Abstract
In recent years, the network approach to psychopathology has been advanced as an alternative way of conceptualizing mental disorders. In this approach, mental disorders arise from direct interactions between symptoms. Although the network approach has led to many novel methodologies and substantive applications, it has not yet been fully articulated as a scientific theory of mental disorders. The present paper aims to develop such a theory, by postulating a limited set of theoretical principles regarding the structure and dynamics of symptom networks. At the heart of the theory lies the notion that symptoms of psychopathology are causally connected through myriads of biological, psychological and societal mechanisms. If these causal relations are sufficiently strong, symptoms can generate a level of feedback that renders them self‐sustaining. In this case, the network can get stuck in a disorder state. The network theory holds that this is a general feature of mental disorders, which can therefore be understood as alternative stable states of strongly connected symptom networks. This idea naturally leads to a comprehensive model of psychopathology, encompassing a common explanatory model for mental disorders, as well as novel definitions of associated concepts such as mental health, resilience, vulnerability and liability. In addition, the network theory has direct implications for how to understand diagnosis and treatment, and suggests a clear agenda for future research in psychiatry and associated disciplines.
Keywords: Psychopathology, network approach, mental disorders, symptom networks, mental health, resilience, vulnerability, diagnosis, treatment
Like all medical branches, psychiatry is a problem‐oriented discipline that is motivated by and rooted in the practice of clinical work. That practice revolves around certain sets of problems that people present themselves with. For instance, a person may be referred to a psychiatrist because he is afraid that other people can read his mind, causing anxiety and social isolation. Or, a person may approach a doctor because his drinking behavior starts interfering with his work, and he is unable to quit or cut back. Another person may have developed a fear of social situations that has started to interfere with his social life, leading to feelings of loneliness and sadness. An important task of psychiatry (and associated disciplines, such as clinical psychology) is to find out where these problems come from and how they can be solved. The present paper proposes a theoretical framework that addresses this issue.
Given the heterogeneity of the problems that psychiatry and clinical psychology deal with, it would perhaps be best to categorize them broadly as “problems of living”. In the past century, however, scientific terminology took a very different turn, and as a result it has become commonplace to talk about people who struggle with such problems as “suffering from mental disorders”. Accordingly, the problems found in clinical practice have been categorized as symptoms, as exemplified in diagnostic manuals like the DSM‐5 and ICD‐10. Via the analogy with medical work, this use of the word “symptom” suggests the presence of a “disease”, and this provides a suggestive answer to the question of why some people suffer from certain sets of symptoms, while others do not; namely, because they have particular kinds of diseases, to wit, mental disorders1, 2.
However, there is an important difference between mental disorders and diseases. The use of the term “disease” implies a worked out etiology, by which symptoms arise from a common pathogenic pathway, while the term “mental disorder” refers to a syndromic constellation of symptoms that hang together empirically, often for unknown reasons. Unfortunately, for all but a few constellations of the symptoms that arise in mental disorders, common pathogenic pathways have proven elusive1, 3, 4. This frustrates the application of one of the most important explanatory schemes in general medicine: the search for common causes that give rise to overt symptomatology1, 2. For instance, if a person coughs up blood, has pain in the chest, and is short of breath, a physician may hypothesize the presence of a tumor in the lungs. Such a tumor is a localized, physically identifiable abnormality in the body, that acts as a common cause with respect to the symptomatology1. As a result, even though the symptoms are phenomenologically distinct, they are causally homogeneous, because they are causal effects of the same disease. In this case, removing the disease entity (e.g., killing the cancer cells through chemotherapy) removes the common cause of the symptoms, which wane as a result. This type of strategy has not been very effective in psychiatry, precisely because no central disease mechanisms or pathogenic pathways have been identified for mental disorders. The question is why.
Recent work has put forward the hypothesis that we cannot find central disease mechanisms for mental disorders because no such mechanisms exist. In particular, instead of being effects of a common cause, psychiatric symptoms have been argued to cause each other 5, 6. For instance, if one thinks that other people can read one's mind (delusion), this may generate extreme suspicion (paranoia); this paranoia can lead one to avoid other people (social isolation), which, because one is no longer exposed to corrective actions of the social environment, may serve to sustain and exacerbate the relevant delusions. In this way, symptoms may form feedback loops that lead the person to spiral down into the state of prolonged symptom activation that we phenomenologically recognize as a mental disorder6, 7.
Because the interactions between symptoms can be understood as a network, in which symptoms are nodes and causal interactions between symptoms are connections between nodes, this conceptualization has become known as the network approach to psychopathology. Methodological research within this approach has focused on developing statistical techniques designed to identify network structures among psychiatric symptoms from empirical data7, 8, 9, 10, 11, 12. These techniques have now been applied to a range of constructs, such as depression13, 14, 15, 16, 17, 18, 19, 20, anxiety disorders21, 22, post‐traumatic stress23, complex bereavement24, autism25, 26, psychotic disorders27, 28, 29, substance abuse30, the general structure of psychiatric symptomatology31, 32, 33, 34, diagnostic manuals themselves34, 35, health‐related quality of life36, and personality traits37.
