Abstract
Background
Long courses of oral corticosteroids are commonly used in children in the management of chronic conditions. Various adverse drug reactions (ADRs) are known to occur with their use. This systematic review aimed to identify the most common and serious ADRs and to determine their relative risk levels.
Methods
A literature search of Embase, Medline, International Pharmaceutical Abstracts, CINAHL, Cochrane Library and PubMed was performed with no language restrictions in order to identify studies where oral corticosteroids were administered to patients aged 28 days to 18 years of age for at least 15 days of treatment. Each database was searched from their earliest dates to January 2016. All studies providing clear information on ADRs were included.
Results
One hundred and one studies including 33 prospective cohort studies; 21 randomised controlled trials; 21 case series and 26 case reports met the inclusion criteria. These involved 6817 children and reported 4321 ADRs. The three ADRs experienced by the highest number of patients were weight gain, growth retardation and Cushingoid features with respective incidence rates of 21.1%, 18.1% and 19.4% of patients assessed for these ADRs. 21.5% of patients measured showed decreased bone density and 0.8% of patients showed osteoporosis. Biochemical HPA axis suppression was detected in 269 of 487 patients where it was measured. Infection was the most serious ADR, with twenty one deaths. Varicella zoster was the most frequent infection (9 deaths).
Conclusions
Weight gain, growth retardation and Cushingoid features were the most frequent ADRs seen when long-course oral corticosteroids were given to children. Increased susceptibility to infection was the most serious ADR.
Introduction
Corticosteroids are used widely for their immunosuppressant and anti-inflammatory properties. They may be used individually or in combination with other drugs and are prescribed in both short and long courses depending on the condition being treated and the response of the patient [1]. The adverse effects from short-course use have been described recently and include changes in mood and behaviour, vomiting and sleep disturbance [2]. Long-course use of corticosteroids may lead to additional side effects [3]. Many of the side effects are reversible if the medication is stopped, while others may be permanent [4][5].
It is known that higher doses of corticosteroids, particularly when used for prolonged courses can cause hypothalamic-pituitary-adrenal axis (HPA axis) suppression. This can result in increased susceptibility to infections including viral infections such as varicella zoster, bacterial infections such as cellulitis and fungal infections such as candida, tinea, etc. [6].
The risk of specific adverse drug reactions (ADRs) following long term corticosteroids in children is unknown and these effects are of major concern. We therefore performed a systematic review to determine the toxicity associated with long course oral corticosteroids, to identify the most common and serious ADRs and to determine their relative risk levels. We defined long-course oral corticosteroids as use for at least 15 days.
Methods
A systematic literature search was performed to identify all papers describing toxicity of corticosteroids in children. Six databases were searched up to January 2016: MEDLINE, EMBASE, International Pharmaceutical Abstracts, CINAHL, Cochrane Library and PubMed. The databases were searched separately and combined together to remove duplications. The search strategy included all languages and involved the keywords "prednis* or dexamethasone or betamethasone" which are the most frequent medications given orally to children for long periods. "Corticosteroid" was added to cover all other oral corticosteroid medication. The keywords "toxicity* or adverse drug reaction* or adverse event* or side effect* or adverse effect*" were used as recommended by the BMC Medical Research Methodology for systematic reviews of adverse effects [7]. Additionally, the keyword ‘‘safety*”, was used as in a previous systematic review [8]. The terms recommended by search strategies for Medline were used to cover the paediatric age group ‘‘child* or children* or p*ediatric* or infant* or adolescent*” [9]. The terms neonate, newborn and gestation were excluded. The keywords: oral, tablet, syrup and PO (abbreviation meaning by mouth) were used to cover all possibilities of oral administration of corticosteroids.
Inclusion criteria were original research studies assessing corticosteroid toxicity in children from 28 days up to 18 years of age. These included randomised controlled trials (RCTs), case series, case reports, cohort studies and letters. Five percent of randomly selected abstracts were independently assessed for eligibility by a second reviewer for assurance that no relevant studies were missed. Data including the number of patients, drug name, duration, diagnosis, number and type of ADRs were extracted.
Exclusion criteria included; review articles, editorials, studies that did not give ADR data, studies in adults, studies involving adults and children where paediatric data was not presented separately and studies in which corticosteroids were not given orally and/or were administered for less than 15 days.
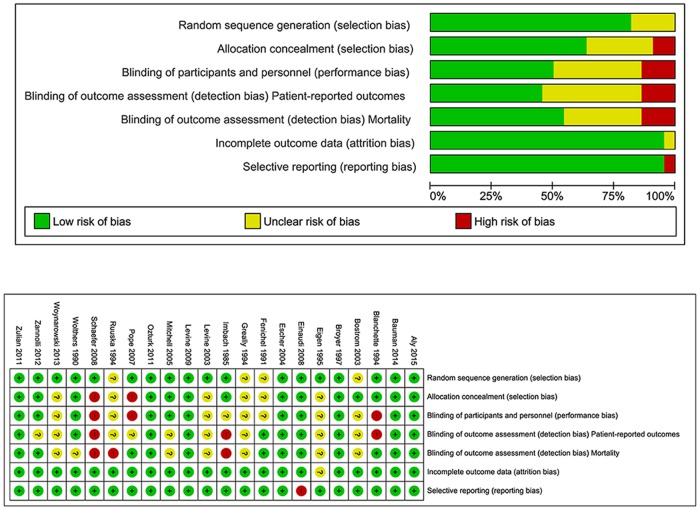
The quality of included RCTs was assessed using the Cochrane collaborations tool for assessing risk of bias in randomised trials [10]. Any study showing a high risk of bias on three or more parameters was thereafter excluded. Prospective cohort studies were assessed using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist [11], where a score of over 70% is required for inclusion. Other studies were quality assessed using the Health Technology Assessment checklist [12]. All studies achieving at least satisfactory criteria were included. All quality assessments were independently assessed for eligibility and scored by two reviewers using a specially designed form. Any discrepancies were resolved by a third reviewer.
The incidence of ADRs was calculated from the RCTs and prospective cohort studies when more than one study reported the ADR.
Meta-analysis of included RCTs was performed using RevMan 5.3, software provided by Cochrane, used for organising the quality assessment for RCTs and for carrying out meta-analysis. Chi2 analysis of the difference between treatment duration periods (short- and long-course) was performed for the discussion section. P-values <0.05 were considered statistically significant.
Results
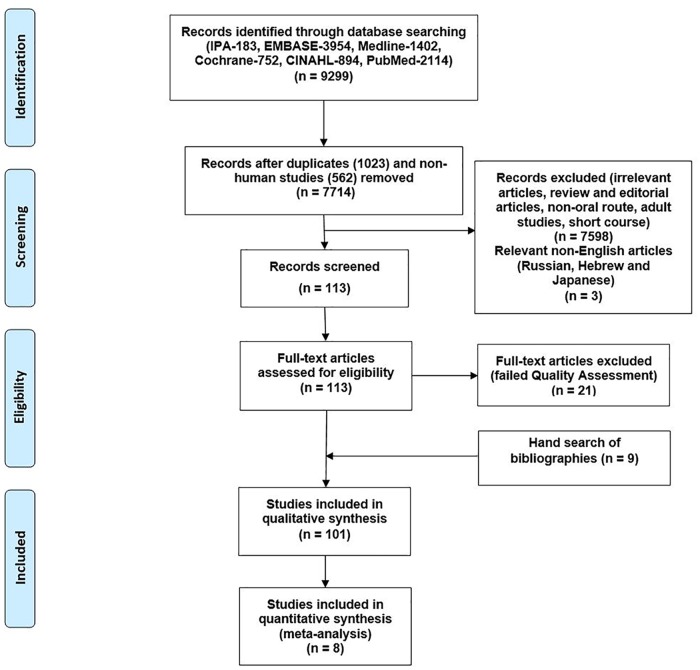
7,714 articles were identified in total. 101 articles met the inclusion criteria after nine papers were added from manual searches of bibliographies, [13–33] [34–66] [67–87] [88–113] (S1 Appendix 1). The remaining articles were excluded for the reasons shown in Fig 1. Twenty one articles were excluded after quality assessment. Only one RCT contained four criteria with high risks of bias, and this study was excluded from the results [114] (Schaefer 2008, Fig 2). Twelve studies scoring < 70% in the STROBE checklist (range 30–57.5%) were excluded [115–126]. Eight case series were excluded for poor ratings in the Health Technology Assessment checklist [127–134].
