Abstract
We propose a taxonomy of psychopathology based on patterns of shared causal influences identified in a review of multivariate behavior genetic studies that distinguish genetic and environmental influences that are either common to multiple dimensions of psychopathology or unique to each dimension. At the phenotypic level, first-order dimensions are defined by correlations among symptoms; correlations among first-order dimensions similarly define higher-order domains (e.g., internalizing or externalizing psychopathology). We hypothesize that the robust phenotypic correlations among first-order dimensions reflect a hierarchy of increasingly specific etiologic influences. Some nonspecific etiologic factors increase risk for all first-order dimensions of psychopathology to varying degrees through a general factor of psychopathology. Other nonspecific etiologic factors increase risk only for all first-order dimensions within a more specific higher-order domain. Furthermore, each first-order dimension has its own unique causal influences. Genetic and environmental influences common to family members tend to be nonspecific, whereas environmental influences unique to each individual are more dimension-specific. We posit that these causal influences on psychopathology are moderated by sex and developmental processes. This causal taxonomy also provides a novel framework for understanding the heterogeneity of each first-order dimension: Different persons exhibiting similar symptoms may be influenced by different combinations of etiologic influences from each of the three levels of the etiologic hierarchy. Furthermore, we relate the proposed causal taxonomy to transdimensional psychobiological processes, which also impact the heterogeneity of each psychopathology dimension. This causal taxonomy implies the need for changes in strategies for studying the etiology, psychobiology, prevention, and treatment of psychopathology.
Keywords: Psychopathology, taxonomy, etiology, general factor, p-factor
Research on psychopathology has many goals, but the identification of its causes is one of the most important. Knowledge of the causes of psychopathology will greatly improve our chances of effectively ameliorating and preventing the suffering and functional impairment associated with it. Psychopathology research is now moving from a long phase of documenting correlations between psychopathology and variables that might be causes to studies that use experimental and quasi-experimental designs to conduct informative tests of causal hypotheses (Jaffee & Price, 2012; Jaffee, Strait, & Odgers, 2012; Lahey & D’Onofrio, 2010; Rutter, 2007b). The goal of this paper is to facilitate studies of the genetic and environmental etiology of psychopathology by providing an organizational framework in the form of a causal taxonomy of psychopathology in children, adolescents, and adults.
The purpose of any taxonomy is to organize disparate elements according to their common and varying properties to reveal higher-order relations among them. The taxonomies of organisms proposed by Aristotle (384–322 BCE), Pliny the Elder (23–79 CE), and Carl Linnaeus (1707–1778) organized living things according to a hierarchy of similarities in their physical characteristics that ranged from more specific (e.g., species) to more general (e.g., taxa). Without the heuristic of the Linnaean taxonomy, which placed humans with other primates based on physical similarities, Darwin’s subsequent articulation of the theory of natural selection may have been far more difficult, if not impossible (Hernadi, 1981).
The taxonomies of psychopathology that currently dominate research and clinical practice are phenomenologic. That is, they are based on observations—both formal and informal—that some symptoms co-occur more often than other symptoms (Quay, 1986). Herein, we propose a causal taxonomy of psychopathology based on a systematic review of the literatures (see online Supplement 1 for a description of the review process) on both: (1) correlations among observed measures of psychopathology within individuals in the population (i.e., phenotypic correlations), and (2) correlations among inferred genetic and environmental influences on psychopathology. The causal influences referred to in this paper are inferred using a variety of methods, particularly multivariate behavior genetic analyses of twin and other family data that can parse phenotypic correlations into genetic and environmental influences (Neale & Cardon, 1992).
Our central hypothesis is that the primary reason that phenotypic dimensions are correlated is that they have shared causes—and shared causes are the basis for a causal taxonomy. At this point in the development of the causal taxonomy, we are agnostic about the specific mechanism(s) through which causal influences are shared. There are at least three ways in which such sharing could occur. First, a causal influence (e.g., a set of genetic variants or an experience) may directly influence multiple dimensions of psychopathology in nonspecific (i.e., pleiotropic i) ways. As we describe below, this may be mediated by a transdiagnostic psychobiological process (e.g., responsiveness to reward) that is related to multiple dimensions of psychopathology. Second, a causal influence could influence one symptom (or dimension of symptoms), which could then increase risk for another symptom (e.g., insomnia may cause anergia) (Borsboom & Cramer, 2013; Fergusson, Boden, & Horwood, 2011; Hofmann, Curtiss, & McNally, 2016), indirectly resulting in the same etiologic factor influencing both symptoms. These two pathways of shared causal influences may prove difficult to resolve, but ultimately both can and should be incorporated in any causal taxonomy. Third, causal influences may themselves be correlated, but not linked to different dimensions of psychopathology through the same causal pathway. This could happen, for example, if two genetic variants are in linkage disequilibrium (i.e., correlated in the genome) and related to different dimensions of psychopathology through independent causal processes. Whereas the first two causal pathways can be easily incorporated in a causal taxonomy, the third complicates it. Two correlated causal factors that operate independently would give the appearance of shared causation when it does not exist. Thus, future efforts will need to determine the extent to which each pattern occurs.
We propose a causal taxonomy that is hierarchical in the sense that it organizes psychopathology from specific symptoms to first-order dimensions of those symptoms to higher-order domains that are defined by correlations among first-order dimensions—and their inferred causes (Krueger & Piasecki, 2002). The proposed taxonomy is relatively comprehensive in the sense that it addresses a broad range of psychopathology across the life span. Most of the existing data reviewed in this paper are on relatively common forms of psychopathology, but there are now sufficient data on autism spectrum disorder, mania, and schizophrenia to offer new hypotheses on their relationship to the taxonomy. To limit the scope of this initial taxonomy, however, we do not address personality disorders. Instead, we provide a brief review of the small relevant literature on personality disorders in Supplement 2 and suggest a framework for their necessary integration into future expanded causal taxonomies.
It is important to distinguish the goals of a causal taxonomy of psychopathology from those of causal models. A causal taxonomy organizes dimensions of psychopathology according to what is known or hypothesized about their shared and unique causes. In contrast, a causal model offers more detailed hypotheses regarding the specific shared and unique causal pathways and mechanisms that give rise to psychopathology. At this stage in the science, a causal taxonomy is the more attainable goal; once attained, a causal taxonomy should substantially facilitate proposing and testing causal models.
NATURE OF DEVELOPING PSYCHOPATHOLOGY
We use the classic psychological definition of psychopathology as any pattern of behavior—broadly defined to include actions, emotions, motivations, and cognitive and regulatory processes—that causes personal distress or impairs significant life functions, such as social relationships, education, work, and health maintenance (Bandura, 1969; Ullmann & Krasner, 1975).ii
Dimensions and Categories of Psychopathology
Practitioners and scientists have long created taxonomies of psychological dysfunction to organize observations and to generalize what was learned about one person to other persons with similar problems. The first taxonomies treated psychopathology as mutually exclusive nominal conditions (Kraepelin, 1919, 1921). This view provides the basis for the various versions of the Diagnostic and Statistical Manual and International Classification of Diseases. It is now clear, however, that at least the most prevalent forms of psychopathology can be understood as dimensional phenomena (Broman-Fulks et al., 2006; Crome, Baillie, Slade, & Ruscio, 2010; Hankin, Fraley, Lahey, & Waldman, 2005; Haslam et al., 2006; Krueger et al., 2004; Markon & Krueger, 2005; Pickles & Angold, 2003; Prisciandaro & Roberts, 2009; Van Os, Verdoux, Bijl, & Ravelli, 1999). Nonetheless, even if all forms of psychopathology prove to be inherently continuous, the causal taxonomy presented here is still relevant to categorical diagnoses (Pickles & Angold, 2003). Diagnoses can be viewed as pragmatic dichotomizations of continuous underlying dimensions when binary decisions must be made, as when clinicians must make the binary choice to treat or not treat (Kamphuis & Noordhof, 2009; Lahey, Applegate, Barkley, et al., 1994; Lahey, Applegate, McBurnett, et al., 1994). Thus, attempts have been made to select diagnostic thresholds for dichotomizing each dimension of psychopathology based on their relative levels of distress and functional impairment (Lahey, Applegate, Barkley, et al., 1994; Lahey, Applegate, McBurnett, et al., 1994). This allows one to attempt, within the limits imposed by existing knowledge (Rapee, Bogels, van der Sluis, Craske, & Ollendick, 2012), to select diagnostic thresholds at the point on each continuum above which the risks inherent in labeling and treating are less than the risks inherent in not labeling and treating (Kamphuis & Noordhof, 2009). Such dichotomization may come at the cost of decreased reliability, however (Fergusson & Horwood, 1995; Markon, Chmielewski, & Miller, 2011).
Structure of the Present Review
The most basic empirical basis for a causal taxonomy is the structure of cross-sectional phenotypic correlations: (a) among the symptoms that define each first-order dimension of psychopathology, (b) among first-order dimensions of psychopathology that define higher-order domains of psychopathology, and (c) among the higher-order domains. We briefly summarize these well-known patterns of cross-sectional correlations in this paper (and provide detailed reviews of this literature and the related literature on the criterion validity of first-order dimensions of psychopathology in Supplement 3). We then review the growing evidence that a hierarchical phenotypic model of the structure of psychopathology that includes a general factor, on which every first-order dimension loads, fits the data better—and provide more interpretive leverage—than models specifying only more specific higher-order (e.g., internalizing and externalizing) factors of psychopathology (Caspi et al., 2014; Lahey et al., 2012; Lahey et al., 2015). We next move from cross-sectional studies to longitudinal evidence on the correlational structure of dimensions of psychopathology over time. We examine the extent to which each first-order dimension measured at some time t predicts both itself and other dimensions of psychopathology at some future time t+1 (i.e., homotypic and heterotypic continuity, respectively). The observed patterns of cross-sectional and longitudinal phenotypic correlations among first-order dimensions of psychopathology (Angold, Costello, & Erkanli, 1999; Clark, Watson, & Reynolds, 1995) imply that some hypotheses regarding the causal influences that give rise to these correlations are more likely to be empirically supported than others. We then discuss evidence from behavior genetic and molecular genetic studies that allow inferences regarding the structure of genetic and environmental influences on psychopathology.
To facilitate communication, we employ commonly used terms in this paper. The downside of this choice is that the denotative and connotative meanings of these terms may communicate unintended propositions. For example, we use the terms “symptom” and “psychopathology” in a descriptive spirit and explicitly reject the medical-model implications of those terms (Bandura, 1969). Similarly, we use the terms, “internalizing” and “externalizing,” descriptively to refer to relatively specific higher-order factors of symptoms of depression and anxiety disorders (internalizing) and symptoms of attention-deficit/hyperactivity disorder (ADHD), oppositional defiant disorder (ODD), and conduct disorder (CD) in children and adolescents and to antisocial personality disorder (APD) and substance use disorders in adults (externalizing). We do not imply, however, that internalizing psychopathology reflects the internalization of psychic conflict or the overcontrol of emotions or that externalizing psychopathology reflects the acting out of mental conflicts or the undercontrol of impulses.
Overview of the Proposed Causal Taxonomy
Based on the systematic review of evidence, we state 12 hypotheses that constitute a causal taxonomy of psychopathology. These hypotheses describe a hierarchy of causal influences: Some genetic and environmental influences nonspecifically increase risk for all common first-order dimensions of psychopathology to varying degrees, other pleiotropic causal factors influence multiple dimensions only within more specific higher-order domains of psychopathology, and other casual influences are specific to each first-order dimension of psychopathology, or perhaps even to fine-grain subsets of symptoms.
The hypotheses that constitute the causal taxonomy have clear implications for understanding both the causes and the mechanisms underlying psychopathology. We hypothesize that the genetic and environmental influences on psychopathology operate through a number of psychobiological mechanisms, by which we mean relatively trait-like processes that can be understood at both psychological and biological levels of analysis. Most of these are hypothesized to be transdimensional psychobiological mechanisms, in the sense that individual differences in them operate at the level of higher-order factors, including the general factor, of psychopathology rather than individual first-order dimensions. This hypothesis is based on, and is consistent with, decades of research on relations between dispositional traits and psychopathology (Brooker et al., 2013; Kendler & Myers, 2010; Krueger, 1999; Krueger & Tackett, 2003; Nigg, 2006; Tackett, 2006; Vasey et al., 2013; Widiger, 2011), the transdiagnostic approach to psychopathology (Barlow, Sauer-Zavala, Carl, Bullis, & Ellard, 2014; Nolen-Hoeksema & Watkins, 2011), and is consistent with key aspects of the Research Domains Criteria (RDoC) initiative of the National Institute of Mental Health (Cuthbert & Kozak, 2013; Insel et al., 2010; Sanislow et al., 2010). We conclude with a discussion of important implications of the proposed causal taxonomy for the design of future research on etiology, prevention, and treatment.
CORRELATIONAL STRUCTURE OF FIRST-ORDER DIMENSIONS OF PSYCHOPATHOLOGY
First-order dimensions of psychopathology are defined by correlations among symptoms. These dimensions can be viewed as latent constructs in which each correlated symptom is viewed as an exchangeable indicator of the dimension and no single symptom is necessary to define the dimension. The fundamental questions for research at this level of taxonomy are which symptoms are correlated and how many relatively distinct first-order dimensions they define (Waldman, Lilienfeld, & Lahey, 1995). In Supplement 3, we review the empirical literature on first-order dimensions defined by symptoms in preschool children, school-age children and adolescents, and adults.
It is central to our thesis that the first-order dimensions defined by correlated DSM-IV symptoms are themselves correlated (Krueger & Markon, 2006a; Lahey, Rathouz, et al., 2008). Such correlations typically have been viewed as an inconvenient problem for categorical taxonomies, which seek to place each person in a single category of mental disorder that is qualitatively distinct from, and mutually exclusive of, all other mental disorders. The correlations among diagnoses mean that a person can, and often does, meet criteria for more than one diagnosis at the same time (Angold et al., 1999; Caron & Rutter, 1991). This extensive “comorbidity” often has been viewed as a sign of the failure of categorical taxonomies to achieve the Platonic goal of “carving nature at its joints” (Meehl, 2001).
Like others (Angold & Costello, 2009; Angold et al., 1999; Kendler et al., 2011; Lilienfeld, Waldman, & Israel, 1994), however, we believe that a new Gestalt is needed for the conceptualization of correlations (comorbidity) among mental disorders and first-order dimensions of psychopathology. These correlations are not a problem, but a profoundly important source of information about the nature of psychopathology (Krueger & Markon, 2006a, 2006b; Lahey, Van Hulle, Singh, Waldman, & Rathouz, 2011). Comorbidity is the figure, not the ground. Studying the nature of one dimension or category of psychopathology at a time, and ignoring the rich information inherent in its correlations with other dimensions or categories, is limiting in completely unnecessary ways (Lahey & Waldman, 2012).
The extensive research on the correlations among first-order dimensions (and diagnoses) of psychopathology is summarized in Supplement 3. The results of these studies support two conclusions:
Positive correlations among common forms of psychopathology, whether treated as dimensions or categories, are ubiquitous. This includes correlations among dimensions of psychopathology both within and across internalizing and externalizing domains.
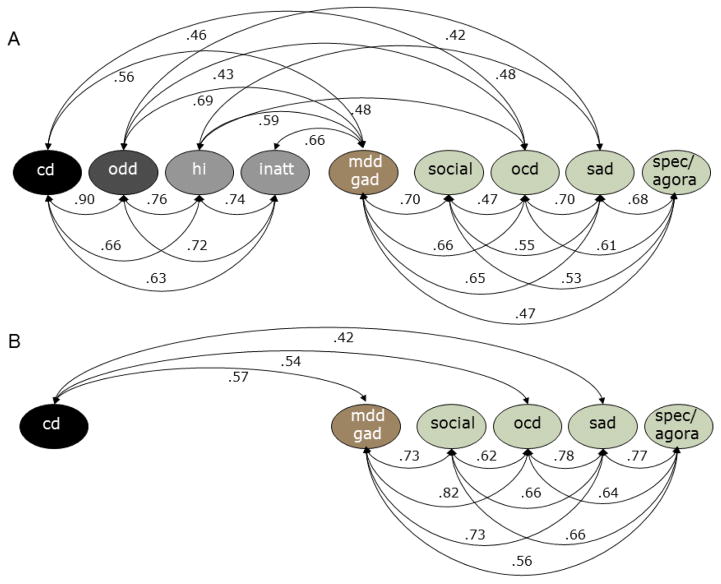
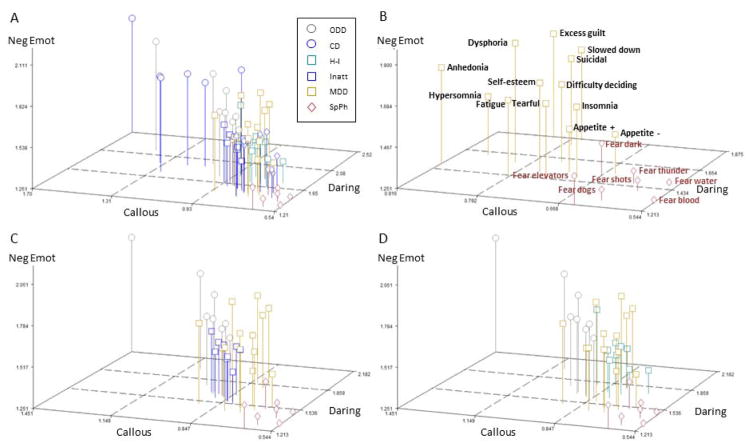
The correlations among the various forms of psychopathology are not uniform in their magnitudes, but are patterned. That is, some sets of dimensions (or categories) are consistently more strongly correlated than other sets. To fully discern the importance of the correlations among dimensions and categories of psychopathology, it is essential to recognize and model this patterning. The implications are discussed below in detail, but we present an illustrative example here. Correlations among latent first-order dimensions of psychopathology based on DSM-IV symptoms assessed in 2,025 pairs of 6–17 year olds in the representative Tennessee Twins Study twins (Lahey, Rathouz, et al., 2008) are shown in Figures 1A (for parent reports) and 1B (for youth self-reports). Although only correlations r ≥ .40 are shown to simplify the figure, all dimensions of symptoms were found to be significantly correlated at p < .05 in this sample with all other dimensions based on both informants. The highest correlations were among first-order dimensions within the higher-order internalizing and externalizing dimensions, but there were robust correlations between first-order dimensions across internalizing and externalizing domains, as well.
Figure 1.
Correlations among first-order latent dimensions of psychopathology identified in a sample of 2,025 pairs of 6–17 year old twins based on adult caretaker reports (A) and youth reports (B) of symptoms. Panel A redrawn from Figure 5 page 196 and panel B redrawn from Figure 7 page 199 (Lahey, Rathouz, et al., 2008). Note: ODD = oppositional defiant disorder; CD = conduct disorder; HI = hyperactivity-impulsivity; INATT = inattention; MDD = major depressive disorder; GAD = generalized anxiety disorder; social = social anxiety disorder; SAD = separation anxiety disorder; spec = specific phobia; agora = agoraphobia.
Note that if the correlational structure of dimensions of psychopathology were to vary substantially across age, sex, and other demographic groups, different causal taxonomies would be needed for different groups. In contrast, if the same structure emerges across groups, it would suggest a universal causal taxonomy of psychopathology. A review of the published literature on the invariance of the correlational structure of first-order dimensions of psychopathology is presented in Supplement 4, which suggests that the structure is substantially the same across age, sex, and race-ethnic groups in spite of differences in mean levels of some dimensions across groups.
Higher-order Factors of Psychopathology
Over 35 years ago, Achenbach made the seminal observation that matrices of the patterned correlations among symptoms of psychopathology could be subjected to factor analysis to identify broad higher-order dimensions of psychopathology (Achenbach & Edelbrock, 1978). Numerous studies have consistently extracted two higher-order factors, often labeled internalizing and externalizing, based on the pattern of correlations among first-order dimensions expressed as loadings on the higher-order factors in children, adolescents, and adults (Achenbach & Edelbrock, 1978; Blanco et al., 2015; Cosgrove et al., 2011; Kessler, Petukhova, & Zaslavsky, 2011; Lahey, Rathouz, et al., 2008; Quay, 1986; Slade & Watson, 2006). Other studies have supported somewhat different higher-order factors of psychopathology. Krueger and Markon (2006a) conducted a meta-analysis of studies involving a total of 23,000 adults and found that the best-fitting model, which was invariant in females and males, was a 3-factor model specifying higher-order externalizing, distress, and fears factors. Thus, in studies of categorical diagnoses in adults, there is support for the distinction of three higher-order domains.
Robust Correlations among Higher-order Factors
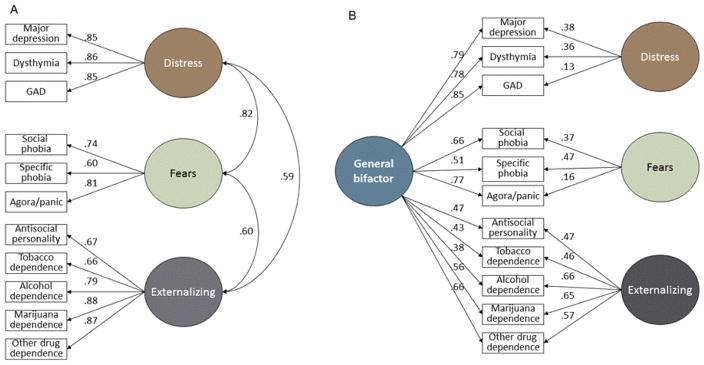
The cross-sectional studies noted above indicate that at least two higher-order factors account for much of the patterned correlations among first-order psychopathology dimensions across the life span. Nonetheless, it is also clear that these higher-order factors fail to fully account for the phenotypic correlations among first-order dimensions of psychopathology. This is because the higher-order factors are themselves substantially correlated. In children and adolescents, Lahey et al. (2008) reported that the higher-order internalizing and externalizing factors were significantly correlated at r = .54, and Krueger & Markon (2006a) found that higher-order latent internalizing and externalizing factors were correlated at r = 0.51. When three higher-order factors were extracted in the NESARC sample of adults, correlations among higher-order latent distress, fears, and externalizing factors ranged from r = 0.82 for distress and fears to r = 0.59 for externalizing and distress (Figure 2A) (Lahey et al., 2012).
Figure 2.
Best fitting models of the correlational structure of 11 categorical mental disorders in confirmatory factor analyses of diagnosis data from wave 1 of the NESARC sample (A) without a general psychopathology factor, and (B) with a general psychopathology factor. Figure 1, page 973 (Lahey et al., 2012), used by permission.
It may be fair to say that these correlations among higher-order factors of psychopathology are no longer a surprise to most psychologists. Indeed, as scientific findings go, these correlations seem be a bit of a yawn at first glance. This may explain why their profound importance has gone unnoticed for so long. Nonetheless, the replicated observation that the higher-order factors of psychopathology are robustly correlated with one another is central to the hypotheses developed in this paper regarding the causal taxonomy of psychopathology.
GENERAL FACTOR OF PSYCHOPATHOLOGY
A central element of the proposed causal taxonomy is the hypothesis that the extensively replicated pattern of correlations among both first- and higher-order factors of psychopathology described above reflects a general factor of psychopathology on which every first-order dimension loads.
Findings on the General Factor Model in Adults
In the large and representative NESARC sample (Lahey et al., 2012), we used a bifactor model (Holzinger & Swineford, 1937) in CFA to test the hypothesis of general factor psychopathology. A bifactor model quantifies the extent to which correlations among a set of dimensions reflect both a general factor on which every dimension loads and some number of more specific subfactors on which subsets of the same dimensions load. The more specific subfactors are specified as orthogonal to (i.e., uncorrelated with) the general factor and reflect correlations among the subsets of dimensions after the correlations among all dimensions captured by the general factor have been taken into account (Reise, 2012). Figure 2B illustrates the bifactor model of correlations among diagnoses in the last 12 months in NESARC consisting of a general factor on which all diagnoses loaded and more specific fears, distress, and externalizing factors. In this bifactor model, the correlations among the fears, distress, and externalizing factors were constrained to be zero to test the hypothesis that they were explained by the general factor (Brown, 2006). A model specifying three correlated higher-order factors of externalizing, fears, and distress plus the general psychopathology factor (Figure 2B) fit significantly better than the correlated 3-factor model in Figure 2A (Lahey et al., 2012). This suggests that the significant loadings of every first-order dimension on the general factor substantially account for the correlations among the higher-order externalizing, distress, and fears factors. In interpreting these findings, it is important to note that the inclusion of a general psychopathology factor in a bifactor model changes the interpretation of the higher-order fears, distress, and externalizing factors. They reflect the residual covariation among the diagnoses loading on each of these factors above and beyond the correlations among all diagnoses captured by the general factor.
A subsequent study tested the general factor hypothesis in young adults using a partly different set of mental disorders and somewhat different methods (Caspi et al., 2014). In the longitudinal Dunedin Study, mental disorders were repeatedly assessed using reliable and valid measures in a birth cohort of about 1,000 individuals. Symptoms of each disorder in the past 12 months were assessed across ages 18, 21, 26, 32, and 38 years. Aggregated counts of symptoms over the repeated assessments were treated as ordinal scales for 10 mental disorders. In addition, fears were quantified by counting the number of diagnoses of simple phobia, social anxiety disorder, agoraphobia, and panic disorder. Thus, the data used by Caspi et al. (2014) differed from that used by Lahey et al. (2012) by being averaged over multiple assessments across early adulthood, including symptoms of serious but low-prevalence disorders (mania and schizophrenia), and combining fears dimensions into a single first-order dimension. Caspi and colleagues hypothesized three correlated higher-order factors of internalizing (MDD, GAD, and fears), externalizing (CD and four dimensions of substance dependence), and “thought disorder” (mania, schizophrenia, and OCD), and a general factor specified in a bifactor model. Formal tests of improvement in fit were not be conducted because their alternative models were not nested, but the fit statistics suggested that a bifactor model specifying a general factor fit as well or better than a model specifying three correlated dimensions of psychopathology, but only when mania, schizophrenia, and OCD loaded only on the general factor and not also on their own higher-order “thought disorder” factor (Caspi et al., 2014). Thus, the findings of the Caspi et al. study are generally consistent with those of Lahey et al. (2012), but provide additional information on uncommon but serious forms of psychopathology.
Findings on the General Factor Model in Children and Adolescents
A number of studies also have tested the applicability of the general factor model to children and adolescents. Parent-reported symptoms of psychopathology were assessed in a community sample of 3-year olds (Olino, Dougherty, Bufferd, Carlson, & Klein, 2014). In CFA, a model that included internalizing and externalizing factors and a general factor on which all first-order dimensions of psychopathology loaded fit better than a correlated 2-factor (internalizing, externalizing) model (Olino et al., 2014). We also conducted a replication test of the general factor model using data on parent ratings of psychopathology in 5–11 year old girls from the large and representative Pittsburgh Girls Study (Keenan et al., 2010). A model that included higher-order internalizing and externalizing factors and a general factor fit significantly better than a correlated 2-factor model (Lahey et al., 2015).
We conducted a test of the general factor model in children and adolescents using data from the Tennessee Twin Study sample of 1,569 twin pairs (ages 9–17 years) (Lahey, Rathouz, et al., 2008). Data on symptoms of 11 common dimensions of psychopathology were collected from both parents and youth using a reliable and valid structured interview. Two alternative models of the phenotypic structure of the dimensions of psychopathology were compared using CFA (Tackett et al., 2013). First, a correlated 2-factor model was specified by allowing CD, ODD, inattentive, and hyperactive/impulsive symptom dimensions to load on the externalizing factor. The internalizing factor was defined by the dimensions of MDD, GAD, social anxiety disorder, agoraphobia, separation anxiety disorder (SAD), specific phobia, and OCD. This model fit the data well, but with a correlation between the latent internalizing and externalizing factors of r = 0.84. This correlated 2-factor model was compared to a general factor model, in which internalizing and externalizing were defined in the same way, but all symptom dimensions also were allowed to load on a general factor. This model fit significantly better than the correlated 2-factor model without a general factor (Tackett et al., 2013). In a separate study of a representative sample of adolescents, CFAs indicated that the best-fitting bifactor model included a general factor (Noordhof, Krueger, Ormel, Oldehinkel, & Hartman, 2015). Furthermore, other studies that support the general factor model in adolescents are discussed below in relation to specific issues (Carragher et al., 2016; Laceulle, Vollebergh, & Ormel, 2015; Patalay et al., 2015).
ALTERNATIVE EXPLANATIONS FOR THE HIERARCHICAL CORRELATIONAL STRUCTURE OF PSYCHOPATHOLOGY
To this point, we have developed the argument that a hierarchical model of the phenotypic structure of common forms of psychopathology that includes a general factor and at least two more specific higher-order factors of psychopathology fits the data on the correlations among first-order dimensions of psychopathology better than alternative structural models. To evaluate this hypothesis, both theoretically and empirically, it is important to consider viable alternative interpretations of the findings just reviewed that view the general factor as an artifact of how psychopathology is defined and measured. One such alternative hypothesis is that the general factor is potentially an artifact of using the same symptoms to define multiple first-order dimensions of psychopathology. A second alternative hypothesis is that the general factor could be an artifact of imprecise or systematically biased measurement.
Is the General Factor an Artifact of Shared Symptoms?
It is possible that dimensions of psychopathology load on the general factor of psychopathology partly or wholly because essentially the same symptoms are used to define multiple first-order dimensions.
Role of Shared Symptoms within Higher-order Domains of Psychopathology
The use of essentially the same symptoms to define more than one diagnosis varies across higher-order domains. Table 1 shows that the four DSM diagnoses in the distress domain share many similar symptoms. Thus, it seems likely that the first-order dimensions within the distress domain are correlated with one another at least partly because the same or similar symptoms are used in the definition of each dimension. In contrast, no symptoms are explicitly shared by the various diagnoses in the fears domain (not tabled for that reason). During adulthood, there are no symptoms shared by the externalizing diagnoses of APD and substance use disorders, although some substance abuse criteria are similar to APD symptoms. Similarly, there are no symptoms common to the externalizing dimensions of inattention, hyperactivity-impulsivity, ODD, and CD during childhood and adolescence. Thus, the robust correlations among the first-order dimensions within the externalizing domains are not solely artifacts of shared symptoms, but shared symptoms clearly could be part of the basis of the higher-order distress domain.
Table 1.
Identical and similar symptoms that define dimensions of psychopathology in the distress and externalizing domains.
|
Distress
|
Externalizing (childhood and adolescence)
|
Externalizing (adulthood)
|
||||||
|---|---|---|---|---|---|---|---|---|
| MDD | Dysthymia | GAD | PTSD | ADHD | ODD | CD | SUD | APD |
| Dysphoria | Dysphoria | |||||||
| Anhedonia | Anhedonia | |||||||
| Fatigue | Fatigue | Fatigue | ||||||
| Worthlessness | Worthlessness | |||||||
| Irritability | Irritability | Irritability | Irritability | |||||
| Eating | Eating | |||||||
| Insomnia | Insomnia | Insomnia | Insomnia | |||||
| Concentration | Concentration | Concentration | Concentration | Concentration | ||||
| Restlessness | Restlessness | Restlessness | ||||||
| Impulsivity | Impulsivity | |||||||
Note: MDD = major depressive disorder; GAD = generalized anxiety disorder; PTSD = post-traumatic stress disorder; ADHD = attention-deficit/hyperactivity disorder; ODD = oppositional defiant disorder; CD = conduct disorder; SUD = substance use disorder; APD = antisocial personality disorder.
Role of Shared Symptoms in Correlations between Higher-order Dimensions of Psychopathology
It is important to note in Table 1 that three symptoms (irritability, restlessness, and difficulty concentrating) are common to dimensions in two different higher-order domains. This raises the possibility that the phenotypic correlations between the distress and externalizing factors shown in Figure 2A are partly an artifact of shared symptoms across domains. In contrast, shared symptoms cannot explain the finding that the higher-order fears and distress factors, which share no symptoms, are the two most strongly correlated higher-order factors (Krueger & Markon, 2006a).
Role of Shared Symptoms in the General Factor of Psychopathology
It is possible that the general factor of psychopathology could partly reflect the subset of symptoms that are shared across externalizing and distress dimensions—irritability, dysphoria, inattention, anhedonia, fatigue, and others. Indeed, these symptoms may appear in the definitions of multiple first-order dimensions precisely because they reflect the general nature of psychopathology. Thus, we propose that these symptoms are closely related to the general factor of psychopathology because they are correlated with the dispositional traits of negative emotionality, which is related to the general factor (Tackett et al., 2013). Nonetheless, shared symptoms do not provide a complete explanation of the general factor of psychopathology. Figure 2B shows that dimensions of psychopathology in the fears domain load significantly on the general factor in spite of there being no symptoms that are shared with either the distress or externalizing dimensions.
