Abstract
OBJECTIVE
To create a simple tool for predicting the likelihood of successful trial of labor after cesarean delivery (TOLAC) during the pregnancy after a primary cesarean delivery using variables available at the time of admission.
METHODS
Data for all deliveries at 14 regional hospitals over an 8-year period were reviewed. Women with one cesarean delivery and one subsequent delivery were included. Variables associated with successful VBAC were identified using multivariable logistic regression. Points were assigned to these characteristics, with weighting based on the coefficients in the regression model to calculate an integer VBAC score. The VBAC score was correlated with TOLAC success rate and was externally validated in an independent cohort using a logistic regression model.
RESULTS
A total of 5,445 women met inclusion criteria. Of those women, 1,170 (21.5%) underwent TOLAC. Of the women who underwent trial of labor, 938 (80%) had a successful VBAC. AVBAC score was generated based on the Bishop score (cervical examination) at the time of admission, with points added for history of vaginal birth, age younger than 35 years, absence of recurrent indication, and body mass index less than 30. Women with a VBAC score less than 10 had a likelihood of TOLAC success less than 50%. Women with a VBAC score more than 16 had a TOLAC success rate more than 85%. The model performed well in an independent cohort with an area under the curve of 0.80 (95% confidence interval 0.76–0.84).
CONCLUSIONS
Prediction of TOLAC success at the time of admission is highly dependent on the initial cervical examination. This simple VBAC score can be utilized when counseling women considering TOLAC.
With the increasing rate of cesarean delivery, counseling women regarding the option of trial of labor after cesarean delivery (TOLAC) is becoming increasingly important. Data clearly demonstrate that women with a successful vaginal birth after cesarean delivery (VBAC) have less morbidity than women undergoing an elective repeat cesarean delivery.1–3 However, women undergoing an elective repeat cesarean delivery have less morbidity than those in whom TOLAC fails.1–3 Therefore, several investigators have developed models to predict successful VBAC.4–12 Some of these models were intended for use at the time of the first prenatal visit,11,12 and others were intended for use at the time of admission.4–8
Women who are counseled early during pregnancy using antepartum factors alone may have a greater chance of success if they present for delivery with a favorable cervix. Being able to improve the accuracy of predicting a successful VBAC at the time of admission may encourage more women to undergo TOLAC, thereby preventing the downstream morbidity associated with multiple cesarean deliveries, including increased operative risk and abnormal placentation.13
The pregnancy after a primary cesarean delivery is the time when most patients and physicians consider TOLAC. In the majority of women, the delivery outcome will strongly influence the mode of delivery in all subsequent deliveries. Women who opt for an elective repeat cesarean delivery likely will have cesarean deliveries for future deliveries, whereas those who have a successful VBAC likely will opt for future TOLACs. Therefore, we sought to develop a simple model that could be used to validly predict the likelihood of TOLAC success at the time of admission for women who opted for TOLAC.
MATERIALS AND METHODS
This was a retrospective cohort study of all women delivering a singleton pregnancy at 14 Intermountain Healthcare hospitals from July 2000 to July 2008. All patients who had a primary cesarean delivery and at least one subsequent delivery were included. The study size was dictated by the available cohort for the years of collected data. This study was approved by the Intermountain Healthcare Institutional Review Board.
Only the delivery immediately after the primary cesarean delivery was used for analysis. Newborns with anomalies and stillbirths were excluded. Women undergoing TOLAC were identified by patient TOLAC request documented by the labor and delivery nurse at admission, the use of oxytocin, intrauterine pressure catheter placement, vaginal delivery, arrest of dilation or arrest of descent as the indication for a second cesarean delivery, or a billing code for failed TOLAC. All other women were classified as having an elective repeat cesarean delivery and were excluded from analysis. To determine whether women were appropriately classified as undergoing TOLAC or elective repeat cesarean delivery, 10% of the charts were pulled randomly and assessed by manual chart review. All other data were populated directly from the electronic medical record system in use at these hospitals.
The electronic medical records of the women undergoing TOLAC were queried to abstract demographic and obstetric data. Data were gathered from the admission when the participant delivered. Demographic variables included maternal age, parity, gestational age at delivery by best obstetric estimate, self-reported race, marital status, prepregnancy body mass index (BMI, calculated as weight (kg)/[height (m)]2), and insurance status. Recorded obstetric variables included preeclampsia or eclampsia, gestational diabetes, mode of delivery, use of oxytocin, small-for-gestational-age neonate, cervical examination during admission when delivery occurred, and indication for cesarean delivery. The Bishop score14 was calculated using the first digital cervical examination at the time of admission by a resident (second-year or third-year resident in a university-based program), attending physician, hospital-based certified nurse midwife, or trained labor and delivery nurse. Women with missing cervical examination data were excluded. Complete data for all other variables in the final model were available.
