *P<0.05, **P<0.01.
Abbreviations: CCK8, Cell Counting Kit-8; LncRNA, long noncoding RNAs; qRT-PCR, quantitative real-time polymerase chain reaction; siRNA, small interfering RNA; NS, nonsignificant; si-NC, small interference-negative control; OD, optical density.
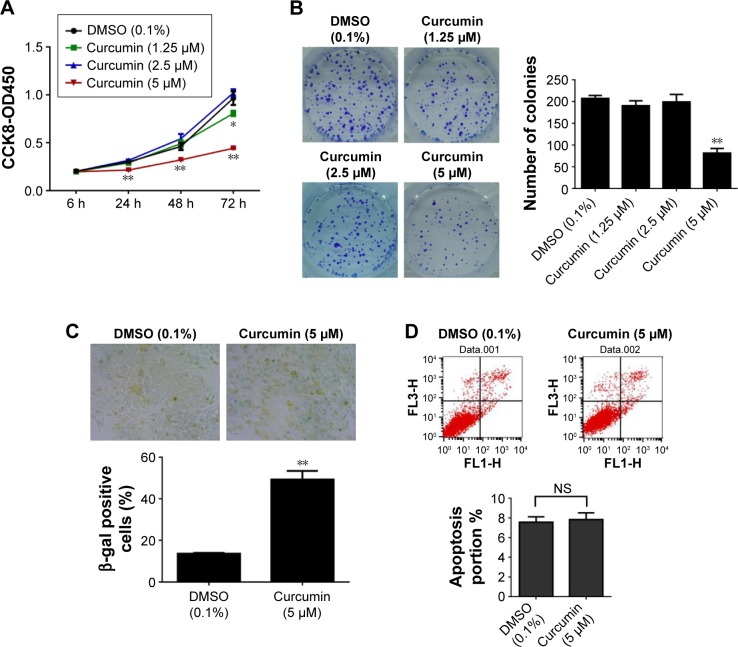
Low-dose curcumin triggers senescence but not apoptosis response in CRC cell
Recently, curcumin has been widely reported to play an important role in various types of cancer. In this study, curcumin was given to DLD-1 cells in vitro at a dose of 1.25–5 μM for 24 h. Then, we found that 5 μM curcumin initially induced detectable inhibition of cell proliferation (P<0.01; Figure 2A) and colony formation (P<0.01; Figure 2B), which was consistent with the lowest effective concentration 5–10 μM in CRC cells.7,20 Consequently, we decided to test the effects of curcumin on senescence and apoptosis phenotypes of DLD-1 cells at a concentration of 5 μM. To detect curcumin-related induction of senescence, we measured the SA-β-Gal activity in DLD-1 cells. In our studies, cells treated with curcumin (5 μM) for 24 h demonstrated a significant increase in β-galactosidase staining compared with the sham-treated (DMSO) group (P<0.01; Figure 2C). The apoptosis effects of curcumin on DLD-1 cells were analyzed using flow-cytometric analysis. However, we could not observe a significantly higher percentage of apoptotic cells following curcumin treatment (P≥0.05; Figure 2D). These results reflected that low-dose curcumin (5 μM) inhibited proliferation of CRC cell line DLD-1 potentially by inducing senescence rather than apoptosis.
Figure 2.
Low-dose curcumin triggers senescence but not apoptosis response in colorectal cancer cells.
Notes: (A) Curcumin was given to DLD-1 cells in vitro at a dose of 1.25–5 μM for 24 h. Then, cell viability was measured using CCK8 assay. (B) Colony-forming growth assay was used to investigate the proliferation of DLD-1 cells. (C) DLD-1 cells were treated with curcumin at a dose of 5 μM for 24 h, and the effect of curcumin on cellular senescence was observed by senescence-associated β-galactosidase staining. (D) The percentage of apoptotic cells was determined by flow-cytometric analysis. The experiments were repeated at least three times. *P<0.05, **P<0.01.
Abbreviations: CCK8, Cell Counting Kit-8; DMSO, dimethylsulfoxide; SA-β-Gal, senescence-associated β-galactosidase; NS, nonsignificant; OD, optical density; FL, fluorescence.
