Abstract
Background.
Ethical, logistical, and funding approaches preclude conducting randomized control trials (RCTs) in some humanitarian crises. A lack of RCTs and other intervention research has contributed to a limited evidence-base for mental health and psychosocial support (MHPS) programs after disasters, war, and disease outbreaks. Propensity score methods (PSMs) are an alternative analysis technique with potential application for evaluating MHPS programs in humanitarian emergencies.
Methods.
PSMs were used to evaluate impacts of education reintegration packages (ERPs) and other (vocational or economic) reintegration packages (ORPs) v. no reintegration programs on mental health of child soldiers. Propensity scores were used to determine weighting of child soldiers in each of the three treatment arms. Multiple linear regression was used to estimate adjusted changes in symptom score severity on culturally validated measures of depression, post-traumatic stress disorder (PTSD), and functional impairment from baseline to 1-year follow-up.
Results.
Among 258 Nepali child soldiers participating in reintegration programs, 54.7% completed ERP and 22.9% completed ORP. There was a non-significant reduction in depression by 0.59 (95% CI −1.97 to 0.70) for ERP and by 0.60 (95% CI −2.16 to 0.96) for ORP compared with no treatment. There were non-significant increases in PTSD (1.15, 95% CI −1.55 to 3.86) and functional impairment (0.91, 95% CI −0.31 to 2.14) associated with ERP and similar findings for ORP (PTSD: 0.66, 95% CI −2.24 to 3.57; functional impairment (1.05, 95% CI −0.71 to 2.80).
Conclusion.
In a humanitarian crisis in which a non-randomized intervention assignment protocol was employed, the statistical technique of PSMs addressed differences in covariate distribution between child soldiers who received different integration packages. Our analysis did not demonstrate significant changes in psychosocial outcomes for ERPs and ORPs. We suggest the use of PSMs in evaluating non-randomized interventions in humanitarian crises when non-randomized conditions are not utilized.
Key words: Children and adolescents, intervention, post-traumatic stress disorder (PTSD), statistical methods, war
Background
A challenge in global mental health research is identifying research methods and statistical techniques to evaluate interventions in settings that may not be amenable to randomized control trials (RCTs). For example, RCTs may be difficult to implement in humanitarian crises, such as environmental disasters, political violence, and infectious disease outbreaks. Only a few RCTs have been conducted in humanitarian crises, and they have tended to focus on adults or have examined interventions that are not widely used in humanitarian crises (Tol et al. 2011); moreover, Tol and colleagues observed that the most frequently used interventions in humanitarian crises are unfortunately the least studied approaches. Ethical issues related to appropriateness of waitlist conditions and lack of acceptable treatment-as-usual alternatives may preclude conducting an RCT (Allden et al. 2009). Logistical issues related to blinding, randomization, and intervention contagion are also challenges for RCTs in humanitarian crises. In addition, there are limited funding mechanisms that can rapidly make research grants available to study mental health and psychosocial in these settings.
These factors have contributed to a lack of intervention research in humanitarian crises, leaving the field with a limited evidence-base for best practices to promote mental health and psychosocial well-being (Tol et al. 2011). Because humanitarian crises disproportionately affect low- and middle-income countries (LMICs) (Tol et al. 2011) and children in LMICs bear the greatest burden of crises such as armed conflict (United Nations, 2014), addressing this gap between research and practice is an important area for global mental health.
Propensity score methods (PSMs) to evaluate humanitarian interventions
In context where it is not ethical or feasible to implement RCTs, one alternative is to use statistical methods to evaluate the impact of intervention components in contexts where a population is given non-randomized access to services. For example, play-interventions, safe spaces, and other activities are commonly provided to children in humanitarian psychosocial responses. In most contexts, these services will not be used by all children and families or at least not used to the same degree. While statistical approaches can be used to compare outcomes between children who did and did not use these services, there are likely multiple confounds that influence which children and families use these services; e.g. either more distressed or less distress children may be using the services thus precluding general comparison of mental health after participating in such an intervention.
PSMs are a set of statistical techniques that can be employed in such contexts because they can account for observed potential confounds between children who are low and high service users. PSMs provide an estimate of treatment effects in non-randomized intervention trials by identifying a control group that is similar to the intervention group with respect to the observed covariates (Rosenbaum & Rubin, 1985). The technique yields treatment and control groups that have similar distributions of observed covariates, thereby approximating one of the fundamental benefits of RCTs in an observational study (Stuart, 2010).
PSM approaches proceed using a two-step analytic approach: first, data are preprocessed (without reference to outcome data) in order to match or weight participants on a combination of observed covariates, with the aim of reducing the association between the treatment assignment and confounding variables. The method assumes that this preprocessing minimizes differences between treatment and control groups on factors that would be expected to affect outcomes (i.e. confounders). Second, after the propensity score model is finalized, matches and/or weighting are incorporated into outcome models as appropriate.
In addition to the philosophical appeal of separating decisions about controlling for confounding from outcome model development, PSMs have several advantages over standard regression techniques (Stuart, 2010): first, PSMs identify and help to account for areas in which covariate distributions do not overlap sufficiently. Insufficient overlap often leads to extrapolation and poor performance of standard regression techniques. Second, PSMs include more straightforward diagnostic approaches to check model assumptions. Third, PSMs can be used in combination with and improve the performance of other regression models. Finally, standard regression relies heavily on correct specification of the underlying model (of confounding), whereas PSMs are more flexible in the typical case in which the exact relationships between confounders and treatment assignments are unknown.
