Abstract
Background
Childhood obesity prevalence remains high and racial/ethnic disparities may be widening. Studies have examined the role of health behavioral differences. Less is known regarding neighborhood and built environment mediators of disparities. The objective of this study is to examine the extent to which racial/ethnic disparities in elevated child body mass index (BMI) are explained by neighborhood socioeconomic status (SES) and built environment.
Methods
We collected and analyzed race/ethnicity, BMI, and geocoded address from electronic health records of 44,810 children 4 to 18 years-old seen at 14 Massachusetts pediatric practices in 2011–2012. Main outcomes were BMI z-score and BMI z-score change over time. We used multivariable linear regression to examine associations between race/ethnicity and BMI z-score outcomes, sequentially adjusting for neighborhood SES and the food and physical activity environment.
Results
Among 44,810 children, 13.3% were black, 5.7% Hispanic, and 65.2% white. Compared to white children, BMI z-scores were higher among black (0.43 units [95% CI: 0.40–0.45]) and Hispanic (0.38 [0.34–0.42]) children; black (0.06 [0.04–0.08]), but not Hispanic, children also had greater increases in BMI z-score over time. Adjusting for neighborhood SES substantially attenuated BMI z-score differences among black (0.30 [0.27–0.34]) and Hispanic children (0.28 [0.23–0.32]), while adjustment for food and physical activity environments attenuated the differences but to a lesser extent than neighborhood SES.
Conclusions
Neighborhood SES and the built environment may be important drivers of childhood obesity disparities. To accelerate progress in reducing obesity disparities, interventions must be tailored to the neighborhood contexts in which families live.
Keywords: childhood obesity, BMI, disparities, built environment, Socioeconomic Risk Factors, Electronic Health Records
INTRODUCTION
Childhood obesity rates appear to have reached a plateau in the U.S. and may be decreasing among white children and those of higher socioeconomic status (SES). Yet, overall childhood obesity prevalence remains high, and despite decades of research to reduce disparities and improve health outcomes among children at highest risk, substantial racial/ethnic and socioeconomic disparities persist for child obesity (Centers for Disease Control and Prevention (CDC), 2013; Ogden et al., 2012; Rokholm et al., 2010; Taveras et al., 2010; Wang and Beydoun, 2007; Wen et al., 2012). The role of individual health behaviors in observed disparities has been examined in prior studies revealing racial/ethnic and socioeconomic differences in obesity risk factors starting in early childhood, with higher prevalence of obesogenic risk factors such as higher sugar-sweetened beverage intake among children from racial/ethnic minority groups compared to their white counterparts (Flores and Committee On Pediatric Research, 2010; Taveras et al., 2010). In considering childhood obesity disparities, less is known regarding the role of the neighborhood context in which decisions are being made related to health behaviors and in which behavior change is expected to occur.
Geographic information systems (GIS) data can provide neighborhood-level information on access to and distribution of food establishments, including supermarkets and fast food restaurants, as well as recreational spaces and neighborhood walkability that might influence decision-making regarding food choices and physical activity options (Matthews et al., 2009). Studies have demonstrated associations of such factors with obesity and weight-related behaviors such as physical activity among children and adolescents (Bell et al., 2008; Ding et al., 2011; Duncan et al., 2014; Feng et al., 2010; Fiechtner et al., 2015; Galvez et al., 2009; Gordon-Larsen et al., 2006; Lawman and Wilson, 2012; Liu et al., 2007; Papas et al., 2007; Powell et al., 2007). Prior analyses have demonstrated that environmental features promoting energy expenditure and intake vary by neighborhood income and education levels (Gordon-Larsen et al., 2006; Oreskovic et al., 2009). Yet, the majority of literature evaluating childhood obesity disparities lack the large sample size, objective BMI measures, longitudinal data, or broad range of area-based and GIS measures needed to adequately assess the potential relationship between childhood weight disparities and the socioeconomic and built-environment characteristics of neighborhoods.
In this study, we aimed to: (1) assess racial/ethnic differences in cross-sectional BMI z-score and longitudinal change in BMI z-score among children and adolescents and (2) examine the extent to which any observed differences are explained by differences in neighborhood socioeconomic status (SES) and features of the built environment, which we hypothesized to be potential drivers of childhood obesity disparities.
METHODS
Study design and participants
Electronic health record (EHR) data on height, weight, age, sex, race/ethnicity, date and location of well-child visits, and most recent residential address were collected and analyzed in 2012–2013 for all children age 4 to 18 years seen for well-child care between August 2011 and August 2012 at the 14 pediatric practices of Harvard Vanguard Medical Associates (HVMA), a large multi-site, multi-specialty physician group practice in eastern Massachusetts. Patients were excluded if they had (1) a residential address outside of Massachusetts, (2) any history of medical diagnoses affecting growth and nutrition, including pregnancy, (3) incomplete data on child’s race/ethnicity, or (4) any outlier BMI z-score values (less than −6 and greater than 6) based on US 2000 reference data (Kuczmarski et al., 2002). For longitudinal analyses, the inclusion criteria additionally required that children have two or more BMI measurements between January 2008 and August 2012 with a span of at least 1 year between the earliest available and most recent BMI measurements. The Institutional Review Board of Harvard Pilgrim Health Care approved the study protocol.
Independent Variable
The independent variable of child’s race/ethnicity was based on parent report on a written card completed during the patient registration process as part of previously implemented quality-improvement efforts to improve race/ethnicity documentation at these practices. The original entries were categorized to non-Hispanic white, non-Hispanic black, Hispanic, Asian, and other race/ethnicity. Multivariate analyses of BMI disparities focused on minority racial ethnic populations with BMI disparities. Thus, we included black and Hispanic children given higher mean BMI z-scores and obesity prevalence for these children compared to their white counterparts and excluded Asian children given lower mean BMI z-scores and obesity prevalence. We also excluded children with other race/ethnicity because this heterogeneous category, which includes multiracial children, would be difficult to characterize as a single group or to make generalizations from.
