Abstract
Introduction:
Injection drug use (IDU) is intricately linked to preventive aspects for human immunodeficiency virus from a public health perspective. No large-scale data are yet available for injectable drug use among children and adolescents in India, apart from few anecdotal reports.
Aims and Methods:
The present paper reports on the profile and substance use pattern of 509 child IDU users, among a total sample of over 4000 children using substances across 100 sites from 27 states and 2 UTs in India. It was undertaken in 2012–2013 by the National Commission of Protection for Child Rights in collaboration with the National Drug Dependence Treatment Centre, All India Institute of Medical Sciences, New Delhi. For inclusion, participants had to be 18 years or less, should have used at least one other substance besides tobacco in the last 1 year, and should be living at home/street, in or out of school. Data were gathered using a 95-item semi-structured questionnaire.
Results:
A large proportion of ever users of IDU also reported use in the past year (96.5%) and past month (92.7%). Apart from IDU, tobacco, alcohol, cannabis, and pharmaceutical opioids were the most common substances of abuse in order of frequency. There was an interval of about 3 years from the initiation of tobacco to the initiation of IDU. Average age of onset for IDU was a year lesser in males than female users. The street children initiated IDU earlier than out-of-school and schoolgoing children. No quit attempt was made by more than half of the children. More than 40% had frequent familial conflicts, more than half had a familial history of substance use, and three-fourths had drug-using peers.
Conclusion:
The paper highlights the profile and pattern of children and adolescents using IDU across many parts of India, dispelling the myth that IDU is largely an adult phenomenon in India. There is a clear need to promote different harm reduction and preventive strategies across the “hard-to-reach” younger age groups using injecting drugs.
Key words: Adolescents, children, India, injection drug use, substance use
INTRODUCTION
Globally, the number of people who inject drugs has been estimated to be nearly 12.7 million, which corresponds to a prevalence of 0.27% (0.19%–0.48%) among those aged 15–64 years.[1] In India, an estimated number of 177,000 adults are injection drug users (IDUs), defined as those with ever use of injecting drugs in their lifetime.[2] The onset of IDU typically occurs in adulthood after 20 years of age, with a gradual progression from licit, gateway drugs in early adolescence to illicit substances later on in course.[3,4] The data from the National Household Survey, the only available nationwide survey for the extent and pattern of substance use in India, suggest that about 0.1% of the male population (aged 12–60 years) reported ever injecting any illicit drug.[5] Most IDUs were aged around 20 years of age and had used another substance prior to starting to inject.
No large-scale data are yet available for injectable drug use among children and adolescents in India, apart from few anecdotal reports. Further, not much is known about the pattern and correlates of IDU in children and adolescents in India.
IDU is one of the main driving forces behind the human immunodeficiency virus (HIV) epidemic, linking it intricately to preventive aspects for HIV from a public health perspective. The national HIV prevalence for IDUs is 7.14%.[2] However, as IDU is not usually considered to be a widespread or significant phenomenon in younger age groups, consequently the young population is underrepresented in HIV behavioral surveillance. Recent international studies found that the injecting drug use may vary from <1% of adolescents in Australia to as high as 2.5% in the US male adolescents.[6,7] Information on factors associated with adolescent-onset IDU would help initiate and percolate the existent preventive, treatment, and control strategies for IDU and prevention of HIV to child/adolescent population in India.
In view of the above gaps in knowledge, the National Commission for Protection of Child Rights took the initiative for a nationwide study in more than 100 cities/towns across India in collaboration with the National Drug Dependence Treatment Centre, All India Institute of Medical Sciences, New Delhi.[8] It examined the pattern of substance use and profile of children using substances (schoolgoing, out of school, and street children) in a sample of more than 4000 children using substances, which also tapped children using injectable drugs. The present paper reports on IDU among this sample of children and adolescents across India.
METHODS
It was a cross-sectional study, carried out in 2012–2013, across sites from 27 states and 2 UTs in the country.[9] Rest one state and 5 UTs were not covered due to operational reasons. The nongovernmental organizations (NGOs) funded by the Ministry of Social Justice and Empowerment were responsible for the collection of data monitored by the Regional Resource and Training Centres. The specific NGOs in the town/city were identified in unison with the National Institute of Social Defence and Federation of Indian NGOs in drug abuse prevention. Finally, a total of 102 NGOs participated.
