Abstract
Do day-to-day emotions, social interactions, and sleep play a role in determining which anxious youth respond to supportive child-centered therapy (CCT) versus cognitive behavioral therapy (CBT)? We explored whether measures of day-to-day functioning (captured through ecological momentary assessment, sleep diary, and actigraphy), along with clinical and demographic measures, were predictors or moderators of treatment outcome in 114 anxious youth randomized to CCT or CBT. We statistically combined individual moderators into a single, optimal composite moderator to characterize subgroups for which CCT or CBT may be preferable. The strongest predictors of better outcome included: (a) experiencing higher positive affect when with one’s mother and (b) fewer self-reported problems with sleep duration. The composite moderator indicated that youth for whom CBT was indicated had: (a) more day-to-day sleep problems related to sleep quality, efficiency, and waking, (b) day-to-day negative events related to interpersonal concerns, (c) more DSM-IV anxiety diagnoses, and (d) college-educated parents. These findings illustrate the value of both day-to-day functioning characteristics and more traditional sociodemographic and clinical characteristics in identifying optimal anxiety treatment assignment. Future studies will need to enhance the practicality of real-time measures for use in clinical decision making and evaluate additional anxiety treatments.
Keywords: Ecological momentary assessment, sleep diary, actigraphy, cognitive behavioral therapy, client-centered therapy, optimal combined moderator
Introduction
Anxiety disorders in youth are disabling (Langley, Bergman, McCracken, & Piacentini, 2004) and costly (Bodden, Dirksen, & Bögels, 2008; Greenberg et al., 1999), have a chronic course that does not typically remit without treatment (Hudson, Kendall, Coles, Robin, & Webb, 2002; Kovacs & Devlin, 1998), and have unwanted functional outcomes (Swan & Kendall, 2016). There is strong empirical support for the use of cognitive behavioral therapy (CBT) for treatment of pediatric anxiety (James, Soler, & Weatherall, 2005; Kendall, Hudson, Gosch, Flannery-Schroeder, & Suveg, 2008; Ollendick, Jarrett, Grills-Taquechel, Hovey, & Wolff, 2008; Walkup et al., 2008; Weisz, Weiss, Han, Granger, & Morton, 1995). However, CBT requires specialized therapist training, and CBT therapists are not easily accessible in all communities. As such, broad dissemination efforts are needed, but have proven challenging (Southam-Gerow, Rodríguez, Chorpita, & Daleiden, 2012).
For some anxious youth, supportive psychotherapy approaches that draw on core nonspecific therapeutic ingredients may be sufficient in treating anxiety. To evaluate the efficacy of supportive psychotherapy approaches for youth with PTSD, in comparison with more active CBT approaches, Cohen and colleagues developed Child-Centered Therapy (CCT), a manualized supportive psychotherapy for anxious youth. CCT draws on principles from client-centered therapy, which is widely used in the community (Cohen, Deblinger, Mannarino, & Steer, 2004). CCT includes an emphasis on active listening, reflection, accurate empathy, and encouragement to talk about feelings, but unlike CBT does not include directive problem solving, psychoeducation about anxiety and coping skills, or exposure. CCT was previously used as an active comparison condition for trauma-focused CBT for youth with PTSD to account for effects of attention and therapeutic alliance (Cohen et al., 2004; Cohen, Mannarino, & Iyengar, 2011; Cohen, Mannarino, & Knudsen, 2005). It was also an active comparison condition for CBT for youth with anxiety in the sample from which the current study is based (Silk et al., 2016). Findings from these previous comparisons of CBT versus CCT indicated that both treatments provided improvement pre- to post-treatment, but that CBT was superior to CCT in long-term outcomes.
Given the advantages and disadvantages of both CBT and CCT, it will be important to identify and characterize youth for whom CBT is likely to result in a preferable outcome over supportive therapy CCT, and vice versa. One of the first steps in understanding who will benefit from CBT and/or supportive treatments like CCT is to identify predictors (pretreatment characteristics associated with outcome, regardless of treatment) and, more importantly, moderators of treatment response. Moderators are pretreatment characteristics that are independent of treatment assignment and which indicate a different treatment effect depending on the value of that characteristic (Kraemer, 2013). For example, Compton et al. (2014) found that type of anxiety diagnosis moderated treatment outcome for anxious youth. CBT was preferable to both sertraline and placebo for youth with generalized anxiety disorder (GAD), similar to both sertraline and placebo for youth with separation anxiety disorder (SAD), and less preferable to sertraline but similar to placebo for youth with social anxiety disorder (SocAD).
