Abstract
Background
It is unclear whether adult offenders with a history of attention deficit hyperactivity disorder (ADHD) are more likely to re-offend and, if so, in any specific offences.
Aim
To examine correlates of childhood ADHD symptoms among prisoners.
Methods
A randomly selected sample of 1,179 participants from the adult sentenced population of Puerto Rico (USA) reported their history of violent and non-violent offences, age of first arrest and reoffending. Participants completed retrospective measures of ADHD and a diagnostic interview for substance use disorders.
Results
Self-reported ADHD was associated with age of first arrest, a number of violent and non-violent offences and re-offending. The association with any non-violent offending was explained statistically by substance use disorders and other psychosocial covariates. ADHD was independently associated with being under 15 years of age at first arrest, and with re-offending.
Conclusions
Although some associations between ADHD and offending may be accounted for by comorbidity with substance use disorders, early onset of offending and repeated violent offending appear to be directly related to ADHD. Criminal justice policies should, therefore, incorporate ADHD screening accompanied by appropriate rehabilitation programmes when such neurodevelopmental disorder is identified.
Introduction
Attention deficit hyperactivity disorder (ADHD) starts before the age of 12 years and is characterized by symptoms of inattention, excessive physical activity and impulsivity(American Psychiatric Association, 2013) as well as executive dysfunction (Velez-Pastrana et al., 2015). The estimated prevalence of ADHD among adults in the USA is 4.4% (Kessler et al., 2006); worldwide the estimated prevalence according to meta-analysis is 2.5% (Simon et al., 2009). ADHD has been associated with higher than average rates of criminal behavior in several studies (Babinski et al., 1999; Barkley et al., 2004; Mannuzza et al., 2008; Satterfield et al., 2007). Adult criminal involvement may be the result of a developmental progression from childhood behavioural problems through adolescent delinquency to later offending (Babinski et al., 1999).
ADHD has also been identified as a risk factor for crime and delinquency later in life (Pratt et al., 2002). Significantly more hyperactive participants engage in various forms of antisocial activities by young adulthood than their control counterparts in follow-up studies (Barkley et al., 2004; Satterfield et al., 2007). Barkley et al. (2004), for example, reported that 40% of their hyperactive participants had been arrested at least twice, compared to 12% of their non-hyperactive group. In a 30-year longitudinal study, participants with ADHD had a greater number of arrests for any offence (44%), any felony (38.5%), and multiple felonies (26%) than controls (15%, 13%, and 8% respectively; (Satterfield et al., 2007). A significantly greater number of convictions and incarcerations was also reported in the hyperactive group. Given the nature of ADHD symptoms, offending related to it is most likely to be impulsive and reactive (Gonzalez et al., 2016) to satisfy an immediate need (Young, 2007). In addition, by nature of their cognitive impairments, people with ADHD seem more easily apprehended for their antisocial activities (Young & Thome, 2011).
International studies, variously from North America (Eyestone & Howell, 1994), Sweden (Ginsberg et al., 2010) and Germany (Rosler et al., 2004), have consistently reported a higher prevalence of childhood ADHD and ADHD symptoms among adult prisoners. A systematic review and meta-analysis confirmed that prevalence may be as high as 26 per hundred (Young et al., 2015). Various studies have also found that participants with childhood disturbance of attention and activity were convicted at an earlier age than those without these symptoms (Dalteg et al., 1999; Rosler et al., 2004). Earlier arrests linked with positive ADHD screening have also been associated with increased likelihood of reoffending (Gonzalez et al., 2016).
Another moderating factor is the extent of substance use disorders (SUD), which have also been consistently linked with ADHD across several studies (Clure et al., 1999; Ginsberg et al., 2010; Gonzalez et al., 2015). Mannuzza et al. (2008) reported that substance use disorders remain a significant predictor of criminality after allowing for the confounding effects of antisocial personality disorder (ASPD). In another study, adolescent drug use was the main contributor to drug-related crime by young adulthood (Barkley et al., 2004). In the UK opiate dependence amongst prisoners with ADHD was a significant predictor of acquisitive offending (Young et al., 2011).
In the study we report here, we conducted secondary analysis of a representative sample of the Puerto Rican sentenced prisoners. We examined the correlates of childhood ADHD symptoms and signs with early criminal offending, re-incarceration rates and types of offending. The age of criminal responsibility in Puerto Rico is 18 years unless otherwise specified by the juvenile law (Puerto Rico’s Penal Code, 2012). We hypothesized that: (1) retrospectively recognised childhood ADHD symptoms and signs would be associated with proportionately more incarcerations and earlier onset of criminal activity; (2) prisoners with ADHD would have committed proportionately more specific violent and non-violent crimes; (3) the ADHD group would have a higher number of violent and non-violent crimes overall than the non-ADHD group; and (4) substance use disorders would be more likely to account for some offending outcomes in the ADHD group.
Methods
The study was reviewed and approved by the University of Puerto Rico Medical Sciences Campus Institutional Review Board.