Multivariable, stepwise, backwards logistic regression was utilized to determine which variables were associated with successful VBAC. The variables included in our original model were gestational age at delivery, gestational diabetes, small for gestational age, history of vaginal delivery, BMI, Bishop score at admission, primary cesarean delivery performed for recurrent indication (arrest of dilation or arrest of descent), age older than 35 years, presence of preeclampsia or eclampsia, and Hispanic or African American race. For the analysis, BMI was grouped as less than18.5, 18.5–24.9, 25–29.9, and 30 or more, corresponding to standard underweight, normal weight, overweight, and obese categories.15 The gestational age was initially used in the model as a continuous variable, with 40 weeks as the referent. The model was performed again with gestational age categorized into 34 weeks or less, 34 1/7 weeks to 38 6/7 weeks, 39 0/7 weeks to 40 6/7 weeks, and 41 weeks or more. Bishop score was recorded as an integer value. All other variables were maintained as continuous or dichotomous variables. The variables included in the model were selected based on predictors of successful VBAC previously reported in the literature.4–12
After determining the variables associated with VBAC in the logistic regression, a bootstrap inclusion fraction was utilized to determine the percentage of time that each variable would be retained in the model as a significant predictor in the bootstrap resample for the model.16 Any variables that would appear less than 50% of the time in the bootstrap resample were not included in the final model.16 After removal of these variables, the final regression model was plotted as a receiver operating characteristic (ROC) curve. The area under the ROC curve is an index of discrimination and is frequently referred to as the c-statistic.17
The established model was then internally validated with bootstrapping.18 Bootstrapping is a superior statistical method for randomly splitting the study sample into test and validation groups.19 It also allows for the use of the entire study group to develop the model. An optimism coefficient was generated and subtracted from the initial area under the curve (AUC) to give an internal bootstrap validation AUC. An AUC of at least 0.70 is generally considered to be an acceptable level of discrimination.20
Points were assigned to specific clinical and demographic characteristics, with weighting based on the coefficients in the regression model. An integer VBAC score was then calculated for each woman undergoing TOLAC and was correlated with the chance of successful VBAC. A fractional polynomial smoothing function through the predicted probabilities with 95% confidence intervals (CI) was computed using fractional polynomial regression.
Our model also was compared with two existing models.8,12 This was performed by comparing the area under the ROC for the models using the method of DeLong et al.21 Only women with all variables available for both models were used in the comparison.
In addition, we externally validated our calculated VBAC score in an independent sample from the Perinatal Database at the University of Colorado Denver. The Perinatal Database is a prospectively collected database that includes all women who have delivered at the University of Colorado Denver over a 7-year period (http://cctsi.ucdenver.edu/CMH/Pages/BabyBlanket.aspx). All women in the data set undergoing TOLAC with one previous cesarean delivery were included in the validation. In this data set, fetal station above zero was delineated as high, and more specific details were not available. For the purpose of this analysis, any station higher than zero was not assigned any points in the calculation of the Bishop score for that individual patient. Within decile of predicted probability, the predicted and observed VBAC rates were compared. A logistic regression model of the probability of VBAC success was estimated with calculated VBAC score as the only predictor. The corresponding AUCs and 95% CIs of the ROC curves were calculated. The external validation portion of the study was approved by the Colorado Multiple Institutional Review Board.
The statistical software package STATA 11.0 was used for the initial analyses. SAS was used for the external validation of the model. Statistical significance was defined as a two-sided P<.05.
RESULTS
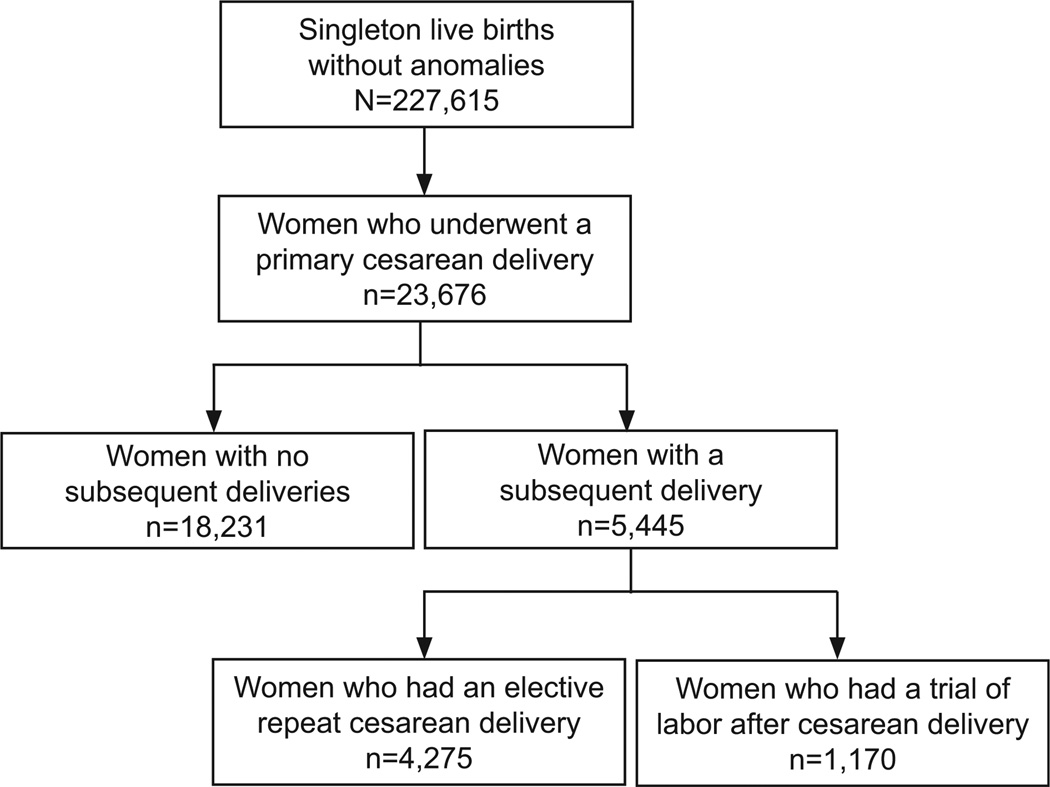
There were 227,615 nonanomalous, singleton, live births over the course of the 8-year study period (Fig. 1). Of these, 5,445 women had a primary cesarean delivery and a subsequent delivery. Of these women, 1,170 (21.5%) women underwent TOLAC with their next pregnancy. The rate of successful VBAC among these women was 80% (n = 938).
Fig. 1.
Flow of study participants.
Metz. Simple VBAC Prediction Model. Obstet Gynecol 2013.
The majority of the study population was Caucasian, married, privately insured, and had a normal BMI (Table 1). There were relatively low rates of preeclampsia, gestational diabetes, and small-for-gestational-age neonates (Table 1). Overall, 364 (31.1%; 95% CI 27.9–34.3) women undergoing TOLAC after primary cesarean delivery had a previous vaginal birth. There was a 98.7% accuracy of classification (TOLAC compared with elective repeat cesarean delivery) found on manual review of the charts.
