With the advent of spinal cord epidural stimulation techniques, i.e., electrically enabled motor control (eEmc) in combination with activity dependent locomotor training, humans with traumatic complete sensori-motor paralysis are able to initiate voluntary leg movements and achieve gains in postural control, and bladder and sexual function (Angeli et al., 2014). However, there are yet some technological barriers of eEmc for therapeutic purposes in humans that prevent weight bearing stepping. In this perspective, we highlight novel features of eEmc techniques based off our recent work in spinalized rats and suggest their implementation in patients with a SCI for more meaningful functional motor outcomes.
In rodents, step-like locomotor movements are generated when the spinal cord is stimulated at the rostral lumbar (L2) or sacral (S1) spinal segments (monopolar stimulation, with the reference electrode placed elsewhere in the body) (Ichiyama et al., 2005). Bipolar stimulation strategies that involve passing current between L2 and S1 (where electrodes implanted over one of these segments is used as the reference electrode) have been most successful in eliciting robust stepping patterns in the rodent (Shah et al., 2012). Frequencies of 40 Hz and pulse width of 0.2 ms have been widely adopted in almost all rodent studies. Similar to the rodent, in persons with a functionally complete SCI too, eEmc of the rostral or caudal spinal segments using bipolar configuration strategies and frequencies ranging from 30–40 Hz, pulse width of 0.2–0.5 ms has resulted in generating voluntary joint movements in the supine position.
These data collectively suggest that although the entire lumbosacral cord possesses rhythmogenic properties, the rostral lumbar and sacral cords are more robust in generating a motor output. The uniqueness of lumbar cord is most likely attributable to its greater potential in generating bursting rhythm and pattern of movement (McCrea and Rybak, 2008). The sacral cord, in contrast maintains its rhythmogenic capacity by direct activation of afferent fibers and motor axons due to the common course of ascending afferent fibers (nerve roots) around sacral segments_ENREF_10. Additionally, ascending propriospinal circuits within the sacral cord terminate into and have an excitatory effect on rostral lumbar locomotor networks (Etlin et al., 2010). Given these unique features of the lumbosacral cord, an obvious scientific inquiry is – what is the potential significance of the interactions of this input between the lumbar and sacral neuronal circuitries in defining locomotor success? Will eEmc strategies that adopt spatio-temporal neuromodulation of the lumbar and sacral cords lead to more meaningful functional motor outcomes?
Given the relative preferential activation of rostral and caudal motor pools based on their topographical distribution along the spinal cord, the scientific goal of multi-site eEmc stimulation strategies is to spatially and functionally activate a wide and discrete neuronal populations to synergistically influence and modulate the excitability of sensorimotor pathways for an effective motor output. For example, in non-injured human subjects, addition of stimulation at L1 and/or at C5 to an existing stimulation at T11 immediately results in enhanced kinematics, interlimb coordination as well as EMG patterns in proximal and distal leg muscles. Sequential cessation of stimulation at C5 and then at L1 results in progressive degradation of the stepping pattern (Gerasimenko et al., 2015). Similarly, a stronger patterned EMG response from multiple leg muscles is observed with eEmc applied at multiple segments of the lumbosacral enlargement in contrast to localized individual segments in persons with a complete SCI (Angeli et al., 2014).
However, one of the limitations of multi-site stimulation programs employed thus far, consists of stereotyped high-frequency trains of electrical pulses simultaneously delivered through multiple electrodes in the array. The effects of alterations in parameters such as frequency of stimulation or the relative timing of stimulation pulses at distinct electrode sites using independent monopolar configurations on locomotor output have not been adequately explored. Because spinal locomotor related neural networks have varied functional and anatomical characteristics, it seems reasonable to suggest that their selective activation using unique spatial and temporal stimulation configurations will yield significant interactive effects for locomotion regulation; thereby rendering multi-site eEmc more conducive for translation to humans.
Recently, we tested the interactive effects of different stimulation frequencies and pulse intervals delivered at multiple spinal cord sites (independent monopolar stimulation at each stimulation site) in facilitating locomotion in spinal rats (Shah et al., 2016). We kept the frequency of stimulation at L2 constant at 40 Hz and varied the frequency of stimulation at S1 (five different frequencies) to allow rats spinalized at T10 to step bipedally on a moving treadmill. Our goal was to target the rostral lumbar spinal cord and the sacral spinal cord for their unique capacities to generate bursting rhythmic patterns. Our data demonstrate that at 20 and 40 Hz frequencies of S1 stimulation, and when stimulating the L2 (40 Hz) and S1 spinal segments independently, but with specific inter stimulation time intervals, an obviously more robust stepping performance is observed in comparison to stimulation of lumbar or sacral segments alone. Noteworthily too, the stepping is achievable as early as three weeks after the injury, with only six training sessions and without the use of a pharmacological agent (Shah et al., 2016). Stepping kinematics and coordinated locomotor EMG patterns of muscle activation throughout a step cycle are closer to pre-injury levels when the independent source multi-segmental stimulation is used.