Furthermore, studies of correlations among non-overlapping individual symptoms—rather than among dimensions of symptoms—provide strong tests of the extent to which the symptoms that are part of the definition of multiple dimensions could play a role in the general factor of psychopathology. Two such studies of item-level data confirmed the improved fit of models that include a general factor. CFAs of data from a representative sample of 2,175 Australian adolescents found that symptoms loaded on three correlated factors (internalizing, externalizing, and thought disorder). The addition of a general factor in a bifactor model significantly improved model fit, with strong evidence for invariance in the general factor model across sex (Carragher et al., 2016). Similarly, analyses of parent-rated symptoms in a large representative sample of 11–13 year olds found that a bifactor model specifying a general factor along with internalizing and externalizing factors fit better than a correlated internalizing-externalizing model (Patalay et al., 2015). Thus these findings argue against the possibility that overlapping symptoms contribute importantly to the general factor. Nonetheless, future research should consider the possibility that at least some similar symptoms that help define different disorders (e.g., irritability and insomnia) are important because they reflect transdiagnostic constructs.
Is the General Factor an Artifact of Imprecise Symptom Measurement?
The framers of the DSM/ICD nomenclatures incorporated the prevailing view that the same symptoms may occur for different reasons, which must be distinguished to make valid diagnoses. For example, different persons may express fear of flying in airplanes due to fear of crashing, being in a closed space, or being trapped in the event of panic, with the first two reasons viewed as indicative of specific phobia and the latter of agoraphobia. Similarly, a child might express fear of sleeping alone due to fear of the dark (specific phobia) or fear of separation from the caretaker (SAD). It is possible that some (or all) diagnostic interviews, and particularly rating scales, fail to make such subtle distinctions adequately, which could inflate correlations among these dimensions of psychopathology. Such imprecise measurement of symptoms could inflate correlations among dimensions in the fears domain to an extent that is currently unknown. Imprecise measurement could even explain some correlations across domains. For example, in some cases, the defiance symptom in ODD could reflect a child’s refusal to go to school due to separation anxiety or fear of something at school.
Whereas imprecise symptom measurement undoubtedly inflates correlations among some similar symptoms, and is therefore an important topic for future research, it seems improbable that imprecise measurement could explain most of the broad patterns of correlations among dimensions that give rise to the general factor of psychopathology. As examples, it is unlikely that the correlations among the distinct symptoms of hyperactivity-impulsivity, social anxiety, depression, and alcohol use disorder reflect imprecise measurement that creates nonveridical correlations among these symptoms to a substantial degree.
Is the General Factor an Artifact of Systematic Measurement Biases?
It is also necessary to evaluate the alternative hypothesis that the general factor is an artifact of systematically correlated measurement error. It is important to note, however, that the issue of biased measurement discussed here is not specific to the hypothesized general factor of psychopathology. Rather, it is a fundamental issue that must be addressed in every psychological study in which any two similarly measured variables are found to be correlated. It is as true for studies examining the bivariate correlation of one dimension of psychopathology with another as it is for studies that extract higher-order factors based on matrices of correlations among multiple dimensions of psychopathology. In classical measurement theory, each observed score is posited to reflect both the ‘true score’ and some combination of random and systematic error of measurement (Nunnally, 1978; Spearman, 1904). Random measurement error is a problem because it attenuates veridical correlations among symptoms and psychopathology dimensions (Spearman, 1904; Thorndike, 1920). In contrast, systematically biased measurement (i.e., correlated measurement error) would inflate correlations among symptoms and dimensions of psychopathology, perhaps even creating spurious factors that have no substantive meaning.
Could the structure of correlations among first-order dimensions of psychopathology arise largely or even solely from systematically biased measurement? It is difficult to imagine that the phenotypic correlations of dimensions of psychopathology reviewed above are not biased to some degree by correlated measurement error. There is no reason to advance a causal taxonomy, however, unless there is a basis for believing that systematic measurement error is not the only important source of correlations among psychopathology dimensions. Therefore, in discussing each source of systematic error, we (a) logically evaluate the likelihood that it is the primary source of observed patterns of correlations among dimensions of psychopathology, (b) review evidence from validity studies that such that correlated measurement error does not fatally obscure the correlational structure of psychopathology, and (c) suggest further tests of the role of systematic measurement error in structural models of psychopathology.
Three types of systematically correlated measurement error have been proposed that could give rise to nonveridical correlations among symptoms and dimensions of psychopathology:
1. Common method variance
This refers to any systematic influence of the method of measurement that causes two or more measures to be more correlated when quantified using the same versus different methods of measurement (Campbell & Fiske, 1959; Podsakoff, MacKenzie, Lee, & Podsakoff, 2003). Most of the correlations among psychopathology dimensions reviewed above were estimated using a single method of measurement with one informant (i.e., parent reports of symptoms for children or self-reports for adolescents and adults) and, as a result, are likely to be inflated to some degree by common method variance. Notably, however, if common method variance were uniform across dimensions of psychopathology, it would not be a threat to the validity of studies that identified more than one higher-order domain of psychopathology (e.g., internalizing and externalizing) based on correlations among first-order dimensions of psychopathology. This is because these findings are based on patterns of differences among correlations and uniform common method variance would be expected to inflate correlations to the same extent among everything measured using the same method. Thus, uniform common method variance would not be expected to create the patterned differences in correlations that are a primary basis for the proposed taxonomy.
Nonetheless, uniform common method variance could contribute to the general factor of psychopathology (Caspi et al., 2014; Lahey et al., 2012). Because the loadings of each dimension on the general factor reflects the extent to which each dimension is correlated with all other dimensions, after correlations among the specific first-order dimensions within higher-order domains are taken into account, it could partly or entirely reflect correlations among dimensions arising from common method variance. One would expect less varied loadings on the general factor than are observed if the general factor were an artifact of common method variance, but because the general factor plays an essential role in the present causal taxonomy, we evaluate the extent to which it could be an artifact of common method variance using tests of external validity and other methods presented below.
2. Implicit theories
Informants may report on symptoms in themselves and in others partly based on implicit theories they hold regarding how different behaviors are correlated (Cronbach & Meehl, 1955; Korman, 1960). If they observe one behavior, their implicit theories may lead them to report another behavior believed to be correlated with it, even if the latter behavior was not actually observed (Schneider, 1973). An important problem with this alternative hypothesis is that the observed widespread correlations among dimensions of psychopathology reviewed here are not consistent with current implicit theories of psychopathology in the cultures in which the studies reviewed above were conducted. Although in our culture one may expect people who experience one fear to experience other fears and for people who worry to be unhappy, it seems less likely that we would expect antisocial individuals to also worry, be fearful, and be sad. Yet, that is what the phenotypic correlational evidence shows.
Another possible implicit theory that should be considered is the belief that all negative traits are positively correlated. That is, observers may have a tendency to globally endorse negatively worded descriptors of themselves or others in a biased manner that increases correlations among negatively worded items (Pettersson & Turkheimer, 2010). Because questions about psychopathology symptoms almost always imply negative evaluation, such a bias could be strong enough to lead to the reporting of symptoms that are not observed. This would artifactually increase correlations among all symptoms. A simple tendency for observers to endorse all positive or negative characteristics of persons seems unlikely to be the sole cause of correlations among dimensions among negatively worded dimensions of psychopathology, however. If that were the case, all negatively worded symptoms of psychopathology would be equally correlated. Again, the pattern of varying magnitudes of correlations among dimensions of psychopathology reviewed above is evidence against this explanation. Nonetheless, the extent to which implicit theories contribute to a nonveridical general factor of psychopathology can be evaluated best using the kinds of tests of criterion validity discussed below.
3. Halo effects
Halo effects (Thorndike, 1920) are another potential source of systematic measurement error that could confound the interpretation of correlations among different forms of psychopathology and distort structural models of psychopathology. A halo effect is a general tendency for informants to view persons, either themselves or others, in a positive or negative light (Schneider, 1973; Thorndike, 1920). A negative halo of this sort could lead unobserved symptoms of psychopathology to be attributed to an individual, which could artificially increase correlations among symptoms and dimensions of psychopathology. Such negative halos could arise in at least two ways. First, when an individual displays some salient negative characteristics, many informants may acquire a generally negative view of that person and report other characteristics in a biased manner (Abikoff, Courtney, Pelham, & Koplewicz, 1993; Nisbett & Wilson, 1977). Second, some informants may be characteristically disposed to rate themselves or others in ways that are positively or negatively biased. Thus, the high correlations among factors of psychopathology could reflect individual differences in a tendency to portray oneself in generally negative (or positive) terms. This general tendency would not explain the observed patterning of varying correlations among symptoms, however. Note that this explanation refers to more than just biased reporting of symptoms, and contains a substantive component. That is, a general tendency to describe oneself in negative terms could reflect one of the nonspecific processes that underlie the general factor and creates risk for all forms of prevalent psychopathology.
Testing the Impact of Common Method Variance on Higher-Order Factors Using Multitrait-Multimethod Matrices
The contribution of common method variance to the correlations among first-order dimensions of psychopathology that give rise to higher-order factors can be assessed using a multitrait-multimethod matrix (MTMM) (Campbell & Fiske, 1959). This classic method provides a simple way to evaluate the convergent and divergent validity of constructs. If two measures of the same construct reflect more than systematic measurement error, they should correlate regardless of the measurement method (convergent validity) whereas correlations among different constructs should be lower both within and across measurement methods (divergent validity). Because the MTMM approach to the measurement of symptoms and dimensions of psychopathology has not been used previously in representative samples, we examined it for this paper using new analyses of data on 826 9–17 year old children and adolescents in the representative sample of the Georgia Health and Behavior Study whose symptoms were assessed by two independent methods: parent and youth reports of symptoms (Lahey et al., 2004). Psychopathology was assessed by each informant using parallel versions of the same structured interview used in the Tennessee Twin Study (Lahey, Rathouz, et al., 2008)in which each symptom was rated on a 0–3 scale reflecting severity and frequency (Lahey et al., 2004). We generated an MTMM matrix of correlations among eight dimensions of symptoms (Table 2): CD, MDD, GAD, social anxiety disorder, specific phobia, agoraphobia, SAD, and obsessive-compulsive disorder (OCD). All correlations in the table are significant at the Bonferroni-corrected value of .05/112 = .0005, except for those between CD and most anxiety dimensions (in italics).
Table 2.
Multi-trait multi-method correlations among first-order dimensions of psychopathology in 9–17 year olds based on reports of parents (method 1) and youth self-reports (method 2) in the Georgia Health and Behavior Study (N =826) (Lahey et al., 2004).
| Method 1: Parent Reports of Youth Symptoms | Method 2: Youth Self Reports of Symptoms | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Method 1: Parent | CD | MDD | GAD | SOC | SP | AG | SAD | OCD | CD | MDD | GAD | SOC | SP | AG | SAD | OCD |
| CD | (.89) | |||||||||||||||
| MDD | .40 | (.82) | ||||||||||||||
| GAD | .29 | .84 | (.80) | |||||||||||||
| SOC | .11 | .54 | .56 | (.65) | ||||||||||||
| SP | .03 | .29 | .36 | .33 | (.84) | |||||||||||
| AG | .12 | .41 | .43 | .40 | .49 | (.77) | ||||||||||
| SAD | .20 | .61 | .58 | .47 | .48 | .49 | (.76) | |||||||||
| OCD | .32 | .47 | .44 | .31 | .32 | .45 | .51 | (.73) | ||||||||
| Method 2: Youth | ||||||||||||||||
| CD | .58 | .30 | .21 | .08 | -.02 | .05 | .15 | .18 | (.78) | |||||||
| MDD | .15 | .50 | .44 | .29 | .13 | .18 | .29 | .21 | .39 | (.69) | ||||||
| GAD | .10 | .43 | .43 | .27 | .12 | .17 | .25 | .16 | .30 | .90 | (.65) | |||||
| SOC | -.03 | .26 | .29 | .35 | .19 | .24 | .23 | .13 | .07 | .59 | .62 | (.62) | ||||
| SP | -.01 | .20 | .24 | .24 | .48 | .27 | .30 | .18 | .08 | .46 | .47 | .47 | (.83) | |||
| AG | .03 | .25 | .25 | .23 | .32 | .35 | .28 | .24 | .12 | .48 | .48 | .51 | .61 | (.70) | ||
| SAD | .08 | .32 | .29 | .22 | .27 | .21 | .50 | .24 | .24 | .63 | .59 | .52 | .57 | .54 | (.70) | |
| OCD | .16 | .33 | .31 | .26 | .19 | .21 | .33 | .32 | .37 | .68 | .64 | .50 | .51 | .53 | .66 | (.67) |
CD = conduct disorder; MDD = major depressive disorder; GAD = generalized anxiety disorder; SOC = social anxiety disorder; SAD = separation anxiety disorder; OCD = obsessive compulsive disorder.
Note: Values on the convergent validity diagonal in the lower-left block are in bold; the two sets of heterotrait-monomethod correlations are shaded in blue; the heterotrait-heteromethod correlations shaded in light green; reliability coefficients in parentheses on the diagonal are reported as intra-class correlations; correlations in italics are not significant at Bonferroni-corrected p < .00045.
As shown in Table 2, the convergent validity correlations shown in bold (i.e., correlations of ratings of the same dimension by different informants) on the diagonal through the lower-left block in green were all significant (median r = .46). Following the method of Campbell and Fiske (1959), all of the convergent validity correlations between ratings of the same dimension by different informants were tested for significant differences compared to all correlations between ratings of different dimensions by different informants in the same row and column. In every case except youth-reported OCD, the convergent validity correlations were significantly greater than all corresponding off-diagonal correlations. Thus, with the exception of youth-reported OCD, both convergent and divergent validity were demonstrated for these first-order dimensions of psychopathology.
Second, and most pertinent to our thesis, the MTMM matrix can be used to estimate an upper bound for the extent to which the observed correlations among different first-order dimensions of psychopathology assessed by the same informant reflect common method variance. That is, correlations among first-order dimensions reflect common method variance to a degree, but it is essential to quantify its role to determine if dimensions also are correlated for substantive reasons. As shown in Table 2, the within-informant correlations among the eight dimensions of psychopathology measured by parent reports in the upper left triangle (median r = .42), and the within-informant correlations among different dimensions measured by youth reports in the lower right triangle (median r = .51) are larger than the corresponding correlations among different dimensions across informants (median r = .23). These differences could reflect differences in the perspectives of the two informants, but also could mean that common method variance magnifies within-informant correlations among first-order dimensions to some extent. Nonetheless, the present findings argue that these correlations are not only the spurious result of common method variance. First and foremost, 91% of the correlations among different dimensions rated by different informants were statistically significant, indicating that these correlations among different first-order dimensions are not found only within one method of assessment, but also across methods (i.e., informants). Thus, the results of the present MTMM analyses do not support the alternative hypothesis that the correlations among different first-order dimensions of psychopathology that are the basis for the general factor of psychopathology are primarily the result of common method variance.
It is also important to note the pattern of correlations within and between informants in Table 2. If phenotypic dimensions were correlated only due to uniformly biased measurement, one would expect the correlations among all phenotypes to be of uniform magnitudes. Instead, they are patterned in a way that has been replicated in the many studies reviewed above that used a variety of different informants and measures. Furthermore, the patterns of correlations among different dimensions in Table 2 are similar both within and across informants. For example, MDD is more strongly correlated with GAD than with specific phobia, both within and across informants. We cannot rule out the possibility that this patterning reflects widely held implicit theories of which dimensions should co-occur, leading to non-veridical reports of some symptoms when other symptoms are observed. Such implicit theories would need to be shared by parents reporting on their children, and by adolescents and adults reporting on themselves, however, to obtain the results in Table 2 and the other findings reviewed in this paper.
Criterion Validity of Higher-Order Factors of Psychopathology
The strongest test of all of the alternative hypotheses stated above that the correlations among first-order dimensions are artifacts of systematic measurement biases that give rise to a spurious general factor of psychopathology is to test the criterion validity (Cronbach & Meehl, 1955) of each higher-order factor in the proposed hierarchical model. That is, it is necessary to determine if the hypothesized higher-order dimensions are uniquely related to relevant external criterion variables that are independent of the definitions of the symptom dimensions and measured by different informants. Data supporting the criterion validity of each first-order dimensions are reviewed in Supplement 3; here we address the criterion validity of the higher-order dimensions, including the general factor.
Criterion Validity of Internalizing and Externalizing Factors
An analysis of NESARC data found that the higher-order internalizing dimension was valid in the sense of predicting future angina, ulcer, and suicide attempts (Eaton et al., 2013). In another representative sample of 8,580 adults, internalizing factor scores were found to be inversely associated with daily living skills (e.g., preparing meals and managing money) (Markon, 2010a). Similarly, using data from assessments of psychopathology during early adulthood in the longitudinal Dunedin Study, higher-order internalizing, externalizing, and thought problems factors were positively correlated with receipt of social welfare benefits, inpatient mental health treatment, and conviction for a violent crime, but the other two factors were not controlled when testing these associations (Caspi et al., 2014). We similarly reported evidence supporting the criterion validity of distinguishing the higher-order fears, distress, and externalizing dimensions in adults using NESARC data (Lahey et al., 2012). In this sample, associations with validity criteria were tested in multiple regression models in which the three higher-order dimensions were simultaneous predictors, adjusting for age, sex, and race-ethnicity. Many of the criterion validity criteria were significantly correlated in the same direction with more than one of the three dimensions, but there were important exceptions that supported the discriminant validity of these higher-order dimensions of psychopathology. For example, unintentional injury was uniquely associated with the externalizing factor and receipt of disability income in wave 2 was independently predicted by levels of distress but not by fears or externalizing factors in wave 1 (Lahey et al., 2012). Nonetheless, the symptoms and criterion variables in this study were reported by the same informant, however, leaving open the possibility that common method variance could have contributed to these correlations.
Criterion Validity of the General Factor of Psychopathology
In the NESARC sample, we tested several aspects of criterion validity of the general factor when higher-order fears, distress, and externalizing factors also were specified in the model (Lahey et al., 2012). In simultaneous regressions adjusting for age, sex, and race-ethnicity, the general factor in wave 1 prospectively predicted several aspects of future psychopathology and adaptive functioning assessed in wave 2, over and above the variance accounted for by the fears, distress, and externalizing factors. In addition, the general factor was uniquely associated with retrospective reports of physical or sexual abuse and neglect, whereas the fears, distress, and externalizing factors were not consistently related to these measures when the general factor was included in the model. Thus, these analyses support the discriminant criterion validity of the general factor, in terms of associations with putative risk factors and the prediction of independent aspects of future functioning (Lahey et al., 2012). In simultaneous multiple regression analyses of data from the Dunedin Study, Caspi et al. (2014) similarly found the general psychopathology factor to be independently associated with multiple lifetime measures of impairment, when higher-order factors defined by internalizing symptoms, externalizing symptoms, and symptoms of psychosis, mania, and OCD were controlled. The externalizing factor showed reduced but significant independent associations with impairment measures when the general factor was a simultaneous predictor, but the internalizing factor showed little evidence of independent association with impairment when the general factor was in the model.
Although the potential value of the findings of the studies just reviewed is diminished by the fact that the same informant reported on psychopathology, risk factors, and impairment, other studies provide data on the criterion validity of the general factor of psychopathology using independently measured variables. These criterion variables are particularly important because their correlations with the general factor are not contaminated by either common method variance or implicit theories. In the Dunedin Study, intelligence and other cognitive ability measures were found to be inversely associated with both the internalizing and externalizing dimensions. When the general factor was added to the model, however, these cognitive ability measures were inversely correlated with the general factor, but only weakly with internalizing or externalizing scores (Caspi et al., 2014). Furthermore, in the longitudinal Pittsburgh Girls Study (Lahey et al., 2015), associations of parent ratings of their children’s symptoms across 5–11 years of age were tested with the fully independent criterion measures of intelligence and teacher reports of academic learning and classroom behavior, averaged across 5–11 years and averaged across 12–16 years. Multiple regression models tested the unique associations of the general, externalizing, and internalizing factor scores at 5–11 years extracted from the best-fitting CFA with each criterion measure, controlling for each of the other factor scores and demographics. This confirmed the previous finding (Caspi et al., 2014) that the general psychopathology factor was independently and inversely associated with intelligence. This supports for the criterion validity of the general factor, but it also means that intelligence needs to be controlled in testing associations with teacher-reported ratings of academic performance in reading, spelling, and mathematics, and classroom behavior. In such controlled analyses, the general psychopathology factor robustly explained unique variance in each independent teacher measure of classroom and academic functioning, both concurrently at 5–11 years and prospectively at 12–16 years (Lahey et al., 2015). Similar prospective tests of the criterion validity of the general factor were conducted in a large population-based British study of children (Patalay et al., 2015). The general factor of psychopathology predicted both future psychopathology and fully independent measures of academic achievement, when sex, race-ethnicity, socioeconomic status, and the internalizing and externalizing factor scores were controlled. These results of these tests of criterion validity strongly argue against the alternative hypotheses that the general factor reflects no more than spurious correlations based on either overlapping symptoms or any form of systematic measurement bias. Unfortunately, however, intelligence was not controlled in the Patalay et al. (2015) study. Additional support for the criterion validity of the general factor is described below in the discussion of findings from common pathways models of twin data.
HOMOTYPIC AND HETEROTYPIC CONTINUITY: PHENOTYPIC STRUCTURE OF PSYCHOPATHOLOGY OVER TIME
The cross-sectional studies reviewed above make it clear that (1) there is a robust pattern in the magnitudes of correlations among common forms of psychopathology when psychopathology is measured at a single point in time, and (2) this pattern of correlations is explained well by the hierarchical general factor model just described. As important as the cross-sectional structure of correlations among dimensions of psychopathology is to our thesis, however, it provides an incomplete picture of the extents to which dimensions of psychopathology are correlated. In this section, we add the dimension of time to our analyses by taking a longitudinal perspective on the correlational structure of common forms of psychopathology. Specifically, based on earlier analyses by Angold et al. (1999), we interrogated the correlational structure of psychopathology by examining patterns in the continuity of psychopathology over time. In this context, continuity refers to a significant positive correlation of psychopathology measured at time t with psychopathology measured at time t+1 in the same person. Developmental theorists distinguish two types of continuity that can be applied to our analysis. Each categorical diagnosis or first-order dimension of psychopathology may predict itself at a later point in time. This is referred to as homotypic continuity, as opposed to heterotypic continuity in which one dimension of psychopathology predicts another dimension at a later time (Beauchaine & McNulty, 2013; Kagan & Moss, 1962; Rutter, Kim-Cohen, & Maughan, 2006; Rutter & Sroufe, 2000).
Evidence of Homotypic Continuity
Many longitudinal studies have revealed moderate to substantial homotypic continuity in all common first-order dimensions and diagnoses of psychopathology across multiple years. This is clearly the case with the externalizing domain across childhood, adolescence, and into adulthood (Barkley, Fischer, Edelbrock, & Smallish, 1990; Bufferd, Dougherty, Carlson, Rose, & Klein, 2012; Burke, Waldman, & Lahey, 2010; Bussing, Mason, Bell, Porter, & Garvan, 2010; Copeland et al., 2013; Copeland, Shanahan, Costello, & Angold, 2009; Costello, Mustillo, Erkanli, Keeler, & Angold, 2003; Lahey, Loeber, Burke, & Applegate, 2005; Lahey, Pelham, Loney, Lee, & Willcutt, 2005; Miettunen et al., 2014; Ormel et al., 2015; Reef, van Meurs, Verhulst, & van der Ende, 2010; Zoccolillo, Pickles, Quinton, & Rutter, 1992). Similarly, across childhood and adolescence, significant homotypic continuity has been found for all symptom dimensions and diagnoses in the fears domain (Bittner et al., 2007; Broeren, Muris, Diamantopoulou, & Baker, 2013; Bufferd et al., 2012; Copeland et al., 2013; Costello et al., 2003; Ferdinand, Dieleman, Ormel, & Verhulst, 2007; Silberg, Rutter, & Eaves, 2001; Waszczuk, Zavos, Gregory, & Eley, 2016) and in the distress domain (Broeren et al., 2013; Copeland et al., 2013; Copeland et al., 2009; Costello et al., 2003; Ferdinand et al., 2007; Keenan, Feng, Hipwell, & Klostermann, 2009; Luby, Si, Belden, Tandon, & Spitznagel, 2009; Silberg et al., 2001; Waszczuk et al., 2016; Wickrama, Conger, Lorenz, & Martin, 2012) over long periods of time. Furthermore, there is clear evidence of homotypic continuity in all common diagnoses within and across internalizing and externalizing domains over 3+ year-long spans of the years of adulthood (Beard et al., 2006; Eaton et al., 2013; Krueger, Caspi, Moffitt, & Silva, 1998; Lahey, Zald, Hakes, Krueger, & Rathouz, 2014; Vollebergh et al., 2001). Robust homotypic continuity is important because it implies that the causal influences on prevalent forms of psychopathology either are relatively unchanging over time, self-sustaining, and/or have relatively long-lasting effects on psychopathology.
Evidence of Heterotypic Continuity
We next examine heterotypic continuity and discuss its implications for the causal taxonomy of psychopathology. We first review evidence of bivariate heterotypic continuity—prediction of diagnosis Y2 from diagnosis X1. We then consider the possibility that any observed heterotypic continuity is an artifact of homotypic continuity, by examining the prediction of Y2 from X1, while controlling Y1.
Heterotypic Continuity within and across Higher-order Domains
There is extensive evidence of widespread and robust bivariate heterotypic continuity within higher-order externalizing, fears, and distress domains in which one first-order dimension of psychopathology (or diagnosis) at time t significantly predicts a different dimension or diagnosis in the same domain at time t+1 during childhood, adolescence, and adulthood (Beauchaine & McNulty, 2013; Beesdo-Baum et al., 2015; Bittner et al., 2004; Bruckl et al., 2007; Bufferd et al., 2012; Burke et al., 2010; Bussing et al., 2010; Copeland et al., 2009; Gregory et al., 2007; Horn & Wuyek, 2010; Koenen et al., 2008; Kossowsky et al., 2013; Lahey et al., 2014; S. S. Lee, Humphreys, Flory, Liu, & Glass, 2011; Lewinsohn, Holm-Denoma, Small, Seeley, & Joiner, 2008; Moffitt et al., 2007; Ormel et al., 2015; Roberson-Nay, Eaves, Hettema, Kendler, & Silberg, 2012; Rowe, Costello, Angold, Copeland, & Maughan, 2010; Silberg et al., 2001; Waszczuk et al., 2016). There is also evidence of heterotypic continuity of first-order dimensions across higher-order domains at all ages:
From fears to distress and vice-versa
There is evidence that first-order dimensions (and diagnoses) in the higher-order fears domain significantly predict other dimensions or diagnoses in the higher-order distress domain (Ball, Otto, Pollack, & Rosenbaum, 1994; Beesdo et al., 2007; Bittner et al., 2004; Bufferd et al., 2012; Copeland et al., 2009; Goodwin et al., 2004; Horn & Wuyek, 2010; Keenan et al., 2009; Lavigne, Hopkins, Gouze, & Bryant, 2015; Ormel et al., 2015; Pine, Cohen, & Brook, 2001; Silberg et al., 2001; Trumpf, Margraf, Vriends, Meyer, & Becker, 2010; Wilson & Hayward, 2005). There also is evidence that first-order dimensions (and diagnoses) in the distress domain significantly predict other dimensions or diagnoses in the fears domain (Copeland et al., 2009; Lavigne et al., 2015; Mathyssek, Olino, Verhulst, & van Oort, 2012; Ormel et al., 2015). The studies reviewed in this section did not consistently find that every fears dimension prospectively predicted every distress dimension and vice versa, perhaps due partly to insufficient statistical power. For this reason, it is important that analyses of data from the large and representative NESARC sample over three years revealed universally significant heterotypic continuity from all diagnoses in the fears domain to all diagnoses in the distress domain, and vice-versa, across 3 years during adulthood (Lahey et al., 2014).
From externalizing to distress and vice-versa
Although there are inconsistencies across relatively small studies, there also is evidence that dimensions and diagnoses in the externalizing domain predict other dimensions and diagnoses in the distress domain (Bittner et al., 2007; Briere, Rohde, Seeley, Klein, & Lewinsohn, 2014; Burke & Loeber, 2010; Burke, Loeber, Lahey, & Rathouz, 2005; Capaldi, 1992; Chronis-Tuscano et al., 2010; Copeland et al., 2009; Hinshaw et al., 2012; Hipwell et al., 2008; Kosterman et al., 2010; Lahey, Loeber, Burke, Rathouz, & McBurnett, 2002; Patterson & Stoolmiller, 1991; Reef, Diamantopoulou, van Meurs, Verhulst, & van der Ende, 2009; Stringaris, Lewis, & Maughan, 2014). Among adults, analyses of data from NESARC showed that all diagnoses in the externalizing domain significantly predicted all diagnoses in the distress domain (Lahey et al., 2014). Although one study found that childhood depression predicted conduct problems 5 years later (Reinke & Ostrander, 2008), most studies of children and adolescents did not find MDD to predict future CD (Burke et al., 2005; Capaldi, 1992; Hipwell et al., 2011; Kosterman et al., 2010; Lahey et al., 2002; Patterson & Stoolmiller, 1991). From adolescence to adulthood MDD predicted alcohol use disorder (Briere et al., 2014). Among adults, moreover, all diagnoses in the distress domain significantly predicted all diagnoses in the externalizing domain 3 years later in the NESARC sample (Lahey et al., 2014).
From externalizing to fears and vice-versa
There is little evidence of heterotypic continuity from externalizing to fears dimensions based on representative samples of children and adolescents, although there is some evidence that childhood ADHD predicts later social anxiety disorder (Bittner et al., 2007) and self-reported symptoms of ADHD, ODD, and CD during adolescence predict panic attacks during early adulthood (Mathyssek et al., 2012). Among adults in the NESARC study, in contrast, heterotypic continuity from externalizing diagnoses to diagnoses in the fears domain was universally significant, albeit modest in magnitudes (Lahey et al., 2014). We found no published evidence of significant heterotypic continuities from diagnoses in the fears domain to diagnoses in the externalizing domain among children or adolescents. Nonetheless, among adults in the NESARC study, all diagnoses in the fears domain significantly but modestly predicted all externalizing diagnoses 3 years later, except that specific phobia did not predict future drug abuse (Lahey et al., 2014). It is important to consider the implications of the differences in the consistency of significant findings on heterotypic continuity across domains in the NESARC study of adults and other studies, many of which were of children and adolescents. These differences could reflect true developmental differences, but they may simply be an artifact of the much greater statistical power of the larger NESARC study of adults.
Is Heterotypic Continuity an Artifact of Uncontrolled Homotypic Continuity?
It is essential to determine if heterotypic continuity in psychopathology is an artifact of testing the predictive association between disorder X at time 1 (X1) and disorder Y at time 2 (Y2) without controlling disorder Y at time 1 (Y1). This is because X1 could predict Y2 when Y1 is not controlled because X exhibits homotypic continuity and because X and Y are correlated at both time points. We conducted tests of this possibility using data on prevalent diagnoses in adults in waves 1 and 2 of NESARC (Lahey et al., 2014). When homotypic continuity was controlled, heterotypic continuity was still widespread.
The strictest test of heterotypic continuity is to determine if each wave 1 diagnosis independently predicts each wave 2 diagnosis simultaneously controlling for both homotypic continuity and every other wave 1 diagnosis. This strict test was conducted from childhood to adolescence, childhood to adulthood, and from adolescence to adulthood in the Great Smokey Mountain Study (Copeland et al., 2009) and in a synthetic combination of that sample with two cohorts in New Zealand (Copeland et al., 2013). In both analyses, significant heterotypic continuity was found for some pairs of diagnoses. In addition, in the much larger NESARC sample, every wave 1 diagnosis in the distress domain accounted for significant independent variance in the prediction of each other distress diagnosis in wave 2, and each wave 1 diagnosis in the fears domain independently predicted each other fears diagnosis in wave 2 (Lahey et al., 2014). Similarly, heterotypic continuity was universal in the externalizing domain, except that wave 1 drug dependence did not predict wave 2 tobacco dependence. In addition, there were less consistent, but still widespread heterotypic continuities from diagnoses in one higher-order domain to diagnoses in a different higher-order domain, even when homotypic continuity and the heterotypic associations of all other wave 1 diagnoses were controlled (Lahey et al, 2014). These findings argue that heterotypic continuity is not an artifact of uncontrolled homotypic continuity.