Table 1.
Demographic Characteristics of Women Undergoing Trial of Labor After Cesarean Delivery
| Demographic Characteristic | Successful VBAC (n=5938) | Failed TOLAC (n=5232) | P |
|---|---|---|---|
| Maternal age (y) | 27.9±4.3 | 27.5±4.6 | .20 |
| Gestational age at delivery (wk) | 38.6±1.7 | 38.5±1.6 | .59 |
| Race | .13 | ||
| White | 846 (90.2) | 199 (85.8) | |
| Hispanic | 54 (5.8) | 20 (8.6) | |
| Asian | 11 (1.2) | 7 (3.0) | |
| African American | 7 (0.7) | 1 (0.4) | |
| Other | 20 (2.1) | 5 (2.2) | |
| BMI (kg/m2) | <.001 | ||
| Less than 18.5 | 33 (3.5) | 8 (3.4) | |
| 18.5–24.9 | 542 (57.8) | 99 (42.7) | |
| 25–29.9 | 225 (24.0) | 66 (28.4) | |
| More than 30 | 138 (14.7) | 59 (25.4) | |
| Insurance status | .002 | ||
| Private insurance | 720 (76.8) | 164 (70.6) | |
| Medicaid | 186 (19.8) | 63 (27.2) | |
| Medicare | 0 (0) | 1 (0.4) | |
| Uninsured | 32 (3.4) | 3 (1.3) | |
| Unknown | 0 (0) | 1 (0.4) | |
| Marital status | .37 | ||
| Married | 879 (93.7) | 215 (92.7) | |
| Single | 41 (4.4) | 15 (6.5) | |
| Divorced or separated | 13 (1.4) | 1 (0.4) | |
| Unknown | 5 (0.5) | 1 (0.4) | |
| History of vaginal delivery | 322 (34.3) | 42 (18.1) | <.001 |
| Recurrent indication for primary cesarean delivery | 84 (9.0) | 44 (19.0) | <.001 |
| Induction of labor | 216 (23.0) | 39 (16.8) | .05 |
| Maternal preeclampsia or eclampsia | 31 (3.3) | 9 (3.9) | .65 |
| Maternal gestational diabetes | 34 (3.6) | 12 (5.2) | .27 |
| Small-for-gestational-age neonate | 41 (4.4) | 9 (3.9) | .76 |
| Neonatal birth weight (g) | 3,378±519 | 3,413±512 | .42 |
VBAC, vaginal birth after cesarean delivery; TOLAC, trial of labor after cesarean delivery; BMI, body mass index.
Data are mean±standard deviation or n (%) unless otherwise specified.
Six of those women (0.5%; 95% CI 0.1–0.9) undergoing TOLAC had uterine rupture diagnosed. One uterine rupture occurred in a woman undergoing postdates induction of labor with oxytocin. All other ruptures occurred in the setting of spontaneous labor. Three were discovered at 5–6 cm of dilation. One was noted at complete dilation and zero station, with variable decelerations and pain. The other two were noted after successful operative vaginal deliveries for fetal decelerations. None of the ruptures necessitated a hysterectomy. All cases of uterine rupture involved fetal heart rate changes (variable decelerations or bradycardia) before delivery. All of these newborns survived without apparent neurologic impairment.
The rates of other obstetric complications in the women with a successful VBAC (n = 938) are as follows: shoulder dystocia in 1.8% (n = 17; 95% CI 1.0–2.7); third-degree or fourth-degree laceration in 8.4% (n = 79; 95% CI 6.6–10.2); and operative vaginal delivery in 10.3% (n = 97; 95% CI 8.4–12.3). Multivariable logistic regression identified the following five variables that were associated with successful TOLAC: history of vaginal birth (odds ratio [OR] 2.7, 95% CI 1.8–4.1); absence of recurrent indication for primary cesarean delivery (OR 2.0, 95% CI 1.3–3.1); age younger than 35 years (OR 2.0, 95% CI 1.1–3.4); BMI less than 30 (OR 1.6, 95% CI 1.1–2.4); and each point of Bishop score (OR 1.3, 95% CI 1.2–1.4). Hispanic ethnicity was excluded from the model because it was deemed to be included in bootstrap replications less than 50% of the time. Additionally, when the model was performed with Hispanic ethnicity included, it only affected the AUC at the third decimal place. Similarly, induction was excluded because it did not substantially improve the fit of our model (AUC was 0.720 with induction and was 0.715 without). Women in our study population who were induced had a favorable initial Bishop score (7.68±2.10) and were more likely to have a history of vaginal delivery than were the rest of the cohort (45.1 compared with 27.2%; P<.001).