Outcomes: BMI z-score and Change in BMI z-score
The main outcome measure for cross-sectional analyses was the child’s age- and sex-specific BMI z-score derived from height and weight measured and recorded in the EHR at their most recent well-child care visit between August 2011 and August 2012. For longitudinal analyses, change in BMI z-score was calculated using the child’s earliest available BMI measure from January 2008 to August 2011 and his or her most recent BMI measure from August 2011 to August 2012. At each well-child visit, medical assistants measured height and weight based on the written standardized protocol of HVMA, which is consistent with the standard of care in pediatric primary care and has been described in previously published work (Wen et al., 2012). BMI was calculated as kg/m2. CDC growth curves were used to define the participants’ age- and sex-specific BMI z-score and percentile (Kuczmarski et al., 2002). Overweight was defined as BMI ≥85th – <95th percentile and obesity as BMI ≥95th percentile.
Potential Intermediates and Effect Modifiers: Neighborhood SES and Built-Environment Characteristics
Geographic information system (GIS) software (ArcGIS 10.1, ESRI, Redlands CA) was used to characterize neighborhood SES, food environment, and the physical activity environment of participants based on geocoded residential addresses.
To characterize neighborhood SES, geocoded addresses were linked with area-based socioeconomic measures from 2006–2010 American Community Survey data on median household income (in 2009 dollars) and the percent of adults without a high school diploma at the US census tract level.
Spatial datasets used to characterize the built environment included: complete street network and pedestrian street network (ArcGIS Data and Maps 2010 StreetMap USA); businesses, including food establishments (InfoUSA 2009); and open space used for recreation (Office of Geographic Information [MassGIS], Commonwealth of Massachusetts, Information Technology Division).
To characterize the food environment, we calculated the network distance to the nearest fast-food and non-fast-food restaurants, supermarket (≥50 employees) and small food store (<50 employees) using food establishments categories consistent with the North American Industry Classification System (NAICS) definitions in use by US federal agencies. Distances along the street network were calculated using geocoded residential address and the ArcGIS Network Analyst Extension Closest Facility tool.
Based on prior work describing street connectivity, residential density, and mixed land use as key components of neighborhood walkability, (Frank et al., 2008; Sallis et al., 2009) the following recreational space and land use variables were calculated to characterize the physical activity environment: (1) recreational open space density (a count of open spaces for recreation such as parks within 800 meter line-based network buffers); (2) intersection density (the number of intersections per square km within 800 meter network buffers with intersections defined as points where 3 or more road segments come together); (3) residential density (the number of housing units per square km of the census tract); and (4) land use mix, an entropy score ranging from 0 to 1 which defines the level of variety of businesses in an area among 5 land use types (food, retail, services, cultural/educational, and physical activity) with a score of 0 corresponding to no variety in land use whereas a score of 1 indicates an equal mixture among all five land use types.
Other variables
Individual-level EHR data was collected on each child’s date of birth and sex. The dates of well-child visits were also extracted to calculate the child’s age at the most recent visit and the time interval in years from the earliest available to the most recent BMI measure for longitudinal analysis.
Statistical analysis
Descriptive analyses were conducted to examine child individual-level and neighborhood characteristics. We examined potential difference in race/ethnicity between the cross-sectional sample and the longitudinal sub-sample using chi square tests. Bivariate and multivariable linear regression models were then utilized to assess the association between child’s race/ethnicity and cross-sectional BMI z-score as well as longitudinal change in BMI z-score, adjusting for covariates and potential intermediates. Five multivariable models were developed – four partially-adjusted and one fully-adjusted model. Model 1 was adjusted for the child’s age and sex. Model 2 was additionally adjusted for neighborhood SES by adding neighborhood median household income and the percent of adults without a high school diploma. Model 3 was adjusted for variables in Model 1 and added the food environment measures, including the network distance to the nearest fast-food restaurant, non-fast-food restaurant, supermarket and small food store. Model 4 controlled for the physical activity environment variables of recreational open space density, intersection density, residential density and land use mix. Model 5 included all the above individual-level covariates and potential neighborhood and built-environment intermediates. The percent attenuation of observed disparities in BMI for each model was calculated as the percent change in each point estimate compared to the estimate obtained from Model 1. For the longitudinal BMI z-score change analyses, all of the same models listed above were utilized but additionally adjusted for the time interval in years from the earliest available to the most recent BMI measure in all models.
The variance inflation factor (VIF) was calculated for all variables in both cross-sectional and longitudinal fully adjusted models to test for potential collinearity between neighborhood socioeconomic and built-environment variables. All VIF values for the fully adjusted models were less than 4 suggesting that collinearity was less likely to be of concern (Kleinbaum DG, Kupper LL, Muller KE, Nizam, 1998).
All analyses were completed using SAS version 9.3 (SAS Institute Inc., Cary, NC).
RESULTS
Table 1 shows individual-level and neighborhood characteristics, overall and stratified by child race/ethnicity, for all 44,810 children and adolescents included in the study. Non-Hispanic white children represented 65.2% of total participants, while 13.3% were non-Hispanic black, 5.7% Hispanic, 9.3% Asian and 6.6% other race/ethnicity. Among these children, longitudinal BMI z-score data was available for 42,395 (94.6%). We did not observe statistically significant difference in race/ethnicity between the longitudinal sub-sample and the cross-sectional sample. Based on 2010 Census estimates, nearly 600,000 children under 18 years live in the three main counties in eastern Massachusetts wherein the majority of children in our study sample reside (Suffolk, Middlesex and Norfolk), and among these children, 76% are white, 8.5% black, and 8.5% Hispanic. Thus, in comparison to eastern MA overall, our sample may be over-represented in the proportion of black children and under-represented in white and Hispanic children.