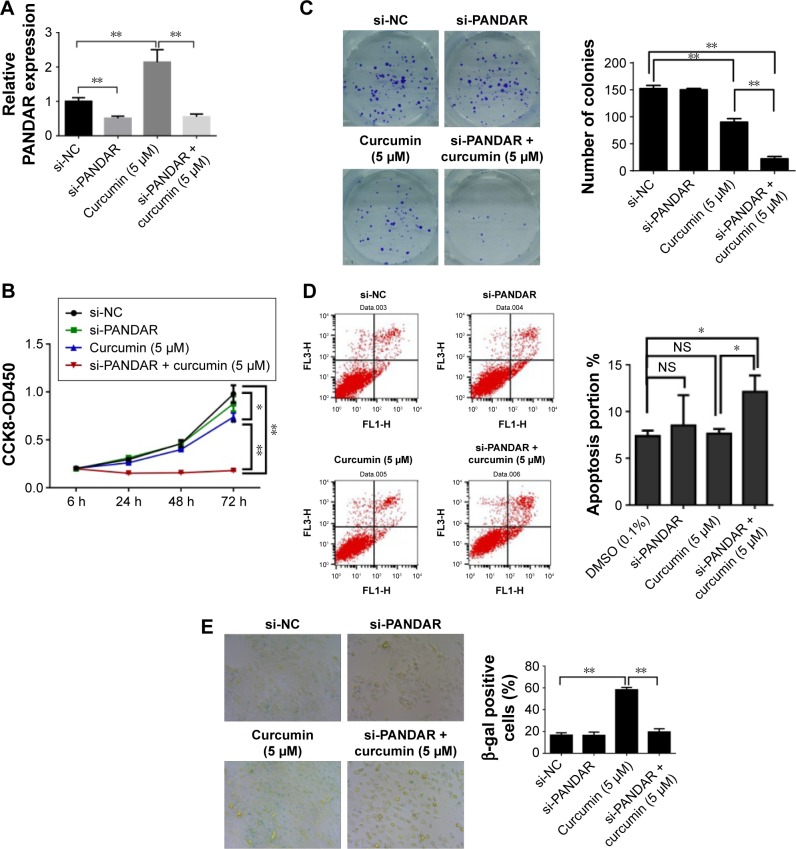
Downregulation of PANDAR in curcumin-treated CRC cells increases apoptosis but attenuates senescence
The results of Hung et al revealed that PANDAR was specifically upregulated by doxorubicin-induced DNA damage, and depletion of PANDAR sensitized fibroblasts to DNA-damage-induced apoptosis.17 Consequently, we detected the change of expression of PANDAR in DLD-1 cells treated with curcumin (5 μM) for 24 h. Our results demonstrated that the expression of PANDAR was increased compared with the control group, and transfection with si-PANDAR for 24 h before curcumin treatment could reverse the expression of PANDAR induced by curcumin (P<0.01; Figure 3A). Moreover, knockdown of PANDAR combined with curcumin treatment resulted in a significant inhibition of cell proliferation (P<0.01; Figure 3B) and clonogenic survival (P<0.01; Figure 3C) compared with the curcumin-alone-treated group. The findings described above raised the question that whether silencing PANDAR would sensitize curcumin-treated cells to apoptosis. Flow-cytometric analysis was performed and revealed that the percentages of apoptotic cells were increased in the combined treatment group (si-PANDAR and curcumin) compared with the curcumin-alone-treated group (P<0.05; Figure 3D), while the number of senescent cells was significantly decreased (P<0.01; Figure 3E). Our data also showed that the silencing of PANDAR alone had little to no effect on the apoptosis and senescence of DLD-1 cells (P≥0.05; Figure 3D and E).
Figure 3.
Downregulation of PANDAR in curcumin-treated CRC cells increases apoptosis but attenuates senescence.
Notes: (A) Expression of PANDAR was increased in DLD-1 cells treated with curcumin (5 μM) for 24 h by qRT-PCR. (B) CCK8 assay was used to investigate the proliferation of DLD-1 cells treated with knockdown of PANDAR combined with curcumin. (C) Colony-forming growth assay was used to investigate the proliferation of DLD-1 cells treated with knockdown of PANDAR combined with curcumin. (D) Flow-cytometric analysis was performed to determine the apoptotic percentage of curcumin-treated cells following PANDAR siRNA. (E) SA-β-Gal staining was performed to determine the cellular senescence of curcumin-treated cells following PANDAR siRNA. The experiments were repeated at least three times. *P<0.05, **P<0.01.