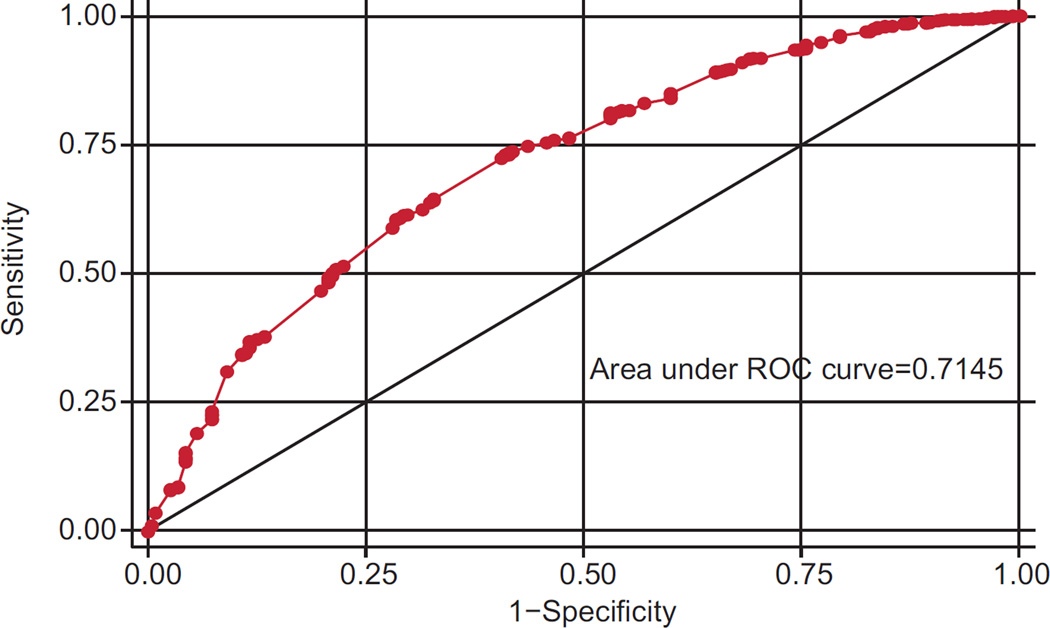
The plotted ROC curve for the final model is shown in Figure 2. The internal bootstrap validation AUC was 0.70 (95% CI 0.67–0.74) after adjustment for optimism.
Fig. 2.
Receiver operating characteristic (ROC) curve for multivariable regression model to predict vaginal birth after cesarean delivery success. An internal bootstrap validation area under the curve was 0.70 (95% confidence interval 0.67–0.74) after adjustment for optimism.
Metz. Simple VBAC Prediction Model. Obstet Gynecol 2013.
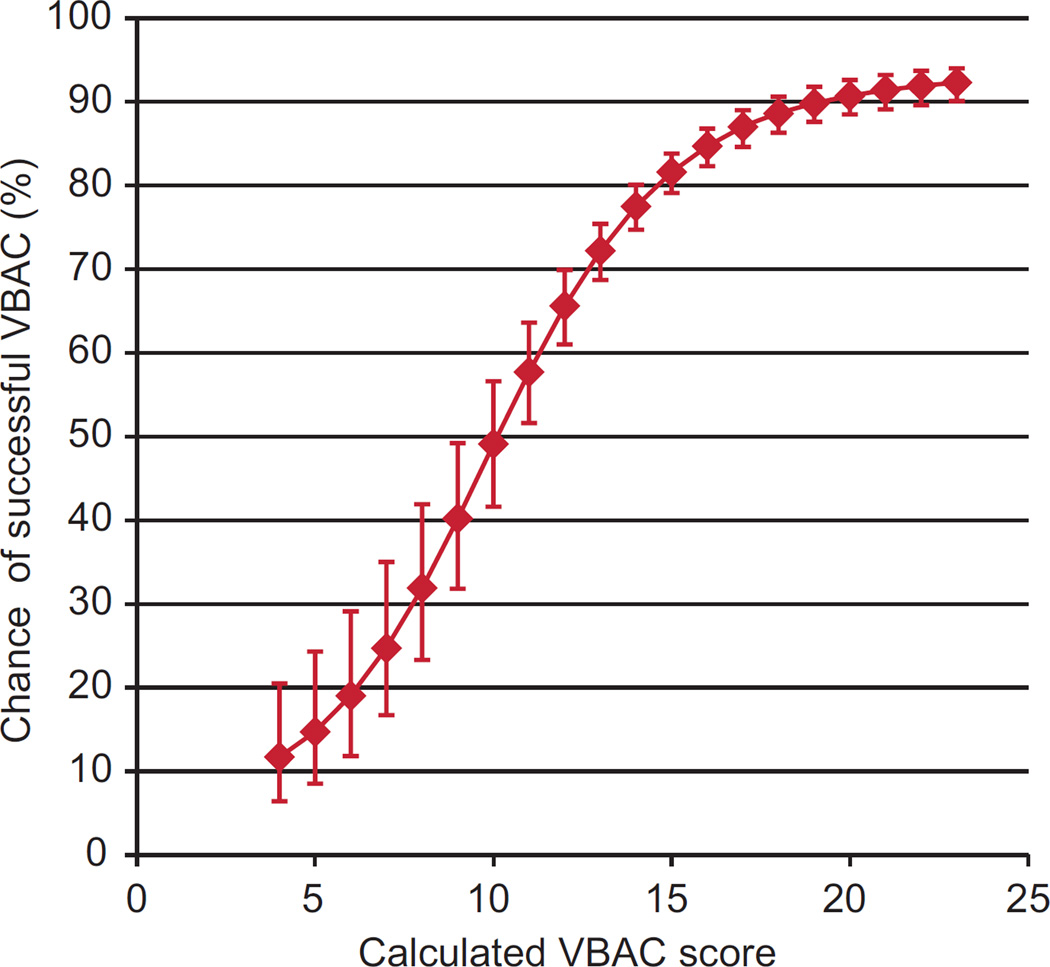
The coefficients of the regression equation were integrated into a prediction model based on the initial cervical examination to calculate an integer VBAC score (Box 1). The VBAC score was correlated with the TOLAC success rate, as demonstrated in Table 2 and graphically depicted in Figure 3. Prediction of TOLAC success at the time of admission was highly dependent on the initial cervical examination. However, using the Bishop score alone would only generate an AUC of 0.65. Women with an admission integer VBAC score less than 10 had a likelihood of TOLAC success of less than 50%. Patients with an admission score more than 16 had a TOLAC success rate more than 85%. Even when women without a history of vaginal delivery were analyzed separately, these cutoffs remained the same.
Box 1. Calculation of Integer Vaginal Birth After Cesarean Score.
Calculate the Bishop score using the cervical examination at the time of admission
Add 4 points for history of vaginal delivery
Add 2 points if prepregnancy body mass index is less than 30
Add 3 points if primary cesarean delivery was not because of a recurring indication
Add 2 points if maternal age at the time of delivery is younger than 35 years
Sum total score
Table 2.
