Abstract
Objective
To identify and describe new roles for medical assistants (MAs) in innovative care models that improve care while providing training and career advancement opportunities for MAs.
Data Sources/Study Setting
Primary data collected at 15 case study sites; 173 key informant interviews and de‐identified secondary data on staffing, wages, patient satisfaction, and health outcomes.
Study Design
Researchers used snowball sampling and screening calls to identify 15 organizations using MAs in new roles. Conducted site visits from 2010 to 2012 and updated information in 2014.
Data Collection/Extraction Methods
Thematic analysis explored key topics: factors driving MA role innovation, role description, training required, and wage gains. Categorized outcome data in patient and staff satisfaction, quality of care, and efficiency.
Principal Findings
New MA roles included health coach, medical scribe, dual role translator, health navigator, panel manager, cross‐trained flexible role, and supervisor. Implementation of new roles required extensive training. MA incentives and enhanced compensation varied by role type.
Conclusions
New MA roles are part of a larger attempt to reform workflow and relieve primary care providers. Despite some evidence of success, spread has been limited. Key challenges to adoption included leadership and provider resistance to change, cost of additional MA training, and lack of reimbursement for nonbillable services.
Keywords: Health care workforce, medical assistants, primary care, new models of care
The need to reform primary care delivery models has been extensively discussed in the literature, in clinical forums, and in policy arenas (Bodenheimer 2007; Gawande 2011; Fernandopulle 2013; Porter, Pabo, and Lee 2013; Bodenheimer et al. 2014a). The challenges in primary care delivery have been attributed to workforce shortages of primary care providers, an aging population with an increase in chronic conditions, reimbursement models that do not adequately compensate for primary care services, and the drive to improve patient outcomes (Bodenheimer 2006; Bodenheimer and Pham 2010; Phillips et al. 2011; IHS Inc. 2015). In addition, there is a growing acknowledgement that the current primary care workforce is not always used in a way that maximizes each profession's unique skills and training. Clinicians often spend time on tasks that could be safely and perhaps be better performed by other staff members (Yarnall et al. 2003; Fiscella and Epstein 2008; Bodenheimer and Smith 2013; Bodenheimer, Willard‐Grace, and Ghorob 2014b). Medical assistants (MAs) have been identified as one of the team members who could take on expanded or new roles within teams (Bodenheimer and Laing 2007; Anderson and Halley 2008; Balasa 2008; Nelson et al. 2010; Sinsky et al. 2010; Patel, Nadel, and West 2014; Witgert et al. 2014).
The purpose of this article is to describe new roles for MAs, the preparation needed, evidence of impact, and challenges in implementing those new roles. We also focus on the MA career ladder and potential wage gains for MAs in those new roles. The research is based on a series of case studies conducted between 2012 and 2014 (Healthforce Center at UCSF 2015). This study adds to our knowledge of expanded MA roles as part of overall primary care redesign.
Who Are Medical Assistants?
Medical assistants are one of the fastest growing occupations in the United States. The traditional clinical role of the MA is typically limited to escorting patients to an exam room, taking vital signs, noting the chief complaint in the record, and then leaving the exam room unless assistance is needed with a procedure. Postvisit interactions are limited. That role is now being transformed in many settings.
The MA occupation is defined by the Bureau of Labor Statistics with a Standard Occupational Code and is regulated by each state. By MA role, we mean the duties and responsibilities of the MA in relation to other members of the health care team, including the patient. New roles for MAs include job enlargement (horizontal expansion to include more and more varied tasks), job enrichment (vertical expansion including more autonomy and responsibility for tasks), and/or job rotation (shifting between two or more assignments at regular intervals of time) (Belias and Sklikas 2013; Zareen, Razzaq, and Mujtaba 2013). Job titles for MAs are often organization specific and new roles may include a new job title for the MA.
Some new roles include taking on some functions that overlap with other occupations such as phlebotomist or radiologic technician, while retaining the primary role as an MA.
There are currently more than 591,000 MAs in the United States, with the Bureau of Labor Statistics projecting 138,900 new MA jobs within the next decade (U.S. Bureau of Labor Statistics 2015). MAs are racially and ethnically diverse—57 percent white non‐Hispanic, 23 percent Hispanic, 14 percent African American, 4 percent Asian (U.S. Census Bureau 2010). The majority of training programs are 1 year or less and result in a certificate of completion. Private for‐profit schools are a major source of MA education, producing 82 percent of all MAs in 2013, and may be flexible in ramping up or down enrollment according to market demand (Chapman, Marks, and Dower 2015; National Center for Education Statistics 2015). The median wage for MAs in 2014 was $14.41 per hour (U.S. Bureau of Labor Statistics 2015).
Why Medical Assistants for New Roles on the Primary Care Team?
The upsurge in MA training indicates an increased interest in this workforce (Atkins and Dye 2014; National Center for Education Statistics 2015). MAs may be selected for new roles on the team for several reasons. The short time for pre‐employment or on‐the‐job training makes them relatively easy to hire. The MA is also a relatively low‐cost addition to the team. MAs often come from the community and population they serve. They connect with the patient population in outreach roles that are an important contribution to team care (Blash, Chapman, and Dower 2010b; Chen et al. 2010; Naughton et al. 2013). In addition, the regulations around MA scope of practice often follow the basic model of physician delegation of tasks and supervision (McCarty 2012). Practices innovating the role of the MA generally began with an organizational decision to reform and redesign practice, often including other innovations in addition to changing the MA role (Naughton et al. 2013; Sinsky et al. 2013; Bodenheimer et al. 2014a). In our case studies, this innovation was facilitated by internal funding of training, grant funding, and partnerships with MA training organizations, Area Health Education Centers, and unions (Nelson et al. 2010; Trimble and Wielawski 2013).
Previous Research on New Roles for Medical Assistants
In 2007 Bodenheimer first described the “Teamlet model” (Bodenheimer and Laing 2007) in which a clinician and MA dyad work closely as a team to provide comprehensive care, including previsit planning, a team visit, postvisit health coaching, and follow‐up coaching, to ensure that the patient understands medications and follows the treatment plan. This model was intended to replace the 15‐minute clinician‐only visit in which few of these goals could be accomplished. Since Bodenheimer's paper, there has been increased attention to the MA role on primary care teams and how that role may be enhanced to provider better care with better patient outcomes (Alssid and Goldberg 2013; Ladden et al. 2013; Naughton et al. 2013; Adewale, Anthony, and Borkan 2014; Lichtenstein et al. 2015; Bodenheimer and Willard‐Grace 2016; Freund et al. 2016). In addition to the Teamlet model, other models of care have called for multiple MAs working with a provider to enhance productivity. In these models, MAs serve as a translator, scribe, or health coach (Anderson and Halley 2008; Sinsky et al. 2010; Broughton 2016).
