Abstract
Objective
Historically marginalized groups are likely to be exposed to social adversity, which predicts important mental health outcomes (e.g., depression). Despite the well-established relationship between adversity and poor health, few studies have examined how adversity differentially predicts mental health among people living with multiple, co-occurring marginalized identities or statuses. The current study fills this gap by examining whether relationships between social adversity and depressive symptoms differed between those living with or without a stigmatized disease (i.e., HIV) and/or marginalized racial/ethnic identity (i.e., African American).
Method
A community sample of men and women (n = 149) completed questionnaires assessing demographics and depressive symptoms. Additionally, a composite index of social adversity was derived from measures of perceived discrimination, socioeconomic status, financial restriction to receiving medical care, and perceived neighborhood characteristics. Multiple regression was used to test whether relationships between adversity and depressive symptoms differed as a function of HIV-status and racial/ethnic identity.
Results
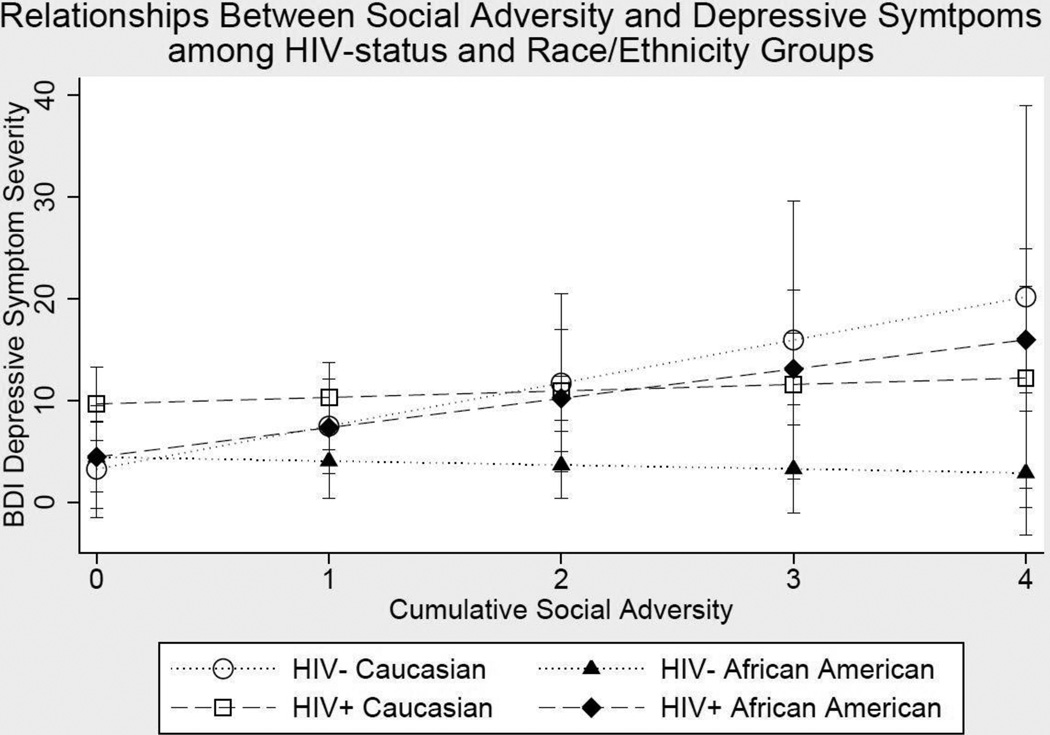
A significant three-way interaction between social adversity, HIV-status, and racial/ethnic identity indicated that there was a direct relationship between adversity and depressive symptoms for HIV-positive (HIV+) African Americans but not for HIV-negative (HIV-) African Americans, HIV+ Caucasians, or HIV- Caucasians. Further, HIV+ African Americans evidenced a significantly greater relationship between adversity and depressive symptoms, as compared to HIV- African Americans but not as compared to other groups.
Conclusions
The findings suggest that HIV+ African Americans may be at risk for higher depressive symptoms amidst adversity, highlighting the importance of evaluating intersectional identities/statuses in the context of mental health.
Keywords: social adversity, race/ethnicity, HIV/AIDS, depressive symptoms, discrimination, intersectionality
Social marginalization and disadvantage are associated with marked health disparities. Historically marginalized groups (e.g., racial/ethnic minorities) are more likely to be exposed to adversity (e.g., discrimination, financial barriers to receiving medical care), making them particularly vulnerable to poor health outcomes, compared to mainstream groups (Bynum, Burton & Best, 2007; Geronimus, Hicken, Keene & Bound, 2006; Miller & Taylor, 2012; Wight, Botticello & Aneshensel, 2006). Research has shown that repeated exposure to adversity builds over time (e.g., Steptoe & Marmot, 2003) and results in myriad negative health outcomes, including depression (Turner & Lloyd, 2004). Despite the established relationship between social adversity and negative mental health sequelae, few studies have examined how adversity differentially predicts health outcomes among people with multiple, co-occurring marginalized identities or statuses. As such, the primary aim of this study was to examine how social adversity is differentially related to depressive symptoms among those living with or without a stigmatized chronic disease (i.e., HIV) and/or marginalized racial/ethnic identity (i.e., African American).
The “weathering hypothesis” (Geronimus, 1992; Geronimus, Hicken, Keene & Bound, 2006) posits that confronting multiple sources of stress will confer risk for poorer health over time, including increased depressive symptoms. Based on this framework, researchers have aggregated multiple sources of stress into a composite index to assess the relationship between adversity and health (Steptoe & Marmot, 2003; Troxel, Matthews, Bromberger, & Sutton-Tyrrell, 2003; Toussaint, Shield, Dorn, & Slavich, 2014). Although several psychosocial determinants of health (e.g., discrimination, socioeconomic status) have been identified from theory and research, it is common for studies to investigate these determinants separately rather than exploring the cumulative burden of stress exposure. However, utilizing a composite index of adversity allows for a sophisticated analysis of stressors that commonly co-occur.
Research has shown that an index of cumulative stress was related to psychological health morbidity, including higher levels of depressive symptoms and poorer quality of life (Steptoe & Marmot, 2003). These findings provide a multifaceted perspective on how a global measure of strain is related to important health-related outcomes. Further, findings from another study (Troxel, Matthews, Bromberger, & Sutton-Tyrrell, 2003) demonstrated that a composite index of stress, which included a measure of racial/ethnic discrimination, was positively associated with cardiovascular risk among African American but not among Caucasian women, perhaps due to their double minority status of being African American and female. Thus, there is clear importance in examining the relationship between adversity and health for those living with multiple marginalized identities or statuses.
Living with a chronic disease such as HIV can be stressful—it is often stigmatized, and the disease necessitates considerable adjustment (e.g., Hays et al., 2000; Hermann et al., 2013). Several studies have characterized the HIV-positive (HIV+) population as a group that experiences frequent social stress related to how others perceive their HIV status (see Mahajan et al., 2008 for review), which predicts poorer quality of life and higher depressive symptoms (Simbayi et al., 2007; Holzemer et al., 2009). Depression is an important outcome to assess in HIV+ adults, given that it is associated with HIV illness progression and HIV-associated mortality (Leserman, 2008; Rabkin, 2008). Indeed, longitudinal research has demonstrated that depressive symptoms predict an elevated risk for progressing to AIDS, but disease progression did not predict later depression (Leserman et al., 2002; Leserman et al., 1999). Additionally, the prevalence of major depression is almost twice as high among HIV+ adults, as compared to HIV-negative (HIV-) controls (for meta-analysis, see Ciesla & Roberts, 2001).