Chance of Successful Vaginal Birth After Cesarean Delivery Based on Calculated Vaginal Birth After Cesarean Delivery Score
| Calculated VBAC Score |
No. of Study Participants |
Chance of Successful VBAC |
Actual VBAC Success Rate |
|---|---|---|---|
| 4 | 2 (0.17) | 11.7 (6.4–20.5) | 0.0 |
| 5 | 3 (0.26) | 14.7 (8.5–24.3) | 33.3 |
| 6 | 5 (0.43) | 19.0 (11.8–29.1) | 20.0 |
| 7 | 5 (0.43) | 24.7 (16.7–35.0) | 40.0 |
| 8 | 7 (0.60) | 31.9 (23.3–41.9) | 42.9 |
| 9 | 16 (1.37) | 40.2 (31.8–49.2) | 25.0 |
| 10 | 23 (1.97) | 49.1 (41.6–56.6) | 60.9 |
| 11 | 46 (3.93) | 57.7 (51.6–63.6) | 58.7 |
| 12 | 58 (4.96) | 65.6 (61.0–69.9) | 65.5 |
| 13 | 95 (8.12) | 72.2 (68.7–75.4) | 73.7 |
| 14 | 102 (8.72) | 77.5 (74.7–80.1) | 71.3 |
| 15 | 150 (12.82) | 81.6 (79.1–83.8) | 80.7 |
| 16 | 134 (11.45) | 84.7 (82.3–86.8) | 84.2 |
| 17 | 144 (12.31) | 87.0 (84.6–89.0) | 86.1 |
| 18 | 139 (11.88) | 88.6 (86.3–90.6) | 92.1 |
| 19 | 94 (8.03) | 89.8 (87.6–91.8) | 90.4 |
| 20 | 62 (5.30) | 90.7 (88.5–92.6) | 91.9 |
| 21 | 48 (4.10) | 91.4 (89.1–93.2) | 91.7 |
| 22 | 25 (2.14) | 91.9 (89.6–93.7) | 96.0 |
| 23 | 12 (1.03) | 92.3 (90.1–94.0) | 91.7 |
VBAC, vaginal birth after cesarean delivery; CI, confidence interval.
Data are n (%),% (95% CI), or %.
Fig. 3.
Correlation between calculated vaginal birth after cesarean delivery (VBAC) score and successful trial of labor after cesarean delivery.
Metz. Simple VBAC Prediction Model. Obstet Gynecol 2013.
The model also was compared with two existing nomograms for prediction of successful VBAC using the method of Delong et al.21 When compared with the model developed by Grobman et al12 for use at the time of the first prenatal visit, our model performed better with an AUC of 0.71 compared with 0.65 (P = .004). The majority of the discrepancy between the two models was found in women with lower VBAC scores having lower predicted success in our model than in the Grobman et al12 model (Table 3). Similarly, when compared with the later model by Grobman et al8 for use at the time of admission, our model performed comparably with an AUC of 0.70 compared with 0.66 (P = .046). In this comparison, most of the discrepancy between the models was found at the high end of our calculated integer VBAC score (Table 3).
Table 3.
Comparison of Proposed Vaginal Birth After Cesarean Delivery Score With Existing Nomograms
| Calculated VBAC Score |
Successful VBAC With Proposed Model |
Successful VBAC Calculated From Grobman et al12 Model (2007) |
Successful VBAC Calculated From Grobman et al8 Model (2009) |
|---|---|---|---|
| 4 | 11.7 | 49.0 | 35.9 |
| 5 | 14.7 | 58.5 | 31.5 |
| 6 | 19.0 | 56.0 | 37.5 |
| 7 | 24.7 | 52.4 | 29.6 |
| 8 | 31.9 | 56.6 | 50.7 |
| 9 | 40.2 | 63.0 | 43.1 |
| 10 | 49.1 | 65.2 | 46.8 |
| 11 | 57.7 | 67.6 | 54.0 |
| 12 | 65.6 | 71.1 | 56.0 |
| 13 | 72.2 | 72.6 | 57.8 |
| 14 | 77.5 | 73.8 | 60.5 |
| 15 | 81.6 | 75.9 | 64.3 |
| 16 | 84.7 | 78.4 | 68.4 |
| 17 | 87.0 | 79.5 | 71.6 |
| 18 | 88.6 | 81.4 | 75.4 |
| 19 | 89.8 | 82.1 | 77.9 |
| 20 | 90.7 | 87.7 | 83.1 |
| 21 | 91.4 | 88.8 | 84.5 |
| 22 | 91.9 | 89.1 | 85.5 |
| 23 | 92.3 | 89.2 | 88.5 |
VBAC, vaginal birth after cesarean delivery
Data are %.