Considering the study time frame, it was planned that each NGO would collect data from one or more sites on a convenience sample of thirty children who fulfilled the inclusion and exclusion criteria. As there were two types of NGOs collecting data (NGOs working with street children and NGOs working with substance users), to avoid overlap in data collection, recruitment settings were specified. NGOs working in the area of substance use used “snowball technique” to identify children, conducting community awareness programs regarding substance use and interviewing children of substance users who came to their drug treatment center and shops visited to buy substances besides community where they lived. On the other hand, NGOs working for the street children recruited majority sample from railway station, traffic signals, and those coming to them for services/activities.
To be eligible, participants had to be 18 years or less and should have used at least one other substance besides tobacco in the past 1 year. They were not included in the study if they reported use of only tobacco in the past 1 year, showed unwillingness for inclusion in the study, or were unable to comprehend and provide information.
The children were interviewed by specifically identified and trained NGO staff. All interviews were conducted anonymously and no personal identifiers were recorded. Each interview commenced with prior verbal consent of guardian/parent/NGO staff and assent. An interviewer-administered 95-item questionnaire was developed based on the variables of a previous multinational study, which covered these sections (1) demographic, (2) family and peer related, (3) stress, physical, and psychological health, (4) substance use, and (5) legal issues. No incentive was provided to the children to participate in the study.
Statistical analysis
Data analysis was performed using licensed SPSS software (IBM SPSS Statistics for Windows, Version 21.0, Armonk, New York, USA)[9] on data pertaining to children/adolescents who reported ever use of injection. Descriptive statistics are being presented.
RESULTS
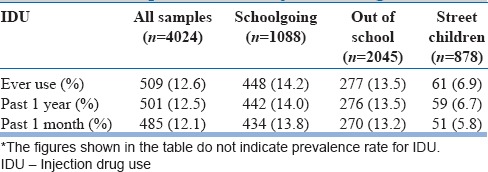
Of the total sample of children using drugs (n = 4024), 12.6% (n = 509) reported ever injection use [Table 1]. A large proportion of them reported use in the past 1 year (96.5%) as well as in the past 1 month (92.7%).
Table 1.
Proportion of the study sample with self-reported use of injection drugs
Profile
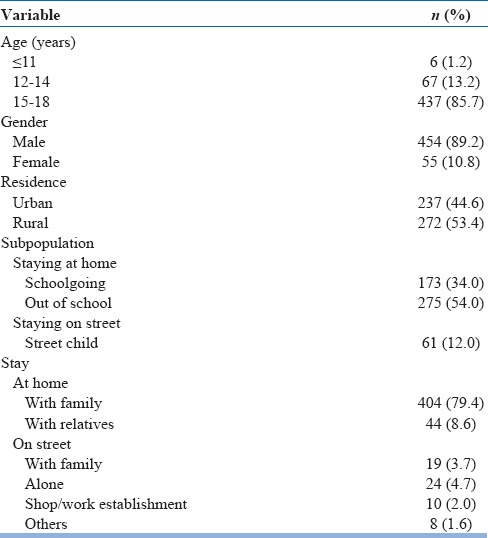
The sociodemographic profile of the sample of IDUs is shown in Table 2.
Table 2.
Sociodemographic profile of children with injection drug use (n=509)
Pattern of substance use
The average number of days per month for which the sample reported the use of IDUs was 16 days/month. The pattern of other substance use among this sample of IDUs is shown in Table 3. Table 4 shows the age of initiation for various substances in the sample of children/adolescents with IDUs. It was noteworthy that the street children initiated injection use at an early age (13.98 years) compared to out-of-school (15.19 years) and schoolgoing children (15.56 years). The male sample initiated injection use at an average at 15.03 ± 1.46 years, almost a year earlier compared to females (16.00 ± 1.20 years). Those belonging to rural areas started injection use at 15.09 ± 1.14 years and those in urban areas at 15.12 ± 1.70 years.