Fig 1. Flow chart of the literature search performed (PRISMA flow diagram).
Fig 2. Risk of bias summary and graph.
Corticosteroids were used to manage a wide variety of medical conditions, of which the most common were leukaemia, haemangioma, asthma, nephrotic syndrome, cystic fibrosis and Crohn’s disease. Prednisolone and dexamethasone were the most commonly used drugs.
The studies included a total of 6817 patients and 4321 ADRs (Table 1). RCTs accounted for over half of the studies and patients (n = 3484) and one third (34.8%) of ADRs [13–33]. The 33 prospective cohort studies included 43% of patients (n = 2936) but reported half of the ADRs [34–66]. Prospective cohort studies detected more ADRs per patient than RCTs.
Table 1. Summary of included articles.
| Type of Study | No. of Studies | No. of Patients | Total | No. of ADRs | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pred | Dexa | Bud | Methyl | Def | Beta | Pred | Dexa | Bud | Methyl | Def | Beta | ||||
| RCT* | 21 | 1947 | 1352 | 130 | 22 | 20 | 13 | 3484 | 946 | 220 | 226 | 32 | 52 | 21 | 1497 |
| Prospective Cohort Studies (PCS) | 33 | 2834 | 102 | - | - | - | - | 2936 | 1795 | 355 | - | - | - | - | 2150 |
| Case Series (CS) | 21 | 255 | 66 | 23 | 21 | - | - | 365 | 335 | 203 | 26 | 42 | - | - | 606 |
| Case Report (CR) | 26 | 28 | 3 | 1 | - | - | - | 32 | 60 | 6 | 2 | - | - | - | 68 |
| Total | 101 | 5064 | 1523 | 154 | 43 | 20 | 13 | 6817 | 3136 | 784 | 254 | 74 | 52 | 21 | 4321¶ |
Abbreviation: Pred, Prednisolone; Dex, Dexamethasone; Bud, Budesonide; Methyl, Methylprednisolone; Def, Deflazacort; Beta, Betamethasone.
* Only data from patients taking oral corticosteroids were included.
¶Some patients had more than one adverse drug reaction
Forty two studies looked for all possible symptomatic ADRs [13–28,30–41,44,47,48,52,53,55–62,64]. Fourteen of them also evaluated HPA axis suppression specifically [14–16,22,32,36,41,51–53,55–58]. Twenty five measured the weight [13,14,16–18,20–27,30–34,38,39,41,57–59,62], nineteen measured growth [19–22,27,30,32–35,37–41,57,59,61,62], eighteen evaluated blood pressure [20–22,24,27,31–35,37–39,44,47,59,60,62], fourteen evaluated blood glucose [20–22,26–28,30–33,39,59,60,62], and one measured bone mineral density [21].
Three studies evaluated HPA axis suppression only [29][54][66].
Two studies evaluated behavioural change and sleep disturbance only [50][65].
One study evaluated both blood pressure and osteoporosis [49].
One study measured weight only [46].
One study measured bone mineral density only [42].
One study evaluated infection only [63].
Thirty six different ADRs were reported from the RCTs and prospective cohort studies (Tables 2 and 3). In terms of numbers of patients experiencing them the three most common ADRs were weight gain, growth retardation and Cushingoid features, affecting between 21.1 to 18.1% of children.
Table 2. Observed/reported ADRs from RCTs and prospective cohort studies.
| Adverse effects | No. of pt with ADRs¶ | No. of studies reporting ADR | Denominators | Incidence (%) | |
|---|---|---|---|---|---|
| No. of studies looking for ADR | Total no. of patients | ||||
| Cushingoid features | 353 | 16 | 20 | 1817 | 19.4 |
| Increased appetite | 42 | 3 | 8 | 227 | 18.5 |
| Gastrointestinal upset | 86 | 6 | 16 | 543 | 15.8 |
| Hirsutism | 42 | 5 | 9 | 347 | 12.1 |
| Acne | 34 | 6 | 8 | 314 | 10.8 |
| Gastric wall abnormality | 163 | 5 | 16 | 1573 | 10.4 |
| Insomnia | 153 | 9 | 16 | 1538 | 9.9 |
| Skin atrophy | 123 | 2 | 9 | 1356 | 9.1 |
| Infection | 278 | 22 | 33 | 3203 | 8.7 |
| Behavioural changes | 257 | 14 | 19 | 3164 | 8.1 |
| Rash | 20 | 2 | 10 | 342 | 5.8 |
| Skin striae | 12 | 4 | 8 | 270 | 4.4 |
| Headache | 15 | 3 | 8 | 349 | 4.3 |
| Fever | 9 | 2 | 8 | 285 | 3.2 |
| Myopathy | 89 | 6 | 10 | 2974 | 3.0 |
| Hair loss | 6 | 2 | 6 | 217 | 2.8 |
| Bruising easily | 5 | 2 | 5 | 226 | 2.2 |
| Fatigue | 58 | 4 | 10 | 2974 | 2.0 |
| Peripheral oedema | 2 | 2 | 8 | 254 | 0.8 |
| Hypopigmentation | 108 | 1 | - | - | - |
| Anorexia | 3 | 1 | - | - | - |
| Ulceration (arterial bleed) | 1 | 1 | - | - | - |
| Unknown | 11 | 2 | - | - | - |
¶Some patients had more than one adverse drug reaction
Table 3. ADRs from RCTs and prospective cohort studies requiring specific measurements.
| Adverse effects | No. of pt with ADRs¶ | No. of studies reporting ADR | Denominators | Incidence (%) | |
|---|---|---|---|---|---|
| No. of studies looking for ADR | Total no. of patients | ||||
| HPA axis suppression | 267 | 17 | 17 | 456 | 58.6 |
| Decreased bone density | 197 | 2 | 2 | 917 | 21.5 |
| Weight gain | 556 | 21 | 26 | 2636 | 21.1 |
| Growth retardation | 358 | 13 | 21 | 1983 | 18.1 |
| Cataracts | 25 | 5 | 8 | 424 | 5.9 |
| Hypertension | 176 | 14 | 19 | 3164 | 5.6 |
| Hyperglycaemia | 112 | 7 | 14 | 3272 | 3.4 |
| Weight loss | 33 | 3 | 26 | 2636 | 1.3 |
| Osteoporosis | 21 | 5 | 5 | 2552 | 0.8 |
| Avascular necrosis | 18 | 2 | 2 | 2663 | 0.7 |
| Pancreatitis | 9 | 1 | - | - | - |
| Hypernatraemia | 3 | 1 | - | - | - |
| Hypokalaemia | 1 | 1 | - | - | - |
| Hypercholesterolaemia | 1 | 1 | - | - | - |
¶Some patients had more than one adverse drug reaction
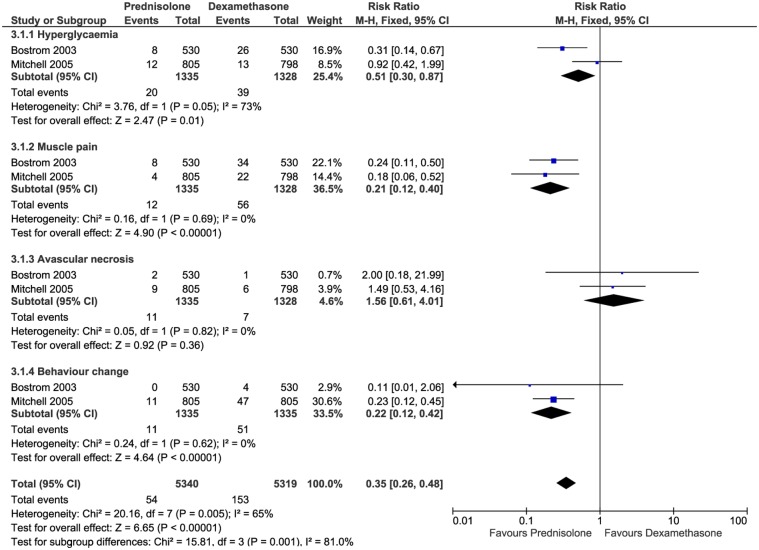
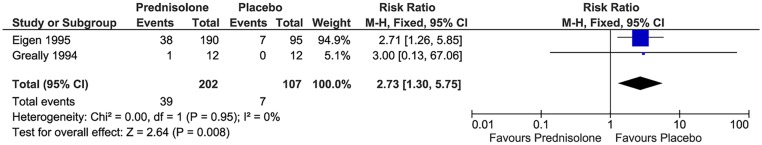
Six RCTs and one prospective cohort study reported that 112 children experienced hyperglycaemia during treatment periods (incidence 3.4%) [20,22,27,28,30,31,60]. Two cases series and two case reports also reported 22 children who experienced hyperglycaemia [67][76][90][92]. The risk of hyperglycaemia was more frequent among older children (>10 years) [27][28]. Some patients with leukaemia and nephrotic syndrome required daily insulin [27][28][90]. Meta-analysis across two RCTs [27][28] showed statistically significant hyperglycaemia associated with oral dexamethasone compared to oral prednisolone in leukaemic patients (Fixed model, I2 = 73%, P = 0.01, RR = 0.51). (Fig 3). Meta-analysis across two RCTs [30][31] showed statistically significant hyperglycaemia associated with oral prednisolone compared to placebo in cystic fibrosis patients (Fixed model, I2 = 0%, P = 0.008, RR = 2.73). (Fig 4).