HIV disproportionately affects African Americans in the U.S., as African Americans represent over 50% of the HIV+ population but only 14% of the U.S. population at-large (CDC, 2014). As such, there is a need to assess whether HIV+ African Americans are particularly vulnerable for poor mental health outcomes due to the intersecting identities of living as a racial/ethnic minority with a stigmatized disease. African Americans report greater exposure to several types of stressors, including major life events, witnessed violence, traumatic news, and death events (Turner & Lloyd, 2004; Myers, 2009; Myers et al., 2015; Zimmerman & Messner, 2013). Research also demonstrates that racial discrimination robustly predicts adverse physical and mental health outcomes among African Americans (e.g., Fang & Myers, 2001; Pascoe & Smart Richman, 2009; Williams & Mohammed, 2009; Williams, Yu, Jackson, & Anderson, 1997). Notably, however, many African Americans evidence resiliency in the face of discrimination, owing to factors such as social support, active coping, and group identification (see Pascoe & Smart Richman, 2009). These findings demonstrate the disproportionate exposure to many types of stressors that African Americans experience.
The Current Study
The goal of the current study was to investigate the relationship between social adversity and depressive symptoms among HIV+ and HIV- adults who self-identify as either African American or Caucasian using a diatheses-stress model. Theories of diathesis-stress in depression have posited that a diathesis (i.e., pre-existing vulnerability) that is activated by stress (e.g., social adversity) confers risk for depression (Monroe & Simons, 1991). Diatheses may be biological, but they may also be conceptualized as social (e.g., stigmatized social identity). In some cases, diatheses may represent a combination of social and biological vulnerability (e.g., HIV+ status).
In the current study, HIV status and race/ethnicity are conceptualized as quasi-continuous diatheses (Monroe & Simons, 1991). Specifically, it is posited that HIV+ African Americans will evidence a “high loading” onto the diathesis, HIV+ Caucasians and HIV- African Americans will evidence a lower loading onto the diathesis, and HIV- Caucasians will evidence the lowest loading onto the diathesis (see Electronic Supplementary Materials for a conceptual diagram). In this model, HIV+ status and African American race/ethnicity, whether alone or in combination, would not be sufficient to result in higher depressive symptoms. Rather, exposure to social adversity is theorized to predict depressive symptoms at differential rates among the four aforementioned groups. Specifically, it is hypothesized that those with the lowest diathetic loading (i.e., HIV- Caucasians) are require a greater amount of adversity to evidence high levels of depressive symptoms, whereas those with the highest diathetic loading (i.e., HIV+ African Americans) require a lower amount of adversity to evidence comparable levels of depressive symptoms.
An index of social adversity was derived to assess the following hypotheses: 1) The strength of the relationship between social adversity and depressive symptoms would vary as a function of HIV-status and self-identified race/ethnicity; 2) All groups would evidence a positive relationship between adversity and depressive symptoms; 3) HIV+ African Americans would evidence the strongest relationship between adversity and depressive symptoms, as compared to all other groups; 4) HIV- African Americans and HIV+ Caucasians would evidence a stronger relationship between adversity and depressive symptoms as compared to HIV- Caucasians.
Method
Participants
Participants included 149 adults who were either HIV+ (n = 93; confirmed by serologic testing) or HIV- (n = 56), and they participated in a larger study examining the effects of HIV and psychosocial factors on neurocognitive functioning among African American and Caucasian individuals (NIMH K23 MH095661; PI: A.D.T.). HIV+ participants were recruited from local HIV clinics in the Greater Los Angeles area. HIV- participants were recruited from flyers posted at local medical care clinics as well as advertisements on the Internet and participant word of mouth. Participants were included in the study if they were over the age of 18, reported English as their primary language, self-identified as African American or Caucasian, and were able to provide informed consent. Those who had current abuse or dependence of alcohol, marijuana, opiates, cocaine or amphetamines, or were found to have past stimulant abuse/dependence were excluded. Participants were also excluded if they evidenced a current or past diagnosis of a psychotic-spectrum disorder. The aforementioned inclusion and exclusion criteria for participation was determined from those established by the parent study1. Current illicit drug use was confirmed via urine toxicology. HIV+ African Americans were oversampled in the parent study, which explains the larger number of HIV+ African Americans in the current study. There were four groups: HIV+ African Americans (n =64); HIV- African Americans (n = 33); HIV+ Caucasians (n =29); and HIV- Caucasians (n = 23).
Procedure
Eligible participants who provided informed consent completed questionnaires and interviews regarding medical history, demographic information, and psychosocial characteristics with a research assistant in a controlled setting. Past substance abuse, substance dependence, and major depressive disorder were evaluated using an abbreviated version of the SCID-IV (Spitzer, Williams, Gibbons, & First, 1995). Medical comorbidities were assessed from an interview, which assessed history of several chronic medical conditions (e.g., diabetes, cancer, hypertension). Age, gender identity, racial/ethnic identity, medical comorbidities, and marital status were determined via self-report. Additionally, participants underwent measurements of resting blood pressure, height, and weight. Body mass index (BMI) was calculated for each participant using the following formula: (weight in kilograms) / (height in meters × height in meters). Finally, HIV+ participants provided HIV-specific disease information (e.g., nadir CD4 count) and underwent a blood draw, which was used to assess serologic indicators of HIV illness (i.e., viral load, CD4 T-cell count). All procedures were approved by the University of California, Los Angeles (UCLA) Institutional Review Board (IRB).
Measures
Social Adversity
A composite index of social adversity was developed using five indicators of social disadvantage (i.e., racial/ethnic discrimination, socioeconomic status, financial restriction to needed care, neighborhood socioeconomic status (SES) during childhood, current neighborhood SES, current personal SES). These areas were selected based on research that demonstrates their independent associations with adverse mental health (e.g., Haines, Beggs, & Hurlbert, 2011; Hazel, Hammen, Brennan, & Najman, 2008; Karlsen & Nazroo, 2002; Pascoe & Smart Richman, 2009; Ross, 2000). Based on published methodology (Troxel, Matthews, Bromberger, & Sutton-Tyrrell, 2003), each indicator was dichotomized at the top 20–30% of the distribution, except for financial restriction to needed care, which was dichotomized at the top 13% (based on its distribution). Social adversity scores were derived from the sum of these dichotomous values and ranged from 0–5, with higher scores representing greater amounts of adversity. Of the full sample, 34.1%, 34.1%, 18.8%, 8.7%, 3.6%, and 0.7% of participants had scores of 0, 1, 2, 3, 4, and 5, respectively. For this reason, scores of 4 and 5 were combined into one group. As a result, social adversity was entered as a continuous predictor, ranging from 0 to 4 in all subsequent analyses.
Perceived racial/ethnic discrimination
Perceived discrimination was assessed using the Perceived Ethnic Discrimination Questionnaire (PED-Q; Contrada et al., 2001), a 17-item questionnaire that assess the frequency and intensity of participant-reported experiences of discrimination based on his or her self-identified race/ethnicity. Items are scored on a Likert scale from 1–5, with higher scores representing higher amounts of perceived racial/ethnic discrimination. This questionnaire has established good reliability (current α = .80) and validity in assessing perceived racial/ethnic discrimination (Brondolo et al., 2005). There are no established cut-offs from the PEDQ; thus, this variable was dichotomized so that the top quartile of the total sample (25.2% of the sample reported a total score of 35 or above) represented one group, which was coded as 1. The other group was comprised of participants who reported total scores of 34 or below (coded as 0).