A problem with individual moderators is that they are often very weak and inconsistent across studies (Compton et al., 2014). Furthermore, if multiple moderators are identified they can provide contradictory treatment indications for the same youth. For example, if type of anxiety diagnosis and age were both identified as moderators, it is possible that a single youth may be indicated for one treatment based on their anxiety diagnosis and a different treatment based on their age, thereby offering no practical treatment recommendation. To address this problem, a novel method for optimally combining individual moderators was recently developed and demonstrated (Kraemer, 2013; Wallace, Frank, & Kraemer, 2013). This method integrates information from multiple potentially weak and/or contradictory individual moderators into a single, stronger, combined moderator that can provide a clear indication of the treatment on which a youth will have a preferable outcome through a weighted prediction algorithm. After rigorous validation, an optimal combined moderator could provide personalized anxiety treatment by indicating which youth could receive effective treatment through supportive community psychotherapy such as CCT, and which should be encouraged to seek out CBT (e.g., through the use of a hand-held computer).
Existing studies of childhood anxiety treatment have searched for individual predictors and moderators (rather than combining them), and have focused largely on sociodemographic, clinical, and family climate measures obtained in a clinical setting (Knight, McLellan, Jones, & Hudson, 2014; Lundkvist-Houndoumadi, Hougaard, & Thastum, 2014). Although these traditional pre-treatment characteristics have been considered in numerous studies, relatively few consistent recommendations have emerged (Herres, Cummings, Swan, Makover, & Kendall, 2015; Knight et al., 2014; Lundkvist-Houndoumani et al., 2014). Severity of primary diagnosis appears to be one of the most robust predictors (Berman, Weems, Silverman, & Kurtines, 2000; Compton et al., 2014). Type of anxiety disorder was revealed to be an important predictor and moderator of treatment effect in more recent studies (Compton et al., 2014; Crawley, Beidas, Benjamin, Martin, & Kendall, 2008; Hudson et al., 2015) but earlier studies provided little conclusive evidence of such effects (Lundkvist-Houndoumani et al., 2014). Similarly, comorbid diagnoses including depressive and externalizing disorders were important in some studies (Crawley et al., 2008; Knight et al., 2014; Rapee et al., 2013; Liber et al., 2010) but not others (Kerns, Read, Klugman, & Kendall, 2013; Rapee, 2003; Shortt, Barrett, & Fox, 2001). Family psychopathology (Berman et al., 2000; Bodden et al., 2008; Compton et al., 2014; Hudson et al., 2015; Schleider et al., 2015; Southam-Gerow, Kendall, & Weersing, 2001) and age (Bodden et al., 2008; Southam-Gerow et al., 2001) have also been identified as predictors, albeit somewhat inconsistently (Bennett et al., 2013; Kendall & Peterman, 2015; Knight et al., 2014).
Although clinical and sociodemographic characteristics captured in a clinical setting may be important, anxious youth also have difficulty with aspects of day-to-day functioning, including emotional reactivity and regulation, social interactions, and sleep (Walz, Nauta, & aan het Rot, 2014; Willis & Gregory, 2015). Anxiety treatments such as CBT and CCT aim to help youth generalize improvements beyond the clinic and enhance day-to-day functioning in a youth’s life. However, retrospective questionnaire measures about daily functioning are subject to recall and rater biases, may not sufficiently capture nuances in the quality of social and emotional functioning, and also cannot tap into the complex dynamic emotional processes that anxious youth experience. Thus, real-time measures of day-to-day functioning merit consideration as predictors and moderators of treatment outcome. Prior research suggests that the mean and variability of day-to-day negative and positive emotions (Forbes et al., 2012; Mor et al., 2010), emotional reactivity and regulation in response to negative events (Tan et al., 2012), parental and social interactions (Oppenheimer et al., 2016; Beidel, Turner, & Morris, 1999; Guyer et al., 2008), and sleep (Alfano, Pina, Zerr, & Villalta, 2010; Brent et al., 2008; Cousins et al., 2011; McMakin & Alfano, 2015; McMakin et al., 2016) play important roles in the daily lives of anxious youth. Both objective and subjective measures of day-to-day sleep are important to consider, as findings based on these two measurement types do not always correspond in youth with anxiety (Alfano, Patriquin, & De Los Reves, 2015) or adolescents more generally (Short et al., 2012).
