Introduction
Over two thirds of individuals over 65 years report pain which affects many aspects of daily life such as stress levels, mood, functional ability, and cognition (Herr and Garand, 2001). Most research on pain only studies its intensity and forgoes its interference in daily life activities. In this cross-sectional study of older adults, we aimed to evaluate levels of distinct dimensions of pain (intensity and interference) and their associations with cognitive function within the domains of episodic memory (EM: recall of discrete events) and executive function (EF: planning, problem solving, and direct attention).
Methods
We studied 1527 above 70-year-old non-demented participants in the Einstein Aging Study (see Zammit et al., 2015). The Short Form 36 (Ware and Sherbourne, 1992) was used to measure pain intensity (how much bodily pain a person has experienced over the past 4 weeks on an ascending scale of 0–5) and pain interference (how much pain has interfered with a person’s activities of daily life over the past 4 weeks on an ascending scale of 0–4). We created pain groups by combining levels of pain intensity and interference, as follows: no pain (intensity = 0 and interference = 0), LL [low intensity (≤2) and low interference (≤1)], LH [low intensity (≤2) and high interference (≥3)], HL [high intensity (≥3) and low interference (≤1)], and HH [high intensity (≥3) and high interference (≥2)]. Summary measures of two cognitive functions (EM and EF; both measures in z-scores) previously derived from principal component analysis in the Einstein Aging Study (Zammit et al., 2015) were used as independent variables. Multinomial logistic regressions were used to analyze the association between pain groups and EM and EF, adjusting for demographics (age, gender, ethnicity, and years of education), non-steroidal anti-inflammatory drug use, and depression by using the Geriatric Depression Scale (GDS; Sheikh and Yesavage, 1986; classified non-depressed: GDS ≤5 and depressed: GDS > 5). Data are expressed as %, mean ± SD, or odds ratio with 95% confidence interval. stata/ic 13.1 (StataCorp LP) was used for analyses.
Results
In our analysis population (1527), 62% were women and 66% were white. The mean age was 77.8 ± 5.3 years, and 51% had more than 13 years of education. The mean EM score was −0.3 ± 1.0 (range: −3.5 to 2.7) and that of EF was −0.2 ± 0.9 (range: −3.0 to 2.1). Thirty-one percent of participants belonged to the no pain group. Among those with pain (1503), 50% were classified as LL, 1% as LH, 38% as HL, and 11% as HH. Women were more likely to report pain than men, with 61.8% women classified as LL and 75.6% as HH. The proportion of non-steroidal anti-inflammatory drug users was higher in each pain group (range: 10.1% in LL to 18.5% in HH) compared with the no pain group (3.6%). We found higher percentages of people with depression within the LH (33.3%) and HH (35.3%) groups than in the no pain group (7.6%). Participants with high pain interference had lower scores on EM composite (group LH: −0.8 ± 0.6; group HH: −0.6 ± 0.9) and EF (group LH: −0.8 ± 0.6; group HH: −0.5 ± 0.9) than those with low pain interference (for LL group, EM: −0.2 ± 1.0 and EF: −0.2 ± 0.9; for HL group, EM: −0.2 ± 0.9 and EF: −0.2 ± 0.8) or the no pain (EM: −0.3 ± 1.0; EF: −0.2 ± 0.8) group. Fully adjusted multinomial logistic regressions revealed that for each standardized unit increase in EM or EF scores, there were increased odds of belonging to the no pain, LL, or HL groups versus the HH group (Figure 1).
Figure 1.
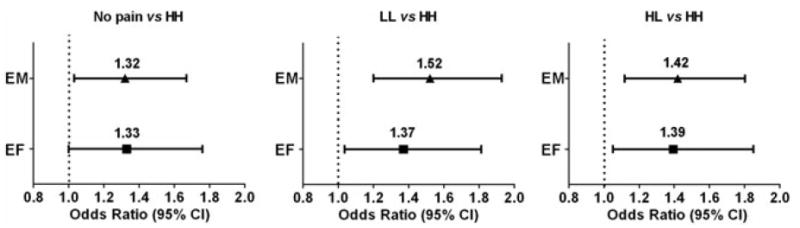
Associations of cognitive function and pain groups. Fully adjusted odds ratio (95% confidence interval) for the association of no pain, low intensity and low interference, and high intensity and low interference pain groups with episodic memory and executive function obtained from multinomial logistic regression, adjusted for demographics, use of non-steroidal anti-inflammatory drugs, and depression. The high intensity with high interference pain group was set as the reference. N = 1527 participants.
Conclusions
The present population-based study is in line with those obtained in clinical settings, reporting that pain and cognitive function are associated (see Moriarty et al., 2011). We examined two aspects of pain—intensity and interference—and found an inverse relationship between cognitive function and pain, particularly pain interference; even among those with high pain intensity, low pain interference was associated with higher cognitive function scores. This implies the importance of analyzing pain interference in addition to intensity when studying pain in older adults. Further study is needed to establish a causal relationship of the association between pain and cognition.
Acknowledgments
This work was supported by the National Institutes of Health: National Center for Advancing Translational Science (NCATS) Einstein-Montefiore CTSA (UL1TR001073) and the National Institute of Aging (P01AG003949).
Footnotes
Conflict of interest
None declared.
References
- Herr KA, Garand L. Assessment and measurement of pain in older adults. Clin Geriatr Med. 2001;17(3):457–478. doi: 10.1016/s0749-0690(05)70080-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriarty O, McGuire BE, Finn DP. The effect of pain on cognitive function: a review of clinical and preclinical research. Prog Neurobiol. 2011;93:385–404. doi: 10.1016/j.pneurobio.2011.01.002. [DOI] [PubMed] [Google Scholar]
- Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontol. 1986;5(1/2):165–173. [Google Scholar]
- Ware JE, Sherbourne CD. The MOS 36 item short-form health survey (SF-36) Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- Zammit AR, Katz MJ, Lai JY, et al. Association between renal function and cognitive ability domains in the Einstein Aging Study: a cross-sectional analysis. J Gerontol A Biol Sci Med Sci. 2015;70(6):764–770. doi: 10.1093/gerona/glu185. [DOI] [PMC free article] [PubMed] [Google Scholar]