Previous studies have described new MA roles across settings, including academic primary care practices (Chen et al. 2010; Blash, Dower, and Chapman 2011a, b), community health clinics (Baker et al. 2014), rural family care practices (MacKay et al. 2014), large urban health centers (Nelson et al. 2010), and large managed care organizations (Blash, Chapman, and Dower 2010a).
The evidence for practice change innovations that include new roles for MAs on patient, staff, and provider satisfaction and clinical outcomes is building (Baker et al. 2009; Magill et al. 2009; Ruggiero et al. 2010, 2014; Day et al. 2013; Ladden et al. 2013; Sinsky et al. 2013; Thom et al. 2014, 2015; Dubé et al. 2015; Lichtenstein et al. 2015; Reedy et al. 2016). There are few rigorous studies of cost effectiveness or evidence of return on investment of implementing new models (Anderson and Halley 2008; Reid et al. 2010; Sinsky et al. 2010; Day et al. 2013). Even fewer studies have focused on the impact of these new roles on MA retention, satisfaction, or career advancement and wage gains (Nelson et al. 2010; Willard‐Grace et al. 2013; Gerstein et al. 2015).
Methods
Potential case study sites were selected via an environmental scan and snowball sampling. To be eligible for the case study, health care organizations had to meet several criteria, including employing MAs in an innovative model of care with new roles; documented improvements in organizational efficiency, patient outcomes, and/or staff members and patient satisfaction; and a focus on career advancement, training, and enhanced compensation for the new MA roles. This study was approved by the Committee on Human Research at the University of California at San Francisco.
Over 95 screening interviews and/or email exchanges were conducted to locate the 15 sites chosen for in‐depth study. Many sites were dropped for consideration because they had not yet implemented any career or wage gains for MAs in their practice model change. At each of the 15 selected sites, two researchers spent 1–2 days on site conducting individual or small group interviews with MAs, CEOs, medical directors, human resources representatives, clinical providers, supervisors, nurses, union representatives, and training directors about their care models and workforce initiatives. The interviews lasted approximately an hour with each researcher taking detailed interview notes. From six to twenty‐four individuals were interviewed at each site for a total of 173 interviewees. After completion of the site visits, interview notes, outcomes data summaries, and other site background documents were input into Atlas.ti software and analyzed first within sites by predetermined categories based on interview questions and then across sites for broader themes. Three study researchers independently reviewed the data and shared key themes for the case studies. MA roles were identified, coded, and reviewed to identify basic models of MA tasks, duties, and assignments. Three roles, including relational, cross‐trained, and leadership, clearly emerged from the analysis as distinct; the health information technology (HIT) role required further discussion and analysis about the functions related to this role. The case study outline is included in Appendix SA2.
Results
Study Sites
Case study sites ranged from small, rural, federally qualified health centers (FQHCs) to an urban medical center that was a part of a large national HMO. Table 1 describes the 15 case study sites, including name, practice location, organization type, reported number of MAs and providers, and approximate ratio of MAs to providers in practice teams. Ratios are approximate but describe a key characteristic of the staffing model—the number of providers and MAs per practice team. Many study sites achieved efficiencies by assigning more than one MA to each provider. The number of support staff per provider has emerged as an important factor in practice efficiency (Anderson and Halley 2008; Sinsky et al. 2010). Ratios listed in Table 1 include MAs serving as health coaches, dual role interpreters, health navigators, and sometimes supervisors.
Table 1.
Description of Case Study Sites
| Name | State | Organization Type | No. of MAs | No. of Providers | MA‐to‐Provider Ratio |
|---|---|---|---|---|---|
| Asian Health Services | CA | FQHC | 55a | 33 | 1.5:1a |
| Cabin Creek Health Systems | WV | FQHC | 33a | 18 | 2:1a |
| Family Health Center of Worcester, Inc. | MA | FQHC | 25 | 26 | 1:1 |
| DFD Russell Medical Centers | ME | FQHC | 22 | 11 | 1.5:1 |
| Franklin Square Medical Center, Family Health Center | MD | Not‐for‐profit regional health care system (residency site) | 15 | 18 providers/28 residents | 3:3 |
| High Plains Community Health Center | CO | FQHC | 29a | 10 | 4:1a |
| Kaiser Permanente Baldwin Park Medical Center | CA | Nationwide staff model HMO | 115b | 94 | 1:1b |
| Northwestern Medical Group | IL | Academic medical center | 84 | 120 | 1:1 |
| PeaceHealth; Team Fillingame | OR | Not‐for‐profit regional health care system | 3a | 2 | 1.5:1a |
| Southcentral Foundation | AK | Indian Health/Alaska Native corporation | 132 | 240 | 2:1 |
| Special Care Center/AtlantiCare | NJ | Not‐for‐profit regional health care system | 9a | 2 | 4.5:1a |
| UC Davis Family Practice Center | CA | Academic medical center | 14 | 17 faculty/54 residents | 1:1 |
| Union Health Center | NY | Comprehensive multispecialty care clinic | 38a | 12 | 1.5:1a |
| University of Utah Health Care | UT | Academic medical center | 195 | 111 | 2.5:1 |
| WellMed Medical Group/Medical Preparatory School of Allied Health | TX | Private, physician‐ owned practice management company | 200+ | ~90 | 3:1b |
Includes health coaches who can rotate to MA role.
Includes LPNs in same role.
New Roles and Models
After reviewing the data, the research team developed the following categories to describe those new roles, MA activities in those roles, and additional training, beyond basic MA preparation, needed to prepare MAs for those roles. Flexibility is a key factor in expanded MA roles and MAs often rotate between traditional MA tasks and new roles (see Table 2). Nearly all sites reported that the basic education that MAs received was insufficient for new roles, necessitating additional training. Most of the sites paid for this training out of their own resources. Only a few sites were able to raise grant funding to support curriculum development for new roles or training.
Table 2.