Table 1.
Participant and neighborhood characteristics, overall and by race/ethnicity, among 44,810 children aged 4 to 18 years seen at 14 Massachusetts pediatric practices in 2011–2012
| Overall | Black | Hispanic | Asian | White | Other | |
|---|---|---|---|---|---|---|
|
Number of participants, N (%) |
44810 (100) |
5943 (13.3) |
2549 (5.7) |
4166 (9.3) |
29206 (65.2) |
2946 (6.6) |
| Mean (SD) or N (%) | ||||||
|
Participant Characteristics |
||||||
| Female sex | 22143 (49.4) |
2903 (48.8) |
1213 (47.6) |
2137 (51.3) |
14448 (49.5) |
1442 (48.9) |
|
Most recent well- child visit in 2011– 2012 |
||||||
| Age, years | 11.3 (4.5) | 11.5 (4.4) | 10.9 (4.4) | 10.2 (4.4) | 11.5 (4.5) | 10.4 (4.5) |
| BMI, kg/m2 | 19.9 (4.9) | 21.6 (6.0) | 20.8 (5.5) | 18.3 (3.9) | 19.7 (4.5) | 19.7 (5.0) |
| BMI z-score | 0.43 (1.04) |
0.79 (1.06) |
0.74 (1.10) |
0.11 (1.07) |
0.36 (0.99) |
0.49 (1.07) |
| BMI category | ||||||
| <85th percentile | 32181 (71.8) |
3438 (57.8) |
1514 (59.4) |
3354 (80.5) |
21856 (74.8) |
2019 (68.5) |
| 85th – <95th Percentile |
6766 (15.1) |
1080 (18.2) |
474 (18.6) | 490 (11.8) | 4257 (14.6) |
465 (15.8) |
| ≥95th percentile | 5863 (13.1) |
1425 (24.0) |
561 (22.0) | 322 (7.7) | 3093 (10.6) |
462 (15.7) |
|
Change from earliest (2008– 2011) to most recent visita |
||||||
| Age, years | 3.2 (0.8) | 3.2 (0.8) | 3.1 (0.8) | 3.1 (0.9) | 3.3 (0.8) | 3.1 (0.8) |
| BMI, kg/m2 | 1.5 (2.3) | 1.9 (2.5) | 1.6 (2.5) | 1.0 (1.9) | 1.5 (2.2) | 1.4 (2.3) |
| BMI z-score | 0.07 (0.71) |
0.11 (0.69) |
0.08 (0.72) |
0.08 (0.78) |
0.05 (0.69) |
0.13 (0.76) |
|
Neighborhood Socioeconomic Measures |
||||||
| Percent of adults without high school diploma |
8.4 (7.7) | 15.7 (9.1) | 14.7 (10.1) |
8.8 (8.6) | 6.2 (5.2) | 10.1 (8.5) |
| Median household income, dollars |
86002 (32578) |
57717 (22619) |
62952 (25206) |
88039 (33272) |
94403 (30535) |
76780 (29832) |
|
Food Environment |
||||||
|
Networked Distance (miles) to: |
||||||
| Supermarkets | 1.6 (1.1) | 1.1 (0.6) | 1.2 (0.8) | 1.5 (0.9) | 1.8 (1.2) | 1.3 (0.8) |
| Small Food Stores |
1.2 (1.0) | 0.7 (0.6) | 0.7 (0.7) | 1.1 (0.9) | 1.4 (1.1) | 1 (0.9) |
| Fast Food | 0.9 (0.7) | 0.5 (0.4) | 0.5 (0.5) | 0.8 (0.7) | 1 (0.8) | 0.7 (0.6) |
| Non-Fast Food | 0.8 (0.7) | 0.5 (0.4) | 0.5 (0.5) | 0.7 (0.6) | 0.9 (0.8) | 0.6 (0.5) |
|
Physical Activity Environment |
||||||
| Recreational open space, count within 800m buffer |
2.7 (2.9) | 3.4 (3.2) | 4 (3.4) | 2.9 (2.9) | 2.4 (2.7) | 3.4 (3.2) |
| Residential density, housing units per square km |
1047 (1514) |
1910 (1682) |
1834 (1947) |
1038 (1482) |
769 (1321) |
1394 (1589) |
| Intersections per square km |
77.6 (37.4) |
99.7 (33.5) |
101 (35.6) | 81 (35.3) | 69.3 (35.6) |
89.8 (35.7) |
| Land use mix | 0.5 (0.4) | 0.6 (0.3) | 0.6 (0.3) | 0.5 (0.3) | 0.4 (0.4) | 0.6 (0.3) |
Includes the longitudinal subsample of children with at least 2 BMI data points at least 1 year apart (n=42,395)
BMI z-score and the prevalence of obesity and overweight were substantially higher among black and Hispanic children compared to white children, and black children had the greatest increase in BMI z-score over time. Asian children in this sample had the lowest prevalence of overweight and obesity, mean BMI z-score, and longitudinal change in BMI. Compared to white children, black and Hispanic children on average lived in neighborhoods with lower median incomes, higher proportions of adults without high school diplomas, closer proximity to all food establishments, greater recreational open space density, higher residential and intersection density, and higher land use mix.