In general, findings from these studies are encouraging, in the sense that results accord with clinical intuition and standing theory. However, although the network approach has generated an important new way of thinking about the problems in psychopathology research, it has not yet been developed as an overarching theory of mental disorders. The goal of this paper is to present a set of explanatory mechanisms that may be combined into a general framework which specifies: a) what mental disorders are, b) how they arise, and c) how they may be optimally treated.
SYMPTOM NETWORKS
The central tenet of the network approach is that mental disorders arise from the causal interaction between symptoms in a network1, 6. Such causal interaction between symptoms can be interpreted using interventionist theories of causation38. In this interpretation, the presence of a causal connection means that, if an (experimental or natural) intervention changed the state of one symptom, this would change the probability distribution of the other symptom38, 39. Importantly, network theory is agnostic with regard to how these causal relations are instantiated. Direct causal connections between symptoms may be grounded in basic biological (e.g., insomnia → fatigue) or psychological (e.g., loss of interest → feelings of guilt) processes, in homeostatic couplings (e.g., appetite and sleep both interact with the biological clock, so that when one is disturbed, the other is likely to be disturbed as well), in societal norms (e.g., dependence on heroin increases the probability of contact with law enforcement agencies in countries where it is prohibited by law), or in still other processes.
Patterns of symptom‐symptom interaction can be encoded in a network structure. In such a structure, symptoms are represented as nodes. Nodes corresponding to symptoms that directly activate each other are connected, while nodes corresponding to symptoms that do not directly activate each other are not. An example of a network structure is given in Figure 1.
Figure 1.
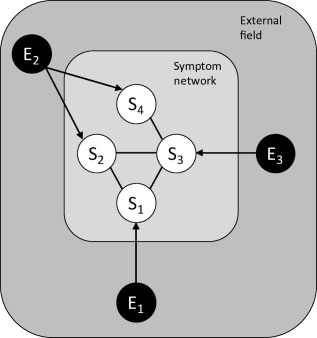
A symptom network of four symptoms (S1‐S4). If two symptoms have the tendency to activate each other, they are connected by a line (e.g., S1‐S2). Symptoms that are not directly connected to each other (e.g., S1‐S4) can still synchronize if they share a common neighbor in the network (e.g., S3). External factors that affect the network (e.g., adverse life events) are represented in the external field. These may be symptom‐specific (E1, E3) or shared across symptoms (E2).
Conditions that can influence symptoms from outside the network (e.g., adverse life events) form the external field of the symptoms. Changes in the external field (e.g., losing one's partner) may activate symptoms in the network (e.g., depressed mood). In turn, this may cause the symptom's neighbors (e.g., insomnia, reproach, anxiety) to align their states with the depression symptom. Note that factors in the external field are outside of the network, but need not be outside of the person7. Inflammation40, for instance, is a process inside the person, but its effects on symptoms like fatigue, mood and anxiety nevertheless come from outside of the symptom network, because there is no node in the network that corresponds to inflammation. Thus, the external field is external relative to the psychopathology network, but not relative to the physical boundaries of the person. Importantly (and, in some cases, plausibly), the external field may include abnormal brain functioning, commonly thought to be associated with mental disorders41; for instance, delusions or hallucinations may arise in this way.
If all symptoms in a network interact with each other, and these interactions also have the same strength, symptoms are exchangeable, except for their dependence on the external field. In this case, if the connections are strong, the symptoms in the network will show highly synchronized behavior: if one symptom is active, it is more likely than not that the other symptoms are also active. However, if not all symptoms directly interact or if certain interactions are much stronger than others, certain symptoms in the network can be active, while others are not. In this case, the network structure will feature clustering: within the archipelago of psychopathology symptoms, we will find particular island groups that are very closely related and thus influence each other to a greater degree34.
For instance, insomnia is likely to have a strong direct effect on fatigue, but a much weaker effect on feelings of guilt; if insomnia does influence feelings of guilt, that effect is likely to be mediated by, for instance, loss of interest or concentration problems. Similarly, excessive alcohol use will first impact one's ability to fulfill daily duties, a symptom that will probably mediate the origination of further problems (e.g., losing one's job). If such symptom groups form more tightly connected sub‐networks in the larger psychopathology network, this will produce reliable patterns of co‐activation among symptoms.
NETWORK THEORY
The ideas presented above can be generalized to a comprehensive theoretical model of psychopathology. In particular, I propose the following four principles to encode the backbone of the network theory of mental disorders:
Principle 1. Complexity: Mental disorders are best characterized in terms of the interaction between different components in a psychopathology network.
Principle 2. Symptom-component correspondence: The components in the psychopathology network correspond to the problems that have been codified as symptoms in the past century and appear as such in current diagnostic manuals.
Principle 3. Direct causal connections: The network structure is generated by a pattern of direct causal connections between symptoms.
Principle 4. Mental disorders follow network structure: The psychopathology network has a non‐trivial topology, in which certain symptoms are more tightly connected than others. These symptom groupings give rise to the phenomenological manifestation of mental disorders as groups of symptoms that often arise together.
