Abstract
Objective
Anxious and depressive states are associated with increased cardiovascular disease (CVD) risk and a proinflammatory phenotype, although the latter appears to be at least partially explained by adiposity. We hypothesized that depression and anxiety would be associated with elevated inflammation independent of adiposity in persons with obesity at high risk of CVD.
Methods
We explored the relation between baseline anxiety as measured by the Beck Anxiety Inventory (BAI) and depression as measured by the Beck Depression Inventory-II (BDI-II), and baseline serum c-reactive protein (CRP) in a cross-sectional sample of 100 participants [mean (SD) age 57.8 (7.7) years; 64% female] with obesity [mean (SD) body mass index, BMI 37.3 (5.5) kg/m2] enrolled in a clinical trial for pharmacological weight loss interventions.
Results
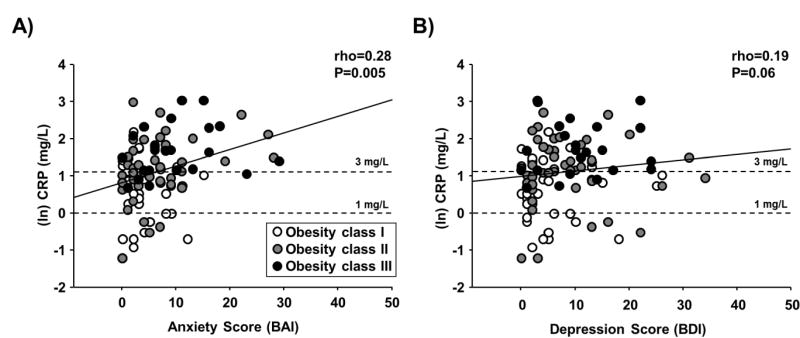
BAI, but not BDI-II, scores were significantly correlated with CRP (rho=0.28, p=0.005). BMI was also highly correlated with CRP (rho=0.42, p<0.0001). In multivariate models, the relation between anxiety and CRP remained significant (p=0.038), independent of BMI, age and sex.
Conclusion
Anxiety, but not depression, is associated with elevated inflammation in persons with obesity beyond that attributable to higher BMI. Further study is warranted to assess whether anxiety represents a potential therapeutic target to mitigate corresponding CVD risk associated with elevated inflammation in persons with obesity.
Keywords: body mass index, depression, c-reactive protein, risk factors
INTRODUCTION
Anxiety and mood disorders are established risk factors for cardiovascular disease (CVD) [1, 2]. The CVD risk associated with anxiety and mood disorders has been purported to be, in part, from elevations in circulating pro-inflammatory markers, such as c-reactive protein (CRP) [3–7], tumor necrosis factor-α [3, 7] and interleukin-6 [3, 7]. This is important because chronic elevations in circulating CRP, for example, predict myocardial infarction, stroke and sudden cardiac death in prospective studies [8]. However, anxiety is often linked with comorbidities and other mood disorders such as depression, therefore, it remains unclear the extent to which higher anxiety alone contributes to elevated inflammation.
Circulating CRP concentrations are also elevated in persons with obesity [9], an established CVD risk factor and promoter of a proinflammatory phenotype. Importantly, individuals with obesity are more likely to suffer from anxiety or mood disorders such as depression, particularly when obesity is severe [1, 10]. In bariatric surgery candidates, the lifetime prevalence of anxiety disorders has been estimated to be as high as 15–27% [11–12]. Given this high prevalence of anxiety among obese individuals, a focus on whether anxiety is linked with inflammation independent of adiposity is clinically important. Previous findings have demonstrated that most of the relation between anxiety and CRP was explained by body mass index (BMI) [7], while in two similar samples the association between anxiety measures and CRP remained independent of BMI [3, 6]. Thus, findings have been mixed, perhaps in part because studies have included non-obese participants (mean BMI values of ~25 kg/m2) [3, 6, 7] which may limit interpretation. Investigations focused on the relation between anxiety and inflammation in obese individuals (i.e., BMI ≥ 30 kg/m2) are needed to extend previous findings and further understand the advanced CVD risk in obese individuals with anxiety and depression.
Therefore, we sought to assess the magnitude of the association between anxiety, depression and inflammation, as measured by CRP, in a cross-sectional sample of participants with obesity at high risk of CVD. We hypothesized that both anxiety and depression levels would be associated with higher CRP independent of BMI in obese participants.