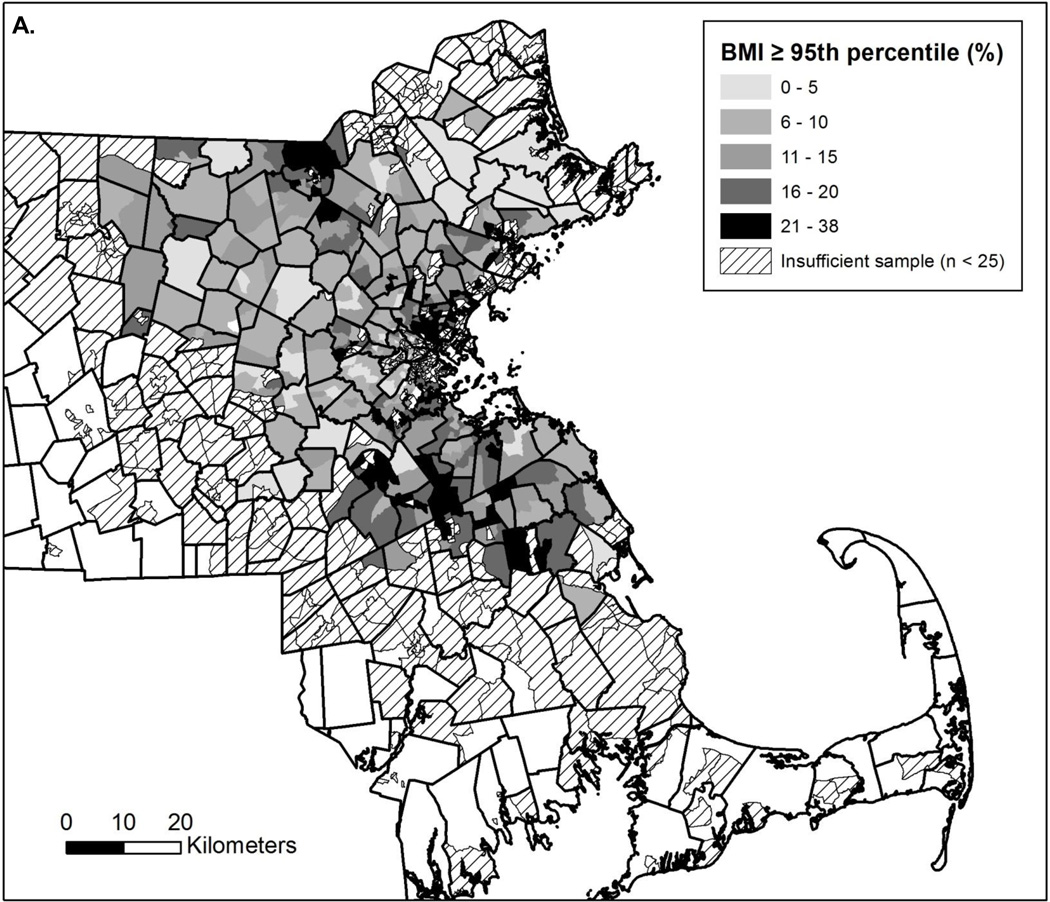
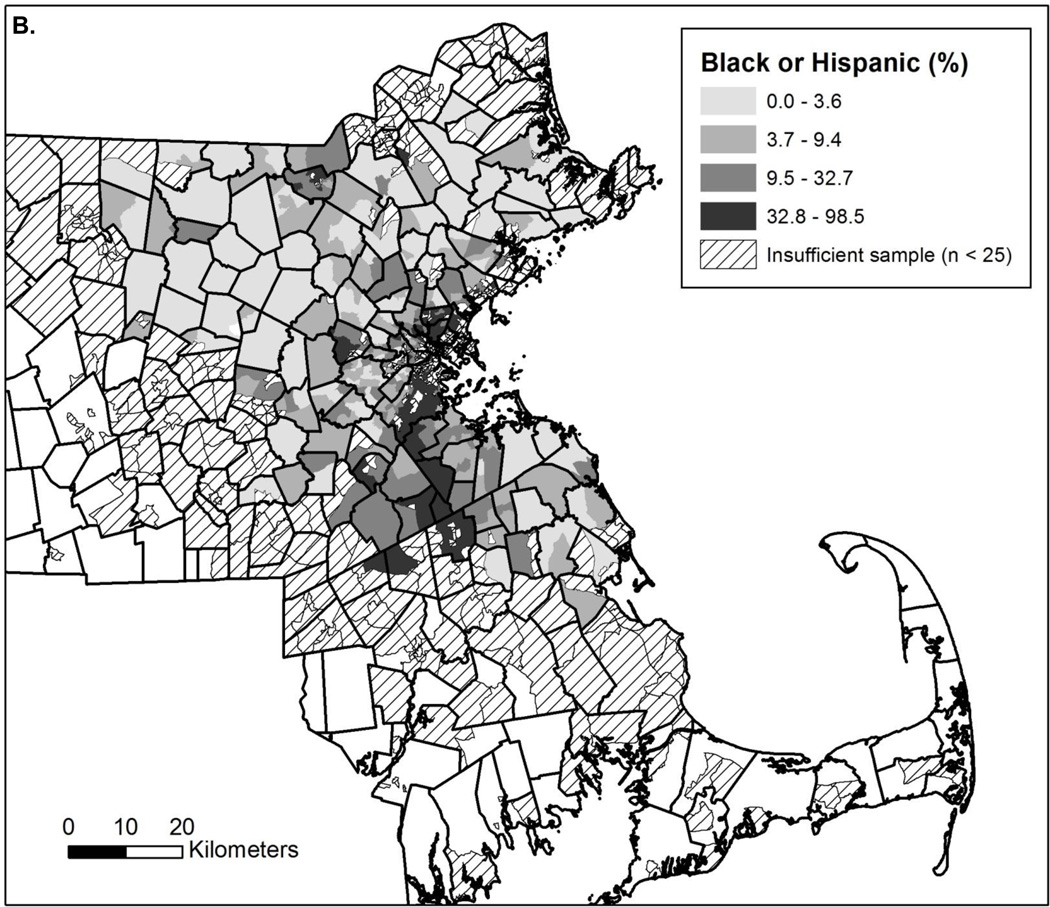
The maps of eastern Massachusetts displayed in Figure 1 visually demonstrate the percentage of children in the sample with BMI ≥95th percentile by US census tract (Figure 1A) and the percentage of children from minority racial/ethnic groups (non-Hispanic black or Hispanic) by census tract (Figure 1B). The darkest shaded areas of each map, representing highest prevalence of obesity among the sample and highest concentration of black or Hispanic participants, correlate (Pearson’s correlation coefficient = 0.61, p-value<0.001).