Participants and procedures
We used data from a 2004 cross-sectional survey of sentenced inmates in the state prisons of Puerto Rico (PR), designed to assess drug treatment needs and inform prevention strategies for blood-borne pathogens (Albizu-Garcia et al., 2012; Pena-Orellana et al., 2011). The study sample consisted of 1,331 randomly selected sentenced inmates from 26 of the 39 institutions in the Puerto Rican prison system, representing 13% of the total sentenced inmate population. Details of the sampling procedures have been described elsewhere (Albizu-Garcia et al., 2012). In brief, after orientation, inmates who provided oral consent to participate were interviewed, and their data anonymised. A total of 1,179 inmates participated, representing an 89% response rate. Two computerized interview modalities were used for data gathering: CAPI (Computer Assisted Personal Interview) and ACASI (Audio Computer Assisted Self Interview). ACASI has been shown to increase disclosure of risk behaviors among injecting drug users (Des Jarlais et al., 1999; Perlis et al., 2004) and in individuals seropositive for HIV (Macalino et al., 2002; Simoes et al., 2006). Trained interviewers conducted the computerized personal interview and were available to answer questions during the self-administered procedure.
Measures
Offending history and reoffending
Sociodemographic covariates included in the study were gender, age, education level and history of placement in foster care and/or local authority. Offending history included early onset criminal activity (coded as first arrest before age 15), number of previous incarcerations, which for our purposes here we defined as recidivism, and number of types of violent and non-violent offences. Violent crimes included armed robbery, aggression, rape, attempted murder, threatening with a weapon, arson, and murder; non-violent crimes included burglary, theft, drug possession, drug trafficking, possession of an illegal firearm, prostitution, vandalism, and fraud. Criminal history was entirely from self-report.
ADHD symptoms
The Spanish-language version of the Wender Utah Rating Scale (WURS)(González & Vélez Pastrana, 2007) was completed by all participants. This is a self-rating instrument for retrospective assessment of features of ADHD (Ward, Wender, & Reimherr, 1993). These are rated on a 5-point Likert scale, ranging from 0 (“not at all or very slightly”) to 4 (“very much”). The WURS authors originally suggested 36 and 46 cut-off scores, the latter associated with greater specificity. Considering the high indices of psychopathology and comorbidity amongst inmate populations, we used the stricter 46 cut-score, as recommended by (Gudjonsson et al., 2009; Ward et al., 1993). The instrument’s psychometric properties have been extensively documented, including construct and discriminant validity, and internal and test retest reliability (>0.92)(González & Vélez Pastrana, 2007; McCann et al., 2000).
Analytical strategy
Weighted percentages were reported on all categorical variables. Associations between groups based on the binary WURS classification were established using logistic regression with odds ratios (OR) as the measure of their effect size. To examine associations with number of previous incarcerations and number of violent and non-violent crimes we used ordinal logistic regression. The latter was preferred in favour of models for count data because these variables were recoded in ordered categorical format (e.g. 0 “never”, 1 “sometimes”, 2 “often”). Multiple categorical predictor covariates (e.g. education level) were assigned a reference category against which other categories were contrasted.
We examined interaction effects of gender on the associations between features of ADHD and number of violent and non-violent offences.
All statistical analyses are presented both unadjusted and adjusted by including covariates in each model simultaneously. Adjustments for previous and repeated offences included age, gender, education level and age of first arrest. For modeling number of classes of criminal offences, we adjusted for age, gender and education level, and lifetime substance abuse/dependence, where age of first arrest was used as a proxy measure of likelihood of early conduct problems. All analyses were weighted to account for the characteristics of sampling and the target population. Details of the procedures used in weighting have previously been described (Pena-Orellana et al., 2011). All analyses were performed using STATA 13 (StataCorp.).
Results
Demographic characteristics
Two hundred and sixty-seven (21%) prisoners screened positive for features of ADHD in childhood. About one third of the women screened positive, but just one fifth of the men (Table 1). The oldest age group (≥ 35) had the lowest proportion of inmates who screened positive for childhood ADHD symptoms.
Table 1.