These principles imply that the etiology of mental disorders can be thought of in terms of a process of spreading activation in a symptom network34, 42, 43, 44. If a symptom arises (which may occur for different reasons depending on person, time and context), this will influence the probability that a connected symptom arises as well. Thus, coupled sets of symptoms, which are close in the network structure, will tend to synchronize. Mental disorders then arise when groups of tightly coupled symptoms actively maintain each other, leading to a cluster of psychopathology symptoms that becomes self‐sustaining.
Some remarks on these principles are in order. Principle 1, Complexity, appears the least problematic. With the exception of a few illustrative cases3, no theoretically singular causes of mental disorders have so far been identified; therefore, accounts of mental disorders in terms of interacting components of a complex system are not only plausible, but in a sense the only game in town. Thus, this principle encodes the consensus that mental disorders are multifactorial in constitution, etiology, and causal background, which appears overwhelmingly plausible given the current scientific record3, 45.
Principle 2, Symptom‐component correspondence, is less straightforward. The assumption implies that psychopathology symptoms are defined at the right level of granularity, and successfully identify the important components in the psychopathology network. Insofar as factors not encoded in common diagnostic systems play a role (e.g., psychological processes not included in the symptomatology, neural conditions, genetic antecedents), they must do so by: a) constituting the symptom in question (e.g., the symptom of anxiety involves a neural realization in the brain, which partly constitutes that symptom), b) constituting a symptom‐symptom connection (e.g., the biological clock is part of the system that generates the insomnia → fatigue relation), or c) acting as a variable in the external field (e.g., chronic pain is likely to be an external factor that causes fatigue).
Principle 3, Direct causal connections, appears plausible on several grounds. First, diagnostic systems often explicitly require the presence of symptom‐symptom connections for diagnosis. Second, clinicians spontaneously generate causal networks when asked how symptoms hang together1, 46, and people in general seem to experience little trouble listing the causal relations between their symptoms47, 48. Third, momentary mood states that are closely related to symptomatology, as measured through experience sampling49, indeed appear to interact15, 50, 51, 52, 53. Finally, network analyses of, for instance, DSM‐5 symptoms show that many symptom pairs remain statistically associated, while controlling for all other symptoms31; this provides evidence, although indirect, for the hypothesis that the relevant symptoms are causally connected.
Principle 4, Mental disorders follow network structure, holds that the stable phenomenological grouping of symptoms, which forms the basis of the current syndromic definitions of mental disorders, as for instance presented in the DSM‐5, results from the causal architecture of the symptom network at large: symptoms that belong to the same disorder are more strongly causally related than symptoms that belong to different disorders, as is illustrated in Figure 2. As a result, in factor analyses of the covariance among symptoms or total scores defined on them54, 55, tightly coupled groups of symptoms will tend to load on the same factor. If this is correct, existing factor‐analytic work on the covariance structure of symptoms can be interpreted as yielding a first approximation to the network architecture of psychopathology.
Figure 2.
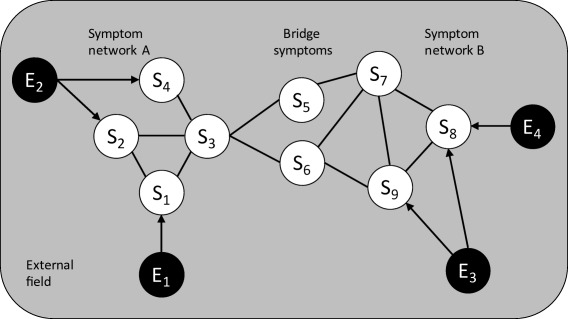
Two disorders (A and B) that are connected through bridge symptoms (S5 and S6) which play a role in both networks. Although the association of symptoms will be strongest within each network, structural overlap between the disorders is unavoidable, and as a result comorbidity will arise.
An important consequence of the above principles is that comorbidity is an intrinsic feature of mental disorders6. That is, even though processes of symptom‐symptom interaction may be most active within symptom sets that are associated with a given mental disorder, they will not stop at the border of a DSM diagnosis. For instance, if a person develops insomnia in the context of post‐traumatic stress disorder, that may cause fatigue and concentration problems – bridge symptoms that also belong to networks associated with major depressive episode and generalized anxiety disorder – and as a result comorbid patterns of symptom interactions will arise in the major depressive episode/generalized anxiety disorder network. Thus, instead of a nuisance that will go away once we have better measurement equipment, more insight in the biology of the brain, or more knowledge of the genetic structure of disorders, comorbidity should be seen as part of the flesh and bones of psychopathology6.
THE DYNAMICS OF SYMPTOM NETWORKS
The implications of network thinking for the structure and comorbidity of mental disorders are straightforward, and as a result they were quickly identified once the network approach surfaced5, 6. It took longer to realize that the network theory also has implications for the dynamics of mental disorders. Especially Cramer's work56 was instrumental in this regard, because it proved the existence of a phenomenon called hysteresis in realistically parameterized symptom networks57. This is a major discovery which may hold the key to connecting the structure of symptom networks to their dynamics.
