Abstract
Objective
The study examined diurnal regulation of salivary alpha-amylase (sAA) in association with daily stressors, adult day services (ADS) use, and other caregiving characteristics.
Methods
A sample of 165 family caregivers of individuals with dementia (IWD) completed an 8-day diary study. Caregivers provided 5 saliva samples across the 8 days. On some days, caregivers provided all or most of the care. On other days, their relative attended ADS for part of the day. A 3-level unconditional linear spline model was fit to describe the typical sAA diurnal rhythms. Predictors were then added to the unconditional model to test the hypotheses on ADS use and daily stressors.
Results
Daily ADS use did not have an effect on diurnal sAA regulation. However, controlling for daily ADS use, greater ADS use over the 8 days was associated with a more prominent rise between 30 minutes after wake-up and before lunch, and a more prominent decline between before lunch and late afternoon. Fewer ADS days were associated with a more flattened sAA diurnal rhythm. Additionally, greater daily care-related stressor exposures had a within-person association with lower sAA levels in the late afternoon. Care-related stressor exposures had significant within- and between-person associations with sAA diurnal slopes. Furthermore, daily positive experiences had a significant between-person association with sAA diurnal slopes.
Conclusions
Caring for a disabled family member may heighten the vulnerability to potential physiological conditions. Respite from care stressors from ADS use may have some biobehavioral benefits on sAA regulations.
Keywords: adult day services (ADS), daily stressors, salivary alpha-amylase, family caregivers
Family caregiving to individuals with dementia (IWDs), which is usually sustained for years, has been found to be both physically and emotionally challenging (Aneshensel, Pearlin, Mullan, Zarit, & Whitlatch, 1995). The chronicity of helping IWDs with daily, recurrent tasks can take a toll on caregivers’ health and well-being (Pinquart & Sörensen, 2003). Contemporary theories suggest that individual differences in the reactivity and regulation of biobehavioral stress responses moderate the link between caregiving stress and risk for negative health outcomes. Two major components of the stress response involve activation of the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic nervous system (SNS) (Chrousos & Gold, 1992). This activation results in key biomarkers of HPA-axis and SNS activity, which can be measured non-invasively in saliva, such as salivary cortisol and salivary alpha-amylase (sAA) respectively (Granger, Kivlighan, El-Sheikh, Gordis, & Stroud, 2007).
In spite of the large number of studies showing stress reactivity between acute stressors and sAA levels in the laboratories, few studies have focused on effects of different types of stressors on sAA diurnal rhythms in the naturalistic settings of everyday lives. It is known that chronic stress that is traumatic and largely uncontrollable in nature is associated with a flat diurnal cortisol rhythm with elevated daily total output (Miller, Chen & Zhou, 2007). However, much less is known about sAA level changes and its diurnal profiles in response to daily stress among people who experience chronic stress. Using daily diaries, this study aims to examine the biobehavioral stress response among dementia family caregivers, and the effects of a caregiving intervention on caregivers’ sAA diurnal regulation.
Salivary alpha-amylase: An indicator of SNS reactivity and regulation
sAA is a well characterized non-invasive surrogate marker of SNS reactivity and regulation (Granger et al., 2007; Nater & Rohleder, 2009). Unique from most other common salivary biomarkers, sAA is produced in the oral cavity by the salivary glands in response to SNS stimulation. sAA appears to be a viable stress marker as it parallels increases in SNS-induced release of norepinephrine, a stress hormone associated with SNS activation (Rohleder & Nater, 2009). Studies in the laboratories showed that sAA levels increase in response to acute stressors such as physical exercise, heat and cold stress, the Trier Social Stress Test, as well as taking examinations and competitions (see Klein et al., 2010; Nater & Rohleder, 2009 for reviews).
While a number of studies have found increased sAA levels in response to acute stressors, only a handful of studies in naturalistic settings measured changes in sAA. These studies have suggested different patterns of association in sAA levels and diurnal rhythms with repeated stressors (i.e., chronic stress), which is characteristic of a physiological toll on sAA output. In a study on competitive ballroom dancers, Strahler and colleagues (2010) found that younger male dancers showed a blunted diurnal profile of sAA with flattened slopes throughout the day, which is believed to reflect the cumulative wear and tear of the body. In a caregiver study, Rohleder and colleagues (2009) found that, compared to controls, caregivers of cancer patients showed a decreasing-and-increasing pattern over time in diurnal output of sAA, which paralleled the timing of patient radiotherapy. During the most stressful period of radiotherapy, caregivers’ sAA showed lower levels throughout the day, and a less pronounced increase in the early afternoon. Furthermore, the changes in caregiver sAA profile were accompanied by a profound increase in systemic inflammation. These studies suggest that chronic stress was associated with lower levels of sAA, including lower daily output, and flattened diurnal rhythms (i.e., less pronounced nadir in the morning and less afternoon increase).
Thus dysregulated sAA response to stressors can be either hyper or hypo depending on the specific types of stressors. In the laboratory-induced acute stress situations, sAA dysregulation can mean poor sAA recovery from pre- to post-stress conditions (i.e., hyper). Whereas in the naturalistic settings of everyday lives, sAA dysregulation can mean attenuation with lowered levels and less output under chronic stress (i.e., hypo). Further, both hyper and hypo sAA dysregulation has been associated with physical health problems. Laboratory studies showed that sustained high sAA levels in post-stress conditions and poor sAA recovery from pre- to post-stress conditions were associated with increased health problems such as fatigue and frequency of illness among children (Granger et al., 2007). Additionally, sAA levels were positively associated with SIgA, an antibody playing a critical role in mucosal immune protection against upper respiratory infection, during post-challenge conditions and recovery from pre- to post-challenge conditions (Granger et al., 2007). Studies in naturalistic and everyday settings showed that lower sAA activity in response to chronic stress (i.e., lower daily sAA output) was found among children and adolescents with asthma (Wolf, Nicholls, & Chen, 2008).
The daily stress of caregiving and physiology
Recent studies have utilized daily diaries to uncover the dynamics and varying pathways in caregiver health and well-being (Zarit, Kim, Femia, Almeida, & Klein, 2016; Zarit et al., 2011). Daily diaries afford an up-close perspective on experiences, which capture caregiving challenges in detail without the omissions or distortions associated with recall over longer time periods. The most common daily stressors are behavioral and psychological symptoms of dementia (BPSD), such as wandering, agitation, and resistance. BPSD can pose considerable challenges to caregivers on a daily basis, which lead to heightened negative feelings such as burden, overload, and role captivity.
