Abstract
Objective
The aim of the current study was to empirically examine naturally occurring groups of individuals with bulimia nervosa (BN) based on their childhood trauma (CT) histories and to compare these groups on a clinically relevant external validator, borderline personality disorder (BPD) psychopathology.
Method
The present study examined the relationship between CT and BPD psychopathology among 133 women with BN using latent profile analysis (LPA) to classify participants based on histories of CT. Participants completed the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I/P), the Diagnostic Interview for Borderlines-Revised (DIB-R), and the Childhood Trauma Questionnaire (CTQ).
Results
The LPA revealed four trauma profiles: low/no trauma, emotional trauma, sexual trauma, and polytrauma. Results indicated that the sexual and polytrauma profiles displayed significantly elevated scores on the DIB-R and that the low/no and emotional trauma profiles did not differ significantly on the DIB-R. Secondary analyses revealed elevated levels of a composite CT score among those with both BN and BPD psychopathology compared to those with BN only.
Discussion
These findings suggest that both childhood sexual abuse and the additive effects of childhood polytrauma may be linked to BPD psychopathology in BN.
Keywords: childhood abuse, childhood trauma, bulimia nervosa, borderline personality disorder, classification, latent profile analysis
Childhood trauma (CT) has been linked to the development of nearly all psychiatric disorders1. Research on the role of CT specifically in relation to eating disorders (EDs) and borderline personality disorder (BPD) has focused primarily on specific types of CT, including sexual abuse, physical abuse, and emotional abuse or neglect. Findings from studies of the association between these specific types of trauma and EDs have shown that: 1) there is a significant association between sexual abuse history and lifetime ED diagnoses2 and this history appears to be more common in EDs that include binge eating symptoms, such as bulimia nervosa (BN) and binge eating disorder (BED)3; 2) a history of physical abuse is associated with all ED diagnoses3; and 3) a history of emotional abuse is more common than other forms of abuse in bulimic samples and is more common in bulimic samples than controls4. Notably, though, contrasting findings have revealed that certain types of abuse are risk factors for psychopathology in general that includes, but is not specific to, EDs5–6. Similarly, findings on specific types of CT and their relationship with BPD lack consensus, as some studies have shown that certain types of CT are uniquely associated with BPD, while others have demonstrated relationships between certain types of CT and a number of different personality disorders7–10 or an indirect link between CT and BPD (e.g., through heritable vulnerabilities)11. Findings demonstrating differential relationships between CT and BPD suggest that: 1) sexual abuse is common, often co-occurs with other types of trauma, and can differentiate BPD from other personality disorder diagnoses12–15; 2) physical abuse is associated with the development of BPD13, but often not independently of other types of abuse16–17; and 3) a history of emotional abuse and/or neglect is a risk factor for the development of BPD7, 18 and it is uniquely related to BPD severity compared to sexual and physical abuse19. Taken together, these findings suggest that different forms of childhood abuse may have differential effects with regard to EDs and BPD psychopathology.
Given BN and BPD have common psychopathological features, including emotion dysregulation and impulsivity20–22, it is unsurprising that these two disorders are often comorbid23–27. However, although several studies have separately examined the role of CT in BN and CT in BPD, few studies have examined the role of CT in those with both BN and BPD. Results from these studies demonstrate that in bulimic samples: 1) sexual or physical abuse differentiates those with comorbid BPD from those without28; and 2) rates of sexual or physical abuse are higher in those with comorbid BPD, but proportions of any abuse (combined sexual and physical) do not significantly differentiate the two subgroups29. In addition to mixed findings, these studies did not examine other types of trauma exposure, such as emotional abuse or neglect. Further, evidence suggests there is a correlation between the presence of sexual abuse, physical abuse, and emotional abuse/neglect30–31, yet there have been no studies of the effects of polytrauma exposure in childhood relative to BPD psychopathology in BN samples. Thus, it is unclear how individual forms of CT co-vary among individuals with BN and furthermore, how multiple forms of CT may influence comorbid psychopathology in BN.
The aim of the current study, therefore, was to investigate the presence of different types of CT among individuals with BN and to examine the relationship between different types of CT and BPD psychopathology. To achieve this objective, a latent profile analysis (LPA) was conducted to derive an empirical taxonomy of individuals diagnosed with BN based on CT history. After identifying a meaningful classification system, the diagnostic validity of the CT-based profiles was tested by comparing the profiles on BPD psychopathology. To our knowledge, this was the first classification study of individuals with BN based on a taxonomy of CT history and validated with a clinically relevant construct.