To illustrate the importance of hysteresis, we need to specify how the etiology of mental disorders pans out in a network. Figure 3 gives a representation of that process. Assume that we start from a fully asymptomatic Phase 1. In this phase, no symptoms are present, and the properties that underlie the causal interactions between symptoms in later phases are dormant (i.e., dispositional, in that they describe what would happen upon symptom activation, but not what does happen at that moment). In Phase 2, trigger events in the external field (e.g., adverse life events) produce network activation. In Phase 3, symptom activation will spread through the network via connections between symptoms. In a strongly connected symptom network, symptoms can enter Phase 4, in which they keep each other activated due to feedback relations. As a result, the network can become self‐sustaining, and may stay active long after the events in the external field that triggered its activation have waned.
Figure 3.
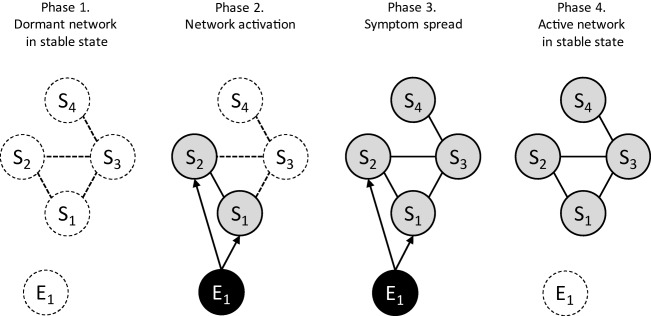
Phases in the development of mental disorders according to the network theory. After an asymptomatic phase, in which the network is dormant (Phase 1), an external event (E1) activates some of the symptoms (Phase 2), which in turn activate connected symptoms (Phase 3). If the network is strongly connected, removal of the external event does not lead to recovery: the network is self‐sustaining and is stuck in its active state (Phase 4).
Strongly connected networks thus feature an asymmetry in their dynamics: although the presence of a given trigger event can activate a strongly connected network, the subsequent absence of that event needs not de‐activate it. This is the phenomenon of hysteresis, a hallmark of phase transitions58 that is present in many complex systems. Hysteresis is, in my view, a very plausible feature of psychopathology networks, because – in many cases of psychopathology – triggering events can cause pervasive problems long after the triggers themselves have disappeared. An important example would be the etiology of post‐traumatic stress disorder, which develops and endures after the traumatic event itself has subsided23, but we see similar examples in the development of major depression after the loss of a spouse16 and in the effects of childhood abuse, which persist long after the abuse has ended27. The network theory thus offers an explanatory mechanism for these phenomena in the form of self‐sustaining feedback between symptoms, as coded in its final principle:
Principle 5. Hysteresis: Mental disorders arise due to the presence of hysteresis in strongly connected symptom networks, which implies that symptoms continue to activate each other, even after the triggering cause of the disorder has disappeared.
Note that these dynamics only occur in strongly connected networks, because only these networks display hysteresis56, 57. In weakly connected networks, more serious triggers can evoke strong reactions but, because the connections between the symptoms are not strong enough to render them self‐sustaining, the network will gradually recover and return to its asymptomatic state. A process that may instantiate this phenomenon in networks of depression symptoms is normal grief. Normal grief can cause a symptom pattern that is indistinguishable from major depression but, because the symptoms do not engage in feedback, the symptom pattern is not self‐sustaining, so that in time the system returns to its healthy stable state. This difference is represented in Figure 4.
Figure 4.

A weakly connected network (top panel) is resilient. Symptoms may be activated by events in the external field, but the symptom‐symptom interactions are not strong enough to lead to self‐sustaining symptom activity. A strongly connected network (bottom panel), instead, can sustain its own activity and thus develop into a disorder state.
The different dynamics of symptom networks under various parameterizations suggest novel definitions of well‐known concepts in psychopathology research. First, the notion of mental health may be defined as the stable state of a weakly connected network. Note that this definition does not coincide with a definition of mental health as “absence of symptoms”; instead, it defines mental health as an equilibrium state, to which a healthy system returns if perturbed. Weakly connected networks can, however, feature symptomatology given stressors in the external field (e.g., normal grief); conversely, strongly connected networks can have temporarily absent symptomatology due to local suppression of that symptomatology (for instance, a person with a vulnerable network involving psychotic symptoms may be temporarily asymptomatic due to medication).
In parallel, the notion of a mental disorder itself assumes a new definition as the (alternative) stable state of a strongly connected network, i.e., the state of disorder that is separated from the healthy state by hysteresis. The concept of resilience can be defined as the disposition of weakly connected networks to quickly return to their stable state of mental health, and the concept of vulnerability as the disposition of strongly connected networks to transition into a state of disorder upon a perturbation in the external field. Individual differences in liability to develop different kinds of disorders (e.g., internalizing versus externalizing disorders) are due to differences in the network parameters of the corresponding symptoms7. This system of definitions is represented in Table 1.
Table 1.
Network connectivity and the external field
| Network connectivity | |||
|---|---|---|---|
| Weak | Strong | ||
| Stressors in external field | Weak | Mental health with high resilience | Elevated vulnerability (possibly remission state) |
| Strong | Elevated symptomatology | Mental disorder | |
A weakly connected network will, under low external stress levels, occupy a stable state of mental health (top left cell). The network is resilient because — even if it may feature symptomatology if put under stress from the external field (bottom left cell) — it will return to its stable state when that stress level diminishes. In contrast, a highly connected network may be asymptomatic (top right cell), but is vulnerable because — as soon as a stressor arises in the external field — it can transition to an alternative stable state of mental disorder (bottom right cell).