Abbreviations: CCK8, Cell Counting Kit-8; CRC, colorectal cancer; DMSO, dimethylsulfoxide; qRT-PCR, quantitative real-time polymerase chain reaction; SA-β-Gal, senescence-associated β-galactosidase; siRNA, small interfering RNA; NS, nonsignificant; FL, fluorescence; OD, optical density; si-NC, small interference-negative control.
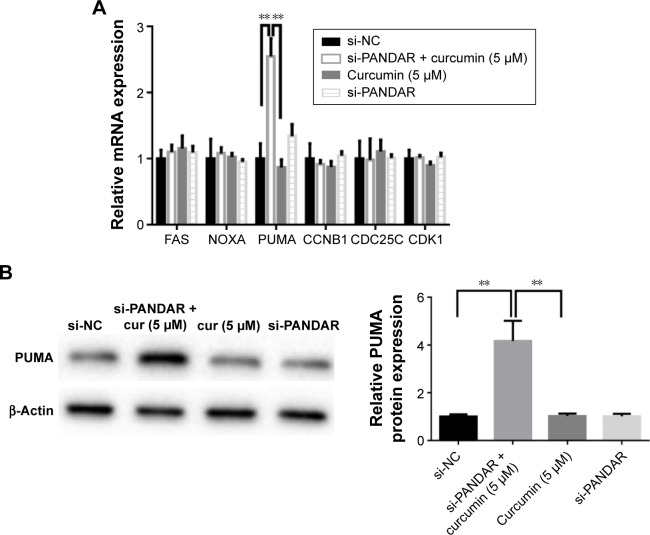
Silence of PANDAR switches curcumin-induced senescence into apoptosis possibly by stimulating the expression of PUMA
Previous studies revealed that PANDAR depletion could sensitize doxorubicin-treated fibroblasts to apoptosis through stimulating the expression of pro-apoptotic genes (FAS, NOXA, and PUMA) and also led to an exit from senescence in senescent fibroblasts by increasing the expression of cell-cycle genes (CCNB1, CDC25C, and CDK1).17,18 To probe the downstream genes regulated by PANDAR in curcumin-treated CRC cells, we detected the messenger RNA (mRNA) expression levels of these six protein-coding genes using qRT-PCR. Compared with the negative control cells and the curcumin-alone-treated group, the data showed that the knockdown of PANDAR in curcumin-treated CRC cells led to increased PUMA expression (P<0.01; Figure 4A). Meanwhile, the Western blot assays showed the same results (P<0.01; Figure 4B). These data indicated that knockdown of PANDAR might induce a part of the senescent cells treated by curcumin into apoptosis partly by stimulation of PUMA expression.
Figure 4.
qRT-PCR and Western blotting screening genes associated with the switch from senescence to apoptosis.
Notes: (A) qRT-PCR was used to detect the mRNA levels of FAS, NOXA, PUMA, CCNB1, CDC25C, and CDK1 in the DLD-1 cells treated with negative control, si-PANDAR combined with curcumin, curcumin alone, and si-PANDAR alone. (B) Western blotting analysis showed that the protein levels of PUMA were detected in DLD-1 negative control, si-PANDAR combined with curcumin, curcumin alone, and si-PANDAR cells. The experiments were repeated at least three times. *P<0.05, **P<0.01.
Abbreviations: qRT-PCR, quantitative real-time polymerase chain reaction; si-NC, small interference-negative control.