METHOD
Participants
Participants were 133 women who met Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)32 criteria for BN. Most were single or never married (64.7%), Caucasian (97%), and had at least some college experience (62.4%). All participants were at least 18 years of age (M = 25.32, SD = 7.56, range 18–55). Recruitment of participants involved advertisements placed in ED clinics, college campuses, and throughout the community. Women participating in the study met the following inclusion criteria: a DSM-IV diagnosis of BN, medical stability, and no major changes in prescribed psychotropic medication for a minimum of six weeks. Those excluded from the study included pregnant women, men, and individuals under 18 years of age.
Measures
The Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-I/P)33 has been broadly utilized and is strongly endorsed as a psychometrically sound instrument. The SCID was used to assess BN and other comorbid psychiatric conditions. The kappa coefficient for interrater reliability of BN diagnoses based upon 25 randomly selected cases in the current study was 1.00.
The Diagnostic Interview for Borderlines-Revised (DIB-R)34 is a semi-structured interview that provides a diagnostic assessment of lifetime history of BPD psychopathology. The DIB-R has displayed sound psychometric properties35. The intraclass correlation coefficient for the DIB-R total score based upon 25 randomly selected cases in the current study was .98.
The Childhood Trauma Questionnaire (CTQ)36 is a 28-item retrospective, self-report measure of CT. Each item begins with the statement, “When I was growing up . . . “ Participants respond to items on a 5-point Likert scale that ranges from “never true” to “very often true”, indicating the frequency with which the experiences occurred. The CTQ contains five subscales measuring emotional abuse (e.g., “people in my family called me things like stupid, lazy, or ugly”), physical abuse (e.g., “people in my family hit me so hard that it left me with bruises or marks”), sexual abuse (e.g., “someone molested me”), emotional neglect (e.g., “I felt loved”), and physical neglect (e.g., “I didn’t have enough to eat”). Subscale scores each range from 5–25 and total scores, calculated by summing all five subscale scores, range from 25–125. The CTQ has been shown to have strong internal consistency, with alphas ranging from .68–.93 on the five subscales37, and good reliability for the total score38. CTQ scores have also been significantly related to trauma ratings from clinicians, welfare records, and reports from family members37.
Procedure
The data reported on in this investigation were drawn from a larger project that included ecological momentary assessment and other measures, which are not presented in this report (see Smyth et al., 200739 for more details). Phone screens were conducted to assess if interested participants met preliminary DSM-IV diagnostic criteria for BN. A total of 154 women were invited to an informational meeting to learn more about the study. Potential participants completed the informed consent documents and provided blood samples to determine medical stability (i.e., electrolyte screen) during this meeting. Eleven individuals were screened out of the study based upon the exclusion criteria. Structured clinical interviews and self-report measures were scheduled for completion during two additional assessment meetings, which each lasted approximately two hours. During the data collection period seven participants withdrew and three were excluded due to incomplete data, leaving 133 total subjects in the study. University of North Dakota and MeritCare Health System Institutional Review Boards approved the protocol.
Statistical Analysis
LPA, an extension of latent class analysis for categorical, ordinal, or continuous “indicator” variables, was used to classify individuals into unobserved (i.e., latent) categorical groups based on the principal of conditional independence where indicator variables are uncorrelated within classes40. Four CTQ subscales (emotional abuse, physical abuse, sexual abuse, and emotional neglect) were used as the indicator variables in the current study. The fifth CTQ subscale, physical neglect, was dropped from this analysis because it did not contribute to the differentiation of latent classes.
Latent Gold version 5.0 was used to compare 1- to 5-class models on the basis of the following fit indices: Consistent Akaike Information Criterion (cAIC)41, the Bayesian Information Criterion (BIC)42, and the sample size Adjusted BIC (aBIC)43. Pairwise residuals were used to evaluate the assumption of conditional independence. Class membership assignments were based on posterior Bayesian probabilities. In order to characterize the latent profiles, a series of one-way analyses of variance (ANOVAs) were used to compare classes on indicator variables. Post hoc comparisons between groups were based upon Tukey’s b.