Socioeconomic status
The Hollingshead Index of Social Status (i.e., a weighted average of years of education, current or longest held occupation, and total household income of the participant) was used to assess current personal SES. Years of education were based upon self-report from the participant and occupation was coded using the Hollingshead Index (Hollingshead, 1975). For married participants, the spouse’s education and occupation were also used to compute the score. The Hollingshead Index is a reliable and valid measure of social status (Cirino et al., 2002), and it has been used in a racially diverse sample of HIV+ adults (Arentoft et al., 2015). Hollingshead scores range from 0–4, with higher scores representing higher levels of SES. Of the total sample, 4.8%, 14.3%, 31.3%, 38.8%, and 10.9% were given a Hollingshead Index score of 0, 1, 2, 3, and 4, respectively. This measure was dichotomized by assigning a code of 1 to participants with a Hollingshead Index of either 0 or 1 and assigning a code of 0 to participants with an Index score of 2, 3, or 4.
Financial restriction to needed care
Financial restriction to receiving medical care was assessed through a single-item measure, which asked whether the participant had ever “not received medical care because of financial problems.” This method has been used in previous research (e.g., Bernard, Selden, & Yeh, 2016). The response format in the current study was a dichotomous “yes or no.” Of the sample, 12.9% reported yes and were coded as 1, whereas 86.4% of participants reported no and were coded as 0.
Perceived neighborhood characteristics
Subjective reports of neighborhood characteristics are related to self-rated health (Weden, Carpiano, & Robert, 2008). In the current study, participants rated the economic status of their neighborhood communities as a child and as an adult, respectively. Neighborhood SES during childhood was assessed retrospectively through a single item. Participants were asked to rate the SES of their neighborhood while growing up as either “low income/poor”, “middle class”, “upper-middle class”, or “wealthy.” Of the sample, 24.5%, 57.1%, 14.3%, and 4.1% of participants reported their childhood neighborhood SES to be “low income poor”, “middle class”, “upper-middle class”, and “wealthy”, respectively. Those who reported their community SES during childhood to be “low income/poor” were assigned a code of 1, and all other participants were assigned a code of 0. Participants were also asked to rate the SES of their current neighborhood through a single item, using the aforementioned anchors. Of the sample, 31.5% of participants reported their neighborhood SES to be “low income poor”, 48.6% reported “middle class”, 15.8% reported “upper-middle class”, and 4.1% reported “wealthy.” Those who reported their neighborhood SES to be “low income/poor” were assigned a code of 1, and all other participants were assigned a code of 0.
Depressive symptoms
The Beck Depression Inventory-II (BDI; Beck, Steer, & Brown, 1996) was used to assess depressive symptoms. Participants completed 21 items on a scale from 0–3, indicating their mood during the past two weeks. The BDI assesses both cognitive-affective symptoms of depression (e.g., pessimism) and somatic symptoms of depression (e.g., lack of appetite). The BDI total score2 ranges from 0–63, with higher scores indicating more depressive symptoms. The BDI has demonstrated excellent validity and reliability (current α = .91), and it has been widely used to measure depressive symptoms among people living with HIV (e.g., Berger-Greenstein et al., 2007; Castellon et al., 2001; Gibbie et al., 2006; Ransom et al., 2008).
Analytic Strategy
Eleven participants were missing data on one or more of the variables that was used to derive the index of social adversity or were missing a total score for depressive symptoms. Thus, these participants were excluded from all analyses, and the analytic sample consisted of 62 HIV+ African Americans, 26 HIV- African Americans, 32 HIV+ Caucasians, and 18 HIV- Caucasians.
Control variables
Research has demonstrated that age (e.g., Kessler & Bromet, 2013), gender (e.g., Steel et a., 2015; Su et al., 2016), past substance abuse and dependence (Davis, Uezato, Newell, & Frazier, 2008), medical comorbidities (Moussayi et al., 2007), and marital status (Sbarra, Emery, Beam & Ocker, 2014; Schaan, 2013; Strine, et al., 2015) are uniquely related to depressive symptoms. Accordingly, these variables were included as covariates in all subsequent analyses. Age was analyzed as a continuous variable, whereas gender, past substance abuse and dependence, medical comorbidities, and marital status were analyzed as categorical variables. Male gender, no past diagnosis of substance abuse/dependence, no medical comorbidities, and “single/never married” served as referent groups, respectively.
Analytic plan
Chi-square tests, independent samples t-tests, and ANOVAs were used to evaluate group differences in demographic and medical characteristics. In the case of a significant omnibus group difference among the four groups, post-hoc tests (i.e., Tukey’s HSD) were conducted to evaluate pairwise differences. Self-identified race/ethnicity was operationalized using a dummy code (Caucasian = 0, African American = 1). Similarly, HIV status was dummy coded (HIV- = 0, HIV+ = 1). For Hypothesis 1, a hierarchical multiple regression was conducted using the following steps: 1) age, gender, past substance abuse, past substance dependence, medical comorbidities, and marital status as control variables; 2) social adversity, race, and HIV status; 3) all two-way interactions between social adversity, race, and HIV status; 4) the three-way interaction between social adversity, race, and HIV status. To evaluate Hypothesis 2, simple slopes were estimated for the relationships between social adversity and depressive symptoms for all four groups (e.g., Aiken & West, 1991). To evaluate Hypotheses 3 and 4, simple slope analyses were conducted to test differences between the four simple slopes (Dawson & Richter, 2006).
Results
Sample Characteristics
Groups did not differ with regard to gender, past history of substance abuse or dependence, medical comorbidities, marital status, or history of past major depressive disorder (p’s > .05). Additionally, groups did not differ on BMI, systolic blood pressure, diastolic blood pressure, or working status (p’s > .05). Groups differed on age (F(3, 134) = 4.33, p = .006); specifically, HIV+ African Americans and HIV+ Caucasians were older as compared HIV- African Americans. HIV- Caucasians did not differ in age from any other group. The groups also differed in years of education (F(1,34) = 11.68, p < .001). Specifically, HIV+ African Americans evidenced significantly fewer years of education, as compared to HIV+ Caucasians and HIV- Caucasians; additionally, HIV- African Americans evidenced fewer years of education as compared to HIV+ Caucasians. There were no differences between the proportion of African-American and Caucasian participants who were HIV+ (χ2 = 0.61, p = .434). Additionally, there were no differences between HIV+ African Americans and HIV+ Caucasians with regard to CD4 T cell count, HIV viral load, and CD4 to CD8 ratio (p’s > .261). Table 1 provides the sample characteristics among HIV-status and race/ethnicity groups (also see Electronic Supplementary Materials for additional descriptive statistics).
Table 1.