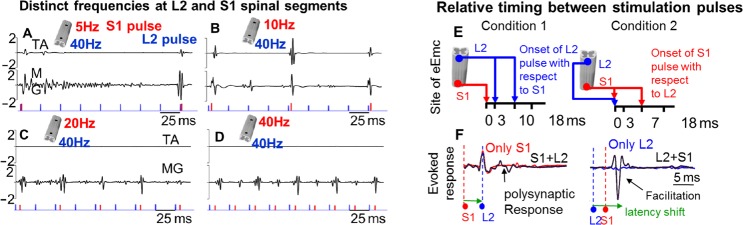
Although use of specific frequencies to elicit a locomotor response from independent eEmc at L2 or S1 has been previously reported; our data specifically reveal that with the combined L2 40 Hz – S1 40 Hz and L2 40 Hz – S1 20 Hz sequences, a greater number of evoked responses are generated in a given time (Figure 1A–D); suggesting the need to activate an optimal population of interneuronal networks or activate the same interneuronal pools more frequently for robust stepping to occur. Additionally, at the higher frequency, the presynaptic cell's repeated and persistent stimulation of the postsynaptic cell most likely enhances synaptic efficacy to allow for consistent motor output (Hebbian learning).
Figure 1.
Multi-site stimulation that utilizes spatio-temporal independent monopolar stimulation strategies at L2 and S1 reveal unique effects of change in frequency of stimulation and relative timing between stimulation pulses.
(A–D) During a testing session rats are suspended using a body weight support system over a moving treadmill and stimulated at the L2 and S1 spinal segments to elicit a stepping response. In this demonstration, a single rat is stimulated (monopolar) at the L2 spinal segment with a frequency of 40 Hz (L2 only) and S1 stimulation is altered between four different frequencies. Note that with increasing frequency of stimulation, the number of spinal evoked responses from the tibialis anterior (TA) and medial gastrocnemius (MG) muscles also increases. Trials C and D resulted in the best stepping pattern and suggests interaction of frequencies in a way that engages a wider flexor-extensor neuronal pool for robust locomotor output. Note that a clear interaction response is evoked only in the presence of S1 stimulation pulse. E–F) Keeping the frequency of stimulaiton at S1 constant, our data also reveal that the time at which the L2 or S1 pulse is initiated with respect to each other strongly shapes locomotor success. Two distinct relative times that enhance step quality were identified. Red and blue traces in F indicate responses to individual S1 or L2 pulses respctively. Traces in black are a resultant evoked response consequent to the added pulse from L2 or S1. Note that a L2 pulse initiated 3–19 ms after onset of the S1 pulse results in a polysynaptic response (condition 1); while a S1 pulse initiated after the L2 pulse drastically amplifies the interaction evoked response.
Noticeably too, different interpulse intervals between the onset of L2 and S1 pulses elicit unique interactions in spinal evoked response in the muscle and this directly coincides with stepping ability [Figure 6 in (Shah et al., 2016)]. Specifically, near-normal stepping is best attained when 1) the L2 pulse is applied at 3–10 ms after the onset of the S1 pulse, [relative timing between stimulation pulses- condition 1] or when 2) the S1 pulse is applied 0–7 msec after the L2 pulse, [condition 2] (Figure 1E, F). Our neurophysiology data demonstrate that in condition 1, the L2 pulse modulates evoked response by S1 pulse to result in a robust polysynaptic response; whereas in condition 2, the S1 pulse significantly amplifies the evoked response elicited at L2. These findings lead us to suggest that the rostral lumbar segments play a greater role in generating stepping patterns; while sacral segments strongly facilitate the activity induced by L2. Specifically, for condition 1, eEmc at S1 excites a larger pool of both lumbar and sacral neurons through the common course of ascending afferent fibers (nerve roots) around sacral segments; while the L2 pulse retains these excitability features of the evoked middle response (by S1) and engages a wider pool of neuronal networks (reflected in a polysynaptic response) that are crucial in generating an effective locomotor pattern. For condition 2, eEmc at L2 excites afferent nerves entering the cord and cord dorsum to initiate a rhythm and stepping pattern (Kiehn, 2006). Subsequent eEmc at S1 retrogradely activates spinal interneuronal pools, and through the propriospinal pathways that reside in the VII lamina of the sacral cord, can activate the lumbar locomotor related networks (see details in Shah et al., 2016). As such, the physiological mechanisms by which neural networks at lumbar and sacral interact are unique for the two segments. And depending on whether one segment is stimulated prior to the other, motor output is also altered.