Savla and colleagues (2013) examined BPSD of persons with mild cognitive impairment and associations with spouse caregiver well-being. On days when primary stressors such as memory problems and sundowning effect were experienced, caregivers showed shallow-declining cortisol slopes and higher cortisol levels throughout the day; unpleasant marital interactions were associated with flatter sAA diurnal slopes. Daily positive events, on the other hand, are associated with improved positive affect (Lawton, DeVoe, & Parmelee, 1995), which in turn can relate to enhanced biobehavioral regulation. A recent study found that failure to keep up a positive mood when facing daily challenges may associate with elevated inflammation levels (Sin, Graham-Engeland, Ong, & Almeida, 2015).
Adult day services (ADS) use in relation to caregiving stress and biobehavioral health
ADS programs provide IWDs with social and therapeutic activities and some medical care typically from 9:00 am to 5:00 pm. The time-away from IWDs on ADS days may restructure caregivers’ days differently from non-ADS days with decreased exposure to care-related stressors (BPSD) and increased positive events for caregivers on ADS days (Zarit, Kim, et al., 2014). Daily stressor exposure can be decreased by over 40 percent compared to days when caregivers provide most or all of the care (Zarit et al., 2011). This daily reduction in stressors has been found to be associated with improved well-being (Zarit, Kim, et al., 2014) and improved regulation of two HPA markers, salivary cortisol and salivary dehydroepiandosterone-sulfate (DHEA-S) (Klein et al., 2016; Zarit, Whetzel, et al., 2014). No studies, however, have examined the effect of ADS use on sAA regulation in a dementia caregiver sample.
The current study
Building on prior research that identified the effects of stressor exposures on sAA diurnal rhythm, the current study examines sAA diurnal trajectory among a sample that experienced the chronic stress of dementia caregiving who also had a relatively high level of daily stressors. Caregivers were observed over 8 consecutive days, using ADS on some days of observation and not others. In effect, ADS represents a manipulation by which exposure to naturally occurring daily stressors is varied, with low exposure on ADS days and high exposure on non-ADS days (Zarit, Kim, et al., 2014; Zarit et al., 2011). The study tests whether sAA diurnal slopes vary with daily ADS use compared to non-ADS use, total ADS use over the 8 days, and daily experiences (i.e., stressors and positive experiences) across the 8 days. As there are few studies that have examined sAA diurnal rhythms at the daily level, the typical diurnal trajectory of sAA among caregivers was modeled first using unconditional piecewise linear spline growth curves, which have been applied to model cortisol diurnal rhythms (Ranjit, Young, Raghunathan, & Kaplan, 2005). Guided by prior research, a typical sAA trajectory across the day can be represented by a linear decrease during the 30 minutes of awakening, and a gradual increase throughout the day, with a slight decline between late evening and before bed (Nater, Rohleder, Schlotz, Ehlert, & Kirschbaum, 2007). Specifically, the following hypotheses were tested.
Hypothesis 1
Daily ADS use will be associated with steeper sAA diurnal slopes at the within-person level, whereas on non-ADS days when care-related stressors are relatively high, caregivers will have attenuated or flattened diurnal slopes, controlling for daily experiences (non-care stressors and positive events) and other caregiving characteristics. Specifically, sAA levels are hypothesized to decrease faster in the morning upon awakening, and increase more prominently thereafter on an ADS day.
Hypothesis 2
Total ADS days across the observation period will be associated with sAA diurnal slopes at the between-person level. Specifically, more ADS days will be associated with a faster decreasing slope upon awakening and a more prominent increasing slope throughout the day.
Hypothesis 3
Daily stressor exposures and positive experiences will be associated with sAA diurnal slopes. Specifically, greater daily stressor exposures will be associated with attenuated or flattened sAA diurnal slopes. Positive experiences will be associated with a faster decreasing slope upon awakening and a more prominent increasing slope throughout the day.
Methods
Participants
Participants were 176 family caregivers who participated in an 8-day diary study, the Daily Stress and Health (DaSH) study (Zarit, Kim, et al, 2014). Eligibility for the study included: a) providing primary care to IWDs who lived in the same household, b) reporting the IWD having a type of dementia such as Alzheimer’s disease that was diagnosed by a physician, c) using ADS programs at least two days a week, and d) had no medical problems that limited production of saliva (Zarit, Kim, et al., 2014). Eleven participants (6.3%) who provided daily diaries and sAA samples were excluded from the analysis. Three had mixed up or missed samples (1.7%) and two (1.1%) were sisters who shared care responsibilities equally. An additional six caregivers (3.4%) who only provided a homogeneous set of interviews (i.e., all ADS or all non-ADS days) were also excluded from the analysis. In total, the 165 caregivers provided 6,121 valid sAA samples (95.6 % compliance) on 1,281 valid diary days (97.0 % compliance). Of these 6,121 samples, 3,183 in total (52 %) were collected on ADS days (M = 4.16, SD = 1.45), and 2,938 in total were collected on days when IWDs were at home with their caregivers (M = 3.78, SD = 1.43). Demographic characteristics of caregivers and the IWD they were caring for are presented in Table 1.
Table 1.
Caregivers’ Characteristics at Baseline (N = 165)
| M or Freq | SD or % | Min | Max | |
|---|---|---|---|---|
| Age | 61.99 | 10.70 | 39 | 89 |
| Female | 119 | 87.50 | 0 | 1 |
| Spouse | 64 | 38.79 | 0 | 1 |
| Child | 80 | 58.82 | 0 | 1 |
| Educationa | 4.41 | 1.21 | 1 | 6 |
| Married with a partner | 89 | 65.44 | 0 | 1 |
| Depressive symptomsb | 1.53 | 0.62 | 1 | 5 |
| Role overloadc | 2.81 | 0.65 | 1 | 4 |
| Role captivityc | 2.13 | 0.77 | 1 | 4 |
| Duration of cared | 64.42 | 46.76 | 3 | 216 |
| Number of ADS days per week | 3.86 | 1.17 | 2 | 5 |
| IWD’s ADLs dependencye | 3.01 | 0.50 | 2 | 4 |
Note. ADS = adult day services; IWD = individual with dementia; ADL = activities of daily living.