Sample demographic characteristics and associations with retrospective ADHD classification (N = 1,179)
| Characteristics | ADHD WURS (≥ 46) | OR (95% CI) | p-value | |||
|---|---|---|---|---|---|---|
| No | Yes | |||||
|
| ||||||
| N | % | n | % | |||
| Gender | ||||||
| Male | 761 | 79.1 | 198 | 20.9 | Ref. | - |
| Female | 151 | 67.2 | 69 | 32.8 | 1.85 (1.17, 2.91) | 0.011 |
| Age (groups) | ||||||
| 18–24 yrs | 196 | 72.4 | 81 | 27.6 | Ref. | - |
| 25–34 yrs | 437 | 79.4 | 124 | 20.6 | 0.68 (0.39, 1.20) | 0.17 |
| ≥ 35 yrs | 279 | 82.5 | 62 | 17.5 | 0.56 (0.37, 0.85) | 0.01 |
| Education | ||||||
| ≤ 6th (grade) | 69 | 63.9 | 47 | 36.1 | 2.91 (1.41, 6.00) | 0.007 |
| 7th to 9th | 237 | 71.8 | 95 | 28.2 | 2.02 (1.51, 2.71) | <0.001 |
| > 9th to < 12th | 153 | 82.7 | 31 | 17.3 | 1.08 (0.60, 1.93) | 0.79 |
| High School | 306 | 83.8 | 71 | 16.2 | Ref. | - |
| University | 147 | 86.0 | 22 | 14.0 | 0.84 (0.55, 1.27) | 0.39 |
| Experience | ||||||
| Foster care | ||||||
| No | 869 | 80.9 | 225 | 19.1 | Ref. | - |
| Yes | 42 | 47.3 | 42 | 52.7 | 4.71 (2.62, 8.49) | <0.001 |
| Nationality | ||||||
| Puerto Rico | 792 | 78.4 | 237 | 21.6 | Ref. | - |
| North America | 101 | 79.4 | 26 | 20.6 | 0.94 (0.66, 1.35) | 0.73 |
| Cuba and DR | 16 | 88.8 | 2 | 11.2 | 0.46 (0.09, 2.38) | 0.33 |
| Other incl. EU | 3 | 74.5 | 2 | 25.5 | 1.24 (0.14, 10.77) | 0.83 |
| Total | 912 | 78.7 | 267 | 21.3 | - | - |
Note: DR- Dominican Republic; EU- European Union; WURS- Wender Utah Rating Scale
All weighted percentages and estimates
Lower education levels were associated with higher rates of ADHD, using high school as the reference category. The group that had completed only up to 6 years of schooling was three times as likely to reach the 46-point cut-off on the WURS. More than half (53%) of inmates who reported having been under the care of the state or placed in foster care also screened positive for ADHD in childhood, with more than a four-fold increase in the odds (p < 0.001).
Associations with incarceration history
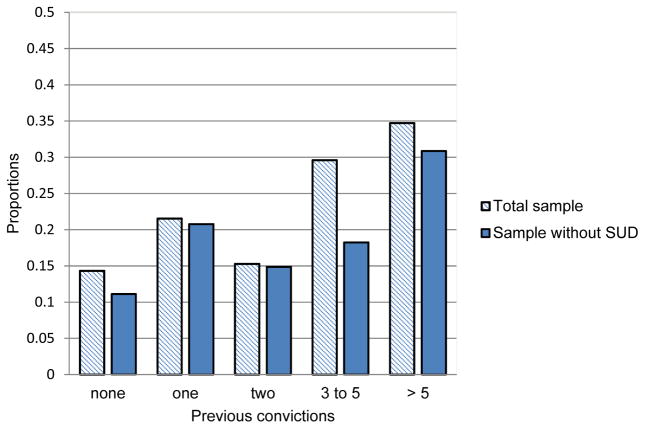
Table 2 shows that childhood ADHD symptoms are significantly associated with first arrest before age 15, after adjusting for age, gender and education (p < 0.05). ADHD symptoms in childhood were associated with a two-fold increase in the likelihood of an inmate being a repeat offender (p < 0.001). An ordinal logistic regression model, adjusted for socio-demographic characteristics and age of first arrest, shows a linear association between childhood ADHD features and number of previous incarcerations (p < 0.001). Figure 1 provides a graphical representation of this showing that the proportion of inmates who screened positive for childhood ADHD increases for each category of number of previous incarcerations (F = 6.35, p < 0.001). On repeating the bivariate analysis only with inmates who did not have substance use disorders, we found that the relationships between ADHD and previous incarcerations was no longer significant (F = 2.06, p = 0.08).
Table 2.
Incarceration and criminal history in association with retrospective ADHD classification (N = 1,179)
| Outcomes | ADHD WURS (≥ 46)
|
|||||
|---|---|---|---|---|---|---|
| n | % | OR (95% CI) | p-value | aOR (95% CI)b | p-value | |
| Early criminal activity | ||||||
| ≥ 15 yr | 83 | 15.8 | Ref. | Ref. | ||
| < 15 yr | 167 | 25.7 | 1.85 (1.29, 2.65) | 0.002 | 1.76 (1.17, 2.67) | 0.01 |
| Number of incarcerationsa, c | ||||||
| None | 69 | 14.3 | 2.06 (1.51, 2.82) | <0.001 | 2.04 (1.47, 2.82) | <0.001 |
| Once | 47 | 21.6 | ||||
| Twice | 35 | 15.3 | ||||
| 3 –5 times | 67 | 29.6 | ||||
| 5 > times | 48 | 34.7 | ||||
| Previous incarceration | ||||||
| No | 69 | 14.3 | Ref. | Ref. | ||
| Yes | 197 | 24.7 | 1.96 (1.51, 2.55) | <0.001 | 1.96 (1.42, 2.71) | <0.001 |
Ordinal logistic regression for this outcome, otherwise logistic regressions
Adjusted for age, gender, education level and
Adjusted forb and age of first arrest (early criminal activity)
Figure 1. Number of previous incarcerations among inmates with childhood ADHD symptoms (WURS ≥ 46).