Fig 3. Relative risk of ADRs between prednisolone and dexamethasone for leukaemia patients.
Fig 4. Relative risk of hyperglycaemia between prednisolone and placebo in cystic fibrosis patients.
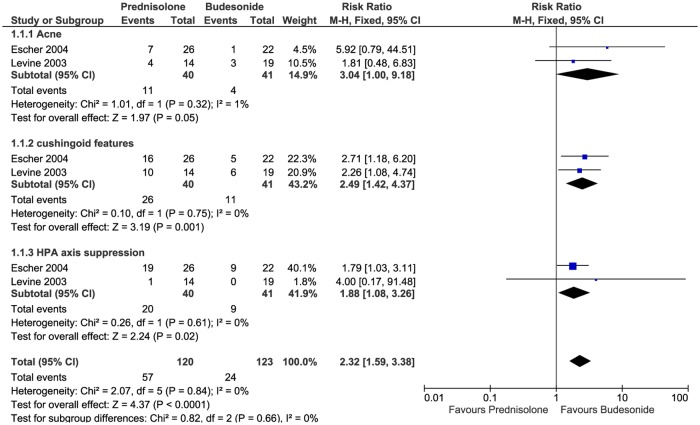
Seventeen studies (eleven prospective cohort studies and six RCTs) and two case series specifically evaluated the HPA axis [14–16,22,29,32,36,41,51–58,66,81,84] 269 of the 487 patients tested showed biochemical HPA axis suppression. Meta-analysis across two RCTs [14][15] showed statistically significant biochemical HPA axis suppression associated with oral prednisolone compared to oral budesonide (Fixed model, I2 = 0%, P = 0.02, RR = 1.88). (Fig 5). Some patients did not achieve adequate adrenal function (cortisol level >18 μg/dL) until eight weeks after completion of therapy with dexamethasone [57]. Also some children still had adrenal suppression (cortisol level <18 μg/dL) after withdrawal of dexamethasone for up to 4–8 months [58]. One infant with a haemangioma withdrew from treatment with oral prednisolone due to adrenal crisis [36].
Fig 5. Relative risk of ADRs between prednisolone and budesonide in crohn's disease patients.
Twenty six RCTs and cohort studies evaluated weight changes in patients (Table 3). Thirteen case series and case reports also reported 49 children experiencing weight gain (Table 4). Weight was measured in patients with idiopathic thrombocytopenic purpura (ITP) in two RCTs [17][18], three case series [72–74] and one case report [101]. The majority of patients had significant weight increase of 6% to 10% during oral corticosteroid treatment.
Table 4. ADRs from case series and case reports.
| Adverse effects | No. of pt with ADRs¶ | No. of studies reporting ADR |
|---|---|---|
| Cushingoid features | 120 | 21 |
| Behavioural changes | 105 | 10 |
| Increased appetite | 83 | 4 |
| Weight gain | 49 | 13 |
| Hypertension | 36 | 8 |
| Infection | 29 | 10 |
| Growth retardation | 27 | 10 |
| Gastrointestinal upset | 23 | 4 |
| Hyperglycaemia | 22 | 4 |
| Fatigue | 21 | 3 |
| Hypokalaemia | 19 | 1 |
| Myopathy | 17 | 4 |
| Insomnia | 16 | 3 |
| Headache | 15 | 4 |
| Cataracts | 14 | 3 |
| Gastric wall abnormalities | 11 | 6 |
| Osteoporosis | 10 | 6 |
| Dizziness | 8 | 2 |
| Oedema | 8 | 2 |
| Acne | 7 | 4 |
| Skin striae | 7 | 3 |
| Hirsutism | 5 | 4 |
| HPA axis suppression | 2 | 2 |
| Fever | 2 | 2 |
| Pigmentation | 1 | 1 |
| Rash | 1 | 1 |
| Increased intraocular pressure | 1 | 1 |
| Pancreatitis | 1 | 1 |
| Obstructive sleep apnoea | 1 | 1 |
| Oral Ulceration | 1 | 1 |
| Hypocalcaemia | 1 | 1 |
| Unknown | 11 | 1 |
| Total | 674 | 47 |
¶Some patients had more than one adverse drug reaction
Thirty one different ADRs were reported from case series and case reports with a total of 674 ADRs in 397 patients (Table 4). [67–87] [88–113].
In total, 43 patients died during treatment with oral corticosteroids (Table 5). Sixteen cohort studies and six RCTs reported that 278 children experienced infection during treatment periods (incidence 8.7%). Five studies reported 21 patients who died due to infection [28][63][89][96][106]. Infection was the commonest cause of death, accounting for half of the deaths. The majority of the children (nine patients) died after admission to intensive care with varicella zoster virus. Seven of these patients received oral prednisolone [28][63][89][96], and two leukaemic patients received oral dexamethasone [28][106]. Another two children with Kearns-Sayre syndrome died from hyperglycaemia after receiving oral prednisolone [92]. Twenty children (six prednisolone, 14 dexamethasone) with leukaemia died due to unknown reasons [27]. (Table 5).
Table 5. ADRs that led to death or drug discontinuation.
| Causes | Discontinue | Death |
|---|---|---|
| Infection | 2 | 21 |
| Hyperglycaemia | - | 2 |
| Behaviour changes | 9 | - |
| Growth retardation | 4 | - |
| Cushingoid features | 4 | - |
| Hypertension | 2 | - |
| Ulceration | 2 | - |
| HPA axis suppression | 1 | - |
| Vomiting | 1 | - |
| Increased intraocular pressure | 1 | - |
| Obstructive sleep apnoea | 1 | - |
| Unknown ADRs | 65 | 20 |
| Total | 92 | 43 |
Behavioural changes were one of the most common causes for medication withdrawal, reported in three studies with nine leukaemia patients, all of whom were treated with oral dexamethasone [27][28][98]. Additionally growth retardation in four infants with haemangioma led to discontinuation of oral prednisolone [32]. (Table 5).
Discussion
Forty three patients died during treatment with oral corticosteroids. Infection was the most serious ADR and was responsible for half of the deaths. The incidence of infection with short course oral corticosteroids in children has previously been reported as (0.9%) [2]. It was significantly higher (8.7%) with long course treatment (P <0.0001). It is already well known that the immunosuppressant effects of corticosteroids in supra-physiological doses can lead to patients having increased susceptibility to infection, to deterioration in those with existing infections or to activation of latent infection [135]. To compound this their anti-inflammatory effects may mask symptoms and allow infections to progress significantly before detection. We believe this is the first study to quantify this greatly increased incidence of infection in patients on long-course rather than short-course oral corticosteroids.
Hyperglycaemia was another serious side effect associated with long courses of oral corticosteroids. There were no differences between the incidence of this ADR during short and long course treatment [2]. The risk during short course corticosteroids however was transient and resolved shortly after discontinuing the medication without intervention, however during long course treatment some patients needed daily insulin [27][28][90].
Behavioural change was twice as common during long course treatment (8.1%) compared with short course (4.7%) [2] and this difference was significant (P <0.0001). Treatment withdrawal and medication intervention were often required with long course treatment. Psychiatric ADRs ranging from insomnia to mood change and dementia have also been reported in adult patients [136][137]. The incidence of behavioural change in adults was reported as 5.7% in a review written in 1983 [138]. Our study suggests that behavioural problems may be more common in children.