Measured on a 6-point scale: 1 (less than high school) to 6 (post college degree).
Measured as the mean of 7 items on a 5-point scale: 1 (none of the day) to 5 (all day).
Measured as the mean of 3 items on a 4-point scale: 1 (none of the time) to 4 (all of the time).
Measured in months.
Measured as the mean of 13 ADL items on a 4-point scale: 1 (does not need help) to 4 (cannot do without help).
Procedures
ADS programs were identified through regional and state Adult Day Services associations. Programs that agreed to participate were provided with detailed information about the study, recruitment brochures, and announcements that could be included in the newsletters. Over a 3-year period, family caregivers from 57 ADS programs expressed interest in participation. These caregivers were phoned by the research coordinator, given additional information about the study, and screened for eligibility. Subsequently, an initial face-to-face interview was conducted at the caregiver’s home, during which they signed consent forms and completed a set of questionnaires. After the initial meeting and baseline assessment, caregivers participated in daily interviews for 8 consecutive days via evening phone calls (conducted by the Penn State Survey Research Center); they also provided saliva samples five times each day. Caregivers received $150 for completing the entire study protocol.
Using previously published methods for saliva collection, participants were instructed to: a) provide saliva samples at 5 specified times during the day by rolling an absorbent swab across the tongue for 2 minutes, b) record their saliva collection times, c) avoid taking samples within 30 minutes of eating, drinking, brushing teeth, using tobacco or caffeinated products, and d) refrigerate saliva samples until the end of the 8 days (e.g., Klein et al., 2016). Additionally, participants recorded medications taken over the past 48 hours, tobacco smoking status, and, for women, information on hormone status (e.g., menstrual cycle, hormone therapy use). Instructions for saliva collection were reviewed during an initial in-home interview and in the first phone interview. At the end of the saliva collection period, saliva samples were couriered overnight at room temperature to the Penn State Biomarker Core Lab where they were frozen at − 80 degrees C until assay. On testing day, samples were thawed at room temperature and tested for sAA using a commercially available kinetic enzyme reaction assay kit without modification to the manufacturers recommended protocol (Salimetrics, LLC; State College, PA). The sample test volume was 10 ul of saliva. Salivary alpha-amylase measurement units are expressed in U/mL. The assay range of sensitivity was 2 to 400 U/mL, with average inter- and intra-assay coefficients of variation less than 6% and 7.5%, respectively. Per assay protocol, sAA activity was tested for each sample in singlet. Samples were excluded from the analysis if participants were awake for less than 12hr or greater than 20hr (n = 65) or woke up after 12:00 pm (n = 0). Samples with missing values (n = 171), too little saliva for assaying (n = 103), or missing time or dates (n = 10) were also excluded from the final analysis. The skewness of sAA samples ranged from 2 to 2.69, which was considered not severe (e.g., George & Mallery, 2010). Thus the analysis was done using the original sAA values without any transformation.
Measures
Daily ADS use
In each daily interview the caregivers indicated whether they had made use of ADS that day. From these reports, both time-varying and time-invariant variables were derived. The time-varying (i.e., within-person and daily) ADS use was a binary variable indicating use (= 1) or nonuse (= 0) that day. A time-invariant (i.e., between-person) ADS use was computed as the sum of total ADS days across the daily interview period.
Daily stressors
Two types of daily stressors were distinguished: care-related stressors and non-care stressors. Care-related stressors were considered in relation to the IWD’s daily behavior problems and were measured using the Daily Record of Behavior (DRB). The DRB, designed specifically for use in daily diaries, assesses the frequency with which 19 behaviors occurred over a 24-hour time frame (α = .78; see Femia, Zarit, Stephens, & Greene, 2007 for detailed psychometric properties). To assist caregivers in reporting, the day is broken up into four time-blocks that correspond to the modal periods during which caregivers use ADS: a) waking to 9:00 a.m., b) 9:00 a.m. to 4:00 p.m. (typical ADS attendance hours), c) 4:00 p.m. to bedtime, and d) overnight. For each period of the day, caregivers were asked whether each behavior had occurred (yes/no). From these reports, both time-varying and time-invariant variables were derived. Because overnight stressor exposures were very low, the current study only utilized stressor exposures reported during three day-time windows. The time-varying care-related stressors were the sum of total behavior occurrences reported that day, excluding the overnight period; the time-invariant care-related stressors were the average level of daily behavior occurrences reported across the interview period.
Caregivers may experience daily stressors in other life domains that are unrelated to caring for their relatives. Non-care stressors were measured using the Daily Inventory of Stressful Events (DISE; Almeida, Wethington, & Kessler, 2002). Each evening, caregivers reported on the occurrence (yes/no) of eight events over the previous 24-hour period (α = .59): arguments with other people, whether they avoided an argument with someone, incidents concerning their friends or family, health-related issues or incidents, money or finance-related issues, work-related issues, and other stressful issues or incidents. Separating care-related and non-care stressors, caregivers were specifically instructed to report events they found stressful other than those encountered when assisting their relative. Both time-varying and time-invariant variables were derived based on the daily reports. The time-varying non-care stressors were the sum of stressors reported across all eight categories that day; the time-invariant non-care stressors were the average level of daily stressors reported across the interview period.
Daily positive events
Positive experiences were also assessed as they have been found to reduce the effects of stressors on daily affect and physiological responses (e.g., Zarit, Kim, et al., 2014). Using five items drawn from the DISE (α = .63, Almeida et al., 2002), caregivers reported occurrences of positive experiences during the past 24 hours: sharing a laugh with someone, having an experience at home, with a close friend or relative, or at work that others would consider positive, and any other positive experience. Both time-varying and time-invariant variables based on the daily reports were derived. The time-varying variable was the sum of positive events reported across all five categories that day; the time-invariant variable was the average level of daily positive events across the interview period.