Descriptive statistics for participants (n = 138) who were included in the analytic sample
| HIV+ African Americans (n = 62) |
HIV+ Caucasians (n = 32) |
HIV- African Americans (n = 26) |
HIV- Caucasians (n = 18) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group A | Group B | Group C | Group D | |||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | F | p | Tukey’s HSD | ||
| Age (in years) | 52.77 | 10.53 | 55.00 | 11.93 | 44.81 | 13.85 | 48.00 | 13.75 | 4.33 | 0.006 | A & B > C | |
| Years of Education | 12.87 | 1.68 | 15.13 | 2.14 | 13.54 | 2.08 | 15.11 | 2.68 | 11.68 | < .001 | A < B & D; C < B | |
| n | % | n | % | n | % | n | % | χ2 | p | |||
| Gender | 5.85 | 0.054 | ||||||||||
| Male | 42 | 67.74% | 30 | 93.75% | 15 | 57.69% | 12 | 6.67% | ||||
| Female | 17 | 27.42% | 1 | 3.13% | 11 | 42.31% | 6 | 3.33% | ||||
| Transgender | 3 | 4.84% | 1 | 3.13% | 0 | - | 0 | - | ||||
| Past Substance Abuse | 0.71 | 0.398 | ||||||||||
| Yes | 28 | 45.16% | 17 | 53.13% | 6 | 23.08% | 6 | 33.33% | ||||
| No | 34 | 54.84% | 15 | 46.87% | 20 | 76.92% | 12 | 66.67% | ||||
|
Past Substance Dependence |
1.08 | 0.299 | ||||||||||
| Yes | 29 | 46.77% | 13 | 40.63% | 7 | 26.92% | 3 | 16.67% | ||||
| No | 33 | 53.23% | 19 | 59.37% | 19 | 73.08% | 15 | 83.33% | ||||
| Medical Comorbidities | 3.91 | 0.418 | ||||||||||
| 0 | 20 | 32.26% | 4 | 12.50% | 18 | 69.23% | 15 | 83.33% | ||||
| 1 | 16 | 25.81% | 8 | 12.90% | 6 | 23.08% | 1 | 5.56% | ||||
| 2 | 15 | 24.19% | 8 | 12.90% | 2 | 7.69% | 2 | 11.11% | ||||
| 3 | 7 | 11.29% | 6 | 18.75% | 0 | - | 0 | - | ||||
| 4+ | 4 | 6.45% | 6 | 18.75% | 0 | - | 0 | - | ||||
| Marital Status | 4.36 | 0.499 | ||||||||||
| Never Married/Single | 37 | 59.68% | 15 | 46.87% | 16 | 61.54% | 11 | 61.11% | ||||
| Currently Married | ||||||||||||
| Domestic Partnership | 2 | 3.23% | 4 | 12.50% | 4 | 15.38% | 1 | 5.56% | ||||
| Legally Separated | 5 | 8.06% | 6 | 18.75% | 1 | 3.85% | 1 | 5.56% | ||||
| Divorced | 4 | 6.45% | 1 | 3.13% | 1 | 3.85% | 0 | - | ||||
| Widowed | 8 | 12.90% | 4 | 12.50% | 4 | 15.38% | 5 | 27.77% | ||||
| Disability/Welfare | 6 | 9.68% | 2 | 6.25% | 0 | - | 0 | - | ||||
| Homemaker | 37 | 59.68% | 15 | 46.87% | 16 | 61.54% | 11 | 61.11% | ||||
|
Past Major Depressive Disorder |
3.55 | 0.060 | ||||||||||
| Yes | 10 | 16.13% | 10 | 31.25% | 3 | 11.54% | 4 | 22.22% | ||||
| No | 52 | 83.87% | 22 | 68.75% | 23 | 88.46% | 14 | 77.78% | ||||
Groups differed on the index of social adversity (F(3, 34) = 9.41, p < .001), with HIV+ African Americans and HIV- African Americans evidencing higher scores as compared to HIV+ Caucasians and HIV- Caucasians. When comparing race/ethnicity groups (regardless of HIV-status) on the individual indices of social adversity, results further showed that African Americans reported significantly higher discrimination (t(136) = 3.11, p = .002), lower neighborhood SES during childhood (t(136) = 5.09, p < .001), lower current neighborhood SES (t(136) = 3.06, p = .003), and lower current personal SES (t(136) = 4.56, p <.001). Race/ethnicity groups did not differ, however, on the measure of financial restriction to needed care (χ2 = 0.64, p = .424).
Finally, HIV+ African Americans (M = 8.92, SD = 8.86), HIV- African Americans (M = 3.23, SD = 3.85), HIV+ Caucasians (M = 10.28, SD = 7.27), and HIV- Caucasians (M = 5.06, SD = 6.15) reported minimal to low levels of total BDI depressive symptom severity.
Hypothesis 1: Three-way Interaction Between Adversity, Race, and HIV-status on Depressive Symptoms
Multiple regression analysis was used to test the three-way interaction between social adversity, race/ethnicity, and HIV-status on depressive symptoms, controlling for age, gender, past substance abuse, past substance dependence, medical comorbidities, and marital status. Results from the regression are presented in Table 2. The final step of the hierarchical regression was statistically significant (ΔR2 = .025, F(1, 116) = 3.94, p = .049), indicating a significant three-way interaction term. These results indicate that the relationships between social adversity and depressive symptoms differ as a function of HIV-status and racial/ethnic identification, controlling for important demographic and medical characteristics. Simple slopes analyses below provide a full evaluation of this significant three-way interaction.
Table 2.
Analysis of BDI-depressive symptoms as a function of social adversity, HIV-status, and racial/ethnic identity
| Step | Predictor | Model R2 | ΔR2 | F | p-value | b (se) | p-value |
|---|---|---|---|---|---|---|---|
| 1 | .118 | -- | 1.16 | .303 | -- | -- | |
| Age | -- | -- | -- | -- | -0.08 (0.06) | .196 | |
| Gender (female vs. male) | -- | -- | -- | -- | -0.46 (1.82) | .799 | |
| Gender (transgender vs. male) | -- | -- | -- | -- | 1.86 (4.23) | .660 | |
| Substance Abuse (past dx vs. no past dx) | -- | -- | -- | -- | 0.06 (1.46) | .968 | |
| Substance Dependence (past dx vs. no past dx) | -- | -- | -- | -- | 1.56 (1.49) | .300 | |
| Medical Comorbidities (1 vs. 0) | -- | -- | -- | -- | 1.05 (1.98) | .918 | |
| Medical Comorbidities (2 vs. 0) | -- | -- | -- | -- | 3.19 (2.06) | .125 | |
| Medical Comorbidities (3 vs. 0) | -- | -- | -- | -- | 1.78 (2.72) | .513 | |
| Medical Comorbidities (4+ vs. 0) | -- | -- | -- | -- | 0.95 (3.05) | .755 | |
| Marital Status (currently married vs. never married) | -- | -- | -- | -- | -1.33 (2.55) | .603 | |
| Marital Status (domestic partnership vs. never married) | -- | -- | -- | -- | 0.29 (2.42) | .904 | |
| Marital Status (separated vs. never married) | -- | -- | -- | -- | -2.69 (3.47) | .440 | |
| Marital Status (divorced vs. never married) | -- | -- | -- | -- | 2.03 (2.22) | .363 | |
| Marital Status (widowed vs. never married) | -- | -- | -- | -- | 1.95 (3.21) | .545 | |
| 2 | .220 | .102 | 5.21 | .002* | -- | -- | |
| Social Adversity | -- | -- | -- | -- | 4.23 (2.67) | .116 | |
| HIV Status (HIV+ vs. HIV-) | -- | -- | -- | -- | 6.41 (3.09) | .040* | |
| Race/Ethnicity (African American vs. Caucasian) | -- | -- | -- | -- | 1.19 (3.33) | .722 | |
| 3 | .232 | .013 | 0.64 | .593 | -- | -- | |
| Adversity × HIV | -- | -- | -- | -- | -3.59 (3.10) | .249 | |
| Adversity × Race | -- | -- | -- | -- | -4.62 (2.91) | .115 | |
| Race × HIV | -- | -- | -- | -- | -6.40 (4.02) | .115 | |
| 4 | .257 | .025 | 3.94 | .049* | |||
| Adversity × Race × HIV | -- | -- | -- | -- | 6.86 (3.46) | .049** | |
Note:
indicates p < .05;
Hypothesis 2: Simple Slopes of Adversity and Depression by Race and HIV-Status
Simple slopes were estimated to evaluate the relationship between social adversity and depressive symptoms among the four groups (i.e., HIV+ African Americans, HIV- African Americans, HIV+ Caucasians, HIV- Caucasians). As predicted, HIV+ African Americans evidenced a positive relationship between adversity and depressive symptoms (b = 2.88, SE = 0.98, p = .004). Contrary to what was hypothesized, there was no relationship between adversity and depressive symptoms for HIV- African Americans (b = −0.39, SE = 1.14, p = .735), HIV+ Caucasians (b = 0.64, SE = 1.81, p = .725), or HIV- Caucasians (b = 4.23, SE = 2.67, p = .116). The pattern of these results is presented in Figure 1.