Figure 1.
Percentage of participants by census tract with BMI ≥95thpercentile (A) and from black or Hispanic racial/ethnic groups (B) among 44,810 children aged 4 to 18 years seen at 14 Massachusetts pediatric practices in 2011–2012
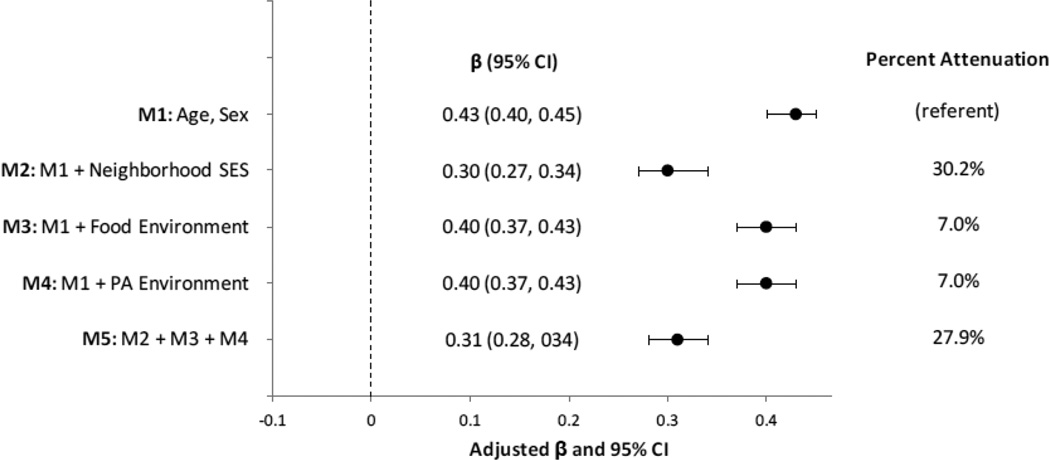
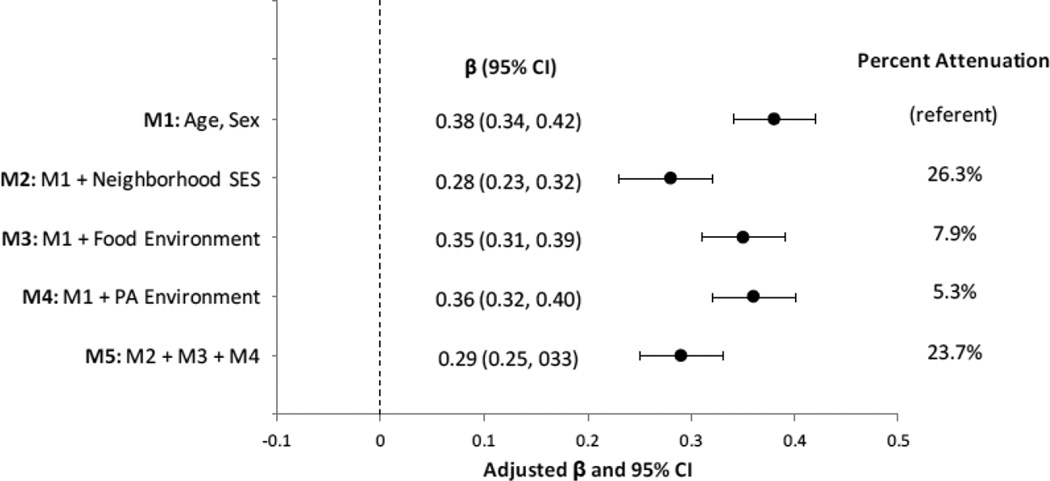
Results of multivariate analyses examining the relationship between race/ethnicity and cross-sectional BMI z-score are displayed in Figure 2 for black and Hispanic children compared to their white counterparts. In Model 1, adjusted for child’s age and sex, higher BMI z-scores of 0.43 units (95% CI: 0.40, 0.45) were observed among black children and 0.38 units (95% CI: 0.34, 0.42) among Hispanic children compared to the referent group of white children. Additionally adjusting for neighborhood SES in Model 2 resulted in a 30.2% attenuation of the BMI z-score difference observed for black children and a 26.3% attenuation for Hispanic children compared to their white counterparts. Adjustment for food environment characteristics in Model 3 resulted in a 7.0% attenuation in the BMI z-score difference for black and a 7.9% attenuation for Hispanic children compared to white children. Model 4 adjusted for the physical activity environment measures with a similar degree of attenuation, 7.0% for black and 5.3% for Hispanic children compared to white children. Adjusting for all individual-level covariates and potential intermediates including neighborhood SES, food and physical activity environments in Model 5, resulted in a 27.9% attenuation of the difference in BMI z-scores for black children and a 23.7% attenuation for Hispanic compared to white children.
Figure 2.