METHODS
Sample
The current analysis uses baseline data from a clinical trial of pharmacotherapy for weight loss (ClinicalTrials.gov Identifier NCT01351753) [13]. Persons age 40 to 75 with a BMI ≥ 30 kg/m2 and at least one additional risk factor for CVD (e.g., diabetes mellitus, elevated fasting glucose, hyperlipidemia, hypertension and metabolic syndrome) were eligible. Exclusion criteria have been described in detail elsewhere [13]. Participants provided written informed consent as part of a University of Iowa Institutional Review Board approved protocol. Of the 106 participants with baseline assessments, we restricted our sample to the 100 participants with available CRP measurements.
Exposure and Outcome Assessments
Anxious and depressive symptoms were measured using the Beck Anxiety Inventory (BAI) and Beck Depression Inventory (BDI-II) [14], which have been utilized commonly in samples with obesity [15]. On the same day, participants underwent phlebotomy and serum CRP concentrations were measured by a high sensitivity turbidimetric assay with a lower level of detection of 0.2 mg/L.
Statistical Analysis
Non-parametric bivariate correlations were assessed between the BAI and BDI-II questionnaires and CRP with a Bonferroni-corrected α=0.025 for statistical significance. Correlations with BMI were also assessed. For use in regression, CRP was natural log transformed (lnCRP), consistent with prior methods [4]. Multivariate linear regression models were adjusted for potential confounding variables (age, sex and BMI) in pursuit of significant bivariate correlations. Moderation by sex and BMI (as both linear effect and indicator for Class III or greater obesity) were explored through interaction terms. Sensitivity analyses controlled for a non-linear effect of BMI by adjusting for obesity class rather than the continuous measure. Sensitivity analyses also assessed relations with untransformed CRP. All statistical analyses were performed using SAS software, version 9.4. (SAS Institute, Inc., Cary, NC).
RESULTS
Clinical characteristics of the sample are highlighted in Table 1. Average scores of measures of psychological distress were in the minimal range (BAI ≤ 9, BDI-II ≤ 13). With regard to anxiety symptoms, 16 persons had scores in the mild (BAI 10–16) and 7 in the moderate range (BAI 17–29). With regard to depressive symptoms, 9 had scores in the mild (BDI-II 14–19), 9 in the moderate (BDI-II 20–28) and 2 in the severe (BDI-II 29–63) range. Eighty-five (85%) participants had CRP concentrations >1.0 mg/L, and fifty-five participants (55%) had CRP concentrations ≥ 3.0 mg/L, the threshold most consistently associated with elevated CVD risk (8).
Table 1.
Clinical Characteristics of Sample (n=100).
| N (%) | |
|---|---|
| Female Sex | 64 (64%) |
| Race/Ethnicity | |
| White, Non-Hispanic | 90 (90%) |
| Unknown/not reported | 10 (10%) |
| Smoking Status | |
| Current Smoker | 4 (4%) |
| Former Smoker | 21 (21%) |
| Obesity Class: | |
| Class I (BMI 30–34.9 kg/m2) | 41 (41%) |
| Class II (BMI 35–39.9 kg/m2) | 38 (38%) |
| Class III (BMI ≥ 40 kg/m2) | 21 (21%) |
| NCEP-defined Metabolic Syndrome | 56 (56%) |
| Medications: | |
| Antihypertensive | 60 (65%) |
| Lipid lowering | 39 (42%) |
| Estrogen replacement therapy | 12 (12%) |
| Systemic | 5 (5%) |
| Vaginal | 7 (7%) |
|
| |
| Mean (SD) | |
|
| |
| Age, years | 55.8 (7.7) |
| Body mass index, kg/m2 | 37.3 (5.2) |
| Hemodynamics: | |
| Systolic blood pressure, mmHg | 128.2 (14.9) |
| Diastolic blood pressure, mmHg | 73.1 (8.9) |
| Heart Rate, bpm | 70.3 (9.9) |
| Lipid Profile: | |
| Total cholesterol, mg/dL (n=99) | 198.3 (38.8) |
| LDL-cholesterol, mg/dL | 116.2 (34.6) |
| HDL-cholesterol, mg/dL | 54.4 (16.1) |
| Triglycerides, mg/dL (n=99) | 140.1 (56.9) |
| Glucose Metabolism: | |
| Fasting glucose, mg/dL (n=99) | 97.4 (10.8) |
| Insulin, mIU/L (n=97) | 14.7 (8.4) |
| HOMA-IR (n=96) | 3.6 (2.2) |
| Hemoglobin A1C, % (n=95) | 6.0 (2.4) |
| Ratings of Psychological Distress: | |
| Beck Anxiety Inventory (n=98) | 6.7 (6.3) |
| Beck Depression Inventory - II (n=99) | 8.4 (7.7) |
| CRP, mg/L | 4.4 (4.2) |
BMI, body mass index; LDL, low density lipoprotein; HDL, high denisty lipoprotein; HOMA-IR, homestasis model of insulin resistance; CRP, c-reactive protein; NCEP, National Cholesterol Education Program.