The risk of HPA axis suppression during long course corticosteroids was greater with dexamethasone than prednisolone in leukaemia patients [29,51–58]. Also suppression was greater with oral corticosteroids (66% of patients) than inhaled corticosteroids (31% of patients) in asthmatic patients [66]. The suppression reported during the long course corticosteroids studies was severe and led to adrenal crisis. Fourteen patients with HPA axis suppression during long course treatment needed months to regain adequate adrenal function [36][57][58]. On the other hand, all the children with HPA axis suppression during short course treatment returned to a normal level of endogenous cortisol secretion within 10–12 days after discontinuation of the corticosteroids [2].
The three most commonly observed ADRs associated with long-course oral corticosteroids were weight gain, growth retardation and cushingoid features.
Weight gain was the most common side effect. This was not however significantly different to that reported for short-course corticosteroid treatment [2]. The risk of this ADR was greater with prednisolone than budesonide in children [26]. In adult patients weight gain was associated with longer duration of corticosteroids use, even with low-dose [139].
Growth retardation was the second most frequently observed side effect. The risk of this ADR was significantly greater with prednisolone than intravenous methylprednisolone [22]. Also the risk was significantly greater with boys than girls [43]. Comparing oral corticosteroids with inhaled corticosteroids (ICS), one study found that inhaled medication is significantly better than oral in terms of growth retardation [140]. This ADR has not been reported during short-course corticosteroid treatment. [2]
Cushingoid features were the third most frequently observed side effect caused by oral corticosteroids. The risk of this ADR was significantly greater with prednisolone than budesonide [14][15] (Fig 5). This ADR was not reported during short-course corticosteroids treatment [2]. In adult patients Cushingoid features were associated with longer duration of corticosteroids use, even with low-dose [139].
Hypertension was another side effect associated with long courses of oral corticosteroids occurring in 5.6% patients. This ADR was severe in some patients and occasionally needed medical intervention. Two infants stopped their medication because of this ADR and another eight required antihypertensive medication [22][38][70][109].
The prevalence of overall ADRs associated with long course corticosteroid use was high, and this finding may be underappreciated by clinicians. Because parents and patients may be concerned about the potential ADRs of corticosteroids prior to use, physicians need to be well apprised of their relative risks.
In conclusion this systematic review showed that the most serious ADR associated with long-course oral corticosteroids was infection reported in 9% patients and resulting in 21 deaths. The most frequent ADRs were weight gain, growth retardation and cushingoid features. Behavioural changes were the main reason for treatment discontinuation.
Registration number
CRD42014010501
By PROSPERO International prospective register of systematic reviews
Supporting Information
(DOCX)
(DOCX)
Acknowledgments
We would like to thank Janine Abramson and Coral Smith for assisting with the quality assessment of the articles.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work. Fahad Aljebab is a postgraduate student and would like to acknowledge his sponsor the Saudi Arabian government (Prince Mohammed Medical City). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Williams KW, Andrews AL, Heine D, Russell WS, Titus MO. Parental preference for short- versus long-course corticosteroid therapy in children with asthma presenting to the pediatric emergency department. Clin Pediatr (Phila). 2013;52: 30–4. [DOI] [PubMed] [Google Scholar]
- 2.Aljebab F, Choonara I, Conroy S. Systematic review of the toxicity of short-course oral corticosteroids in children. Arch Dis Child. 2016;101: 365–70. 10.1136/archdischild-2015-309522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Citterio F. Steroid side effects and their impact on transplantation outcome. Transplantation. 2001;72: S75–80. [PubMed] [Google Scholar]
- 4.Hunder GG, Sheps SG, Allen GL, Joyce JW. Daily and alternate-day corticosteroid regimens in treatment of giant cell arteritis: comparison in a prospective study. Ann Intern Med. 1975;82: 613–8. [DOI] [PubMed] [Google Scholar]
- 5.REICHLING GH, KLIGMAN AM. Alternate-day corticosteroid therapy. Arch Dermatol. 1961;83: 980–3. [DOI] [PubMed] [Google Scholar]
- 6.Katzung BG, Masters SB, Trevor AJ. Basic and Clinical Pharmacology, 11th Edition New York: McGraw-Hill Education; 2009. [Google Scholar]
- 7.Loke YK, Price D, Herxheimer A. Systematic reviews of adverse effects: framework for a structured approach. BMC Med Res Methodol. 2007;7: 32 10.1186/1471-2288-7-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Egunsola O, Adefurin A, Fakis A, Jacqz-Aigrain E, Choonara I, Sammons H. Safety of fluconazole in paediatrics: a systematic review. Eur J Clin Pharmacol. Springer Berlin Heidelberg; 2013;69: 1211–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kastner M, Wilczynski NL, Walker-Dilks C, McKibbon KA, Haynes B. Age-specific search strategies for Medline. J Med Internet Res. 2006;8: e25 10.2196/jmir.8.4.e25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343: d5928 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335: 806–8. 10.1136/bmj.39335.541782.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hailey D. Toward transparency in health technology assessment: a checklist for HTA reports. Int J Technol Assess Health Care. 2003;19: 1–7. [DOI] [PubMed] [Google Scholar]
- 13.Ruuska T, Savilahti E, Mäki M, Ormälä T, Visakorpi JK. Exclusive whole protein enteral diet versus prednisolone in the treatment of acute Crohn’s disease in children. J Pediatr Gastroenterol Nutr. 1994;19: 175–80. [DOI] [PubMed] [Google Scholar]
- 14.Levine A, Weizman Z, Broide E, Shamir R, Shaoul R, Pacht A, et al. A comparison of budesonide and prednisone for the treatment of active pediatric Crohn disease. J Pediatr Gastroenterol Nutr. 2003;36: 248–52. [DOI] [PubMed] [Google Scholar]
- 15.Escher JC. Budesonide versus prednisolone for the treatment of active Crohn’s disease in children: a randomized, double-blind, controlled, multicentre trial. Eur J Gastroenterol Hepatol. 2004;16: 47–54. [DOI] [PubMed] [Google Scholar]
- 16.Levine A, Kori M, Dinari G, Broide E, Shaoul R, Yerushalmi B, et al. Comparison of two dosing methods for induction of response and remission with oral budesonide in active pediatric Crohn’s disease: a randomized placebo-controlled trial. Inflamm Bowel Dis. 2009;15: 1055–61. 10.1002/ibd.20881 [DOI] [PubMed] [Google Scholar]
- 17.Imbach P, Wagner HP, Berchtold W, Gaedicke G, Hirt A, Joller P, et al. Intravenous immunoglobulin versus oral corticosteroids in acute immune thrombocytopenic purpura in childhood. Lancet. 1985;2: 464–8. [DOI] [PubMed] [Google Scholar]