Table 3.
Pattern of other substance use among a sample of child/adolescent injection drug users (n=509)
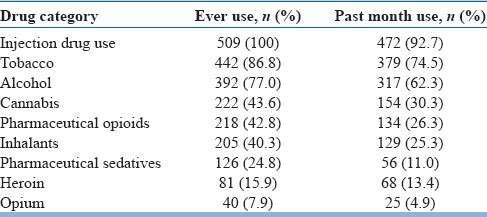
Table 4.
Age of initiation for various substances in a sample of child/adolescent injection drug users (n=509)
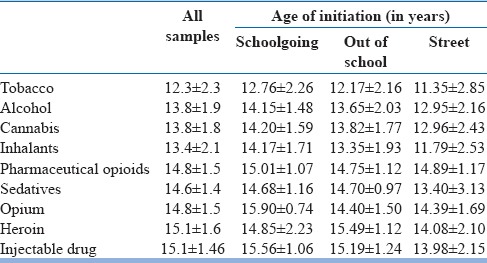
Regarding average length of time from the first drug use to initiation of injection, there was an interval of about 3 years from the initiation of tobacco to the initiation of IDU (ranged between 2.63 years for street children and 3.02 years for out-of-school children).
Risk factors and complications associated with injection drug users
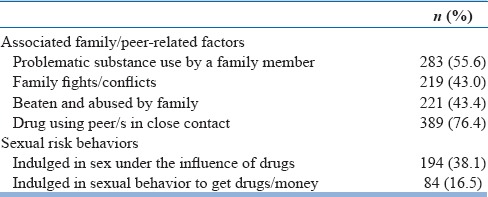
Table 5 shows the familial and peer-related factors associated with substance use in the study sample. Problematic substance use was present in more than half of the children, with more than 40% having frequent familial conflicts and abuse. A large proportion (76.4%) had regular contact with drug-using peers. A significant proportion of the sample engaged in risky sexual behaviors as shown in Table 5.
Table 5.
Factors associated with substance use in child/adolescent injection drug users (n=509)
Mental symptoms in the form of sadness and anxiety associated with substance use were reported by 59.5% of the IDUs and 66% reported in affirmative that the life is difficult and stressful.
Help seeking
Only 91 (17.9%) children reported that they need help for quitting, while 171 (33.6%) reported that they have a problem, but can quit on their own, and rest 195 (38.3%) did not think that they have any problem requiring help. No quit attempt was made by 267 (52.5%) children, 15.5% attempted quitting more than 3 months back, 11.8% between 1 and 3 months back, and 18.3% attempted to quit less than a month back.
Regional patterns
Among the sample of children contacted in each state, an alarmingly high proportion of IDU children were from the state of Mizoram (89.4%) followed by the states of Rajasthan, Maharashtra, Meghalaya, Punjab, Chandigarh, Arunachal Pradesh, and Manipur (varying between 11% and 27%). The statewise sample of children contributed from each state and the proportion or subsample of children/adolescents using IDU is provided in Box 1.
Box 1.
Statewise sample of children with injection drug use in the study

DISCUSSION
The present paper reports on IDU among children using substances from a large-scale study conducted across 100 cities in various states and regions of India. Among the sample recruited for the study (n = 4024), a high proportion (12.1%) reported current (1 month) use of injecting drugs and 12.6% reported ever injecting drugs. People who inject drugs are often described as “hard to reach” population and within this, the children and adolescents using IDUs are almost “invisible.”
To the best of our knowledge, this is the first study that has researched children using substances in a nationwide effort. Further, it included children from various settings: those living at home (schoolgoing: 34% and out of school: 54%) and those living on streets (12%), either alone/with families. Use of injections was reported by substance-using children across majority of states/UTs of India and not only restricted to the northeastern region.
It is important to emphasize at the beginning that the study did not aim to assess the prevalence rates of IDU in younger population across India, and consequently, the figures available from the study findings should not be interpreted as the prevalence figures. Rather than focusing on prevalence, we employed alternate sampling methods (e.g., snowball technique) which would help to tap into an otherwise “harder-to-reach” subgroup population to document their profile and pattern of substance use.