Therefore, PSMs have promise as a tool to improve evaluation for humanitarian programs. There is a growing precedent for the use of PSMs to evaluate ‘natural experiments’, e.g. the effects of remittances on disaster preparedness (Mohapatra et al. 2012), and domestic and international policies, e.g. the effects of foreign aid on civil conflict intensity (Strandow, 2014). PSMs have been used to evaluate planned interventions in humanitarian crises, such as food supplementation for children in Niger (Isanaka et al. 2010). In relation to demobilization and reintegration humanitarian programs for former combatants, studies in Burundi and Sierra Leone have employed PSMs to evaluate economic impacts (Humphreys & Weinstein, 2007; Gilligan et al. 2013). PSMs have also been used to assess political, economic, and psychological consequences of child soldiering in Uganda (Blattman & Annan, 2010). In this paper, we apply PSMs to evaluate the impact of reintegration packages on child soldier mental health and psychosocial well-being in Nepal.
Gaps in evaluation of child soldier reintegration research
Child soldiers, also known as children associated with armed forces and armed groups, are defined as any person below 18 years of age who is or who has been recruited or used by an armed force or armed group in any capacity, including but not limited to fighters, cooks, porters, messengers, spies, or for sexual purposes. It does not only refer to a child who is taking or has taken a direct part in hostilities (UNICEF, 2007, p. 7).
Child soldiers commonly have adverse psychological and psychosocial outcomes following involvement in armed conflicts (Betancourt et al. 2013). In studies using comparison groups, the burden of mental health and psychosocial problems is greater among child soldiers than among civilian children experiencing the conflict (Okello et al. 2007; Kohrt et al. 2008; Blattman & Annan, 2010; Betancourt et al. 2011). In addition to greater exposure to traumatic wartime events, child soldiers often experience rejection and discrimination from families, teachers, peers, and other community members (Betancourt et al. 2013).
The standard practice for international non-governmental organizations (NGOs) and other institutions involved in humanitarian assistance for child soldiers is to conduct disarmament, demobilization, and reintegration (DDR) activities (Williamson, 2006; Humphreys & Weinstein, 2007; Annan et al. 2009). There are many schools of thought about the best approaches to improve psychosocial well-being and mental health among former child soldiers in DDR programs. For example, some practitioners and advocates have argued against mental health terminology and psychotherapeutic interventions because of concerns that they may be stigmatizing, unhelpful, and potentially harmful in non-Western cultural settings (Bracken et al. 1996; Bracken & Petty, 1998). Others have argued for the need to assure availability of psychiatric and psychological services because these have a strong evidence-base (in high resource settings) for reducing distress (Dyregrov et al. 2002). The majority of the field, however, calls for a combination of services ranging from assuring basic economic and livelihood needs to community-based psychosocial care to specialized mental health services (Betancourt & Khan, 2008a; Betancourt & Williams, 2008b), as exemplified by the Inter-Agency Standing Committee (IASC) Intervention pyramid for mental health and psychosocial support (MHPS) in emergencies (IASC, 2007, p. 12).
Unfortunately, there is a dearth of evidence on the mental health impact of these different types of services in humanitarian settings. Although there have been randomized trials of specific interventions for child soldiers (Ertl et al. 2011) and other children affected by war (Jordans et al. 2009), the most commonly used general psychosocial services and reintegration support models have received little evaluation (Tol et al. 2011). The theory of change for education, economic, and social programs is that returning to normal activities will allow children to undergo natural processes of recovery. Moreover, education, economic, and social programs are believed to improve mental health by increasing likelihood of access to basic needs and other resources required for survival and well-being.
However, research on educational, economic, and social reintegration programs during DDR is lacking to determine if and how they impact mental health. From the studies that have been conducted, the benefits of some DDR programming is variable. For example, in Burundi, a retrospective tracer approach was used to compare child soldiers receiving socioeconomic reintegration support with civilian children, which revealed no differences in the groups approximately 3 years after the reintegration support (Jordans et al. 2012). In contrast, a prospective study in Nepal among child soldiers (referred to as verified minors) failed to identify a contribution of reintegration packages to changes in mental health, with the exception that vocational reintegration packages predicted poorer mental health outcomes in the domain of post-traumatic stress disorder (PTSD) symptoms (Adhikari et al. 2014). However, these studies are limited by potential confounds in the design and analysis.
PSMs can address some of these limitations. Therefore, the goal of this study was to address the gap in research literature regarding benefits of reintegration packages on mental health. We used PSMs to study the impact of reintegration packages v. no treatment on psychosocial and mental health outcomes of child soldiers in Nepal.
Methods
Setting: child soldiers in Nepal
Nepal is a landlocked country north of India and south of the Tibetan autonomous region of China, with a population of approximately 28 million. Nepal is a low development country with a rank of 157 out of 186 countries, a life expectancy of 69.1 years, a mean of 3.2 years of education, and a gross national income per capita of US$1,137 (UNDP, 2013). Nepal's population comprises more than 60 ethnic and caste groups (Whelpton, 2005). The society traditionally has been categorized according to a Hindu caste system with Bahun (priest caste) and Chhetri (warrior/royalty caste) at the top of the hierarchy. Dalit/Nepali (untouchables) are the lowest strata of castes. Other ethnic groups (referred to as Janajati), which include other Hindu groups, Buddhists, Muslims, and Kirantis, have different positions in the social hierarchy based on their degree of Hindu purity. The caste stratification influences society heavily with Bahun and Chhetri dominating institutions of government, education, and business (Kohrt, 2009). Dalit/Nepali castes bear the greatest burden of common mental disorders in adult community populations (Kohrt et al. 2009).