Shown is the linear increase of number of previous incarcerations among inmates with childhood ADHD positive screening in the total sample (F = 6.35, p < 0.001), and those with childhood ADHD positive screening in a subsample of inmates without a history of substance use disorders (F = 2.06, p = 0.08).
Childhood ADHD symptoms and violent and non-violent offending
Baseline models for associations between ADHD and individual categories of self-reported violent and non-violent offences were adjusted for demographic characteristics and for age of first arrest before 15. Those who reported features of ADHD were also more likely to have been convicted of rape or attempted murder, after adjustments (Table 3). Childhood ADHD symptoms were also associated with total number of violent offences (OR 1.46 [1.05, 2.04] p < 0.05). Again, after examining the explanatory role of lifetime SUD (OR 1.63 [1.37, 1.94] p <0.001) the association was no longer evident (OR 1.35 [0.94, 1.93] p <0.10) (Table 4).
Table 3.
Self-reported offending and childhood ADHD symptoms (N = 1,179)
| Offense type | ADHD WURS (≥ 46)
|
||
|---|---|---|---|
| N (%) | OR (95% CI)a | aOR (95% CI)b | |
| Violent, P% | |||
| Armed robbery, 72.6 | 202 (79.3) | 1.69(0.97, 2.93) | 1.30(0.73, 2.31) |
| Aggression, 40.8 | 123 (47.4) | 1.45(1.15, 1.82)** | 1.17(0.90, 1.52) |
| Rape, 3.0 | 19 (5.7) | 3.04(1.44, 6.42)** | 3.03(1.20, 7.68)* |
| Attempted murder, 33.6 | 105 (42.1) | 1.62(1.27, 2.08)** | 1.40(1.05, 1.87)* |
| Threaten w/weapon, 47.8 | 133 (54.2) | 1.43(0.90, 2.27) | 1.17(0.69, 1.98) |
| Arson, 16.0 | 51 (21.1) | 1.47(0.99, 2.20) | 1.17(0.74, 1.86) |
| Murder, 25.2 | 67 (30.4) | 1.41(1.14, 1.75)** | 1.19(0.95, 1.49) |
| Count violent typesc | - | 1.93(1.45, 2.56)*** | 1.46(1.05, 2.04)*¶† |
| Non- Violent, P% | |||
| Burglary, 53.7 | 151 (63.7) | 1.67(1.21, 2.31)** | 1.34(1.01, 1.78)*§ |
| Theft, 61.5 | 179 (73.4) | 1.95(1.30, 2.93)** | 1.66(1.06, 2.60)*¶ |
| Drug possession, 68.3 | 183 (71.9) | 1.26(0.82, 1.94) | 0.94(0.58, 1.54) |
| Drug trafficking, 72.5 | 205 (80.0) | 1.64(0.87, 3.10) | 1.29(0.65, 2.57) |
| Poss.Illegal firearm, 72.5 | 190 (77.9) | 1.53(1.06, 2.22)* | 1.10(0.69, 1.74) |
| Prostitution, 15.5 | 63 (21.8) | 1.82(0.94, 3.54) | 1.64(0.76, 3.54) |
| Vandalism, 34.8 | 110 (45.6) | 1.74(1.26, 2.39)** | 1.53(1.02, 2.31)*¶ |
| Fraud, 19.7 | 50 (22.5) | 1.35(0.99, 1.84) | 1.22(0.87, 1.71) |
| Count non-violent typesc | - | 1.83(1.26, 2.67)** | 1.42(0.98, 2.07)§ |
Baseline logistic regression models adjusted for age, gender and education
Adjusted for a and age of first arrest (i.e., early criminal onset)
Ordinal logistic regression for these outcomes
Effect explained by lifetime SUD
Lifetime SUD significant correlate
Significant interaction by gender
Table 4.