IDU clearly places individuals at a high risk of acquiring HIV and hepatitis C virus and of experiencing other harms such as overdose. Injecting drug use among children can be a serious public health problem for any country and underscores the urgent need to intervene and protect this vulnerable group from falling prey to HIV.[10,11] The sample had the onset of IDU at an average of 1–1.5 years before the current assessment. It appears that almost all children who initiated IDU continued to use it. Further, the average number of days per month for which the sample reported the use of IDUs was 16 days per month, pointing to a frequent, risky pattern of use. It has been seen from various international studies that risk of becoming HIV infected is especially high during the period immediately following the initiation of injection (within the first 1–2 years). There is, thus, only a brief “window of opportunity” to intervene and prevent infections among this child population.[11,12]
IDU was more commonly reported by those living at home compared to street sample. This finding is most likely due to sampling bias toward the child substance users living at home. Those using harder substances are likely to be the “known substance users” in their neighborhood, and probably, had more chances to be included in the study by the NGO working in that area. In contrast, those using licit substances at homes may be able to hide their substance use and had less likelihood to be contacted for the study inclusion. This may have also led to a higher proportion of IDUs in this sample. Street sample in this study more often preferred the use of inhalants, which could be because they are easily available, accessible, and cheaper. It is in consonance with previous studies on street children in New Delhi and Bengaluru.[13,14] It is also to be noted that among those street children who had IDU, they initiated injection use more than a year earlier (14.0 ± 2.0 years) compared to those who were schoolgoing (15.5 ± 1.1 years) and out of school (15.26 ± 1.3 years), pointing to a subsample of street children in whom IDU makes an earlier onset. Regarding average time from the first drug use to initiation of injections, there was an interval of about 3 years from the initiation of tobacco to the initiation of IDU in this sample, which is a potential time for preventive interventions for IDU initiation.[15]
Family factors such as parental substance use, physical abuse, and poor quality of relationship between parents and children is a known risk factor for substance use among children as seen in international studies.[16] Presence of substance use in another family member may act through a variety of mechanisms such as by increasing genetic risk or by negative role modeling to increase a child's susceptibility to substance use. Childhood sexual abuse places a higher risk for initiating injection use among substance users.[17] Further, substance use in a family member often leads to familial quarrels or discord, poor supervision of the children, lack of parental involvement in child's activities, and may pose several other environmental risk factors for the child, for example, easy availability of substance. Many of these well-established risk factors for child substance use are also prominent in the present study sample. Nearly 56% of the sample also reported the presence of substance use in a family member and 43% reported frequent familial quarrels and being beaten/abused by family members. Poor family bonding and attachment to parents has been linked to increase in the likelihood of substance use in children, while close emotional ties with parents is a protective factor for substance use.[16,18]
The most powerful of the social influences for substance use at a younger age is that of peer influences. The association with the peers who approve the use of substances or use substances themselves predisposes a child to substance use.[16,19] In this study, more than 76% of IDUs had a close contact with friends who use substances. From the perspective of prevention, it is important to impart the basic skills to children such as resisting peer pressure and being assertive to say “no” when offered substances by peers. An enhanced contact with the nonsubstance using friends is often recommended as part of the treatment process for the children using substances.
A significant proportion of the sample engaged in risky sexual behaviors, including sex in exchange for money/drugs. The presence of substance abuse in a child may facilitate, in some ways, the involvement in sexual behaviors, for example, impaired decision-making or disinhibition may occur under the influence of a substance, which may make a person more likely to indulge in sexual behaviors. As the study was cross-sectional, it might be difficult to comment about the directionality of the association. The association between early-onset substance use and involvement in sexual behaviors has been observed in previous studies.[20,21] Nearly 10% of the present sample of IDUs comprised female children/adolescents. In a previous Indian study on adult female IDUs, a significantly higher proportion of female IDUs were uneducated, unemployed, worked as sex workers, and switched to injecting drug use faster as compared with male IDUs.[22] These high-risk sexual behaviors represent an additional risk for developing and transmitting HIV. Injection substance use also has a possible link with mental health, as seen in literature including an association with suicide attempts.[23] Mental health needs of this subpopulation often remain neglected and may contribute to continuing substance use. In this sample, nearly 60% of children with IDU reported sadness/anxiety and a stressful life, pointing to a need to pay more attention to the associated psychological symptoms from a preventive and management perspective, as a risk factor or as a consequence of persistent substance use.