Implications of Robust Heterotypic Continuity
The findings of widespread heterotypic continuity reviewed above raise two fundamentally important issues for the construction of a causal taxonomy of psychopathology:
1. Changing manifestations over time
The findings on widespread heterotypic continuity suggest that although psychopathology is quite persistent (i.e., homotypic continuity is strong), persons with psychopathology symptoms also experience changes in symptoms over time (i.e., heterotypic continuity also is common). In the NESARC study, it was particularly striking that the magnitudes of zero-order bivariate homotypic (ρ = .47 – .53) and heterotypic continuities (ρ = .41 – .50) among diagnoses within the distress domains differed very little, suggesting remarkable shifting over time among the distress diagnoses. This could be fostered by the overlap in symptoms among the distress diagnoses, but high levels of heterotypic continuity were also observed across domains that do not share symptoms in the NESARC study. For example, persons who met criteria for MDD in wave 1 were significantly more likely to meet criteria for social anxiety disorder in wave 2. This means that persons with MDD in wave 1 were more likely than persons without MDD in wave 1 to add enough new symptoms of social anxiety disorder after wave 1 to meet criteria for social anxiety disorder in wave 2, whether or not they continued to meet criteria for MDD in wave 2. Notably a separate analysis of NESARC data found that higher-order factors predict future specific diagnoses in wave 2 better than the same specific diagnosis in wave 1 (Kim & Eaton, 2015). These findings are support the previously articulated view of psychopathology as relatively persistent over time, but subject to what has been termed “changing manifestations” (Loeber & Hay, 1997) and “phenotypic plasticity” (Nolen-Hoeksema & Watkins, 2011).
2. Heterotypic continuity arises for the same reasons as cross-sectional correlations
Our analyses of patterns of heterotypic continuities over 3 years in NESARC (Lahey et al., 2014) were conducted to examine a key prediction relevant to the causal taxonomy stated in the present paper. We predicted that the magnitudes of heterotypic associations from wave 1 to wave 2 would recapitulate the magnitudes of cross-sectional phenotypic associations among different mental disorders in wave 1. Using age- and sex-adjusted tetrachoric correlations to quantify (a) the bivariate cross-sectional associations among 10 different diagnoses in wave 1, and (b) the corresponding bivariate correlations for prospective heterotypic associations among the same diagnoses from wave 1 to wave 2, we assessed the similarity in these two sets of correlations using Spearman’s rank correlation. The cross-sectional and heterotypic correlations were highly correlated at ρ = .86 (Lahey et al., 2014). Consistent with the present causal taxonomy, the finding that disorder X1 predicts Y2 to a degree that closely mirrors the magnitudes of the cross-sectional correlations between X1 and Y1 strongly suggests that the same shared etiologic factors and mechanisms that give rise to cross-sectional correlations among multiple mental disorders at time 1 also underlie the heterotypic continuities among those disorders over time.
GENETIC AND ENVIRONMENTAL STRUCTURE OF PSYCHOPATHOLOGY
There are two fundamental questions for a causal taxonomy of multiple dimensions of psychopathology. What etiologic factors cause first-order dimension to be correlated with one another? What etiologic factors differentiate first-order dimensions of psychopathology from one another?
Family Studies
If familial causes (i.e., genetic influences and environmental influences shared by family members) nonspecifically increase risk for multiple dimensions of psychopathology through the general factor, one would predict that family members with closer genetic and environmental relatedness would show stronger correlations among both the same and different dimensions of psychopathology. The most informative tests come from family studies in which probands are identified in nonreferred samples, since referred cases tend to be more comorbid than in the general population (Goodman et al., 1997), which could bias the test. In a number of such studies, persons with each mental disorder are significantly more likely to have family members who meet criteria for each other mental disorder in a nonspecific manner (Arcos-Burgos, Velez, Solomon, & Muenke, 2012; Saha, Stedman, Scott, & McGrath, 2013; Shankman, Klein, Lewinsohn, Seeley, & Small, 2008; Song et al., 2015). Furthermore, one study found that the magnitudes of these associations with other mental disorders in family members declined with the degree of genetic relatedness of the siblings, suggesting a role for pleiotropic (i.e., nonspecific) genetic influences on all mental disorders (Song et al., 2015).
Bivariate Biometric Models of the Covariation among First-Order Dimensions of Psychopathology
Biometric models use differences in correlations between family members of varying degrees of genetic relatedness, often members of monozygotic and dizygotic twin pairs, to estimate the proportion of variation in a trait among persons in the population that is due to genetic influences, shared environmental influences (familial factors that influence all siblings equally and operate independent of genetic influences), and nonshared environmental influences (which vary among siblings and operate independent of both genetic influences and shared environmental influences). If two different phenotypes are more correlated within monozygotic twin pairs than within dizygotic pairs, the difference provides the basis for inferring common genetic influences on the two phenotypes (Neale & Cardon, 1992). Studies using bivariate biometric modeling of cross-sectional twin data have consistently indicated that first-order dimensions within the higher-order externalizing domain in children, adolescents, and adults share a considerable proportion of their genetic influences (Dick, 2007; Dick, Viken, Kaprio, Pulkkinen, & Rose, 2005; Korhonen et al., 2012; Nadder, Rutter, Silberg, Maes, & Eaves, 2002; Tuvblad, Zheng, Raine, & Baker, 2009; Waldman, Rhee, Levy, & Hay, 2001). Similarly, bivariate twin studies reveal that common genetic influences are primarily responsible for the correlations among anxiety disorders and depression within the internalizing domain in children and adolescents (Middeldorp, Cath, Van Dyck, & Boomsma, 2005) and adults (Hettema, 2008; Ogliari et al., 2010; Smoller, 2013). Furthermore, bivariate twin studies also reveal common genetic influences on first-order dimensions in different higher-order domains (Smoller, 2013). For example, both CD (Subbarao et al., 2008; Tackett, Waldman, Van Hulle, & Lahey, 2011) and tobacco dependence (Tsuang, Francis, Minor, Thomas, & Stone, 2012) in the externalizing domain share a substantial proportion of their genetic influences with MDD in the internalizing domain. These studies suggest that the phenotypic correlations among pairs of first-order dimensions of psychopathology both within and across domains are at least partly—and likely substantially—due to common genetic influences.
Multivariate Biometric Models of the Hierarchy of Shared Etiologic Influences on Psychopathology
Of direct importance to the present paper, biometric models have been extended to bivariate and multivariate analyses (Neale & Cardon, 1992) to quantify the degree of sharing of each of these kinds of etiologic influences across more than one trait (Jang & Livesley, 1999; Lahey et al., 2011; Neale & Cardon, 1992; Spatola et al., 2007). Multivariate behavior-genetic studies provide considerably more information on the shared etiologic factors underlying phenotypic correlations among first-order dimensions of psychopathology than bivariate models. These models are based on genetic and environmental correlations among multiple measures of psychopathology derived from differences in the genetic relatedness of different kinds of twins and other siblings (Neale & Cardon, 1992). As detailed in the following paragraphs, two types of multivariate behavior genetic models— independent and common pathways models—based on somewhat different assumptions (Neale & Cardon, 1992) have been used to understand genetic and environmental contributions to the covariation among symptom dimensions, .
Independent Pathways Models
In independent pathways models (Neale & Cardon, 1992), one or more factors are derived from matrices of genetic and environmental correlations among every first-order symptom dimension. To consider a hypothetical example, this could yield one genetic (or environmental) factor that influences ADHD, ODD, and CD, and a second genetic (or environmental) factor that influences MDD, GAD, and other anxiety dimensions. An independent pathways model was specified for diagnoses of MDD, GAD, phobias, alcohol dependence, drug abuse/dependence, adult antisocial behavior, and CD in a large study of adult twins (Kendler, Prescott, Myers, & Neale, 2003). In the best-fitting model, which was invariant across sex, two genetic factors were identified, with diagnoses generally considered to be in the internalizing domain loading most strongly on one genetic factor and diagnoses considered to be in the externalizing domain loading on the second genetic factor, but with most diagnoses having significant loadings on both genetic factors. Two factors of nonshared environmental influences had large loadings, with most diagnoses considered to be in the internalizing domain loading on one factor, and most diagnoses considered to be in the externalizing domain loading on the second factor. Shared environmental influences accounted for little variance in these analyses.
A similar model was applied to parent-rated DSM-like internalizing and externalizing symptom dimensions in a population-based sample of children and adolescents (Pesenti-Gritti et al., 2008; Spatola et al., 2007). The best-fitting model included a single genetic factor on which all dimensions of psychopathology loaded and two nonshared environmental factors on which dimensions generally considered to be in the internalizing and externalizing domains loaded, respectively. In addition, the small shared environmental influences were generally common to all dimensions of psychopathology.
Analyses of data on 11 first-order internalizing and externalizing psychopathology dimensions were conducted using an independent pathways model in 1571 pairs of 9- to 17-year-old twins in the population-based Tennessee Twin Study (Lahey et al., 2011). We first considered the structure of the genetic correlations among the psychopathology dimensions in a correlated 2-factor model in which depression and six dimensions of anxiety loaded on an internalizing factor and the remaining four dimensions loaded on an externalizing factor. In this model, the genetic correlation between the internalizing and externalizing domains was r = 0.89, indicating that their genetic influences were substantially shared. We then tested the possibility that this robust correlation between the internalizing and external genetic factors could be explained by a general genetic factor in a bifactor model. The best-fitting model of genetic influences included higher-order internalizing and externalizing factors and a higher-order general factor on which all first-order dimensions of psychopathology had significant loadings. In a separate analysis of the nonshared environmental correlations among the 11 dimensions of psychopathology, the same alternative models were compared in CFA. Like the analyses of genetic correlations, the best-fitting model for nonshared environmental correlations included an internalizing factor, an externalizing factor, and a general factor on which every dimension of psychopathology significantly loaded. Unlike the model for genetic correlations, however, the proportion of dimension-specific nonshared environmental influences was much higher for each dimension, with the general factor and internalizing and externalizing factors explaining a relatively small amount of the total nonshared environmental variance of each first-order dimension.
Similar analyses using an independent pathways model were conducted of data on 6,595 child twin pairs (Pettersson, Anckarsater, Gillberg, & Lichtenstein, 2013). In this case, however, the unit of measurement was symptoms rather than dimensions of psychopathology, and the range of symptoms was different from other studies: ADHD, tics, autism, and specific learning disorders. Nonetheless, EFA of the genetic covariances indicated that most genetic covariance was explained by a general genetic factor. Nonshared environmental influences on these symptoms were sizable, but a general factor did not emerge in EFA of the nonshared environmental correlations (Pettersson et al., 2013).
The largest study to date using an independent pathways model to assess the sharing of causal influences on psychopathology was based on records of clinical diagnoses for 1.7 million pairs of full and half adult siblings in the population of Sweden (Pettersson, Larsson, & Lichtenstein, 2016). These diagnoses included both prevalent mental disorders (MDD, anxiety, ADHD, alcohol use disorder, drug use disorder, and antisocial behavior) and the less common but serious disorders of schizophrenia, schizoaffective disorder, and bipolar disorder. They found a general factor of genetic influences on all mental disorders and two additional factors reflecting genetic influences shared by just the psychotic disorders and by just the non-psychotic disorders. In addition, they found a nonshared environmental factor, on which mood disorders, anxiety, and ADHD loaded most strongly.
These studies using independent pathways models provide fundamental information for the construction of a causal taxonomy. They suggest that genetic and environmental influences are (a) shared among the internalizing disorders, (b) shared among the externalizing disorders, and (c) broadly shared across internalizing and externalizing disorders. Nonshared environmental influences are thinly shared by first-order dimensions, but are mostly dimension-specific. In contrast, genetic influences tend to be robustly shared across multiple dimensions of psychopathology. Indeed, a general genetic factor influencing all dimensions of psychopathology was identified in four of these studies (Lahey et al., 2011; Pettersson et al., 2013; Pettersson et al., 2016; Spatola et al., 2007).
Common Pathways Models
Common pathways behavior genetic models provide information on the causal structure of psychopathology that is complementary to independent pathways models. Unlike independent pathways models, common pathways models are based on the strong assumption that there are meaningful higher-order phenotypic constructs and that genetic and environmental influences on first-order dimensions operate through them (Franic et al., 2013; Neale & Cardon, 1992). Therefore, higher-order phenotypic factors are defined in common pathways models and the genetic and environmental influences on these phenotypes are estimated. For example, each first-order dimension might load on either a higher-order externalizing or internalizing phenotypic factor. In such a simple two-factor model, all of the common genetic and environmental influences on each first-order symptom dimension would pass through these higher-order phenotypic factors, rather than influencing the first-order symptom dimensions directly, as in the independent pathways model.
Several analyses of the hierarchy of genetic and environmental influences have been conducted using common pathways models, in which higher-order phenotypic factors were specified. Data on mental disorder diagnoses among 3,372 male–male adult twin pairs in the Vietnam Era Twin Registry were examined using such a model (Wolf et al., 2010). Higher-order phenotypic factors of internalizing and externalizing psychopathology were specified and the analyses revealed that the correlation between these phenotypic internalizing and externalizing factors was mostly due to common genetic influences, but also partly due to common nonshared environmental influences. The externalizing factor also had genetic and environmental influences that did not also influence the internalizing factor. Each specific diagnosis had relatively little diagnosis-specific genetic influences, but there were substantial diagnosis-specific nonshared environmental influences (Wolf et al., 2010).
Using a common pathways model, an analysis was conducted of data on measures of MDD, GAD, SAD, ADHD, ODD, and CD in adolescent twins and siblings (Cosgrove et al., 2011). Higher-order phenotypic internalizing and externalizing factors were specified. Shared environmental influences common to family members were small and largely dimension-specific. In contrast, two genetic factors were identified in the best-fitting model that influenced the internalizing and externalizing factors, respectively. Notably, the correlation between these genetic factors was r = .75, indicating substantial overlap in the genetic influence on these higher-order factors. Similarly, the correlation between two nonshared environmental factors influencing the internalizing and externalizing factors was r = .74.
We used a common pathways model in a recent new set of analyses of Tennessee Twin Study data (Waldman, Poore, Van Hulle, Rathouz, & Lahey, in press). Unlike our previous independent pathways modeling of the Tennessee Twin Study data (Lahey et al., 2011), which only examined genetic and nonshared environmental influences, potentially important shared environmental influences on psychopathology (Burt, 2014) also were analyzed using the common pathways model. More importantly, unlike the other studies using common pathways models, a general factor of psychopathology was considered in these analyses. The best-fitting common pathways model for the combination of parent- and youth-reported dimensions of psychopathology in these analyses included a phenotypic general factor of psychopathology and higher-order internalizing and externalizing phenotypic factors. The latter factors reflect the causal influences shared by the first-order dimensions in the internalizing domain and in the externalizing domain, respectively, after the causal variance shared by all first-order dimensions was captured by the general factor.
In considering the specific quantitative results of these new common pathways model analyses of Tennessee Twin Study data (Waldman et al., in press), it is important to bear in mind that estimates of proportions of genetic and environmental influences are likely to vary by measures and samples. In particular, because a meta-analysis showed that estimates of the heritability of mental disorders increase with age (Bergen, Gardner, & Kendler, 2007), it is possible that the present analyses of children and adolescents yielded lower estimates of heritability and higher estimates of environmental influences than would studies of adults. In the recent common pathways model, the genetic component of the causal influences shared by the externalizing dimensions was substantial, with the estimated heritability of the higher-order externalizing factor being h2 = .65. The phobias (specific and agoraphobia), social anxiety disorder, SAD, and OCD all had significant loadings on the internalizing factor. In contrast, the MDD and GAD dimensions had very small loadings on the internalizing factor. Thus, a portion of the etiologic influences on the fear-related dimensions are through the higher-order internalizing factor. Genetic influences on the internalizing factor were modest (h2 =.19), with both moderate shared (c2 = .44) and nonshared environmental influences (e2 = .37). In addition, all first-order dimensions also loaded significantly on the general factor of psychopathology. These loadings ranged from modest for specific phobia to high for GAD and MDD, reflecting the shared causal influences on all 11 first-order dimensions to varying degrees through the general factor. Genetic influences on the general factor were moderate (h2 = .43), with moderate shared environmental influences (c2 = .25) and nonshared environmental influences as well (e2 = .32). Consistent with these estimates, the heritability of a general factor of psychopathology was estimated from single nucleotide polymorphisms to be .37 in a large representative sample of children (Neumann et al., in press).
Figure 3 presents a full quantitative description of the hierarchy of causal influences on these 11 first-order dimensions of psychopathology in children and adolescents as revealed in the common pathways model fitted to Tennessee Twins Study data (Waldman et al., in press). The three panels in Figure 3 illustrate the patterns of sharing of each type of causal influence. The widths of the arrows from each higher-order factor to each phenotypic dimension of psychopathology reflect the estimated proportions of the total phenotypic variance in each first-order dimension attributable to genetic, shared environmental, and nonshared environmental influences that are (a) common to all dimensions of psychopathology, as captured in the general factor, (b) common to dimensions that load on either the internalizing or externalizing factors, and (c) specific to each first-order dimension of psychopathology. The sum of these contributions to the phenotypic variance from each level of the causal hierarchy reflects the net variance explained by shared and dimension-specific genetic and environmental influences. For example, in the top panel of Figure 3, the total proportion of phenotypic variance in hyperactivity-impulsivity attributed to genetic influences through the general and externalizing factors plus dimension-specific influences (i.e., its heritability) was estimated to be 62%. Just over half of this genetic variance in hyperactivity-impulsivity was found to be shared with other externalizing dimensions (34%), but 5% of the phenotypic variance in hyperactivity-impulsivity was due to genetic influences shared with all dimensions through the general factor and 23% was due to dimension-specific genetic influences. Similarly, the heritability of SAD was estimated to be 32%, with nearly half of these genetic influences shared with all other dimensions through the general factor (15%) and most of the remainder of genetic influences being dimension specific.
Figure 3.
Variance components from the best-fitting common pathways model from twin analyses of combined parent and youth ratings of 11 dimensions of psychopathology in 9–17 year old children and adolescents in the Tennessee Twin Study (Lahey, Rathouz, et al., 2008) indicating the estimated proportion of phenotypic variance in each of the dimensions explained by shared and dimension-specific additive genetic, shared environmental, and nonshared environmental influences from each higher-order factor. The magnitude each variance component is proportional to the width of the connecting arrow.
Figure 3 also reveals that more than half of the genetic influences on most first-order dimensions of psychopathology were shared with other dimensions, either through the general factor or the internalizing or externalizing factors, with shared genetic influences through the externalizing factor being especially strong. The exceptions were CD and social phobia, for which a majority of their genetic influences were dimension-specific. Similarly, virtually all of the nonshared genetic influences on each dimension are shared through the general or the internalizing factor. Thus, familial influences tend to be nonspecific at the level of one or both of the higher-order factors. In contrast, the majority of the nonshared environmental influences are dimension-specific, except for MDD and GAD.
The proposed causal taxonomy is valuable in revealing both similarities and differences in the patterns of causal influences on each first-order dimension. The nonspecific causal influences that create widespread phenotypic correlations among these dimensions of psychopathology in this study can be seen in all three panels of Figure 3. It is also clear that the patterns of causal influences on each dimension seen in these hierarchies vary considerably, albeit with similarities in some pairs of dimensions. For example, specific phobia and agoraphobia show very similar patterns of genetic and environmental influences. Indeed, they share considerable genetic and nonshared environmental influences above and beyond the sharing at the levels of the general and internalizing factors. MDD and GAD also exhibit nearly identical patterns of causal influences. Inattention and hyperactivity-impulsivity also have very similar patterns of causal influences, although each has dimension-specific genetic and nonshared environmental influences.
It is important to note that the results of the common pathways model analyses of the Tennessee Twins Study (Waldman et al., in press) support the criterion validity of the general factor in two important ways. First, if the general factor reflected no more than correlated error variance, one would expect 100% nonshared environmental influences because this term includes error of measurement. In contrast, the moderate genetic and shared environmental influences on the general factor support its validity. Second, the model that included the general factor accounted for substantially more of the total pleiotropic genetic variance due to higher-order factors than the model including only internalizing and externalizing factors (Waldman et al., in press). This suggests that attempts to define empirical phenotypes for genetic research that optimally reflect pleiotropic genetic influences on psychopathology should include the general factor of psychopathology.
Shared Genetic Influences over Time
Although much remains to be learned, a longitudinal study of a large representative sample of twins found that adult ratings of externalizing problems at age 5 years significantly predicted new internalizing problems at age 12 largely because of shared genetic influences on these two domains of problems at the two ages (Wertz et al., in press). Similarly, in the British Genesis Study of 2,619 twins and siblings, depression, GAD, and fears dimensions were assessed across adolescence. Each dimension at age 15 years significantly predicted both itself and each other dimension at 17 and 20 years of age. Stable shared genetic influences explained most of the homotypic and heterotypic continuity, but a modest degree of stability was due to enduring nonshared environmental influences. In contrast, changes in symptoms over time were mostly due to nonshared environmental influences that were both dimension-specific and time-specific, although some change was due to novel genetic influences that came on line at each age. Interestingly, these age-specific genetic influences were common to multiple dimensions, contributing to their comorbidity at each age (Waszczuk et al., 2016).
Measurement Error in Multivariate Biometric Twin Models
It is important to consider measurement error when interpreting the results of any statistical model of psychopathology, including twin models. For example, when error in the measurement of each dimension is uncorrelated across dimensions, it inflates estimates of the extent to which nonshared environmental influences are dimension-specific. In contrast, when measurement error is correlated across dimensions (e.g., individuals ‘exaggerate’ or ‘minimize’ two or more dimensions of their symptoms to similar extents), such correlated measurement error would increase the extent to which nonshared environmental influences are common to all dimensions. Furthermore, if mothers tend to exaggerate or minimize reports of a dimension of symptoms in their twin children, such correlated measurement error would inflate cross-twin correlations on that dimension. If this inflation were to be the same extent for monozygotic and dizygotic twins, it would increase estimates of shared environmental influences. In contrast, if mothers of monozygotic twins tend to rate their twins in systematically more correlated ways than do mothers of dizygotic twins, that would inflate estimates of heritability. Nonetheless, although twin modeling must be interpreted with due caution, it provides a strong basis for causal hypotheses that can be tested with other research strategies with different threats to their internal validity, such as tests of associations with genetic polymorphisms (discussed below).
Severe Psychopathology and the General Factor of Psychopathology
The evidence reviewed above was based on common (i.e., prevalent) forms of psychopathology. In contrast, little evidence exists on the placement of uncommon but severe forms of psychopathology in the causal taxonomy. Nonetheless, there is now sufficient evidence to advance a hypothesis regarding the role of mania, nonaffective psychosis, and autism in the causal taxonomy that, if supported, would substantially change our understanding of these disorders by suggesting that they deeply share causal influences with more common forms of psychopathology. One study of a large representative sample of adults found that the diagnosis of bipolar disorder loaded on an internalizing rather than an externalizing factor (Forbush & Watson, 2013), but analyses of NESARC data found that mania loaded on both internalizing and externalizing factors (Keyes et al., 2013). In contrast, other factor analytic studies found that symptoms of mania and psychosis load on a higher-order factor that is separate from internalizing and externalizing factors, but robustly correlated with them (Kotov, Chang, et al., 2011; Kotov, Ruggero, et al., 2011; Markon, 2010b; Wright et al., 2013).
None of these studies specified a general factor of psychopathology, however. This is important because bipolar disorder and schizophrenia are robustly comorbid with essentially all other common mental disorders in representative samples of adults (McMillan, Enns, Cox, & Sareen, 2009; Merikangas et al., 2011). Data from the longitudinal TRAILS study were analyzed using the same models employed by Caspi et al. (2014) to test the general factor hypothesis, but across younger ages (i.e., 11 – 19 years (Laceulle et al., 2015). Their results supported the general factor hypothesis and like Caspi et al. (2014), they found that the general factor model fit slightly better than a correlated three-factor model when psychotic symptoms and OCD loaded only on the general factor. In addition, a CFA of data from two representative samples of adolescents similarly identified a general factor based on multiple dimensions of anxiety, depression, and psychotic symptoms, even though they did not include externalizing symptoms in their model (Stochl et al., 2015). These findings suggest that the causal risk factors for mania and psychosis may be the same as the factors that nonspecifically increase risk for all common internalizing and externalizing disorders.
This hypothesis is strengthened by the results of analyses of data from three large representative samples of adults: the National Comorbidity Study (Kessler, 1995), National Comorbidity Study-Replication (Kessler, Chiu, Demler, & Walters, 2005), and wave 2 of NESARC (Ruan et al., 2008). Person-based analyses of diagnoses of mental disorders were conducted using latent class analysis. In each of these studies, persons who met criteria for bipolar disorder and nonaffective psychosis were almost exclusively found in the latent class of persons who exhibited multiple internalizing and externalizing mental disorders (El-Gabalawy et al., 2013; Vaidyanathan, Patrick, & Iacono, 2011, 2012). One likely possibility is that the members of this class, who exhibited multiple mental disorders across domains, would have exhibited high scores on a general factor of psychopathology had it been specified.
To further evaluate this hypothesis, we conducted additional new analyses of data on the 29,958 adults ages 18–65 who participated in both waves 1 and 2 of NESARC. The lifetime prevalence of experiencing a manic episode by wave 1 was 3.8%. We tested the association of these manic episodes in wave 1 with latent general, externalizing, and internalizing factors derived from a bifactor CFA, as shown in Figure 2B (Lahey et al., 2012). The general factor score was robustly associated with mania, but mania also had a weaker but also significant association with the externalizing factor. Neither the fears nor the distress factors were correlated with manic episodes in this model. Of great interest, the strong association with the general factor reflected the fact that 100% of the persons who had experienced a manic episode by wave 1 were in the top 16% of scores on the general psychopathology factor. That is, although the general score was derived from common internalizing and externalizing disorders (i.e., not including mania), the diagnosis of mania was exclusively found in individuals with scores on the general factor that were at least 1 standard deviation about the sample mean. An additional 1.9% of the sample experienced a first episode of mania during the next three years. Only the general psychopathology factor scores significantly predicted these incident manic episodes.
Two studies addressed the place of autism in the hierarchical structure of psychopathology. In a study of a broad range of symptoms in 9–12 year old twins (Pettersson et al., 2013), a general factor accounted for a large proportion of the phenotypic covariation among symptoms of ADHD, autism, tics, and specific learning disorders. Furthermore, an analysis of data from a large sample adolescents also supported the existence of a general factor of psychopathology, with symptoms of autism loading significantly on the general factor (Noordhof et al., 2015).
Moderation of Causal Influences by Sex and Age
As noted above, the existing evidence suggests that the correlational structure of psychopathology is largely invariant across sex and age. Nonetheless, there are widespread and robust sex and age differences in mean levels of most first- and higher-order dimensions of psychopathology—including sex differences that change with age—that must be explained to achieve a full understanding of the nature and causes of psychopathology (Crick & Zahn-Waxler, 2003; Eaton et al., 2012; Keenan & Shaw, 1997; Rutter, Caspi, & Moffitt, 2003). These topics require careful scrutiny, both because of the inherent importance in understanding sex and age differences and because of what understanding them will tell us about the nature of psychopathology itself. Therefore, we briefly address these topics in Supplement 4.
Evidence from Molecular Genetic Studies
Biometric studies of twins and other siblings are not the only source of information on the hierarchy of causal influences on dimensions of psychopathology. Although nearly all molecular genetic studies of psychopathology have tested for associations of genetic variants with only a single diagnosis at a time in case-control designs, recent studies suggest that at least some specific molecular genetic variants are pleiotropically associated with multiple mental disorders (Davis et al., 2013; Havik et al., 2012; Maier et al., 2015; Smoller, 2013; Smoller et al., 2013; Williams et al., 2011). In particular, a series of recent studies from the Psychiatric Genomics Consortium (PGC) examined pleiotropic genetic effects on five disorders (schizophrenia, bipolar disorder, MDD, ADHD, and autism). In the first of these studies, four genomic loci were found to be associated with multiple disorders at genome-wide levels of significance (Smoller et al., 2013). Similarly, polygenic risk scores based on large numbers of common single nucleotide polymorphisms (SNPs) were found to be associated with these five disorders, particularly the adult-onset disorders, although some associations were disorder-specific (Smoller et al., 2013). In a follow up study by the same consortium, univariate heritabilities for each of the five disorders and bivariate heritabilities among them were estimated using common SNPs (S. H. Lee et al., 2013). The SNP-based heritabilities of each disorder were significant, although considerably lower (17–29%) than that estimated from twin studies. Importantly, however, there was a high genetic correlation between schizophrenia and bipolar disorder (r = .68), moderate genetic correlations of MDD with bipolar disorder, schizophrenia, and ADHD (r = .47, .43, and .32, respectively), and a low but significant genetic correlation between schizophrenia and autism (r = .16) (S. H. Lee et al., 2013). Importantly, these findings indicate that the pattern of pleiotropic genetic influences estimated from large numbers of common SNPs is consistent with the results of the multivariate twin studies reviewed above (Lee et al., 2013; Smoller, 2013).
DISPOSITIONAL CONSTRUCTS AND THE CAUSAL STRUCTURE OF PSYCHOPATHOLOGY
Psychologists have long studied the complex associations between mental disorders and traits of temperament and personality (Carey & DiLalla, 1994; Cattell, Bjersted, & Schmidt, 1972; Clark, Watson, & Mineka, 1994; S. B. G. Eysenck, White, & Eysenck, 1976). In this section, we use some of what is known about such traits to further our understanding of the heterogeneous causal structure of psychopathology. Like others, we use the term ‘disposition’ to refer to these constructs to avoid unnecessary theoretical implications (Mischel, 2004). Our view is that the distinction between ‘disposition’ and ‘psychopathology’ is inherently and unavoidably fuzzy, but nonetheless important. Conceptually, the term dispositional traits refers to relatively enduring individual differences in dimensions of behavior that span ‘normal’ and ‘abnormal’ functioning, whereas psychopathology refers to dimensions of behavior that are maladaptive, but the boundary between disposition and psychopathology is so ill-defined as to suggest a continuum (Krueger & Markon, 2006b). The fuzziness of the distinction between dispositions and psychopathology in research also derives from the fact that nearly all measures of dispositional traits include many items that are synonyms or antonyms of symptoms of psychopathology, which may inflate correlations between the two constructs (Lahey, 2004; Lahey, Applegate, et al., 2008). Although there is some encouraging evidence that item overlap is not the primary source of most disposition-psychopathology correlations (Lahey, Applegate, et al., 2008; Lahey, Rathouz, Applegate, Tackett, & Waldman, 2010; Lemery, Essex, & Smider, 2002), it is essential for future studies of dispositions and psychopathology to consider the issue of confounding due to overlapping items.
Acknowledging these limitations, we discuss relations between dispositions and psychopathology in this paper for three reasons. First, if the higher-order general, externalizing, fears, and distress factors of psychopathology are found to correlate differentially with dispositional traits that would support the discriminant validity of these factors of psychopathology and reveal something of their natures. Second, research on dispositional traits, and on associations between dispositional traits and psychopathology, are topics of vibrant research and theory (Brooker et al., 2013; Kendler & Myers, 2010; Krueger & Tackett, 2003; Nigg, 2006; Tackett, 2006; Vasey et al., 2013; Widiger, 2011). As the nature of dispositions is clarified, the vast existing body of research on them will become a rich source of information regarding the nature of the dimensions of psychopathology that are correlated with them. Third, although the data are inconsistent, there is evidence that the influence of environmental factors on psychopathology is moderated by dispositional traits (Kushner, 2015; Ormel et al., 2013). For example, a prospective study of adult women measured dispositions and depression symptoms prior to Hurricane Sandy (Kopala-Sibley et al., 2016). Women exposed to the hurricane exhibited increased depression symptoms, but only if they were high in negative emotionality or low in positive emotionality before the hurricane.
Dispositions are Transdiagnostic/Transdimensional Processes
The present hypotheses regarding associations between dispositional traits and psychopathology are partly based on, and are very similar to, those advanced in the transdiagnostic model of psychopathology advanced by David Barlow and colleagues (Barlow, Allen, & Choate, 2004; Barlow, Sauer-Zavala, et al., 2014) and Susan Nolen-Hoeksema and Edward Watkins (Nolen-Hoeksema & Watkins, 2011). The transdiagnostic approach hypothesizes that individual differences in a relatively small number of processes are related to risk for multiple different diagnoses of mental disorder and help explain their comorbidities. Some transdiagnostic processes in these models can be viewed as dispositional constructs, such as trait negative and positive emotionality, whereas other hypothesized transdiagnostic processes may be facets of dispositions, such as a trait-like tendency to ruminate (Barlow et al., 2004; McLaughlin & Nolen-Hoeksema, 2011; Nolen-Hoeksema & Watkins, 2011).