Self-reported convictions and childhood ADHD symptoms (N = 1,179)
| Offense type | ADHD WURS (≥ 46)
|
||
|---|---|---|---|
| N (%) | OR (95% CI)a | aOR (95% CI)b | |
| Violent, P% | |||
| Armed robbery, 52.9 | 149 (59.0) | 1.43(0.79, 2.57) | 1.23(0.62, 2.43) |
| Aggression, 15.0 | 57 (20.0) | 1.67(1.13, 2.48)* | 1.48(0.99, 2.23) |
| Rape, 0.2 | 1 (0.2) | -- | -- |
| Attempted Murder, 7.5 | 19 (8.4) | 1.16(0.62, 2.17) | 1.02(0.50, 2.07) |
| Threaten w/weapon, 22.7 | 63 (25.5) | 1.25(0.93, 1.67) | 1.08(0.82, 1.43) |
| Arson, 1.6 | 5 (1.4) | 0.74(0.14, 3.99) | 0.63(0.12, 3.25) |
| Murder, 12.3 | 38 (13.6) | 1.19(0.71, 2.01) | 1.11(0.69, 1.79) |
| Count violent typesc | - | 1.40(1.08, 1.82)* | 1.22(0.84, 1.76) |
| Non- Violent, P% | |||
| Burglary, 36.1 | 97 (39.9) | 1.17(0.88, 1.56) | 1.03(0.80, 1.34) |
| Theft, 19.0 | 68 (25.0) | 1.49(0.64, 3.46) | 1.40(0.61, 3.22) |
| Drug possession, 37.4 | 111 (41.0) | 1.18(0.84, 1.67) | 1.02(0.66, 1.55) |
| Drug trafficking, 36.8 | 107 (40.3) | 1.18(0.79, 1.75) | 1.04(0.71, 1.52) |
| Poss. Illegal firearm, 33.1 | 87 (34.6) | 1.16(0.82, 1.65) | 1.03(0.72, 1.47) |
| Prostitution, 0.9 | 9 (1.6) | 1.46(0.13, 16.52) | 1.68(0.11, 26.25) |
| Vandalism, 11.2 | 41 (20.0) | 2.23(1.32, 3.77)** | 2.01(1.17, 3.44)*§ |
| Fraud, 4.7 | 12 (6.8) | 1.83(0.92, 3.63) | 1.70(0.87, 3.35) |
| Count non-violent typesc | - | 1.45(1.01, 2.09)* | 1.25(0.81, 1.91)§ |
Baseline logistic regression models adjusted for age, gender and education
Adjusted for a and age of first arrest (i.e., early criminal onset)
Ordinal logistic regression for these outcomes
Lifetime SUD significant correlate
An effect modification test by gender showed significantly higher odds of violent offences among women screening positive for ADHD (OR 1.88 [1.15, 3.05] p < 0.05).
Adjusted models for non-violent offending show that features of ADHD were significantly associated with burglary, theft and vandalism, but so were substance use disorders (OR 3.77 [2.55, 5.56] p <0.001). Again, after introducing these into the statistical models, ADHD was no longer related.
Discussion
Our first hypothesis that retrospectively self-reported features of ADHD would be associated with a higher number of incarcerations and early onset of criminal activity amongst prison inmates was sustained. Features of ADHD were also associated with history of any repeated incarcerations, total number of offending and conviction categories, indicating versatility in offending patterns. The latter were, however, mainly explained by comorbid substance misuse in adjusted models. Our second hypothesis was only partly confirmed in that only female inmates appeared to be more likely to report both violent offending and features of ADHD. There is currently a wealth of evidence of that ADHD is a risk factor for substance use disorders and that, perhaps together with conduct disorder, this may form part of a pathway to delinquency. Gittelman and colleagues reported on the arrest rates of 103 hyperactive people at several time points (Mannuzza et al., 1991; Mannuzza et al., 1993; Mannuzza et al., 1998; Mannuzza et al., 2008). At their 26–32 years follow-up, adults with a history of hyperactivity were more likely to have been arrested (47% vs. 24%) and convicted (42% vs. 14%) than those without. More recently, Klein et al. (2012) reported a 65% arrest rate from two cohort studies over an average follow-up of 33 years; one third (36%) of those originally diagnosed as hyperactive were incarcerated compared with just 12% of those not so diagnosed. In this cohort, those with hyperactivity consistently preceded substance use disorders at 16 (Mannuzza et al., 1993), 17 (Mannuzza et al., 1998) and 33 (Klein et al., 2012) years follow-up, confirming that early ADHD symptoms and their persistence are a risk factor for SUD.
We found that a linear increase in prevalence of violent offending related to ADHD symptoms was higher among women than in men. According to the ‘group resistance hypothesis’ (Sellin, 1938), women are thought less likely to engage in violence, according to socially constructed gender roles. Men would therefore be expected to perpetrate more violence in this population sample. The symptom by gender interaction shows that ADHD may upset this usual relationship, putting women at disproportionate risk of becoming violent.
Inmates with early features of ADHD were almost twice as likely to have early onset of criminal activity compared with those without ADHD. This finding is consistent with other studies (Dalteg et al., 1999; Retz et al., 2004). It was also corroborated by our analyses demonstrating that, as the number of previous incarcerations increased, so the proportion of inmates with ADHD symptoms also increased. It seems logical to think that this may be a result of rushing to action without much thought, it may not be the ADHD per se which underpins this problem. The relationship was not significant without a comorbid substance use disorders, an indication that involvement in these types of crimes may be influenced by substance-seeking behavior among those with ADHD. In particular, violent and non-violent offending appears to be better accounted for by comorbidity with SUD, as has been reported elsewhere (Ginsberg et al., 2010; Young et al., 2011).
For specific types of offending that did not necessarily lead to incarceration, associations were limited to arrests for attempted murder and rape; these associations were not present when analyses were based on actual convictions. These categories of violent offending may be more reactive-impulsive acts than premeditated or instrumental. Retz & Rösler (2009) have argued in favour of a particular association between reactive types of violence and ADHD. Because we lack details on the specific context of these offences in our sample, however, we could not classify them in this way, so these findings should be interpreted with caution. No other specific categories of offending were associated with ADHD after adjusting for early onset criminality, whilst some were better explained by substance use disorders, which seemed to account better for the linear increase observed between ADHD symptoms and number of previous incarcerations. A potential pathway to offending for these people is likely to be through substance misuse. Once they become intertwined in the criminal justice system, they also become more vulnerable to the emergence of further comorbidity (Gonzalez et al., 2015; Young et al., 2015), perhaps developing ever more serious forms of substance use disorders and, unless the cycle is interrupted, offending is likely to persist.