- 18.Blanchette V, Imbach P, Andrew M, Adams M, McMillan J, Wang E, et al. Randomised trial of intravenous immunoglobulin G, intravenous anti-D, and oral prednisone in childhood acute immune thrombocytopenic purpura. Lancet. 1994;344: 703–7. [DOI] [PubMed] [Google Scholar]
- 19.Wolthers OD, Pedersen S. Short term linear growth in asthmatic children during treatment with prednisolone. BMJ. 1990;301: 145–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fenichel GM, Mendell JR, Moxley RT, Griggs RC, Brooke MH, Miller JP, et al. A comparison of daily and alternate-day prednisone therapy in the treatment of Duchenne muscular dystrophy. Arch Neurol. 1991;48: 575–9. [DOI] [PubMed] [Google Scholar]
- 21.Broyer M, Terzi F, Lehnert A, Gagnadoux MF, Guest G, Niaudet P. A controlled study of deflazacort in the treatment of idiopathic nephrotic syndrome. Pediatr Nephrol. 1997;11: 418–22. [DOI] [PubMed] [Google Scholar]
- 22.Pope E, Krafchik BR, Macarthur C, Stempak D, Stephens D, Weinstein M, et al. Oral versus high-dose pulse corticosteroids for problematic infantile hemangiomas: a randomized, controlled trial. Pediatrics. 2007;119: e1239–47. 10.1542/peds.2006-2962 [DOI] [PubMed] [Google Scholar]
- 23.Zulian F, Martini G, Vallongo C, Vittadello F, Falcini F, Patrizi A, et al. Methotrexate treatment in juvenile localized scleroderma: a randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2011;63: 1998–2006. 10.1002/art.30264 [DOI] [PubMed] [Google Scholar]
- 24.Ozturk F, Bakirtas A, Ileri F, Turktas I. Efficacy and tolerability of systemic methylprednisolone in children and adolescents with chronic rhinosinusitis: a double-blind, placebo-controlled randomized trial. J Allergy Clin Immunol. 2011;128: 348–52. 10.1016/j.jaci.2011.04.045 [DOI] [PubMed] [Google Scholar]
- 25.Zannolli R, Buoni S, Betti G, Salvucci S, Plebani A, Soresina A, et al. A randomized trial of oral betamethasone to reduce ataxia symptoms in ataxia telangiectasia. Mov Disord. 2012;27: 1312–6. 10.1002/mds.25126 [DOI] [PubMed] [Google Scholar]
- 26.Woynarowski M, Nemeth A, Baruch Y, Koletzko S, Melter M, Rodeck B, et al. Budesonide versus prednisone with azathioprine for the treatment of autoimmune hepatitis in children and adolescents. J Pediatr. 2013;163: 1347–53.e1. 10.1016/j.jpeds.2013.05.042 [DOI] [PubMed] [Google Scholar]
- 27.Mitchell CD, Richards SM, Kinsey SE, Lilleyman J, Vora A, Eden TOB. Benefit of dexamethasone compared with prednisolone for childhood acute lymphoblastic leukaemia: results of the UK Medical Research Council ALL97 randomized trial. Br J Haematol. 2005;129: 734–45. 10.1111/j.1365-2141.2005.05509.x [DOI] [PubMed] [Google Scholar]
- 28.Bostrom BC, Sensel MR, Sather HN, Gaynon PS, La MK, Johnston K, et al. Dexamethasone versus prednisone and daily oral versus weekly intravenous mercaptopurine for patients with standard-risk acute lymphoblastic leukemia: a report from the Children’s Cancer Group. Blood. 2003;101: 3809–17. 10.1182/blood-2002-08-2454 [DOI] [PubMed] [Google Scholar]
- 29.Einaudi S, Bertorello N, Masera N, Farinasso L, Barisone E, Rizzari C, et al. Adrenal axis function after high-dose steroid therapy for childhood acute lymphoblastic leukemia. Pediatr Blood Cancer. 2008;50: 537–41. 10.1002/pbc.21339 [DOI] [PubMed] [Google Scholar]
- 30.Eigen H, Rosenstein BJ, FitzSimmons S, Schidlow DV. A multicenter study of alternate-day prednisone therapy in patients with cystic fibrosis. Cystic Fibrosis Foundation Prednisone Trial Group. J Pediatr. 1995;126: 515–23. [DOI] [PubMed] [Google Scholar]
- 31.Greally P, Hussain MJ, Vergani D, Price JF. Interleukin-1 alpha, soluble interleukin-2 receptor, and IgG concentrations in cystic fibrosis treated with prednisolone. Arch Dis Child. 1994;71: 35–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bauman NM, McCarter RJ, Guzzetta PC, Shin JJ, Oh AK, Preciado DA, et al. Propranolol vs prednisolone for symptomatic proliferating infantile hemangiomas: a randomized clinical trial. JAMA Otolaryngol Head Neck Surg. 2014;140: 323–30. 10.1001/jamaoto.2013.6723 [DOI] [PubMed] [Google Scholar]
- 33.Aly MMD, Hamza AF, Abdel Kader HM, Saafan HA, Ghazy MS, Ragab IA. Therapeutic superiority of combined propranolol with short steroids course over propranolol monotherapy in infantile hemangioma. Eur J Pediatr. 2015;174: 1503–9. 10.1007/s00431-015-2561-1 [DOI] [PubMed] [Google Scholar]
- 34.Boon LM, MacDonald DM, Mulliken JB. Complications of systemic corticosteroid therapy for problematic hemangioma. Plast Reconstr Surg. 1999;104: 1616–23. [DOI] [PubMed] [Google Scholar]
- 35.Pandey A, Gangopadhyay AN, Gopal SC, Kumar V, Sharma SP, Gupta DK, et al. Twenty years’ experience of steroids in infantile hemangioma—a developing country’s perspective. J Pediatr Surg. 2009;44: 688–94. 10.1016/j.jpedsurg.2008.10.038 [DOI] [PubMed] [Google Scholar]
- 36.Jalil A, Maino A, Bhojwani R, Vose M, Ashworth J, Lloyd IC, et al. Clinical review of periorbital capillary hemangioma of infancy. J Pediatr Ophthalmol Strabismus. 2011;48: 218–25. 10.3928/01913913-20100719-04 [DOI] [PubMed] [Google Scholar]
- 37.Bertrand J, McCuaig C, Dubois J, Hatami A, Ondrejchak S, Powell J. Propranolol versus prednisone in the treatment of infantile hemangiomas: a retrospective comparative study. Pediatr Dermatol. 2011;28: 649–54. 10.1111/j.1525-1470.2011.01551.x [DOI] [PubMed] [Google Scholar]
- 38.Grover C, Kedar A, Arora P, Lal B. Efficacy of oral prednisolone use in the treatment of infantile hemangiomas in Indian children. Pediatr Dermatol. 2011;28: 502–6. 10.1111/j.1525-1470.2011.01491.x [DOI] [PubMed] [Google Scholar]
- 39.Price CJ, Lattouf C, Baum B, McLeod M, Schachner LA, Duarte AM, et al. Propranolol vs corticosteroids for infantile hemangiomas: a multicenter retrospective analysis. Arch Dermatol. 2011;147: 1371–6. 10.1001/archdermatol.2011.203 [DOI] [PubMed] [Google Scholar]
- 40.Rooklin AR, Lampert SI, Jaeger EA, McGeady SJ, Mansmann HC. Posterior subcapsular cataracts in steroid-requiring asthmatic children. J Allergy Clin Immunol. 1979;63: 383–6. [DOI] [PubMed] [Google Scholar]
- 41.Nassif E, Weinberger M, Sherman B, Brown K. Extrapulmonary effects of maintenance corticosteroid therapy with alternate-day prednisone and inhaled beclomethasone in children with chronic asthma. J Allergy Clin Immunol. 1987;80: 518–29. [DOI] [PubMed] [Google Scholar]
- 42.Kelly HW, Van Natta ML, Covar RA, Tonascia J, Green RP, Strunk RC. Effect of long-term corticosteroid use on bone mineral density in children: a prospective longitudinal assessment in the childhood Asthma Management Program (CAMP) study. Pediatrics. 2008;122: e53–61. 10.1542/peds.2007-3381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wiersbitzky S, Ballke EH, Patzschke V. The growth of children with bronchial asthma treated by different therapeutic regimens. [German] Das Somatische Gedeihen Von Kindern Mit Asthma Bronchiale Unter Verschiedenen Therapie-Regimen. Arztl Jugendkd. 1982;73: 225–232. [PubMed] [Google Scholar]
- 44.Miltenyi M, Homoki J, Fazekas AK. Posterior subcapsular cataracts, associated with long-term corticosteroid therapy. Prednisolone versus 6alpha-fluor-16alpha-methyl-1-dehydrocorticosterone. Helv Paediatr Acta. 1983;38: 141–147. [PubMed] [Google Scholar]
- 45.Foote KD, Brocklebank JT, Meadow SR. Height attainment in children with steroid-responsive nephrotic syndrome. Lancet. 1985;2: 917–919. [DOI] [PubMed] [Google Scholar]