Discussion
In recent years, 5-year survival rate of CRC has increased with the help of early diagnostic technologies, but metastatic CRC (mCRC) remains inoperable and fatal.21,22 For these incurable patients, the previous standard of treatment is to continue chemotherapy until disease progression, unacceptable side effects, or death.23 Among these chemotherapy strategies including continued treatment, intermittent treatment, and maintenance with the least toxic regimens, the maintenance therapy minimizes the side effects without compromising the therapeutic efficacy and quality of life of the patients. In addition, prolonged progression free survival of mCRC can be achieved with maintenance therapy.21 As a cancer chemopreventive agent, curcumin has been shown to inhibit the growth of CRC cells in vitro and in animal models, and reduce colon carcinogenesis in clinical trials.24 However, past studies suggested that high-dose curcumin supplementation could interfere with iron absorption in mice and induces senescence of cells building the vasculature.10,25 Hence, we intended to explore the effects of a modest dose of curcumin on CRC cancer cells, which might serve as a guideline for the maintenance therapy of curcumin clinically.
Emerging evidence highlighted that lncRNAs provided a critical role in the progression of CRC. Using microarray analysis, we previously identified that hundreds of lncRNAs were upregulated in metastatic lymph node compared with normal lymph node.26 Among these differentially expressed lncRNAs, long intergenic noncoding RNA GAPLINC was confirmed to promote CRC cell invasion by targeting SNAI2 through binding with PSF and NONO and might serve as a promising therapeutic target for CRC.27 Moreover, Lee et al reported that lncRNA snaR could sensitize CRC cells to 5-fluorouracil, providing novel insights into the relationship between lncRNAs and cancer chemotherapy.28 Our present study explored the expression patterns of lncRNA PANDAR in CRC patients, but no significant difference of expression between CRC and paracancerous tissues was observed. Moreover, the silencing of PANDAR could not change the proliferation of DLD-1 cells, which did not coincide with the previous data that PANDAR was upregulated in CRC tissues than in the paired normal tissues and promoted malignant phenotypes of CRC cells LoVo and SW480.19 Considering the limited sample size and the cell specificity in the present study, the carcinogenesis roles of PANDAR in CRC needed to be further confirmed.
Increasing data reported that low doses of chemotherapeutics are able to induce cellular senescence, a permanent proliferative arrest which has been documented as a tumor suppression mechanism.29,30 However, compared with apoptosis response, cellular senescence revealed some serious limitations in anticancer therapy. Cancer cells that underwent senescence usually developed senescence-associated secretory phenotype, which could promote proliferation and detrimental chemoresistance properties of neighboring cancer cells. In addition, these chemoresistant cells might become the source of tumor recurrence.31 Our present results showed that silencing PANDAR expression could increase the apoptotic percentage of the DLD-1 cells treated by low-dose curcumin, suggesting that appropriate gene stress is required for PANDAR silencing-mediated apoptosis of CRC cell. This process was also accompanied by a decrease in the proportion of senescent cells, which shed new light on chemotherapy treatment for CRC.
Puvvula et al revealed that PANDAR knockdown could decrease the senescent percentage of human fibroblasts partly by stimulating the expression of cell cycle-related genes such as CCNB1, CDC25C, and CDK1.18 However, we could not detect any changes in mRNA levels of these three genes in DLD-1 cells under the combined treatment of silencing PANDAR and curcumin. While in the research of Hung et al,17 they found that DNA damage induced the expression of PANDAR. Moreover, elevated expression of PANDAR could interact with the transcription factor NF-YA to attenuate the expression of pro-apoptotic genes including FAS, NOXA, and PUMA. Among these genes, PUMA was significantly induced in DLD-1 cells with combined treatment described above and identified as a candidate gene in our present research. PUMA, a BH3-only Bcl-2 family member, can initiate apoptotic response in several human cancers.32 Consequently, our data suggested that the decrease in senescent cells might be a passive process because a portion of senescent cells probably entered into the apoptosis pathway partly by increasing the expression of PUMA. However, how low-dose curcumin-induced PANDAR and how PANDAR limited the expression of PUMA needed to be further explored in our study.
Conclusion
Taken all together, low-dose curcumin-induced senescent CRC cells can be switched from senescence to apoptosis by knockdown of lncRNA PANDAR. Therefore, we provided an enlightening insight into CRC chemotherapy.
Acknowledgments
This research was supported by the Science and Technology projects of Jiangsu Province, Bureau of Traditional Chinese Medicine (YB2015171).