New Roles for MAs, Skills, and Training Requirements
| Roles | Skills Emphasized | Additional Training | |
|---|---|---|---|
| Relational |
|
Use interpersonal skills and personal cultural/linguistic skills to communicate health education, medical system, and community resources information to patients. May use motivational interviewing to assist patients in setting health goals |
|
| HIT/Documentation |
|
Use computer skills to document and analyze patient data, review care gaps, report on trends, or teach others to utilize EHR and other HIT systems |
|
| Cross‐Trained Rotation |
|
Use multiple clinical and clerical skills to rotate through front and back office tasks based on practice workflow needs. Requires flexibility and willing to learn and maintain multiple skills. May require additional clinical skills and training as well as good customer service skills |
|
| Leadership/Managerial |
|
Use leadership skills to assist in supervising, training, and assessing other MAs and/or in coordinating practice workflow and supplies distribution |
|
EHR, electronic health record; MA, medical assistant; OJT, on‐the‐job training.
Relational roles included health coach, patient navigator, community health worker, care coordinator, and dual role interpreter. In health coaching models in particular, MAs were selected because of their ability to communicate with and gain the trust of a particular patient population, and they were often required to be bilingual. Health coaches worked with patients with chronic diseases, helping them to set and keep self‐management goals. Patient navigators and care coordinators helped patients navigate the health care system across the continuum of care and access resources. Dual role interpreters used their first language, enhanced by professional training in interpretation and medical terminology, to interpret throughout the visit, rotating back to basic MA roles when their translation skills were not needed. Relational roles required extensive and ongoing training often involving motivational interviewing, various types of screening procedures, and information on chronic disease management. One site required MAs to complete nine monthly in‐house health coaching modules as well as additional shadowing, observation, and assessment prior to promotion to health coach. The site employing MAs as community health workers received grant funding to send employees offsite for specialized training. MAs serving as dual role interpreters at one site were required to take a 60‐hour accredited course and pass a language aptitude screening exam.
Other new roles focused on health information technology and increased skills in documentation. Those roles included medical scribe, panel manager, quality improvement assistant, and electronic health record (EHR) super‐user. Medical scribes stayed in the room during a patient visit and entered information into the EHR. MA panel managers scanned the medical records for a provider's “panel” of patients, looking for care gaps, and contacted patients in need of follow‐up. MA quality improvement assistants produced reports on quality measures that clinical teams could use for planning and patient care. Super‐users became highly proficient with the EHR. One organization that relied on computer‐based protocols for MA/patient encounters and panel management conducted a 1‐month training in computer skills in a skills lab followed by intensive observation and tailored one‐on‐one training to help staff members integrate the new system into their workflow.
The third category of new roles involved cross‐training MAs to rotate through multiple roles in addition to add‐on skills, including phlebotomist, limited license radiologic technician, pharmacy technician, receptionist, greeter, referral coordinator, and medical records clerk. In these models, the MA often served as a patient ambassador, escorting the patient through the visit and providing as many services as possible in the exam room. In these models, there was often a higher ratio of MAs per provider. Administrators observed that it was more efficient to use MAs as flexible, redeployable employees who could cover multiple roles rather than hire specialized staff members that were more expensive and could not cross‐cover. MAs generally received on‐the‐job (OJT) training for these roles, although, at one site, staff members were sponsored to take courses to become pharmacy technicians and limited license radiology technicians.
The final category of new MA roles included leadership and supervisory positions. Examples of those new roles included lead MA, supervisor, mentor, preceptor, floor coordinator, and trainer. In those roles, MAs often still served as MAs, but also took on more responsibility coordinating the work of other MAs, organizing daily patient workflow, and training and assessing other MAs. Those roles could lead to higher administrative and management positions such as clinic supervisor. MAs were often selected for promotion into these new roles based on aptitude and identified leadership skills. They also required additional training. At one site, lead MAs received training in management and conflict resolution; at another, MAs were sponsored to take part in an extensive leadership training course followed by a 6‐month mentorship.
MA Career Ladders and Incentives
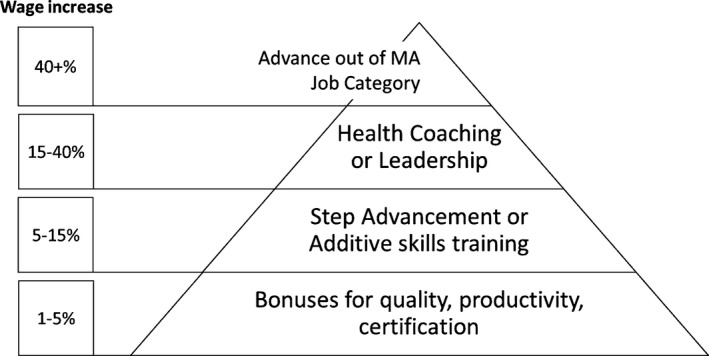
To retain their investment in MAs, many sites developed career ladders, financial incentives, and wage gains. Figure 1 shows compensation gains that were available to MAs in one or more of the case study sites in the new roles developed. The pyramid displays smaller wage gains available to larger numbers of MAs within an organization at the base of the pyramid, with correspondingly smaller segments representing advancements available to fewer MAs but yielding higher pay differentials. The base represents quality and productivity bonuses that MAs might receive either as individuals or part of high‐performing teams. For example, one clinic set up a system whereby MAs could access a dashboard to check their progress in achieving various quality goals related to clinical care. Achieving a certain level on a number of predetermined measures resulted in a $500 annual bonus.
Figure 1.
Wage Changes for MAs in New Roles
In the next row up are step advancements and wage increases related to additional training. Step advancements include formal career ladders with different step levels within the MA job category (MA I, MA II, etc.). Additive skills pay included “pay bumps” MAs might achieve for additional training in areas like phlebotomy or radiation technology.
The second‐to‐the‐top row represents advanced positions like health coaching and leadership, which required extended training and commitment and often yielded substantially greater wage gains.
At the top of the pyramid are greater wage gains related to movement out of the MA job category. A few of the sites offered educational stipend support for MAs to grow into nursing or other health careers with the agreement that they would return to work for the organization in an advanced role upon program completion.
The one organization that offered the overall highest wages for the greatest number of MAs did so via its union contract.
Evidence of Impact
All 15 sites provided some evidence of the positive impacts of practice change. However, it was seldom possible to distinguish the unique impact of new MA roles from the overall impacts of care model redesign. Our ability to compare outcomes across sites was limited. A few sites provided pre‐ and post‐implementation data; others simply compared a single data point to regional, statewide, or national averages or benchmarks. Organizations with research infrastructure generally had more formal evaluation data and published results on their care change models (Magill et al. 2009; Kanter et al. 2010; Egger et al. 2012; Day et al. 2013; Driscoll et al. 2013). Table 3 displays sample outcomes measures reported by the case study sites.
Table 3.