To evaluate the external validity of the LPA results, an ANOVA was used to compare the latent profiles on the lifetime DIB-R total score. Pairwise differences between groups were based upon Tukey’s b post hoc comparisons. Adjusted analyses were conducted to control for the presence of any Axis I psychiatric comorbidity (i.e., presence/absence of any mood disorders, anxiety disorders (including posttraumatic stress disorder), or substance use disorders) using an ANCOVA to assess the external validity of the LPA results on the lifetime DIB-R total score. Pairwise differences between groups were again examined using Tukey’s b post hoc comparisons.
RESULTS
Trauma Subtype Identification and Description
The LPA supported a four-profile solution (see Table 1). The four profiles reflected distinct patterns of CT including low/no trauma (Profile 1, n=65; 47.87%), emotional trauma (Profile 2, n=37; 27.82%), sexual trauma (Profile 3, n=13; 9.77%), and polytrauma (Profile 4, n=18; 13.53%). As shown in Table 1, the polytrauma group displayed significantly higher scores on emotional abuse, physical abuse, and sexual abuse than the other three groups. The sexual trauma group displayed greater sexual abuse scores than the emotional trauma and low/no trauma groups, but did not differ from these groups on other forms of trauma. The emotional trauma group distinguished itself from the sexual trauma group and the low/no trauma group in terms of emotional abuse and emotional neglect scores. As expected, the low/no trauma group showed consistently low scores across all forms of trauma.
Table 1.
Latent Profile Analysis Indicators across Childhood Trauma Subtypes
| Indicator Variables | Low/No Trauma (n = 65) | Emotional Trauma (n = 37) | Sexual Trauma (n = 13) | Polytrauma (n = 18) | Test Statistic | Effect Size | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | F(3, 129) | p | partial η2 | |
| CTQ Emotional Abuse | 7.52a | 2.57 | 17.08b | 3.33 | 8.77a | 2.46 | 21.00c | 2.61 | 164.00 | <.001 | .79 |
| CTQ Physical Abuse | 5.48a | 0.87 | 7.54a | 3.02 | 6.69a | 2.36 | 14.28b | 6.15 | 43.44 | <.001 | .50 |
| CTQ Sexual Abuse | 5.00a | 0.00 | 5.49a | 0.93 | 14.00b | 5.48 | 19.72c | 5.74 | 170.04 | <.001 | .80 |
| CTQ Emotional Neglect | 8.06a | 3.07 | 15.32b | 3.92 | 8.46a | 3.89 | 17.39b | 3.17 | 58.54 | <.001 | .58 |
Note: M = Mean; SD = Standard Deviation; CTQ = Childhood Trauma Questionnaire. Different superscripts denote differences between the subtypes at p < .05
Trauma Subtype Validation
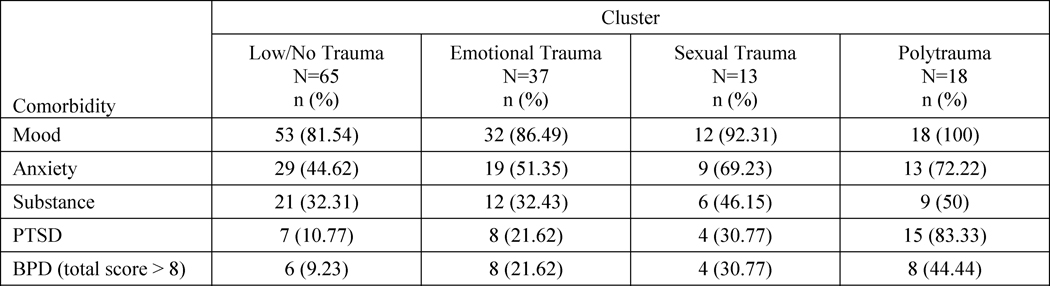
There were significant differences between the trauma profiles on the total score of the DIB-R [F(3,129)=6.50; p<.001; partial η2=.131]. Specifically, the polytrauma group (M=7.61; SD=2.25) was characterized by significantly higher DIB-R total scores compared to the emotional trauma (M=5.08; SD=3.15) and low/no trauma (M=4.17; SD=2.98) groups, but did not differ from the sexual trauma group (M=5.62; SD=3.28). Taking into consideration the size of the CT clusters and frequency of comorbid diagnoses in each group (see Table 2 for distribution of Axis I disorders and BPD psychopathology across CT clusters), adjusted analyses were conducted to compare the four CT profiles on the presence of BPD psychopathology after controlling for history of any psychiatric comorbidity. Results continued to show significant differences between the trauma profiles on the total score of the DIB-R [F(3,126)=3.57; p=.016; partial η2=.08]. Post hoc comparisons revealed that significantly more individuals in the polytrauma cluster had features of BPD than individuals in the low/no trauma group (p<.001) and the emotional trauma group (p<.05). However, there were no significant differences between the polytrauma and sexual trauma groups.