Covariates
Additional variables that have been associated with sAA levels were considered as covariates. Caregivers’ chronological age, gender (1 = female and 0 = male), duration of care provision (months), and the IWD’s ADL dependency (mean of 13 items; coded on a 4-point scale; 1 = does not need help to 4 = cannot do without help; higher scores indicated greater dependency; α = .83). Additionally, sAA shows a moderate diurnal rhythm and there is an awakening response similar to the cortisol awakening response. Because sAA is a surrogate marker of sympathetic nervous system (SNS) activity and sleep affects processes that influence SNS activity, caregivers’ sleep quality was considered as a covariate in the current study. Caregivers responded to the following item each day: “Rate the quality of your sleep last night” (5-point scale; 1 = poor to 5 = excellent). Caregivers’ daily sleep quality was used as a time-varying covariate and caregivers’ mean sleep quality across days was used as a time-invariant covariate.
Analytical strategy
The goal of the analysis was to describe the diurnal rhythm and examine the regularities of naturally-occurring sAA in the daily context. Preliminary analyses were run first using sAA levels at each sampling occasion and daily total output as outcomes. To describe the typical sAA diurnal rhythms among the sample of dementia caregivers, an unconditional four-part piecewise linear spline model was fit with time as the only independent variable. Specifically, daily sAA levels were modeled as functions of time elapsed since wake-up, with knots (where the linear components join in) fixed at 0.5 hr, 6 hr, 10.5 hr and 16 hr after wakeup. Fixed knots allowed the timing of the sAA peak to vary across caregivers. These fixed inflection time points reflected the observed average sampling time. A 3-level unconditional model was used to model the sAA diurnal slopes to account for within-day and within-person correlations in sAA levels.
To test all three hypotheses on ADS use and daily stressor exposures, predictors and covariates were added to the unconditional piecewise linear spline model. To test Hypotheses 1 and 2 on within- and between-person effects of ADS use, daily ADS use and total ADS days were added to the unconditional piecewise linear spline model, respectively. ADS effects were reevaluated after controlling for covariates of other daily experiences and caregiving characteristics. Then this full model was also used to test Hypothesis 3 on effects of daily stressor exposures and positive experiences on sAA diurnal slopes, in the context of ADS use. The full model was specified with the four linear slopes of the four-part linear spline model (i.e., S1, S2, S3, & S4; detailed multilevel equations are provided as supplemental materials). Specifically, S1 was the first linear decline slope from wake-up to 30min after wake-up; S2 was the first linear rise from 30min after wake-up to before lunch; S3 was the second linear rise from before lunch to late afternoon, and S4 the third linear rise from late afternoon to before bed. These four linear slopes were then specified to vary based on within- and between-person ADS use, stressor exposures, and other caregiving characteristics.
Results
Descriptives of individual sAA samples, including the collection time, levels, and the intraclass correlations (ICC) on each individual sample across days, are presented in Table 2. Substantial variation in sampling time and levels was observed. Preliminary analyses were run using each individual sample and daily total output calculated as area under the curve with respect to ground (AUCg) as outcomes (Pruessner, Kirschbaum, Meinlschmid, & Hellhammer, 2003). The purpose of these models was to examine associations between sAA levels and daily stressor exposure as well as effects of caregiving characteristics. Parameter estimates from these models are presented in Table 3. The models showed no within-person (i.e., daily) ADS effect. However, between-person ADS use (i.e., total ADS days) had significant associations with sAA levels from three sampling occasions, and the daily total output as measured by AUCg. Specifically, more ADS days used were associated with higher levels and greater daily output. Additionally, better sleep quality the previous night was associated with lower sAA levels before lunch; more daily care-related stressors were associated with lower sAA levels in the late afternoon.
Table 2.
Daily salivary alpha-amylase sample descriptives
| Collection time |
Level (U/mL) |
||||
|---|---|---|---|---|---|
| Mean | SD (Min) | ICC | Mean (SD) | ICC | |
| Wake-up | 6.44 h | 76.2 | 0.58 | 139.29 (134.06) | 0.59 |
| 30min after wake-up | 7.23 h | 79.2 | 0.57 | 87.39 (80.69) | 0.64 |
| Before lunch | 12.50 h | 74.4 | 0.36 | 162.59 (133.04) | 0.63 |
| Late afternoon | 17.28 h | 71.4 | 0.48 | 169.00 (136.33) | 0.59 |
| Before bed | 22.38 h | 69.6 | 0.66 | 153.89 (137.28) | 0.51 |
Notes. Descriptives were based on 6,121 samples from 1,281 days and 165 caregivers.
Table 3.
Associations between salivary alpha-amylase levels, daily experiences, and caregiving characteristics
| Wake-up | 30-min after Wake-up |
Before Lunch |
Late Afternoon |
Before Bed |
AUCg | |
|---|---|---|---|---|---|---|
|
|
||||||
| Estimate (SE) | Estimate (SE) | Estimate (SE) | Estimate (SE) | Estimate (SE) | Estimate (SE) | |
| Intercept | 144.66 (9.35)*** | 88.80 (5.61) *** | 164.13 (9.34) *** | 168.42 (9.54) *** | 155.88 (9.15) *** | 147.10 (7.64) *** |
| Within-person covariate | ||||||
| Daily ADS use | −7.55 (5.56) | −5.64 (3.04) | −1.09 (5.12) | −6.37 (5.56) | −4.20 (6.09) | −4.03 (3.19) |
| Daily non-care stressors | 0.92 (2.81) | −1.90 (1.55) | 2.41 (2.57) | −1.49 (2.84) | 2.63 (3.09) | −0.29 (1.61) |
| Daily care-related stressors | 1.31 (0.76) | 0.53 (0.42) | −0.39 (0.70) | −1.95 (0.77)* | 0.20 (0.84) | −0.35 (0.44) |
| Daily positive experience | −3.26 (2.73) | −1.02 (1.49) | 3.00 (2.50) | −1.59 (2.72) | −1.51 (2.97) | −0.27 (1.58) |
| Daily sleep quality | 4.58 (3.45) | 1.05 (1.89) | −6.54 (3.13)* | 1.87 (3.41) | −4.47 (3.73) | −1.58 (2.01) |
| Between-person covariate | ||||||
| Total ADS days | 9.38 (6.35) | 8.73 (3.85)* | 16.65 (6.41)** | 10.21 (6.50) | 12.20 (6.12)* | 12.69 (5.38)* |
| Caregiver age | 0.70 (0.88) | 0.82 (0.54) | 0.03 (0.89) | 0.11 (0.90) | 0.44 (0.85) | 0.43 (0.75) |
| Caregiver gender | 22.57 (26.69) | 3.23 (16.21) | −3.82 (26.99) | 21.00 (27.35) | 19.13 (25.76) | 9.44 (22.58) |
| Duration of care | −0.15 (0.20) | −0.15 (0.12) | 0.08 (0.20) | −0.04 (0.20) | 0.04 (0.19) | 0.05 (0.16) |
| IWD's ADL dependency | −1.21 (18.77) | 5.58 (11.38) | 5.69 (18.93) | 9.26 (19.18) | 13.11 (18.07) | 6.66 (15.93) |
| Average non-care stressors | −3.30 (7.26) | −6.43 (4.38) | −4.59 (7.30) | −7.24 (7.42) | −8.17 (7.07) | −6.93 (6.06) |
| Average care-related | 0.06 (1.20) | 0.80 (0.72) | −0.90 (1.20) | −1.60 (1.22) | 0.48 (1.16) | −0.31 (1.01) |
| Average positive | 4.40 (7.11) | 3.43 (4.30) | −4.84 (7.16) | −8.37 (7.27) | 3.28 (6.87) | −1.10 (5.96) |
| Average sleep quality | 0.20 (8.78) | −4.42 (5.30) | −12.95 (8.82) | −9.69 (8.96) | −7.23 (8.49) | −8.96 (7.36) |
Notes. All daily (within-person) covariates were person-mean centered. All between-person covariates were grand-mean centered.