Sample Outcomes Measured by Case Study Sites
| Measure | How Collected | Outcomes of Practice Change Including New MA Roles | |
|---|---|---|---|
| Patient Satisfaction Survey | |||
| Example 1 | Doctor seems to know the important information about your medical history? | CAHPS Survey | 93% of patients report that this is true of intervention site; 53% report this is true of prior PCP comparison |
| Example 2 | Patient confidence in provider (previsit planning is conducted by MAs) | Press‐Ganey Patient Satisfaction Survey | 87% for comparison and 99% for intervention group after implementing pre‐visit planning |
| Example 3 | Overall positive customer satisfaction scores | CAHPS Survey | 88.5–91% post‐implementation |
| Example 4 | Doctor spending time with patient and not seeming rushed | PRC Patient Experience Survey | 48% pre‐implementation to 65% post‐implementation |
| Staff/Provider Satisfaction Survey | |||
| Example 1 | Aggregate score of provider satisfaction with practice | AMGA provider satisfaction | 69% pre‐implementation to 81% post‐implementation |
| Example 2 | Provider satisfaction with self‐management supports (MA health coaching) | Evaluation survey for pilot project | 7.8 pre‐implementation to 8.7 post‐implementation (1–10 scale) |
| Example 3 | Aggregate score of employees agreeing “I am a satisfied employee” | Morehead Employee Opinion Survey | 3.7 pre‐implementation to 4.2 post‐implementation (1–5 scale) |
| Example 4 | Aggregate score of employees agreeing “I would recommend this organization as a good place to work” | Morehead Employee Opinion Survey | 3.82–4.16 over 3 years of implementation period (1–5 scale) |
| Quality of care | |||
| Example 1 | Asthma screening: ≥1 office visit over past 12 months) | HEDIS | 40% pre‐implementation to 70% post‐implementation |
| Example 2 | Childhood immunization status for children from birth to 2 years of age | HEDIS | 57% pre‐implementation to 100% post‐implementation |
| Example 3 | Proportion of hypertensive patients with controlled blood pressure | HEDIS | 56% pre‐implementation to 76% post‐implementation |
| Example 4 | Percentage of diabetic patients with at least one HbA1c test over 12 months | HEDIS | 83% in 2003; 92% in 2010 (improvement over time) |
| Efficiency/operations | |||
| Example 1 | Dropped calls (MA phone bank) | Organization records | 3.1% reduction 1 year post‐implementation |
| Example 2 | Employee retention rate | Organization records | ~60% pre‐implementation to 83% post‐ implementation |
| Example 3 | Patient visit time | Organization records | 2.62 hours preimplementation to 57 minutes post‐implementation |
| Example 4 | Patient visit time | Organization records | 90 minutes pre‐implementation to 45 minutes post‐implementation |
| Costs/productivity/utilization | |||
| Example 1 | The number of patients per provider hour | Organization records | 1.82 patients pre‐implementation to 2.8 post‐implementation; Increased revenue of over $400,000 per year |
| Example 2 | PMPM cost | Payer records | Intervention site patients cost 17% less PMPM than comparable patients |
| Example 3 | (i) Emergency department and urgent care visits; (ii) hospital admissions and days | Records from partner hospital | (i) 50% reduction, (ii) 53% reduction post‐implementation |
| Example 4 | Emergency department and hospital visits | Payer records | Both decreased by 40% resulting in 10–25% reduction in costs post‐implementation |
CAHPS, Consumer Assessment of Healthcare Providers and Systems; HEDIS, Healthcare Effectiveness Data and Information Set; MA, medical assistants; PCP, primary care provider; PMPM, per member per month; PRC, Professional Research Consultants, Inc.
Six sites provided patient satisfaction measures that indicated either improved satisfaction or continued high satisfaction, after implementing practice change with new MA roles. One site documented higher patient confidence in providers at sites with MA‐conducted previsit planning than at comparable sites without (99 percent vs 87 percent).
Three organizations reported staff engagement survey data indicating multiple findings of greater staff satisfaction and engagement after implementing the new MA roles. For example, one site improved on the overall average score of employees agreeing “I am a satisfied employee” from 3.7 on a five point scale prior to implementation to 4.2 post‐implementation. One site documented overall improvement in physician satisfaction with their medical practice from about 69 percent overall prior to practice change to 81 percent post‐implementation.
Quality outcomes most commonly tracked were standard quality measures such as in the Healthcare Effectiveness Data and Information Set (HEDIS) dataset. All case study sites had evidence of at least some improvement in clinical screening and/or outcomes measures. However, most sites did not formally tie these data to points before and after innovations in the care model. At least two sites were able to track outcomes back to team or individual MA performance. For example, one site recorded an increase in childhood immunizations—from 57 percent to 100 percent—as a result of implementing a new protocol for MAs.
At least four of the sites tracked organizational efficiency or human resources outcomes related to practice change. For example, one site reduced patient visit cycle times from 90 minutes to 45 minutes as a result of improvements in workflow, adoption of open‐access scheduling, and implementation of self‐check‐in kiosks. Surprisingly few sites tracked changes in staff retention related to practice change.
Measures of cost and utilization differed by reimbursement model. One site using a fee‐for‐service model improved volume and productivity through increasing the MA to provider ratio and consequently almost doubled the number of patients seen per provider hour, resulting in increased revenue of over $400,000 a year. Two sites using MA health coaches under a capitated model reported reduced costs in the form of lower ER use and hospitalization rates, and reduced length of hospitalizations among patients with multiple chronic diseases (Nelson et al. 2010; Gawande 2011; Trimble and Wielawski 2013).
Challenges in Adoption of New Roles
Lack of clarity of MA scope of practice regulations was a challenge in developing new MA roles in several sites. Many site leaders were unsure of the MA scope of practice in their state. A few of the sites imposed more stringent restrictions on MA practice than did state regulations. Injections and protocol‐based triage were often areas of doubt. Site leaders interviewed reported that scope of practice concerns were sometimes raised by nurses who feared displacement if MAs were allowed to take on expanded roles.
Both providers and staff reported that they found practice change challenging. MAs reported lacking confidence to take on new roles and some resented taking on more challenging work. Providers and nurses were reluctant to delegate tasks, concerned about relinquishing patient contact, and distrusting of the skills and reliability of the MAs. A few sites addressed this by engaging providers and nurses in training and assessing MA skills, allowing them to decide if “their” MA met the required competencies for the new roles.
Sustaining practice change required the buy‐in of top leadership. All of the case study sites had a practice change champion who also championed the development of new MA roles. At two sites, visionary champions initiated a small‐scale practice change in MA roles that was discontinued when that champion left the organization.