Multivariable modelsa of the association between black versus white race and cross-sectional BMI z-scoreb
aMultivariable Models - Model 1: adjusted for age and sex; Model 2: Model 1 + neighborhood median household income + percent adults with no high school diploma; Model 3: Model 1 + network distance to nearest fast food restaurant, non-fast food restaurant, supermarket and small food store; Model 4: Model 1 + recreational open space density, intersection density, residential density, and land use mix; Model 5: Model 2 + Model 3 + Model 4.
bAmong 44,810 children aged 4 to 18 years seen at 14 Massachusetts pediatric practices in 2011–2012
In longitudinal analyses of BMI z-score change over time adjusted for age and sex, a 0.06 unit (95% CI: 0.04, 0.08) greater increase between the earliest and most recent well-child visit was observed among black children compared to their white counterparts. This difference was not substantially attenuated in partially- or fully-adjusted models. No significant difference in BMI z-score change was observed between Hispanic and white children (0.00 units; 95% CI: −0.03, 0.03).
DISCUSSION
In this large sample of 44,810 children and adolescents seen for well child care in eastern Massachusetts, we observed a higher prevalence of obesity and higher cross-sectional BMI z-scores among black and Hispanic children of 0.43 BMI z units (95% CI: 0.40, 0.45) and 0.38 units (95% CI: 0.34, 0.42), respectively, compared to white children. Black but not Hispanic children also a greater increase in BMI z-scores over time compared to their white counterparts. To put the observed BMI z-score differences in context, a 0.4 units higher BMI z-score translates to about a 2 kilogram or 4.4 pound difference in weight compared to an 11 year-old male (the study sample’s average age) with height, weight and BMI at approximately the 50th percentile (The Children’s Hospital of Philadelphia Research Institute, n.d.). Adjusting for neighborhood SES attenuated the cross-sectional BMI z-score differences by 30.2% for black and 26.3% for Hispanic children compared to white children. Controlling for features of the food and physical activity environment also attenuated the observed BMI z-score differences but to a lesser extent than neighborhood SES. The observed racial/ethnic disparities in childhood obesity persisted, even after adjustment for all confounders and potential intermediates examined in this study.
This study’s results suggest that neighborhood SES may be an important mediator of racial/ethnic disparities among children with obesity. Additionally, features of the built environment contribute to the observed obesity disparities but to a lesser degree than neighborhood SES. Prior work suggests that the built environment may moderate the effect of childhood obesity interventions (Epstein et al., 2012). Our findings further indicate that interventions seeking to reduce racial/ethnic disparities in childhood obesity should be individually tailored in a way that facilitates effective navigation of potentially obesogenic environments.
Models adjusting for neighborhood SES and features of the built environment did not substantially differ from models adjusting for neighborhood SES alone. Many factors may potentially explain this finding. Quantity and access may not necessarily correlate with quality and affordability. For example, the same proximity to a supermarket in a low-income versus high-income neighborhood may not reflect comparable access to healthful food options (Glanz et al., 2007) or similar levels of exposure to advertising promoting unhealthy choices (Yancey et al., 2009). Walkability measures may not reflect other relevant conditions of the environment that are likely to impact energy expenditure such as safety, crime and maintenance of public facilities such as playgrounds and parks, which can vary by neighborhood socioeconomic factors and racial/ethnic composition (Zhu and Lee, 2008).
Neither neighborhood SES nor the built environment completely explained the racial/ethnic disparities observed in this study. This is an important finding that may be the result of several unmeasured factors driving racial/ethnic disparities in child BMI. In addition to unmeasured differences in individual and household factors, the school environment may play an important role in health disparities (Schuster et al., 2012) and in mediating energy intake and expenditure. One recent review of over 300 published studies compared school- versus community-based interventions to increase physical activity and found that built-environment changes increasing access to parks had far less impact on energy expenditure than mandatory physical education in school, active classroom breaks, and built-environment changes promoting active commuting to schools (Bassett et al., 2013). It is possible that the inclusion of information about the school environment among this sample would have further attenuated observed racial/ethnic disparities.
There is also evidence of disparities in access, delivery, and utilization of health care services among low income and minority racial/ethnic populations (Epstein and Ayanian, 2001; Flores and Committee On Pediatric Research, 2010; Flores and Tomany-Korman, 2008; U.S. Department of Health and Human Services Agency for Healthcare Research and Quality, 2013) which may also play a part in explaining the persistent BMI disparities observed in this study. Although the extent of this role is unclear, the success of some pediatric clinical interventions in improving weight status among low-income pre-school age children supports the feasibility of this potential pathway (Taveras et al., 2011).
The strengths of this study include the large sample size of nearly 45,000 children and adolescents with objectively measured height and weight obtained from EHR data and parent-reported data on race and ethnicity. GIS methods were utilized to characterize multiple components of the neighborhood context in order to examine the association between race/ethnicity and BMI. The study also has a few limitations that should be noted. Foremost is the potential for residual confounding secondary to unmeasured aspects of the neighborhood or individual-level SES measures, parents’ BMI, or schools. The observational design of this study limits the ability to examine causes of racial/ethnic disparities. In longitudinal analyses, black children demonstrated a greater increase in BMI z-scores over time compared to their white counterparts of 0.06 unit (95% CI: 0.04, 0.08); no significant difference was noted for Hispanic children. Adjusting for neighborhood SES and features of the built environment had minimal impact on these observed differences. Longitudinal data on residential address for participants were unavailable; thus, all neighborhood-level variables were cross-sectional which may limit our ability to evaluate the true impact of the neighborhood on the observed racial disparities in BMI change over time. Furthermore, the relatively short longitudinal time frame of mean (SD) 3.2 (0.8) years may not have been sufficient to detect large changes in BMI z-score or to examine the extent to which neighborhood factors may contribute to observed racial/ethnic differences. Finally, the use of EHR data from an insured patient sample presenting for well child care may restrict the generalizability of these results to uninsured and lower income patient populations.