Footnotes
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Brenner H, Kloor M, Pox CP. Colorectal cancer. Lancet. 2014;383(9927):1490–1502. doi: 10.1016/S0140-6736(13)61649-9. [DOI] [PubMed] [Google Scholar]
- 2.Strum WB. Colorectal adenomas. N Engl J Med. 2016;374(11):1065–1075. doi: 10.1056/NEJMra1513581. [DOI] [PubMed] [Google Scholar]
- 3.Heger M, van Golen RF, Broekgaarden M, Michel MC. The molecular basis for the pharmacokinetics and pharmacodynamics of curcumin and its metabolites in relation to cancer. Pharmacol Rev. 2013;66(1):222–307. doi: 10.1124/pr.110.004044. [DOI] [PubMed] [Google Scholar]
- 4.He ZY, Shi CB, Wen H, Li FL, Wang BL, Wang J. Upregulation of p53 expression in patients with colorectal cancer by administration of curcumin. Cancer Invest. 2011;29(3):208–213. doi: 10.3109/07357907.2010.550592. [DOI] [PubMed] [Google Scholar]
- 5.Patel VB, Misra S, Patel BB, Majumdar AP. Colorectal cancer: chemopreventive role of curcumin and resveratrol. Nutr Cancer. 2010;62(7):958–967. doi: 10.1080/01635581.2010.510259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Toden S, Okugawa Y, Buhrmann C, et al. Novel evidence for curcumin and Boswellic acid-induced chemoprevention through regulation of miR-34a and miR-27a in colorectal cancer. Cancer Prev Res. 2015;8(5):431–443. doi: 10.1158/1940-6207.CAPR-14-0354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guo LD, Chen XJ, Hu YH, Yu ZJ, Wang D, Liu JZ. Curcumin inhibits proliferation and induces apoptosis of human colorectal cancer cells by activating the mitochondria apoptotic pathway. Phytother Res. 2013;27(3):422–430. doi: 10.1002/ptr.4731. [DOI] [PubMed] [Google Scholar]
- 8.Mosieniak G, Adamowicz M, Alster O, et al. Curcumin induces permanent growth arrest of human colon cancer cells: link between senescence and autophagy. Mech Ageing Dev. 2012;133(6):444–455. doi: 10.1016/j.mad.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 9.Mosieniak G, Sliwinska MA, Przybylska D, et al. Curcumin-treated cancer cells show mitotic disturbances leading to growth arrest and induction of senescence phenotype. Int J Biochem Cell Biol. 2016;74:33–43. doi: 10.1016/j.biocel.2016.02.014. [DOI] [PubMed] [Google Scholar]
- 10.Grabowska W, Kucharewicz K, Wnuk M, et al. Curcumin induces senescence of primary human cells building the vasculature in a DNA damage and ATM-independent manner. Age. 2015;37(1):9744. doi: 10.1007/s11357-014-9744-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huarte M. The emerging role of lncRNAs in cancer. Nat Med. 2015;21(11):1253–1261. doi: 10.1038/nm.3981. [DOI] [PubMed] [Google Scholar]
- 12.Guil S, Esteller M. RNA-RNA interactions in gene regulation: the coding and noncoding players. Trends Biochem Sci. 2015;40(5):248–256. doi: 10.1016/j.tibs.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 13.Iyer MK, Niknafs YS, Malik R, et al. The landscape of long noncoding RNAs in the human transcriptome. Nat Genet. 2015;47(3):199–208. doi: 10.1038/ng.3192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sun M, Kraus WL. From discovery to function: the expanding roles of long noncoding RNAs in physiology and disease. Endocr Rev. 2015;36(1):25–64. doi: 10.1210/er.2014-1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yan X, Hu Z, Feng Y, et al. Comprehensive genomic characterization of long non-coding RNAs across human cancers. Cancer Cell. 2015;28(4):529–540. doi: 10.1016/j.ccell.2015.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schmitt AM, Chang HY. Long noncoding RNAs in cancer pathways. Cancer Cell. 2016;29(4):452–463. doi: 10.1016/j.ccell.2016.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hung T, Wang Y, Lin MF, et al. Extensive and coordinated transcription of noncoding RNAs within cell-cycle promoters. Nat Genet. 