DIAGNOSIS AND TREATMENT
In the network theory, diagnosis should be understood as a process by which a clinician identifies: a) which symptoms are present, and b) which network interactions sustain them. Arguably, this is quite close to how clinicians naturally conceptualize and diagnose disorders. For example, diagnostic manuals routinely require one to code not only the presence of symptoms, but also the interactions between them. The DSM‐5 diagnosis of obsessive‐compulsive disorder, for instance, not only requires the presence of obsessions and compulsions, but of their causal coupling (e.g., a person is driven to compulsive cleaning in response to an obsession with cleanliness); the diagnosis of substance use disorder requires giving up important activities because of substance use.
In addition, the DSM‐5 contains many specifications of the context in which symptoms should arise (e.g., the presence of insomnia only counts as a symptom of major depressive episode in the context of a prolonged period of depressed mood and/or loss of interest). Finally, the DSM‐5 contains a great many negative causal specifications, which require certain causes to be absent (e.g., substance use as a cause of symptoms in schizophrenia). Thus, although the DSM‐5 may be “theoretically neutral” with respect to other theories of psychopathology59, it is not neutral with respect to the network theory; rather, it specifies causal network structures throughout its definitional apparatus.
Naturally, there are also important aspects of the network theory that the DSM‐5 does not articulate, such as the importance of feedback between symptoms in sustaining mental disorders. In addition, findings of network analysis may generate novel insights into the functional role and importance of specific symptoms in maintaining disorders (e.g., the centrality of symptoms in the network). Thus, while the network theory accords well with current diagnostic practice, it can also be expected to enhance that practice with novel concepts and methodology12, 13, 14.
If diagnosis involves identifying a symptom network, then treatment must involve changing or manipulating that network. Due to the simplicity of networks, such manipulations can be organized in just three categories: a) symptom interventions, which directly change the state of one or more symptoms, b) interventions in the external field, which remove one or more triggering causes, and c) network interventions, which change the network structure itself by modifying symptom‐symptom connections. As an example, consider a drug‐using psychotic person who is convinced that other people can hear his thoughts, as a result does not go out, and becomes socially isolated, which in turn serves to sustain the delusion in question. In this case, an example of a symptom intervention may involve prescribing antipsychotic medication in order to suppress the delusion directly. A change in the external field may involve an intervention that suppresses one or more triggering events (e.g., get the person to quit precipitating drug use). Finally, a network intervention may involve cognitive behavioral therapy, which aims to teach the person how to deal with the delusion in question so that, even if it does arise sometimes, it no longer has the effect of causing social isolation.
If mental disorders can indeed be understood as symptom networks, and treatment can be categorized as suggested above, then one could couple a “library” of treatment interventions to a set of network structures, in order to optimally select and plan interventions. That is, if we could detect the network structure that governs a specific individual's pattern of symptom‐symptom interaction – e.g., through the analysis of perceived causal relations47 or the experience sampling method49, 50, 51, 52, 53 – then we could search for the combination of treatment strategies that would most effectively lead the network to transition into a healthy state. It would seem likely that successful treatment will generally require a combination of network interventions (in order to make the healthy state accessible) and symptom interventions (to knock the system into that healthy state).
CONCLUSIONS
The network theory of mental disorders, as advanced here, offers a consistent and transparent theoretical framework for thinking about psychopathology. The first empirical steps along the lines of this theory have already been taken, in the form of explorative studies that chart the network architecture of symptomatology13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37. Assuming that, in time, the structure of symptom networks becomes increasingly clear, the second empirical step would be to connect (individual differences in) the architecture of these networks to (individual differences in) relevant biological, psychological and socio‐cultural factors. Finally, a better understanding of the processes that instantiate symptom thresholds and network connectivity parameters should allow us to optimally organize existing treatment interventions, and develop new ones. This presents a new kind of roadmap for progress in psychopathology research, which hopefully will be more successful than past attempts to understand and combat mental disorders.
A question that arises is how far the theory generalizes and what kind of theory it is. Because the network model is not tied to a particular level of explanation (e.g., biological, psychological or environmental), and does not single out particular mechanisms that generate the network structure, it is perhaps best interpreted as an organizing framework – an explanatory scheme with broad use across sub‐domains of psychopathology. In this respect, the theory is reminiscent of Darwin's theory of evolution, which also yields a set of explanatory mechanisms (e.g., mutation, natural selection, adaptation) that may play out in different ways in different species. Like the theory of evolution, the network theory of psychopathology yields broad explanatory principles (e.g., hyperconnectivity in symptom networks yields alternative stable states that correspond to disorders), without specifying, in advance, the realization or implementation of these principles. This is an advantage, because it means that the network theory offers a framework for the integration of different levels of explanation (i.e., biological, psychological, sociological) that, in my view, is a necessary feature of any successful theory of mental disorders. At the same time, the model is not merely metaphorical or verbal: granted some simplifying assumptions, the network theory can be represented in mathematical form60, 61 and thus allows for simulating both the course of disorders and the effects of various treatment interventions.