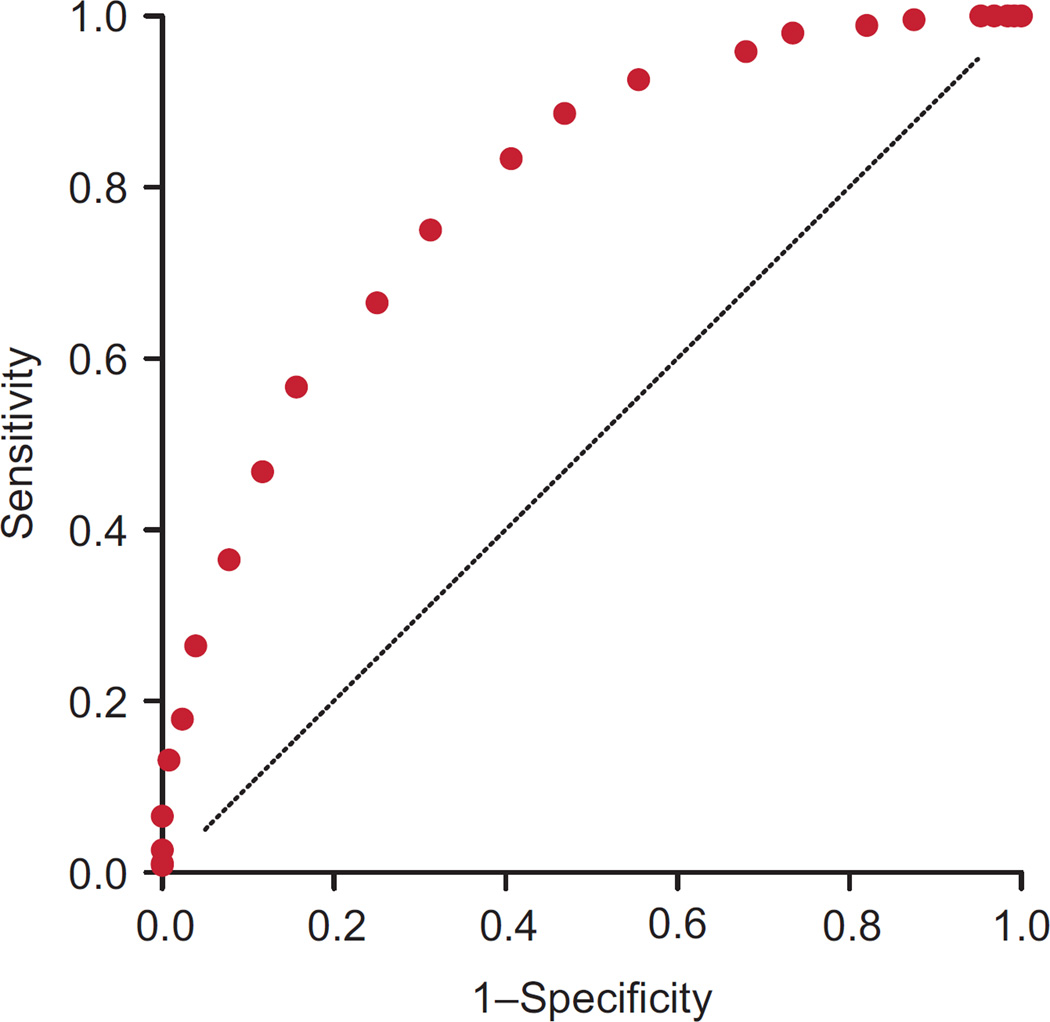
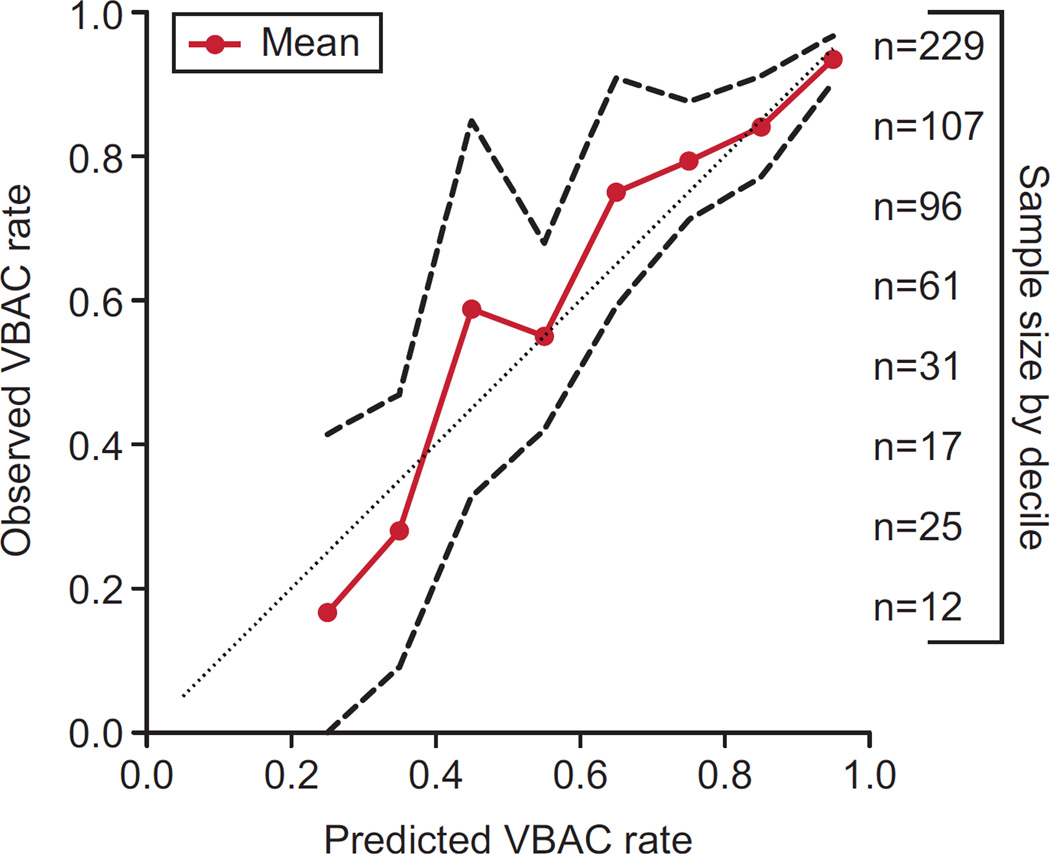
An external validation of the model also was pursued. Five hundred eighty-five women with one previous cesarean delivery undergoing TOLAC were identified from an independent database at another institution. The overall rate of VBAC success in this patient population was 78.3% (n = 457). The VBAC score performed well in this independent cohort, with an AUC of 0.80 (95% CI 0.76–0.84) (Fig. 4). The predictions of our model were similar to observed values across all deciles of predicted probabilities (Fig. 5). In addition, the cut points of less than 10 and more than 16 were appropriate, with a rate of success of 37.4% (95% CI 27.2–47.5) and 94.4% (90.9–97.8), respectively.