- 46.Merritt RJ, Hack SL, Kalsch M, Olson D. Corticosteroid therapy-induced obesity in children. Clin Pediatr (Phila). 1986;25: 149–52. [DOI] [PubMed] [Google Scholar]
- 47.Garin EH, Sleasman JW, Richard GA, Iravani AA, Fennell RS. Pulsed methylprednisolone therapy compared to high dose prednisone in systemic lupus erythematosus nephritis. Eur J Pediatr. 1986;145: 380–3. [DOI] [PubMed] [Google Scholar]
- 48.Nammalwar BR, Vijaykumar M, Prahlad N, Jain DV. Steroid resistant nephrotic syndrome is sustained remission attainable. Indian Pediatr. 2006;43: 39–43. [PubMed] [Google Scholar]
- 49.Bahat E, Akkaya BK, Akman S, Karpuzoglu G, Guven AG. Comparison of pulse and oral steroid in childhood membranoproliferative glomerulonephritis. J Nephrol. 2007;20: 234–245. [PubMed] [Google Scholar]
- 50.Drigan R, Spirito A, Gelber RD. Behavioral effects of corticosteroids in children with acute lymphoblastic leukemia. Med Pediatr Oncol. 1992;20: 13–21. [DOI] [PubMed] [Google Scholar]
- 51.Lightner ES, Johnson H, Corrigan JJ. Rapid adrenocortical recovery after short-term glucocorticoid therapy. Am J Dis Child. 1981;135: 790–2. [DOI] [PubMed] [Google Scholar]
- 52.Mahachoklertwattana P, Vilaiyuk S, Hongeng S, Okascharoen C. Suppression of adrenal function in children with acute lymphoblastic leukemia following induction therapy with corticosteroid and other cytotoxic agents. J Pediatr. 2004;144: 736–40. 10.1016/j.jpeds.2004.03.033 [DOI] [PubMed] [Google Scholar]
- 53.Rix M, Birkebaek NH, Rosthøj S, Clausen N. Clinical impact of corticosteroid-induced adrenal suppression during treatment for acute lymphoblastic leukemia in children: a prospective observational study using the low-dose adrenocorticotropin test. J Pediatr. 2005;147: 645–50. 10.1016/j.jpeds.2005.06.006 [DOI] [PubMed] [Google Scholar]
- 54.Petersen KB, Müller J, Rasmussen M, Schmiegelow K. Impaired adrenal function after glucocorticoid therapy in children with acute lymphoblastic leukemia. Med Pediatr Oncol. 2003;41: 110–4. 10.1002/mpo.10316 [DOI] [PubMed] [Google Scholar]
- 55.Gordijn MS, van Litsenburg RR, Gemke RJBJ, Bierings MB, Hoogerbrugge PM, van de Ven PM, et al. Hypothalamic-pituitary-adrenal axis function in survivors of childhood acute lymphoblastic leukemia and healthy controls. Psychoneuroendocrinology. 2012;37: 1448–56. 10.1016/j.psyneuen.2012.01.014 [DOI] [PubMed] [Google Scholar]
- 56.Cunha C de F, Silva IN, Finch FL. Early adrenocortical recovery after glucocorticoid therapy in children with leukemia. J Clin Endocrinol Metab. 2004;89: 2797–802. 10.1210/jc.2003-031165 [DOI] [PubMed] [Google Scholar]
- 57.Felner EI, Thompson MT, Ratliff AF, White PC, Dickson BA. Time course of recovery of adrenal function in children treated for leukemia. J Pediatr. 2000;137: 21–4. 10.1067/mpd.2000.107385 [DOI] [PubMed] [Google Scholar]
- 58.Kuperman H, Damiani D, Chrousos GP, Dichtchekenian V, Manna TD, Filho VO, et al. Evaluation of the hypothalamic-pituitary-adrenal axis in children with leukemia before and after 6 weeks of high-dose glucocorticoid therapy. J Clin Endocrinol Metab. 2001;86: 2993–6. 10.1210/jcem.86.7.7629 [DOI] [PubMed] [Google Scholar]
- 59.Connolly AM, Schierbecker J, Renna R, Florence J. High dose weekly oral prednisone improves strength in boys with Duchenne muscular dystrophy. Neuromuscul Disord. 2002;12: 917–25. [DOI] [PubMed] [Google Scholar]
- 60.Miura M, Tamame T, Naganuma T, Chinen S, Matsuoka M, Ohki H. Steroid pulse therapy for Kawasaki disease unresponsive to additional immunoglobulin therapy. Paediatr Child Health. 2011;16: 479–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Torok KS, Arkachaisri T. Methotrexate and corticosteroids in the treatment of localized scleroderma: a standardized prospective longitudinal single-center study. J Rheumatol. 2012;39: 286–94. 10.3899/jrheum.110210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shiff NJ, Brant R, Guzman J, Cabral DA, Huber AM, Miettunen P, et al. Glucocorticoid-related changes in body mass index among children and adolescents with rheumatic diseases. Arthritis Care Res (Hoboken). 2013;65: 113–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dowell SF, Bresee JS. Severe varicella associated with steroid use. Pediatrics. 1993;92: 223–8. [PubMed] [Google Scholar]
- 64.Ait Ourhroui M, Hassam B, Khoudri I. [Treatment of alopecia areata with prednisone in a once-monthly oral pulse]. Ann Dermatol Venereol. 2010;137: 514–8. 10.1016/j.annder.2010.06.002 [DOI] [PubMed] [Google Scholar]
- 65.Upadhyay A, Mishra OP, Prasad R, Upadhyay SK, Schaefer F. Behavioural abnormalities in children with new-onset nephrotic syndrome receiving corticosteroid therapy: results of a prospective longitudinal study. Pediatr Nephrol. 2016;31: 233–8. 10.1007/s00467-015-3216-1 [DOI] [PubMed] [Google Scholar]
- 66.Hawcutt DB, Jorgensen AL, Wallin N, Thompson B, Peak M, Lacy D, et al. Adrenal responses to a low-dose short synacthen test in children with asthma. Clin Endocrinol (Oxf). 2015;82: 648–56. [DOI] [PubMed] [Google Scholar]
- 67.Bakchine H, Niaudet P, Gagnadoux MF. Steroid-induced diabetes in 6 children after renal transplantation. [French] Diabete Induit Par Les Corticoides. Chez Six Enfants Apres Transplantation Renale. Arch Fr Pediatr. 1984;41: 261–264. [PubMed] [Google Scholar]
- 68.Elliott AJ, Oakhill A, Goodman S. Cataracts in childhood leukaemia. Br J Ophthalmol. 1985;69: 459–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Enjolras O, Riche MC, Merland JJ, Escande JP. Management of alarming hemangiomas in infancy: a review of 25 cases. Pediatrics. 1990;85: 491–8. [PubMed] [Google Scholar]
- 70.Sanders BP, Portman RJ, Ramey RA, Hill M, Strunk RC. Hypertension during reduction of long-term steroid therapy in young subjects with asthma. J Allergy Clin Immunol. 1992;89: 816–21. [DOI] [PubMed] [Google Scholar]
- 71.Sadan N, Wolach B. Treatment of hemangiomas of infants with high doses of prednisone. J Pediatr. 1996;128: 141–6. [DOI] [PubMed] [Google Scholar]
- 72.Borgna-Pignatti C, Rugolotto S, Nobili B, Amendola G, De Stefano P, Maccario R, et al. A trial of high-dose dexamethasone therapy for chronic idiopathic thrombocytopenic purpura in childhood. J Pediatr. 1997;130: 13–6. [DOI] [PubMed] [Google Scholar]
- 73.Kühne T, Freedman J, Semple JW, Doyle J, Butchart S, Blanchette VS. Platelet and immune responses to oral cyclic dexamethasone therapy in childhood chronic immune thrombocytopenic purpura. J Pediatr. 1997;130: 17–24. [DOI] [PubMed] [Google Scholar]
- 74.Chen JS, Wu JM, Chen YJ, Yeh TF. Pulsed high-dose dexamethasone therapy in children with chronic idiopathic thrombocytopenic purpura. J Pediatr Hematol Oncol. 1997;19: 526–9. [DOI] [PubMed] [Google Scholar]
- 75.Uysal KM, Olgun N, Erbay A, Sarialioğlu F. High-dose oral methylprednisolone therapy in childhood hemangiomas. Pediatr Hematol Oncol. 2001;18: 335–41. 10.1080/088800101300312609 [DOI] [PubMed] [Google Scholar]
- 76.Wali YA, Al Lamki Z, Shah W, Zacharia M, Hassan A. Pulsed high-dose dexamethasone therapy in children with chronic idiopathic thrombocytopenic purpura. Pediatr Hematol Oncol. 2002;19: 329–35. [DOI] [PubMed] [Google Scholar]