However, to what extent the network theory may serve as an exhaustive explanatory model remains to be seen; clearly there are some disorders that fit the framework better than others. The match with episodic disorders and chronic disorders with a relatively well‐delineated onset (e.g., major depression, post‐traumatic stress disorder, obsessive‐compulsive disorder, substance use disorder, panic disorder, generalized anxiety disorder, phobias, eating disorders) appears reasonable. Disorders with a cyclic pattern (e.g., bipolar disorder) may be accommodated in models for which the stable state is a cycle rather than a fixed point. It is less obvious that the theory could accommodate the genesis of slowly developing disorders (e.g., autism spectrum disorders, personality disorders, some aspects of schizophrenia). These disorders are likely to feature an interaction between different symptoms as well, but this must partly involve developmental processes that play out on very different time scales. For example, in autism, it is likely that a symptom such as avoiding eye contact, in the long run, will limit the ability of a child to learn the ways of social interaction, leading to a symptom like problems in maintaining relationships. However, this process itself likely includes fast feedback processes involving the reward structure of social interaction, leading to a Russian doll of networks within networks. Whether such disorders are amenable to a network theory, and what such a theory would look like, is therefore an important question for future research.
It is worth noting that the theory proposed in this paper is very simple. Especially principle 2, symptom‐component correspondence, appears quite strict, but there are various other properties of the theory that, as research progresses, may well turn out to be strong idealizations and abstractions. This is a deliberate choice. Networks are quite complex by nature, and I think that, given our current state of ignorance, it is better to have at least a relatively tractable network theory, which may need to be altered as research data come in, than to start out with an overly complicated model, involving an indefinite set of variables, that places no restrictions on the data and bears unclear relations to the evidence. My hope is that, through successive iterations of the network model, we will ultimately converge on a reasonable model of mental disorders that, while probably more complex than the current formulation, will still be sufficiently tractable as to be scientifically workable.
Finally, as may be clear from the examples given in this paper, connections between symptoms are often prosaic. If you do not sleep, you get tired; if you see things that are not there, you get anxious; if you use too much drugs, you get into legal trouble, etc.. It is, in my view, likely that these symptom‐symptom connections are rooted in very ordinary biological, psychological and societal processes (and thus may involve harmful dysfunctions in these processes59). This is surprising, because it means that disorders are not ill‐understood ephemeral entities, the nature of which will have to be uncovered by future psychological, neuroscientific or genetic research (which appears a widespread conviction, if not the received view, among researchers). Rather, the fact that we have the set of basic symptoms, and also understand many of the relations between them, means that we already have a quite reasonable working model of what disorders are and how they work.
If so, our current lack of understanding of mental disorders may not have resulted from limited observational capacities, noisy measurement instruments, or inadequate data, as is typically supposed. Instead, we may have simply lacked a theoretical framework to organize the available empirical facts.
ACKNOWLEDGEMENTS
This research was supported by European Research Council Consolidator Grant no. 647209. The author would like to thank E. Fried, R. McNally, S. Epskamp, M. Wichers, C. van Borkulo, P. Zachar and K. Kendler for their valuable comments on a draft of this paper.
REFERENCES
- 1. Borsboom D, Cramer AOJ. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol 2013;9:91‐121. [DOI] [PubMed] [Google Scholar]
- 2. Hyland ME. The origins of health and disease. Cambridge: Cambridge University Press, 2011. [Google Scholar]
- 3. Kendler KS. The dappled nature of causes of psychiatric illness: replacing the organic‐functional/hardware‐software dichotomy with empirically based pluralism. Mol Psychiatry 2013;17:377‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kendler KS, Zachar P, Craver C. What kinds of things are psychiatric disorders? Psychol Med 2011;41:1143‐50. [DOI] [PubMed] [Google Scholar]
- 5. Borsboom D. Psychometric perspectives on diagnostic systems. J Clin Psychol 2008;64:1089‐108. [DOI] [PubMed] [Google Scholar]
- 6. Cramer AOJ, Waldorp LJ, van der Maas HLJ et al. Comorbidity: a network perspective. Behav Brain Sci 2010;33:137‐93. [DOI] [PubMed] [Google Scholar]
- 7. Borsboom D. Mental disorders, network models, and dynamical systems In: Kendler KS, Parnas J. (eds). Philosophical issues in psychiatry, Vol. 4: Nosology. Oxford: Oxford University Press; (in press). [Google Scholar]