In conclusion, this study contributes to the understanding of potential socio-contextual pathways that may underlie alarming disparities in childhood obesity. The results suggest that neighborhood SES is an important driver of disparities in child and adolescent BMI and that built environment characteristics also help explain obesity disparities. These results highlight the imperative need to address contextual factors that contribute to disparities in childhood overweight and obesity such as the neighborhoods and built environments in which children live. Effective interventions will not only need to be mindful of the built-environment context of health behaviors but also the perhaps more critical socioeconomic barriers to achieving a healthy weight in lower SES communities. The implementation and evaluation of interventions and policies that address neighborhood-level differences among racial/ethnic groups may yield additional valuable information, as would further detailed examination of the role that the quality of built-environment features and resources play in mediating differences in energy intake, physical activity, and weight status.
Figure 3.
Multivariable modelsa of the association between Hispanic versus white race/ethnicity and cross-sectional BMI z-scoreb
aMultivariable Models - Model 1: adjusted for age and sex; Model 2: Model 1 + neighborhood median household income + percent adults with no high school diploma; Model 3: Model 1 + network distance to nearest fast food restaurant, non-fast food restaurant, supermarket and small food store; Model 4: Model 1 + recreational open space density, intersection density, residential density, and land use mix; Model 5: Model 2 + Model 3 + Model 4.
bAmong 44,810 children aged 4 to 18 years seen at 14 Massachusetts pediatric practices in 2011–2012
HIGHLIGHTS.
This study examines the role of neighborhood features in child obesity disparities.
We collected race/ethnicity, growth data and geocoded address for 44,810 children.
Adjusting for neighborhood SES attenuated observed racial/ethnic BMI disparities.
Built environment measures also attenuated BMI differences but to a lesser extent.
Interventions to reduce child obesity must address neighborhood context.
Acknowledgments
This study was conducted with support from an Academic Pediatric Association Young Investigator Award (PI: Sharifi) and the Harvard Catalyst | The Harvard Clinical and Translational Science Center (UL1 TR001102) and financial contributions from Harvard University and its affiliated academic healthcare centers. Dr. Sharifi is supported by an AHRQ Mentored Career Development Award for Child and Family Centered Outcomes Research (K12 HS022986). Dr. Taveras is supported by grant K24 DK10589 from the National Institute of Diabetes and Digestive and Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic health care centers, the NIH, AHRQ or the Academic Pediatric Association.
Abbreviations
- BMI
body mass index
- CI
confidence interval
- EHR
electronic health record
- GIS
geographic information system
- HVMA
Harvard Vanguard Medical Associates
- SES
socioeconomic status
- VIF
variance inflation factor
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement: The authors declare that there are no conflicts of interest.
REFERENCES
- assett DR, Fitzhugh EC, Heath GW, Erwin PC, Frederick GM, Wolff DL, Welch Wa, Stout AB. Estimated energy expenditures for school-based policies and active living. Am. J. Prev. Med. 2013;44:108–113. doi: 10.1016/j.amepre.2012.10.017. [DOI] [PubMed] [Google Scholar]
- Bell JF, Wilson JS, Liu GC. Neighborhood greenness and 2-year changes in body mass index of children and youth. Am. J. Prev. Med. 2008;35:547–553. doi: 10.1016/j.amepre.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Obesity prevalence among low-income, preschool-aged children--New York City and Los Angeles County, 2003–2011. MMWR. Morb. Mortal. Wkly. Rep. 2013;62:17–22. [PMC free article] [PubMed] [Google Scholar]
- Ding D, Sallis JF, Kerr J, Lee S, Rosenberg DE. Neighborhood environment and physical activity among youth a review. Am. J. Prev. Med. 2011;41:442–455. doi: 10.1016/j.amepre.2011.06.036. [DOI] [PubMed] [Google Scholar]
- Duncan DT, Sharifi M, Melly SJ, Marshall R, Sequist TD, Rifas-Shiman SL, Taveras EM. Characteristics of walkable built environments and BMI z-scores in children: evidence from a large electronic health record database. Environ. Health Perspect. 2014;122:1359–1365. doi: 10.1289/ehp.1307704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein AM, Ayanian JZ. Racial disparities in medical care. N. Engl. J. Med. 2001;344:1471–1473. doi: 10.1056/NEJM200105103441911. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Raja S, Daniel TO, Paluch Ra, Wilfley DE, Saelens BE, Roemmich JN. The built environment moderates effects of family-based childhood obesity treatment over 2 years. Ann. Behav. Med. 2012;44:248–258. doi: 10.1007/s12160-012-9383-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng J, Glass Ta, Curriero FC, Stewart WF, Schwartz BS. The built environment and obesity: a systematic review of the epidemiologic evidence. Health Place. 2010;16:175–190. doi: 10.1016/j.healthplace.2009.09.008. [DOI] [PubMed] [Google Scholar]
- Fiechtner L, Sharifi M, Sequist T, Block J, Duncan DT, Melly SJ, Rifas-Shiman SL, Taveras EM. Food environments and childhood weight status: effects of neighborhood median income. Child. Obes. 2015;11:260–268. doi: 10.1089/chi.2014.0139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores G Committee On Pediatric Research. Technical report--racial and ethnic disparities in the health and health care of children. Pediatrics. 2010;125:e979–e1020. doi: 10.1542/peds.2010-0188. [DOI] [PubMed] [Google Scholar]