Table 2.
Distribution of Comorbid Psychiatric Disorders and Borderline Personality Disorder Psychopathology
Note: PTSD = posttraumatic stress disorder; BPD = borderline personality disorder psychopathology
Examination of CT Relative to BPD Psychopathology in BN
Given that a polytrauma group was identified in the LPA and because this subgroup was found to have elevated BPD psychopathology, a post hoc analysis was conducted to test the association between childhood polytrauma and co-occurring BN and BPD psychopathology. An ANOVA was used to compare those with BN and BPD psychopathology to those with BN only on the cumulative severity of any type of trauma using the CTQ total score. Results from this comparison revealed that the subgroup of women with BN and elevated levels of BPD psychopathology (using a cutoff of DIB-R total score > 8) had significantly higher total scores on the CTQ than those with a diagnosis of BN only [F(1,131)=12.83; p<.01).
DISCUSSION
The results of this study indicated that among women with BN, there were four distinct subgroups based on traumatic experiences during childhood. The largest subgroup consisted of those who reported low levels of all types of trauma (low/no trauma profile). Of the subgroups with trauma histories, the subgroup characterized by elevated emotional trauma relative to other types of trauma (emotional trauma profile) was larger than both the sexual trauma and polytrauma subgroups. This is consistent with literature demonstrating that childhood emotional trauma is more common than physical or sexual abuse in bulimic samples4.
The validity of these CT-based subgroups of women with BN was supported by the finding that there were significant group differences in the presence of BPD psychopathology. The polytrauma subgroup had significantly higher rates of BPD psychopathology compared to the low/no and emotional trauma subgroups, even after controlling for other psychiatric comorbidities. Notably, though, there were no significant differences between the polytrauma subgroup and the sexual abuse subgroup. Given that individuals with BPD psychopathology are more likely to endorse histories of sexual trauma than comparison groups44, it is unsurprising that the polytrauma and sexual trauma profiles displayed the most consistent elevations of features of BPD. Surprisingly, the emotional trauma group did not differ from the low/no trauma group in the presence of BPD psychopathology despite previous research demonstrating that emotional abuse is uniquely associated with personality pathology in EDs compared to other forms of CT45. Overall, our findings suggest that elevated levels of sexual trauma or elevated levels of multiple types of trauma (polytrauma) are associated with BPD psychopathology in BN, which is consistent with studies reporting that severity of trauma is a significant predictor of various forms of psychopathology, including BPD psychopathology46–48.
In examining the relationship between severity of all CT (as a composite variable) and the presence of BPD psychopathology, results revealed that those with BN and comorbid BPD psychopathology had significantly higher levels of CT than those with BN only. This finding suggests that both the severity of specific types of trauma and the combination of different forms of trauma is associated with BPD psychopathology in BN. Further, this finding supports the hypothesis that polytrauma may me more relevant to comorbid BPD psychopathology in BN than a specific type of trauma alone or less severe occurrences of trauma. On the other hand, consistent with findings linking sexual trauma to BPD psychopathology44, the lack of significant differences in the current study between the polytrauma and sexual abuse groups in the presence of BPD psychopathology suggests that childhood sexual abuse may be equally as important.
The present findings should be interpreted in light of certain limitations. First, the assessments of trauma, BPD psychopathology, and BN are subject to the limitations of retrospective self-report (e.g., recall bias). Additionally, this sample was largely composed of Caucasian women and the results may not generalize to more diverse populations. However, there were also strengths to the current investigation, including a large sample size and thorough diagnostic interviews. Further, the use of LPA to classify participants based on trauma history in this study is innovative and provides clarification of the naturally occurring classes of traumatized individuals within those diagnosed with BN. Finally, this was the first study to examine the impact of polytrauma in childhood on the comorbidity of BN and BPD psychopathology.