In 1996, the Communist Party of Nepal [Maoists, CPN (M)] presented demands to the government of Nepal to address economic and social injustices, abolish the monarchy, end caste- and gender-based discrimination, and establish a constituent assembly. When the government refused to address these demands, the CPN (M) began an agrarian revolution. Government security forces and Maoists killed over 17,000 people during the People's War, which lasted 11 years; with the majority of deaths at the hands of the Royal Nepal Army and the government's police force (INSEC, 2008). The war ended in November of 2006, when the CPN (M) signed a peace treaty with the government. During 2008 elections, the CPN (M) won a two-thirds majority but later abandoned their top government positions (Adhikari, 2014).
During the war, the CPN (M)'s People's Liberation Army (PLA) and the Royal Nepal Army conscripted children as soldiers, sentries, spies, cooks, and porters (United Nations, 2006; Human Rights Watch, 2007). Local groups estimate that at the conclusion of the war approximately 9000 members – one-third of the PLA – comprised 14–18 year old with 40% being girls (Human Rights Watch, 2007). An estimated 10% of the Royal Nepal Army during the conflict was below the age of 18 (Singh, 2004).
Our prior research demonstrated that child soldiers in Nepal showed a higher burden of depression, PTSD, and functional impairment than civilian children who were not associated with armed groups at the conclusion of the war (Kohrt et al. 2008). In 2007, a few months after signing peace accords, 55% of child soldiers had PTSD compared with 20% of matched civilian children (Kohrt et al. 2008).
While differences in war trauma exposure (i.e. the greater exposure among child soldiers compared with civilian children) explains some of the difference between child soldiers and civilian children, there was still a significant difference between the two groups even after controlling for war-related exposures (Kohrt et al. 2008). After the war, discrimination against child soldiers in their homes, schools, and communities contributed to mental health and psychosocial problems (Kohrt et al. 2010a, c). This is consistent with findings regarding stigma and discrimination affecting mental health of former child soldiers in other conflicts (Betancourt et al. 2013). Reintegration packages represent one commonly used approach to improve former child soldiers’ education, economic, and psychosocial status, as well as a technique used in hopes of decreasing re-recruitment into armed groups or involvement in other violent activities.
Reintegration packages
In 2007–2008, Transcultural Psychosocial Organization (TPO) Nepal conducted a study of child soldiers before and after participating in psychosocial and reintegration services provided by UNICEF Partner NGOs in eight districts of Nepal (Kohrt et al. 2010b). Child soldiers in program districts could select among different reintegration packages. The main packages were education, vocational training, apprenticeship, and income-generating activities.
Education reintegration packages (ERPs) were designed to address the lost years of education experienced by child soldiers during their association with an armed group. In Nepal, education reintegration programs were supported through block grants to schools or materials support through School Management Committees, i.e. individual children and families were not given money to send child soldiers back to school. Funds provided in block grants can be used to waive tuition fees for former child soldiers, to buy supplies for target children such as stationery and uniforms, and to support activities such as hiring new teachers and building classrooms to address the influx of children in post-war context. In addition, educational grants can be used to design and implement accelerated 6- or 9-month curriculums that allow former child soldiers to master material from multiple grades in a brief period so that they can then mainstream with same-age peers. Without accelerated programs, former child soldiers in their late teens may join classroom cohorts 5–6 years younger than them.
Vocational training reintegration packages are an alternative to formal education. Former child soldiers who are unable to meet acceptance standards for schools or choose not to rejoin school select vocational training reintegration packages. Vocational training programs for boys tended to focus on radio repair and for girls the skill was typically tailoring. Local NGOs that facilitated vocational training were encouraged to provide certification of vocational training that may help the child soldiers find employment after the training. Vocational training grants included materials (e.g. sewing machines and radio repair kits), in some programs.
Apprenticeship reintegration packages were also available. As opposed to vocational training structured courses, apprenticeship comprised pairing a former soldier with an employer in the community and having them learn a trade. For example, child soldiers entered apprenticeships with truck drivers and other professionals. A reintegration programs subsidized these learning and training opportunities by providing a stipend to the trainee and materials for teaching to the master trainer. Apprenticeship and on-the-job training should reflect the local market demand to ensure sustainability.
Income generation reintegration packages were provided in instances where former child soldiers had an opportunity to pursue a business endeavor and required start-up funds in the form of micro-grants or loans. For example, some former child soldiers received micro-grants to raise poultry or goats. Others used micro-grants to start small businesses such as roadside stalls for tea and household goods.
Each child soldier participated in only one reintegration package. Those in school did not participate in the vocational training, apprenticeship, or income-generating programs. Selection of reintegration packages was based on preferences reported by the child soldier. From an evaluation standpoint, this thus represented an equipoise condition in which beneficiaries selected among interventions available to them. In addition to participation in one reintegration package, all child soldiers were in communities with post-war psychosocial support programs that were made available to both former child soldiers and other children impacted by war. For a description of the psychosocial program, see Kohrt et al. (2015).
Our objective was to evaluate the impact of the reintegration packages on mental health. Specifically, we were most interested in evaluating the impact of the formal ERP, which was the most commonly selected package, v. no reintegration package on mental health. We were also interested in evaluating the impact of ORPs (i.e. vocational, apprenticeship, and income generation) v. no reintegration package on mental health outcomes. We hypothesized that the ERP would have the largest effect on mental health outcomes, specifically on depression. We hypothesized this because our qualitative work suggested that education was the most prioritized resource of returning child soldiers (Morley & Kohrt, 2013); moreover, referral to programs such as vocational training was often seen as secondary option for former child soldiers who were assumed by parents or NGO staff to not be capable of succeeding in school (Adhikari et al. 2014). Therefore, education was expected to be the highest priority support and have the greatest benefit to those who could obtain the package from a mental health and psychosocial perspective.