After having been imprisoned for any length of time, offenders with psychiatric disorders including personality disorders or substance use disorders, may become dependent upon a highly structured lifestyle. Being suddenly released to the community may pose overwhelming stress, decreasing the likelihood of their success in the community, and increasing the probability of their return to either the criminal justice or mental health services (Roesch et al., 1995). Aftercare programmes may provide the most suitable environment for offenders generally at high risk of recidivism, and are probably more effective in predominantly violent samples (James et al., 2013). Individualised interventions appear to be the most effective in decreasing recidivism (James et al., 2013), therefore it is very important to screen for ADHD as well as other conditions and to provide specific treatment for it.
Limitations
The data for our study was prisoners and based entirely on self-report. Since official criminal records or collateral reports were not available, the information on criminal history could not be corroborated, and recall biases could have been present. In addition, the instrument used (WURS) evaluates the presence of childhood symptoms when those being asked to complete it are adult, a process that could be very vulnerable to this type of bias. Another limitation of the WURS is the fact that it is not strictly based on DSM-IV criteria. Research in this context has shown limitations of using screening tools that are not based on diagnostic criteria (Young et al., 2016). Comorbidity between ADHD and conduct disorder is high, and in the prison context any associations with offending may have been better explained by this comorbidity. Future studies of this type should measure both conditions and attempt differentiation of their effects.
The cross-sectional design of the study does not allow any conclusions on causal associations between ADHD and offending outcomes, nor the actual mediating effects of early arrest and/or substance misuse on these associations.
Despite the limitations discussed, our study has several advantages. It was conducted with a random sample of sentenced prisoners in the Puerto Rican Correctional System, who were also representative of them. Furthermore, we used interview techniques that encourage truthful responses (Pena-Orellana et al., 2011), such as computer-assisted interviews. This mitigated the effects that the unavailability of official offence records and collateral reports can have on the truthfulness of the data.
Conclusions
Our findings do not support a direct association between ADHD and specific types of offending. ADHD was more associated with early onset of offending and the suggestion from this cross-sectional study is that the link might be better explained by comorbid conditions such as substance use disorders. Research that allows estimation of indirect paths is essential to elucidate this relationship. Further research on ADHD and its comorbidities is needed, given its high prevalence of among prisoners. Clarification of these relationships has important implications for prevention and treatment.
Acknowledgments
This research was partly supported by a grant from the National Institute on Drug Abuse (NIDA 5R24DA024868-05, C. Albizu).
Footnotes
The authors have no conflicts of interest to declare.
References
- Albizu-Garcia CE, Caraballo JN, Caraballo-Correa G, Hernandez-Viver A, Roman-Badenas L. Assessing need for medication-assisted treatment for opiate-dependent prison inmates. Subst Abus. 2012;33(1):60–69. doi: 10.1080/08897077.2011.620462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: Author; 2013. [Google Scholar]
- Babinski LM, Hartsough CS, Lambert NM. Childhood conduct problems, hyperactivity-impulsivity, and inattention as predictors of adult criminal activity. J Child Psychol Psychiatry. 1999;40(3):347–355. [PubMed] [Google Scholar]
- Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult follow-up of hyperactive children: antisocial activities and drug use. Journal of Child Psychology and Psychiatry. 2004;45(2):195–211. doi: 10.1111/j.1469-7610.2004.00214.x. [DOI] [PubMed] [Google Scholar]
- Clure C, Brady KT, Saladin ME, Johnson D, Waid R, Rittenbury M. Attention-deficit/hyperactivity disorder and substance use: symptom pattern and drug choice. Am J Drug Alcohol Abuse. 1999;25(3):441–448. doi: 10.1081/ada-100101871. [DOI] [PubMed] [Google Scholar]
- Dalteg A, Lindgren M, Levander S. Retrospectively rated ADHD is linked to specific personality characteristics and deviant alcohol reactions. The Journal of Forensic Psychiatry. 1999;10(3):623–634. [Google Scholar]