In summary, the results of this study offer additional support for the role of CT in the clinical presentation of BN. Specifically, individuals with BN who have a history of childhood sexual abuse or polytrauma may be at an increased risk for displaying BPD symptomatology. Given the potential for BPD psychopathology to impact the treatment of BN, careful assessment of CT appears warranted in this population.
References
- 1.McLaughlin KA, Greif Green J, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. Arch Gen Psychiatry. 2012;69(11):1151–1160. doi: 10.1001/archgenpsychiatry.2011.2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen LP, Hassan Murad M, Paras ML, Colbenson KM, Sattler AL, Goranson EN, et al. Sexual abuse and lifetime diagnosis of psychiatric disorders: Systematic review and meta-analysis. Mayo Clin Proc. 2010;85(7):618–629. doi: 10.4065/mcp.2009.0583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Caslini M, Bartoli F, Crocamo C, Dakanalis A, Clerici M, Carra G. Disentangling the association between child abuse and eating disorders: A systematic review and meta-analysis. Psychosom Med. 2016;78(1):79–90. doi: 10.1097/PSY.0000000000000233. [DOI] [PubMed] [Google Scholar]
- 4.Groleau P, Steiger H, Bruce K, Israel M, Sycz L, Ouellette AS, et al. Childhood emotional abuse and eating symptoms in bulimic disorders: An examination of possible mediating variables. Int J Eat Disord. 2012;45(3):326–332. doi: 10.1002/eat.20939. [DOI] [PubMed] [Google Scholar]
- 5.Welch SL, Fairburn CG. Sexual abuse and bulimia nervosa: Integrated case control comparisons. Am J Psychiatry. 1994;151(3):402–407. doi: 10.1176/ajp.151.3.402. [DOI] [PubMed] [Google Scholar]
- 6.Folsom V, Krahn D, Nairn K, Gold L, Demitrack MA, Silk KR. The impact of sexual and physical abuse on eating disordered and psychiatric symptoms: A comparison of eating disordered and psychiatric inpatients. Int J Eat Disord. 1993;13(3):249–257. doi: 10.1002/1098-108x(199304)13:3<249::aid-eat2260130302>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 7.Lobbestael J, Arntz A, Bernstein DP. Disentangling the relationship between different types of childhood maltreatment and personality disorders. J Pers Disord. 2010;24(3):285–295. doi: 10.1521/pedi.2010.24.3.285. [DOI] [PubMed] [Google Scholar]
- 8.Cohen LJ, Tanis T, Bhattacharjee R, Nesci C, Halmi W, Galynker I. Are there differential relationships between different types of childhood maltreatment and different types of adult personality pathology? Psychiatry Res. 2014;215(1):192–201. doi: 10.1016/j.psychres.2013.10.036. [DOI] [PubMed] [Google Scholar]
- 9.Waxman R, Fenton MC, Skodol AE, Grant BF, Hasin D. Childhood maltreatment and personality disorders in the USA: Specificity of effects and the impact of gender. Personal Ment Health. 2014;8(1):30–41. doi: 10.1002/pmh.1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Battle CL, Shea MT, Johnson DM, Yen S, Zlotnick C, Zanarini MC, et al. Childhood maltreatment associated with adult personality disorders: Findings from the collaborative longitudinal personality disorders study. J Pers Disord. 2004;18(2):193–211. doi: 10.1521/pedi.18.2.193.32777. [DOI] [PubMed] [Google Scholar]
- 11.Bornovalova MA, Huibregtse BM, Hicks BM, Keyes M, McGue M, Iacono W. Tests of a direct effect of childhood abuse on adult borderline personality disorder traits: A longitudinal discordant twin design. J Abnorm Psychol. 2013;122(1):180–194. doi: 10.1037/a0028328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ogata SN, Silk KR, Goodrich S, Lohr NE, Westen D, Hill EM. Childhood sexual and physical abuse in adult patients with borderline personality disorder. Am J Psychiatry. 1990;147(8):1008–1013. doi: 10.1176/ajp.147.8.1008. [DOI] [PubMed] [Google Scholar]
- 13.Zanarini MC, Williams AA, Lewis RE, Reich RB, Vera SC, Marino MF, et al. Reported pathological childhood experiences associated with the development of borderline personality disorder. Am J Psychiatry. 1997;154(8):1101–1106. doi: 10.1176/ajp.154.8.1101. [DOI] [PubMed] [Google Scholar]