However, there are a number of pathways in which mental health may have influenced selection choice and participation that would bias interpretation of mental health outcomes. In prior samples of child soldiers in Nepal, low educational achievement prior to reintegration associated with poor mental health outcomes (Kohrt et al. 2008). Because limited prior educational achievement may bias against participation in the formal education reintegration program, the impact of education may be over-estimated in standard comparisons. Other factors such as low caste and female gender are associated with poor mental health outcomes (Kohrt et al. 2008, 2010a). These demographic characteristics are also associated with educational barriers in Nepal. Thus, numerous socioeconomic and demographic factors may associate with poor mental health and lack of participation in ERPs. One way to address such potential confounding factors is by using propensity score weighting to account for differences in the distribution of these demographic characteristics between those who received the ERP compared with those who did not.
Sample size
The sample size for this study was 258 child soldiers who were all offered enrollment in their choice of reintegration packages, in addition to being offered psychosocial support activities provided by TPO-Nepal and partner NGOs. Community-wide psychosocial support activities (e.g. awareness raising, psychosocial support for teachers, and non-religious child activities) were delivered in all target communities [see Kohrt et al. (2015)] regardless of individual former child soldiers’ decisions to participate in specific reintegration packages. All subjects were included in subsequent analyses. Missing data (less than 15% on all variables and less than 6% on all variables except 3) was imputed using single imputation in the Amelia II package in R, which utilizes random sampling from a distribution calculated from observed values on each variable (Honaker et al. 2011). Table 1 indicates the baseline characteristics observed in the full sample, prior to and after weighting.
Table 1.
Means and maximum ASMDs of covariates before and after weighting
| Treatments/baseline characteristics | Education package (n = 141) (mean or %) | Other package (n = 59) (mean or %) | No treatment (n = 58) (mean or %) | Maximum ASMDa before weighting | Maximum ASMDa after weighting |
|---|---|---|---|---|---|
| % Female | 32.7% | 50.1% | 39.7% | 0.37 | 0.15 |
| Age (years) | 15.3 | 16.0 | 15.8 | 0.52 | 0.13 |
| Caste (Dalit) | 19.9% | 27.1% | 31.0% | 0.26 | 0.13 |
| Total traumas (count) | 2.0 | 2.0 | 2.4 | 0.33 | 0.18 |
| DSRS score | 12.9 | 13.6 | 13.0 | 0.15 | 0.07 |
| CPSS score | 17.9 | 18.4 | 17.8 | 0.07 | 0.05 |
| CFI score | 5.9 | 4.9 | 5.9 | 0.21 | 0.11 |
ASMD, absolute standardized mean difference; DSRS, depression self-rating scale; CPSS, child PTSD symptom scale; CFI, child functional impairment scale.
Maximum ASMD is reported as the highest ASMD across all pairwise comparisons (i.e. between treatment groups).
Independent/treatment variable
Participation in the formal reintegration packages was the independent or treatment variable of interest. We evaluated three treatment conditions: (1) ERPs, (2) ORPs (i.e. vocational, apprenticeship, or income generation), and (3) no treatment. The reintegration packages were implemented by local NGOs partnering with UNICEF and are described in detail above. Participants in the two active treatment arms (ERPs and ORPs) were compared with those who did not participate in any reintegration packages.
Propensity score variables
Weighting variables were selected based on anticipated and observed association with both the outcome of interest and treatment assignment. Age in years was measured at the time of enrollment in the study. Sex was self-reported as male or female. Total number of traumatic events at baseline was a count of traumatic events derived from previous ethnographic research and had a possible range from 0 to 13 (Kohrt et al. 2008). Baseline depression self-rating scale (DSRS) for children, child PTSD symptom scale (CPSS), and child functional impairment (CFI) scale scores measured by self-report at the time of study enrollment were also used as weighting variables. The DSRS for children is an 18-item scale assessing depression symptoms on a ‘Mostly’, ‘Sometimes’, or ‘Never’ scale that corresponded with item scores of 2, 1, or 0 (Birleson, 1981), with a range of possible scores on the DSRS is from 0 to 36. The DSRS has been transculturally translated and validated in Nepal (Kohrt et al. 2011). The CPSS (Foa et al. 2001) is a 17-item scale corresponding to DSM-IV-TR symptoms of PTSD with a range of 0–68 and has previously been transculturally translated and validated in Nepal (Kohrt et al. 2011). The CFI is a 10-item scale (range: 0–30) assessing impairment in daily functional role expectations of children in Nepal (Kohrt et al. 2010a).
Outcome variables
The primary outcomes assessed were the changes in DSRS, CPSS, and CFI scores from baseline to 1-year follow-up assessment. That is, positive values represented an increase in depression, PTSD, and functional impairment scores from baseline to follow-up, whereas negative values represented a decrease in symptom and impairment scores.
Details of PSMs
Propensity scores for the three treatment groups were estimated using the mnps (multinomial propensity score) function in the twang statistical package in R (McCaffrey et al. 2013; Burgette et al. 2014). Propensity score weighting to estimate the average treatment effect (ATE) yielded good balance on the measured covariates (see Table 1) and allowed pairwise comparisons between all three treatment arms (Stuart, 2010). ATE refers to the difference in the outcome comparing a (hypothetical) condition where the whole sample received education (or other) reintegration to a (hypothetical) condition where the whole sample received no reintegration package. We applied the absolute standardized mean difference (ASMD) balance metric as the stopping rule in twang. Weights were assigned by twang to individuals in order to achieve maximum balance across the set of observed covariates in the propensity score model. A given individual's weight is the inverse probability of their being in the treatment group they were in. After this weighting, the covariate distributions in all three groups are more similar to that in the original full sample. The calculated weights were then incorporated into the final outcome models (below).