Barlow’s (2000, 2014) seminal transdiagnostic model focuses on the internalizing disorders rather than the full spectrum of psychopathology. Similarly, our first model of relations between dispositions and psychopathology addressed only externalizing psychopathology in children and adolescents (Lahey & Waldman, 2003, 2012; Lahey, Waldman, & McBurnett, 1999). Although the dimensions of psychopathology addressed in these two sets of papers were different, both sets of papers viewed negative emotionality as a key cross-cutting construct that is related to multiple dimensions of psychopathology and reflects etiologic influences that nonspecifically increase risk for all disorders. In Barlow’s model (2000, 2014), GAD, MDD, and panic attacks are viewed, in part, as varying expressions of the same processes that influence negative emotionality. In Lahey and Waldman’s (1999, 2012) model, negative emotionality is viewed as nonspecifically related to risk for ADHD, ODD, and CD. In both models, the various dimensions of psychopathology are viewed as being partly differentiated by their associations with other transdiagnostic dispositions. For example, in Barlow’s model, deficient positive emotionality is hypothesized to be related only to depression and social anxiety disorder, whereas heightened autonomic arousability is related specifically to panic and agoraphobia (Brown, Chorpita, & Barlow, 1998). In some ways, therefore, the present discussion of the role of dispositional constructs in the heterogeneous causal structure of psychopathology can be viewed as an expansion of earlier transdiagnostic models that addressed only internalizing or only externalizing psychopathology.
Dispositions and the Hierarchical Structure of Psychopathology
There is abundant evidence of correlations between dispositional dimensions and psychopathology across the lifespan in the research literature. Consider the dispositional construct of negative emotionality or neuroticism. These terms have been defined in a variety of different but overlapping ways that refer to a tendency to experience negative emotions frequently and out of proportion to the provocation (Barlow, Ellard, Sauer-Zavala, Bullis, & Carl, 2014; H. J. Eysenck, 1947; Lahey et al., 2010; McCrae & Costa, 2003). The multiple scales based on these various definitions are highly correlated (Lahey et al., 2010; Zuckerman, Kuhlman, Teta, Joireman, & Kraft, 1993) and there is extensive evidence of robust correlations between negative emotionality and every first-order dimension of common forms of psychopathology in both the internalizing and externalizing domains across the lifespan (Barlow, Ellard, et al., 2014; Gjone & Stevenson, 1997; Hink et al., 2013; Jeronimus, Kotov, Riese, & Ormel, 2016; Kendler & Myers, 2010; Krueger, 1999; Krueger, Caspi, Moffitt, Silva, & McGee, 1996; Krueger & Markon, 2006b; Lahey, 2009; Lahey et al., 2010; Ormel et al., 2013; Stringaris & Goodman, 2009). Similarly, in the large 3-year longitudinal NEMESIS study of adults, neuroticism predicted first (i.e., incident) diagnoses in every measured domain of disorders (mood, anxiety, and substance use disorders) and the degree of comorbidity among them (de Graaf, Bijl, ten Have, Beekman, & Vollebergh, 2004). Furthermore, neuroticism explained a large proportion of the phenotypic correlations among specific internalizing diagnoses, among specific externalizing diagnoses, and between latent internalizing and externalizing factors in a large representative sample of adults (Khan, Jacobson, Gardner, Prescott, & Kendler, 2005). The consistent evidence that negative emotionality is robustly related to all first-order dimensions of psychopathology, and even predicts the magnitudes of the correlations among them, strongly suggests that negative emotionality lies at the heart of the general factor of psychopathology. As such, everything that has been learned about negative emotionality is potentially relevant to the psychobiological processes that are common to all prevalent forms of psychopathology (Lahey, 2009; Lilienfeld, 2003).
In contrast, constraint has been found to be inversely correlated with externalizing psychopathology across the lifespan, but positively, if weakly, associated with the internalizing domain (Hink et al., 2013; Krueger, 1999; Krueger & Markon, 2006b; Krueger, McGue, & Iacono, 2001; Lahey, 2009; Lahey et al., 2010). Constraint refers to domain of dispositions related to the inhibitory control of emotion and behavior, that is often conceptualized as the opposite of impulsivity (Beauchaine & McNulty, 2013; Carver, 2005; Patrick, Curtin, & Tellegen, 2002) and/or disinhibition (Gray & McNaughton, 2003; Latzman, Vaidya, Clark, & Watson, 2011). Thus, the observed inverse correlation of dispositions in the constraint domain with externalizing psychopathology, but not with internalizing psychopathology, supports the criterion validity of the distinction between the higher-order internalizing and externalizing psychopathology factors and suggests important hypotheses regarding the psychobiological processes that differentiate these two broad domains of psychopathology.
Based on the observations just reviewed, phenotypic correlations were assessed between parent ratings of the dispositional dimensions measured by the Child and Adolescent Dispositions Scale (CADS) (Lahey, Applegate, et al., 2008) and latent phenotypic dimensions of parent-rated psychopathology in the Tennessee Twin Study (Tackett et al., 2013). The CADS was developed to test hypotheses regarding associations between dispositions and symptoms using a pool of items from which clear synonyms and antonyms of symptoms of psychopathology were excluded to avoid confounding. CFAs of CADS items yielded three factors: Negative emotionality reflects individual differences in the labile expression of negative emotions. The second factor measures prosocial feelings and behaviors. Following current usage (Frick, Ray, Thornton, & Kahn, 2014), these items were scored inversely and labeled callousness. The third factor, termed daring, measures adventurousness and the enjoyment of situations that are loud, exciting, and risky. These three dispositional dimensions have each been shown to be reliable and valid in terms of their differential correlations with direct observations and other external criteria (Lahey, Applegate, et al., 2008). As shown in Figure 4, the phenotypic correlation of negative emotionality with the latent general psychopathology factor was r = .58. The correlation of negative emotionality with externalizing psychopathology also was significant, but significantly smaller than the correlation with the general factor, and the correlation of negative emotionality with internalizing was quite small. This does not mean that the emotions involved in internalizing dimensions are not ‘negative,’ only that the correlation between the internalizing factor and the dispositional construct of negative emotionality is small when the much stronger correlation of negative emotionality with the general factor—on which the internalizing dimensions all load—is modeled. The two CADS dispositional dimensions that are most related to constraint in this study (callousness and daring) each exhibited small correlations with the general factor of psychopathology (Tackett et al., 2013). Nonetheless, consistent with our model relating dispositions to externalizing psychopathology (Lahey & Waldman, 2003, 2012), callousness (low prosociality) was moderately correlated with the latent externalizing factor, but was correlated with internalizing psychopathology at a significantly smaller level (Tackett et al., 2013). Again, it is important to keep in mind when considering these findings that the inclusion of a general psychopathology factor in a bifactor model changes the interpretation of the internalizing and externalizing factors, which are, in essence, residualized on the general factor.
Figure 4.
Phenotypic correlations of three dispositional constructs measured by the Child and Adolescent Dispositions Scale (Lahey, Applegate, et al., 2008) with latent factors from a bifactor model of the phenotypic correlational structure among 11 first-order dimensions of psychopathology (redrawn from Figure 2, Tackett et al., 2013).
Associations between higher-order dimensions of psychopathology and dispositions also were tested in a study of a community sample of 3-year olds (Olino et al., 2014). Consistent with findings at older ages, the general factor was positively correlated with negative emotionality. After residualizing on the general factor, the internalizing factor was inversely correlated with surgency whereas externalizing was positively correlated with surgency and inversely associated with effortful control (Olino et al., 2014). In the study of young adults by Caspi et al. (2014) described earlier, phenotypic correlations between a general factor of psychopathology and dispositions were assessed using the NEO-PIR, which assesses the five-factor model of personality (Costa & McCrae, 1992). Consistent with the findings of Tackett et al. (2013) with children and adolescents, Caspi et al. (2013) also found a moderate phenotypic correlation between the general factor of psychopathology and NEO neuroticism.
ETIOLOGIC HETEROGENEITY OF CATEGORIES AND DIMENSIONS OF PSYCHOPATHOLOGY
The evidence just reviewed reveals and emphasizes the need to look beyond dimension-specific etiologic influences to also address the broadly shared etiologic influences that link the dimensions of psychopathology in a taxonomy of causes. It is very important to note that the present causal taxonomy addresses more than just the broad sharing of causal influences, however. It also provides a powerful novel framework for revealing the equally important heterogeneity in the causes and mechanisms underlying each first-order dimension of psychopathology. There are two ways in which such heterogeneity in etiologies and mechanisms can be understood in the present causal taxonomy:
Reversing the logic of the hierarchical causal taxonomy suggests that the reasons why different dimensions of psychopathology are correlated are the same reasons why each first-order dimension of psychopathology is heterogeneous. That is, the present causal taxonomy provides a revealing new splitting-by-lumping perspective on why different persons with the same level of symptoms of a given first-order dimension can be influenced by different etiologies. The hierarchical causal taxonomy implies that the etiologic influences on each first-order dimension of psychopathology are heterogeneous largely because they can arise from (at least) three separate and largely orthogonal sources. For example, some persons who meet criteria for CD may not carry any risk genotypes for those behaviors and may exhibit them due to environmental influences. Other persons who meet criteria for CD may carry only genotypes that pleiotropically increase risk for all dimensions of psychopathology, including CD, through the general factor. Other persons may carry only genotypes that increase risk for all externalizing dimensions, whereas others may carry only genotypes that specifically increase risk only for CD, and many others will carry varying combinations of genotypes from each of these sources. The result is likely to be a degree of heterogeneity in the genetic influences on each form of psychopathology that will challenge, and likely defeat, studies seeking to identify genetic variants associated with only one dimension of psychopathology. It should be far more efficient to identify such diverse etiologic influences and their related mechanisms at their source —by modeling higher-order phenotypes—than by attempting to fractionate each first-order dimension into its multiple etiologies and mechanisms.
Heterogeneity in the causes and mechanisms operating within each first-order dimension also arises when more than one etiologic factor operates at any level of the causal hierarchy. That is, each level of the taxonomy is unlikely to be homogeneous in terms of its etiologic and psychobiological mechanisms. Hypothetically, if some genetic variants related to the dispositional trait of callousness and other genetic variants related to the inhibition of prepotent responses each nonspecifically contribute to the risk for all first-order dimensions in the higher-order externalizing domain, different persons could display the same number of symptoms of any first-order externalizing dimension because of the risk conferred by different combinations of these two sets genetic influences. Such heterogeneity may be revealed in variations in fine-grain subsets of symptoms in some cases. This possibility has been cogently addressed in studies of adult twins (Kendler, Aggen, & Neale, 2013; Kendler, Aggen, & Patrick, 2012; Kendler, Aggen, Prescott, Crabbe, & Neale, 2012). In one study, factor analysis of the symptoms of antisocial personality disorder yielded two factors, with symptoms of irritability, fighting, and reckless disregard for others loading strongly on one factor, and lack of remorse, deceit, failure to plan ahead, and irresponsibility loading on the second factor (Kendler et al., 2012). Furthermore, the best-fitting behavior genetic model included two genetic factors, each with stronger loadings on one of the two phenotypic factors. One possibility, therefore, is that antisocial personality disorder is heterogeneous in the sense that (at least) two genetic processes each give rise to different fine-grain subsets of antisocial symptoms. A possibility that has not yet been examined is that the subset of irritability symptoms causally is linked to the general factor and the lack of subset of remorse symptoms is linked to the externalizing factor. Similar behavior genetic analyses of symptoms of MDD and alcohol use disorder indicated similar patterns of different etiologic influences on different subsets of symptoms of each of these disorders (Kendler et al., 2013; Kendler, Aggen, Prescott, et al., 2012). Including the full causal taxonomy of psychopathology in future studies would reveal the level(s) of the hierarchy at which each source of such causal heterogeneity operate.
Transdimensional Dispositions and the Causal Heterogeneity of Psychopathology
There are fundamental similarities between the present causal taxonomy and key tenets of the NIMH RDoC initiative (Cuthbert & Kozak, 2013; Insel et al., 2010; Sanislow et al., 2010). Like the game-changing transdiagnostic models of psychopathology (Barlow, Sauer-Zavala, et al., 2014; Nolen-Hoeksema & Watkins, 2011), the central hypothesis of the RDoC approach is that psychobiological constructs do not align one-to-one with categorical mental disorders, but are related to diagnoses in a cross-cutting manner (Cuthbert & Insel, 2013). As a result, each mental disorder is heterogeneous and reflects dysfunction in more than one psychobiological construct, and the same psychobiological construct may be related to multiple categorical mental disorders. Therefore, persons who meet criteria for a given categorical diagnosis often differ from one another so much that studying the etiology and mechanisms of that diagnosis would be fruitless and even misleading (Sanislow et al., 2010). We have adopted a similar view of the heterogeneity of first-order dimensions of psychology. Therefore, we agree with the RDoC perspective that the “grain size” of first-order dimensions (and diagnoses) of psychopathology is often too large and that a focus on transdimensional psychobiological constructs may be far more productive (Cuthbert & Insel, 2013). We differ, however, by positing that the “grain size” of first-order dimensions is also often too small, and that much will be learned about the fine-grain heterogeneity of first-order dimensions by modeling the higher-order factors of psychopathology that provide a platform for understanding the origins of the causal and mechanistic heterogeneity of first-order dimensions.
Viewing Symptoms through the Lens of Dispositions
The RDoC initiative shifts the focus of research from diagnoses to constructs: “Rather than starting with symptom-based definitions of disorders and working toward their pathophysiology, RDoC inverts this process.” [p. 4] (Cuthbert & Insel, 2013). Many elements in the RDoC matrix (www.nimh.nih.gov/research-priorities/rdoc/constructs/rdoc-matrix.shtml) can be viewed as dispositional psychobiological constructs that are jointly defined by individual differences at both behavioral and biological levels of analysis (Cuthbert & Insel, 2013). That is, one potentially productive route to understanding the nature of psychopathology would be to study a dispositional construct at both biological and behavioral levels and relate it to symptoms of psychopathology. Because the ultimate aim of the NIMH RDoC approach is to reduce the burden of mental health problems, its emphasis is on understanding the constructs associated with impairing symptoms of psychopathology; its innovative strategy is to ignore diagnostic definitions of categorical mental disorders in doing so (Sanislow et al., 2010).
From Dispositions to Symptoms: An Illustration
Here we explore the potential advantages of viewing symptoms from the starting point of psychobiological constructs rather than diagnoses. We conducted a new empirical exercise for this paper using data on dispositional constructs and symptoms from the population-based sample of 1,358 4–17 year old children and adolescents in the Georgia Health and Behavior Study (Lahey et al., 2004). In this study, parents rated dispositional items and symptoms of psychopathology. Dispositions of negative emotionality, callousness, and daring were measured using the CADS (Lahey, Applegate, et al., 2008), but we use these dispositions simply as examples of the many dispositional constructs that could be studied in the same way. Similarly, the DSM-IV symptoms of specific phobia, SAD, MDD, inattention, hyperactivity-impulsivity, ODD, and CD used in Figure 5 are examples of the broader range of symptoms of psychopathology that could be studied in the same way.
Figure 5.
Three-dimensional plots of illustrative parent-reported symptoms of psychopathology of selected disorders based on the mean ratings received by children and adolescents who exhibit the specific symptom on three dispositional constructs measured by the Child and Adolescent Dispositions Scale (Lahey, Applegate, et al., 2008). Neg Emot = negative emotionality.
In the four panels of Figure 5, each symptom is plotted in three-dimensional ‘dispositional space,’ with the coordinates being the mean ratings on each disposition given to all children and adolescents who exhibited each specific symptom. For this purpose, children were said to exhibit a symptom if they received a rating of ‘pretty much’ or ‘very much’. Following the RDoC strategy, diagnoses were ignored in this empirical exercise. Nonetheless, Figure 5A shows that many symptoms of each mental disorder generally cluster with one another in ‘dispositional space.’ For example, the symptoms of specific phobia are all associated with relatively low ratings on all three dispositional dimensions. In contrast, some symptoms of ODD and CD are associated with very high ratings on all three of these dispositions.
Figure 5B presents the mean dispositional ratings on symptoms of MDD and specific phobia on expanded scales of the mean dispositional ratings. In this ‘close up’ view, there is separation of these two clusters of symptoms on all three dispositional dimensions, although some symptoms of MDD (i.e., the core mood symptoms of anhedonia and dysphoria along with hypersomnia, fatigue, and low self-esteem) are more distant from specific phobias than are the other MDD symptoms. Not all clusters of symptoms of a different mental disorder are equally well separated in dispositional space, however. For example, in Figure 5C, although the symptoms of inattention (blue squares) are tightly grouped with one another, they occupy dispositional space that is very close to both the ODD symptoms and the core mood symptoms of MDD. In contrast, Figure 5D shows that the symptoms of hyperactivity-impulsivity (green squares) are clustered with the remaining MDD symptoms. Associations of the symptoms with callousness and daring were less widespread and less consistent among the symptoms of a given disorder. Nonetheless, the odds of all symptoms of ODD and inattention were reliably greater for youth given higher ratings on callousness. In addition, the odds of most symptoms of CD were reliably greater at higher ratings on callousness. Only fear of blood was inversely related to callousness. Daring was positively associated with symptoms of hyperactivity-impulsivity and ODD/CD symptoms of defying adults, spiteful and vindictive, and lying to con. In contrast, daring was inversely related to fears of dogs and blood.
These illustrative findings suggest three important things for the study of psychopathology. First, the robust associations of symptoms with dispositional constructs indicate that one could productively follow an RDoC strategy and study, for example, the dispositional trait of negative emotionality at both neurobiological and behavioral levels to relate variation in that construct to impairing symptoms of psychopathology. Second, these illustrative findings suggest that different symptoms are related to different combinations of multiple dispositions. For example, youth who are spiteful and vindictive are rated high in negative emotionality, callousness, and daring. In contrast, children who are fearful of blood are also high in negative emotionality, but low in callousness and daring. This suggests that it could be very limiting to study the association of psychopathology with one disposition at a time.
Third, a potential limitation inherent in relating dispositional constructs only to dimensions of psychopathology is that it assumes that each symptom that defines a first-order dimension of psychopathology is related to each dispositional construct under study in the same way. The data shown in Figure 5 suggest that this may not always be the case. For example, Figure 5 confirms the strong hypothesized associations between negative emotionality (on the vertical axis) and ODD symptoms, but reveals a substantial degree of heterogeneity in the magnitudes of those correlations. Understandably, ODD symptoms that reflect experiencing negative emotion (e.g., irritability and temper tantrums) are more strongly correlated with the disposition of negative emotionality than are the two ODD symptoms that reflect acting against others (deliberately annoys others and acting in spiteful or vindictive ways). Furthermore, consistent with the high loadings of MDD and GAD on the general psychopathology factor, each of these symptom dimensions shows a significant correlation with negative emotionality (consistent with Figure 4). Perhaps the most interesting finding for MDD and GAD symptoms in Figure 5, however, is the heterogeneity in the magnitudes of their correlations with negative emotionality, with symptoms reflecting fatigue, hypersomnia, psychomotor retardation, mind going blank, and suicidal behavior showing weaker correlations with negative emotionality than other MDD and GAD symptoms. Thus, the two strategies of relating RDoC-like dispositional constructs to individual symptoms or to hierarchically ordered dimensions of symptoms should be viewed as complementary. They each paint essentially the same picture of how dispositional constructs are related to psychopathology symptoms, but each reveals different information.
Causal Connections between Dispositions and Psychopathology
What causes the robust phenotypic correlations between dispositional and psychopathology dimensions just described? Analyses of data from a large study of adult twins found that genetic influences on neuroticism account for at least one-third of the genetic influences on each individual internalizing diagnosis, with additional sharing of nonshared environmental influences (Hettema, Neale, Myers, Prescott, & Kendler, 2006). Similarly, a study of a representative sample of 4–17 year old twins collected parent ratings on both multiple dimensions of externalizing psychopathology and the dispositional dimension of negative emotionality (Singh & Waldman, 2010). Both bivariate and multivariate biometric analyses indicated that much of the phenotypic correlation between each first-order dimension of externalizing psychopathology and negative emotionality was due to pleiotropic genetic influences. Similarly, a study of same-sex 6- to 12-year old twins (Taylor, Allan, Mikolajewski, & Hart, 2013) estimated the extent to which a higher-order factor of parent-rated externalizing psychopathology shared its genetic influences with parent ratings on three dispositional dimensions measured by the CADS (Lahey, Applegate, et al., 2008). A Cholesky decomposition model (Neale & Cardon, 1992) revealed that the genetic influences on dispositions and psychopathology dimensions overlapped substantially.
A key issue for the present causal taxonomy, however, is the sharing of genetic influences on dispositions and on both internalizing and externalizing psychopathology. In separate multivariate biometric analysis of data on the same twins studied by Taylor et al. (2013), but at older ages, the same team (Mikolajewski, Allan, Hart, Lonigan, & Taylor, 2013) defined a latent trait of negative affect based on parent ratings of both CADS negative emotionality (Lahey, Applegate, et al., 2008) and the negative affect scale of the PANAS (Watson, Clark, & Tellegen, 1988). An independent pathways model (Neale & Cardon, 1992), revealed that both parent-rated externalizing and internalizing psychopathology factors loaded on the same latent factor of additive genetic influences on which negative affect had the strongest loading. This suggests that the phenotypic correlation between higher-order internalizing and externalizing factors is at least partly due to genetic influences that both internalizing and externalizing psychopathology also share with negative emotionality. Another similar study of adolescent twin pairs also found considerable overlap between the genetic influences on negative emotionality and both internalizing and externalizing disorders (Hink et al., 2013). One possible implication of these findings is that negative emotionality may be related to psychopathology through genetic influences shared with the general factor.
Analyses of data from the Tennessee Twin Study revealed that the general factor of psychopathology shared 50% of its additive genetic influences with CADS negative emotionality, but shared only 6% and 4% of its additive genetic influences with callousness and daring, respectively (Tackett et al., 2013). In contrast, the externalizing factor in this hierarchical factor model shared 31% of its latent additive genetic influences with CADS callousness and 15% with negative emotionality (Tackett et al., 2013). The internalizing factor in this model did not significantly share genetic influences with any of the CADS dispositional dimensions (Tackett et al., 2013). A twin study of MDD in adults similarly found that phenotypic correlations of neuroticism and conscientiousness with MDD were partially due to shared genetic influences on each trait-disorder pair (Kendler & Myers, 2010). Consistent with these findings, a meta-analysis of large samples of adults found that a polygenic risk score derived from common genetic variants associated with neuroticism was also significantly associated with MDD (Genetics of Personality Consortium, 2015). This is interesting given the central role of MDD in defining the general factor of psychopathology and its clear relation with negative emotionality. Taken together, the findings of these several multivariate behavior genetic studies suggest that the general factor of psychopathology substantially shares its genetic influences with negative emotionality. This hypothesis may help guide future research on the genetics of the general factor. For this reason, recent findings of the association of 11 genetic markers with a measure of negative emotionality (and the estimated genetic correlation between negative emotionality and depression estimated from SNPs of r = .75) are very encouraging (Okbay et al., 2016).
Psychobiological Constructs in the Hierarchical Causal Structure of Psychopathology
The hypotheses just stated regarding causal links between dispositions and psychopathology have clear implications for the mechanisms underlying psychopathology. We conceptualize genetic and environmental influences on psychopathology as operating through psychobiological constructs, which we define as processes that can be studied at both psychological and biological levels of analysis. Individual differences in the genetic processes that encode proteins almost certainly interplay with environments to create variations among persons in such psychobiological constructs. These include variations the structure and function of the brain, endocrine systems, and other processes and parallel individual differences in behavior. Although it is likely that individual differences in such psychobiological constructs vary over time, they are also relatively trait-like dispositions.
HYPOTHESES OF THE CASUAL TAXONOMY
Based on the evidence reviewed above, we posit a hierarchy of distributed causal influences on psychopathology that operates at multiple levels, all of which must be considered simultaneously to fully understand any first-order dimension of psychopathology. Some highly pleiotropic genetic and environmental causal factors broadly increase risk for all first-order dimensions of prevalent symptoms of psychopathology to varying degrees. Other causal factors pleiotropically increase risk only for any of the internalizing disorders (perhaps with distinctions between distress and fears dimensions), whereas other causal risk factors increase risk only for any of the externalizing dimensions. In addition to these pleiotropic casual factors, each first-order dimension likely has some degree of its own specific genetic and particularly environmental influences. Thus, studying the etiology of any first-order dimension of psychopathology by itself puts unnecessary blinders on research. One must look beyond each single first-order dimension of psychopathology to comprehensively identify its causal influences; both pleiotropic and dimension-specific causes must be considered at the same time (Lahey & Waldman, 2012).
The patterns of cross-sectional phenotypic correlations among dimensions of psychopathology reviewed above provide important initial clues to the underlying causal structure of psychopathology. This is because any causal taxonomy that is inconsistent with observed patterns of phenotypic correlations among psychopathology phenotypes can be ruled out. In particular, the widespread phenotypic correlations among first-order dimensions of psychopathology mean that it is virtually impossible for each first-order dimension to be influenced only by its own unique (i.e., distinct and uncorrelated) causal influences. Otherwise, these dimensions would not be correlated. Furthermore, bivariate and multivariate modeling of cross-sectional data from twin studies allow a disentangling of inferred genetic and environmental causal influences on psychopathology. Although more evidence is also needed from other types of studies that can disentangle causes, we offer hypotheses in Table 3 based on the available evidence to explain both (a) the sources of the extensive correlations among first-order dimensions of psychopathology, and (b) why—beyond random measurement error—first-order dimensions of psychopathology are not perfectly correlated (i.e., why first-order dimensions are differentiated as much as they are, in spite of their widely shared causal influences).
Table 3.
Hypotheses of the causal taxonomy.
Hypotheses Based on Cross-sectional Evidence
|
Hypotheses Regarding Heterogeneity in Casual Influences within Dimensions
|
Hypotheses Based on Longitudinal Evidence
|
Hypotheses Regarding Dispositional Constructs and Psychobiological Mechanisms
|
Hypotheses 1–5 in Table 3 are based on cross-sectional evidence; they address the hierarchy of shared causal influences that account for the correlated phenotypic and causal structure of psychopathology measured at any single point in time. Hypotheses 6 and 7 reverse the logic of the causal hierarchy to address the heterogeneity of each first-order dimension of psychopathology. This heterogeneity is the natural by-product of each first-order dimension of psychopathology receiving causal inputs from three separate and largely orthogonal sources. Hypotheses 8 and 9 address persistence and change in psychopathology over time. The patterns of homotypic and heterotypic continuity revealed by longitudinal studies are important in stimulating hypotheses regarding both fixed and particularly time-varying causal influences on psychopathology and in constraining the range of viable causal hypotheses. The high degree of homotypic continuity suggests that fixed factors (e.g., DNA sequences) and/or relatively unchanging or recurrent etiologic factors (e.g., chronic or intermittent stressful environments associated with poverty) are important influences on psychopathology. The genetic and environmental influences that foster homotypic continuity may work together through gene-environment correlation (Plomin, DeFries, & Loehlin, 1977), such as when genetic variation selects individuals into maladaptive environments that maintain the maladaptive behavior.
Although homotypic continuity is robust due to such constant or lasting causal influences, there is more than enough variation in psychopathology over time to indicate the operation of causal influences that drive changes in psychopathology. These may include developmental processes (e.g., neural maturation) that play out over time and time-varying factors that both (a) change levels of symptoms, and (b) give rise to the changes in symptoms that constitute heterotypic continuity. These factors may include genetic influences that come on line at particular points in development and time-varying environmental influences (e.g., changes in peer influences or acute stressors). Gene-environment correlation may operate in heterotypic continuity as well. That is, genetically influenced dimension X1 may preferentially predict dimension Y2 because X1 creates environmental conditions that foster symptoms of Y2.
Hypotheses 10–12 address the role of dispositional constructs defined jointly at the level of behavior and biology in the causal structure of psychopathology. Individual differences in such psychobiological constructs play a key role in the origins of psychopathology by moderating the impact of environmental influences. Furthermore, causal influences on first-order dimensions of psychopathology are hypothesized to be mediated by multiple psychobiological constructs. Individual differences in some dispositions are broadly related to risk for multiple dimensions of psychopathology, whereas other dispositional constructs are specifically related to fewer or even one first-order dimension of psychopathology.
IMPLICATIONS OF THE CAUSAL TAXONOMY FOR FUTURE RESEARCH
A primary motive for advancing the present causal taxonomy is to foster discussion of the most fruitful strategies for studying the etiologies and psychobiological mechanisms of psychopathology across the lifespan. To begin this dialogue, we aver that the current strategy of studying the neurobiology or the genetic influences on one categorically defined mental disorder at a time is the wrong way to proceed, and may be one reason for the slow progress in identifying specific causal risk factors. If the present causal taxonomy is substantially correct, the efficiency of etiologic research could be significantly improved.
Implications of the Causal Taxonomy for Studies of Molecular Genetics
Some genetic risk variants may be associated with a single mental disorder, but as reviewed above at least some common SNPs are pleiotropically associated with more than one mental disorder (Gratten, Wray, Keller, & Visscher, 2014; Kendler, 2005; S. H. Lee et al., 2013; Ruderfer et al., 2014; Sivakumaran et al., 2011; Smoller, 2013). Other studies similarly indicate that some rare copy number variants and other structural variants are nonspecifically associated with multiple mental disorders (Bergen et al., 2012; Ionita-Laza et al., 2014; Levinson et al., 2011; Malhotra et al., 2011; Sanders et al., 2011). A more powerful strategy for identifying pleiotropic molecular genetic variants that operate each level of the dimensional hierarchy of psychopathology would be to measure a broad range of first-order dimensions of psychopathology and define a latent general factor and two or more specific higher-order factors (e.g., internalizing and externalizing) in a bifactor model so that associations of genetic variants with each level of this hierarchy could be individually or jointly tested in structural equation modeling.iii This strategy would avoid a potentially widespread but unnecessary problem of false negatives. For example, assume that genetic variant x is pleiotropically associated with risk for any externalizing dimension of psychopathology. If one only tested associations with the diagnosis of ODD, for example, a person with the risk allele of variant x who met criterion for ADHD but not for ODD would be counted as a ‘miss.’ Similarly, a person with the risk allele of variant x who exhibited CD but not ODD would be considered a ‘miss.’ If associations of the same genetic variant with the higher-order externalizing phenotype had been studied instead, both of these associations would be ‘hits’, resulting in more accurate estimates of effect size for variant x. Following this strategy, Dick and colleagues conducted two studies of adults and adolescents and found that two candidate genetic variants in GABRA2 and CHRM2 were weakly associated with each specific externalizing disorder, but were more strongly associated with a higher-order externalizing factor derived from correlations among the specific disorders (Dick, Aliev, Wang, & al., 2008; Dick et al., 2009). The same logic would apply to the identification of genetic risk variants for the higher-order general and internalizing factors.
It is important to note that the case-control study designs typically used in genetic research are problematic for the discovery of pleiotropic molecular genetic variants associated with multiple first-order dimensions of psychopathology through higher-order phenotypes. Although the selection of individuals at the extremes of phenotypes (i.e., diagnosed cases and controls) can increase statistical power (Dolan & Boomsma, 1998; Eaves & Meyer, 1994), selecting cases based on a single diagnosis and controls based on the absence of that (or perhaps any) diagnosis biases correlations among the target disorder and other dimensions of psychopathology, making accurate estimates of higher-order phenotypes based on correlations among dimensions of psychopathology difficult. For example, selecting cases on the basis of a diagnosis of bipolar disorder would increase the likelihood of selecting individuals who also have other mental disorders that often co-occur with bipolar disorder and decrease the likelihood of selecting individuals with forms of psychopathology that co-occur less often with bipolar disorder, biasing estimates of correlations among the full range of psychopathology dimensions. Such biases might be corrected through weighting, but only if the control group were sufficiently large and representative. Given this, large representative samples in which multiple dimensions of psychopathology are measured provide the optimal data for discovering pleiotropic genetic risk variants associated with the dimensional hierarchy of psychopathology.
Furthermore, a series of simulations (van der Sluis, Posthuma, Nivard, Verhage, & Dolan, 2013; van der Sluis, Verhage, Posthuma, & Dolan, 2010) considered the power of genome wide association studies in which the phenotype was characterized by a diagnosis, a unidimensional composite score, a multi-dimensional characterization of the underlying phenotypic structure, and a multi-dimensional measurement model incorporating IRT properties. Substantial gains in power were found moving from a diagnosis to a unidimensional composite symptom dimension, to a more appropriate multi-dimensional structure, to testing such associations within the context of an IRT measurement model that allows for differences in factor loadings and item difficulties across symptoms. Such dimensional models also better reflect the complex pleiotropic nature of psychopathology that underlies multiple disorders (O’Dushlaine et al., 2015; Purcell et al., 2009).