Nearly half of the children acknowledged that they have a problem with regard to substance use. No quit attempt was made by 52.5% children, but nearly 18% of the children attempted quitting less than a month back, and quit attempts were made at some point by half of the sample. Every IDU child should have suitable access to treatment and support. The tremendous benefits of provision of treatment services to children in short- and long-term justify the support, development, and investment in programatic responses. Protecting children from potential harms of IDU must be at the forefront of concerns when developing or strengthening and scaling national programs. During planning, it is of utmost importance to ensure that children who inject drugs are also covered under the gamut of services. In a systematic review, the peer-based behavior modification and addiction treatment interventions were found to be most effective in younger people to reduce the risk of initiation of injecting drugs.[15] It is crucial that the targeted intervention sites with IDUs should review their existing policies to include child population below 18 years of age for a diverse range of harm reduction services, which are currently limited to adult age groups. With emerging evidence that the age of initiation of IDU is low and/or decreasing, there is a need to reconsider these age restrictions for maximal benefit. Recently, after gaining more evidence for safety, buprenorphine substitution is now being offered to adolescent IDUs which is a welcome step.[24] Adopting a flexible approach would enable these services as a first point of contact with IDU children and possibly a link to connect them with drug treatment services.
Given the hidden nature of the IDU population, it is extremely challenging for service providers to identify and reach them for services. The study used a mix of recruitment methods which was successful to identify child IDUs in the current study. The similar approach can be used for enrollment for an intervention, which will allow for IDUs with different demographic characteristics and risk profiles to be enrolled for intervention as and when they are implemented.
The study findings counter the popular perceived belief that the injecting drug use problem was mainly concentrated among adult males and was limited to northeastern region only.[25,26] Although the worst-hit site appeared to be from Mizoram, this study was able to identify children who were currently injecting drugs from most other states and regions in India. Unlike past, the IDU in adult population too have spread outside northeastern region with emerging epidemics to southern and northern states.[27,28]
The study findings are subject to some limitations. The main focus of the study was on the pattern and correlates of children using substances, therefore information pertaining to some other details/factors specific to IDU behavior was not collected, including the circumstances around IDU initiation, sharing practices, and kinds of drugs injected. A previous Indian survey on adult IDUs found pharmaceutical opioids and heroin to be the most injected drugs,[29] which might be present in younger population too although these details were not specifically gathered in the present study. Second, the survey used a convenience sample and consequently nonrepresentative for the entire population. However, the present study did not aim to assess the prevalence rates of IDU in younger population, rather sampling methods which would facilitate penetration into this “hard-to-reach” and “invisible” population were employed in an effort to document the presence of IDU in children. Children were sampled through mixed methods and it was unknown how deep this approach penetrated the subpopulation at the study sites; it may be possible that who were not recruited had different characteristics to the study participants.
In future directions, there is a need for more comprehensive research among newly initiated young IDUs so that early intervention and prevention programs may be implemented. There is a need to target harm reduction messages for IDU to younger age group children who use substances. Strategies need to be devised specifically for young IDUs to reduce the impact of injecting drug use on the HIV epidemic in India, especially as adolescents may have lesser awareness about risks and may have a lower harm perception or higher risk-taking behaviors. Routine surveys should include the child and adolescent population, and more qualitative studies should be undertaken for better, in-depth understanding.
CONCLUSION
The paper highlights the profile and pattern of children and adolescents using IDU across many parts of India, dispelling the myth that IDU is largely an adult phenomenon in India. There is a clear need to promote different harm reduction and preventive strategies across the “hard to reach” younger age groups using injecting drugs.
Financial support and sponsorship
The National Commission for Protection of Child Rights (NCPCR), Govt of India, supported the larger, nation-wide survey 'Assessment of pattern, profile and correlates of substance use among children in India' (2013).