Figure 1.
Predicted model of BDI-depressive symptoms by social adversity, HIV-status, and racial/ethnic group. Outcomes are statistically adjusted for age, gender, past diagnosis of substance abuse and dependence, medical comorbidities, and marital status.
Hypotheses 3 and 4: Comparative Differences in Relationships between Social Adversity and Depressive Symptoms by Race and HIV-Status
The simple slopes were compared among these four groups to assess differences in the strength of association between adversity and depressive symptoms. HIV+ African Americans evidenced a significantly greater relationship between adversity and depressive symptoms, as compared to HIV- African Americans (F(1, 116) = 4.52, p = .036) but not compared to HIV+ Caucasians (F(1, 116) = 1.28, p = .260) or HIV- Caucasians (F(1, 116) = 0.23, p = .632). There were no differences among the slopes between any of the other groups (F’s < 2.52, p’s > .115).
Post-Hoc Analyses
To investigate the individual contribution from each of the five indices (i.e., financial restriction to needed care, racial/ethnic discrimination, neighborhood SES during childhood, current neighborhood SES, current personal SES) that were used to derive the social adversity score, a series of post-hoc analyses were conducted within the HIV+ African American subsample. After controlling for all covariates, results from separate hierarchical regressions indicated that financial restriction to needed care (ΔR2 = .195, b = 15.33, SE = 3.87, p < .001) and perceived racial/ethnic discrimination (ΔR 2 = .127, b = 0.29, SE = 0.96, p = .004) were each related to higher depressive symptoms, whereas there was no predictive utility of neighborhood SES during childhood (ΔR 2 = .020, b = −2.49, SE = 2.25, p = .275), current neighborhood SES (ΔR2 = .006, b = 1.22, SE = 2.03, p = .551), or current personal SES (ΔR2 = .009, b = −1.07, SE = 1.48, p = .472) on depressive symptoms.
To investigate the unique predictive utility of each predictor, a hierarchical regression was conducted with the five indices simultaneously entered into the second step of the model after entering all covariates in the first step. The second step was significant (ΔR2 = .218, F(5, 42) = 3.34, p = .012). Among the individual predictors, however, only financial restriction to needed care carried unique predictive utility (b = 11.92, SE = 4.96, p = .021) in explaining depressive symptoms for HIV+ African Americans. By contrast, perceived racial/ethnic discrimination (b = 0.13, SE = 0.12, p = .275), current neighborhood SES (b = 0.32, SE = 1.83, p = .862), neighborhood SES from childhood (b = 0.05, SE = 2.13, p = .980), current personal SES (b = 1.07, SE = 1.33, p = .428), did not explain any unique proportion of the variance in depressive symptoms.
Discussion
The current study investigated how social adversity interacts with HIV-status and racial/ethnic affiliation to predict depressive symptoms. Hypothesis 1 was supported: the relationship between social adversity and depressive symptoms significantly differed as a function of HIV-status and self-identified race/ethnicity. In partial support of Hypothesis 2, the findings indicate that HIV+ African Americans evidenced a positive relationship between social adversity and depressive symptoms. Unexpectedly, however, there was no relationship between social adversity and depressive symptoms for all other groups. With regard to Hypothesis 3, the relationship was stronger among HIV+ African American as compared to HIV- African Americans (but not HIV+ Caucasians or HIV- Caucasians). The results did not support Hypothesis 4; HIV+ Caucasians and HIV- African Americans did not evidence a stronger relationship between adversity and depressive symptoms, as compared to HIV- Caucasians.
These findings highlight HIV+ African Americans as an at-risk population for depressive symptoms amidst high adversity. Although not assessed in the current study, it is possible that living with HIV as an African American increases the likelihood of subsequent stigmatization, which has been shown to predict adverse mental health outcomes across many groups (e.g., Hatzenbuehler, Phelan, & Link, 2013). Living with HIV can be conceptualized as a chronic social stressor that may have more deleterious mental health consequences for African Americans, as compared to Caucasians, due to the pervasive HIV-related stigma that exists within the African American community (Fullilove & Fullilove, 1999; Laurencin, Christensen, & Taylor, 2008). As compared to Caucasians, HIV+ African Americans also tend to receive worse health care (Shaprio et al., 1999) and often evidence a longer illness duration without treatment. Additionally, HIV+ African Americans evidenced a significantly greater relationship between social adversity and depressive symptoms, as compared to HIV- African Americans. Thus, the combination of being HIV+ and living as African American may confer a greater vulnerability to the effect of adversity on poor mental health than either factor alone. These results underscore the importance of evaluating intersectional identities and statuses, suggesting that those with multiple marginalized identities/statuses may be at high risk for poor mental health outcomes amidst adversity.
When investigating the relationships among depressive symptoms and the individual components of the social adversity index among HIV+ African Americans, only financial restriction to needed care and perceived racial/ethnic discrimination were related to depressive symptoms. Further, when examining the unique predictive utility of these components, results indicated that financial restriction to needed care was the only unique predictor. These findings point to financial barriers to receiving medical care as a potent predictor of depression, over and above measures of discrimination and SES. This indicator may be particularly important for the mental health of HIV+ African Americans, given that African Americans have been historically identified as a HIV+ group that is disproportionately exposed to inequitable health care access (Andersen et al., 2000) and poorer health care service delivery (Mayberry, Mili, & Ofili, 2000). Access to care has been shown to prospectively predict better physical and mental health outcomes for those living with HIV (Cunningham et al., 1998). These findings should be interpreted with caution, however, due to the small percentage (i.e., 9.7%) of HIV+ African American participants who endorsed experiencing financial restriction to receiving needed care.
Researchers have posited that exposure to adversity prompts an accelerated risk trajectory for poor health, particularly for African Americans (e.g., Troxel, Mathhews, Bromberger, & Sutton-Tyrrell, 2003). As such, it was hypothesized that HIV+ African Americans would be at a greater risk for depressive symptoms amid adversity, as compared to their HIV+ and HIV- Caucasian counterparts. However, the results did not support this hypothesis, and three potential explanations are offered below. First, the four groups in the study were well matched and did not statistically differ on several demographic (e.g., working status), behavioral (e.g., past substance abuse/dependence), medical (e.g., number of comorbidities), and physical health-related variables (e.g., BMI, blood pressure) that often explain racial/ethnic disparities in health. Second, although African Americans are more likely to evidence a greater exposure to both general and race-related stressors (Turner & Lloyd, 2004; Myers, 2009; Myers et al., 2015; Zimmerman & Messner, 2013), meta-analytic findings have shown that race/ethnicity does not moderate the relationship between perceived discrimination and mental health outcomes (Pascoe & Smart Richman, 2009). Although HIV+ African Americans endorsed a higher level of cumulative adversity in the current study, the current results indicated that the relationship between social adversity and depressive symptoms was not necessarily greater among HIV+ African Americans, as compared to Caucasians. Third, it is notable that that the standard error of the slope for HIV- Caucasians was larger as compared to all other groups, indicating substantial intragroup variability. It may be the case that HIV+ African Americans evidence a stronger relationship between adversity and depressive symptoms, but only when compared to a subset of the Caucasian groups. An examination of intragroup variability would be valuable. However, the current study is not powered enough to conduct such an investigation.