Implications for the Study of Causal Environmental Influences
Based on the available evidence, we hypothesize that environmental influences on psychopathology that are not shared by family members are mostly dimension-specific and contribute to differentiation and change in psychopathology over time. Furthermore, as illustrated in Figure 3, there is evidence that both shared and nonshared environmental factors influence multiple dimensions of psychopathology at the level of the general factor and at the levels of externalizing or internalizing factors. The finding of substantial dimension-specific environmental influences is consistent with the findings of some longitudinal studies that most measured environmental variables were related specifically to one disorder or one higher-order domain (Shanahan, Copeland, Costello, & Angold, 2008). Not all environmental influences are likely to prove to be dimension-specific, however. The present causal taxonomy implies that, analogous to studies of molecular genetic risk variants, progress in discovering causal environmental risk variables may be more rapid if their associations with the hierarchy of phenotypes are studied (Lahey et al., 2011). For example, three studies found child maltreatment to be a predictor of scores on the general factor of psychopathology (Caspi et al., 2014; Lahey et al., 2012; Waldman et al., in press). These findings are consistent with the results of many studies that suggest that child abuse and neglect are related nonspecifically to future psychopathology (McLaughlin, 2016). In considering such findings on measured variables thought to reflect environmental influences, however, it is important to keep in mind that they could reflect gene-environment correlations instead of causal environmental influences (D’Onofrio, Lahey, Turkheimer, & Lichtenstein, 2013; McAdams, Gregory, & Eley, 2013; Plomin et al., 1977; Power et al., 2013). Therefore, much remains to be learned about environmental risks for psychopathology from studies using designs that support strong causal inferences (D’Onofrio, Lahey, Turkheimer, & Lichtenstein, 2013; Jaffee et al., 2012). One informative strategy would be to use multivariate biometric analyses of twin data to determine if observed correlations of phenotypic general, internalizing, and externalizing dimensions with putative environmental risk variables are due to genetic or environmental influences shared with the phenotypic dimensions (Neale & Cardon, 1992). In addition studies are needed that can address both gene-environment correlation and interaction (Plomin et al., 1977; Rutter, 2007a; Tarantino et al., 2014; Zheng, Van Hulle, & Rathouz, 2015).
Implications for the Study of Psychobiological Mechanisms
A key implication of the present hierarchical causal taxonomy is that each first-order dimension of psychopathology does not have its own unique pathophysiology. Dimensions of psychopathology are too highly correlated and there is too much sharing of etiologic processes at multiple levels not to hypothesize that variations in some neurobiological systems nonspecifically underlie multiple dimensions of psychopathology (Buckholtz & Meyer-Lindenberg, 2012). Thus, we expect individual differences in some neural networks to be related to all dimensions of psychopathology, other neural networks to be related to all internalizing dimensions, and others to be related to all externalizing dimensions. That is, consistent with the NIMH RDoC initiative (Cuthbert & Kozak, 2013), the current causal taxonomy asserts that the functioning of some number of transdimensional psychobiological systems aligned with these three levels of the causal taxonomy will be found to underlie multiple first-order dimensions of psychopathology. In contrast, it also is important to consider that each first- or higher-order factor of psychopathology—general, internalizing, and externalizing—may be related to individual differences in multiple psychobiological systems. For example, there is evidence that the general factor of psychopathology is likely related to the psychobiological systems that underlie both negative emotionality (Caspi et al., 2014; Tackett et al., 2013) and aspects of cognitive ability (Caspi et al., 2014; Lahey et al., 2015). In some cases, psychobiological systems may be related to fine-grain subsets of the larger set of symptoms that define a first-order dimension of psychopathology. In other cases, they may be related to fine-grain subsets of symptoms that are part of the definition of multiple first-order dimensions in the same higher-order domain (see Table 1) (Buckholtz & Meyer-Lindenberg, 2012). Therefore, if research on psychobiological models is to move forward it will require specific hypotheses regarding the level of the hierarchical taxonomy at which each mechanism plays a role.
Detecting associations between neural features and higher-order dimensions of symptoms should be straightforward. The focus of most studies on the neural correlates of categorical diagnoses rather than higher-order domains of psychopathology has often precluded the ability to look for neural correlates at different levels of hierarchical taxonomy, however. Nonetheless, three emerging lines of existing research suggest that at least some psychobiological variables are related to higher-order factors:
1. Psychophysiological research
A recent review of “fear”-potentiated startle (in which viewing a negatively-valenced scene enhances startle responses) provides an example of possible relations of psychophysiological measures to higher-order dimensions of psychopathology (Vaidyanathan, Nelson, & Patrick, 2012). Fear potentiated startle was found to be enhanced in individuals who are high on the higher-order fears factor, even though persons with specific phobias exhibited greater fear-potentiated startle than persons with social anxiety disorder or panic disorder (Vaidyanathan, Nelson, et al., 2012). This suggests that the biological mechanisms underlying startle may be expressed at the level of the higher-order fears dimension level, on which specific phobia has a strong loading (Lahey et al., 2012).
Similarly, analyses of P3 evoked response potentials (ERPs) indicate that reduced amplitude and phase locking of P3 waveforms during oddball tasks are common to all externalizing disorders (Burwell, Malone, Bernat, & Iacono, 2014; Iacono, Carlson, Malone, & McGue, 2002). Biometric analyses further indicates that genetic influences contribute to the correlation between externalizing symptoms and the P3 (Hicks et al., 2007). It is not yet clear that P3 is specific to externalizing disorders as opposed to psychopathology in general, however. There is also evidence that more peripheral indices of parasympathetic autonomic control are related to the hierarchy of psychopathology dimensions. In particular, low levels of tonic high-frequency heart rate variability (HF-HRV), and the reactive decline in HF-HRV in response to challenge, appear to be related to both internalizing and externalizing psychopathology (Beauchaine & Thayer, 2015). This suggests that HF-HRV, which is often interpreted as reflecting deficient emotional regulation, may be nonspecifically associated with all dimensions of psychopathology through the general factor.
2. MRI studies of brain structure
To date, most studies of the psychobiological correlates of psychopathology have only examined a single diagnosis, but recent neuroimaging studies have examined brain correlates of higher-order internalizing (Jensen et al., 2015) and externalizing (Ameis et al., 2014) dimensions of psychopathology. Furthermore, a meta-analysis of differences in brain structure assessed with voxel-based morphometry was conducted using data from 193 studies of over 15,000 persons (Goodkind et al., 2015). This revealed that gray matter reductions in several brain regions, particularly the anterior cingulate and bilateral insula, were nonspecifically related to diagnoses of schizophrenia, affective disorders, substance use disorders, and anxiety disorders. In contrast, gray matter differences in only a few regions distinguished one disorder from another. Although these findings do not reveal if the structural differences are the cause, consequence, or some other correlate of psychopathology, they suggest the important possibility that at least some structural abnormalities are related to the general factor of psychopathology in a manner that is consistent with the present causal taxonomy.
3. Functional MRI research
A series of studies suggest that it may be revealing to test associations of data from functional MRI paradigms to higher-order dimensions of psychopathology. Castellanos-Ryan and colleagues (Castellanos-Ryan et al., 2014) examined whether a latent externalizing factor was related to functional MRI responses on tasks related to inhibition and to reward in a large sample of adolescents. Scores on the latent externalizing factor showed associations with differential responses during a stop-signal task in a network of regions including the substantia nigra, subthalamic nucleus, and pre-supplemental motor area. By contrast, other associations, such as reduced frontal activations were more specifically linked to ADHD and CD symptoms, while individuals with substance misuse showed lowered responses in the left inferior frontal gyrus during reward anticipation on a monetary incentive delay task. In addition, one study has found an association between higher-order externalizing psychopathology and variation in intrinsic connectivity networks (Abram et al., 2015). A meta-analysis provides an elegant example of cross-disorder convergence among specific phobia, social anxiety disorder, and PTSD (Etkin & Wager, 2007). Examining activations during fear conditioning paradigms across studies, common hyperactivation was found in all three internalizing diagnostic groups relative to healthy controls in both the amygdala and insula bilaterally. Some evidence of disorder-specific effects also was observed, with portions of the cingulate showing hypoactivation in persons with PTSD, but not the other groups.
These studies suggest that it will be possible to identify transdiagnostic structural and functional individual differences in psychobiological processes. There also is evidence that these may be linked to dispositional dimensions, such as negative emotionality and positive emotionality. For example, variations in the neural systems that support negative emotionality should be related to all first-order dimensions through the general factor of psychopathology, whereas neural systems underlying positive emotionality may be specifically related inversely to MDD (Carl, Soskin, Kerns, & Barlow, 2013). The finding of associations of many different forms of psychopathology with both structural and/or functional abnormalities in the bilateral insula, amygdala, and anterior cingulate (Etkin & Wager, 2007; Goodkind et al., 2015) is striking given: 1) the importance of these brain regions in individual differences in negative emotionality (Eisenberger, Lieberman, & Satpute, 2005; Feinstein, Stein, & Paulus, 2006; Haas, Omura, Constable, & Canli, 2007; Kumari, Das, Wilson, Goswami, & Sharma, 2007; Paulus, Rogalsky, Simmons, Feinstein, & Stein, 2003; Stein, Simmons, Feinstein, & Paulus, 2007), and 2) our hypothesis that the disposition of negative emotionality is closely linked to the general factor of psychopathology. Thus, these regions appear to be prime candidates for a role in the general psychopathology factor.
IMPLICATIONS FOR RESEARCH ON CLINICAL INTERVENTIONS
The full clinical implications of the proposed causal taxonomy of psychopathology will need to be worked out after the model has been thoroughly tested. Some obvious implications of the model and some key hypotheses can be discussed at this point, however. One immediate implication is the value of broadly assessing a wide range of symptoms of psychopathology. There are many reasons not to examine only the “presenting complaint,” of course, not the least of which is the importance of not missing salient symptoms. The current taxonomy further implies that children with higher overall numbers of symptoms may be at greater risk for continuing difficulties. Indeed, the results of a longitudinal study of adults in NESARC suggested that the general factor of psychopathology predicted future functioning over and above predictions based on higher-order externalizing, distress, and fears disorders (Lahey et al., 2012).
Furthermore, there is considerable evidence of nonspecific effects of some interventions. It is well known that some pharmacologic agents labeled antidepressants also are effective in treating some forms of anxiety (Barlow et al., 2004). In addition, proponents of the unified approach to treatment have hypothesized that treatments designed to impact transdiagnostic processes, such as negative emotionality that underlie multiple mental disorders, may effectively reduce symptoms of multiple forms of psychopathology (Barlow et al., 2004; Barlow, Sauer-Zavala, et al., 2014; Nolen-Hoeksema & Watkins, 2011). It also has long been observed, for example, that effective treatments focused on a specific anxiety disorder also produce collateral improvements in both co-occurring anxiety disorders and depression (Barlow et al., 2004). Based on such observations, a unified treatment protocol for emotional disorders designed to reduce negative emotionality was found to reduce a wide range of anxiety and depression problems in a controlled trial (Bullis, Fortune, Farchione, & Barlow, 2014; Farchione et al., 2012).
CONCLUSIONS
We reviewed evidence on patterns of correlations among first-order dimensions and on the sharing of causal influences to propose a causal taxonomy of prevalent forms of psychopathology across the lifespan. We proposed a taxonomy in which phenotypic correlations among diverse forms of psychopathology reflect a hierarchy of pleiotropic etiologic influences. Some etiologic factors are hypothesized to nonspecifically increase risk for all common first-order dimensions of psychopathology to varying degrees. Other pleiotropic etiologic factors are hypothesized to nonspecifically increase risk only for all dimensions within one more specific higher-order domain. Our review indicates that pleiotropic etiologic influences are largely familial, including both genetic and shared environmental influences common to family members. In contrast, environmental influences unique to each family member tend to be more dimension-specific and thereby serve to differentiate dimensions from one another. In addition, there are dimension-specific genetic influences that serve to differentiate first-order dimensions of psychopathology.
The present causal taxonomy implies that a broad range of dimensions of psychopathology previously thought to be distinct in their natures actually have at least partly shared etiologies and neurobiological mechanisms. This implication is particularly important because it could change how the origins and nature of apparently diverse forms of psychopathology are conceptualized and studied. If this view is supported in future studies, more will be learned by studying the etiologies and mechanisms common to multiple forms of psychopathology simultaneously than by only studying the etiology of one mental disorder at a time. This can be accomplished far better in representative samples that are large enough to include sufficient variation in all dimensions of psychopathology (or that are selected through oversampling on risk for the full range of psychopathology) than in clinical case-control samples, which bias correlations among first-order dimensions of psychopathology.
These hypotheses do not mean that all dimensions of psychopathology are influenced by the same genetic and environmental influences. Indeed, each dimension of psychopathology is distinguishable because it has some dimension-specific etiologic influences. Moreover, there is considerable variation in the degree to which the shared etiologic influences at different levels of the hierarchy influence each dimension of psychopathology, which also differentiates first-order dimensions. Thus, although simultaneously studying the etiology of the full range of common dimensions of psychopathology is the surest way to identify both shared and unique etiologic influences, each specific dimension (or perhaps even fine-grain subsets of symptoms) will require a somewhat different focus at different levels of the hierarchical causal taxonomy. The degree of emphasis at each level of the hierarchy for each form of psychopathology can be derived from the causal taxonomy to guide research.
Limitations and Future Directions
An important goal for future research is to determine the extent to which different symptoms and dimensions share causal influences due to pleiotropy (a single cause directly influences dimensions A and B) versus causal chains (e.g., a cause influences dimension A, which increases the likelihood of dimension B) (Bornstein, Hahn, & Wolke, 2013; Borsboom & Cramer, 2013). Both mechanisms of shared causal influences are equally important to the causal taxonomy and both imply that reducing the initial causal influence would reduce both dimensions of psychopathology. Nonetheless, these two mechanisms of shared causes have different implications for the development and application of more specific causal models and interventions. For example, in the latter case, it may be possible to treat dimension A to prevent dimension B, but this would not be true in the case of causal influences shared through pleiotropy.
We advanced 12 hypotheses that constitute a causal taxonomy (Table 3). These include the hypothesis that more serious forms of psychopathology (i.e., autism, mania, and schizophrenia) share a large proportion of their causal influences with the general factor of psychopathology. As noted in the introduction, the present review and taxonomy did not adequately address personality disorders, however. Further elucidation of the joint phenotypic and causal structure of the full range of dimensions of psychopathology, including personality disorders, is a high priority for fully understanding the causal taxonomy of maladaptive behavior. In particular, it is important to determine the degree to which the general factor identified in a recent study of personality disorder symptoms (Sharp et al., 2015) is related to the general factor of psychopathology in ‘Axis I’ dimensions of psychopathology.
Nearly all of the evidence on the shared causes of psychopathology reviewed in this paper has come from twin and other family studies. Although such evidence is powerful, and is consistent with the results of the smaller literature on molecular genetics, future studies should include direct measures of both environments and molecular genetic variants as rapidly as improving technologies and knowledge permit. Another powerful approach that is needed in the near future is the use of neuroimaging to test the hypotheses of the causal taxonomy regarding general and specific relations between neurobiological mechanisms and psychopathology. Such studies would almost certainly benefit from the inclusion of a transdimensional dispositional approach. Together, the results of such future studies should provide the empirical basis for moving from a causal taxonomy to more specific causal models of psychopathology.
Our goal in proposing this causal taxonomy is not to state conclusions, but to stimulate attempts to refute the present hypotheses with data (Popper, 1963). If this causal taxonomy, or a stronger alternative that emerges from tests of its hypotheses, is supported, the new taxonomy would have very important implications for understanding the nature of psychopathology. In turn, this knowledge can be expected to improve research, prevention, and treatment of psychopathology. In order to advance research on treatment and prevention, it will be necessary to move from a causal taxonomy to more detailed causal models. One particular need will be to include hypotheses in those models regarding the causal factors that foster homotypic and heterotypic continuity over time—i.e., persistence and lead to worsening or improvement in symptoms over time—as these are prime targets for interventions.
Supplementary Material
Acknowledgments
This paper was supported in part by grant R01-MH098098 from the National Institute of Mental Health. We greatly appreciate the helpful comments of Quetzal A. Class and Uma Vaidyanathan on earlier drafts of this manuscript.
Footnotes
We use the term pleiotropy broadly in this paper to refer to genetic and environmental factors that nonspecifically influence more than one dimension of psychopathology.
Bandura specifically acknowledged that the judgement of maladaptiveness is a social construction that carries inherent risks of misapplication that must be assiduously guarded against.
Alternatively, factor scores estimated in SEM could be exported for association tests in specialized statistical software, but the exported factor scores would no longer have the measurement properties of latent factors.
Contributor Information
Benjamin B. Lahey, University of Chicago
Robert F. Krueger, University of Minnesota
Paul J. Rathouz, University of Wisconsin School of Medicine and Public Health
Irwin D. Waldman, Emory University
David H. Zald, Vanderbilt University
References
- Abikoff H, Courtney M, Pelham WE, Koplewicz HS. Teachers ratings of disruptive behaviors: The influence of halo effects. Journal of Abnormal Child Psychology. 1993;21:519–533. doi: 10.1007/BF00916317. [DOI] [PubMed] [Google Scholar]
- Abram SV, Wisner KM, Grazioplene RG, Krueger RF, MacDonald AW, III, DeYoung CG. Functional coherence of insula networks is associated with externalizing behavior. Journal of Abnormal Psychology. 2015;124:1079–1091. doi: 10.1037/abn0000078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Achenbach TM. The Child Behavior Profile: I. Boys aged 6–11. Journal of Consulting and Clinical Psychology. 1978;46:478–488. doi: 10.1037//0022-006x.46.3.478. [DOI] [PubMed] [Google Scholar]
- Achenbach TM. Multicultural evidence-based assessment of child and adolescent psychopathology. Transcultural Psychiatry. 2010;47:707–726. doi: 10.1177/1363461510382590. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, Becker A, Dopfner M, Heiervang E, Roessner V, Steinhausen HC, Rothenberger A. Multicultural assessment of child and adolescent psychopathology with ASEBA and SDQ instruments: research findings, applications, and future directions. Journal of Child Psychology and Psychiatry. 2008;49:251–275. doi: 10.1111/j.1469-7610.2007.01867.x. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, Conners CK, Quay HC, Verhulst FC, Howell CT. Replication of empirically derived syndromes as a basis for taxonomy of child and adolescent psychopathology. Journal of Abnormal Child Psychology. 1989;17:299–323. doi: 10.1007/BF00917401. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, Edelbrock CS. Classification of child psychopathology: Review and analysis of empirical efforts. Psychological Bulletin. 1978;85:1275–1301. [PubMed] [Google Scholar]
- Ahola K, Virtanen M, Honkonen T, Isometsa E, Aromaa A, Lonnqvist J. Common mental disorders and subsequent work disability: A population-based Health 2000 Study. Journal of Affective Disorders. 2011;134:365–372. doi: 10.1016/j.jad.2011.05.028. [DOI] [PubMed] [Google Scholar]
- Al-Hamzawi AO, Rosellini AJ, Lindberg M, Petukhova M, Kessler RC, Bruffaerts R. The role of common mental and physical disorders in days out of role in the Iraqi general population: Results from the WHO World Mental Health Surveys. Journal of Psychiatric Research. 2014;53:23–29. doi: 10.1016/j.jpsychires.2014.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, … Vollebergh WAM. 12-Month comorbidity patterns and associated factors in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatrica Scandinavica. 2004a;109:28–37. doi: 10.1111/j.1600-0047.2004.00328.x. [DOI] [PubMed] [Google Scholar]
- Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, … Vollebergh WAM. Disability and quality of life impact of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatrica Scandinavica. 2004b;109:38–46. doi: 10.1111/j.1600-0047.2004.00329.x. [DOI] [PubMed] [Google Scholar]
- Ameis SH, Ducharme S, Albaugh MD, Hudziak JJ, Botteron KN, Lepage C, … Karama S. Cortical thickness, cortico-amygdalar networks, and externalizing behaviors in healthy children. Biological Psychiatry. 2014;75:65–72. doi: 10.1016/j.biopsych.2013.06.008. [DOI] [PubMed] [Google Scholar]
- Anderson JC, Williams S, McGee R, Silva PA. DSM-III disorders in preadolescent children: Prevalence in a large sample from the general population. Archives of General Psychiatry. 1987;44:69–76. doi: 10.1001/archpsyc.1987.01800130081010. [DOI] [PubMed] [Google Scholar]
- Andrews G, Henderson S, Hall W. Prevalence, comorbidity, disability and service utilisation: Overview of the Australian National Mental Health Survey. British Journal of Psychiatry. 2001;178:145–153. doi: 10.1192/bjp.178.2.145. [DOI] [PubMed] [Google Scholar]
- Andrews G, Slade T, Issakidis C. Deconstructing current comorbidity: Data from the Australian National Survey of Mental Health and Well-Being. British Journal of Psychiatry. 2002;181:306–314. doi: 10.1192/bjp.181.4.306. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ. Puberty and depression. Child and Adolescent Psychiatric Clinics of North America. 2006;15:919–937. doi: 10.1016/j.chc.2006.05.013. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ. Nosology and measurement in child and adolescent psychiatry. Journal of Child Psychology and Psychiatry. 2009;50:9–15. doi: 10.1111/j.1469-7610.2008.01981.x. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1999;40:57–87. [PubMed] [Google Scholar]
- Angold A, Erkanli A, Silberg J, Eaves L, Costello EJ. Depression scale scores in 8–17-year-olds: effects of age and gender. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2002;43:1052–1063. doi: 10.1111/1469-7610.00232. [DOI] [PubMed] [Google Scholar]
- Arcos-Burgos M, Velez JI, Solomon BD, Muenke M. A common genetic network underlies substance use disorders and disruptive or externalizing disorders. Human Genetics. 2012;131:917–929. doi: 10.1007/s00439-012-1164-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker JH, Maes HH, Larsson H, Lichtenstein P, Kendler KS. Sex differences and developmental stability in genetic and environmental influences on psychoactive substance consumption from early adolescence to young adulthood. Psychological Medicine. 2011;41:1907–1916. doi: 10.1017/S003329171000259X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball SG, Otto MW, Pollack MH, Rosenbaum JF. Predicting prospective episodes of depression in patients with panic disorder: A longitudinal study. Journal of Consulting and Clinical Psychology. 1994;62:359–365. doi: 10.1037//0022-006x.62.2.359. [DOI] [PubMed] [Google Scholar]
- Bandura A. Principles of behavior modification. New York: Holt, Rinehart & Winston; 1969. [Google Scholar]
- Barkley RA, Fischer M, Edelbrock CS, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria, 1: An 8-year prospective follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry. 1990;29:546–557. doi: 10.1097/00004583-199007000-00007. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behavior Therapy. 2004;35:205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Ellard KK, Sauer-Zavala S, Bullis JR, Carl JR. The origins of neuroticism. Perspectives on Psychological Science. 2014;9:481–496. doi: 10.1177/1745691614544528. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Sauer-Zavala S, Carl JR, Bullis JR, Ellard KK. The nature, diagnosis, and treatment of neuroticism: Back to the future. Clinical Psychological Science. 2014;2:344–365. [Google Scholar]
- Bauermeister JJ, Canino G, Polanczyk G, Rohde LA. ADHD across cultures: Is there evidence for a bidimensional organization of symptoms? Journal of Clinical Child and Adolescent Psychology. 2010;39:362–372. doi: 10.1080/15374411003691743. [DOI] [PubMed] [Google Scholar]
- Beard JR, Dietrich UC, Brooks LO, Brooks RT, Heathcote K, Kelly B. Incidence and outcomes of mental disorders in a regional population: The Northern Rivers Mental Health Study. Australian and New Zealand Journal of Psychiatry. 2006;40:674–682. doi: 10.1080/j.1440-1614.2006.01867.x. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, McNulty T. Comorbidities and continuities as ontogenic processes: Toward a developmental spectrum model of externalizing psychopathology. Development and Psychopathology. 2013;25:1505–1528. doi: 10.1017/S0954579413000746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, Thayer JF. Heart rate variability as a transdiagnostic biomarker of psychopathology. International Journal of Psychophysiology. 2015;98:338–350. doi: 10.1016/j.ijpsycho.2015.08.004. [DOI] [PubMed] [Google Scholar]
- Beesdo-Baum K, Knappe S, Asselmann E, Zimmermann P, Brueckl T, Hoefler M, … Wittchen H-U. The ‘Early Developmental Stages of Psychopathology (EDSP) study’: a 20-year review of methods and findings. Social Psychiatry and Psychiatric Epidemiology. 2015;50(6):851–866. doi: 10.1007/s00127-015-1062-x. [DOI] [PubMed] [Google Scholar]
- Beesdo K, Bittner A, Pine DS, Stein MB, Hofler M, Lieb R, Wittchen HU. Incidence of social anxiety disorder and the consistent risk for secondary depression in the first three decades of life. Archives of General Psychiatry. 2007;64:903–912. doi: 10.1001/archpsyc.64.8.903. [DOI] [PubMed] [Google Scholar]
- Beiser M, Dion R, Gotowiec A. The structure of attention-deficit and hyperactivity symptoms among Native and non-Native elementary school children. Journal of Abnormal Child Psychology. 2000;28:425–437. doi: 10.1023/a:1005179521820. [DOI] [PubMed] [Google Scholar]
- Bergen SE, Gardner CO, Kendler KS. Age-related changes in heritability of behavioral phenotypes over adolescence and young adulthood: A meta-analysis. Twin Research and Human Genetics. 2007;10:423–433. doi: 10.1375/twin.10.3.423. [DOI] [PubMed] [Google Scholar]
- Bergen SE, O’Dushlaine CT, Ripke S, Lee PH, Ruderfer DM, Akterin S, … Sullivan PF. Genome-wide association study in a Swedish population yields support for greater CNV and MHC involvement in schizophrenia compared with bipolar disorder. Molecular Psychiatry. 2012;17:880–886. doi: 10.1038/mp.2012.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkson J. Limitations of the application of fourfold table analysis to hospital data. Biometrics Bulletin. 1946;2:47–53. [PubMed] [Google Scholar]
- Berletch JB, Yang F, Xu J, Carrel L, Disteche CM. Genes that escape from X inactivation. Human Genetics. 2011;130:237–245. doi: 10.1007/s00439-011-1011-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bezdjian S, Krueger RF, Derringer J, Malone S, McGue M, Iacono WG. The structure of DSM-IV ADHD, ODD, and CD criteria in adolescent boys: A hierarchical approach. Psychiatry Research. 2011;188:411–421. doi: 10.1016/j.psychres.2011.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bijl RV, Ravelli A. Current and residual functional disability associated with psychopathology: findings from the Netherlands Mental Health Survey and Incidence Study (NEMESIS) Psychological Medicine. 2000;30:657–668. doi: 10.1017/s0033291799001841. [DOI] [PubMed] [Google Scholar]
- Bijl RV, Ravelli A, van Zessen G. Prevalence of psychiatric disorder in the general population: Results of the Netherlands Mental Health Survey and Incidence Study (NEMESIS) Social Psychiatry and Psychiatric Epidemiology. 1998;33:587–595. doi: 10.1007/s001270050098. [DOI] [PubMed] [Google Scholar]
- Bittner A, Egger HL, Erkanli A, Costello EJ, Foley DL, Angold A. What do childhood anxiety disorders predict? Journal of Child Psychology and Psychiatry. 2007;48:1174–1183. doi: 10.1111/j.1469-7610.2007.01812.x. [DOI] [PubMed] [Google Scholar]
- Bittner A, Goodwin RD, Wittchen HU, Beesdo K, Hofler M, Lieb R. What characteristics of primary anxiety disorders predict subsequent major depressive disorder? Journal of Clinical Psychiatry. 2004;65:618–626. doi: 10.4088/jcp.v65n0505. [DOI] [PubMed] [Google Scholar]
- Blanco C, Wall MM, He JP, Krueger RF, Olfson M, Jin CJ, … Merikangas KR. The space of common psychiatric disorders in adolescents: Comorbidity structure and individual latent liabilities. Journal of the American Academy of Child and Adolescent Psychiatry. 2015;54:45–52. doi: 10.1016/j.jaac.2014.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornstein MH, Hahn CS, Wolke D. Systems and cascades in cognitive development and academic achievement. Child Development. 2013;84:154–162. doi: 10.1111/j.1467-8624.2012.01849.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D, Cramer AOJ. Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- Boyd JH, Burke JD, Gruenberg E, Holzer CE, Rae DS, George LK, … Nestadt G. Exclusion criteria of DSM-III: A study of co-occurrence of hierarchy-free syndromes. Archives of General Psychiatry. 1984;41:983–989. doi: 10.1001/archpsyc.1984.01790210065008. [DOI] [PubMed] [Google Scholar]
- Briere FN, Rohde P, Seeley JR, Klein D, Lewinsohn PM. Comorbidity between major depression and alcohol use disorder from adolescence to adulthood. Comprehensive Psychiatry. 2014;55:526–533. doi: 10.1016/j.comppsych.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broeren S, Muris P, Diamantopoulou S, Baker JR. The course of childhood anxiety symptoms: Developmental trajectories and child-related factors in normal children. Journal of Abnormal Child Psychology. 2013;41:81–95. doi: 10.1007/s10802-012-9669-9. [DOI] [PubMed] [Google Scholar]