Fig. 4.
Receiver operating characteristic curve for validation of vaginal birth after cesarean score in an independent cohort. The area under the curve was 0.80 (95% confidence interval 0.76–0.84).
Metz. Simple VBAC Prediction Model. Obstet Gynecol 2013.
Fig. 5.
Comparison of observed predicted vaginal birth after cesarean (VBAC) rates in an independent cohort. For each decile of predicted probability, the solid mean line nears the line of equality, with dashed lines indicating 95% confidence intervals. The numbers on the right side of the figure correspond to the number of patients in each decile (each of these numbers correspond to a dot on the plot moving from highest to lowest).
Metz. Simple VBAC Prediction Model. Obstet Gynecol 2013.
DISCUSSION
A number of VBAC prediction models have been developed,4–12 some of which incorporate the cervical examination.4–8 However, many of these models do not use variables available at the time of admission or were not created using a regression model. We have developed and validated a simple prediction model based on the Bishop score at the time of admission to more accurately counsel women regarding their chances of successful VBAC.
The most recently published nomogram for use at the time of admission utilizing data from the Maternal-Fetal Medicine Units Network includes several other variables such as a history of VBAC and ethnicity.8 Although useful and reproducible,22 the model used by Grobman et al8 is somewhat complicated. Our model is simple to use at the time of admission and performed comparably, especially at the extremes of our prediction score. Our data are in agreement with those of Grobman et al,8 in that they indicate that data available at the time of admission improve the ability to predict VBAC success.
In the initial publications by Grobman et al,8,12 the AUC was more favorable. This is likely, in part, a result of the inclusion of women who had a history of successful VBAC. This variable was the strongest predictor of successful VBAC in their model but was not utilized in our study because women with a history of successful VBAC were excluded. These women are highly likely to have another successful VBAC and would improve the fit and AUC of the model. We thought that a prediction model would be most useful clinically in counseling women with only a primary cesarean delivery and only for the birth immediately after the primary cesarean delivery. Thus, we did not include women with a history of successful VBAC in our model development, because it is likely that these women would reattempt VBAC regardless of counseling. Unique to our study is the assessment of women who had a primary cesarean delivery in our system with an analysis of only their next delivery within our system. Therefore, our study population is the group for which the decision of proceeding with TOLAC is most important and will influence the mode of delivery for all subsequent pregnancies. Additionally, our population is representative of both tertiary and community centers. There was no specific hospital or institutional protocol delineating which patients should be offered TOLAC during this time period; the decision to offer TOLAC was practitioner-dependent.
One of the strengths of the study is that we validated the model both internally with bootstrapping and externally in an independent cohort. The strength of the model was further demonstrated by comparing the observed compared with expected success rates for each decile of predicted probability in this independent cohort. Given the best performance of the model at the upper end of the curve, we know that it can be used to reliably counsel women with a high VBAC score and inform them that pursuing a TOLAC is worthwhile. If women who had otherwise planned a repeat cesarean delivery are found to have a high chance of VBAC success at the time of admission, some of them may opt to pursue TOLAC, with a resultant reduction in the number of cesarean deliveries. There is more variance with the lower VBAC scores, with less of our population in these deciles. We would not advocate for practitioner refusal to pursue TOLAC based simply on a low VBAC score, but we hope this model can guide patient counseling.
The study is limited by its retrospective nature. We relied on input into the electronic medical record by trained nursing staff. Also, our obstetric population is relatively homogeneous (mostly Caucasian, married, insured), which may favor the performance of our model when compared with previously created models. It also may limit the generalizability to more heterogeneous and high-risk populations. As with any model assessing TOLAC success, we were unable to account for physician counseling, labor management, or patient preference. There were many women who chose an elective repeat cesarean delivery even though they would be considered good candidates for TOLAC. Some of these women presented in spontaneous labor with a favorable cervical examination. If anything, inclusion of these women in the development of the prediction models would make a favorable cervix seem less predictive of successful TOLAC and likely would falsely lower the calculated AUC.
Although our model accounts for the initial cervical examination, it does not account for whether a patient was induced. Other published literature suggests that women undergoing induction of labor are less likely to have a successful VBAC.23 Women in our study population who were induced had a favorable initial Bishop score and were more likely to have a history of vaginal delivery than the rest of the cohort. We suspect that this reflects a decision of practitioners before the time of admission to proceed with elective repeat cesarean delivery in women with an unfavorable cervix, and to proceed with induction only in women whom they anticipated would have a successful VBAC. Our model can be applied to women in spontaneous labor as well as to those undergoing induction of labor, because both of these groups were included in the development of the prediction model.
In conclusion, we have generated a simple, validated, clinically useful model for prediction of TOLAC success at the time of admission for the pregnancy after a primary cesarean delivery. This model is most applicable in women with a favorable or unfavorable cervical examination at the time of admission to the labor and delivery unit and allows for more directed TOLAC counseling, rather than quoting a general population-based 60–80% chance of success. These methods can be applied to other populations to establish region-specific prediction models, and they can be applied prospectively to determine success in a population committed to TOLAC.
Acknowledgments
Supported by the University of Utah Study Design and Biostatistics Center, with funding, in part, from research grant number 8UL1-TR000105 (National Center for Research Resources).
The authors thank Anne Lynch, MD, MSPH, Jan Hart, MSPH, and Amanda Allshouse, MS, for the provision of data and statistical analysis used in the external validation portion of the study.
Footnotes
Presented in abstract form at the 59th Annual Meeting of the Society for Gynecologic Investigation, March 21–24, 2012, San Diego, California.
Financial Disclosure
The authors did not report any potential conflicts of interest.