Contrary to Hypothesis 4, HIV- African Americans and HIV+ Caucasians did not evidence a greater relationship between adversity and depressive symptoms, as compared to HIV- Caucasians. This result may be driven by the unexpected null relationships between adversity and depressive symptoms for HIV- African Americans and HIV+ Caucasians. It is unclear why there was no relationship between adversity and depressive symptoms among these groups as previous work has indicated that exposure to adversity confers risk for depression across a wide range of groups (e.g., Myers et al., 2015). It may be the case that there is a moderating variable not measured in the current study (e.g., personality, coping strategy, group identification) that could be affecting the relationship between the variables. It also may be the case that the current investigation is underpowered to detect a relationship due to smaller sample sizes among the HIV- African American and HIV+ Caucasian subsamples.
An alternative explanation for the null relationships within the HIV- African American and the HIV+ Caucasian groups could be that these groups evidenced a “toughening” effect, which improves coping with adversity. This would be consistent with theory (Rutter, 2006) and research (Seery, Holman, & Silver, 2010; Seery, Leo, Lupien, Kondrak, & Almonte, 2013) on the toughening effects that result from challenging but manageable amounts of stress. HIV- African Americans and HIV+ Caucasians may have confronted challenging yet manageable stressful situations in their lives that could be helpful for building resilience, because these experiences may provide an opportunity to develop adaptive coping skills. However, in the context of HIV-infection, coping skills may be negatively impacted for African Americans because of the additional challenges they face related to their chronic disease status, rendering this group vulnerable to depression amidst adversity.
It is important to note that participants in the current study reported minimal to mild depressive symptoms overall, which could be indicative of low mood disturbance, general resiliency, and/or underreporting. The ability to detect significant relationships between adversity and depressive symptoms may be greater in a sample that evidenced higher levels of mood disturbance.
Limitations of the study should be addressed. First, the index of social adversity was based on measures of self-report, including those related to neighborhood characteristics. Although efforts were taken to capture multiple domains of social adversity, this measure was not comprehensive and relied on three single-item measures, which has measurement implications with regard to reliability and validity. It is plausible that third variables not measured in the current study may moderate and/or obscure relationships between social adversity on depressive symptoms. The smaller sample sizes among the HIV- Caucasian, HIV+ Caucasian, and HIV- African American groups precluded the ability to conduct analyses with regard to potential gender differences and could also limit statistical power to detect significant results. Additionally, the exclusion criteria from the parent study with regard to current and/or past substance abuse potentially limits generalizability to the broader HIV+ population. Participants endorsed low levels of depressive symptomology on the BDI, which should be considered as a limitation to generalizability. Finally, the use of cross-sectional data in the current study prevents any claim of causality or directionality of the observed relationship. It could be the case that participants who are more depressed were also more likely to recall their previous life experiences as more adverse.
There are also several notable strengths of the current study. This is the first study to test a three-way interaction between social adversity, race/ethnicity, and HIV-status on a mental health outcome. This work serves to extend previous research on intersectional identities (e.g., Logie, James, Tharao, & Loutfy, 2011) by providing evidence that HIV+ African Americans may be at particularly high risk for depressive symptoms in the face of social adversity. Second, this work extends the literature that examines relationships between health and social adversity, utilizing a composite index of social adversity. Third, the four groups were comparable on several important demographic and medical characteristics.
In conclusion, this report provides a sophisticated analysis of the relationships between social adversity and depressive symptoms as a function of HIV-status and racial/ethnic identity. This work demonstrated the utility for composite indices of social adversity that aggregate multiple sources of disadvantage into a singular risk index and underscores the need to examine how adversity and disadvantage differentially affect the health and well-being for those living with multiple marginalized identities or statuses. These findings are important for developing prevention and intervention efforts that target mental health disparities, particularly for HIV+ African Americans.
More work is needed in the future to replicate and extend the current findings with regard to examining potential gender differences. Future studies should incorporate public data related to neighborhood characteristics (e.g., violence, poverty) to further understand how exposure to social adversity from the community setting is related to health and well-being. Additionally, future studies should examine whether protective factors such as optimism buffer the potentially deleterious impact of social adversity on depressive symptoms for this underserved population.
Supplementary Material
Acknowledgments
Sponsors: This work was supported by National Institute of Mental Health Grant K23-MH095661 (PI: Thames) and a National Institute of Mental Health Predoctoral Fellowship (MH 15750, Williamson).
We are grateful to those who participated in the research and to Andy Lin, Joni Ricks-Oddie, and Christine Wells for providing statistical consultation.
Footnotes
There are no other financial disclosures.
Additionally, participants with central nervous system confounds (e.g., HIV associated opportunistic infections), Hepatitis C (confirmed by serology), or MRI contraindications (e.g., claustrophobia) were excluded from participating in the parent study.