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.United Nations Office on Drugs and Crime, World Drug Report, 2014 (United Nations Publication, Sales No. E.14.XI.7) 2014. [Last accessed on 2015 Jul 15]. Available from: https://www.unodc.org/documents/wdr2014/World_Drug_Report_2014_web.pdf .
- 2.National AIDS Control Organization. HIV Sentinel Surveillance 2010-2011: A Technical Brief, Ministry of Health and Family Welfare, Government of India, New Delhi, India. 2012 [Google Scholar]
- 3.Cheng Y, Sherman SG, Srirat N, Vongchak T, Kawichai S, Jittiwutikarn J, et al. Risk factors associated with injection initiation among drug users in Northern Thailand. Harm Reduct J. 2006;3:10. doi: 10.1186/1477-7517-3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Solomon SS, Desai M, Srikrishnan AK, Thamburaj E, Vasudevan CK, Kumar MS, et al. The profile of injection drug users in Chennai, India: Identification of risk behaviours and implications for interventions. Subst Use Misuse. 2010;45:354–67. doi: 10.3109/10826080903452447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ray R. National Survey on Extent, Pattern and Trends of Drug Abuse in India. Ministry of Social Justice and Empowerment and United Nations Office on Drug and Crime Regional Office for South Asia. 2004 [Google Scholar]
- 6.Howard J, Ali H. Injecting drug use among young people in Pacific Island countries and territories: A review of the evidence. Drug Alcohol Rev. 2013;32:631–3. doi: 10.1111/dar.12071. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Youth Risk Behavior Surveys. 2013. [Last accessed on 2016 Mar 15]. Available from: http://www.apps.nccd.cdc.gov/youthonline/App/Default.aspx?SID=HS .
- 8.Tikoo VK, Dhawan A, Pattanayak R, Chopra A. Assessment of Pattern, Profile and Correlates of Substance Use Among Children in India. National Commission for Protection of Child Rights (NCPCR), New Delhi. 2013. [Last accessed on 2016 Sep 01]. Available from: http://www.ncpcr.gov.in/view_file.php?fid=17 .
- 9.Version 21.0. New York, USA: Armonk; 2012. Statistical Package for Social Sciences, IBM SPSS Statistics for Windows. [Google Scholar]
- 10.Beg M, Strathdee SA, Kazatchkine M. State of the art science addressing injecting drug use, HIV and harm reduction. Int J Drug Policy. 2015;26(Suppl 1):S1–4. doi: 10.1016/j.drugpo.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 11.Roy E, Boudreau JF, Boivin JF. Hepatitis C virus incidence among young street-involved IDUs in relation to injection experience. Drug Alcohol Depend. 2009;102:158–61. doi: 10.1016/j.drugalcdep.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 12.Garfein RS, Vlahov D, Galai N, Doherty MC, Nelson KE. Viral infections in short-term injection drug users: The prevalence of the hepatitis C, hepatitis B, human immunodeficiency, and human T-lymphotropic viruses. Am J Public Health. 1996;86:655–61. doi: 10.2105/ajph.86.5.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ray R, Dhawan A, Ambekar A, Yadav D, Chopra A. Inhalant Use Among Street Children in Delhi – A Situation Assessment. Developed under the Ministry of Health, Government of India and WHO Collaborative Programme. Report submitted to WHO, India. 2009 [Google Scholar]
- 14.Benegal V, Bhushan K, Seshadri S, Karott M. Drug Abuse among Street Children in Bangalore. A Project in Collaboration Between NIMHANS, Bangalore and the Bangalore Forum for Street and Working Children, Monograph Funded by CRY. 1998 [Google Scholar]
- 15.Werb D, Buxton J, Shoveller J, Richardson C, Rowell G, Wood E. Interventions to prevent the initiation of injection drug use: A systematic review. Drug Alcohol Depend. 2013;133:669–76. doi: 10.1016/j.drugalcdep.2013.08.017. [DOI] [PubMed] [Google Scholar]