Measures of effectiveness of weighting procedures
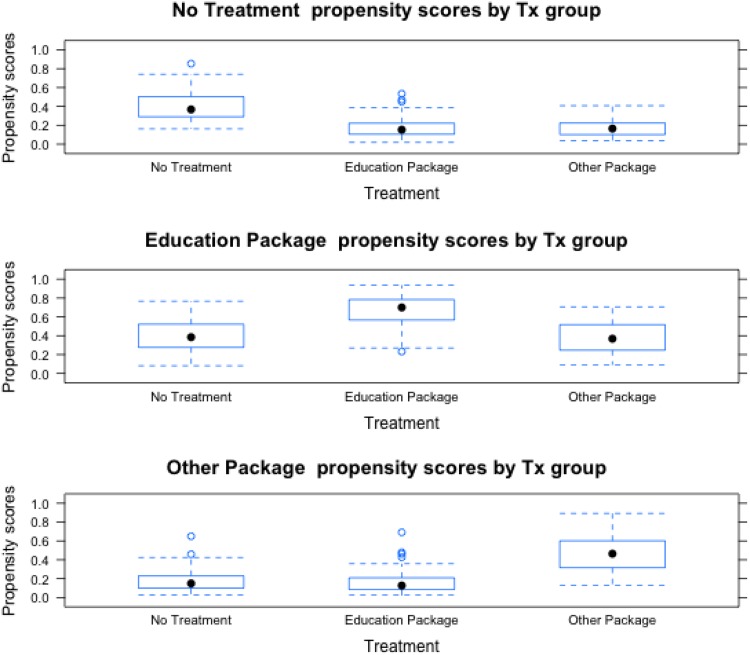
In order to evaluate the effectiveness of the weighting procedures, we examined the covariate balance in the weighted treatment groups. ASMDs were used to evaluate the similarity of the treatment groups. Both numerical and visual inspection (see Fig. 1 and Table 1) were used to assess covariate balance, with standardized mean differences below 0.25 indicating good balance (Rubin, 2001; Stuart, 2010).
Fig. 1.
Boxplot illustrating the spread of propensity scores by treatment group for receiving each treatment (i.e. no treatment, education package, and other package). The filled black circles indicate the median propensity score in each treatment group. As the plot demonstrates, there was substantial overlap in the total spread of propensity scores, but the central tendency differed by treatment group.
Estimation of treatment effects
Following weighting procedures (above), treatment effects were estimated using a doubly robust linear regression model with the outcome predicted by treatment group and covariates and fit using the weights defined above.
Results
Child soldiers in each treatment group differed from comparison child soldiers in other treatment groups (including the no treatment group) on key measured pre-treatment variables. Those receiving the ERPs were less likely to be female or from Dalit/Nepali castes and more likely to be younger than those in the other treatment groups (see Table 1). The three groups were generally comparable on measures of traumatic events and all the three pre-treatment clinical scales (i.e. DSRS, CPSS, and CFI). The application of propensity score weighting addressed these imbalances in the distributions of baseline covariates. Figure 1 illustrates the distribution of propensity scores for each treatment group. The figure demonstrates moderate overlap in the propensity scores between treatment groups.
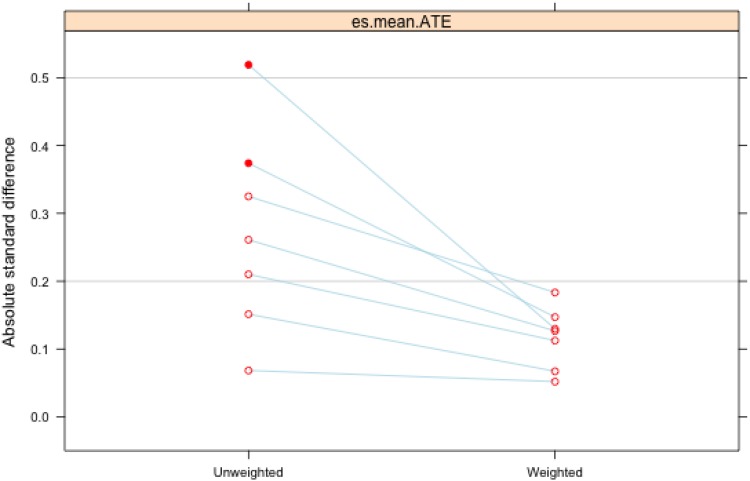
Table 1 displays the means and maximum ASMDs of the covariates of interest before and after weighting. As indicated in the columns in the right side of the table, maximum ASMDs were reduced to less than 0.20 for all covariates of interest after weighting, indicating good balance among the observed covariates. Figure 2 graphically displays the change in maximum ASMDs before and after weighting, again indicating that weighting resulted in a substantial improvement in balance, especially for the variables with highest standardized mean differences prior to weighting.
Fig. 2.
Plot of the maximum absolute standardized mean difference (ASMD) of covariates. Points on the left (‘Unweighted’) represent maximum ASMD (across the three treatment groups) prior to weighting and are connected by lines to the corresponding value of the same covariate's maximum ASMD following weighting on the right (‘Weighted’). Values less than 0.2 indicate adequate balance between treatment and control groups.
Estimated treatment effects
The estimated treatment effect of the ERP on depression compared with no treatment (after adjusting for age, sex, caste, traumatic events, and all the three baseline scale scores) was a non-significant reduction in DSRS symptom score by 0.59 (95% CI −1.97 to 0.79) (Table 2). The ERP was associated with a non-significant increase of 1.15 (95% CI −1.55 to 3.86) in the CPSS score and a non-significant increase of 0.91 (95% CI −0.31 to 2.14) on the CFI.
Table 2.