Research suggests that the somatic symptoms of depression as measured by the BDI may be confounded with HIV illness symptoms. As such, items were summed from the cognitive-affective subscale and results were evaluated without the somatic items. The findings did not differ whether the BDI total score or the cognitive-affective subscale was used. Additionally, BDI total scores were not related to serologic indicators of HIV illness (i.e., viral load, CD4 T-cell count; p’s > .144) in the sample. Therefore, all reported findings were assessed with the BDI total score.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage; 1991. [Google Scholar]
- Andersen R, Bozzette S, Shapiro M, St Clair P, Morton S, Crystal S, Asch S. Access of vulnerable groups to antiretroviral therapy among persons in care for HIV disease in the United States. HCSUS Consortium. HIV Cost and Services Utilization Study. Health Services Research. 2000;35(2):389. [PMC free article] [PubMed] [Google Scholar]
- Arentoft A, Byrd D, Monzones J, Coulehan K, Fuentes A, Rosario A, Rivera Mindt M. Socioeconomic Status and Neuropsychological Functioning: Associations in an Ethnically Diverse HIV+ Cohort. The Clinical Neuropsychologist. 2015;29(2):232–254. doi: 10.1080/13854046.2015.1029974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck depression inventory-II. San Antonio, TX. 1996:78204–82498. [Google Scholar]
- Bernard D, Selden T, Yeh S. Financial burdens and barriers to care among nonelderly adults: The role of functional limitations and chronic conditions. Disability and Health Journal. 2016;9(2):256–264. doi: 10.1016/j.dhjo.2015.09.003. [DOI] [PubMed] [Google Scholar]
- Berger-Greenstein JA, Cuevas CA, Brady SM, Trezza G, Richardson MA, Keane TM. Major depression in patients with HIV/AIDS and substance abuse. AIDS Patient Care and STDs. 2007;21(12):942–955. doi: 10.1089/apc.2006.0153. [DOI] [PubMed] [Google Scholar]
- Brondolo E, Kelly KP, Coakley V, Gordon T, Thompson S, Levy E, Contrada RJ. The Perceived Ethnic Discrimination Questionnaire: Development and Preliminary Validation of a Community Version1. Journal of Applied Social Psychology. 2005;35(2):335–365. [Google Scholar]
- Bynum MS, Burton ET, Best C. Racism experiences and psychological functioning in African American college freshmen: Is racial socialization a buffer? Cultural Diversity and Ethnic Minority Psychology. 2007;13(1):64. doi: 10.1037/1099-9809.13.1.64. [DOI] [PubMed] [Google Scholar]
- Castellon SA, Hardy DJ, Hinkin CH, Satz P, Stenquist PK, van Gorp WG, Moore L. Components of depression in HIV-1 infection: their differential relationship to neurocognitive performance. Journal of Clinical and Experimental Neuropsychology. 2006;28(3):420–437. doi: 10.1080/13803390590935444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. [Accessed Feb 12 2016];HIV Surveillance Report. 2014 26 http://www.cdc.gov/hiv/library/reports/surveillance/. Published November 2015. [Google Scholar]
- Ciesla JA, Roberts JE. Meta-analysis of the relationship between HIV infection and risk for depressive disorders. American Journal of Psychiatry. 2001;158(5):725–730. doi: 10.1176/appi.ajp.158.5.725. [DOI] [PubMed] [Google Scholar]
- Cirino PT, Chin CE, Sevcik RA, Wolf M, Lovett M, Morris RD. Measuring socioeconomic status reliability and preliminary validity for different approaches. Assessment. 2002;9(2):145–155. doi: 10.1177/10791102009002005. [DOI] [PubMed] [Google Scholar]
- Contrada RJ, Ashmore RD, Gary ML, Coups E, Egeth JD, Sewell A, Chasse V. Measures of Ethnicity-Related Stress: Psychometric Properties, Ethnic Group Differences, and Associations with Well-Being. Journal of Applied Social Psychology. 2001;31(9):1775–1820. [Google Scholar]
- Cunningham WE, Hays RD, Ettl MK, Dixon WJ, Liu RCC, Beck CK, Shapiro MF. The prospective effect of access to medical care on health-related quality-of-life outcomes in patients with symptomatic HIV disease. Medical Care. 1998;36(3):295–306. doi: 10.1097/00005650-199803000-00007. [DOI] [PubMed] [Google Scholar]
- Davis L, Uezato A, Newell JM, Frazier E. Major depression and comorbid substance use disorders. Current Opinion in Psychiatry. 2008;21(1):14–18. doi: 10.1097/YCO.0b013e3282f32408. [DOI] [PubMed] [Google Scholar]
- Dawson JF, Richter AW. Probing three-way interactions in moderated multiple regression: development and application of a slope difference test. Journal of Applied Psychology. 2006;91(4):917. doi: 10.1037/0021-9010.91.4.917. [DOI] [PubMed] [Google Scholar]
- Deeks SG. HIV infection, inflammation, immunosenescence, and aging. Annual Review of Medicine. 2011;62:141. doi: 10.1146/annurev-med-042909-093756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang CY, Myers HF. The effects of racial stressors and hostility on cardiovascular reactivity in African American and Caucasian men. Health Psychology. 2001;20(1):64. doi: 10.1037//0278-6133.20.1.64. [DOI] [PubMed] [Google Scholar]
- Fullilove MT, Fullilove RE. Stigma as an obstacle to AIDS action the case of the African American community. American Behavioral Scientist. 1999;42(7):1117–1129. [Google Scholar]
- Geronimus AT. The weathering hypothesis and the relationship of maternal age to birth outcome: evidence and speculations. Ethnicity & Disease. 1992;2:207–221. [PubMed] [Google Scholar]
- Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. American Journal of Public Health. 2006;96(5):826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbie T, Mijch A, Ellen S, Hoy J, Hutchison C, Wright E, Judd F. Depression and neurocognitive performance in individuals with HIV/AIDS: 2-year follow-up. HIV Medicine. 2006;7(2):112–121. doi: 10.1111/j.1468-1293.2006.00350.x. [DOI] [PubMed] [Google Scholar]
- Haines VA, Beggs JJ, Hurlbert JS. Neighborhood disadvantage, network social capital, and depressive symptoms. Journal of Health and Social Behavior. 2011;52(1):58–73. doi: 10.1177/0022146510394951. [DOI] [PubMed] [Google Scholar]
- Hammond ER, Crum RM, Treisman GJ, Mehta SH, Clifford DB, Ellis RJ, Morgello S. Persistent CSF but not plasma HIV RNA is associated with increased risk of new-onset moderate-to-severe depressive symptoms; a prospective cohort study. Journal of Nurovirology. 2016:1–9. doi: 10.1007/s13365-015-0416-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. American Journal of Public Health. 2013;103(5):813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hays RD, Cunningham WE, Sherbourne CD, Wilson IB, Wu AW, Cleary PD, Eggan F. Health-related quality of life in patients with human immunodeficiency virus infection in the United States: results from the HIV Cost and Services Utilization Study. The American Journal of Medicine. 2000;108(9):714–722. doi: 10.1016/s0002-9343(00)00387-9. [DOI] [PubMed] [Google Scholar]
- Hazel NA, Hammen C, Brennan PA, Najman J. Early childhood adversity and adolescent depression: the mediating role of continued stress. Psychological Medicine. 2008;38(04):581–589. doi: 10.1017/S0033291708002857. [DOI] [PubMed] [Google Scholar]
- Herrmann S, McKinnon E, Hyland NB, Lalanne C, Mallal S, Nolan D, Duracinsky M. HIV-related stigma and physical symptoms have a persistent influence on health-related quality of life in Australians with HIV infection. Health and Quality of Life Outcomes. 2013;11(1):1. doi: 10.1186/1477-7525-11-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead AB. Four factor index of social status. 1975 [Google Scholar]
- Holzemer WL, Human S, Arudo J, Rosa ME, Hamilton MJ, Corless I, Willard S. Exploring HIV stigma and quality of life for persons living with HIV infection. Journal of the Association of Nurses in AIDS Care. 2009;20(3):161–168. doi: 10.1016/j.jana.2009.02.002. [DOI] [PubMed] [Google Scholar]
- Karlsen S, Nazroo JY. Relation between racial discrimination, social class, and health among ethnic minority groups. American Journal of Public Health. 2002;92(4):624–631. doi: 10.2105/ajph.92.4.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annual Review of Public Health. 2013;34:119. doi: 10.1146/annurev-publhealth-031912-114409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurencin CT, Christensen DM, Taylor ED. HIV/AIDS and the African-American community: a state of emergency. Journal of the National Medical Association. 2008;100(1):35. doi: 10.1016/s0027-9684(15)31172-x. [DOI] [PubMed] [Google Scholar]