ADS = Adult day services.
AUCg = Area under the curve with respect to ground, calculated using all 5 daily samples. For days missing AUCg, samples #1, 2, and 5 were used to calculate AUCg (n = 72). The total number of days for AUCg in the model was N = 1019.
p ⩽ .05,
p ⩽ .01,
p ⩽ .001.
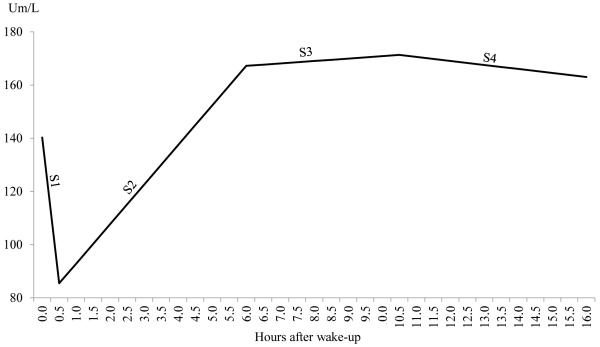
Next, to describe the typical diurnal sAA rhythm, a 3-level unconditional piecewise linear spline model was fit. Parameter estimates are presented for Model 1 in Table 4. The typical diurnal sAA rhythm was graphed in Figure 1, based on parameter estimates from the unconditional model. The model showed that waking sAA level was about 140.26 U/mL, which dropped sharply at a rate of 109.56 U/mL per hour within 30 minutes after wake-up. Then sAA levels gradually increased at a rate of 14.86 U/mL per hour between 30 minutes after wake-up and before lunch. After a stable period between before lunch and late afternoon, sAA decreased slightly at a rate of 1.51 U/mL per hour between late afternoon and before bed.
Table 4.
Effect of ADS use on diurnal salivary alpha-amylase slopes covarying for daily experiences and caregiving characteristics
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
|
|
||||
| Estimate (SE) | Estimate (SE) | Estimate (SE) | Estimate (SE) | |
| Intercept | 140.26 (8.38)*** | 144.59 (8.95)*** | 104.07 (26.27)*** | 143.79 (8.70)*** |
| S1 | −109.56 (11.84)*** | −112.06 (13.86)*** | −95.43 (37.16)* | −107.79 (12.24)*** |
| S2 | 14.86 (1.32)*** | 13.81 (1.53)*** | 6.55 (4.07) | 14.36 (1.32)*** |
| S3 | 0.91 (1.31) | 2.47 (1.68) | 10.25 (4.03)* | 0.57 (1.35) |
| S4 | −1.51 (0.48)*** | −1.71 (0.58)** | −2.95 (1.50)* | −1.30 (0.48)** |
| Within-person covariate | ||||
| Daily ADS use | - | −9.78 (4.98)* | −5.66 (2.65)* | −5.55 (2.67)* |
| S1×daily ADS use | - | 6.51 (13.37) | - | - |
| S2×daily ADS use | - | 1.94 (1.48) | - | - |
| S3×daily ADS use | - | −2.86 (1.99) | - | - |
| S4×daily ADS use | - | 0.37 (0.61) | - | - |
| Daily care-related stressors | - | - | - | 1.05 (0.68) |
| S1×Daily care-related stressors | - | - | - | 0.93 (1.68) |
| S2×Daily care-related stressors | - | - | - | −0.36 (0.18)* |
| S3×Daily care-related stressors | - | - | - | −0.33 (0.24) |
| S4×Daily care-related stressors | - | - | - | 0.17 (0.08)* |
| Between-person covariate | ||||
| Total ADS days | - | - | 9.24 (5.99) | 8.26 (6.16) |
| S1×total ADS days | - | - | −3.21 (8.45) | −1.44 (8.66) |
| S2×total ADS days | - | - | 1.99 (0.92)* | 2.28 (0.94)* |
| S3×total ADS days | - | - | −2.22 (0.91)* | −2.10 (0.94)* |
| S4×total ADS days | - | - | 0.34 (0.34) | 0.16 (0.34) |
| Average care-related stressors | - | - | - | 0.03 (1.12) |
| S1× Average care-related stressors | - | - | - | 1.95 (1.60) |
| S2×Average care-related stressors | - | - | - | −0.31 (0.17) |
| S3×Average care-related stressors | - | - | - | −0.18 (0.18) |
| S4×Average care-related stressors | - | - | - | 0.17 (0.06)** |
| Average positive experience | - | - | - | 4.37 (6.65) |
| S1×Average positive experience | - | - | - | −7.71 (9.38) |
| S2×Average positive experience | - | - | - | −1.53 (1.02) |
| S3×Average positive experience | - | - | - | −0.71 (1.03) |
| S4×Average positive experience | - | - | - | 1.04 (0.36)** |
Notes. All daily (within-person) covariates were person-mean centered. All between-person covariates were grand-mean centered.