The significant costs in time and money for additional MA training were reported to be a challenge across sites. Most sites focused training first on supplementing basic MA skills which newly hired MAs reportedly lacked. Costs included hiring extra staff to cover if a training was conducted during the workday or paying MAs overtime if they were required to attend during nonwork hours. Retention of MAs trained in new roles was a challenge in some of the smaller sites as larger competitors sometimes lured away the newly trained by providing higher wages.
Administrators often had to make the business case to leadership that increasing the number of MAs, providing advanced training, increasing salaries, and changing job descriptions were worth the investment. Reimbursement for unbillable services provided by MAs in new roles presented a significant challenge to sites with a fee‐for‐service reimbursement model.
About one‐third of sites had direct fee‐for‐service arrangements. Two of the fee‐for‐service sites were able to charge facility fees. Two additional sites tracked increased productivity and revenue as a return on the investment of MA development. Four of the remaining sites had some form of per member per month capitation, and five were FQHCs under the prospective payment system —of which two were fee‐for‐service and three were special capitation arrangements. Sites with capitation models or global payments reported that they had an easier time covering the costs of increased MA staffing and incentives.
Discussion
Implementation of the ACA, shortages of primary care providers, and growing recognition that different team members may be better at meeting different patient needs will likely continue to lead to evolution of the MA role. The adoption of new roles for MAs is flourishing in some areas, particularly in large group practices and FQHCs. Some would argue that in small solo or small group practice the MA role has always been expanded and flexible. Providers in small practices expect MAs to multitask. Our methodology did not include case studies in small practices. The new roles that are the focus of this article were usually included as part of a larger organizational innovation encompassing overall practice change.
As noted by most of the case study sites, retraining MAs was costly to employers. Some of the sites formed partnerships with training providers, including community colleges, to better prepare MAs in the skills needed for expanded roles. However, most sites tended to have very individualized needs that necessitated additional training even if basic MA skills were adequate. There is a need for training programs and certification organizations to revise the basic MA training curriculum. One of the certifying organizations, the American Association of MAs has reviewed its recommended curriculum and exam and referenced how these tools address new roles for Certified MAs (Balasa 2016).
The primary care practices selected for these case studies were pioneers in primary care redesign via staffing models that included new roles for MAs. The common thread among these sites was innovation in the extended and flexible use of workers who traditionally functioned largely in supportive roles, with little significant involvement in care or in ongoing relationships with patients. The drivers of practice innovation are well documented and include primary care provider shortages, an aging population, increases in chronic illness, cost pressures to provide more efficient care, and the push to provide better quality care and improved patient outcomes. Primary care redesign necessitates a close look at the workforce to see how care can be better delivered by teams, using the skills and knowledge of members of the health care team most effectively.
Innovation in the use of MAs makes sense from a business and clinical perspective. As noted in the outcomes section, study sites applied differing metrics to make the business case, depending on the organization type and reimbursement model. Sites using fee‐for‐service models often focused on improving productivity and cycle time utilizing multiple MAs while sites serving self‐insured populations under a capitation model were able to track patient utilization rates, sometimes against a comparison group, and demonstrate cost savings to insurers related to MAs' health coaching and other relational roles.
MAs have a relatively short educational preparation time, and their basic education includes clinical as well as practice support skills. MAs are among the lowest wage workers in clinical practice settings and are not in short supply in most parts of the country. The regulatory structure of physician delegation means that MAs can have a fairly wide scope of duties, although the differences in MA scope of practice across states sometimes presents a confusing picture.
Finally, MAs' linguistic and cultural concordance with many of their patients make them well suited for ongoing outreach and follow‐up for patients who may be noncompliant with providers or require close ongoing monitoring.
The flexibility in MA roles has enabled significant experimentation in practice change over the past decade. Role innovations continue as MA roles are combined with other roles. In one setting, MAs have been trained as CHWs for a program in diabetes self‐management (Rice, Kocurek, and Snead 2010; Walton et al. 2012). In dual roles, numerous new job titles are emerging.
There are significant challenges in the replication of new models of care using MAs in new roles. The same high‐performing practices profiled here have also been widely recognized (Kenen 2010; Gawande 2011; Ladden et al. 2013; Bodenheimer, Willard‐Grace, and Ghorob 2014b).
However, there are probably many failed efforts at practice transformation that have not received as much attention. Small pilots may be implemented in one part of a delivery system but fail to be spread across the organization.
It is important for practices transforming MAs roles to consider some of the success factors we identified. Those include having a local champion, preferably a provider, who can guide and promote the process. Leadership buy‐in across the organization is critical to adopt and sustain these efforts. The loss of leadership support or champion can lead to ultimate failure of these models. We found that three of the sites had discontinued their MA innovations between the time of our first site visit and follow‐up interviews. Lack of sustained support from leadership was the reported reason.
The costs to sustain these innovations are substantial and should be considered in overall planning. Training for the MA and the whole team is ongoing. Supporting the incentive structure for the MA and the whole team with bonuses and other productivity and quality incentives were reported to be essential for staff retention and sustainability of the models.
This study has several limitations. The sites selected were those that were already high‐performing and had successfully implemented new roles for MAs. We did not select practices with failed efforts, which might have offered more insights into challenges and pitfalls in implementation. Our site selection process did not include solo and small group practices; thus, we do not have information on MA innovations occurring in those types of practices. We were only able to collect limited data on clinical and administrative outcomes of practice innovation. Case studies sites agreed to give us readily available measures, which meant that data were often short term, limited to outcomes collected for other purposes, and were not uniform across sites. Few of the sites conducted rigorous pre‐ and postevaluation as they implemented new uses for MAs and overall practice redesign. Other than MA retention and satisfaction, few of the measures that were collected could be linked specifically to the MA component of the innovation.
Future research should include rigorous evaluation of these models. A recent initiative funded by the Hitachi Foundation, the Care Team Redesign Initiative, aims to demonstrate the business case for training and empowering frontline health care workers within primary care teams with technical assistance, and a rigorous evaluation (Strong 2015).
Further workforce research should focus on the long‐term career trajectory of MAs who have participated in these new models of care and incentive systems. Do new roles for MAs offer career pathways and growth out of low‐wage occupations? Are there workforce benefits and cost savings from reduced turnover? What future enhanced and combined roles, such as MA/CHW or MA/behavioral health specialist, are needed to further support developing care models?