BAI scores were correlated with both BMI (rho=0.26, 95% C.I. 0.07–0.44, p=0.009) and CRP (rho=0.28, 95% C.I. 0.09–0.45, p=0.005) (Figure 1A). BDI-II scores were similarly correlated with BMI (rho=0.27, 95% C.I. 0.08–0.45, p=0.006), but only marginally with CRP (rho=0.19, 95% C.I. −0.01–0.37, p=0.06) (Figure 1B). As expected, BMI was strongly correlated with CRP (rho=0.42, p<0.0001). In multivariate regression models (Table 2), adjusting for age and sex, anxiety (t=2.11, p=0.038) and BMI (t=2.37, p=0.02) were independent predictors of CRP. In the analogous BDI-II models, BMI was significantly associated with CRP (t=2.80, p=0.006), while depression was not associated with CRP (p=0.59). The anxiety effect persisted (p=0.025) when weight was alternatively modeled by obesity class, when adjusting for current or former smoking (p=0.004), use of lipid lowering medications (p=0.005), use of an antihypertensive (p=0.006) or use of estrogen replacement therapy (p=0.008), in addition to age and sex. Similar findings were observed with untransformed CRP. Although, there were no statistically significant interactions between psychological measures and sex or BMI on CRP, there was a marginally significant interaction for the categorical variable of Class II or greater obesity and anxiety on CRP (p=0.07). When the sample was stratified into those with Class I (n=41) and Class II or greater (n=59) obesity, the association between BAI scores and CRP was significant only for those with Class II or greater obesity (Class I rho=−0.05, p=0.74; Class II or greater rho=0.34, p=0.009). Similar results were seen when stratifying by the presence of metabolic syndrome (no metabolic syndrome rho=0.18, p=0.24; metabolic syndrome rho=0.38, p=0.004).
Figure 1.
Bivariate unadjusted correlations between (ln) c-reactive protein (CRP) and A) anxiety score, and B) depression score in persons with obesity. Dotted lines represent non-log transfomed clinical concentrations of CRP associated with intermediate cardiovascular disease (CVD) risk (≥1 mg/L) and high CVD risk (≥3 mg/L)
Table 2.
Results of Multivariate Linear Regression Models for Anxiety and Depression on Serum CRP.
| b | SE | t | p | |
|---|---|---|---|---|
| Anxiety Model | ||||
| Beck Anxiety Inventory Score | 0.030 | 0.014 | 2.11 | 0.038* |
| Body mass index (kg/m2) | 0.041 | 0.017 | 2.37 | 0.02* |
| Age (years) | 0.010 | 0.011 | 0.89 | 0.38 |
| Male sex | −0.433 | 0.185 | −2.33 | 0.021* |
|
| ||||
| Depression Model | ||||
| Beck Depression Inventory Score | 0.007 | 0.012 | 0.54 | 0.59 |
| Body mass index (kg/m2) | 0.050 | 0.018 | 2.80 | 0.006* |
| Age (years) | 0.009 | 0.012 | 0.78 | 0.44 |
| Male sex | −0.491 | 0.187 | −2.63 | 0.01* |
p < 0.05.
DISCUSSION
The major and novel finding of the present study is that anxiety is associated with elevated inflammation in persons with obesity beyond the level of inflammation attributable to obesity alone. Despite anxiety and depression levels having similar correlations with obesity, only anxiety levels remained significantly associated with inflammation in this sample of individuals with obesity. Furthermore, the persistent correlation between anxiety and inflammation was independent of BMI, in addition to age and sex. Our findings suggest that anxiety and BMI may have independent and additive effects in contributing to a proinflammatory state in human obesity.