S1 = linear slope from wake-up to 30min after wake-up, S2 = linear slope from 30min after wake-up to before lunch, S3 = linear slope from before lunch to late afternoon, S4 = linear slope from late afternoon to before bed. Nonsignificant within- and between-person effects were trimmed from Model 4.
Model 1 = Unconditional linear spline model, Model 2 = Within-person (daily) ADS effect model, Model 3 = Between-person (total) ADS days effect model, Model 4 = Within- and between- person ADS effects model with covariates.
The trimmed within-person effects were: daily non-care stressors, daily positive experience, and daily sleep quality.
The trimmed between-person effects were: age, gender, duration of care, ADL dependency, average non-care stressors, average sleep quality.
p ⩽ .05,
p ⩽ .01,
p ⩽ .001.
Figure 1.
The typical diurnal alpha-amylase trajectory among dementia family caregivers
Notes. Salivary alpha-amylase (sAA) levels were measured in Um/L.
S1-S4 are the four linear components specified in the model.
S1 is the first linear decline slope from wake-up to 30min after wake-up.
S2 is the first linear rise from 30min after wake-up to before lunch.
S3 is the second linear rise from before lunch to late afternoon.
S4 is the third linear rise from late afternoon to before bed.
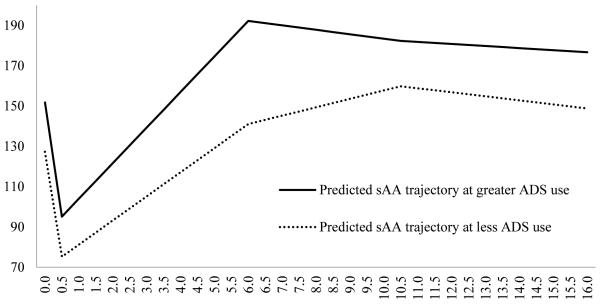
To test the hypotheses on within- and between-person ADS use and diurnal sAA regulations, two models were fit. Daily ADS use and total ADS days used were tested in the unconditional linear spline model respectively, for their main effects and interactions with each of the sAA linear slopes. Parameter estimates are presented for Model 2 and 3 in Table 4. Hypothesis 1 on daily ADS use was not supported, as Model 2 showed no significant interactions of ADS versus non-ADS days with any of the sAA slopes. Hypothesis 2 concerning total ADS days was supported. Model 3 showed that, controlling for daily ADS use, more ADS days were associated with a more prominent rise between 30 minutes after wake-up and before lunch (β = 1.99, p = .03), as well as a more prominent decline between before lunch and late afternoon (β = −2.22, p = .02). Fewer ADS days, on the other hand, were associated with a more flattened sAA diurnal rhythm. This pattern of association between diurnal sAA slopes and total ADS days was graphed in Figure 2.
Figure 2.
The association between total ADS days and alpha-amylase diurnal slopes
Notes
Salivary alpha-amylase (sAA) levels were measured in Um/L.
sAA trajectories were based on parameter estimates in Model 3, the between-person (total) ADS days effect model as presented in Table 3.
Greater ADS use was defined as one standard deviation (SD) above the average ADS days.
Less ADS use was defined as one standard deviation (SD) below the average ADS days.
Finally, a full model was fit with daily stressor exposures and positive experiences, along with within- and between-person ADS effects. The purpose of this full model was to test the third hypothesis on associations between sAA diurnal slopes and daily experiences in the context of ADS use. Nonsignificant effects were trimmed from the final model, and parameter estimates are presented for Model 4 in Table 4. Hypothesis 3 was supported partially. First, care-related stressors had within- and between-person associations with sAA diurnal slopes. Specifically, at the within-person level, more daily care-related stressors were associated with less rise in sAA levels between 30 minutes after wake-up and before lunch (β = −0.36, p = .048); they were also associated with increasing sAA levels between late afternoon and before bed (β = 0.17, p = .03). At the between-person level, more average care-related stressors were associated with increasing sAA levels between late afternoon and before bed (β = 0.17, p = .01). Furthermore, daily positive experiences had a significant between-person association with sAA diurnal slopes only. Specifically, more average positive experiences were associated with increasing sAA levels between late afternoon and before bed (β = 1.04, p = .01). There were no significant associations found for daily non-care stressors.
Additional analysis
To fully evaluate the moderate violation to normality of raw sAA values, additional analyses using square-root transformed sAA values were conducted. The transformation corrected the positive skewness to about 0.8 for all daily samples. Analysis using transformed values showed the same patterns of association with the original analysis using raw values. There were slight differences in p-values found in these two sets of analyses. Lagged analyses were also run using yesterday’s ADS use (=1) as a predictor of today’s sAA levels. The models for testing daily and cumulative ADS effects didn’t show any significant lagged effects. Specifically, the unconditional model did not show significant main effect (β = 2.98, p = .58) of yesterday’s ADS use, or any significant interactions between yesterday’s ADS use and sAA slopes (p-values ranged from .18 to .87). Further, in the full model after adding in all within- and between-person covariates, there were still no significant main effects of yesterday’s ADS use (β = 3.93, p = .47), or any significant interactions between yesterday’s ADS use and sAA slopes (p-values ranged from .36 to .77).
Discussion
The study is one of the first studies to examine sAA diurnal rhythms and the effect of a respite intervention among a sample of dementia family caregivers in the context of daily experiences. The study is unique in many ways. First, participants were experiencing chronic stress, with the majority of the participants providing care for more than one year and less than five years. About a third of the participants has provided care for more than 5 years. In addition to the chronic stress of caregiving, these caregivers also tended to experience a relatively high levels of daily stressors. Second, the study utilized a daily diary design, where caregivers self-reported their daily experiences and provided multiple daily saliva samples across eight days. Such a design is ideal to examine both within- and between-person associations between stressor exposures and health, which has been measured by salivary biomarkers. Third, the respite intervention of day care use was incorporated into the daily design, providing a manipulation on naturally-occuring daily stressor exposures. Thus, it was possible to test if there was any ADS effect on sAA as the high versus low-stress days unfold. Finally, sAA regulation was examined from multiple perspectives of daily levels, daily total output, and diurnal slopes. The sAA diurnal slopes were modeled using a piecewise growth curve approach, which has previously been applied to cortisol diurnal rhythms, but has had limited application in studying sAA diurnal regulations.