Conclusion
Driven by demographic factors and changing health care policy emphasizing primary care, many primary care practices are revising their workflow to enhance efficiency and quality. Influxes of new patients, and increasingly complex patients, require new models of care utilizing nonprovider staff to take on some of the task burden. Innovative models employing MAs in new roles have gained considerable attention, but challenges to spreading these models remain.
Payment model reform may help to address some of those challenges. Further rigorous research on the impact of these new roles is needed.
Supporting information
Appendix SA1: Author Matrix.
Appendix SA2: Case Study Outline.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This research was supported with grant funding from the Hitachi Foundation's Pioneer Employer's Initiative. The purpose of the study was to examine organizations that were expanding the role of MAs in innovative models of care that not only improve quality of care and organizational viability but provide career enhancement for the MAs themselves. The mission of the Hitachi Foundation is to discover, demonstrate, and expand business practices that both measurably improve economic opportunities for low‐wealth individuals in the United States and enhance long‐term business value. An independent Board of Directors composed of distinguished Americans governs the Foundation.
Disclosures: None.
Disclaimers: None.
References
- Adewale, V. , Anthony D., and Borkan J.. 2014. “Medical Assistants' Roles in Electronic Health Record Processes in Primary Care Practices: The Untold Story.” The Journal of Medical Practice Management 30 (3): 190–6. [PubMed] [Google Scholar]
- Alssid, J. L. , and Goldberg M.. 2013. “The Rise of the Medical Assistant: and Five Other Frontline and NonClinical Healthcare Jobs That Are Growing in Number, Complexity, and Importance.” Workforce Strategy Report. Hooksett, NH: College for America. [Google Scholar]
- Anderson, P. , and Halley M. D.. 2008. “A New Approach to Making Your Doctor‐Nurse Team More Productive.” Family Practice Management 15 (7): 35–40. [PubMed] [Google Scholar]
- Atkins, B. and Dye L.. 2014. “Medical Assisting: An Emerging Opportunity for Growth ‐ On‐Demand”. Sparkroom.com [accessed March 8, 2016]. Available at http://sparkroom.com/ondemand/medical-assisting-emergingopportunity-growth/. [Google Scholar]
- Baker, A. N. , Parsons M., Donnelly S. M., Johnson L., Day J., Mervis A., James B., Burt R., and Magill M. K.. 2009. “Improving Colon Cancer Screening Rates in Primary Care: A Pilot Study Emphasing the Role of the Medical Assistant.” Quality and Safety in Health Care 18 (5): 355–9. [DOI] [PubMed] [Google Scholar]
- Baker, D. W. , Brown T., Buchanan D. R., Weil J., Balsley K., Ranalli L., Lee J. Y., Cameron K. A., Ferreira M. R., Stephens Q., Goldman S. N., Rademaker A., and Wolf M. S.. 2014. “Comparative Effectiveness of a Multifaceted Intervention to Improve Adherence to Annual Colorectal Cancer Screening in Community Health Centers: A Randomized Clinical Trial.” Journal of the American Medical Association Internal Medicine 174 (8): 1235–41. [DOI] [PubMed] [Google Scholar]
- Balasa, D. A. 2008. “New Roles for the Certified Medical Assistant to Enhance Quality and Effectiveness of Care.” Medical Practice Management 23 (5): 276–8. [PubMed] [Google Scholar]
- Balasa, D. 2016. “One Credential, Many Roles: Why CMAs (AAMA) Are Uniquely Qualified for Advanced Positions.” CMA Today 49 (3): 1–9. [Google Scholar]
- Belias, D. , and Sklikas D.. 2013. “Aspects of Job Design.” International Journal of Human Resource Management and Research (IJHRMR) 3 (4): 85–94. [Google Scholar]
- Blash, L. , Chapman S., and Dower C.. 2010a. Kaiser Permanente Baldwin Park Medical Center Information Technology Propels Expansion of Medical Assistant Role. San Francisco, CA: Center for the Health Professions, University of California, San Francisco. [Google Scholar]
- Blash, L. , Chapman S., and Dower C.. 2010b. UNITE HERE Health Center—Pioneering the Ambulatory Intensive Caring Unit. San Francisco, CA: Center for the Health Professions, University of California, San Francisco. [Google Scholar]
- Blash, L. , Dower C., and Chapman S.. 2011a. UC Davis Family Practice Center—Medical Assistants Anchor Residency‐based Medical Home. San Francisco, CA: Center for the Health Professions, University of California, San Francisco. [Google Scholar]
- Blash, L. , Dower C., and Chapman S.. 2011b. University of Utah Community Clinics—Medical Assistant Teams Enhance Patient‐Centered, Physician‐Efficient Care. San Francisco, CA: Center for the Health Professions, University of California, San Francisco. [Google Scholar]
- Bodenheimer, T. 2006. “Primary Care—Will It Survive?” The New England Journal of Medicine 355 (9): 861–4. [DOI] [PubMed] [Google Scholar]
- Bodenheimer, T. 2007. Building Teams in Primary Care: Lessons Learned. Oakland, CA: California Health Care Foundation. [Google Scholar]
- Bodenheimer, T. , and Laing B.. 2007. “The Teamlet Model of Primary Care.” The Annals of Family Medicine 5 (5): 457–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodenheimer, T. , and Pham H. H.. 2010. “Primary Care: Current Problems and Proposed Solutions.” Health Affairs 29 (5): 799–805. [DOI] [PubMed] [Google Scholar]
- Bodenheimer, T. S. , and Smith M. D.. 2013. “Primary Care: Proposed Solutions to the Physician Shortage without Training More Physicians.” Health Affairs 32 (11): 1881–6. [DOI] [PubMed] [Google Scholar]
- Bodenheimer, T. , and Willard‐Grace R.. 2016. “Teamlets in Primary Care: Enhancing the Patient and Clinician Experience.” The Journal of the American Board of Family Medicine 29 (1): 135–8. [DOI] [PubMed] [Google Scholar]
- Bodenheimer, T. , Ghorob A., Willard‐Grace R., and Grumbach K.. 2014a. “The 10 Building Blocks of High‐Performing Primary Care.” The Annals of Family Medicine 12 (2): 166–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodenheimer, T. , Willard‐Grace R., and Ghorob A.. 2014b. “Expanding the Roles of Medical Assistants: Who Does What in Primary Care?” Journal of the American Medical Association Internal Medicine 174 (7): 1025–6. [DOI] [PubMed] [Google Scholar]