- Broman-Fulks JJ, Ruggiero KJ, Green BA, Kilpatrick DG, Danielson CK, Resnick HS, Saunders BE. Taxometric investigation of PTSD: Data from two nationally representative samples. Behavior Therapy. 2006;37:364–380. doi: 10.1016/j.beth.2006.02.006. [DOI] [PubMed] [Google Scholar]
- Brooker RJ, Buss KA, Lemery-Chalfant K, Aksan N, Davidson RJ, Goldsmith HH. The development of stranger fear in infancy and toddlerhood: Normative development, individual differences, antecedents, and outcomes. Developmental Science. 2013;16:864–878. doi: 10.1111/desc.12058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LA, Krull JL, Roy-Byrne P, Sherbourne CD, Stein MB, Sullivan G, … Craske MG. An examination of the bidirectional relationship between functioning and symptom levels in patients with anxiety disorders in the CALM study. Psychological Medicine. 2015;45:647–661. doi: 10.1017/S0033291714002062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA. Confirmatory factor analysis for applied research. New York: Guilford; 2006. [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- Bruckl TM, Wittchen HU, Hofler M, Pfister H, Schneider S, Lieb R. Childhood separation anxiety and the risk of subsequent psychopathology: Results from a community study. Psychotherapy and Psychosomatics. 2007;76:47–56. doi: 10.1159/000096364. [DOI] [PubMed] [Google Scholar]
- Bruffaerts R, Vilagut G, Demyttenaere K, Alonso J, AlHamzawi A, Andrade LH, … Kessler RC. Role of common mental and physical disorders in partial disability around the world. British Journal of Psychiatry. 2012;200:454–461. doi: 10.1192/bjp.bp.111.097519. 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckholtz JW, Meyer-Lindenberg A. Psychopathology and the human connectome: Toward a transdiagnostic model of risk for mental illness. Neuron. 2012;74:990–1004. doi: 10.1016/j.neuron.2012.06.002. [DOI] [PubMed] [Google Scholar]
- Bufferd SJ, Dougherty LR, Carlson GA, Rose S, Klein DN. Psychiatric disorders in preschoolers: Continuity from ages 3 to 6. American Journal of Psychiatry. 2012;169:1157–1164. doi: 10.1176/appi.ajp.2012.12020268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bullis JR, Fortune MR, Farchione TJ, Barlow DH. A preliminary investigation of the long-term outcome of the Unified Protocol for Transdiagnostic Treatment of Emotional Disorders. Comprehensive Psychiatry. 2014;55:1920–1927. doi: 10.1016/j.comppsych.2014.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke JD, Loeber R. Oppositional defiant disorder and the explanation of the comorbidity between behavioral disorders and depression. Clinical Psychology: Science and Practice. 2010;17:319–326. [Google Scholar]
- Burke JD, Loeber R, Lahey BB, Rathouz PJ. Developmental transitions among affective and behavioral disorders in adolescent boys. Journal of Child Psychology and Psychiatry. 2005;46:1200–1210. doi: 10.1111/j.1469-7610.2005.00422.x. [DOI] [PubMed] [Google Scholar]
- Burke JD, Waldman I, Lahey BB. Predictive validity of childhood oppositional defiant disorder and conduct disorder: Implications for the DSM-V. Journal of Abnormal Psychology. 2010;119:739–751. doi: 10.1037/a0019708. [DOI] [PubMed] [Google Scholar]
- Burns GL, Boe B, Walsh JA, Sommers-Flanagan R, Teegarden LA. A confirmatory factor analysis on the DSM-IV ADHD and ODD symptoms: What is the best model for the organization of these symptoms? Journal of Abnormal Child Psychology. 2001;29:339–349. doi: 10.1023/a:1010314030025. [DOI] [PubMed] [Google Scholar]
- Burns GL, Walsh JA, Owen SM, Snell J. Internal validity of attention deficit hyperactivity disorder, oppositional defiant disorder, and overt conduct disorder symptoms in young children: Implications from teacher ratings for a dimensional approach to symptom validity. Journal of Clinical Child Psychology. 1997;26:266–275. doi: 10.1207/s15374424jccp2603_5. [DOI] [PubMed] [Google Scholar]
- Burt SA. Research Review: The shared environment as a key source of variability in child and adolescent psychopathology. Journal of Child Psychology and Psychiatry. 2014;55:304–312. doi: 10.1111/jcpp.12173. [DOI] [PubMed] [Google Scholar]
- Burwell SJ, Malone SM, Bernat EM, Iacono WG. Does electroencephalogram phase variability account for reduced P3 brain potential in externalizing disorders? Clinical Neurophysiology. 2014:2007–2015. doi: 10.1016/j.clinph.2014.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bussing R, Mason DM, Bell L, Porter P, Garvan C. Adolescent outcomes of childhood attention-deficit/hyperactivity disorder in a diverse community sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:595–605. doi: 10.1016/j.jaac.2010.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell DT, Fiske DW. Convergent and discriminant validation by the multitrait-multimethod matrix. Psychological Bulletin. 1959;56:81–105. [PubMed] [Google Scholar]
- Capaldi DM. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys.2: A 2-year follow-up at grade 8. Development and Psychopathology. 1992;4:125–144. doi: 10.1017/s0954579499001959. [DOI] [PubMed] [Google Scholar]
- Carey G, DiLalla DL. Personality and psychopathology: Genetic perspectives. Journal of Abnormal Psychology. 1994;103:32–43. doi: 10.1037//0021-843x.103.1.32. [DOI] [PubMed] [Google Scholar]
- Carl JR, Soskin DP, Kerns C, Barlow DH. Positive emotion regulation in emotional disorders: A theoretical review. Clinical Psychology Review. 2013;33:343–360. doi: 10.1016/j.cpr.2013.01.003. [DOI] [PubMed] [Google Scholar]
- Caron C, Rutter M. Comorbidity in child psychopathology: Concepts, issues and research strategies. Journal of Child Psychology and Psychiatry. 1991;32:1063–1080. doi: 10.1111/j.1469-7610.1991.tb00350.x. [DOI] [PubMed] [Google Scholar]
- Carragher N, Teesson M, Sunderland NC, Newton NC, Krueger RF, Conrod PJ, … Slade T. The structure of adolescent psychopathology: A symptom-level analysis. Psychological Medicine. 2016;46:981–994. doi: 10.1017/S0033291715002470. [DOI] [PubMed] [Google Scholar]
- Carver CS. Impulse and constraint: Perspectives from personality psychology, convergence with theory in other areas, and potential for integration. Personality and Social Psychology Review. 2005;9:312–333. doi: 10.1207/s15327957pspr0904_2. [DOI] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, … Moffitt TE. The p factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science. 2014;2:119–137. doi: 10.1177/2167702613497473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellanos-Ryan N, Struve M, Whelan R, Banaschewski T, Barker GJ, Bokde ALW … Consortium I. Neural and cognitive correlates of the common and specific variance across externalizing problems in young adolescence. American Journal of Psychiatry. 2014;171:1310–1319. doi: 10.1176/appi.ajp.2014.13111499. [DOI] [PubMed] [Google Scholar]
- Cattell RB, Bjersted A, Schmidt LR. Clinical diagnosis by objective-analytic personality batteries. Journal of Clinical Psychology. 1972;28:239–312. doi: 10.1002/1097-4679(197207)28:3+<239::aid-jclp2270280302>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Moffitt CE, Gray J. Psychometric properties of the revised child anxiety and depression scale in a clinical sample. Behaviour Research and Therapy. 2005;43:309–322. doi: 10.1016/j.brat.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, Francis SE. Assessment of symptoms of DSM-IV anxiety and depression in children: a revised child anxiety and depression scale. Behaviour Research and Therapy. 2000;38:835–855. doi: 10.1016/s0005-7967(99)00130-8. [DOI] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Molina BSG, Pelham WE, Applegate B, Dahlke A, Overmyer M, Lahey BB. Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Archives of General Psychiatry. 2010;67:1044–1051. doi: 10.1001/archgenpsychiatry.2010.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Cohen DJ, editors. Developmental psychopathology. 2. New York: Wiley; 2006. [Google Scholar]
- Clark LA, Watson D, Mineka S. Temperament, personality, and the mood and anxiety disorders. Journal of Abnormal Psychology. 1994;103:103–116. [PubMed] [Google Scholar]
- Clark LA, Watson D, Reynolds S. Diagnosis and classification of psychopathology: Challenges to the current system and future directions. Annual Review of Psychology. 1995;46:121–153. doi: 10.1146/annurev.ps.46.020195.001005. [DOI] [PubMed] [Google Scholar]
- Comer JS, Blanco C, Hasin DS, Liu SM, Grant BF, Turner JB, Olfson M. Health-related quality of life across the anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Journal of Clinical Psychiatry. 2011;72:43–50. doi: 10.4088/JCP.09m05094blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conner KR, Bohnert AS, McCarthy JF, Valenstein M, Bossarte R, Ignacio R, … Ilgen MA. Mental disorder comorbidity and suicide among 2.96 million men receiving care in the Veterans Health Administration Health System. Journal of Abnormal Psychology. 2013;122:256–263. doi: 10.1037/a0030163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Adair CE, Smetanin P, Stiff D, Briante C, Colman I, … Angold A. Diagnostic transitions from childhood to adolescence to early adulthood. Journal of Child Psychology and Psychiatry. 2013;54:791–799. doi: 10.1111/jcpp.12062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Shanahan L, Costello EJ, Angold A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Archives of General Psychiatry. 2009;66:764–772. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland W, Shanahan L, Costello EJ, Angold A. Cumulative prevalence of psychiatric disorders by young adulthood: A prospective cohort analysis from the Great Smoky Mountains Study. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:252–261. doi: 10.1016/j.jaac.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosgrove VE, Rhee SH, Gelhorn HL, Boeldt D, Corley RC, Ehringer MA, … Hewitt JK. Structure and etiology of co-occurring internalizing and externalizing disorders in adolescents. Journal of Abnormal Child Psychology. 2011;39:109–123. doi: 10.1007/s10802-010-9444-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa PT, McCrae RR. NEO five-factor inventory. Lutz, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- Costello EJ, Copeland W, Angold A. Trends in psychopathology across the adolescent years: What changes when children become adolescents, and when adolescents become adults? Journal of Child Psychology and Psychiatry. 2011;52:1015–1025. doi: 10.1111/j.1469-7610.2011.02446.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Crick NR, Zahn-Waxler C. The development of psychopathology in females and males: Current progress and future challenges. Development and Psychopathology. 2003;15:719–742. [PubMed] [Google Scholar]
- Crome E, Baillie A, Slade T, Ruscio AM. Social phobia: Further evidence of dimensional structure. Australian and New Zealand Journal of Psychiatry. 2010;44:1012–1020. doi: 10.3109/00048674.2010.507544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cronbach LJ, Meehl PE. Construct validity in psychological tests. Psychological Bulletin. 1955;52:281–302. doi: 10.1037/h0040957. [DOI] [PubMed] [Google Scholar]
- Crump C, Sundquist K, Winkleby MA, Sundquist J. Mental disorders and risk of accidental death. British Journal of Psychiatry. 2013a;203:297–302. doi: 10.1192/bjp.bp.112.123992. [DOI] [PubMed] [Google Scholar]
- Crump C, Sundquist K, Winkleby MA, Sundquist J. Mental disorders and vulnerability to homicidal death: Swedish nationwide cohort study. Bmj-British Medical Journal. 2013b;346 doi: 10.1136/bmj.f557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: The seven pillars of RDoC. Bmc Medicine. 2013;11 doi: 10.1186/1741-7015-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuthbert BN, Kozak MJ. Constructing constructs for psychopathology: The NIMH research domain criteria. Journal of Abnormal Psychology. 2013;122:928–937. doi: 10.1037/a0034028. [DOI] [PubMed] [Google Scholar]
- D’Onofrio BM, Lahey BB, Turkheimer E, Lichtenstein P. Critical need for family-based, quasi-experimental designs in integrating genetic and social science research. American Journal of Public Health. 2013;103:46–55. doi: 10.2105/AJPH.2013.301252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Onofrio BM, Lahey BB, Turkheimer E, Lichtenstein P. The critical need for family-based, quasi-experimental research in integrating genetic and social science research. American Journal of Public Health. 2013;103:S46–S55. doi: 10.2105/AJPH.2013.301252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis LK, Yu DM, Keenan CL, Gamazon ER, Konkashbaev AI, Derks EM, … Scharf JM. Partitioning the heritability of Tourette syndrome and obsessive compulsive disorder reveals differences in genetic architecture. PLOS Genetics. 2013;9 doi: 10.1371/journal.pgen.1003864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Graaf R, Bijl RV, Smit F, Vollebergh WAM, Spijker J. Risk factors for 12-month comorbidity of mood, anxiety, and substance use disorders: Findings from the Netherlands Mental Health Survey and Incidence Study. American Journal of Psychiatry. 2002;159:620–629. doi: 10.1176/appi.ajp.159.4.620. [DOI] [PubMed] [Google Scholar]
- de Graaf R, Bijl RV, ten Have M, Beekman ATF, Vollebergh WAM. Rapid onset of comorbidity of common mental disorders: Findings from the Netherlands Mental Health Survey and Incidence Study (NEMESIS) Acta Psychiatrica Scandinavica. 2004;109:55–63. doi: 10.1046/j.0001-690x.2003.00222.x. [DOI] [PubMed] [Google Scholar]
- de Graaf R, Tuithof M, van Dorsselaer S, ten Have M. Comparing the effects on work performance of mental and physical disorders. Social Psychiatry and Psychiatric Epidemiology. 2012;47:1873–1883. doi: 10.1007/s00127-012-0496-7. [DOI] [PubMed] [Google Scholar]
- Dick DM. Identification of genes influencing a spectrum of externalizing psychopathology. Current Directions in Psychological Science. 2007;16:331–335. [Google Scholar]
- Dick DM, Aliev F, Wang JC, et al. Using dimensional models of externalizing psychopathology to aid in gene identification. Archives of General Psychiatry. 2008;65(3):310–318. doi: 10.1001/archpsyc.65.3.310. [DOI] [PubMed] [Google Scholar]
- Dick DM, Latendresse SJ, Lansford JE, Budde JP, Goate A, Dodge KA, … Bates JE. Role of GABRA2 in trajectories of externalizing behavior across development and evidence of moderation by parental monitoring. Archives of General Psychiatry. 2009;66:649–657. doi: 10.1001/archgenpsychiatry.2009.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dick DM, Viken RJ, Kaprio J, Pulkkinen L, Rose RJ. Understanding the covariation among childhood externalizing symptoms: Genetic and environmental influences on conduct disorder, attention deficit hyperactivity disorder, and oppositional defiant disorder symptoms. Journal of Abnormal Child Psychology. 2005;33:219–229. doi: 10.1007/s10802-005-1829-8. [DOI] [PubMed] [Google Scholar]
- Dolan CV, Boomsma DI. Optimal selection of sib pairs from random samples for linkage analysis of a QTL using the EDAC test. Behavior Genetics. 1998;28:197–206. doi: 10.1023/a:1021423214032. [DOI] [PubMed] [Google Scholar]
- DuPaul GJ, Anastopoulos AD, Power TJ, Reid R, Ikeda MJ, McGoey KE. Parent ratings of attention-deficit/hyperactivity disorder symptoms: Factor structure and normative data. Journal of Psychopathology and Behavioral Assessment. 1998;20:83–102. [Google Scholar]
- Eaton NR, Keyes KM, Krueger RF, Balsis S, Skodol AE, Markon KE, … Hasin DS. An invariant dimensional liability model of gender differences in mental disorder prevalence: Evidence from a national sample. Journal of Abnormal Psychology. 2012;121:282–288. doi: 10.1037/a0024780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Keyes KM, Krueger RF, Noordhof A, Skodol AE, Markon KE, … Hasin DS. Ethnicity and psychiatric comorbidity in a national sample: Evidence for latent comorbidity factor invariance and connections with disorder prevalence. Social Psychiatry and Psychiatric Epidemiology. 2013;48:701–710. doi: 10.1007/s00127-012-0595-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, Keyes KM, Skodol AE, Markon KE, Grant BF, Hasin DS. Borderline personality disorder co-morbidity: Relationship to the internalizing-externalizing structure of common mental disorders. Psychological Medicine. 2011;41:1041–1050. doi: 10.1017/S0033291710001662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, Markon KE, Keyes KM, Skodol AE, Wall M, … Grant BF. The structure and predictive validity of the internalizing disorders. Journal of Abnormal Psychology. 2013;122:86–92. doi: 10.1037/a0029598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaves LJ, Meyer J. Locating human quantitative trait loci: Guidelines for the selection of sibling pairs for genotyping. Behavior Genetics. 1994;24:443–455. doi: 10.1007/BF01076180. [DOI] [PubMed] [Google Scholar]
- Eisenberger NI, Lieberman MD, Satpute AB. Personality from a controlled processing perspective: An fMRI study of neuroticism, extraversion, and self-consciousness. Cognitive, Affective, and Behavioral Neuroscience. 2005;5:169–181. doi: 10.3758/cabn.5.2.169. [DOI] [PubMed] [Google Scholar]
- El-Gabalawy R, Tsai J, Harpaz-Rotem I, Hoff R, Sareen J, Pietrzak RH. Predominant typologies of psychopathology in the United States: A latent class analysis. Journal of Psychiatric Research. 2013;47:1649–1657. doi: 10.1016/j.jpsychires.2013.07.028. [DOI] [PubMed] [Google Scholar]
- Etkin A, Wager TD. Functional neuroimaging of anxiety: A meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. American Journal of Psychiatry. 2007;164:1476–1488. doi: 10.1176/appi.ajp.2007.07030504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenck HJ. Dimensions of personality. New York: Praeger; 1947. [Google Scholar]
- Eysenck SBG, White O, Eysenck HJ. Personality and mental illness. Psychological Reports. 1976;39:1011–1022. doi: 10.2466/pr0.1976.39.3.1011. [DOI] [PubMed] [Google Scholar]
- Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Thompson-Hollands J, Carl JR, … Barlow DH. Unified protocol for transdiagnostic treatment of emotional disorders: A randomized controlled trial. Behavior Therapy. 2012;43:666–678. doi: 10.1016/j.beth.2012.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feighner JP, Woodruff RA, Winokur G, Munoz R, Robins E, Guze SB. Diagnostic criteria for use in psyhiatric researh. Archives of General Psychiatry. 1972;26:57–63. doi: 10.1001/archpsyc.1972.01750190059011. [DOI] [PubMed] [Google Scholar]
- Feinstein JS, Stein MB, Paulus MP. Anterior insula reactivity during certain decisions is associated with neuroticism. Social Cognitive and Affective Neuroscience. 2006;1:136–142. doi: 10.1093/scan/nsl016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferdinand RF, Dieleman G, Ormel J, Verhulst FC. Homotypic versus heterotypic continuity of anxiety symptoms in young adolescents: Evidence for distinctions between DSM-IV subtypes. Journal of Abnormal Child Psychology. 2007;35:325–333. doi: 10.1007/s10802-006-9093-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ. Structural models of the comorbidity of internalizing disorders and substance use disorders in a longitudinal birth cohort. Social Psychiatry and Psychiatric Epidemiology. 2011;46:933–942. doi: 10.1007/s00127-010-0268-1. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood J. Predictive validity of categorically and dimensionally scored measures of disruptive childhood behaviors. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:477–485. [PubMed] [Google Scholar]
- Forbush KT, Watson D. The structure of common and uncommon mental disorders. Psychological Medicine. 2013;43:97–108. doi: 10.1017/S0033291712001092. [DOI] [PubMed] [Google Scholar]
- Ford T, Goodman R, Meltzer H. The British child and adolescent mental health survey 1999: The prevalence of DSM-IV disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:1203–1211. doi: 10.1097/00004583-200310000-00011. [DOI] [PubMed] [Google Scholar]
- Foster T, Gillespie K, McClelland R. Mental disorders and suicide in Northern Ireland. British Journal of Psychiatry. 1997;170:447–452. doi: 10.1192/bjp.170.5.447. [DOI] [PubMed] [Google Scholar]
- Franic S, Dolan CV, Borsboom D, Hudziak JJ, van Beijsterveldt CEM, Boomsma DI. Can genetics help psychometrics? Improving dimensionality assessment through genetic factor modeling. Psychological Methods. 2013;18:406–433. doi: 10.1037/a0032755. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Ray JV, Thornton LC, Kahn RE. Can callous-unemotional traits enhance the understanding, diagnosis, and treatment of serious conduct problems in children and adolescents? A comprehensive review. Psychological Bulletin. 2014;140:1–57. doi: 10.1037/a0033076. [DOI] [PubMed] [Google Scholar]
- Genetics of Personality Consortium. Meta-analysis of genome-wide association studies for neuroticism, and the polygenic association with major depressive disorder. Jama Psychiatry. 2015 doi: 10.1001/jamapsychiatry.2015.0554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giedd JN, Rapoport JL. Structural MRI of pediatric brain development: What have we learned and where are we going? Neuron. 2010;67:728–734. doi: 10.1016/j.neuron.2010.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gjone H, Stevenson J. A longitudinal twin study of temperament and behavior problems: Common genetic or environmental influences? Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1448–1456. doi: 10.1097/00004583-199710000-00028. [DOI] [PubMed] [Google Scholar]
- Goldberg D. Psychopathology and classification in psychiatry. Social Psychiatry and Psychiatric Epidemiology. 2015;50:1–5. doi: 10.1007/s00127-014-0924-y. [DOI] [PubMed] [Google Scholar]
- Gomez R, Burns GL, Walsh JA, Hafetz N. A multitrait-multisource confirmatory factor analytic approach to the construct validity of ADHD and ODD rating scales with Malaysian children. Journal of Abnormal Child Psychology. 2005;33:241–254. doi: 10.1007/s10802-005-1831-1. [DOI] [PubMed] [Google Scholar]
- Goodkind M, Eickhoff SB, Oathes DJ, Jiang Y, Chang A, Jones-Hagata LB, … Etkin A. Identification of a common neurobiological substrate for mental illness. Jama Psychiatry. 2015;72:305–315. doi: 10.1001/jamapsychiatry.2014.2206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman SH, Lahey BB, Fielding B, Dulcan M, Narrow W, Regier D. Representativeness of clinical samples of youths with mental disorders: A preliminary population-based study. Journal of Abnormal Psychology. 1997;106:3–14. doi: 10.1037//0021-843x.106.1.3. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Lieb R, Hoefler M, Pfister H, Bittner A, Beesdo K, Wittchen HU. Panic attack as a risk factor for severe psychopathology. American Journal of Psychiatry. 2004;161(1):2207–2214. doi: 10.1176/appi.ajp.161.12.2207. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA. Introduction to the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Research and Health. 2006;29:74–78. [Google Scholar]
- Gratten J, Wray NR, Keller MC, Visscher PM. Large-scale genomics unveils the genetic architecture of psychiatric disorders. Nature Neuroscience. 2014;17:782–790. doi: 10.1038/nn.3708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray JA, McNaughton N. The neuropsychology of anxiety. 2. Oxford: Oxford University Press; 2003. [Google Scholar]
- Gregory AM, Caspi A, Moffitt TE, Koenen K, Eley TC, Poulton R. Juvenile mental health histories of adults with anxiety disorders. American Journal of Psychiatry. 2007;164:301–308. doi: 10.1176/ajp.2007.164.2.301. [DOI] [PubMed] [Google Scholar]
- Haas BW, Omura K, Constable RT, Canli T. Emotional conflict and neuroticism: Personality-dependent activation in the amygdala and subgenual anterior cingulate. Behavioral Neuroscience. 2007;121:249–256. doi: 10.1037/0735-7044.121.2.249. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Fraley RC, Lahey BB, Waldman ID. Is depression best viewed as a continuum or discrete category? A taxometric analysis of childhood and adolescent depression in a population-based sample. Journal of Abnormal Psychology. 2005;114:96–110. doi: 10.1037/0021-843X.114.1.96. [DOI] [PubMed] [Google Scholar]
- Hartman CA, Hox J, Mellenbergh GJ, Boyle MH, Offord DR, Racine Y, … Sergeant JA. DSM-IV internal construct validity: When a taxonomy meets data. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2001;42:817–836. doi: 10.1111/1469-7610.00778. [DOI] [PubMed] [Google Scholar]
- Haslam N, Williams B, Prior M, Haslam R, Graetz B, Sawyer M. The latent structure of attention-deficit/hyperactivity disorder: a taxometric analysis. Australian and New Zealand Journal of Psychiatry. 2006;40:639–647. doi: 10.1080/j.1440-1614.2006.01863.x. [DOI] [PubMed] [Google Scholar]
- Havik B, Degenhardt FA, Johansson S, Fernandes CPD, Hinney A, Scherag A, … Le Hellard S. DCLK1 variants are associated across schizophrenia and attention deficit/hyperactivity disorder. PLOS One. 2012;7 doi: 10.1371/journal.pone.0035424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henriksson MM, Aro HM, Marttunen MJ, Heikkinen ME, Isometsa ET, Kuoppasalmi KI, Lonnqvist JK. Mental disorders and comorbidity in suicide. American Journal of Psychiatry. 1993;150:935–940. doi: 10.1176/ajp.150.6.935. [DOI] [PubMed] [Google Scholar]
- Hernadi P. Linnaeus before Darwin: Response to Frederic Jameson. New Literary History. 1981;12:379–380. [Google Scholar]
- Hettema JM. What is the genetic relationship between anxiety and depression? American Journal of Medical Genetics. 2008;148C:140–146. doi: 10.1002/ajmg.c.30171. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Neale MC, Myers JM, Prescott CA, Kendler KS. A population-based twin study of the relationship between neuroticism and internalizing disorders. American Journal of Psychiatry. 2006;163:857–864. doi: 10.1176/ajp.2006.163.5.857. [DOI] [PubMed] [Google Scholar]
- Hicks BM, Bernat E, Malone SM, Iacono WG, Patrick CJ, Krueger RF, McGue M. Genes mediate the association between P3 amplitude and externalizing disorders. Psychophysiology. 2007:98–105. doi: 10.1111/j.1469-8986.2006.00471.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hink LK, Rhee SH, Corley RP, Cosgrove VE, Hewitt JK, Schulz-Heik RJ, … Waldman ID. Personality dimensions as common and broadband-specific features for internalizing and externalizing disorders. Journal of Abnormal Child Psychology. 2013;41:939–957. doi: 10.1007/s10802-013-9730-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinshaw SP, Owens EB, Zalecki C, Huggins SP, Montenegro-Nevado AJ, Schrodek E, Swanson EN. Prospective follow-up of girls with attention-deficit/hyperactivity disorder Into early adulthood: Continuing impairment Includes elevated risk for suicide attempts and self-injury. Journal of Consulting and Clinical Psychology. 2012;80:1041–1051. doi: 10.1037/a0029451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hipwell AE, Keenan K, Kasza K, Loeber R, Stouthamer-Loeber M, Bean T. Reciprocal influences between girls’ conduct problems and depression, and parental punishment and warmth: A six year prospective analysis. Journal of Abnormal Child Psychology. 2008;36:663–677. doi: 10.1007/s10802-007-9206-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hipwell AE, Stepp S, Feng X, Burke J, Battista DR, Loeber R, Keenan K. Impact of oppositional defiant disorder dimensions on the temporal ordering of conduct problems and depression across childhood and adolescence in girls. Journal of Child Psychology and Psychiatry. 2011;52:1099–1108. doi: 10.1111/j.1469-7610.2011.02448.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoertel N, Franco S, Wall MM, Oquendo MA, Kerridge BT, Limosin F, Blanco C. Mental disorders and risk of suicide attempt: a national prospective study. Molecular Psychiatry. 2015;20:718–726. doi: 10.1038/mp.2015.19. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Curtiss J, McNally RJ. A complex network perspective on clinical science. Perspectives on Psychological Science. 2016;11:597–605. doi: 10.1177/1745691616639283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmstrand C, Bogren M, Mattisson C, Bradvik L. Long-term suicide risk in no, one or more mental disorders: The Lundby Study 1947–1997. Acta Psychiatrica Scandinavica. 2015;132:459–469. doi: 10.1111/acps.12506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holzinger KJ, Swineford F. The bi-factor method. Psychometrika. 1937;2:41–54. [Google Scholar]
- Horn PJ, Wuyek LA. Anxiety disorders as a risk factor for subsequent depression. International Journal of Psychiatry in Clinical Practice. 2010;14:244–247. doi: 10.3109/13651501.2010.487979. [DOI] [PubMed] [Google Scholar]
- Huang B, Grant BF, Dawson DA, Stinson FS, Chou SP, Saha TD, … Pickering RP. Race-ethnicity and the prevalence and co-occurrence of Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, alcohol and drug use disorders and Axis I and II disorders: United States, 2001 to 2002. Comprehensive Psychiatry. 2006;47:252–257. doi: 10.1016/j.comppsych.2005.11.001. [DOI] [PubMed] [Google Scholar]
- Huang YY, Kotov R, de Girolamo G, Preti A, Angermeyer M, Benjet C, … Kessler RC. DSM-IV personality disorders in the WHO World Mental Health Surveys. British Journal of Psychiatry. 2009;195:46–53. doi: 10.1192/bjp.bp.108.058552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacono WG, Carlson SR, Malone SM, McGue M. P3 event-related potential amplitude and the risk for disinhibitory disorders in adolescent boys. Archives of General Psychiatry. 2002;59:750–757. doi: 10.1001/archpsyc.59.8.750. [DOI] [PubMed] [Google Scholar]
- Icick R, Kovess V, Gasquet I, Lepine JP. Days out of role due to common mental and physical disorders: French results from the WHO World Mental Health surveys. Encephale-Revue De Psychiatrie Clinique Biologique Et Therapeutique. 2014;40:338–344. doi: 10.1016/j.encep.2013.11.005. [DOI] [PubMed] [Google Scholar]
- Insel TR, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, … Wang P. Research Domain Criteria (RDoC): Toward a new classification framework for research on mental disorders. American Journal of Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Ionita-Laza I, Xu B, Makarov V, Buxbaum JD, Roos JL, Gogos JA, Karayiorgou M. Scan statistic-based analysis of exome sequencing data identifies FAN1 at 15q13.3 as a susceptibility gene for schizophrenia and autism. Proceedings of the National Academy of Sciences of the United States of America. 2014;111:343–348. doi: 10.1073/pnas.1309475110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivanova MY, Achenbach TM, Rescorla LA, Harder VS, Ang RP, Bilenberg N, … Verhulst FC. Preschool psychopathology reported by parents in 23 societies: Testing the seven-syndrome model of the Child Behavior Checklist for ages 1.5–5. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:1215–1224. doi: 10.1016/j.jaac.2010.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobi F, Hoefler M, Siegert J, Mack S, Gerschler A, Scholl L, … Wittchen H-U. Twelve-month prevalence, comorbidity and correlates of mental disorders in Germany: the Mental Health Module of the German Health Interview and Examination Survey for Adults (DEGS1-MH) International Journal of Methods in Psychiatric Research. 2014;23:304–319. doi: 10.1002/mpr.1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobi F, Wittchen HU, Holting C, Hofler M, Pfister H, Muller N, Lieb R. Prevalence, co-morbidity and correlates of mental disorders in the general population: results from the German Health Interview and Examination Survey (GHS) Psychological Medicine. 2004;34:597–611. doi: 10.1017/S0033291703001399. [DOI] [PubMed] [Google Scholar]
- Jacobson KC, Prescott CA, Kendler KS. Sex differences in the genetic and environmental influences on the development of antisocial behavior. Development and Psychopathology. 2002;14:395–416. doi: 10.1017/s0954579402002110. [DOI] [PubMed] [Google Scholar]
- Jaffee SR, Price TS. The implications of genotype-environment correlation for establishing causal processes in psychopathology. Development and Psychopathology. 2012;24:1253–1264. doi: 10.1017/S0954579412000685. [DOI] [PubMed] [Google Scholar]
- Jaffee SR, Strait LB, Odgers CL. From correlates to causes: Can quasi-experimental studies and statistical innovations bring us closer to identifying the causes of antisocial behavior? Psychological Bulletin. 2012;138:272–295. doi: 10.1037/a0026020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James LM, Taylor J. Revisiting the structure of mental disorders: Borderline personality disorder and the internalizing/externalizing spectra. British Journal of Clinical Psychology. 2008;47:361–380. doi: 10.1348/014466508X299691. [DOI] [PubMed] [Google Scholar]
- Jang KL, Livesley WJ. Why do measures of normal and disordered personality correlate? A study of genetic comorbidity. Journal of Personality Disorders. 1999;13:10–17. doi: 10.1521/pedi.1999.13.1.10. [DOI] [PubMed] [Google Scholar]
- Jensen PS, Rubio-Stipec M, Canino G, Bird HR, Dulcan MK, Schwab-Stone ME, Lahey BB. Parent and child contributions to diagnosis of mental disorder: Are both informants always necessary? Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:1569–1579. doi: 10.1097/00004583-199912000-00019. [DOI] [PubMed] [Google Scholar]