Treatment effect estimates of ERP and ORPs (v. no treatment) on depression, PTSD, and function impairment
| Outcome measure | Education package v. no treatment adjusted treatment effect estimate (95% CI)* | ORP v. no treatment adjusted treatment effect estimate (95% CI)* |
|---|---|---|
| Change in DSRS | −0.59 (−1.97 to 0.79) | −0.60 (−2.16 to 0.96) |
| Change in CPSS | 1.15 (−1.55 to 3.86) | 0.66 (−2.24 to 3.57) |
| Change in CFI | 0.91 (−0.31 to 2.14) | 1.05 (−0.71 to 2.80) |
ERP, education reintegration package; ORPs, other reintegration packages; DSRS, depression self-rating scale; CPSS, child PTSD symptom scale; CFI, child functional impairment scale.
* All multivariate regressions adjusted for age, sex, caste, traumatic events, baseline CPSS score, baseline DSRS score, and baseline CFI score.
The estimated treatment effect of the ORPs on depression compared with no treatment (after adjusting for age, sex, caste, traumatic events, and all the three baseline scale scores) was a non-significant reduction in DSRS symptom score by 0.60 (95% CI −2.16 to 0.96). The ORPs were associated with a non-significant increase of 0.66 (95% CI −2.24 to 3.57) in the CPSS score and a non-significant increase of 1.05 (95% CI −0.71 to 2.80) on the CFI.
Discussion
In the context of demobilizing and reintegrating former child soldiers into their home communities immediately after war, it was not considered ethical to randomize children to a waitlist condition. Moreover, children were given the option to select the type of reintegration package that they wanted, thus it was also not appropriate to randomize them to a package not of their choosing. Therefore, in this context it was not possible to conduct an RCT of the effects of reintegration programs. Instead, propensity score weighting was used as a technique to compare the effect of reintegration packages v. no treatment. We did not find evidence of significant effects on depression, PTSD, or functional impairment for the evaluated reintegration packages compared with no treatment. The findings suggest that compared with no reintegration package, ERPs or ORPs do not result in different outcomes in terms of depression, PTSD, and functional impairment when reintegration packages are conducted in the context of broader community-wide psychosocial support programs (see Kohrt et al. (2015)).
We had hypothesized that education would have been the most beneficial package from a MHPS perspective given outcomes of mixed-methods research that pointed towards the desire of most former children to return to school and cross-sectional associations between education attainment and MHPS outcomes (Morley & Kohrt, 2013). Nearly, half (46%) of eligible participants did not elect to enroll in the education package. Uptake was low among older children who may not have returned to school because of age differences with potential classmates (e.g. returning to school at age 16–17 years with classmates in the 12–13 year age range). Uptake was also particularly low among females and members of Dalit/Nepali castes, which is to be expected given historic trends creating barriers for girls and Dalit/Nepali castes to participate in school. These observations raise some questions about the appropriateness of child-driven selection processes. Some children, especially girls and Dalit/Nepali castes, may not have selected education because of anticipated barriers and discrimination. In such cases, it may have been helpful to explore reasons why the former child soldiers selected certain reintegration packages and then address potential barriers to participation in some packages. For example, future studies would benefit from evaluating parents’ perceived value of education as a determinant of uptake of education packages.
An important issue to consider is that our outcomes for this analysis were limited to depression, PTSD, and function impairment. The benefits of different reintegration programs on other life domains such as employment, economic security, physical health, and social status were not evaluated. There may be differential impact on these outcomes based on type of package received. Moreover, this analysis is limited to the 12-month period during which former child soldiers were receiving services. The longer-term difference in outcomes may have varied based on type of reintegration package, but such differences may not have been observable after only 1 year.
Regarding the statistical approach, a key limitation of the PSMs employed in this analysis is that adjustments could only be made for observed confounders. Thus, there may still be bias due to unobserved confounding. Omitting a key (unobserved) covariate can result in confounding if that characteristic was related to both treatment selection and the outcome(s). For example, in our study parents’ perceived value in education may have affected both treatment assignment (i.e. receipt of education package) and the outcomes of interest. Of note, in addition to balancing the distribution of observed covariates, PSMs may also partially address differences in the distribution of unobserved covariates, at least those correlated with the observed covariates (Stuart, 2010).
Our study was characterized by a relatively small sample size, which reduced statistical power to detect small but true differences in outcomes between treatment groups (i.e. Type II error). A larger study may have been better able to detect true differences between treatment options. That said, the magnitude of the changes observed in this study were very small, suggesting that clinical significant improvement may not be observed even with larger sample sizes. Finally, we note that the use of propensity scores in small samples is a relatively underdeveloped topic and deserves further study.
Conclusion
Alternative approaches to evaluating interventions in humanitarian crises are needed when RCTs are not possible for ethical, logistical, or other feasibility reasons. Propensity scoring weighting is one analytic approach that can be used when relatively large samples are available and there is variation in the type of services received. The technique is only as helpful as the degree to which potential confounders are also recorded. Therefore, if propensity score weighting is a planned analytic approach, then ideally this should be considered at the design stage to assure that a broad range of confounders are assessed. When working with children, potential confounders related to parents and caregivers also should be assessed whenever possible. In the context of this study with child soldiers in Nepal, we were able to demonstrate comparable outcomes for ERPs v. other types of services in the context of a broader community-wide psychosocial intervention. Future research is needed to evaluate long-term outcomes of different packages on mental health and psychosocial well-being, as well as the impact in other key domains of life.
Acknowledgements
The authors thank the TPO-Nepal staff involved in the intervention development including Rohit Karki, Nabin Lamichhane, Rajesh Jha, Mark Jordans, Wietse Tol, and Em Perera. Thanks to Anvita Bhardwaj for her assistance with manuscript preparation.
Financial support
UNICEF Nepal supported Transcultural Psychosocial Organization (TPO) Nepal to conduct this research. The first author (B. A. K.) was supported by the National Institute of Mental Health (NIMH) F31 MH075584.