- 77.Mallo S, Torrelo A, Zambrano A. Treatment of hemangiomas in children with oral corticosteroids. [Spanish] Tratamiento de hemangiomas infantiles con corticoides orales. Actas Dermosifiliogr. 2004;95: 370–373. [Google Scholar]
- 78.Kivity S, Lerman P, Ariel R, Danziger Y, Mimouni M, Shinnar S. Long-term cognitive outcomes of a cohort of children with cryptogenic infantile spasms treated with high-dose adrenocorticotropic hormone. Epilepsia. 2004;45: 255–62. [DOI] [PubMed] [Google Scholar]
- 79.Kossoff EH, Hartman AL, Rubenstein JE, Vining EPG. High-dose oral prednisolone for infantile spasms: an effective and less expensive alternative to ACTH. Epilepsy Behav. 2009;14: 674–6. 10.1016/j.yebeh.2009.01.023 [DOI] [PubMed] [Google Scholar]
- 80.Thacker D, Patel A, Dodds K, Goldberg DJ, Semeao E, Rychik J. Use of oral budesonide in the management of protein-losing enteropathy after the Fontan operation. Ann Thorac Surg. 2010;89: 837–42. 10.1016/j.athoracsur.2009.09.063 [DOI] [PubMed] [Google Scholar]
- 81.Mytinger JR, Quigg M, Taft WC, Buck ML, Rust RS. Outcomes in treatment of infantile spasms with pulse methylprednisolone. J Child Neurol. 2010;25: 948–53. 10.1177/0883073809356107 [DOI] [PubMed] [Google Scholar]
- 82.Schumacher KR, Cools M, Goldstein BH, Ioffe-Dahan V, King K, Gaffney D, et al. Oral budesonide treatment for protein-losing enteropathy in Fontan-palliated patients. Pediatr Cardiol. 2011;32: 966–71. 10.1007/s00246-011-0029-2 [DOI] [PubMed] [Google Scholar]
- 83.Corapcioğlu F, Büyükkapu-Bay S, Binnetoğlu K, Babaoğlu A, Anik Y, Tugay M. Preliminary results of propranolol treatment for patients with infantile hemangioma. Turk J Pediatr. 2011;53: 137–41. [PubMed] [Google Scholar]
- 84.Nieuwenhuis K, de Laat PCJ, Janmohamed SR, Madern GC, Oranje AP. Infantile hemangioma: treatment with short course systemic corticosteroid therapy as an alternative for propranolol. Pediatr Dermatol. 2013;30: 64–70. 10.1111/j.1525-1470.2012.01846.x [DOI] [PubMed] [Google Scholar]
- 85.Gursu HA, Erdogan I, Varan B, Oktay A, Ozcay F, Ozkan M, et al. Oral budesonide as a therapy for protein-losing enteropathy in children after the Fontan operation. J Card Surg. 2014;29: 712–6. 10.1111/jocs.12355 [DOI] [PubMed] [Google Scholar]
- 86.Job JC, Munck A, Chaussain JL, Canlorbe P. Effects and side-effects of dexamethasone used as treatment of congenital virilizing adrenal hyperplasia in adolescent patients. [French] Traitement De L’hyperplasie Surrenale Virilisante Chez Les Adolescents. Emploi Et Inconvenients De La Dexamethasone. Arch Fr Pediatr. 1985;42: 765–769. [PubMed] [Google Scholar]
- 87.Rizzoni G, Todesco L, Callegari M . Long-term alternate-day steroid treatment of frequently relapsing nephrotic syndrome. [Italian] La Corticoterapia Discontinua Prolungata (Cdp) Nel Trattamento Della Sindrome Nefrosica a Frequenti Recidive. Riv Ital di Pediatr. 1986;12: 519–522. [Google Scholar]
- 88.Zychowicz C, Wicinska W. A successful attempt at replacing prednisone and kenalog with inhalations of beclomethasone dipropionate in 2 girls with bronchial asthma and drug-induced growth arrest. [Polish]. Wiad Lek. 1982;35: 1177–1180. [PubMed] [Google Scholar]
- 89.Fujita K, Sanae N, Yoshioka H, Kurokawa H, Sato T. Steroid Therapy and Fatal Varicella in a Nephrotic Patient; A Necropsy case with Atypical Rash. Pediatr Int. Blackwell Publishing Ltd; 1983;25: 322–325. [Google Scholar]
- 90.George WE Jr, Wilmot M, Greenhouse A, Hammeke M. Medical management of steroid-induced epidural lipomatosis. N Engl J Med. 1983;308: 316–319. 10.1056/NEJM198302103080605 [DOI] [PubMed] [Google Scholar]
- 91.Kaneda A, Yamaura I, Kamikozuru M, Nakai O. Paraplegia as a complication of corticosteroid therapy. J Bone Jt Surg—Ser A. 1984;66: 783–785. [PubMed] [Google Scholar]
- 92.Curless RG, Flynn J, Bachynski B, Gregorios JB, Benke P, Cullen R. Fatal metabolic acidosis, hyperglycemia, and coma after steroid therapy for Kearns-Sayre syndrome. Neurology. 1986;36: 872–3. [DOI] [PubMed] [Google Scholar]
- 93.Rejou F, Dumas R, Belon C, Meunier PJ, Edouard C. Fluoride treatment in corticosteroid induced osteoporosis. Arch Dis Child. 1986;61: 1230–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Van Story-Lewis PE, Roberts MW, Klippel JH. Oral effects of steroid therapy in a patient with systemic lupus erythematosus: report of case. J Am Dent Assoc. 1987;115: 49–51. [DOI] [PubMed] [Google Scholar]
- 95.Wales JK, Milner RD. Variation in lower leg growth with alternate day steroid treatment. Arch Dis Child. 1988;63: 981–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Silk HJ, Guay-Woodford L, Perez-Atayde AR, Geha RS, Broff MD. Fatal varicella in steroid-dependent asthma. J Allergy Clin Immunol. 1988;81: 47–51. [DOI] [PubMed] [Google Scholar]
- 97.Splain J, Berman BW. Cyclosporin A treatment for Diamond-Blackfan anemia. Am J Hematol. 1992;39: 208–211. [DOI] [PubMed] [Google Scholar]
- 98.Watanabe TK, Sylvester CE, Manaligod JM. Mania or panic associated with dexamethasone chemotherapy in adolescents. J Adolesc Health. 1994;15: 345–7. [DOI] [PubMed] [Google Scholar]
- 99.Jackson LD, Song E. Cyclosporin in the treatment of corticosteroid resistant autoimmune chronic active hepatitis. Gut. 1995;36: 459–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Abuekteish F, Kirkpatrick JN, Russell G. Posterior subcapsular cataract and inhaled corticosteroid therapy. Thorax. 1995;50: 674–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Sakurai Y, Ohkubo Y, Miura S, Mariko M, Akazawa H, Imanaka Y, et al. Liposteroid therapy for chronic childhood idiopathic thrombocytopenic purpura: Two case reports. Int J Pediatr Hematol. 1999;6: 27–31. [Google Scholar]
- 102.Alessandri AJ, Rogers PC, Wadsworth LD, Davis JH. Diamond-blackfan anemia and cyclosporine therapy revisited. J Pediatr Hematol Oncol. 2000;22: 176–9. [DOI] [PubMed] [Google Scholar]
- 103.Gupta MT, Jerajani HR. Control of childhood pemphigus erythematosus with steroids and azathioprine. Br J Dermatol. 2004;150: 163–4. [DOI] [PubMed] [Google Scholar]
- 104.Teixeira AL Jr, Maia DP, Cardoso F. Treatment of acute Sydenham’s chorea with methyl-prednisolone pulse-therapy. Parkinsonism Relat Disord. 2005;11: 327–30. 10.1016/j.parkreldis.2005.02.007 [DOI] [PubMed] [Google Scholar]
- 105.Herrero Hernández A, Escobosa Sánchez O, Acha García T. Successful treatment with vincristine in PHACES syndrome. Clin Transl Oncol. 2007;9: 262–3. [DOI] [PubMed] [Google Scholar]
- 106.Matsuzaki A, Suminoe A, Koga Y, Kusuhara K, Hara T, Ogata R, et al. Fatal visceral varicella-zoster virus infection without skin involvement in a child with acute lymphoblastic leukemia. Pediatr Hematol Oncol. 2008;25: 237–42. 10.1080/08880010801938215 [DOI] [PubMed] [Google Scholar]
- 107.Tsuruga K, OKI Eishin, Suzuki K, Takahashi Y, Tanaka H. Early initiation of peritoneal dialysis for the treatment of a patient with refractory nephrotic syndrome. [Japanese]. Japanese J Nephrol. 2009;51: 68–73. [PubMed] [Google Scholar]
- 108.Ishigaki K, Shishikura K, Murakami T, Suzuki H, Hirayama Y, Osawa M. Benefits of FK 506 for refractory eye symptoms in a young child with ocular myasthenia gravis. Brain Dev. 2009;31: 634–7. 10.1016/j.braindev.2008.08.016 [DOI] [PubMed] [Google Scholar]