- Jensen SKG, Dickie EW, Schwartz DH, Evans CJ, Dumontheil I, Paus T, Barker ED. Effect of early adversity and childhood internalizing symptoms on brain structure in young men. JAMA Pediatrics. 2015;169:938–946. doi: 10.1001/jamapediatrics.2015.1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeronimus BF, Kotov R, Riese H, Ormel J. Neuroticism’s prospective association with mental disorders halves after adjustment for baseline symptoms and psychiatric history, but the adjusted association hardly decays with time: a meta-analysis on 59 longitudinal/prospective studies with 443,313 participants. Psychological Medicine. 2016;46:2883–2906. doi: 10.1017/S0033291716001653. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Dohrenwend BP, Link BG, Brook JS. A longitudinal investigation of social causation and social selection processes involved in the association between socioeconomic status and psychiatric disorders. Journal of Abnormal Psychology. 1999;108:490–499. doi: 10.1037//0021-843x.108.3.490. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Skodol AE, Oldham JM, Kasen S, Brook JS. Personality disorders in adolescence and risk of major mental disorders and suicidality during adulthood. Archives of General Psychiatry. 1999;56:805–811. doi: 10.1001/archpsyc.56.9.805. [DOI] [PubMed] [Google Scholar]
- Kafali N, Cook B, Wang S, Martinez PG, Selke Z, Blanco C. Impact of mental disorders on employment and receipt of public assistance: An instrumental variables approach. Journal of Mental Health Policy and Economics. 2015;18(3):137–145. [PubMed] [Google Scholar]
- Kagan J, Moss HA. Birth to maturity: A study in psychological development. New York: Wiley; 1962. [Google Scholar]
- Kamphuis JH, Noordhof A. On categorical diagnoses in DSM-V: Cutting dimensions at useful points? Psychological Assessment. 2009;21:294–301. doi: 10.1037/a0016697. [DOI] [PubMed] [Google Scholar]
- Karmiloff A, Casey BJ, Massand E, Przemyslaw T, Thomas MSC. Environmental and genetic influences on neurocognitive development: The importance of multiple methodologies and time-dependent intervention. Clinical Psychological Science. 2014;2:628–637. doi: 10.1177/2167702614521188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasen S, Cohen P, Skodol AE, Johnson JG, Brook JS. Influence of child and adolescent psychiatric disorders on young adult personality disorder. American Journal of Psychiatry. 1999a;156:1529–1535. doi: 10.1176/ajp.156.10.1529. [DOI] [PubMed] [Google Scholar]
- Kasen S, Cohen P, Skodol AE, Johnson JG, Brook JS. Influence of child and adolescent psychiatric disorders on young adult personality disorder. American Journal of Psychiatry. 1999b;156(10):1529–1535. doi: 10.1176/ajp.156.10.1529. [DOI] [PubMed] [Google Scholar]
- Keenan K, Feng X, Hipwell A, Klostermann S. Depression begets depression: Comparing the predictive utility of depression and anxiety symptoms to later depression. Journal of Child Psychology and Psychiatry. 2009;50:1167–1175. doi: 10.1111/j.1469-7610.2009.02080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keenan K, Hipwell A, Chung T, Stepp S, Stouthamer-Loeber M, Loeber R, McTigue K. The Pittsburgh Girls Study: Overview and initial findings. Journal of Clinical Child and Adolescent Psychology. 2010;39:506–521. doi: 10.1080/15374416.2010.486320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keenan K, Shaw DS. Developmental and social influences on young girls’ early problem behavior. Psychological Bulletin. 1997;121(1):95–113. doi: 10.1037/0033-2909.121.1.95. [DOI] [PubMed] [Google Scholar]
- Keenan K, Shaw DS. Starting at the beginning: Exploring the etiology of antisocial behavior in the first years of life. In: Lahey BB, Moffitt TE, Caspi A, editors. Causes of Conduct Disorder and Juvenile Delinquency. New York, NY: Guilford Press Guilford Press; 2003. pp. 153–181. [Google Scholar]
- Kendler KS. A gene for..: The nature of gene action in psychiatric disorders. American Journal of Psychiatry. 2005;162:1243–1252. doi: 10.1176/appi.ajp.162.7.1243. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Aggen SH, Knudsen GU, Roysamb E, Neale MC, Reichborn-Kjennerud T. The structure of genetic and environmental risk factors for syndromal and subsyndromal common DSM-IV axis I and axis II disorders. American Journal of Psychiatry. 2011;168:29–39. doi: 10.1176/appi.ajp.2010.10030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Aggen SH, Neale MC. Evidence for multiple genetic factors underlying DSM-IV criteria for major depression. Jama Psychiatry. 2013;70:599–607. doi: 10.1001/jamapsychiatry.2013.751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Aggen SH, Patrick CJ. A multivariate twin study of the DSM-IV criteria for antisocial personality disorder. Biological Psychiatry. 2012;71:247–253. doi: 10.1016/j.biopsych.2011.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Aggen SH, Prescott CA, Crabbe J, Neale MC. Evidence for multiple genetic factors underlying the DSM-IV criteria for alcohol dependence. Molecular Psychiatry. 2012;17(12):1306–1315. doi: 10.1038/mp.2011.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Jacobson KC, Myers J, Prescott CA. Sex differences in genetic and environmental risk factors for irrational fears and phobias. Psychological Medicine. 2002;32:209–217. doi: 10.1017/s003329170100513x. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Myers J. The genetic and environmental relationship between major depression and the five-factor model of personality. Psychological Medicine. 2010;40:801–806. doi: 10.1017/S0033291709991140. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Myers J. The boundaries of the internalizing and externalizing genetic spectra in men and women. Psychological Medicine. 2014;44:647–665. doi: 10.1017/S0033291713000585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kessler RC. The National Comorbidity Survey: Preliminary Results and Future Directions. International Journal of Methods in Psychiatric Research. 1995;5:139–151. [Google Scholar]
- Kessler RC, Avenevoli S, Costello EJ, Georgiades K, Green JG, Gruber MJ, … Merikangas KR. Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Archives of General Psychiatry. 2012;69:372–380. doi: 10.1001/archgenpsychiatry.2011.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Heeringa S, Lakoma MD, Petukhova M, Rupp AE, Schoenbaum M, … Zaslavsky AM. Individual and societal effects of mental disorders on earnings in the united states: Results from the national comorbidity survey replication. American Journal of Psychiatry. 2008;165:703–711. doi: 10.1176/appi.ajp.2008.08010126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao SY, Nelson CB, Hughes M, Eshleman S, … Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United-States - Results from the National-Comorbidity-Survey. Archives of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, Zaslavsky AM. The role of latent internalizing and externalizing predispositions in accounting for the development of comorbidity among common mental disorders. Current Opinion in Psychiatry. 2011;24:307–312. doi: 10.1097/YCO.0b013e3283477b22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Eaton NR, Krueger RF, Skodol AE, Wall MM, Grant B, … Hasin DS. Thought disorder in the meta-structure of psychopathology. Psychological Medicine. 2013;43:1673–1683. doi: 10.1017/S0033291712002292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan AA, Jacobson KC, Gardner CO, Prescott CA, Kendler KS. Personality and comorbidity of common psychiatric disorders. British Journal of Psychiatry. 2005;186:190–196. doi: 10.1192/bjp.186.3.190. [DOI] [PubMed] [Google Scholar]
- Kim H, Eaton NR. The hierarchical structure of common mental disorders: Connecting multiple levels of comorbidity, bifactor models, and predictive validity. Journal of Abnormal Psychology. 2015;124:1064–1078. doi: 10.1037/abn0000113. [DOI] [PubMed] [Google Scholar]
- Kim-Cohen J, Arseneault L, Caspi A, Tomas MP, Taylor A, Moffitt TE. Validity of DSM-IV conduct disorder in 4 1/2 5-year-old children: A longitudinal epidemiological study. American Journal of Psychiatry. 2005;162(6):1108–1117. doi: 10.1176/appi.ajp.162.6.1108. [DOI] [PubMed] [Google Scholar]
- Kim-Cohen J, Arseneault L, Newcombe R, Adams F, Bolton H, Cant L, … Moffitt TE. Five-year predictive validity of DSM-IV conduct disorder research diagnosis in 4 1/2–5-year-old children. European Child & Adolescent Psychiatry. 2009;18:284–291. doi: 10.1007/s00787-008-0729-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: Developmental follow-back of a prospective-longitudinal cohort. Archives of General Psychiatry. 2003;60:709–717. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- Knudsen AK, Skogen JC, Harvey SB, Stewart R, Hotopf M, Moran P. Personality disorders, common mental disorders and receipt of disability benefits: Evidence from the British National Survey of Psychiatric Morbidity. Psychological Medicine. 2012;42:2631–2640. doi: 10.1017/S0033291712000906. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Moffitt TE, Caspi A, Gregory A, Harrington H, Poulton R. The developmental mental-disorder histories of adults with posttraumatic stress disorder: A prospective longitudinal birth cohort study. Journal of Abnormal Psychology. 2008;117:460–466. doi: 10.1037/0021-843X.117.2.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopala-Sibley DC, Kotov R, Bromet EJ, Carlson GA, Danzig AP, Black SR, Klein DN. Personality diatheses and Hurricane Sandy: Effects on post-disaster depression. Psychological Medicine. 2016;(46):865–875. doi: 10.1017/S0033291715002378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korhonen T, Latvala A, Dick DM, Pulkkinen L, Rose RJ, Kaprio J, Huizink AC. Genetic and environmental influences underlying externalizing behaviors, cigarette smoking and illicit drug use across adolescence. Behavior Genetics. 2012;42:614–625. doi: 10.1007/s10519-012-9528-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korman M. Implicit personality theories of clinicians as defined by semantic structures. Journal of Consulting Psychology. 1960;24:180–186. [Google Scholar]
- Kossowsky J, Pfaltz MC, Schneider S, Taeymans J, Locher C, Gaab J. The separation anxiety hypothesis of panic disorder revisited: A meta-analysis. American Journal of Psychiatry. 2013;170:768–781. doi: 10.1176/appi.ajp.2012.12070893. [DOI] [PubMed] [Google Scholar]
- Kosterman R, Hawkins JD, Mason WA, Herrenkohl TI, Lengua LJ, McCauley E. Assessment of behavior problems in childhood and adolescence as predictors of early adult depression. Journal of Psychopathology and Behavioral Assessment. 2010;32(1):118–127. doi: 10.1007/s10862-009-9138-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Chang SW, Fochtmann LJ, Mojtabai R, Carlson GA, Sedler MJ, Bromet EJ. Schizophrenia in the internalizing-externalizing Framework: A third dimension? Schizophrenia Bulletin. 2011;37:1168–1178. doi: 10.1093/schbul/sbq024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Ruggero CJ, Krueger RF, Watson D, Yuan QL, Zimmerman M. New dimensions in the quantitative classification of mental illness. Archives of General Psychiatry. 2011;68:1003–1011. doi: 10.1001/archgenpsychiatry.2011.107. [DOI] [PubMed] [Google Scholar]
- Kraepelin E. Dementia praecox and paraphrenia. 2. Edinburgh: E. & S. Livingstone; 1919. [Google Scholar]
- Kraepelin E. Manic-depressive insanity and paranoia. Edinburgh: E. & S. Livingstone; 1921. [Google Scholar]
- Kramer MD, Krueger RF, Hicks BM. The role of internalizing and externalizing liability factors in accounting for gender differences in the prevalence of common psychopathological syndromes. Psychological Medicine. 2008;38:51–61. doi: 10.1017/S0033291707001572. [DOI] [PubMed] [Google Scholar]
- Krueger RF. Personality traits in late adolescence predict mental disorders in early adulthood: A prospective-epidemiological study. Journal of Personality. 1999a;67:39–65. doi: 10.1111/1467-6494.00047. [DOI] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999b;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): A longitudinal-epidemiological study. Journal of Abnormal Psychology. 1998;107:216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, Silva PA, McGee R. Personality traits are differentially linked to mental disorders: A multitrait-multidiagnosis study of an adolescent birth cohort. Journal of Abnormal Psychology. 1996;105:299–312. doi: 10.1037//0021-843x.105.3.299. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Chentsova-Dutton YE, Markon KE, Goldberg D, Ormel J. A cross-cultural study of the structure of comorbidity among common psychopathological syndromes in the general health care setting. Journal of Abnormal Psychology. 2003;112:437–447. doi: 10.1037/0021-843x.112.3.437. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Hopwood CJ, Wright AGC, Markon KE. DSM-5 and the path toward empirically based and clinically useful conceptualization of personality and psychopathology. Clinical Psychology-Science and Practice. 2014;21:245–261. [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology. 2006a;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Understanding psychopathology: Melding behavior genetics, personality, and quantitative psychology to develop an empirically based model. Current Directions in Psychological Science. 2006b;15:113–117. doi: 10.1111/j.0963-7214.2006.00418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. The role of the DSM-5 personality trait model in moving toward a quantitative and empirically based approach to classifying personality and psychopathology. In: Cannon TD, Widiger T, editors. Annual Review of Clinical Psychology. Vol. 10. 2014. pp. 477–501. [DOI] [PubMed] [Google Scholar]
- Krueger RF, McGue M, Iacono WG. The higher-order structure of common DSM mental disorders: internalization, externalization, and their connections to personality. Personality and Individual Differences. 2001;30:1245–1259. [Google Scholar]
- Krueger RF, Nichol PE, Hicks BM, Markon KE, Patrick CJ, Iacono WG, McGue M. Using latent trait modeling to conceptualize an alcohol problems continuum. Psychological Assessment. 2004;16:107–119. doi: 10.1037/1040-3590.16.2.107. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Piasecki TM. Toward a dimensional and psychometrically-informed approach to conceptualizing psychopathology. Behaviour Research and Therapy. 2002;40:485–499. doi: 10.1016/s0005-7967(02)00016-5. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Tackett JL. Personality and psychopathology: Working toward the bigger picture. Journal of Personality Disorders. 2003;17:109–128. doi: 10.1521/pedi.17.2.109.23986. [DOI] [PubMed] [Google Scholar]
- Kumari V, Das M, Wilson GD, Goswami S, Sharma T. Neuroticism and brain responses to anticipatory fear. Behavioral Neuroscience. 2007;121:643–652. doi: 10.1037/0735-7044.121.4.643. [DOI] [PubMed] [Google Scholar]
- Kushner SC. A review of the direct and interactive effects of life stressors and dispositional traits on youth psychopathology. Child Psychiatry and Human Development. 2015;46:810–819. doi: 10.1007/s10578-014-0523-x. [DOI] [PubMed] [Google Scholar]
- Laceulle OM, Vollebergh WAM, Ormel J. The structure of psychopathology in adolescence: Replication of a general psychopathology factor in the TRAILS Study. Clinical Psychological Science. 2015;3:1–11. [Google Scholar]
- Lahey BB. Commentary: Role of temperament in developmental models of psychopathology. Journal of Clinical Child and Adolescent Psychology. 2004;33:88–93. doi: 10.1207/S15374424JCCP3301_9. [DOI] [PubMed] [Google Scholar]
- Lahey BB. Public health significance of neuroticism. American Psychologist. 2009;64:241–256. doi: 10.1037/a0015309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Barkley RA, Garfinkel B, McBurnett K, Kerdyk L, … Shaffer D. DSM-IV field trials for oppositional defiant disorder and conduct disorder in children and adolescents. American Journal of Psychiatry. 1994;151:1163–1171. doi: 10.1176/ajp.151.8.1163. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Chronis AM, Jones HA, Williams SH, Loney J, Waldman ID. Psychometric characteristics of a measure of emotional dispositions developed to test a developmental propensity model of conduct disorder. Journal of Clinical Child and Adolescent Psychology. 2008;37:794–807. doi: 10.1080/15374410802359635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Hakes JK, Zald DH, Hariri AR, Rathouz PJ. Is there a general factor of prevalent psychopathology during adulthood? Journal of Abnormal Psychology. 2012;121(4):971–977. doi: 10.1037/a0028355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, McBurnett K, Biederman J, Greenhill L, Hynd GW, … Shaffer D. DSM-IV field trials for attention-deficit/hyperactivity disorder in children and adolescents. American Journal of Psychiatry. 1994;151:1673–1685. doi: 10.1176/ajp.151.11.1673. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Waldman ID, Loft JD, Hankin BL, Rick J. The structure of child and adolescent psychopathology: Generating new hypotheses. Journal of Abnormal Psychology. 2004;113:358–385. doi: 10.1037/0021-843X.113.3.358. [DOI] [PubMed] [Google Scholar]
- Lahey BB, D’Onofrio BM. All in the family: Comparing siblings to test causal hypotheses regarding environmental influences on behavior. Current Directions in Psychological Science. 2010;19:319–323. doi: 10.1177/0963721410383977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Loeber R, Burke J, Rathouz PJ, McBurnett K. Waxing and waning in concert: Dynamic comorbidity of conduct disorder with other disruptive and emotional problems over 17 years among clinic-referred boys. Journal of Abnormal Psychology. 2002;111:556–567. doi: 10.1037//0021-843x.111.4.556. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Loeber R, Burke JD, Applegate B. Predicting future antisocial personality disorder in males from a clinical assessment in childhood. Journal of Consulting and Clinical Psychology. 2005;73:389–399. doi: 10.1037/0022-006X.73.3.389. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Loney J, Lee SS, Willcutt E. Instability of the DSM-IV subtypes of ADHD from preschool through elementary school. Archives of General Psychiatry. 2005;62:896–902. doi: 10.1001/archpsyc.62.8.896. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Rathouz PJ, Applegate B, Hulle CV, Garriock HA, Urbano RC, … Waldman ID. Testing structural models of DSM-IV symptoms of common forms of child and adolescent psychopathology. Journal of Abnormal Child Psychology. 2008;36:187–206. doi: 10.1007/s10802-007-9169-5. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Rathouz PJ, Applegate B, Tackett JL, Waldman ID. Psychometrics of a self-report version of the child and adolescent dispositions scale. Journal of Clinical Child and Adolescent Psychology. 2010;39:351–361. doi: 10.1080/15374411003691784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Rathouz PJ, Keenan K, Stepp SD, Loeber R, Hipwell AE. Criterion validity of the general factor of psychopathology in a prospective study of girls. Journal of Child Psychology and Psychiatry. 2015;4:415–422. doi: 10.1111/jcpp.12300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Schwab-Stone M, Goodman SH, Waldman ID, Canino G, Rathouz PJ, … Jensen PS. Age and gender differences in oppositional behavior and conduct problems: A cross-sectional household study of middle childhood and adolescence. Journal of Abnormal Psychology. 2000;109:488–503. [PubMed] [Google Scholar]
- Lahey BB, Van Hulle CA, Singh AL, Waldman ID, Rathouz PJ. Higher-order genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Archives of General Psychiatry. 2011;68:181–189. doi: 10.1001/archgenpsychiatry.2010.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Waldman ID. A developmental propensity model of the origins of conduct problems during childhood and adolescence. In: Lahey BB, Moffitt TE, Caspi A, editors. Causes of Conduct Disorder and Juvenile Delinquency. New York, NY: Guilford Press Guilford Press; 2003. pp. 76–117. [Google Scholar]
- Lahey BB, Waldman ID. Annual Research Review: Phenotypic and causal structure of conduct disorder in the broader context of prevalent forms of psychopathology. Journal of Child Psychology and Psychiatry. 2012;53:536–557. doi: 10.1111/j.1469-7610.2011.02509.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Waldman ID, McBurnett K. Annotation: The development of antisocial behavior: An integrative causal model. Journal of Child Psychology and Psychiatry. 1999;40:669–682. [PubMed] [Google Scholar]
- Lahey BB, Zald DH, Hakes JK, Krueger RF, Rathouz PJ. Patterns of heterotypic continuity associated with the cross-sectional correlational structure of prevalent mental disorders in adults. Jama Psychiatry. 2014;71:989–996. doi: 10.1001/jamapsychiatry.2014.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latzman RD, Vaidya JG, Clark LA, Watson D. Components of disinhibition (vs. constraint) differentially predict aggression and alcohol Use. European Journal of Personality. 2011;25:477–486. [Google Scholar]
- Lavigne JV, Hopkins J, Gouze KR, Bryant FB. Bidirectional influences of anxiety and depression in young children. Journal of Abnormal Child Psychology. 2015;43:163–176. doi: 10.1007/s10802-014-9884-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, Guo W-j, Tsang A, He Y-l, Huang Y-q, Liu Z-r, … Kessler RC. Impaired role functioning and treatment rates for mental disorders and chronic physical disorders in metropolitan China. Psychosomatic Medicine. 2009;71:886–893. doi: 10.1097/PSY.0b013e3181baa65e. [DOI] [PubMed] [Google Scholar]
- Lee SH, Ripke S, Neale BM, Faraone SV, Purcell SM, Perlis RH … Group. Genetic relationship between five psychiatric disorders estimated from genome-wide SNPs. Nature Genetics. 2013;45:984–990. doi: 10.1038/ng.2711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SS, Humphreys KL, Flory K, Liu R, Glass K. Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: A meta-analytic review. Clinical Psychology Review. 2011;31:328–341. doi: 10.1016/j.cpr.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemery KS, Essex MJ, Smider NA. Revealing the relation between temperament and behavior problem symptoms by eliminating measurement confounding: Expert ratings and factor analyses. Child Development. 2002;73:867–882. doi: 10.1111/1467-8624.00444. [DOI] [PubMed] [Google Scholar]
- Lentini E, Kasahara M, Arver S, Savic I. Sex differences in the human brain and the impact of sex chromosomes and sex hormones. Cerebral Cortex. 2013;23:2322–2336. doi: 10.1093/cercor/bhs222. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Lane MC, Loranger AW, Kessler RC. DSM-IV personality disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;62:553–564. doi: 10.1016/j.biopsych.2006.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson DF, Duan J, Oh S, Wang K, Sanders AR, Shi J, … Gejman PV. Copy number variants in schizophrenia: Confirmation of five previous findings and new evidence for 3q29 microdeletions and VIPR2 duplications. American Journal of Psychiatry. 2011;168:302–316. doi: 10.1176/appi.ajp.2010.10060876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Holm-Denoma JM, Small JW, Seeley JR, Joiner TE. Separation anxiety disorder in childhood as a risk factor for future mental illness. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:548–555. doi: 10.1097/CHI.0b013e31816765e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Adolescent psychopathology .3. The clinical consequences of comorbidity. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:510–519. doi: 10.1097/00004583-199504000-00018. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR, Klein DN. Axis II psychopathology as a function of axis I disorders in childhood and adolescence. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1752–1759. doi: 10.1097/00004583-199712000-00024. [DOI] [PubMed] [Google Scholar]
- Lilienfeld SO. Comorbidity between and within childhood externalizing and internalizing disorders: Reflections and directions. Journal of Abnormal Child Psychology. 2003;31:285–291. doi: 10.1023/a:1023229529866. [DOI] [PubMed] [Google Scholar]
- Lilienfeld SO, Waldman ID, Israel AC. A critical note on the use of the term and concept of “ comorbidity” in psychopathology research. Clinical Psychology: Science and Practice. 1994;1:71–83. [Google Scholar]
- Links PS, Eynan R. The relationship between personality disorders and axis I psychopathology: Deconstructing comorbidity. In: Nolen-Hoeksema S, editor. Annual Review of Clinical Psychology. Vol. 9. 2013. pp. 529–554. [DOI] [PubMed] [Google Scholar]
- Livesley WJ, Jang KL. The Behavioral genetics of personality disorder. Annual Review of Clinical Psychology. 2008;4:247–274. doi: 10.1146/annurev.clinpsy.4.022007.141203. [DOI] [PubMed] [Google Scholar]
- Loeber R, Hay D. Key issues in the development of aggression and violence from childhood to early adulthood. Annual Review of Psychology. 1997;48:371–410. doi: 10.1146/annurev.psych.48.1.371. [DOI] [PubMed] [Google Scholar]
- Loehlin JC. Latent variable models: An introduction to factor, path, and structural equation analysis. 3. Hillsdale, NJ: Lawrence Erlbaum Associates; 1998. [Google Scholar]
- Lokkerbol J, Adema D, de Graaf R, ten Have M, Cuijpers P, Beekman A, Smit F. Non-fatal burden of disease due to mental disorders in the Netherlands. Social Psychiatry and Psychiatric Epidemiology. 2013;48:1591–1599. doi: 10.1007/s00127-013-0660-8. [DOI] [PubMed] [Google Scholar]
- Luby JL, Si X, Belden AC, Tandon M, Spitznagel E. Preschool depression: Homotypic continuity and course over 24 Months. Archives of General Psychiatry. 2009;66:897–905. doi: 10.1001/archgenpsychiatry.2009.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mack S, Jacobi F, Beesdo-Baum K, Gerschler A, Strehle J, Hoefler M, … Wittchen HU. Functional disability and quality of life decrements in mental disorders: Results from the Mental Health Module of the German Health Interview and Examination Survey for Adults (DEGS1-MH) European Psychiatry. 2015;30:793–800. doi: 10.1016/j.eurpsy.2015.06.003. [DOI] [PubMed] [Google Scholar]
- Maier R, Moser G, Chen GB, Ripke S, Coryell W, Potash JB … PGC. Joint analysis of psychiatric disorders increases accuracy of risk prediction for schizophrenia, bipolar disorder, and major depressive disorder. American Journal of Human Genetics. 2015;96:283–294. doi: 10.1016/j.ajhg.2014.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malhotra D, McCarthy S, Michaelson JJ, Vacic V, Burdick KE, Yoon S, … Sebat J. High frequencies of de novo CNVs in bipolar disorder and schizophrenia. Neuron. 2011;72:951–963. doi: 10.1016/j.neuron.2011.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markon KE. How things fall apart: Understanding the nature of internalizing through its relationship with impairment. Journal of Abnormal Psychology. 2010a;119:447–458. doi: 10.1037/a0019707. [DOI] [PubMed] [Google Scholar]
- Markon KE. Modeling psychopathology structure: A symptom-level analysis of Axis I and II disorders. Psychological Medicine. 2010b;40:273–288. doi: 10.1017/S0033291709990183. [DOI] [PubMed] [Google Scholar]
- Markon KE, Chmielewski M, Miller CJ. The reliability and validity of discrete and continuous measures of psychopathology: A quantitative review. Psychological Bulletin. 2011;137:856–879. doi: 10.1037/a0023678. [DOI] [PubMed] [Google Scholar]
- Markon KE, Krueger RF. Categorical and continuous models of liability to externalizing disorders - A direct comparison in NESARC. Archives of General Psychiatry. 2005;62:1352–1359. doi: 10.1001/archpsyc.62.12.1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathyssek CM, Olino TM, Verhulst FC, van Oort FVA. Childhood internalizing and externalizing problems predict the onset of clinical panic attacks over adolescence: The TRAILS Study. PLOS One. 2012;7 doi: 10.1371/journal.pone.0051564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maughan B, Rowe R, Messer J, Goodman R, Meltzer H. Conduct disorder and oppositional defiant disorder in a national sample: Developmental epidemiology. Journal of Child Psychology and Psychiatry. 2004;45:609–621. doi: 10.1111/j.1469-7610.2004.00250.x. [DOI] [PubMed] [Google Scholar]
- McAdams TA, Gregory AM, Eley TC. Genes of experience: Explaining the heritability of putative environmental variables through their association with behavioural and emotional traits. Behavior Genetics. 2013;43:314–328. doi: 10.1007/s10519-013-9591-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrae RR, Costa PT. Personality in adulthood: A five-factor theory perspective. New York: Guilford Press; 2003. [Google Scholar]
- McLaughlin KA. Future directions in childhood adversity and youth psychopathology. Journal of Clinical and Child and Adolescent Psychology. 2016;45:361–382. doi: 10.1080/15374416.2015.1110823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Nolen-Hoeksema S. Rumination as a transdiagnostic factor in depression and anxiety. Behaviour Research and Therapy. 2011;49:186–193. doi: 10.1016/j.brat.2010.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMillan KA, Enns MW, Cox BJ, Sareen J. Comorbidity of axis I and II mental disorders with schizophrenia and psychotic disorders: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Canadian Journal of Psychiatry-Revue Canadienne De Psychiatrie. 2009;54:477–486. doi: 10.1177/070674370905400709. [DOI] [PubMed] [Google Scholar]
- Meehl PE. Comorbidity and taxometrics. Clinical Psychology: Science and Practice. 2001;8:507–519. [Google Scholar]
- Merikangas KR, Jin R, He JP, Kessler RC, Lee S, Sampson NA, … Zarkov Z. Prevalence and correlates of bipolar spectrum disorder in the World Mental Health Survey Initiative. Archives of General Psychiatry. 2011;68:241–251. doi: 10.1001/archgenpsychiatry.2011.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, McClair VL. Epidemiology of substance use disorders. Human Genetics. 2012;131:779–789. doi: 10.1007/s00439-012-1168-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mian ND, Godoy L, Briggs-Gowan MJ, Carter AS. Patterns of anxiety symptoms in toddlers and preschool-age children: Evidence of early differentiation. Journal of Anxiety Disorders. 2012;26:102–110. doi: 10.1016/j.janxdis.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Middeldorp CM, Cath DC, Van Dyck R, Boomsma DI. The co-morbidity of anxiety and depression in the perspective of genetic epidemiology. A review of twin and family studies. Psychological Medicine. 2005;35:611–624. doi: 10.1017/s003329170400412x. [DOI] [PubMed] [Google Scholar]
- Miettunen J, Murray GK, Jones PB, Maki P, Ebeling H, Taanila A, … Moilanen I. Longitudinal associations between childhood and adulthood externalizing and internalizing psychopathology and adolescent substance use. Psychological Medicine. 2014;44:1727–1738. doi: 10.1017/S0033291713002328. [DOI] [PubMed] [Google Scholar]
- Mikolajewski AJ, Allan NP, Hart SA, Lonigan CJ, Taylor J. Negative affect shares genetic and environmental influences with symptoms of childhood internalizing and externalizing disorders. Journal of Abnormal Child Psychology. 2013;41:411–423. doi: 10.1007/s10802-012-9681-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mischel W. Toward an integrative science of the person. Annual Review of Psychology. 2004;55:1–22. doi: 10.1146/annurev.psych.55.042902.130709. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, Poulton R. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychological Medicine. 2010;40:899–909. doi: 10.1017/S0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Harrington H, Caspi A, Kim-Cohen J, Goldberg D, Gregory AM, Poulton R. Depression and generalized anxiety disorder: Cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Archives of General Psychiatry. 2007;64:651–660. doi: 10.1001/archpsyc.64.6.651. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine. 2009:e1000097. [PMC free article] [PubMed] [Google Scholar]
- Molteni R, Lipska BK, Weinberger DR, Racagni G, Riva MA. Developmental and stress-related changes of neurotrophic factor gene expression in an animal model of schizophrenia. Molecular Psychiatry. 2001;6:285–292. doi: 10.1038/sj.mp.4000865. [DOI] [PubMed] [Google Scholar]
- Muris P, Meesters C. The validity of attention deficit hyperactivity and hyperkinetic disorder symptom domains in nonclinical Dutch children. Journal of Clinical Child and Adolescent Psychology. 2003;32:460–466. doi: 10.1207/S15374424JCCP3203_14. [DOI] [PubMed] [Google Scholar]
- Mykletun A, Overland S, Dahl AA, Krokstad S, Bjerkeset O, Glozier N, Aaro LE. A population-based cohort study of the effect of common mental disorders on disability pension awards. American Journal of Psychiatry. 2006;163:1412–1418. doi: 10.1176/ajp.2006.163.8.1412. [DOI] [PubMed] [Google Scholar]
- Nadder TS, Rutter M, Silberg JL, Maes HH, Eaves LJ. Genetic effects on the variation and covariation of attention deficit-hyperactivity disorder (ADHD) and oppositional-defiant disorder/conduct disorder (ODD/CD) symptomatologies across informant and occasion of measurement. Psychological Medicine. 2002;32:39–53. doi: 10.1017/s0033291701004792. [DOI] [PubMed] [Google Scholar]
- Nauta MH, Scholing A, Rapee RM, Abbott M, Spence SH, Waters A. A parent-report measure of children’s anxiety: Psychometric properties and comparison with child-report in a clinic and normal sample. Behaviour Research and Therapy. 2004;42:813–839. doi: 10.1016/S0005-7967(03)00200-6. [DOI] [PubMed] [Google Scholar]
- Neale MC, Cardon LR. Methodology for genetic studies of twins and families. Boston: Kluwer Academic; 1992. [Google Scholar]
- Neumann A, Pappa I, Lahey BB, Verhulst FC, Medina-Gomez C, Jaddoe VW, … Tiemeier H. SNP heritability of a general psychopathology factor in children. Journal of the American Academy of Child and Adolescent Psychiatry. doi: 10.1016/j.jaac.2016.09.498. in press. [DOI] [PubMed] [Google Scholar]