- Des Jarlais DC, Paone D, Milliken J, Turner CF, Miller H, Gribble J, … Friedman SR. Audio-computer interviewing to measure risk behaviour for HIV among injecting drug users: a quasi-randomised trial. Lancet. 1999;353(9165):1657–1661. doi: 10.1016/s0140-6736(98)07026-3. [DOI] [PubMed] [Google Scholar]
- Eyestone LL, Howell RJ. An epidemiological study of attention-deficit hyperactivity disorder and major depression in a male prison population. Bull Am Acad Psychiatry Law. 1994;22(2):181–193. [PubMed] [Google Scholar]
- Ginsberg Y, Hirvikoski T, Lindefors N. Attention Deficit Hyperactivity Disorder (ADHD) among longer-term prison inmates is a prevalent, persistent and disabling disorder. BMC Psychiatry. 2010;10:112. doi: 10.1186/1471-244X-10-112. 1471-244X-10-112 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez RA, Gudjonsson GH, Wells J, Young S. The Role of Emotional Distress and ADHD on Institutional Behavioral Disturbance and Recidivism Among Offenders. J Atten Disord. 2016;20(4):368–378. doi: 10.1177/1087054713493322. [DOI] [PubMed] [Google Scholar]
- González RA, Vélez Pastrana MC. Propiedades psicométricas de la escala de autoinforme Wender Utah Rating Scale para la evaluación de síntomas del tdah en adultos/as puertorriqueños/as [Psychometric properties of the Wender Utah Rating Scale for the assessment of ADHD symptoms in Puerto Rican adults] Ciencias de la Conducta. 2007;23:159–186. [Google Scholar]
- Gonzalez RA, Velez-Pastrana MC, Ruiz Varcarcel JJ, Levin FR, Albizu-Garcia CE. Childhood ADHD symptoms are associated with lifetime and current illicit substance-use disorders and in-site health risk behaviors in a representative sample of Latino prison inmates. J Atten Disord. 2015;19(4):301–312. doi: 10.1177/1087054712461690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gudjonsson G, Sigurdsson JF, Young S, Newton AK, Peersen M. Attention Deficit Hyperactivity Disorder (ADHD). How do ADHD symptoms relate to personality among prisoners? Personality and Individual Differences. 2009;47:64–68. [Google Scholar]
- James C, Stams GJ, Asscher JJ, De Roo AK, der Laan PH. Aftercare programs for reducing recidivism among juvenile and young adult offenders: a meta-analytic review. Clin Psychol Rev. 2013;33(2):263–274. doi: 10.1016/j.cpr.2012.10.013. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, … Zaslavsky AM. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. American Journal of Psychiatry. 2006;163(4):716–723. doi: 10.1176/appi.ajp.163.4.716. 163/4/716 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein RG, Mannuzza S, Olazagasti MA, Roizen E, Hutchison JA, Lashua EC, Castellanos FX. Clinical and functional outcome of childhood attention-deficit/hyperactivity disorder 33 years later. Arch Gen Psychiatry. 2012;69(12):1295–1303. doi: 10.1001/archgenpsychiatry.2012.271. 1378851 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macalino GE, Celentano DD, Latkin C, Strathdee SA, Vlahov D. Risk behaviors by audio computer-assisted self-interviews among HIV-seropositive and HIV-seronegative injection drug users. AIDS Educ Prev. 2002;14(5):367–378. doi: 10.1521/aeap.14.6.367.24075. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Klein RG, Addalli KA. Young adult mental status of hyperactive boys and their brothers: a prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 1991;30(5):743–751. [PubMed] [Google Scholar]
- Mannuzza S, Klein RG, Bessler A, Malloy P, LaPadula M. Adult outcome of hyperactive boys. Educational achievement, occupational rank, and psychiatric status. Archives of General Psychiatry. 1993;50(7):565–576. doi: 10.1001/archpsyc.1993.01820190067007. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Klein RG, Bessler A, Malloy P, LaPadula M. Adult psychiatric status of hyperactive boys grown up. Am J Psychiatry. 1998;155(4):493–498. doi: 10.1176/ajp.155.4.493. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Klein RG, Moulton JL., 3rd Lifetime criminality among boys with attention deficit hyperactivity disorder: a prospective follow-up study into adulthood using official arrest records. Psychiatry Research. 2008;160(3):237–246. doi: 10.1016/j.psychres.2007.11.003. S0165-1781(07)00397-6 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCann BS, Scheele L, Ward N, Roy-Byrne P. Discriminant validity of the Wender Utah Rating Scale for attention-deficit/hyperactivity disorder in adults. J Neuropsychiatry Clin Neurosci. 2000;12(2):240–245. doi: 10.1176/jnp.12.2.240. [DOI] [PubMed] [Google Scholar]
- Pena-Orellana M, Hernandez-Viver A, Caraballo-Correa G, Albizu-Garcia CE. Prevalence of HCV risk behaviors among prison inmates: tattooing and injection drug use. J Health Care Poor Underserved. 2011;22(3):962–982. doi: 10.1353/hpu.2011.0084. S1548686911300186 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlis TE, Des Jarlais DC, Friedman SR, Arasteh K, Turner CF. Audio-computerized self-interviewing versus face-to-face interviewing for research data collection at drug abuse treatment programs. Addiction. 2004;99(7):885–896. doi: 10.1111/j.1360-0443.2004.00740.x. [DOI] [PubMed] [Google Scholar]