- 14.Zanarini MC, Frankenburg FR, Reich DB, Marino MF, Lewis RE, Williams AA, et al. Biparental failure in the childhood experience of borderline patients. J Pers Disord. 2000;14(3):264–273. doi: 10.1521/pedi.2000.14.3.264. [DOI] [PubMed] [Google Scholar]
- 15.Weaver TL, Clum GA. Early family environments and traumatic experiences associated with borderline personality disorder. J Consult Clin Psychol. 1993;61(6):1068–1075. doi: 10.1037//0022-006x.61.6.1068. [DOI] [PubMed] [Google Scholar]
- 16.Winsper C, Lereya ST, Marwaha S, Thompson A, Eyden J, Singh SP. The aetiological and psychopathological validity of borderline personality disorder in youth: A systematic review and meta-analysis. Clin Psychol Rev. 2015;44:13–24. doi: 10.1016/j.cpr.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 17.Laporte L, Paris J, Guttman H, Russell J, Correa JA. Using a sibling design to compare childhood adversities in female patients with BPD and their sisters. Child Maltreat. 2012;17(4):318–329. doi: 10.1177/1077559512461173. [DOI] [PubMed] [Google Scholar]
- 18.Martin-Blanco A, Soler J, Villalta L, Feliu-Soler A, Elices M, Perez V, et al. Exploring the interaction between childhood maltreatment and temperamental traits on the severity of borderline personality disorder. Compr Psychiatry. 2014;55(2):311–318. doi: 10.1016/j.comppsych.2013.08.026. [DOI] [PubMed] [Google Scholar]
- 19.Kuo JR, Khoury JE, Metcalfe R, Fitzpatrick S, Goodwill A. An examination of the relationship between childhood emotional abuse and borderline personality disorder features: The role of difficulties with emotion regulation. Child Abuse Negl. 2015;39:147–155. doi: 10.1016/j.chiabu.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 20.Crosby RD, Wonderlich SA, Engel SG, Simonich H, Smyth J, Mitchell JE. Daily mood patterns in bulimic behaviors in the natural environment. Behav Res Ther. 2009;47(3):181–188. doi: 10.1016/j.brat.2008.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Myers TC, Wonderlich SA, Crosby R, Mitchell JE, Steffen KJ, Smyth J, et al. Is multi-impulsive bulimia a distinct type of bulimia nervosa: Psychopathology and EMA findings. Int J Eat Disord. 2006;39(8):655–661. doi: 10.1002/eat.20324. [DOI] [PubMed] [Google Scholar]
- 22.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: APA Press; 2013. [Google Scholar]
- 23.Reas DL, Rø Ø, Karterud S, Hummelen B, Pedersen G. Eating disorders in a large clinical sample of men and women with personality disorders. Int J Eat Disord. 2013;46(8):801–809. doi: 10.1002/eat.22176. [DOI] [PubMed] [Google Scholar]
- 24.Godt K. Personality disorders in 545 patients with eating disorders. Eur Eat Disord Rev. 2008;16(2):94–99. doi: 10.1002/erv.844. [DOI] [PubMed] [Google Scholar]
- 25.Cassin S, von Ranson K. Personality and eating disorders: A decade in review. Clin Psychol Rev. 2005;25(7):895–916. doi: 10.1016/j.cpr.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 26.Vitousek K, Manke F. Personality variables and disorders in anorexia nervosa and bulimia nervosa. J Abnorm Psychol. 1994;103(1):137–147. doi: 10.1037//0021-843x.103.1.137. [DOI] [PubMed] [Google Scholar]
- 27.Waller G. Sexual abuse and eating disorders. Borderline personality as a mediating factor? Br J Psychiatry. 1993;162:771–775. doi: 10.1192/bjp.162.6.771. [DOI] [PubMed] [Google Scholar]
- 28.Steiger H, Jabalpurwala S, Champagne J. Axis II comorbidity and developmental adversity in bulimia nervosa. J Nerv Ment Dis. 1996;184(9):555–560. doi: 10.1097/00005053-199609000-00007. [DOI] [PubMed] [Google Scholar]
- 29.Steiger H, Leonard S, Ng Ying Kin NMK, Ladouceur C, Dhunraj R, Young SN. Childhood abuse and platelet tritiated-paroxetine binding in bulimia nervosa: Implications of borderline personality disorder. J Clin Psychiatry. 2000;61(6):428–435. doi: 10.4088/jcp.v61n0607. [DOI] [PubMed] [Google Scholar]