- Newman DL, Moffitt TE, Caspi A, Silva PA. Comorbid mental disorders: Implications for treatment and sample selection. Journal of Abnormal Psychology. 1998;107:305–311. doi: 10.1037//0021-843x.107.2.305. [DOI] [PubMed] [Google Scholar]
- Newton-Howes G, Tyrer P, Anagnostakis K, Cooper S, Bowden-Jones O, Weaver T. The prevalence of personality disorder, its comorbidity with mental state disorders, and its clinical significance in community mental health teams. Social Psychiatry and Psychiatric Epidemiology. 2010;45:453–460. doi: 10.1007/s00127-009-0084-7. [DOI] [PubMed] [Google Scholar]
- Nigg JT. Temperament and developmental psychopathology. Journal of Child Psychology and Psychiatry. 2006;47:395–422. doi: 10.1111/j.1469-7610.2006.01612.x. [DOI] [PubMed] [Google Scholar]
- Nisbett RE, Wilson TD. Halo effect: Evidence for unconscious alternation of judgments. Journal of Personality and Social Psychology. 1977;35:250–256. [Google Scholar]
- Nolen-Hoeksema S, Watkins ER. A heuristic for developing transdiagnostic models of psychopathology. Perspectives on Psychological Science. 2011;6:589–609. doi: 10.1177/1745691611419672. [DOI] [PubMed] [Google Scholar]
- Noordhof A, Krueger RF, Ormel J, Oldehinkel AJ, Hartman CA. Integrating autism-related symptoms into the dimensional internalizing and externalizing model of psychopathology: The TRAILS Study. Journal of Abnormal Child Psychology. 2015;43:577–587. doi: 10.1007/s10802-014-9923-4. [DOI] [PubMed] [Google Scholar]
- Nottelmann ED, Jensen PS. Comorbidity of disorders in children and adolescents: Developmental Perspectives. In: Lahey BB, Kazdin AE, editors. Advances in Clinical Child Psychology. Vol. 17. New York: Plenum; 1995. pp. 109–155. [Google Scholar]
- Nunnally JC. Psychometric theory. 2. New York: McGraw-Hill; 1978. [Google Scholar]
- Ober C, Loisel DA, Gilad Y. Sex-specific genetic architecture of human disease. Nature Reviews Genetics. 2008;9:911–922. doi: 10.1038/nrg2415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Dushlaine C, Rossin L, Lee PH, Duncan L, Parikshak NN, Newhouse S … Pathway Anal Subgrp, P. Psychiatric genome-wide association study analyses implicate neuronal, immune and histone pathways. Nature Neuroscience. 2015;18:199–209. doi: 10.1038/nn.3922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogliari A, Spatola CA, Pesenti-Gritti P, Medda E, Penna L, Stazi MA, … Fagnani C. The role of genes and environment in shaping co-occurrence of DSM-IV defined anxiety dimensions among Italian twins aged 8–17. Journal of Anxiety Disorders. 2010;24:433–439. doi: 10.1016/j.janxdis.2010.02.008. [DOI] [PubMed] [Google Scholar]
- Okbay A, Baselmans BML, De Neve JE, Turley P, Nivard MG, Fontana MA, … Cesarini D. Genetic variants associated with subjective well-being, depressive symptoms, and neuroticism identified through genome-wide analyses. Nature Genetics. 2016;48:624–633. doi: 10.1038/ng.3552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olino TM, Dougherty LR, Bufferd SJ, Carlson GA, Klein DN. Testing models of psychopathology in preschool-aged children using a structured interview-based assessment. Journal of Abnormal Child Psychology. 2014;42:1201–1211. doi: 10.1007/s10802-014-9865-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orgiles M, Mendez X, Espada JP, Carballo JL, Piqueras JA. Anxiety disorder symptoms in children and adolescents: Differences by age and gender in a community sample. Revista De Psiquiatria Y Salud Mental. 2012;5:115–120. doi: 10.1016/j.rpsm.2012.01.005. [DOI] [PubMed] [Google Scholar]
- Ormel J, Jeronimus BF, Kotov R, Riese H, Bos EH, Hankin B, … Oldehinkel AJ. Neuroticism and common mental disorders: Meaning and utility of a complex relationship. Clinical Psychology Review. 2013;33:686–697. doi: 10.1016/j.cpr.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormel J, Raven D, van Oort F, Hartman CA, Reijneveld SA, Veenstra R, … Oldehinkel AJ. Mental health in Dutch adolescents: A TRAILS report on prevalence, severity, age of onset, continuity and co-morbidity of DSM disorders. Psychological Medicine. 2015;45:345–360. doi: 10.1017/S0033291714001469. [DOI] [PubMed] [Google Scholar]
- Parsch J, Ellegren H. The evolutionary causes and consequences of sex-biased gene expression. Nature Reviews Genetics. 2013;14:83–87. doi: 10.1038/nrg3376. [DOI] [PubMed] [Google Scholar]
- Patalay P, Fonagy P, Deighton J, Belsky J, Vostanis P, Wolpert M. A general psychopathology factor in early adolescence. British Journal of Psychiatry. 2015;207:15–22. doi: 10.1192/bjp.bp.114.149591. [DOI] [PubMed] [Google Scholar]
- Patrick CJ, Curtin JJ, Tellegen A. Development and validation of a brief form of the Multidimensional Personality Questionnaire. Psychological Assessment. 2002;14:150–163. doi: 10.1037//1040-3590.14.2.150. [DOI] [PubMed] [Google Scholar]
- Patterson GR, Stoolmiller M. Replications of a dual failure model for boys depressed mood. Journal of Consulting and Clinical Psychology. 1991;59:491–498. doi: 10.1037//0022-006x.59.4.491. [DOI] [PubMed] [Google Scholar]
- Paulus MP, Rogalsky C, Simmons A, Feinstein JS, Stein MB. Increased activation in the right insula during risk-taking decision making is related to harm avoidance and neuroticism. Neuroimage. 2003;19:1439–1448. doi: 10.1016/s1053-8119(03)00251-9. [DOI] [PubMed] [Google Scholar]
- Pesenti-Gritti P, Spatola CAM, Fagnani C, Ogliari A, Patriarca V, Stazi MA, Battaglia M. The co-occurrence between internalizing and externalizing behaviors. European Child and Adolescent Psychiatry. 2008;17:82–92. doi: 10.1007/s00787-007-0639-7. [DOI] [PubMed] [Google Scholar]
- Peterson DR. Behavior problems of middle childhood. Journal of Consulting Psychology. 1961;25:205–209. doi: 10.1037/h0038994. [DOI] [PubMed] [Google Scholar]
- Pettersson E, Anckarsater H, Gillberg C, Lichtenstein P. Different neurodevelopmental symptoms have a common genetic etiology. Journal of Child Psychology and Psychiatry. 2013;54:1356–1365. doi: 10.1111/jcpp.12113. [DOI] [PubMed] [Google Scholar]
- Pettersson E, Larsson H, Lichtenstein P. Common psychiatric disorders share the same genetic origin: A multivariate sibling study of the Swedish population. Molecular Psychiatry. doi: 10.1038/mp.2015.116. in press. [DOI] [PubMed] [Google Scholar]
- Pettersson E, Turkheimer E. Item selection, evaluation, and simple structure in personality data. Journal of Research in Personality. 2010;44:407–420. doi: 10.1016/j.jrp.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickles A, Angold A. Natural categories or fundamental dimensions: On carving nature at the joints and the rearticulation of psychopathology. Development and Psychopathology. 2003;15:529–551. doi: 10.1017/s0954579403000282. [DOI] [PubMed] [Google Scholar]
- Pine DS, Cohen P, Brook J. Adolescent fears as predictors of depression. Biological Psychiatry. 2001;50:721–724. doi: 10.1016/s0006-3223(01)01238-0. [DOI] [PubMed] [Google Scholar]
- Pirkola S, Saarni S, Suvisaari J, Elovainio M, Partonen T, Aalto AM, … Lonnqvist J. General health and quality-of-life measures in active, recent, and comorbid mental disorders: a population-based health 2000 study. Comprehensive Psychiatry. 2009;50:108–114. doi: 10.1016/j.comppsych.2008.06.003. [DOI] [PubMed] [Google Scholar]
- Plomin R, DeFries JC, Loehlin JC. Genotype-environment interaction and correlation in the analysis of human behavior. Psychological Bulletin. 1977;84:309–322. [PubMed] [Google Scholar]
- Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: A critical review of the literature and recommended remedies. Journal of Applied Psychology. 2003;88:879–903. doi: 10.1037/0021-9010.88.5.879. [DOI] [PubMed] [Google Scholar]
- Popper K. Conjectures and refutations. London: Routledge and Kegan Paul; 1963. [Google Scholar]
- Power RA, Wingenbach T, Cohen-Woods S, Uher R, Ng MY, Butler AW, … McGuffin P. Estimating the heritability of reporting stressful life events captured by common genetic variants. Psychological Medicine. 2013;43:1965–1971. doi: 10.1017/S0033291712002589. [DOI] [PubMed] [Google Scholar]
- Prisciandaro JJ, Roberts JE. A comparison of the predictive abilities of dimensional and categorical models of unipolar depression in the National Comorbidity Survey. Psychological Medicine. 2009;39:1087–1096. doi: 10.1017/S0033291708004522. [DOI] [PubMed] [Google Scholar]
- Purcell SM, Wray NR, Stone JL, Visscher PM, O’Donovan MC, Sullivan PF, … Scolnick EM. Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature. 2009;460:748–752. doi: 10.1038/nature08185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quay HC. Classification. In: Quay HC, Werry JS, editors. Psychopathological disorders of childhood. 3. New York: Wiley; 1986. pp. 1–42. [Google Scholar]
- Quay HC, Peterson DR. Behavior problem checklist. Champaign, IL: University of Illinois; 1967. [Google Scholar]
- Rapee RM, Bogels SM, van der Sluis CM, Craske MG, Ollendick T. Annual Research Review: Conceptualising functional impairment in children and adolescents. Journal of Child Psychology and Psychiatry. 2012;53:454–468. doi: 10.1111/j.1469-7610.2011.02479.x. [DOI] [PubMed] [Google Scholar]
- Reef J, Diamantopoulou S, van Meurs I, Verhulst F, van der Ende J. Child to adult continuities of psychopathology: a 24-year follow-up. Acta Psychiatrica Scandinavica. 2009;120:230–238. doi: 10.1111/j.1600-0447.2009.01422.x. [DOI] [PubMed] [Google Scholar]
- Reef J, van Meurs I, Verhulst FC, van der Ende J. Children’s problems predict adults’ DSM-IV disorders across 24 years. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:1117–1124. doi: 10.1016/j.jaac.2010.08.002. [DOI] [PubMed] [Google Scholar]
- Reinke WM, Ostrander R. Heterotyic and homotypic continuity: The moderating effects of age and gender. Journal of Abnormal Child Psychology. 2008;36:1109–1121. doi: 10.1007/s10802-008-9236-6. [DOI] [PubMed] [Google Scholar]
- Reise SP. The rediscovery of bifactor measurement models. Multivariate Behavioral Research. 2012;47:667–696. doi: 10.1080/00273171.2012.715555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberson-Nay R, Eaves LJ, Hettema JM, Kendler KS, Silberg JL. Childhood separation anxiety disorder and adult onset panic attacks share a common genetic diathesis. Depression and Anxiety. 2012;29:320–327. doi: 10.1002/da.21931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose AJ, Rudolph KD. A review of sex differences in peer relationship processes: Potential trade-offs for the emotional and behavioral development of girls and boys. Psychological Bulletin. 2006;132:98–131. doi: 10.1037/0033-2909.132.1.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe R, Costello EJ, Angold A, Copeland WE, Maughan B. Developmental pathways in oppositional defiant disorder and conduct disorder. Journal of Abnormal Psychology. 2010;119:726–738. doi: 10.1037/a0020798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roysamb E, Kendler KS, Tambs K, Orstavik RE, Neale MC, Aggen SH, … Reichborn-Kjennerud T. The joint structure of DSM-IV axis I and axis II disorders. Journal of Abnormal Psychology. 2011;120:198–209. doi: 10.1037/a0021660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, … Grant BF. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug and Alcohol Dependence. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruderfer DM, Fanous AH, Ripke S, McQuillin A, Amdur RL, Gejman PV … Cross-Disorder Working Grp P. Polygenic dissection of diagnosis and clinical dimensions of bipolar disorder and schizophrenia. Molecular Psychiatry. 2014;19:1017–1024. doi: 10.1038/mp.2013.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M. Gene-environment interdependence. Developmental Science. 2007a;10:12–18. doi: 10.1111/j.1467-7687.2007.00557.x. [DOI] [PubMed] [Google Scholar]
- Rutter M. Proceeding from observed correlation to causal inference: The use of natural experiments. Perspectives on Psychological Science. 2007b;2:377–395. doi: 10.1111/j.1745-6916.2007.00050.x. [DOI] [PubMed] [Google Scholar]
- Rutter M, Caspi A, Moffitt TE. Using sex differences in psychopathology to study causal mechanisms: Unifying issues and research strategies. Journal of Child Psychology and Psychiatry. 2003;44:1092–1115. doi: 10.1111/1469-7610.00194. [DOI] [PubMed] [Google Scholar]
- Rutter M, Kim-Cohen J, Maughan B. Continuities and discontinuities in psychopathology between childhood and adult life. Journal of Child Psychology and Psychiatry. 2006;47:276–295. doi: 10.1111/j.1469-7610.2006.01614.x. [DOI] [PubMed] [Google Scholar]
- Rutter M, Sroufe LA. Developmental psychopathology: Concepts and challenges. Development and Psychopathology. 2000;12:265–296. doi: 10.1017/s0954579400003023. [DOI] [PubMed] [Google Scholar]
- Saha S, Stedman TJ, Scott JG, McGrath JJ. The co-occurrence of common mental and physical disorders within Australian families: A national population-based study. Australian and New Zealand Journal of Psychiatry. 2013;47:754–761. doi: 10.1177/0004867413486841. [DOI] [PubMed] [Google Scholar]
- Sanders SJ, Ercan-Sencicek AG, Hus V, Luo R, Murtha MT, Moreno-De-Luca D, … State MW. Multiple recurrent de novo CNVs, including duplications of the 7q11.23 Williams syndrome Region, are strongly associated with autism. Neuron. 2011;70:863–885. doi: 10.1016/j.neuron.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanislow CA, Pine DS, Quinn KJ, Kozak MJ, Garvey MA, Heinssen RK, … Cuthbert BN. Developing constructs for psychopathology research: Research Domain Criteria. Journal of Abnormal Psychology. 2010;119:631–639. doi: 10.1037/a0020909. [DOI] [PubMed] [Google Scholar]
- Schneider DJ. Implicit personality theory: A review. Psychological Bulletin. 1973;79:294–309. doi: 10.1037/h0034496. [DOI] [PubMed] [Google Scholar]
- Scott KM, McGee MA, Browne MAO, Wells JE, Team NZMHSR. Mental disorder comorbidity in Te Rau Hinengaro: The New Zealand Mental Health Survey. Australian and New Zealand Journal of Psychiatry. 2006;40:875–881. doi: 10.1080/j.1440-1614.2006.01906.x. [DOI] [PubMed] [Google Scholar]
- Shanahan L, Copeland W, Costello EJ, Angold A. Specificity of putative psychosocial risk factors for psychiatric disorders in children and adolescents. Journal of Child Psychology and Psychiatry. 2008;49:34–42. doi: 10.1111/j.1469-7610.2007.01822.x. [DOI] [PubMed] [Google Scholar]
- Shankman SA, Klein DN, Lewinsohn PM, Seeley JR, Small JW. Family study of subthreshold psychopathology in a community sample. Psychological Medicine. 2008;38:187–198. doi: 10.1017/S0033291707001857. [DOI] [PubMed] [Google Scholar]
- Sharp C, Wright AGC, Fowler JC, Frueh BC, Allen JG, Oldham J, Clark LA. The Structure of Personality Pathology: Both General (‘g’) and Specific (‘s’) Factors? Journal of Abnormal Psychology. 2015;124:387–398. doi: 10.1037/abn0000033. [DOI] [PubMed] [Google Scholar]
- Sheeran T, Zimmerman M. Factor structure of the Psychiatric Diagnostic Screening Questionnaire (PDSQ), a screening questionnaire for DSM-IV axis I disorders. Journal of Behavior Therapy and Experimental Psychiatry. 2004;35:49–55. doi: 10.1016/j.jbtep.2004.02.002. [DOI] [PubMed] [Google Scholar]
- Sijtsema JJ, Verboom CE, Penninx BWJH, Verhulst FC, Ormel J. Psychopathology and academic performance, social well-being, and social preference at school: The TRAILS Study. Child Psychiatry and Human Development. 2014;45:273–284. doi: 10.1007/s10578-013-0399-1. [DOI] [PubMed] [Google Scholar]
- Silberg JL, Rutter M, Eaves L. Genetic and environmental influences on the temporal association between earlier anxiety and later depression in girls. Biological Psychiatry. 2001;49:1040–1049. doi: 10.1016/s0006-3223(01)01161-1. [DOI] [PubMed] [Google Scholar]
- Singh AL, Waldman ID. The etiology of associations between negative emotionality and childhood externalizing disorders. Journal of Abnormal Psychology. 2010;119:376–388. doi: 10.1037/a0019342. [DOI] [PubMed] [Google Scholar]
- Sivakumaran S, Agakov F, Theodoratou E, Prendergast JG, Zgaga L, Manolio T, … Campbell H. Abundant pleiotropy in human complex diseases and traits. American Journal of Human Genetics. 2011;89:607–618. doi: 10.1016/j.ajhg.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skapinakis P, Bellos S, Koupidis S, Grammatikopoulos I, Theodorakis PN, Mavreas V. Prevalence and sociodemographic associations of common mental disorders in a nationally representative sample of the general population of Greece. BMC Psychiatry. 2013;13 doi: 10.1186/1471-244x-13-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade T, Watson D. The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychological Medicine. 2006;36:1593–1600. doi: 10.1017/S0033291706008452. [DOI] [PubMed] [Google Scholar]
- Smoller JW. Disorders and borders: Psychiatric genetics and nosology. American Journal of Medical Genetics Part B-Neuropsychiatric Genetics. 2013;162:559–578. doi: 10.1002/ajmg.b.32174. [DOI] [PubMed] [Google Scholar]
- Smoller JW, Craddock N, Kendler K, Lee PH, Neale BM, Nurnberger JI … Psychiatric Genomics, C. Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet. 2013;381:1371–1379. doi: 10.1016/S0140-6736(12)62129-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song J, Bergen SE, Kuja-Halkola R, Larsson H, Landen M, Lichtenstein P. Bipolar disorder and its relation to major psychiatric disorders: A family-based study in the Swedish population. Bipolar Disorders. 2015;17:184–193. doi: 10.1111/bdi.12242. [DOI] [PubMed] [Google Scholar]
- Spatola CAM, Fagnani C, Pesenti-Gritti P, Ogliari A, Stazi MA, Battaglia M. A general population twin study of the CBCL/6–18 DSM-oriented scales. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:619–627. doi: 10.1097/CHI.0b013e3180335b12. [DOI] [PubMed] [Google Scholar]
- Spearman C. The proof and measurement of association between two things. American Journal of Psychology. 1904;15(72–101) [PubMed] [Google Scholar]
- Spence SH. Structure of anxiety symptoms among children: A confirmatory factor-analytic study. Journal of Abnormal Psychology. 1997;106:280–297. doi: 10.1037//0021-843x.106.2.280. [DOI] [PubMed] [Google Scholar]
- Stein MB, Simmons AN, Feinstein JS, Paulus MP. Increased amygdala and insula activation during emotion processing in anxiety-prone subjects. American Journal of Psychiatry. 2007;164:318–327. doi: 10.1176/ajp.2007.164.2.318. [DOI] [PubMed] [Google Scholar]
- Sterba SK, Copeland W, Egger HL, Costello EJ, Erkanli A, Angold A. Longitudinal dimensionality of adolescent psychopathology: testing the differentiation hypothesis. Journal of Child Psychology and Psychiatry. 2010;51:871–884. doi: 10.1111/j.1469-7610.2010.02234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterba SK, Egger HL, Angold A. Diagnostic specificity and nonspecificity in the dimensions of preschool psychopathology. Journal of Child Psychology and Psychiatry. 2007;48:1005–1013. doi: 10.1111/j.1469-7610.2007.01770.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stochl J, Khandaker GM, Lewis G, Perez J, Goodyer IM, Zammit S, … Jones PB. Mood, anxiety and psychotic phenomena measure a common psychopathological factor. Psychological Medicine. 2015;45:1483–1493. doi: 10.1017/S003329171400261X. [DOI] [PubMed] [Google Scholar]
- Strickland J, Keller J, Lavigne JV, Gouze K, Hopkins J, LeBailly S. The structure of psychopathology in a community sample of preschoolers. Journal of Abnormal Child Psychology. 2011;39:601–610. doi: 10.1007/s10802-011-9487-5. [DOI] [PubMed] [Google Scholar]
- Stringaris A, Goodman R. Mood lability and psychopathology in youth. Psychological Medicine. 2009;39:1237–1245. doi: 10.1017/S0033291708004662. [DOI] [PubMed] [Google Scholar]
- Stringaris A, Lewis G, Maughan B. Developmental pathways from childhood conduct problems to early adult depression: findings from the ALSPAC cohort. British Journal of Psychiatry. 2014;205:17–23. doi: 10.1192/bjp.bp.113.134221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbarao A, Rhee SH, Young SE, Ehringer MA, Corley RP, Hewitt JK. Common genetic and environmental influences on major depressive disorder and conduct disorder. Journal of Abnormal Child Psychology. 2008;36:433–444. doi: 10.1007/s10802-007-9189-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suvisaari J, Aalto-Setala T, Tuulio-Henriksson A, Harkanen T, Saarni SI, Perala J, … Lonnqvist J. Mental disorders in young adulthood. Psychological Medicine. 2009;39:287–299. doi: 10.1017/S0033291708003632. [DOI] [PubMed] [Google Scholar]
- Tackett JL. Evaluating models of the personality-psychopathology relationship in children and adolescents. Clinical Psychology Review. 2006;26:584–599. doi: 10.1016/j.cpr.2006.04.003. [DOI] [PubMed] [Google Scholar]
- Tackett JL, Lahey BB, Van Hulle CA, Waldman ID, Krueger RF, Rathouz PJ. Common genetic influences on negative emotionality and a general psychopathology factor in childhood and adolescence. Journal of Abnormal Psychology. 2013;122:1142–1153. doi: 10.1037/a0034151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tackett JL, Waldman ID, Van Hulle CA, Lahey BB. Shared genetic influences on negative emotionality and major depression/conduct disorder comorbidity. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:818–827. doi: 10.1016/j.jaac.2011.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarantino N, Tully EC, Garcia SE, South S, Iacono WG, McGue M. Genetic and environmental influences on affiliation with deviant peers during adolescence and early adulthood. Developmental Psychology. 2014;50:663–673. doi: 10.1037/a0034345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor J, Allan N, Mikolajewski AJ, Hart SA. Common genetic and nonshared environmental factors contribute to the association between socioemotional dispositions and the externalizing factor in children. Journal of Child Psychology and Psychiatry. 2013;54:67–76. doi: 10.1111/j.1469-7610.2012.02621.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorndike EL. A constant error in psychological ratings. Journal of Applied Psychology. 1920;4:25–29. [Google Scholar]
- Toplak ME, Sorge GB, Flora DB, Chen W, Banaschewski T, Buitelaar J, … Faraone SV. The hierarchical factor model of ADHD: invariant across age and national groupings? Journal of Child Psychology and Psychiatry. 2012;53:292–303. doi: 10.1111/j.1469-7610.2011.02500.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trosper SE, Whitton SW, Brown TA, Pincus DB. Understanding the latent structure of the emotional disorders in children and adolescents. Journal of Abnormal Child Psychology. 2012;40:621–632. doi: 10.1007/s10802-011-9582-7. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Verges A, Wood PK, Jahng S, Sher KJ. The structure of Diagnostic and Statistical Manual of Mental Disorders (4th Edition, Text Revision) personality disorder symptoms in a large national sample. Personality Disorders-Theory Research and Treatment. 2012;3:355–369. doi: 10.1037/a0027766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trumpf J, Margraf J, Vriends N, Meyer AH, Becker ES. Specific phobia predicts psychopathology in young women. Social Psychiatry and Psychiatric Epidemiology. 2010;45:1161–1166. doi: 10.1007/s00127-009-0159-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuang MT, Francis T, Minor K, Thomas A, Stone WS. Genetics of smoking and depression. Human Genetics. 2012;131:905–915. doi: 10.1007/s00439-012-1170-6. [DOI] [PubMed] [Google Scholar]
- Tuvblad C, Zheng M, Raine A, Baker LA. A common genetic factor explains the covariation among ADHD ODD and CD symptoms in 9–10 year oldboys and girls. Journal of Abnormal Child Psychology. 2009;37:153–167. doi: 10.1007/s10802-008-9278-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyrer P, Gunderson J, Lyons M, Tohen M. Extent of comorbidity between mental state and personality disorders. Journal of Personality Disorders. 1997;11:242–259. doi: 10.1521/pedi.1997.11.3.242. [DOI] [PubMed] [Google Scholar]
- Ullmann LP, Krasner L. A psychological approach to abnormal behavior. 2. New York: Prentice-Hall; 1975. [Google Scholar]
- Ullrich S, Coid J. Antisocial personality disorder: Co-morbid Axis I mental disorders and health service use among a national household population. Personality and Mental Health. 2009;3:151–164. [Google Scholar]
- Vaidyanathan U, Nelson LD, Patrick CJ. Clarifying domains of internalizing psychopathology using neurophysiology. Psychological Medicine. 2012;42:447–459. doi: 10.1017/S0033291711001528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaidyanathan U, Patrick CJ, Iacono WG. Patterns of comorbidity among mental disorders: A person-centered approach. Comprehensive Psychiatry. 2011;52:527–535. doi: 10.1016/j.comppsych.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaidyanathan U, Patrick CJ, Iacono WG. Examining the overlap between bipolar disorder, nonaffective psychosis, and common mental disorders using latent class analysis. Psychopathology. 2012;45:361–365. doi: 10.1159/000337265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Sluis S, Posthuma D, Nivard MG, Verhage M, Dolan CV. Power in GWAS: Lifting the curse of the clinical cut-off. Molecular Psychiatry. 2013;18:2–3. doi: 10.1038/mp.2012.65. [DOI] [PubMed] [Google Scholar]
- van der Sluis S, Verhage M, Posthuma D, Dolan CV. Phenotypic complexity, measurement bias, and poor phenotypic resolution contribute to the missing heritability problem in genetic association studies. PLOS One. 2010;5:e13929. doi: 10.1371/journal.pone.0013929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Hulle CA, Rodgers JL, D’Onofrio BM, Waldman ID, Lahey BB. Sex differences in the causes of self-reported adolescent delinquency. Journal of Abnormal Psychology. 2007;116:236–248. doi: 10.1037/0021-843X.116.2.236. [DOI] [PubMed] [Google Scholar]
- Van Oort FVA, Greaves-Lord K, Verhulst FC, Ormel J, Huizink AC. The developmental course of anxiety symptoms during adolescence: the TRAILS study. Journal of Child Psychology and Psychiatry. 2009;50:1209–1217. doi: 10.1111/j.1469-7610.2009.02092.x. [DOI] [PubMed] [Google Scholar]
- Van Os J, Verdoux H, Bijl R, Ravelli A. Psychosis as an extreme of continuous variation in dimensions of psychopathology. In: Gattaz WF, Häfner H, editors. Search for the causes of schizophrenia. Vol. 4. New York: Springer; 1999. pp. 56–79. [Google Scholar]
- Vasey MW, Harbaugh CN, Lonigan CJ, Phillips BM, Hankin BL, Willem L, Bijttebier P. Dimensions of temperament and depressive symptoms: Replicating a three-way interaction. Journal of Research in Personality. 2013;47:908–921. doi: 10.1016/j.jrp.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vesga-Lopez O, Schneier FR, Wang S, Heimberg RG, Liu SM, Hasin DS, Blanco C. Gender differences in generalized anxiety disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Journal of Clinical Psychiatry. 2008;69:1606–1616. [PMC free article] [PubMed] [Google Scholar]
- Vicente B, Saldivia S, de la Barra F, Kohn R, Pihan R, Valdivia M, … Melipillan R. Prevalence of child and adolescent mental disorders in Chile: a community epidemiological study. Journal of Child Psychology and Psychiatry. 2012;53:1026–1035. doi: 10.1111/j.1469-7610.2012.02566.x. [DOI] [PubMed] [Google Scholar]
- Vink JM, Bartels M, van Beijsterveldt TCEM, van Dongen J, van Beek JHDA, Distel MA, … Boomsma DI. Sex differences in genetic architecture of complex phenotypes? Plos One. 2012;7 doi: 10.1371/journal.pone.0047371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogt D, Vaughn R, Glickman ME, Schultz M, Drainoni ML, Elwy R, Eisen S. Gender differences in combat-related stressors and their association with postdeployment mental health in a nationally representative sample of US OEF/OIF veterans. Journal of Abnormal Psychology. 2011;120:797–806. doi: 10.1037/a0023452. [DOI] [PubMed] [Google Scholar]
- Vollebergh WAM, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders - The NEMESIS Study. Archives of General Psychiatry. 2001;58:597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- Waldman ID, Lilienfeld SO, Lahey BB. Toward construct validity in the childhood disruptive behavior disorders: Classification and diagnosis in DSM-IV and beyond. In: Ollendick TH, Prinz RJ, editors. Advances in Clinical Child Psychology. Vol. 17. New York: Plenum; 1995. pp. 323–363. [Google Scholar]
- Waldman ID, Poore H, Van Hulle C, Rathouz PJ, Lahey BB. External validity of a hierarchical dimensional model of child and adolescent psychopathology: Tests using confirmatory factor analyses and multivariate behavior genetic analyses. Journal of Abnormal Psychopathology. doi: 10.1037/abn0000183. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldman ID, Rhee SH, Levy F, Hay DA. Causes of the overlap among symptoms of ADHD, oppositional defiant disorder, and conduct disorder. In: Levy F, Hay DA, editors. Attention, genes, and ADHD. New York: Brunner-Routledge; 2001. pp. 115–138. [Google Scholar]
- Waszczuk MA, Zavos HM, Gregory AM, Eley TC. The stability and change of etiological influences on depression, anxiety symptoms and their co-occurrence across adolescence and young adulthood. Psychological Medicine. 2016;46:161–175. doi: 10.1017/S0033291715001634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wells JE, Browne MAO, Scott KM, McGee MA, Baxter J, Kokaua J, Team NZMHSR. Prevalence, interference with life and severity of 12 month DSM-IV disorders in Te Rau Hinengaro: The New Zealand Mental Health Survey. Australian and New Zealand Journal of Psychiatry. 2006;40:845–854. doi: 10.1080/j.1440-1614.2006.01903.x. [DOI] [PubMed] [Google Scholar]
- Wertz J, Zavos H, Matthews T, Harvey K, Hunt A, Pariante CN, Arseneault L. Why some children with externalising problems develop internalising symptoms: testing two pathways in a genetically sensitive cohort study. Journal of Child Psychology and Psychiatry. doi: 10.1111/jcpp.12333. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitbeck LB, Johnson KD, Hoyt DR, Walls ML. Prevalence and comorbidity of mental disorders among American Indian children in the Northern Midwest. Journal of Adolescent Health. 2006;39:427–434. doi: 10.1016/j.jadohealth.2006.01.004. [DOI] [PubMed] [Google Scholar]
- Wickrama KAS, Conger RD, Lorenz FO, Martin M. Continuity and discontinuity of depressed mood from late adolescence to young adulthood: The mediating and stabilizing roles of young adults’ socioeconomic attainment. Journal of Adolescence. 2012;35:648–658. doi: 10.1016/j.adolescence.2011.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widiger TA. Personality and psychopathology. World Psychiatry. 2011;10:103–106. doi: 10.1002/j.2051-5545.2011.tb00024.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willcutt EG, Nigg JT, Pennington BF, Solanto MV, Rohde LA, Tannock R, … Lahey BB. Validity of DSM-IV attention deficit/hyperactivity disorder symptom dimensions and subtypes. Journal of Abnormal Psychology. 2012;121:991–1010. doi: 10.1037/a0027347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams HJ, Norton N, Dwyer S, Moskvina V, Nikolov I, Carroll L … Group. Fine mapping of ZNF804A and genome-wide significant evidence for its involvement in schizophrenia and bipolar disorder. Molecular Psychiatry. 2011;16:429–441. doi: 10.1038/mp.2010.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson KA, Hayward C. A prospective evaluation of agoraphobia and depression symptoms following panic attacks in a community sample of adolescents. Journal of Anxiety Disorders. 2005;19:87–103. doi: 10.1016/j.janxdis.2003.11.001. [DOI] [PubMed] [Google Scholar]
- Wittchen HU, Nelson CB, Lachner G. Prevalence of mental disorders and psychosocial impairments in adolescents and young adults. Psychological Medicine. 1998;28:109–126. doi: 10.1017/s0033291797005928. [DOI] [PubMed] [Google Scholar]
- Wolf EJ, Miller MW, Krueger RF, Lyons MJ, Tsuang MT, Koenen KC. Posttraumatic stress disorder and the genetic structure of comorbidity. Journal of Abnormal Psychology. 2010;119:320–330. doi: 10.1037/a0019035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Krueger RF, Hobbs MJ, Markon KE, Eaton NR, Slade T. The structure of psychopathology: Toward an expanded quantitative empirical model. Journal of Abnormal Psychology. 2013;122:281–294. doi: 10.1037/a0030133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Simms LJ. A metastructural model of mental disorders and pathological personality traits. Psychological Medicine. 2015 doi: 10.1017/S0033291715000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Thomas KM, Hopwood CJ, Markon KE, Pincus AL, Krueger RF. The hierarchical structure of DSM-5 pathological personality traits. Journal of Abnormal Psychology. 2012;121:951–957. doi: 10.1037/a0027669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng H, Van Hulle CA, Rathouz PJ. Comparing alternative biometric models with and without gene-by-measured environment interaction in behavior genetic designs: Statistical operating characteristics. Behavior Genetics. 2015;45:480–491. doi: 10.1007/s10519-015-9710-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman M, Mattia JI. A self-report scale to help make psychiatric diagnoses: The psychiatric diagnostic screening questionnaire. Archives of General Psychiatry. 2001;58:787–794. doi: 10.1001/archpsyc.58.8.787. [DOI] [PubMed] [Google Scholar]
- Zoccolillo M, Pickles A, Quinton D, Rutter M. The outcome of childhood conduct disorder: Implications for defining adult personality disorder and conduct disorder. Psychological Medicine. 1992;22:971–986. doi: 10.1017/s003329170003854x. [DOI] [PubMed] [Google Scholar]
- Zuckerman M, Kuhlman DM, Teta P, Joireman J, Kraft M. A comparison of three structural models of personality: The big three, the big five, and the alternative five. Journal of Personality and Social Psychology. 1993;65:757–768. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.