- 8. Epskamp S, Cramer AOJ, Waldorp LJ et al. qgraph: network visualizations of relationships in psychometric data. J Stat Softw 2012;48:1‐18. [Google Scholar]
- 9. van Borkulo CD, Borsboom D, Epskamp S et al. A new method for constructing networks from binary data. Sci Rep 2014;4:5918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bringmann LF, Vissers N, Wichers M et al. A network approach to psychopathology: new insights into clinical longitudinal data. PLoS One 2013;8:e60188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Haslbeck J, Waldorp LJ. mgm: Structure Estimation for time‐varying mixed graphical models in high‐dimensional data. J Stat Softw (in press). [Google Scholar]
- 12. Costantini G, Epskamp S, Borsboom D et al. State of the art personality research: a tutorial on network analysis of personality data in R. J Res Pers 2014;54:13‐29. [Google Scholar]
- 13. Boschloo L, van Borkulo CD, Borsboom D et al. A prospective study on how symptoms in a network predict the onset of depression. Psychother Psychosom 2016;85:183‐4. [DOI] [PubMed] [Google Scholar]
- 14. Fried EI, Epskamp S, Nesse RM et al. What are ‘good’ depression symptoms? Comparing the centrality of DSM and non‐DSM symptoms of depression in a network analysis. J Affect Disord 2016;189:314‐20. [DOI] [PubMed] [Google Scholar]
- 15. Wichers M, Groot P, Simons CJP et al. Critical slowing down as a personalized early warning signal for depression. Psychother Psychosom 2016;85:114‐6. [DOI] [PubMed] [Google Scholar]
- 16. Fried EI, Bockting C, Arjadi R et al. From loss to loneliness: the relationship between bereavement and depressive symptoms. J Abnorm Psychol 2015;124:256‐65. [DOI] [PubMed] [Google Scholar]
- 17. Bringmann LF, Lemmens LHJM, Huibers MJH et al. Revealing the dynamic network structure of the Beck Depression Inventory‐II. Psychol Med 2016;45:747‐57. [DOI] [PubMed] [Google Scholar]
- 18. van Borkulo C, Boschloo L, Borsboom D et al. Association of symptom network structure with the course of depression. JAMA Psychiatry 2015;72:1219‐26. [DOI] [PubMed] [Google Scholar]
- 19. Cramer AOJ, Borsboom D, Aggen SH et al. The pathoplasticity of dysphoric episodes: differential impact of stressful life events on the pattern of depressive symptom inter‐correlations. Psychol Med 2011;42:957‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hoorelbeke K, Marchetti I, De Schryver M et al. The interplay between cognitive risk and resilience factors in remitted depression: a network analysis. J Affect Disord 2016;195:96‐104. [DOI] [PubMed] [Google Scholar]
- 21. Beard C, Millner AJ, Forgeard MJ et al. Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychol Med 2016;14:1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Heeren A, McNally RJ. An integrative network approach to Social Anxiety Disorder: the complex dynamic interplay among attentional bias for threat, attentional control, and symptoms. J Anx Disord 2016;42:95‐104. [DOI] [PubMed] [Google Scholar]
- 23. McNally RJ, Robinaugh DJ, Wu GWY et al. Mental disorders as causal systems: a network approach to Posttraumatic Stress Disorder. Clin Psychol Sci 2014;3:836‐49. [Google Scholar]
- 24. Robinaugh DJ, Leblanc NJ, Vuletich HA et al. Network analysis of persistent Complex Bereavement Disorder in conjugally bereaved adults. J Abnorm Psychol 2014;123:510‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Deserno MK, Borsboom D, Begeer S et al. Multicausal systems ask for multicausal approaches: a network perspective on subjective well‐being in individuals with autism spectrum disorder. Autism (in press). [DOI] [PubMed] [Google Scholar]
- 26. Ruzzano L, Borsboom D, Geurts HM. Repetitive behaviors in autism and obsessive‐compulsive disorder: new perspectives from a network analysis. J Autism Dev Disord 2014;45:192‐202. [DOI] [PubMed] [Google Scholar]
- 27. Isvoranu AM, van Borkulo CD, Boyette L et al. A network approach to psychosis: pathways between childhood trauma and psychotic symptoms. Schizophr Bull (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Isvoranu AM, Borsboom D, van Os J et al. A network approach to environmental impact in psychotic disorder: brief theoretical framework. Schizophr Bull 2016;42:870‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bak M, Drukker M, Hasmi L et al. An n=1 clinical network analysis of symptoms and treatment in psychosis. PLoS One 2016;11:e0162811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rhemtulla M, Fried EI, Aggen SH et al. Network analysis of substance abuse and dependence symptoms. Drug Alcohol Depend 2016;161:230‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Boschloo L, van Borkulo CD, Rhemtulla M et al. The network structure of symptoms of the Diagnostic and Statistical Manual of Mental Disorders. PLoS One 2015;10:e0137621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Boschloo L, Schoevers RA, van Borkulo CD et al. The network structure of psychopathology in a community sample of preadolescents. J Abnorm Psychol 2016;125:599‐606. [DOI] [PubMed] [Google Scholar]