Declaration of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The study protocol was approved by the Institutional Review Board of Emory University, Atlanta, USA.
References
- Adhikari A (2014). The Bullet and the Ballot Box: The Story of Nepal's Maoist Revolution. Verso Books: Kathmandu, Nepal. [Google Scholar]
- Adhikari RP, Kohrt BA, Luitel NP, Upadhaya N, Gurung D, Jordans MJD (2014). Protective and risk factors of psychosocial wellbeing related to the reintegration of former child soldiers in Nepal. Intervention: Journal of Mental Health and Psychosocial Support in Conflict Affected Areas 12, 367–378. [Google Scholar]
- Allden K, Jones L, Weissbecker I, Wessells M, Bolton P, Betancourt TS, Hijazi Z, Galappatti A, Yamout R, Patel P, Sumathipala A (2009). Mental health and psychosocial support in crisis and conflict: report of the mental health working group. Prehospital & Disaster Medicine 24 (Suppl. 2), s217–s227. [DOI] [PubMed] [Google Scholar]
- Annan J, Brier M, Aryemo F (2009). From ‘rebel’ to ‘returnee’ daily life and reintegration for young soldiers in Northern Uganda. Journal of Adolescent Research 24, 639–667. doi: 10.1177/0743558409350499. [DOI] [Google Scholar]
- Betancourt TS, Borisova I, Williams TP, Meyers-Ohki SE, Rubin-Smith JE, Annan J, Kohrt BA (2013). Research review: psychosocial adjustment and mental health in former child soldiers – a systematic review of the literature and recommendations for future research. Journal of Child Psychology and Psychiatry 54, 17–36. doi: 10.1111/j.1469-7610.2012.02620.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, Borisova II, de la Soudiere M, Williamson J (2011). Sierra Leone's child soldiers: war exposures and mental health problems by gender. Journal of Adolescent Health 49, 21–28. doi: 10.1016/j.jadohealth.2010.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, Khan KT (2008a). The mental health of children affected by armed conflict: protective processes and pathways to resilience. International Review of Psychiatry 20, 317–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, Williams T (2008b). Building an evidence base on mental health interventions for children affected by armed conflict. Intervention: International Journal of Mental Health, Psychosocial Work & Counselling in Areas of Armed Conflict 6, 39–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birleson P (1981). The validity of depressive disorder in childhood and the development of a self-rating scale: a research report. Journal of Child Psychology and Psychiatry 22, 73–88. [DOI] [PubMed] [Google Scholar]
- Blattman C, Annan J (2010). The consequences of child soldiering. Review of Economics and Statistics 92, 882–898. doi: 10.1162/REST_a_00036. [DOI] [Google Scholar]
- Bracken P, Petty C (1998). Rethinking the Trauma of War. Free Association Books: New York. [Google Scholar]
- Bracken PJ, Giller JE, Ssekiwanuka JK (1996). The rehabilitation of child soldiers: defining needs and appropriate responses. Medicine, Conflict & Survival 12, 114–125. [DOI] [PubMed] [Google Scholar]
- Burgette L, Griffin BA, McCaffrey D (2014). Propensity scores for multiple treatments: a tutorial for the mnps function in the twang package. RAND Corporation: Santa Monica, CA. [Google Scholar]
- Dyregrov A, Gupta L, Gjestad R, Raundalen M (2002). Is the culture always right? Traumatology 8, 135–145. [Google Scholar]
- Ertl V, Pfeiffer A, Schauer E, Elbert T, Neuner F (2011). Community-implemented trauma therapy for former child soldiers in Northern Uganda: a randomized controlled trial. JAMA – Journal of the American Medical Association 306, 503–512. [DOI] [PubMed] [Google Scholar]
- Foa EB, Johnson KM, Feeny NC, Treadwell KR (2001). The child PTSD symptom scale: a preliminary examination of its psychometric properties. Journal of Clinical Child Psychology 30, 376–384. doi: 10.1207/s15374424jccp3003_9. [DOI] [PubMed] [Google Scholar]
- Gilligan MJ, Mvukiyehe EN, Samii C (2013). Reintegrating rebels into civilian life: quasi-experimental evidence from Burundi. Journal of Conflict Resolution 57, 598–626. doi: 10.1177/0022002712448908. [DOI] [Google Scholar]
- Honaker J, King G, Blackwell M (2011). Amelia II: a program for missing data. Journal of Statistical Software 45, 1–47. [Google Scholar]
- Human Rights Watch (2007). Children in the Ranks: The Maoists’ Use of Child Soldiers in Nepal. Human Rights Watch: Kathmandu, Nepal, pp. 74. [Google Scholar]
- Humphreys M, Weinstein JM (2007). Demobilization and reintegration. Journal of Conflict Resolution 51, 531–567. doi: 10.1177/0022002707302790. [DOI] [Google Scholar]
- IASC (2007). Guidelines on Mental Health and Psychosocial Support in Emergency Settings. Inter-Agency Standing Committee: Geneva. [DOI] [PubMed] [Google Scholar]
- INSEC (2008). Fact sheet: number of victims killed by state and Maoist in connection with the ‘People's War’ (12 February 1996–31 December 2006) 1 April 2009. http://www.inseconline.org/.