Individuals with obesity are more likely to suffer from anxiety and depression, and exhibit elevations in systemic inflammation. Previous investigations have reported mixed results in regards to the contribution of higher anxiety to elevated inflammation in obese individuals. Inconsistent findings may be from inclusion of participants with predominantly lower BMI [3, 6, 7]. To our knowledge, only one prior study has been conducted in a sample with obesity [16]. In this similarly sized sample of persons with morbid obesity awaiting bariatric surgery (n=101), trait anxiety and depression were cross-sectionally associated with CRP, even after adjusting for BMI [16]. However, following bariatric surgery, reductions in the anxiety, but not the depression facet of neuroticism, were associated with decreases in CRP [16]. Although the reason for these contrary findings is unclear, results from our study provide support for the associated decrease in CRP with reductions in anxiety but not depression in the aforementioned bariatric study. Although anxiety and depression symptoms had similar correlations with obesity in our study, only anxiety symptoms remained significantly associated with inflammation when adjusting for BMI. Thus, our results extend previous findings to a more representative cohort of adults with obesity not awaiting bariatric surgery but at high CVD risk. The abolishment of the relation between CRP and depression after adjusting for BMI suggests that obesity and depression might share overlapping pathways of inflammatory activation [17, 18], whereas anxiety modulates inflammation in persons with obesity at least partly through mechanisms independent of adiposity.
The present study is limited by its cross-sectional nature which precludes the directionality of the relation between anxiety and inflammation. However, several prospective studies of both depression [19] and anxiety [20] have suggested psychological distress precedes the development of elevated inflammation, but do not rule out that the relation may be bidirectional. Although measuring other inflammatory cytokines (e.g., tumor necrosis factor-α, etc.) may have been helpful to discern a more generalized phenotype of inflammatory activation, CRP is the strongest circulating inflammatory biomarker of CVD risk [8]. Furthermore, our study was limited largely to white, non-Hispanic individuals, therefore, further studies among persons of non-white and Hispanic race/ethnicity are needed.
In summary, we found anxiety to be independently associated with elevated CRP in a sample of adults with obesity and at least one other major CVD risk factor. The magnitude of the association approached that previously reported for BMI. If inflammatory activation in obesity is amplified by anxiety, it may contribute to some long-term complications of obesity such as CVD. Thus, anxiety and any pathways by which anxiety may induce inflammation may be a previously underappreciated target for interventions to mitigate the risk for obesity-related CVD.
What is already known about this subject?
Anxiety states and depressive disorders are associated with elevations in inflammatory markers such as C-reactive protein (CRP)
Circulating CRP concentrations are elevated in persons with obesity and CRP is a strong biomarker of CVD risk
Individuals with obesity are more likely to suffer from anxiety and depressive disorders, but whether anxiety and depression are associated with inflammation independent of adiposity is unclear
What does this study add?
Anxious, but not depressive, symptoms were associated with elevated inflammation as measured by circulating CRP.
The association between CRP and anxiety was independent of age, gender and body mass index (BMI).
Further studies are required to determine if anxiety represents a potential therapeutic target to mitigate corresponding CVD risk associated with elevated inflammation in persons with obesity.
Acknowledgments
The authors are indebted to William G. Haynes, James Chounramany, Tamara Lowe, Elaine Paul, Thomas Sardone, Christine Sinkey and Jane Williams# for their assistance.
# - Deceased
Funding: Dr. Pierce was funded by NHLBI (P01HL014388) and the American Heart Association (13SDG143400012) during the project period. Dr. Kalil and Holwerda were funded by the National Institutes of Health (NIH) T32 Training Grant (HL07121) during the project period. Dr. Fiedorowicz was funded by the NIMH (K23 MH083695) and the NHLBI (P01HL014388) during the project period. The Institute for Clinical and Translational Science at the University of Iowa is supported by the NIH Clinical and Translational Science Award (CTSA) program, grant U54TR001356. The CTSA program is led by the NIH’s National Center for Advancing Translational Sciences (NCATS).