REFERENCES
- 1.Landon MB, Hauth JC, Leveno KJ, Spong CY, Leindecker S, Varner MW, et al. Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med. 2004;351:2581–2589. doi: 10.1056/NEJMoa040405. [DOI] [PubMed] [Google Scholar]
- 2.McMahon MJ, Luther ER, Bowes WA, Olshan AF. Comparison of a trial of labor with an elective second cesarean section. N Engl J Med. 1996;335:689–695. doi: 10.1056/NEJM199609053351001. [DOI] [PubMed] [Google Scholar]
- 3.National Institutes of Health Consensus Development Conference Statement: vaginal birth after cesarean: new insights March 8–10, 2010. Obstet Gynecol. 2010;115:1279–1295. doi: 10.1097/AOG.0b013e3181e459e5. [DOI] [PubMed] [Google Scholar]
- 4.Weinstein D, Benshushan A, Tanos V, Zilberstein R, Rojansky N. Predictive score for vaginal birth after cesarean section. Am J Obstet Gynecol. 1996;174:192–198. doi: 10.1016/s0002-9378(96)70393-9. [DOI] [PubMed] [Google Scholar]
- 5.Pickhardt MG, Martin JN, Jr, Meydrech EF, Blake PG, Martin RW, Perry KG, Jr, et al. Vaginal birth after cesarean delivery: are there useful and valid predictors of success or failure? Am J Obstet Gynecol. 1992;166:1811–1819. doi: 10.1016/0002-9378(92)91572-r. [DOI] [PubMed] [Google Scholar]
- 6.Flamm BL, Geiger AM. Vaginal birth after cesarean delivery: an admission scoring system. Obstet Gynecol. 1997;90:907–910. doi: 10.1016/s0029-7844(97)00531-0. [DOI] [PubMed] [Google Scholar]
- 7.Gonen R, Tamir A, Degani S, Ohel G. Variables associated with successful vaginal birth after one cesarean section: a proposed vaginal birth after Cesarean score. Am J Perinatol. 2004;21:447–453. doi: 10.1055/s-2004-835961. [DOI] [PubMed] [Google Scholar]
- 8.Grobman WA, Lai Y, Landon MB, Spong CY, Leveno KJ, Rouse DJ, et al. Does information available at admission for delivery improve prediction of vaginal birth after cesarean? Am J Perinatol. 2009;26:693–701. doi: 10.1055/s-0029-1239494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith GC, White IR, Pell JP, Dobbie R. Predicting cesarean section and uterine rupture among women attempting vaginal birth after prior cesarean section. PLoS Med. 2005;2:871–878. doi: 10.1371/journal.pmed.0020252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Srinivas SK, Stamilio DM, Stevens EJ, Odibo AO, Peipert JF, Macones GA. Predicting failure of a vaginal birth attempt after cesarean delivery. Obstet Gynecol. 2007;109:800–805. doi: 10.1097/01.AOG.0000259313.46842.71. [DOI] [PubMed] [Google Scholar]
- 11.Hashima JN, Guise JM. Vaginal birth after cesarean: a prenatal scoring tool. Am J Obstet Gynecol. 2007;196:e22–e23. doi: 10.1016/j.ajog.2006.10.884. [DOI] [PubMed] [Google Scholar]
- 12.Grobman WA, Lai Y, Landon MB, Spong CY, Leveno KJ, Rouse DJ, et al. Development of a nomogram for prediction of vaginal birth after cesarean delivery. Obstet Gynecol. 2007;109:806–812. doi: 10.1097/01.AOG.0000259312.36053.02. [DOI] [PubMed] [Google Scholar]
- 13.Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA, et al. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol. 2006;107:1226–1232. doi: 10.1097/01.AOG.0000219750.79480.84. [DOI] [PubMed] [Google Scholar]
- 14.Bishop EH. Pelvic scoring for elective induction. Obstet Gynecol. 1964;24:266–268. [PubMed] [Google Scholar]
- 15.Institute of Medicine. Resource sheet, “weight gain during pregnancy: reexamining the guidelines” May 2009. [Retrieved October 23, 2011]; Available at: www.iom.edu. [Google Scholar]
- 16.Royston P, Sauerbrei W. Bootstrap assessment of the stability of multivariable models. Stata J. 2009;9:547–570. [Google Scholar]
- 17.Harrell FE, Lee KL, Califf RM, Pryor DB, Rosati RA. Regression modelling strategies for improved prognostic prediction. Stat Med. 1984;3:143–152. doi: 10.1002/sim.4780030207. [DOI] [PubMed] [Google Scholar]
- 18.Harrell FE, Jr, Lee KL, Mark DB. Tutorial in biostatistics: multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–387. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 19.Steyerberg EQ, Harrell FE, Borsboom GJ, Eijkemans MJ, Vergouwe Y, Habbema JD. Internal validation of predictive models: efficiency of some procedures for logistic regression analysis. J Clin Epidemiol. 2001;54:774–781. doi: 10.1016/s0895-4356(01)00341-9. [DOI] [PubMed] [Google Scholar]
- 20.Hosmer DW, Lemeshow S. Applied logistic regression. 2nd. New York (NY): John Wiley & Sons; 2000. p. 162. [Google Scholar]
- 21.DeLong ER, DeLong DM, Clark-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–845. [PubMed] [Google Scholar]
- 22.Costantine MM, Fox K, Pacheco LD, Mateus J, Hankins GD, Grobman WA, et al. Does information available at delivery improve the accuracy of predicting of vaginal birth after cesarean? Validation of the published models in an independent patient cohort. Am J Perinatol. 2011;28:293–298. doi: 10.1055/s-0030-1271214. [DOI] [PubMed] [Google Scholar]
- 23.Grobman WA, Gilbert S, Landon MB, Spong CY, Leveno KJ, Rouse DJ, et al. Outcomes of induction of labor after one prior cesarean. Obstet Gynecol. 2007;109:262–269. doi: 10.1097/01.AOG.0000254169.49346.e9. [DOI] [PubMed] [Google Scholar]