2011;43(7):621–629. doi: 10.1038/ng.848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Puvvula PK, Desetty RD, Pineau P, et al. Long noncoding RNA PANDA and scaffold-attachment-factor SAFA control senescence entry and exit. Nat Commun. 2014;5:5323. doi: 10.1038/ncomms6323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lu M, Liu Z, Li B, Wang G, Li D, Zhu Y. The high expression of long non-coding RNA PANDAR indicates a poor prognosis for colorectal cancer and promotes metastasis by EMT pathway. J Cancer Res Clin Oncol. 2017;143(1):71–81. doi: 10.1007/s00432-016-2252-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shakibaei M, Kraehe P, Popper B, Shayan P, Goel A, Buhrmann C. Curcumin potentiates antitumor activity of 5-fluorouracil in a 3D alginate tumor microenvironment of colorectal cancer. BMC Cancer. 2015;15:250. doi: 10.1186/s12885-015-1291-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Esin E, Yalcin S. Maintenance strategy in metastatic colorectal cancer: a systematic review. Cancer Treat Rev. 2016;42:82–90. doi: 10.1016/j.ctrv.2015.10.012. [DOI] [PubMed] [Google Scholar]
- 22.Marin JJ, Sanchez de Medina F, Castano B, et al. Chemoprevention, chemotherapy, and chemoresistance in colorectal cancer. Drug Metabol Rev. 2012;44(2):148–172. doi: 10.3109/03602532.2011.638303. [DOI] [PubMed] [Google Scholar]
- 23.Grem JL. Sequencing of treatment in advanced unresectable colorectal cancer. J Natl Compr Canc Netw. 2013;11(Suppl 4):S28–S37. doi: 10.6004/jnccn.2013.0218. [DOI] [PubMed] [Google Scholar]
- 24.Carroll RE, Benya RV, Turgeon DK, et al. Phase IIa clinical trial of curcumin for the prevention of colorectal neoplasia. Cancer Prev Res. 2011;4(3):354–364. doi: 10.1158/1940-6207.CAPR-10-0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chin D, Huebbe P, Frank J, Rimbach G, Pallauf K. Curcumin may impair iron status when fed to mice for six months. Redox Biol. 2014;2:563–569. doi: 10.1016/j.redox.2014.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Han J, Rong LF, Shi CB, et al. Screening of lymph nodes metastasis associated lncRNAs in colorectal cancer patients. World J Gastroenterol. 2014;20(25):8139–8150. doi: 10.3748/wjg.v20.i25.8139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang P, Chen T, Xu Z, Zhu H, Wang J, He Z. Long noncoding RNA GAPLINC promotes invasion in colorectal cancer by targeting SNAI2 through binding with PSF and NONO. Oncotarget. 2016;7(27):42183–42194. doi: 10.18632/oncotarget.9741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee H, Kim C, Ku JL, et al. A long non-coding RNA snaR contributes to 5-fluorouracil resistance in human colon cancer cells. Mol Cells. 2014;37(7):540–546. doi: 10.14348/molcells.2014.0151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Litwiniec A, Gackowska L, Helmin-Basa A, Zuryn A, Grzanka A. Low-dose etoposide-treatment induces endoreplication and cell death accompanied by cytoskeletal alterations in A549 cells: Does the response involve senescence? The possible role of vimentin. Cancer Cell Int. 2013;13(1):9. doi: 10.1186/1475-2867-13-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kahlem P, Dorken B, Schmitt CA. Cellular senescence in cancer treatment: friend or foe? J Clin Invest. 2004;113(2):169–174. doi: 10.1172/JCI20784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gonzalez LC, Ghadaouia S, Martinez A, Rodier F. Premature aging/senescence in cancer cells facing therapy: good or bad? Biogerontology. 2016;17(1):71–87. doi: 10.1007/s10522-015-9593-9. [DOI] [PubMed] [Google Scholar]
- 32.Chen D, Wei L, Yu J, Zhang L. Regorafenib inhibits colorectal tumor growth through PUMA-mediated apoptosis. Clin Cancer Res. 2014;20(13):3472–3484. doi: 10.1158/1078-0432.CCR-13-2944. [DOI] [PMC free article] [PubMed] [Google Scholar]