That the timing between stimulation pulses is critical in generating stepping response is also supported by experiments that demonstrate the existence of fully alternating locomotor-like cycles when multiple dorsal roots of the neonatal rat spinal cord are electrically stimulated in a staggered manner. In contrast, pulse trains delivered synchronously to multiple dorsal roots (without time intervals) failed to elicit the locomotor rhythm (Dose et al., 2016). Similarly, in a transcutaneous electrical spinal cord stimulation protocol, paired electrical stimulation delivered over the L2 and/or S1 spinal segments with different delays produced considerable post-stimulation modulatory effects in spinally evoked motor potentials in the leg muscles of non-injured humans. Modulation in amplitudes of the evoked responses depended on time intervals between stimulation pulses, as well as on whether the paired stimuli were delivered at a single or dual locations (Sayenko et al., 2015).
Collectively, in this brief perspective, we highlight herein the importance of incorporating a unique set of spatial, and temporal variables delivered through multi-site epidural stimulation to modulate spinal locomotor networks. An approach that capitalizes on 1) stimulation frequencies, 2) the site of stimulation, and 3) the relative timing between stimulation pulses, will eventually permit the complex interaction between excitatory and inhibitory circuits that are important for the generation of smooth locomotor output. Fabrication of multi-electrode arrays that will allow such flexibility might prove most effective in regaining meaningful sensorimotor function after a SCI in humans.
This study was supported by Russian Foundation for Fundamental Research No. 16-29-08173-ofi-m (YG). Partial support for data analysis and interpretation of the results was provided from the Russian Science Foundation No. 14-45-00024 (YG) and the Craig H. Neilsen Foundation #72940 (PKS).
References
- Angeli CA, Edgerton VR, Gerasimenko YP, Harkema SJ. Altering spinal cord excitability enables voluntary movements after chronic complete paralysis in humans. Brain. 2014;137:1394–1409. doi: 10.1093/brain/awu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dose F, Deumens R, Forget P, Taccola G. Staggered multi-site low-frequency electrostimulation effectively induces locomotor patterns in the isolated rat spinal cord. Spinal Cord. 2016;54:93–101. doi: 10.1038/sc.2015.106. [DOI] [PubMed] [Google Scholar]
- Etlin A, Blivis D, Ben-Zwi M, Lev-Tov A. Long and short multifunicular projections of sacral neurons are activated by sensory input to produce locomotor activity in the absence of supraspinal control. J Neurosci. 2010;30:10324–10336. doi: 10.1523/JNEUROSCI.1208-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerasimenko Y, Gorodnichev R, Puhov A, Moshonkina T, Savochin A, Selionov V, Roy RR, Lu DC, Edgerton VR. Initiation and modulation of locomotor circuitry output with multisite transcutaneous electrical stimulation of the spinal cord in noninjured humans. J Neurophysiol. 2015;113:834–842. doi: 10.1152/jn.00609.2014. [DOI] [PubMed] [Google Scholar]
- Ichiyama RM, Gerasimenko YP, Zhong H, Roy RR, Edgerton VR. Hindlimb stepping movements in complete spinal rats induced by epidural spinal cord stimulation. Neurosci Lett. 2005;383:339–344. doi: 10.1016/j.neulet.2005.04.049. [DOI] [PubMed] [Google Scholar]
- Kiehn O. Locomotor circuits in the mammalian spinal cord. Annu Rev Neurosci. 2006;29:279–306. doi: 10.1146/annurev.neuro.29.051605.112910. [DOI] [PubMed] [Google Scholar]
- McCrea DA, Rybak IA. Organization of mammalian locomotor rhythm and pattern generation. Brain Res Rev. 2008;57:134–146. doi: 10.1016/j.brainresrev.2007.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayenko DG, Atkinson DA, Floyd TC, Gorodnichev RM, Moshonkina TR, Harkema SJ, Edgerton VR, Gerasimenko YP. Effects of paired transcutaneous electrical stimulation delivered at single and dual sites over lumbosacral spinal cord. Neurosci Lett. 2015;609:229–234. doi: 10.1016/j.neulet.2015.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah P, Sureddi S, Alam M, Zhong H, Roy RR, Edgerton VRPD, Gerasimenko Y. Unique spatiotemporal neuromodulation of the lumbosacral circuitry shapes locomotor success after spinal cord injury. J Neurotrauma. 2016;33:1709–1723. doi: 10.1089/neu.2015.4256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah PK, Gerasimenko Y, Shyu A, Lavrov I, Zhong H, Roy RR, Edgerton VR. Variability in step training enhances locomotor recovery after a spinal cord injury. Eur J Neurosci. 2012;36:2054–2062. doi: 10.1111/j.1460-9568.2012.08106.x. [DOI] [PMC free article] [PubMed] [Google Scholar]