- 109.Morais P, Magina S, Mateus M, Trindade E, Jesus JM, Azevedo F. Efficacy and safety of propranolol in the treatment of parotid hemangioma. Cutan Ocul Toxicol. 2011;30: 245–8. 10.3109/15569527.2011.554483 [DOI] [PubMed] [Google Scholar]
- 110.Koay ACA, Choo MM, Nathan AM, Omar A, Lim CT. Combined low-dose oral propranolol and oral prednisolone as first-line treatment in periocular infantile hemangiomas. J Ocul Pharmacol Ther. 2011;27: 309–11. 10.1089/jop.2011.0013 [DOI] [PubMed] [Google Scholar]
- 111.Srinivasan A, Lavanya R, Sankar J. Steroid-unresponsive hypereosinophilic syndrome. Ann Trop Paediatr. 2011;31: 273–7. 10.1179/1465328111Y.0000000027 [DOI] [PubMed] [Google Scholar]
- 112.Kim SH, Kwon JE, Kim H-B. Successful treatment of steroid-dependent eosinophilic cellulitis with cyclosporine. Allergy Asthma Immunol Res. 2013;5: 62–4. 10.4168/aair.2013.5.1.62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Gursu HA, Varan B, Erdogan I. Use of oral budesonide in the management of protein-losing enteropathy due to restrictive cardiomyopathy. Cardiol Young. 2014;24: 764–6. 10.1017/S104795111300125X [DOI] [PubMed] [Google Scholar]
- 114.Schaefer ET, Fitzgerald JF, Molleston JP, Croffie JM, Pfefferkorn MD, Corkins MR, et al. Comparison of oral prednisone and topical fluticasone in the treatment of eosinophilic esophagitis: a randomized trial in children. Clin Gastroenterol Hepatol. 2008;6: 165–73. 10.1016/j.cgh.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 115.Grover C, Arora P, Kedar A, Pal P, Lal B. Combination of oral corticosteroids and polidocanol sclerotherapy in the management of infantile hemangiomas. Dermatol Surg. 2010;36: 2030–6. 10.1111/j.1524-4725.2010.01760.x [DOI] [PubMed] [Google Scholar]
- 116.Tan BH, Leadbitter PH, Aburn NH, Tan ST. Steroid therapy for problematic proliferating haemangioma. N Z Med J. 2011;124: 57–65. [PubMed] [Google Scholar]
- 117.Greene AK, Couto RA. Oral prednisolone for infantile hemangioma: efficacy and safety using a standardized treatment protocol. Plast Reconstr Surg. 2011;128: 743–52. 10.1097/PRS.0b013e3182221398 [DOI] [PubMed] [Google Scholar]
- 118.Malone DN, Drever JC, Grant IW, Percy-Robb IW. Endocrine response to substitution of corticotrophin for oral prednisolone in asthmatic children. Br Med J. 1972;3: 202–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sumboonnanonda A, Vongjirad A, Suntornpoch V, Petrarat S. Adrenal function after prednisolone treatment in childhood nephrotic syndrome. J Med Assoc Thail. 1994;77: 126–129. [PubMed] [Google Scholar]
- 120.Buyukcelik M, Cengiz N, Dursun H, Soran M, Bayazit AK, Noyan A, et al. Intravenous pulse cyclophosphamide therapy in focal segmental glomerulosclerosis. Clin Nephrol. 2006;65: 7–12. [DOI] [PubMed] [Google Scholar]
- 121.Ferrara M, Borrelli B, Greco N, Coppola L, Coppola A, Simeone G, et al. Side effects of corticosteroid therapy in children with chronic idiopathic thrombocytopenic purpura. Hematology. 2005;10: 401–3. 10.1080/10245330500168740 [DOI] [PubMed] [Google Scholar]
- 122.Harris JC, Carel CA, Rosenberg LA, Joshi P, Leventhal BG. Intermittent high dose corticosteroid treatment in childhood cancer: behavioral and emotional consequences. J Am Acad Child Psychiatry. 1986;25: 120–4. [DOI] [PubMed] [Google Scholar]
- 123.Sansome A, Royston P, Dubowitz V. Steroids in Duchenne muscular dystrophy; pilot study of a new low-dosage schedule. Neuromuscul Disord. 1993;3: 567–9. [DOI] [PubMed] [Google Scholar]
- 124.Kim SM, Lee HS, Hann SK. The efficacy of low-dose oral corticosteroids in the treatment of vitiligo patients. Int J Dermatol. 1999;38: 546–50. [DOI] [PubMed] [Google Scholar]
- 125.Chiemchanya S, Visudhiphan P. Myasthenia gravis: A clinical study in Thai children at Ramathibodi Hospital. J Med Assoc Thail. 1986;69: 6–11. [PubMed] [Google Scholar]
- 126.Felder-Puig R, Scherzer C, Baumgartner M, Ortner M, Aschenbrenner C, Bieglmayer C, et al. Glucocorticoids in the treatment of children with acute lymphoblastic leukemia and hodgkin’s disease: a pilot study on the adverse psychological reactions and possible associations with neurobiological, endocrine, and genetic markers. Clin Cancer Res. 2007;13: 7093–100. 10.1158/1078-0432.CCR-07-0902 [DOI] [PubMed] [Google Scholar]
- 127.Friedman M, Strang LB. Effect of long-term corticosteroids and corticotrophin on the growth of children. Lancet. University of Witwatersrand; 1966;288: 568–572. [PubMed] [Google Scholar]
- 128.Hawkins DB, Crockett DM, Kahlstrom EJ, MacLaughlin EF. Corticosteroid management of airway hemangiomas: long-term follow-up. Laryngoscope. 1984;94: 633–7. [PubMed] [Google Scholar]
- 129.Delesalle F, Staumont D, Houmany MA, Breviere GM, Piette F. Pulse methylprednisolone therapy for threatening periocular haemangiomas of infancy. Acta Derm Venereol. 2006;86: 429–32. [DOI] [PubMed] [Google Scholar]
- 130.Payne DNR, Balfour-Lynn IM, Biggart EA, Bush A, Rosenthal M. Subcutaneous terbutaline in children with chronic severe asthma. Pediatr Pulmonol. 2002;33: 356–61. [DOI] [PubMed] [Google Scholar]
- 131.Adams DM, Kinney TR, O’Branski-Rupp E, Ware RE. High-dose oral dexamethasone therapy for chronic childhood idiopathic thrombocytopenic purpura. J Pediatr. 1996;128: 281–3. [DOI] [PubMed] [Google Scholar]
- 132.Sogo T, Fujisawa T, Inui A, Komatsu H, Etani Y, Tajiri H, et al. Intravenous methylprednisolone pulse therapy for children with autoimmune hepatitis. Hepatol Res. 2006;34: 187–92. 10.1016/j.hepres.2005.12.002 [DOI] [PubMed] [Google Scholar]
- 133.Turner Z, Lanford L, Webber S. Oral budesonide as a therapy for protein-losing enteropathy in patients having undergone Fontan palliation. Congenit Heart Dis. 2012;7: 24–30. 10.1111/j.1747-0803.2011.00593.x [DOI] [PubMed] [Google Scholar]
- 134.Akyüz C, Yariş N, Kutluk MT, Büyükpamukçu M. Management of cutaneous hemangiomas: a retrospective analysis of 1109 cases and comparison of conventional dose prednisolone with high-dose methylprednisolone therapy. Pediatr Hematol Oncol. 2001;18: 47–55. 10.1080/088800101750059855 [DOI] [PubMed] [Google Scholar]
- 135.Martindale. The complete drug reference. Accessed through Medicines Complete [Internet]. [cited 13 Dec 2016]. https://www.medicinescomplete.com/mc/martindale/current/1060-a2-n.htm
- 136.Kenna HA, Poon AW, de los Angeles CP, Koran LM. Psychiatric complications of treatment with corticosteroids: review with case report. Psychiatry Clin Neurosci. 2011;65: 549–60. 10.1111/j.1440-1819.2011.02260.x [DOI] [PubMed] [Google Scholar]
- 137.Demirci K, Yaman AR, Akpinar A, Demirdas A. Mania after Corticosteroid Withdrawal in Behçet’s Disease: A Case Report. J Mood Disord. 2015;5: 182–184. [Google Scholar]
- 138.Lewis DA, Smith RE. Steroid-induced psychiatric syndromes. A report of 14 cases and a review of the literature. J Affect Disord. 1983;5: 319–32. [DOI] [PubMed] [Google Scholar]
- 139.Curtis JR, Westfall AO, Allison J, Bijlsma JW, Freeman A, George V, et al. Population-based assessment of adverse events associated with long-term glucocorticoid use. Arthritis Rheum. 2006;55: 420–6. 10.1002/art.21984 [DOI] [PubMed] [Google Scholar]
- 140.Philip J. The Effects of Inhaled Corticosteroids on Growth in Children. Open Respir Med J. 2014;8: 66 10.2174/1874306401408010066 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.