- Isanaka S, Roederer T, Djibo A, Luquero FJ, Nombela N, Guerin PJ, Grais RF (2010). Reducing wasting in young children with preventive supplementation: a cohort study in Niger. Pediatrics 126, e442–e450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordans MJD, Komproe IH, Tol WA, Ndayisaba A, Nisabwe T, Kohrt BA (2012). Reintegration of child soldiers in Burundi: a tracer study. BMC Public Health 12, doi: 10.1186/1471-2458-12-905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordans MJD, Tol WA, Komproe IH, De Jong JTVM (2009). Systematic review of evidence and treatment approaches: psychosocial and mental health care for children in war. Child and Adolescent Mental Health 14, 2–14. [Google Scholar]
- Kohrt BA (2009). Vulnerable social groups in post-conflict settings: a mixed-methods policy analysis and epidemiology study of caste and psychological morbidity in Nepal. Intervention: International Journal of Mental Health, Psychosocial Work & Counselling in Areas of Armed Conflict 7, 239–264. [Google Scholar]
- Kohrt BA, Jordans MJD, Koirala S, Worthman CM (2015). Designing mental health interventions informed by child development and human biology theory: a social ecology intervention for child soldiers in Nepal. American Journal of Human Biology 27, 27–40. doi: 10.1002/ajhb.22651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Jordans MJD, Tol WA, Luitel NP, Maharjan SM, Upadhaya N (2011). Validation of cross-cultural child mental health and psychosocial research instruments: adapting the depression self-rating scale and child PTSD symptom scale in Nepal. BMC Psychiatry 11, 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Jordans MJD, Tol WA, Perera E, Karki R, Koirala S, Upadhaya N (2010a). Social ecology of child soldiers: child, family, and community determinants of mental health, psychosocial well-being, and reintegration in Nepal. Transcultural Psychiatry 47, 727–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Jordans MJD, Tol WA, Speckman RA, Maharjan SM, Worthman CM, Komproe IH (2008). Comparison of mental health between former child soldiers and children never conscripted by armed groups in Nepal. JAMA – Journal of the American Medical Association 300, 691–702. doi: 10.1001/jama.300.6.691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Perera E, Jordans MJD, Koirala S, Karki R, Karki R, Shrestha P, Tol W, Upadhaya N (2010b). Psychosocial Support Model for Children Associated with Armed Forces and Armed Groups in Nepal. Transcultural Psychosocial Organization-Nepal/UNICEF: Kathmandu, Nepal. [Google Scholar]
- Kohrt BA, Speckman RA, Kunz RD, Baldwin JL, Upadhaya N, Acharya NR, Sharma VD, Nepal MK, Worthman CM (2009). Culture in psychiatric epidemiology: using ethnography and multiple mediator models to assess the relationship of caste with depression and anxiety in Nepal. Annals of Human Biology 36, 261–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Tol WA, Pettigrew J, Karki R (2010c). Children and revolution: the mental health and psychosocial wellbeing of child soldiers in Nepal's Maoist army In The War Machine and Global Health (ed. Singer M. and Hodge G. D.), pp. 89–116. Altamira Press, Rowan & Littlefield Publishers, Inc.: Lanham, MD. [Google Scholar]
- McCaffrey DF, Griffin BA, Almirall D, Slaughter ME, Ramchand R, Burgette LF (2013). A tutorial on propensity score estimation for multiple treatments using generalized boosted models. Statistics in Medicine 32, 3388–3414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohapatra S, Joseph G, Ratha D (2012). Remittances and natural disasters: ex-post response and contribution to ex-ante preparedness. Environment, Development and Sustainability 14, 365–387. [Google Scholar]
- Morley CA, Kohrt BA (2013). Impact of peer support on PTSD, hope, and functional impairment: a mixed-methods study of child soldiers in Nepal. Journal of Aggression, Maltreatment & Trauma 22, 714–734. doi: 10.1080/10926771.2013.813882. [DOI] [Google Scholar]
- Okello J, Onen T, Musis S (2007). Psychiatric disorders among war-abducted and non-abducted adolescents in Gulu district, Uganda: a comparative study. African Journal of Psychiatry 10, 225–231. [DOI] [PubMed] [Google Scholar]
- Rosenbaum PR, Rubin DB (1985). Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. The American Statistician 39, 33–38. [Google Scholar]
- Rubin D (2001). Using propensity scores to help design observational studies: application to the tobacco litigation. Health Services and Outcomes Research Methodology 2, 169–188. doi: 10.1023/A:1020363010465. [DOI] [Google Scholar]
- Singh S (2004). Post-traumatic stress in former Ugandan child soldiers. The Lancet 363 (9421), 1648. [DOI] [PubMed] [Google Scholar]
- Strandow D (2014). Fighting for Aid: Foreign Funding and Civil Conflict Intensity, PhD Dissertation, Uppsala Universitet, Department of Peace and Conflict Research. [Google Scholar]
- Stuart EA (2010). Matching methods for causal inference: a review and a look forward. Statistical Science: A Review Journal of the Institute of Mathematical Statistics 25, 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tol WA, Barbui C, Galappatti A, Silove D, Betancourt TS, Souza R, Golaz A, van Ommeren M (2011). Mental health and psychosocial support in humanitarian settings: linking practice and research. The Lancet 378, 1581–1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNDP (2013). Human Development Report 2013: The Rise of the South: Human Progress in a Diverse World. United Nations Development Programme: New York, pp. 216. [Google Scholar]
- UNICEF (2007). Paris Principles New York. [Google Scholar]
- United Nations (2006). Report of the Secretary-General on Children and Armed Conflict in Nepal. United Nations Security Council: Geneva, pp. 18. [Google Scholar]
- United Nations (2014). Children and Armed Conflict, A/68/878-S/2014/339. General Assembly Security Council: Geneva. [Google Scholar]
- Whelpton J (2005). A History of Nepal. Cambridge University Press: Cambridge, New York. [Google Scholar]
- Williamson J (2006). The disarmament, demobilization and reintegration of child soldiers: social and psychological transformation in Sierra Leone. Intervention: International Journal of Mental Health, Psychosocial Work & Counselling in Areas of Armed Conflict 4, 185–205. [Google Scholar]