- Pratt TC, Cullen FT, Blevins KR, Daigle L, Unnever FD. The relationship of Attention Deficit Hyperactivity Disorder to crime and delinquency: a meta-analysis. International Journal of Police Science & Management. 2002;4(4) [Google Scholar]
- Retz W, Retz-Junginger P, Hengesch G, Schneider M, Thome J, Pajonk FG, … Rosler M. Psychometric and psychopathological characterization of young male prison inmates with and without attention deficit/hyperactivity disorder. European Archives of Psychiatry and Clinical Neuroscience. 2004;254(4):201–208. doi: 10.1007/s00406-004-0470-9. [DOI] [PubMed] [Google Scholar]
- Retz W, Rosler M. The relation of ADHD and violent aggression: What can we learn from epidemiological and genetic studies? International Journal of Law and Psychiatry. 2009;32(4):235–243. doi: 10.1016/j.ijlp.2009.04.006. S0160-2527(09)00049-1 [pii] [DOI] [PubMed] [Google Scholar]
- Roesch R, Ogloff JR, Eaves D. Mental health research in the criminal justice system: The need for common approaches and international perspectives. Int J Law Psychiatry. 1995;18(1):1–14. doi: 10.1016/0160-2527(94)00023-9. 0160-2527(94)00023-9 [pii] [DOI] [PubMed] [Google Scholar]
- Rosler M, Retz W, Retz-Junginger P, Hengesch G, Schneider M, Supprian T, … Thome J. Prevalence of attention deficit-/hyperactivity disorder (ADHD) and comorbid disorders in young male prison inmates. European Archives of Psychiatry and Clinical Neuroscience. 2004;254(6):365–371. doi: 10.1007/s00406-004-0516-z. [DOI] [PubMed] [Google Scholar]
- Satterfield JH, Faller KJ, Crinella FM, Schell AM, Swanson JM, Homer LD. A 30-year prospective follow-up study of hyperactive boys with conduct problems: adult criminality. J Am Acad Child Adolesc Psychiatry. 2007;46(5):601–610. doi: 10.1097/chi.0b013e318033ff59. S0890-8567(09)61719-6 [pii] [DOI] [PubMed] [Google Scholar]
- Sellin T. Culture conflict and crime. American Journal of sociology. 1938;44(1):97–103. [Google Scholar]
- Simoes AA, Bastos FI, Moreira RI, Lynch KG, Metzger DS. A randomized trial of audio computer and in-person interview to assess HIV risk among drug and alcohol users in Rio De Janeiro, Brazil. J Subst Abuse Treat. 2006;30(3):237–243. doi: 10.1016/j.jsat.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Simon V, Czobor P, Balint S, Meszaros A, Bitter I. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. British Journal of Psychiatry. 2009;194(3):204–211. doi: 10.1192/bjp.bp.107.048827. 194/3/204 [pii] [DOI] [PubMed] [Google Scholar]
- Velez-Pastrana MC, Gonzalez RA, Rodriguez Cardona J, Purcell Baerga P, Alicea Rodriguez A, Levin FR. Psychometric Properties of the Barkley Deficits in Executive Functioning Scale: A Spanish-Language Version in a Community Sample of Puerto Rican Adults. Psychol Assess. 2015 doi: 10.1037/pas0000171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward MF, Wender PH, Reimherr FW. The Wender Utah Rating Scale: an aid in the retrospective diagnosis of childhood attention deficit hyperactivity disorder. Am J Psychiatry. 1993;150(6):885–890. doi: 10.1176/ajp.150.6.885. [DOI] [PubMed] [Google Scholar]
- Young S. Forensic aspects of ADHD. In: Bellgrove M, Fitgerald M, Gill M, editors. The handbook of attention deficit hyperactivity disorder. Chichester: John Wiley & Sons Ltd; 2007. pp. 91–108. [Google Scholar]
- Young S, Gonzalez RA, Mutch L, Mallet-Lambert I, O’Rourke L, Hickey N, … Gudjonsson GH. Diagnostic accuracy of a brief screening tool for attention deficit hyperactivity disorder in UK prison inmates. Psychol Med. 2016;46(7):1449–1458. doi: 10.1017/S0033291716000039. [DOI] [PubMed] [Google Scholar]
- Young S, Moss D, Sedgwick O, Fridman M, Hodgkins P. A meta-analysis of the prevalence of attention deficit hyperactivity disorder in incarcerated populations. Psychol Med. 2015;45(2):247–258. doi: 10.1017/S0033291714000762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young S, Sedgwick O, Fridman M, Gudjonsson G, Hodgkins P, Lantigua M, Gonzalez RA. Co-morbid psychiatric disorders among incarcerated ADHD populations: a meta-analysis. Psychol Med. 2015;45(12):2499–2510. doi: 10.1017/S0033291715000598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young S, Thome J. ADHD and offenders. World J Biol Psychiatry. 2011;12(Suppl 1):124–128. doi: 10.3109/15622975.2011.600319. [DOI] [PubMed] [Google Scholar]
- Young S, Wells J, Gudjonsson GH. Predictors of offending among prisoners: the role of attention-deficit hyperactivity disorder and substance use. Journal of Psychopharmacology. 2011;25(11):1524–1532. doi: 10.1177/0269881110370502. 0269881110370502 [pii] [DOI] [PubMed] [Google Scholar]