Footnotes
Disclosures: none
References
- 1.Fiedorowicz JG, He J, Merikangas KR. The association between mood and anxiety disorders with vascular diseases and risk factors in a nationally representative sample. J Psychosom Res. 2011;70:145–154. doi: 10.1016/j.jpsychores.2010.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roest AM, Martens EJ, de Jonge P, Denollet J. Anxiety and risk of incident cardiovascular disease risk. J Amer Coll Cardiol. 2010;56:38–46. doi: 10.1016/j.jacc.2010.03.034. [DOI] [PubMed] [Google Scholar]
- 3.Pitsavos C, Panagiotakos DB, Papageorgiou C, Tsetsekou E, Soldatos C, Stefanadis C. Anxiety in relation to inflammation and coagulation markers, among healthy adults: the ATTICA study. Atherosclerosis. 2006;185:320–326. doi: 10.1016/j.atherosclerosis.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 4.Vogelzangs N, Beekman AT, de Jonge P, Penninx BW. Anxiety disorders and inflammation in a large adult cohort. Transl Psychiatry. 2013;3:e249. doi: 10.1038/tp.2013.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bankier B, Barajas J, Martinez-Rumayor A, Januzzi JL. Association between C-reactive protein and generalized anxiety disorder in stable coronary heart disease patients. Eur Heart J. 2008;29:2212–2217. doi: 10.1093/eurheartj/ehn326. [DOI] [PubMed] [Google Scholar]
- 6.Liukkonen T, Rasanen P, Jokelainen J, et al. The association between anxiety and C-reactive protein (CRP) levels: results from the Northern Finland 1966 birth cohort study. Eur Psychiatry. 2011;26:363–369. doi: 10.1016/j.eurpsy.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 7.Duivis HE, Vogelzangs N, Kupper N, de Jonge P, Penninx BW. Differential association of somatic and cognitive symptoms of depression and anxiety with inflammation: findings from the Netherlands Study of Depression and Anxiety (NESDA) Psychoneuroendocrinology. 2013;38:1573–1585. doi: 10.1016/j.psyneuen.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 8.Ridker PM. Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation. 2003;107:363–369. doi: 10.1161/01.cir.0000053730.47739.3c. [DOI] [PubMed] [Google Scholar]
- 9.Choi J, Joseph L, Pilote L. Obesity and C-reactive protein in various populations: a systematic review and meta-analysis. Obes Rev. 2013;14:232–244. doi: 10.1111/obr.12003. [DOI] [PubMed] [Google Scholar]
- 10.Onyike CU, Crum RM, Lee HB, Lyketsos CG, Eaton WW. Is obesity associated with major depression? Results from the Third National Health and Nutrition Examination Survey. Am J Epidemiol. 2003;158:1139–1147. doi: 10.1093/aje/kwg275. [DOI] [PubMed] [Google Scholar]
- 11.Jones-Corneille LR, Wadden TA, Sarwer DB, et al. Axis I psychopathology in bariatric surgery candidates with and without binge eating disorder: results of structured clinical interviews. Obes Surg. 2012;22:389–397. doi: 10.1007/s11695-010-0322-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosenberger PH, Henderson KE, Grilo CM. Psychiatric disorder comorbidity and association with eating disorders in bariatric surgery patients: A cross-sectional study using structured interview-based diagnosis. J Clin Psychiatry. 2006;67:1080–1085. doi: 10.4088/jcp.v67n0710. [DOI] [PubMed] [Google Scholar]
- 13.Kalil GZ, Recober A, Hoang-Tienor A, Zimmerman MB, Haynes WG, Pierce GL. Higher augmentation index is associated with tension-type headache and migraine in obese middle-aged/older humans. Obesity. 2016;24:865–870. doi: 10.1002/oby.21414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. Psychological Corp; San Antonio, TX: 1996. [Google Scholar]
- 15.Lent MR, Napolitano NA, Wood GC, et al. Still. Internalized weight bias in weightloss surgery patients: psychosocial correlates and weight loss outcomes. Obes Surg. 2014;24:2195–2199. doi: 10.1007/s11695-014-1455-z. [DOI] [PubMed] [Google Scholar]
- 16.Capuron L, Poitou C, Machaux-Tholliez M, et al. Relationship between adiposity, emotional status and eating behaviour in obese women: role of inflammation. Psychol Med. 2011;41:1517–1528. doi: 10.1017/S0033291710001984. [DOI] [PubMed] [Google Scholar]
- 17.Cheng T, Dimitrov S, Pruitt C, Hong S. Glucocorticoid mediated regulation of inflammation in human monocytes is associated with depressive mood and obesity. Psychoneuroendocrinology. 2016;66:195–204. doi: 10.1016/j.psyneuen.2016.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kiecolt-Glaser JK, Derry HM, Fagundes CP. Inflammation: depression fans the flames and feasts on the heat. Am J Psychiatry. 2015;172:1075–1091. doi: 10.1176/appi.ajp.2015.15020152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stewart JC, Rand KL, Muldoon MF, Kamarck TW. A prospective evaluation of the directionality of the depression-inflammation relationship. Brain Behav Immun. 2009;23:936–944. doi: 10.1016/j.bbi.2009.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Copeland WE, Shanahan L, Worthman C, Angold A, Costello EJ. Generalized anxiety and C-reactive protein levels: a prospective, longitudinal analysis. Psychol Med. 2012;42:2641–2650. doi: 10.1017/S0033291712000554. [DOI] [PMC free article] [PubMed] [Google Scholar]