- 30.Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the adverse childhood experiences study. Am J Psychiatry. 2003;160(8):1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- 31.Kellogg ND, Menard SW. Violence among family members of children and adolescents evaluated for sexual abuse. Child Abuse Negl. 2003;27(12):1367–1376. doi: 10.1016/j.chiabu.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 32.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: APA Press; 1994. (DSM-IV) [Google Scholar]
- 33.First MB, Spitzer RL, Gibbon M, Williams J. Structured Clinical Interview for DSM–IV Axis I Disorders: Patient Edition (SCID I/P) New York: Biometrics; 1995. [Google Scholar]
- 34.Zanarini M, Frankenburg F, Vujanovic A. Inter-rater and test-retest reliability of the Revised Diagnostic Interview for Borderlines. J Pers Disord. 2002;16(3):270–276. doi: 10.1521/pedi.16.3.270.22538. [DOI] [PubMed] [Google Scholar]
- 35.Zanarini M, Gunderson J, Frankenburg F, Chauncey D. The revised diagnostic interview for borderlines: Discriminating BPD from other axis II disorders. J Pers Disord. 1989;3:10–18. [Google Scholar]
- 36.Bernstein D, Fink L. Childhood trauma questionnaire: Manual. San Antonio: The Psychological Corporation; 1998. [Google Scholar]
- 37.Spinhoven P, Penninx BW, Hickendorff M, van Hemert AM, Bernstein DP, Elzinga BM. Childhood trauma questionnaire: Factor structure, measurement invariance, and validity across emotional disorders. Psychol Assess. 2014;26(3):717–729. doi: 10.1037/pas0000002. [DOI] [PubMed] [Google Scholar]
- 38.Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse Negl. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 39.Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, et al. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. J Consult Clin Psychol. 2007;75(4):629–638. doi: 10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- 40.Vermunt JK, Magidson J. Latent GOLD 4.0. User's Guide. Belmont, MA: Statistical Innovations, Inc; 2005. [Google Scholar]
- 41.Bozdogan H. Model selection and Akaike’s information criterion (AIC): The general theory and its analytic extensions. Psychometrika. 1987;52:345–370. [Google Scholar]
- 42.Schwarz G. Estimating the dimension of a model. Ann Stat. 1978;6:461–464. [Google Scholar]
- 43.Sclove LS. Application of model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52:333–343. [Google Scholar]
- 44.Yen S, Shea MT, Battle CL, Johnson DM, Zlotnick C, Dolan-Sewell R, et al. Traumatic exposure and posttraumatic stress disorder in borderline, schizotypal, avoidant, and obsessive-compulsive personality disorders: Findings from the Collaborative Longitudinal Personality Disorders Study. J Nerv Ment Dis. 2002;190(8):510–518. doi: 10.1097/00005053-200208000-00003. [DOI] [PubMed] [Google Scholar]
- 45.Grilo CM, Masheb RM. Childhood maltreatment and personality disorders in adult patients with binge eating disorder. Acta Psychiatr Scand. 2002;106(3):183–188. doi: 10.1034/j.1600-0447.2002.02303.x. [DOI] [PubMed] [Google Scholar]
- 46.Bandelow B, Krause J, Wedekind D, Broocks A, Hajak G, Ruther E. Early traumatic life events, parental attitudes, family history, and birth risk factors in patients with borderline personality disorder and healthy controls. Psychiatry Res. 2005;134(2):169–179. doi: 10.1016/j.psychres.2003.07.008. [DOI] [PubMed] [Google Scholar]
- 47.Bulik CM, Prescott CA, Kendler KS. Features of childhood sexual abuse and the development of psychiatric and substance use disorders. Br J Psychiatry. 2001;179:444–449. doi: 10.1192/bjp.179.5.444. [DOI] [PubMed] [Google Scholar]
- 48.Zanarini MC, Yong L, Frankenburg FR, Hennen J, Reich DB, Marino MF, et al. Severity of reported childhood sexual abuse and its relationship to severity of borderline psychopathology and psychosocial impairment among borderline inpatients. J Nerv Ment Dis. 2002;190:381–387. doi: 10.1097/00005053-200206000-00006. [DOI] [PubMed] [Google Scholar]