The primary purposes of the study were to evaluate the associations between daily stressor exposures and sAA regulation, and to test if there was any ADS effect on participants’ naturally-occuring sAA diurnal profiles in the daily caregiving context. In terms of sAA daily levels, greater daily care-related stressor exposures had a within-person association with lower sAA levels in the late afternoon. Additionally, care-related stressor exposures had significant within- and between-person associations with sAA diurnal slopes. At the within-person level, more daily care-related stressors were related to a blunted rise between 30 minutes after wake-up and before lunch. At both the within- and between-person levels, more daily and average care-related stressors were related to a greater rise between late afternoon and before bed.
These findings on stressor exposures and sAA levels seem to contradict prior research by Nater et al. (2007), where chronic stress was associated with higher average sAA levels across the day. Possible explanations are that their sample of participants were healthier and much younger (mean age was about 27) than the current sample. Their participants were also not experiencing significant chronic stress as measured by the Chronic Stress Screening Scale. The current findings, however, are consistent with a prior caregiving study (Rohleder et al., 2009). That study compared cancer caregivers (mean age was about 50) with a comparison group of non-caregivers. Caregivers had significantly higher perceived stress and depressed mood than the control group. Rohleder and colleagues (2009) also found that during the most stressful period of patient radiotherapy, caregivers showed attenuated sAA patterns with decreased secretion. Specifically, sAA levels were lower in the afternoon, and their sAA diurnal slopes showed a less pronounced rise in the late morning than the controls. Further, the sAA daily total output was steadily increasing among the controls over time, whereas the caregivers had relatively stable output during the study period. These findings confirmed that the chronic stress of caregiving was likely to be associated with an attenuated sAA profile, which reflects the physiological toll of care. Thus, caring for a disabled family member may heighten the vulnerability to potential physiological conditions.
The biobehavioral benefits of ADS use on sAA regulation were twofold. More ADS days used were associated with higher sAA levels in three daily sampling occasions (e.g., 30 min after wake-up, before lunch, and before bed). More ADS days were also associated with higher daily total output. In terms of ADS effect on the sAA diurnal slopes, the study revealed a robust significant between-person association. Specifically, more ADS days were related to a more prominent rise in sAA levels between 30 minutes after wake-up and before lunch, and a more prominent decline in sAA levels between before lunch and late afternoon. It is probable that more ADS days can shield a greater amount of care-related stressor exposures cumulatively, thus the physiological toll of caregiving is not as severe among caregivers who utilized ADS to a greater extent. Rohleder and colleagues (2009) proposed a similar mechanism between stressor exposure and sAA regulation. The current study did not show, however, any within-person association between daily ADS use and sAA diurnal regulation processes, even though ADS use lowered care-related stressor exposure. The absence of a specific within-person effect of ADS may be due to the fast-reacting nature of sAA to stressor exposures and experiences (Granger et al., 2007).
Interestingly, there was a significant association between greater average positive experiences and a steeper sAA slope between late afternoon and before bed. A similar association was also found for daily and average care-related stressors in the same time window during the day. The fact that the SNS is not valence specific, and its arousal is associated with either positive or negative emotions which is driving the reactivity of sAA has been noted in the past research. Adam and colleagues (2011) found that high arousal positive (i.e., feeling excited) and negative emotions (i.e., feeling stressed) were associated with acute sAA increases among youth who had high average levels of these emotions. Thus, sAA increases may reflect emotional arousal in levels of both positive and negative valence. Therefore, the pattern of findings among caregivers in the current study is not surprising.
The study has some limitations. Information on self-reported stressor exposures and positive experiences was collected once at the end of the day. Although the daily diary approach reduces retrospective recall errors compared to use of longer recall periods, the design cannot precisely align stressor exposures with sAA levels within a day. Also, the majority of caregivers self-reported saliva collection time without using a smart time stamp device. This may be another potential source of uncontrolled variation. This is a drawback, especially considering sAA tends to react relatively quickly in response to stressor exposures compared with other kinds of biomarkers such as salivary cortisol (Nater et al., 2006). This limiting feature of the study may be responsible for the nonsignificant association between daily non-care stressors and sAA regulations. Additionally, the study considered a single biomarker of sAA, which mainly reflects stressor reactivity of the SNS. Future studies may consider the synchrony of more than one kind of biomarkers to elucidate the impact of stressors on multiple bodily systems. Further, the study did not control for medication use among caregivers. Some medication taken at specific time may have directly affected the SNS, influencing the sAA diurnal within and between caregivers.
In conclusion, the study expands the scientific understanding on chronic stressor exposures and sAA diurnal regulations. Most importantly, consistent with reports of other studies (Klein et al., 2016; Zarit, Whetzel, et al., 2014) the findings suggest that regular ADS use may have some physiological benefits, which might mitigate the physical toll typically associated with dementia caregiving. Caregiving respite such as ADS use can provide partial but invaluable relief from daily care-related stressor exposures, which can make caregiving more manageable and reduce caregivers’ health risks. Further studies are needed to evaluate the ADS effects from a within-person perspective (i.e., daily ADS use) on other biomarkers and health outcome measures in order to fully realize the broad benefits of respite care on dementia caregiver health and well-being in the long run.
Supplementary Material
Acknowledgments
This research was supported by grant RO1 AG031758 “Daily Stress and Health of Family Caregivers” from the National Institute on Aging (NIA).
Footnotes
In the interest of full disclosure, DAG is founder and Chief Scientific and Strategy Advisor at Salimetrics LLC and Salivabio LLC (Carlsbad, CA) and these relationships are managed by the policies of the committees on conflict of interest at Johns Hopkins University School of Medicine and the Office of Research Integrity and Adherence at Arizona State University.