- Leserman J. Role of depression, stress, and trauma in HIV disease progression. Psychosomatic Medicine. 2008;70(5):539–545. doi: 10.1097/PSY.0b013e3181777a5f. [DOI] [PubMed] [Google Scholar]
- Leserman J, Jackson ED, Petitto JM, Golden RN, Silva SG, Perkins DO, Evans DL. Progression to AIDS: the effects of stress, depressive symptoms, and social support. Psychosomatic Medicine. 1999;61(3):397–406. doi: 10.1097/00006842-199905000-00021. [DOI] [PubMed] [Google Scholar]
- Leserman J, Petitto JM, Gu H, Gaynes BN, Barroso J, Golden RN, Evans DL. Progression to AIDS, a clinical AIDS condition and mortality: psychosocial and physiological predictors. Psychological Medicine. 2002;32(06):1059–1073. doi: 10.1017/s0033291702005949. [DOI] [PubMed] [Google Scholar]
- Logie CH, James L, Tharao W, Loutfy MR. HIV, gender, race, sexual orientation, and sex work: a qualitative study of intersectional stigma experienced by HIV-positive women in Ontario, Canada. PLoS Med. 2011;8(11):e1001124. doi: 10.1371/journal.pmed.1001124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahajan AP, Sayles JN, Patel VA, Remien RH, Ortiz D, Szekeres G, Coates TJ. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS (London, England) 2008;22(Suppl 2):S67. doi: 10.1097/01.aids.0000327438.13291.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayberry RM, Mili F, Ofili E. Racial and ethnic differences in access to medical care. Medical Care Research and Review. 2000;57(4 suppl):108–145. doi: 10.1177/1077558700057001S06. [DOI] [PubMed] [Google Scholar]
- Miller B, Taylor J. Racial and socioeconomic status differences in depressive symptoms among black and white youth: An examination of the mediating effects of family structure, stress and support. Journal of Youth and Adolescence. 2012;41(4):426–437. doi: 10.1007/s10964-011-9672-4. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Simons AD. Diathesis-stress theories in the context of life stress research: implications for the depressive disorders. Psychological Bulletin. 1991;110(3):406. doi: 10.1037/0033-2909.110.3.406. [DOI] [PubMed] [Google Scholar]
- Moskowitz JT, Wrubel J, Hult JR, Maurer S, Acree M. Illness appraisals and depression in the first year after HIV diagnosis. PloS One. 2013;8(10):e78904. doi: 10.1371/journal.pone.0078904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. The Lancet. 2007;370(9590):851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- Myers HF. Ethnicity-and socio-economic status-related stresses in context: an integrative review and conceptual model. Journal of Behavioral Medicine. 2009;32(1):9–19. doi: 10.1007/s10865-008-9181-4. [DOI] [PubMed] [Google Scholar]
- Myers HF, Wyatt GE, Ullman JB, Loeb TB, Chin D, Prause N, Liu H. Cumulative burden of lifetime adversities: Trauma and mental health in low-SES African Americans and Latino/as. Psychological Trauma: Theory, Research, Practice, and Policy. 2015;7(3):243. doi: 10.1037/a0039077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychological Bulletin. 2009;135(4):531. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabkin JG. HIV and depression: 2008 review and update. Current HIV/AIDS Reports. 2008;5(4):163–171. doi: 10.1007/s11904-008-0025-1. [DOI] [PubMed] [Google Scholar]
- Ransom D, Heckman TG, Anderson T, Garske J, Holroyd K, Basta T. Telephone-delivered, interpersonal psychotherapy for HIV-infected rural persons with depression: a pilot trial. Psychiatric Services. 2008;59(8):871–877. doi: 10.1176/ps.2008.59.8.871. [DOI] [PubMed] [Google Scholar]
- Ross CE. Neighborhood disadvantage and adult depression. Journal of Health and Social Behavior. 2000:177–187. [PubMed] [Google Scholar]
- Rutter M. Implications of resilience concepts for scientific understanding. Annals of the New York Academy of Sciences. 2006;1094:1–12. doi: 10.1196/annals.1376.002. [DOI] [PubMed] [Google Scholar]
- Sbarra DA, Emery RE, Beam CR, Ocker BL. Marital Dissolution and Major Depression in Midlife A Propensity Score Analysis. Clinical Psychological Science. 2014;2(3):249–257. doi: 10.1177/2167702613498727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaan B. Widowhood and depression among older Europeans—The role of gender, caregiving, marital quality, and regional context. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2013;68(3):431–442. doi: 10.1093/geronb/gbt015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seery MD, Holman EA, Silver RC. Whatever does not kill us: cumulative lifetime adversity, vulnerability, and resilience. Journal of Personality and Social Psychology. 2010;99(6):1025. doi: 10.1037/a0021344. [DOI] [PubMed] [Google Scholar]
- Seery MD, Leo RJ, Lupien SP, Kondrak CL, Almonte JL. An upside to adversity? Moderate cumulative lifetime adversity is associated with resilient responses in the face of controlled stressors. Psychological Science. 2013 doi: 10.1177/0956797612469210. 0956797612469210. [DOI] [PubMed] [Google Scholar]
- Shapiro MF, Morton SC, McCaffrey DF, Senterfitt JW, Fleishman JA, Perlman JF, Bozzette SA. Variations in the care of HIV-infected adults in the United States: results from the HIV Cost and Services Utilization Study. JAMA. 1999;281(24):2305–2315. doi: 10.1001/jama.281.24.2305. [DOI] [PubMed] [Google Scholar]
- Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Social Science & Medicine. 2007;64(9):1823–1831. doi: 10.1016/j.socscimed.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. Structured clinical interview for DSM-IV (SCID) New York: Biometrics Research; 1995. [Google Scholar]
- Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, Silove D. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. International Journal of Epidemiology. 2014 doi: 10.1093/ije/dyu038. dyu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Marmot M. Burden of psychosocial adversity and vulnerability in middle age: associations with biobehavioral risk factors and quality of life. Psychosomatic Medicine. 2003;65(6):1029–1037. doi: 10.1097/01.psy.0000097347.57237.2d. [DOI] [PubMed] [Google Scholar]
- Strine TW, Mokdad AH, Balluz LS, Gonzalez O, Crider R, Berry JT, Kroenke K. Depression and anxiety in the United States: findings from the 2006 behavioral risk factor surveillance system. Psychiatric Services. 2015 doi: 10.1176/ps.2008.59.12.1383. [DOI] [PubMed] [Google Scholar]
- Su D, Irwin JA, Fisher C, Ramos A, Kelley M, Mendoza DAR, Coleman JD. Mental Health Disparities Within the LGBT Population: A Comparison Between Transgender and Nontransgender Individuals. Transgender Health. 2016;1(1):12–20. doi: 10.1089/trgh.2015.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toussaint L, Shields GS, Dorn G, Slavich GM. Effects of lifetime stress exposure on mental and physical health in young adulthood: How stress degrades and forgiveness protects health. Journal of Health Psychology. 2016;21(6):1004–1014. doi: 10.1177/1359105314544132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, Matthews KA, Bromberger JT, Sutton-Tyrrell K. Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women. Health Psychology. 2003;22(3):300. doi: 10.1037/0278-6133.22.3.300. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Lloyd DA. Stress Burden and the Lifetime Incidence of Psychiatric Disorder in Young Adults: Racial and Ethnic Contrasts. Archives of General Psychiatry. 2004;61(5):481–488. doi: 10.1001/archpsyc.61.5.481. [DOI] [PubMed] [Google Scholar]
- Weden MM, Carpiano RM, Robert SA. Subjective and objective neighborhood characteristics and adult health. Social Science & Medicine. 2008;66(6):1256–1270. doi: 10.1016/j.socscimed.2007.11.041. [DOI] [PubMed] [Google Scholar]
- Wight RG, Botticello AL, Aneshensel CS. Socioeconomic context, social support, and adolescent mental health: A multilevel investigation. Journal of Youth and Adolescence. 2006;35(1):109–120. [Google Scholar]
- Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. Journal of Behavioral Medicine. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health socio-economic status, stress and discrimination. Journal of Health Psychology. 1997;2(3):335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Zimmerman GM, Messner SF. Individual, family background, and contextual explanations of racial and ethnic disparities in youths’ exposure to violence. American Journal of Public Health. 2013;103(3):435–442. doi: 10.2105/AJPH.2012.300931. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.