- Flores G, Tomany-Korman SC. Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121:e286–e298. doi: 10.1542/peds.2007-1243. [DOI] [PubMed] [Google Scholar]
- Frank LD, Kerr J, Sallis JF, Miles R, Chapman J. A hierarchy of sociodemographic and environmental correlates of walking and obesity. Prev. Med. (Baltim) 2008;47:172–178. doi: 10.1016/j.ypmed.2008.04.004. [DOI] [PubMed] [Google Scholar]
- Galvez MP, Hong L, Choi E, Liao L, Godbold J, Brenner B. Childhood obesity and neighborhood food-store availability in an inner-city community. Acad. Pediatr. 2009;9:339–343. doi: 10.1016/j.acap.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K, Sallis JF, Saelens BE, Frank LD. Nutrition Environment Measures Survey in stores (NEMS-S): development and evaluation. Am. J. Prev. Med. 2007;32:282–289. doi: 10.1016/j.amepre.2006.12.019. [DOI] [PubMed] [Google Scholar]
- Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117:417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- Kleinbaum DG, Kupper LL, Muller KE, Nizam A. Applied Regression Analysis and Other Multivariable Methods. 3rd. Brooks/Cole Publishing Company; 1998. [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, Johnson CL. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat. 11. 2002;11:1–190. [PubMed] [Google Scholar]
- Lawman HG, Wilson DK. A review of family and environmental correlates of health behaviors in high-risk youth. Obesity (Silver Spring) 2012;20:1142–1157. doi: 10.1038/oby.2011.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu GC, Wilson JS, Qi R, Ying J. Green neighborhoods, food retail and childhood overweight: differences by population density. Am. J. Health Promot. 2007;21:317–325. doi: 10.4278/0890-1171-21.4s.317. [DOI] [PubMed] [Google Scholar]
- Matthews Sa, Moudon AV, Daniel M. Work group II: Using Geographic Information Systems for enhancing research relevant to policy on diet, physical activity, and weight. Am. J. Prev. Med. 2009;36:S171–S176. doi: 10.1016/j.amepre.2009.01.011. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oreskovic NM, Kuhlthau Ka, Romm D, Perrin JM. Built environment and weight disparities among children in high- and low-income towns. Acad. Pediatr. 2009;9:315–321. doi: 10.1016/j.acap.2009.02.009. [DOI] [PubMed] [Google Scholar]
- Papas MA, Alberg AJ, Ewing R, Helzlsouer KJ, Gary TL, Klassen AC. The built environment and obesity. Epidemiol. Rev. 2007;29:129–143. doi: 10.1093/epirev/mxm009. [DOI] [PubMed] [Google Scholar]
- Powell LM, Auld MC, Chaloupka FJ, O’Malley PM, Johnston LD. Associations between access to food stores and adolescent body mass index. Am. J. Prev. Med. 2007;33:S301–S307. doi: 10.1016/j.amepre.2007.07.007. [DOI] [PubMed] [Google Scholar]
- Rokholm B, Baker JL, Sørensen TIA. The levelling off of the obesity epidemic since the year 1999--a review of evidence and perspectives. Obes. Rev. 2010;11:835–846. doi: 10.1111/j.1467-789X.2010.00810.x. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Saelens BE, Frank LD, Conway TL, Slymen DJ, Cain KL, Chapman JE, Kerr J. Neighborhood built environment and income: examining multiple health outcomes. Soc. Sci. Med. 2009;68:1285–1293. doi: 10.1016/j.socscimed.2009.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuster MA, Elliott MN, Kanouse DE, Wallander JL, Tortolero SR, Ratner JA, Klein DJ, Cuccaro PM, Davies SL, Banspach SW. Racial and ethnic health disparities among fifth-graders in three cities. N. Engl. J. Med. 2012;367:735–745. doi: 10.1056/NEJMsa1114353. [DOI] [PubMed] [Google Scholar]
- Taveras EM, Gillman MW, Kleinman K, Rich-Edwards JW, Rifas-Shiman SL. Racial/ethnic differences in early-life risk factors for childhood obesity. Pediatrics. 2010;125:686–695. doi: 10.1542/peds.2009-2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taveras EM, Gortmaker SL, Hohman KH, Horan CM, Kleinman KP, Mitchell K, Price S, Prosser LA, Rifas-Shiman SL, Gillman MW. Randomized controlled trial to improve primary care to prevent and manage childhood obesity: the High Five for Kids study. Arch. Pediatr. Adolesc. Med. 2011;165:714–722. doi: 10.1001/archpediatrics.2011.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Children’s Hospital of Philadelphia Research Institute. Pediatric Z-Score Calculator [WWW Document] n.d. URL http://stokes.chop.edu/web/zscore/result.php. [Google Scholar]
- U.S. Department of Health and Human Services Agency for Healthcare Research and Quality. National Healthcare Disparities Report 2012. 2013 AHRQ Publication No. 13-0003. [Google Scholar]
- Wang Y, Beydoun Ma. The obesity epidemic in the United States--gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol. Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- Wen X, Gillman MW, Rifas-Shiman SL, Sherry B, Kleinman K, Taveras EM. Decreasing prevalence of obesity among young children in Massachusetts from 2004 to 2008. Pediatrics. 2012;129:823–831. doi: 10.1542/peds.2011-1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yancey AK, Cole BL, Brown R, Williams JD, Hillier A, Kline RS, Ashe M, Grier Sa, Backman D, McCarthy WJ. A cross-sectional prevalence study of ethnically targeted and general audience outdoor obesity-related advertising. Milbank Q. 2009;87:155–184. doi: 10.1111/j.1468-0009.2009.00551.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu X, Lee C. Walkability and safety around elementary schools economic and ethnic disparities. Am. J. Prev. Med. 2008;34:282–290. doi: 10.1016/j.amepre.2008.01.024. [DOI] [PubMed] [Google Scholar]