References
- Adam EK, Hoyt LT, Granger DA. Diurnal alpha amylase patterns in adolescents: Associations with puberty and momentary mood states. Biological Psychology. 2011;88:170–173. doi: 10.1016/j.biopsycho.2011.07.007. doi: 10.1016/j.biopsycho.2011.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aneshensel CS, Pearlin LI, Mullan JT, Zarit SH, Whitlatch CJ. Profiles in caregiving: The unexpected career. Academic Press; San Diego, CA: 1995. [Google Scholar]
- Chrousos GP, Gold PW. The concepts of stress and stress system disorders: Overview of physical and behavioral homeostasis. JAMA: The Journal of the American Medical Association. 1992;267:1244–1252. doi: 10.1001/jama.1992.03480090092034. [PubMed] [Google Scholar]
- George D, Mallery M. SPSS for windows step by step: A simple guide and reference. 10th. Pearson; Boston, MA: 2010. 17.0 update. [Google Scholar]
- Granger DA, Kivlighan KT, El-Sheikh M, Gordis EB, Stroud LR. Salivary α-amylase in biobehavioral research: Recent developments and applications. Annals of the New York Academy of Sciences. 2007;1098:122–144. doi: 10.1196/annals.1384.008. doi: 10.1196/annals.1384.008. [DOI] [PubMed] [Google Scholar]
- Klein LC, Bennett JM, Whetzel CA, Granger DA, Ritter FE. Effects of caffeine and stress on salivary α-amylase in young men. Human Psychopharmacology: Clinical and Experimental. 2010;25:359–367. doi: 10.1002/hup.1126. doi:10.1002/hup.1126. [DOI] [PubMed] [Google Scholar]
- Klein LC, Kim K, Almeida DM, Femia EE, Rovine MJ, Zarit SH. Anticipating an easier day: Effects of Adult Day Services on daily cortisol and stress. The Gerontologist. 2016;56:303–312. doi: 10.1093/geront/gnu060. doi: 10.1093/geront/gnu060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton MP, DeVoe MR, Parmelee P. Relationship of events and affect in the daily life of an elderly population. Psychology and Aging. 1995;10:469–477. doi: 10.1037//0882-7974.10.3.469. doi: 10.1037/0882-7974.10.3.469. [DOI] [PubMed] [Google Scholar]
- Nater UM, La Marca R, Florin L, Moses A, Langhans W, Koller MM, Ehlert U. Stress-induced changes in human salivary alpha-amylase activity—associations with adrenergic activity. Psychoneuroendocrinology. 2006;31:49–58. doi: 10.1016/j.psyneuen.2005.05.010. doi: 10.1016/j.psyneuen.2005.05.010. [DOI] [PubMed] [Google Scholar]
- Nater UM, Rohleder N. Salivary alpha-amylase as a non-invasive biomarker for the sympathetic nervous system: Current state of research. Psychoneuroendocrinology. 2009;34:486–496. doi: 10.1016/j.psyneuen.2009.01.014. doi: 10.1016/j.psyneuen.2009.01.014. [DOI] [PubMed] [Google Scholar]
- Nater UM, Rohleder N, Schlotz W, Ehlert U, Kirschbaum C. Determinants of the diurnal course of salivary alpha-amylase. Psychoneuroendocrinology. 2007;32:392–401. doi: 10.1016/j.psyneuen.2007.02.007. doi: 10.1016/j.psyneuen.2007.02.007. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychology and Aging. 2003;18:250–267. doi: 10.1037/0882-7974.18.2.250. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- Pruessner JC, Kirschbaum C, Meinlschmid G, Hellhammer DH. Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology. 2003;28:916–931. doi: 10.1016/s0306-4530(02)00108-7. doi: 10.1016/S0306-4530(02)00108-7. [DOI] [PubMed] [Google Scholar]
- Ranjit N, Young EA, Raghunathan TE, Kaplan GA. Modeling cortisol rhythms in a population-based study. Psychoneuroendocrinology. 2005;30:615–624. doi: 10.1016/j.psyneuen.2005.02.003. doi: 10.1016/j.psyneuen.2005.02.003. [DOI] [PubMed] [Google Scholar]
- Rohleder N, Marin TJ, Ma R, Miller GE. Biologic cost of caring for a cancer patient: Dysregulation of pro- and anti-inflammatory signaling pathways. Journal of Clinical Oncology. 2009;27:2909–2915. doi: 10.1200/JCO.2008.18.7435. doi: 10.1200/jco.2008.18.7435. [DOI] [PubMed] [Google Scholar]
- Rohleder N, Nater UM. Determinants of salivary α-amylase in humans and methodological considerations. Psychoneuroendocrinology. 2009;34:469–485. doi: 10.1016/j.psyneuen.2008.12.004. doi: 10.1016/j.psyneuen.2008.12.004. [DOI] [PubMed] [Google Scholar]
- Savla J, Granger DA, Roberto KA, Davey A, Blieszner R, Gwazdauskas F. Cortisol, alpha amylase, and daily stressors in spouses of persons with mild cognitive impairment. Psychology and Aging. 2013;28:666–679. doi: 10.1037/a0032654. doi: 10.1037/a0032654. [DOI] [PubMed] [Google Scholar]
- Sin NL, Graham-Engeland JE, Ong AD, Almeida DM. Affective reactivity to daily stressors is associated with elevated inflammation. Health Psychology. 2015;34:1154–1165. doi: 10.1037/hea0000240. doi: 10.1037/hea00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf JM, Nicholls E, Chen E. Chronic stress, salivary cortisol, and α-amylase in children with asthma and healthy children. Biological Psychology. 2008;78:20–28. doi: 10.1016/j.biopsycho.2007.12.004. doi: 10.1016/j.biopsycho.2007.12.004. [DOI] [PubMed] [Google Scholar]
- Zarit SH, Kim K, Femia EE, Almeida DM, Klein LC. The effects of adult day services on family caregivers’ daily stress, affect, and health: Outcomes from the Daily Stress and Health (DaSH) study. The Gerontologist. 2014;54:570–579. doi: 10.1093/geront/gnt045. doi: 10.1093/geront/gnt045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarit SH, Whetzel CA, Kim K, Femia EE, Almeida DM, Rovine MJ, Klein LC. Daily stressors and adult day service use by family caregivers: Effects on depressive symptoms, positive mood, and dehydroepiandrosterone-sulfate. The American Journal of Geriatric Psychiatry. 2014;22:1592–1602. doi: 10.1016/j.jagp.2014.01.013. doi: 10.1016/j.jagp.2014.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.