- 16.Kilpatrick DG, Acierno R, Saunders B, Resnick HS, Best CL, Schnurr PP. Risk factors for adolescent substance abuse and dependence: Data from a national sample. J Consult Clin Psychol. 2000;68:19–30. doi: 10.1037//0022-006x.68.1.19. [DOI] [PubMed] [Google Scholar]
- 17.Hadland SE, Werb D, Kerr T, Fu E, Wang H, Montaner JS, et al. Childhood sexual abuse and risk for initiating injection drug use: A prospective cohort study. Prev Med. 2012;55:500–4. doi: 10.1016/j.ypmed.2012.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vakalahi HF. Adolescent substance use and family-based risk and protective factors: A literature review. J Drug Educ. 2001;31:29–46. doi: 10.2190/QP75-P9AR-NUVJ-FJCB. [DOI] [PubMed] [Google Scholar]
- 19.Rahimi-Movaghar A, Amin-Esmaeili M, Shadloo B, Noroozi A, Malekinejad M. Transition to injecting drug use in Iran: A systematic review of qualitative and quantitative evidence. Int J Drug Policy. 2015;26:808–19. doi: 10.1016/j.drugpo.2015.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mahanta J, Medhi GK, Paranjape RS, Roy N, Kohli A, Akoijam BS, et al. Injecting and sexual risk behaviours, sexually transmitted infections and HIV prevalence in injecting drug users in three states in India. AIDS. 2008;22(Suppl 5):S59–68. doi: 10.1097/01.aids.0000343764.62455.9e. [DOI] [PubMed] [Google Scholar]
- 21.Armstrong G, Nuken A, Medhi GK, Mahanta J, Humtsoe C, Lalmuanpuaii M, et al. Injecting drug use in Manipur and Nagaland, Northeast India: Injecting and sexual risk behaviours across age groups. Harm Reduct J. 2014;11:27. doi: 10.1186/1477-7517-11-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ambekar A, Rao R, Agrawal A, Goyal S, Mishra A, Kishore K, et al. Pattern of drug use and associated behaviors among female injecting drug users from Northeast India: A multi-centric, cross-sectional, comparative study. Subst Use Misuse. 2015;50:1332–40. doi: 10.3109/10826084.2015.1013130. [DOI] [PubMed] [Google Scholar]
- 23.Liu RT, Case BG, Spirito A. Injection drug use is associated with suicide attempts but not ideation or plans in a sample of adolescents with depressive symptoms. J Psychiatr Res. 2014;56:65–71. doi: 10.1016/j.jpsychires.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 24.Rao R, Agrawal A, Ambekar A. Opioid Substitution Therapy Under National AIDS Control Programme: Clinical Practice Guidelines for Treatment with Buprenorphine. Department of AIDS Control, Ministry of Health and Family Welfare, Government of India, New Delhi. 2014 [Google Scholar]
- 25.Medhi GK, Mahanta J, Adhikary R, Akoijam BS, Liegise B, Sarathy K, et al. Spatial distribution and characteristics of injecting drug users (IDU) in five Northeastern states of India. BMC Public Health. 2011;11:64. doi: 10.1186/1471-2458-11-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eicher AD, Crofts N, Benjamin S, Deutschmann P, Rodger AJ. A certain fate: Spread of HIV among young injecting drug users in Manipur, North-East India. AIDS Care. 2000;12:497–504. doi: 10.1080/09540120050123891. [DOI] [PubMed] [Google Scholar]
- 27.Ambekar A, Tripathi BM. Size Estimation of Injecting Drug Use in Punjab and Haryana. UNAIDS. 2008 [Google Scholar]
- 28.Kumar MS, Mudaliar S, Thyagarajan SP, Kumar S, Selvanayagam A, Daniels D. Rapid assessment and response to injecting drug use in Madras, South India. Int J Drug Policy. 2000;11:83–98. doi: 10.1016/s0955-3959(99)00057-2. [DOI] [PubMed] [Google Scholar]
- 29.Ambekar A, Rao R, Mishra AK, Agrawal A. Type of opioids injected: Does it matter? A multicentric cross-sectional study of people who inject drugs. Drug Alcohol Rev. 2015;34:97–104. doi: 10.1111/dar.12208. [DOI] [PubMed] [Google Scholar]