- Broughton, A. C. 2016. “How Innovative Teamwork Saved This Rural Health Center.” Forbes.com [accessed on May 16, 2016]. Available at http://www.forbes.com/sites/thehitachifoundation/2016/03/28/how-innovative-teamwork-saved-this-rural-health-center/#466068a86af6
- Chapman, S. A. , Marks A., and Dower C.. 2015. “Positioning Medical Assistants for a Greater Role in the Era of Health Reform.” Academic Medicine: Journal of the Association of American Medical Colleges 90 (10): 1347–52. [DOI] [PubMed] [Google Scholar]
- Chen, E. H. , Thom D. H., Hessler D. M., Phengrasamy L., Hammer H., Saba G., and Bodenheimer T.. 2010. “Using the Teamlet Model to Improve Chronic Care in an Academic Primary Care Practice.” Journal of General Internal Medicine 25 (Suppl 4): S610–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Day, J. , Scammon D. L., Kim J., Sheets‐Mervis A., Day R., Tomoaia‐Cotisel A., Waitzman N. J., and Magill M. K.. 2013. “Quality, Satisfaction, and Financial Efficiency Associated with Elements of Primary Care Practice Transformation: Preliminary Findings.” The Annals of Family Medicine 11 (Suppl 1): S50–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Driscoll, D. L. , Hiratsuka V., Johnston J. M., Norman S., Reilly K. M., Shaw J., Smith J., Szafran Q. N., and Dillard D.. 2013. “Process and Outcomes of Patient‐Centered Medical Care with Alaska Native People at Southcentral Foundation.” The Annals of Family Medicine 11 (Suppl 1): S41–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubé, K. , Willard‐Grace R., O'Connell B., DeVore D., Prado C., Bodenheimer T., Hessler D., and Thom D. H.. 2015. “Clinician Perspectives on Working with Health Coaches: A Mixed Methods Approach.” Families, Systems & Health: The Journal of Collaborative Family HealthCare 33 (3): 213–21. [DOI] [PubMed] [Google Scholar]
- Egger, M. J. , Day J., Scammon D. L., Li Y., Wilson A., and Magill M. K.. 2012. “Correlation of the Care by Design Primary Care Practice Redesign Model and the Principles of the Patient‐ Centered Medical Home.” The Journal of the American Board of Family Medicine 25 (2): 216–23. [DOI] [PubMed] [Google Scholar]
- Fernandopulle, R. 2013. More or Different? Rethinking the Need for Increasing the Supply of Primary Care Physicians in the Light of Health Reform. San Francisco, CA: Blue Shield of California Foundation. [Google Scholar]
- Fiscella, K. , and Epstein R. M.. 2008. “So Much to Do, So Little Time: Care for the Socially Disadvantaged and the 15‐Minute Visit.” Archives of Internal Medicine 168 (17): 1843–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freund, T. , Peters‐Klimm F., Boyd C. M., Mahler C., Gensichen J., Erler A., Beyer M., Gondan M., Rochon J., Gerlach F. M., and Szecsenyi J.. 2016. “Medical Assistant‐Based Care Management for High‐Risk Patients in Small Primary Care Practices: A Cluster Randomized Clinical Trial.” Annals of Internal Medicine 164 (5): 323–30. [DOI] [PubMed] [Google Scholar]
- Gawande, A. 2011. “The Hot Spotters: Can We Lower Medical Costs by Giving the Neediest Patients Better Care?” The New Yorker Jan: 40–51. [PubMed] [Google Scholar]
- Gerstein, B. S. , Chien A. T., Peters A. S., Rosenthal M., and Singer S.. 2015. “The Medical Assistant Experience in Team‐Based Primary Care: A Qualitative Study.” Journal of General Internal Medicine 30: S278–9. [Google Scholar]
- Healthforce Center at UCSF . 2015. The Care Team Redesign Initiative [accessed on March 9, 2016]. Available at https://healthforce.ucsf.edu/research/projects/care-team-redesign-initiative
- IHS Inc. 2015. The Complexities of Physician Supply and Demand: Projections from 2013 to 2025. Washington, DC: Association of American Medical Colleges. [Google Scholar]
- Kanter, M. , Martinez O., Lindsay G., Andrews K., and Denver C.. 2010. “Proactive Office Encounter: A Systematic Approach to Preventive and Chronic Care at Every Patient Encounter.” The Permanente Journal 14 (3): 38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenen, J. 2010. “Innovative Alaska Health Plan Outperforms Many Others in Lower 48” [accessed on April 12, 2010]. Available at http://health.newamerica.net/publications/articles/2010/innovative_alaska_health_plan_outperforms_many_others_in_lower_48_26996
- Ladden, M. D. , Bodenheimer T., Fishman N. W., Flinter M., Hsu C., Parchman M., and Wagner E. H.. 2013. “The Emerging Primary Care Workforce: Preliminary Observations from the Primary Care Team: Learning from Effective Ambulatory Practices Project.” Academic Medicine: Journal of the Association of American Medical Colleges 88 (12): 1830–4. [DOI] [PubMed] [Google Scholar]
- Lichtenstein, B. J. , Reuben D. B., Karlamangla A. S., Han W., Roth C. P., and Wenger N. S.. 2015. “Effect of Physician Delegation to Other Healthcare Providers on the Quality of Care for Geriatric Conditions.” Journal of the American Geriatrics Society 63 (10): 2164–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKay, F. D. , Anderson J. E., Klein M. C., Berkowitz J., MacKay J. T., and Gailius J.. 2014. “The Modified Medical Office Assistant Role in Rural Diabetes Care.” Canadian Journal of Rural Medicine 19 (2): 49–56. [PubMed] [Google Scholar]
- Magill, M. K. , Day J., Mervis A., Donnelly S. M., Parsons M., Baker A. N., Johnson L., Egger M. J., Nunu J., Prunuske J., James B. C., and Burt R.. 2009. “Improving Colonoscopy Referral Rates through Computer‐Supported, Primary Care Practice Redesign.” Journal for Healthcare Quality 31 (4): 43–53. [DOI] [PubMed] [Google Scholar]
- McCarty, M. 2012. “The Lawful Scope of Practice of Medical Assistants—2012 Update.” AMT Events June: 110–19. [Google Scholar]
- National Center for Education Statistics . 2015. “Integrated Postsecondary Education Data System (IPEDS)” [accessed on April 10, 2015]. Available at http://nces.ed.gov/ipeds/