- 33. Goekoop R, Goekoop JG. A network view on psychiatric disorders: network clusters of symptoms as elementary syndromes of psychopathology. PLoS One 2014;9:e112734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Borsboom D, Cramer AOJ, Schmittmann VD et al. The small world of psychopathology. PLoS One 2011;11:e27407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Tio P, Epskamp S, Noordhof A et al. Mapping the manuals of madness: comparing the ICD‐10 and DSM‐IV‐TR using a network approach. Int J Methods Psychiatr Res (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kossakowski JJ, Epskamp S, Kieffer JM et al. The application of a network approach to health‐related quality of life: introducing a new method for assessing HRQoL in healthy adults and cancer patients. Qual Life Res 2015;25:781‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cramer AOJ, van der Sluis S, Noordhof A et al. Dimensions of normal personality as networks in search of equilibrium: you can't like parties if you don't like people. Eur J Pers 2012;26:414‐31. [Google Scholar]
- 38. Woodward J. Making things happen: a theory of causal explanation. Oxford: Oxford University Press, 2003. [Google Scholar]
- 39. Pearl J. Causality: models, reasoning and inference. Cambridge: MIT Press, 2000. [Google Scholar]
- 40. Jokela M, Virtanen M, Batty GD. Inflammation and specific symptoms of depression. JAMA Psychiatry 2016;73:1‐6. [DOI] [PubMed] [Google Scholar]
- 41. Insel TR, Cuthbert BN. Brain disorders? Precisely. Science 2015;348:499‐500. [DOI] [PubMed] [Google Scholar]
- 42. Segal ZV, Williams JM, Teasdale JD et al. A cognitive science perspective on kindling and episode sensitization in recurrent affective disorder. Psychol Med 1996;26:371‐80. [DOI] [PubMed] [Google Scholar]
- 43. Wichers M, Geschwind N, van Os J et al. Scars in depression: is a conceptual shift necessary to solve the puzzle? Psychol Med 2009;40:359‐65. [DOI] [PubMed] [Google Scholar]
- 44. Kramer I, Simons CJP, Wigman JTW et al. Time‐lagged moment‐to‐moment interplay between negative affect and paranoia: new insights in the affective pathway to psychosis. Schizophr Bull 2014;40:278‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Nolen‐Hoeksema S, Watkins ER. A heuristic for developing transdiagnostic models of psychopathology. Explaining multifinality and divergent trajectories. Perspect Psychol Sci 2011;6:589‐609. [DOI] [PubMed] [Google Scholar]
- 46. Kim NS, Ahn W. Clinical psychologists’ theory‐based representations of mental disorders predict their diagnostic reasoning and memory. J Exp Psychol Gen 2002;131:451‐76. [PubMed] [Google Scholar]
- 47. Frewen PA, Allen SL, Lanius RA et al. Perceived Causal Relations: novel methodology for assessing client attributions about causal associations between variables including symptoms and functional impairment. Assessment 2012;19:480‐93. [DOI] [PubMed] [Google Scholar]
- 48. Frewen PA, Schmittmann VD, Bringmann LF et al. Perceived causal relations between anxiety, posttraumatic stress and depression: extension to moderation, mediation, and network analysis. Eur J Psychotraumatol 2013;4:20656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Myin‐Germeys I, Oorschot M, Collip D et al. Experience sampling research in psychopathology: opening the black box of daily life. Psychol Med 2009;39:1533‐47. [DOI] [PubMed] [Google Scholar]
- 50. Wigman JTW, Van Os J, Borsboom D et al. Exploring the underlying structure of mental disorders: cross‐diagnostic differences and similarities from a network perspective using both a top‐down and a bottom‐up approach. Psychol Med 2015;45:1‐13. [DOI] [PubMed] [Google Scholar]
- 51. Wichers M. The dynamic nature of depression: a new micro‐level perspective of mental disorder that meets current challenges. Psychol Med 2014;44:1349‐60. [DOI] [PubMed] [Google Scholar]
- 52. Bringmann LF, Madeline LP, Vissers N et al. Assessing temporal emotion dynamics using networks. Assessment (in press). [DOI] [PubMed] [Google Scholar]
- 53. Pe ML, Kircanski K, Thompson RJ et al. Emotion‐network density in major depressive disorder. Clin Psychol Sci 2015;3:292‐300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Krueger RF. The structure of common mental disorders. Arch Gen Psychiatry 1999;56:921‐6. [DOI] [PubMed] [Google Scholar]
- 55. Caspi A, Houts RM, Belsky DW et al. The p factor: one general psychopathology factor in the structure of psychiatric disorders? Clin Psychol Sci 2014;2:119‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Cramer AOJ. The glue of (ab)normal mental life: networks of interacting thoughts, feelings and behaviors. Doctoral dissertation, University of Amsterdam, 2013.
- 57. Cramer AOJ, van Borkulo CD, Giltay EJ et al. Major depression as a complex dynamic system. PLoS One (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. van der Maas HLJ, Molenaar PCM. Stagewise cognitive development: an application of catastrophe theory. Psychol Rev 1992;99:395‐417. [DOI] [PubMed] [Google Scholar]
- 59. Wakefield JC. The concept of disorder as a foundation for the DSM's theory‐neutral nosology: response to Folette and Houts, Part 2. Behav Res Ther 1999;10:1001‐27. [DOI] [PubMed] [Google Scholar]
- 60. Epskamp S, Maris G, Waldorp LJ et al. Network psychometrics In: Irwing P, Hughes D, Booth T. (eds). Handbook of psychometrics. New York: Wiley; (in press). [Google Scholar]
- 61. Marsman M, Maris G, Bechger T et al. Bayesian inference for low‐rank Ising networks. Sci Rep 2015;5:9050. [DOI] [PMC free article] [PubMed] [Google Scholar]