- Naughton, D. , Adelman A. M., Bricker P., Miller‐Day M., and Gabbay R.. 2013. “Envisioning New Roles for Medical Assistants: Strategies from Patient‐Centered Medical Homes.” Family Practice Management 20 (2): 7–12. [PubMed] [Google Scholar]
- Nelson, K. , Pitaro M., Tzellas A., and Lum A.. 2010. “Transforming the Role of Medical Assistants in Chronic Disease Management.” Health Affairs 29 (5): 1–3. [DOI] [PubMed] [Google Scholar]
- Patel, K. , Nadel J., and West M.. 2014. Redesigning the Care Team: The Critical Role of Frontline Workers and Models for Success. Washington, DC: Engelberg Center for Health Care Reform at Brookings. [Google Scholar]
- Phillips, R. L. , Bronnikov S., Petterson S., Cifuentes M., Teevan B., Dodoo M., Pace W. D., and West D. R.. 2011. “Case Study of a Primary Care‐Based Accountable Care Systems Approach to Medical Home Transformation.” Journal of Ambulatory Care Management 34 (1): 67–77. [DOI] [PubMed] [Google Scholar]
- Porter, M. E. , Pabo E. A., and Lee T. H.. 2013. “Redesigning Primary Care: A Strategic Vision to Improve Value by Organizing Around Patients' Needs.” Health Affairs 32 (3): 516–25. [DOI] [PubMed] [Google Scholar]
- Reedy, A. B. , Yeh J. Y., Nowacki A. S., and Hickner J.. 2016. “Patient, Physician, Medical Assistant, and Office Visit Factors Associated with Medication List Agreement.” Journal of Patient Safety 12 (1): 18–24. [DOI] [PubMed] [Google Scholar]
- Reid, R. J. , Coleman K., Johnson E. A., Fishman P. A., Hsu C., Soman M. P., Trescott C. E., Erikson M., and Larson E. B.. 2010. “The Group Health Medical Home at Year Two: Cost Savings, Higher Patient Satisfaction, and Less Burnout for Providers.” Health Affairs 29 (5): 835–43. [DOI] [PubMed] [Google Scholar]
- Rice, D. , Kocurek B., and Snead C. A.. 2010. “Chronic Disease Management for Diabetes: Baylor Health Care System's Coordinated Efforts and the Opening of the Diabetes Health and Wellness Institute.” Proceedings of the Baylor University Medical Center 23 (3): 230–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggiero, L. , Moadsiri A., Butler P., Oros S. M., Berbaum M. L., Whitman S., and Cintron D.. 2010. “Supporting Diabetes Self‐Care in Underserved Populations: A Randomized Pilot Study Using Medical Assistant Coaches.” The Diabetes Educator 36 (1): 127–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggiero, L. , Riley B. B., Hernandez R., Quinn L. T., Gerber B. S., Castillo A., Day J., Ingram D., Wang Y., and Butler P.. 2014. “Medical Assistant Coaching to Support Diabetes Self‐ Care among Low‐Income Racial/Ethnic Minority Populations: Randomized Controlled Trial.” Western Journal of Nursing Research 36 (9): 1052–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinsky, C. A. , Sinsky T. A., Althaus D., Tranel J., and Thiltgen M.. 2010. “‘Core Teams': Nurse‐Physician Partnerships Provide Patient‐Centered Care at an Iowa Practice.” Health Affairs 29 (5): 966–8. [DOI] [PubMed] [Google Scholar]
- Sinsky, C. A. , Willard‐Grace R., Schutzbank A. M., Sinsky T. A., Margolius D., and Bodenheimer T.. 2013. “In Search of Joy in Practice: A Report of 23 High‐Functioning Primary Care Practices.” The Annals of Family Medicine 11 (3): 272–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strong, T. 2015. “Care Team Redesign: Transforming Medical Assistant Roles in Primary Care.” HealthAffairs Blog. Bethesda, MD: Project HOPE—The People‐to‐People Health Foundation, Inc. [Google Scholar]
- Thom, D. H. , Hessler D., Willard‐Grace R., Bodenheimer T., Najmabadi A., Araujo C., and Chen E. H.. 2014. “Does Health Coaching Change Patients' Trust in Their Primary Care Provider?” Patient Education & Counseling 96 (1): 135–8. [DOI] [PubMed] [Google Scholar]
- Thom, D. H. , Willard‐Grace R., Hessler D., DeVore D., Prado C., Bodenheimer T., and Chen E.. 2015. “The Impact of Health Coaching on Medication Adherence in Patients with Poorly Controlled Diabetes, Hypertension, and/or Hyperlipidemia: A Randomized Controlled Trial.” The Journal of the American Board of Family Medicine 28 (1): 38–45. [DOI] [PubMed] [Google Scholar]
- Trimble, C. , and Wielawski I.. 2013. Case Study: The AtlantiCare Special Care Center. Hanover, NH: The Dartmouth Center for Health Care Delivery Science. [Google Scholar]
- U.S. Bureau of Labor Statistics, Department of Labor . 2015. “Occupational Outlook Handbook, 2016‐17 Edition, Medical Assistants” [accessed on February 15, 2016]. Available at http://www.bls.gov/ooh/healthcare/medical-assistants.htm
- U.S. Census Bureau. Washington, DC . 2010. “American Community Survey, Public Use Microdata Sample” [accessed April 10, 2015]. Available at http://www.census.gov/programs-surveys/acs/data/pums.htm
- Walton, J. W. , Snead C. A., Collinsworth A. W., and Schmidt K. L.. 2012. “Reducing Diabetes Disparities through the Implementation of a Community Health Worker‐Led Diabetes Self‐ Management Education Program.” Family & Community Health 35 (2): 161–71. [DOI] [PubMed] [Google Scholar]
- Willard‐Grace, R. , Najmabadi A., Araujo C., Canizalez D., DeVore D., Prado C., Ghorob A., and Bodenheimer T.. 2013. ““I Don't See Myself as a Medical Assistant Anymore”: Learning to Become a Health Coach, in Our Own Voices.” Inquiry in Education 4 (2): Article 2. [Google Scholar]
- Witgert, K. , Kinsler S., Dolatshahi J., and Hess C.. 2014. Strategies to Support Expanded Roles for Non‐Clinicians on Primary Care Teams. Washington, DC: National Academy for State Health Policy. [Google Scholar]
- Yarnall, K. S. , Pollak K. I., Ostbye T., Krause K. M., and Michener J. L.. 2003. “Primary Care: Is There Enough Time for Prevention?” American Journal of Public Health 93 (4): 635–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zareen, M. , Razzaq K., and Mujtaba B. G.. 2013. “Job Design and Employee Performance: The Moderating Role of Employee Psychological Perception.” European Journal of Business and Management 5 (5): 46–66. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Appendix SA2: Case Study Outline.