The present study used data from the Child Anxiety Treatment Study (CATS), a randomized trial comparing two active therapies (CBT and CCT) for young adolescents with anxiety disorders (Silk et al, 2016). CATS employed ecological momentary assessment (EMA), daily sleep diaries, and actigraphy to capture emotions, events, social interactions, and sleep in the youth’s naturally-occurring social context. Using these data, we (1) explored predictors of treatment outcome, and (2) demonstrated the feasibility and potential utility of a recently developed “optimal combined moderator” statistical approach to identify and characterize subgroups of youth who may have a preferable outcome with CBT or, conversely, CCT. We use these results as a platform to generate hypotheses for potential ways to enhance and personalize anxiety treatment in youth.
Method
Participants
Participants in CATS were 133 youth aged 9–14 years, recruited through community advertisements or referrals, and required to meet DSM-IV (American Psychiatric Association, 1994) criteria for current GAD, SAD, and/or SocAD. Full study details are in Silk et al. (2016). We report on 114 youth who completed the post-treatment assessment (78 randomized to CBT and 36 randomized to CCT) because post-treatment data were required for calculation of the outcome variable. This sample includes N=8 youth (7%) who did not complete the treatment but who had a post-treatment assessment.
The 114 youth had a mean age of 11 (SD = 1.5). 89% were white, 56% were female, and 63% had at least one parent with a college degree. The mean baseline anxiety on the Pediatric Anxiety Rating Scale (PARS; RUPP Study Group, 2002) was 16.1 (SD = 4.7). 70% (N=80) of youth were diagnosed with GAD, 23% with SocAD (N=26), and 22% (N=25) with SAD. Some youth had additional comorbid diagnoses, as is typical in anxiety disordered youth (Kendall et al., 2010). The most commonly observed comorbid disorders were specific phobias (14%; N=16) and externalizing disorders (ADHD or ODD; 7%, N=8). Only 1 youth had a comorbid depressive disorder. There were no significant differences between the sample of 114 and the full sample of 133 with respect to these characteristics. A full baseline characterization of the analytic sample is provided in Supplemental Table 1.
Procedure
Following screening but before treatment randomization, youth completed diagnostic interviews, questionnaires, and rating scales. Also during this time, they completed five days of Ecological Momentary Assessment (EMA) to assess emotional functioning in daily life. In conjunction with the EMA study, youth also recorded sleep characteristics in a sleep diary each morning and wore an actigraph to capture behavioral aspects of sleep. Youth were then randomized to either CBT or CCT with a 2:1 ratio, which was used because the primary goal of the study was to explore mechanisms of change within CBT. Treatment was delivered by seven therapists, each of whom delivered both interventions to control for therapist characteristics. Therapists followed manualized CBT and CCT protocols that included 16 sessions (14 with the child and 2 with parent(s)). The University’s Institutional Review Board approved all study procedures.
Ecological Momentary Assessment Procedure
Prior to treatment, a cellular phone was used to obtain ecological momentary data on youths’ day-to-day emotions and behaviors using brief structured interviews. Calls began on Thursday after school and continued through Monday evening. Youth received two calls each day on weekdays and four calls each day on weekends, for a total of 14 calls. Calls were random within pre-specified 3-hour time windows and were conducted by trained research assistants. During each call, youth were asked to identify their momentary positive and negative emotions at the time of the call and identify individuals with whom they were interacting. They were also asked to indicate the most negative and positive events that occurred within the past hour (even if they were minor events). Youth were then asked to rate emotions associated with the “worst” event (peak negative affect) and coping strategies used (see Tan et al. 2012). Current and peak affect ratings were made using four negative (nervous, upset, sad, angry) and four positive items (excited, cheerful, interested, happy) based on previous research (Laurent et al., 1999; Silk et al., 2011). Emotions were rated on a scale from 1 (very slightly or not at all) to 5 (extremely). One of the 114 youth did not have any EMA data. Among the remaining 113, the mean number of calls with any observed data was 12.9 (SD = 1.4), ranging from 8 – 14.
Actigraphy and Sleep Diary Procedures
Each morning during the EMA protocol, youth completed a pencil-and-paper sleep diary in which they reported sleep characteristics of the previous night. Characteristics included bed time, wake time, sleep latency (minutes to fall asleep), wake after sleep onset (minutes awake after sleep onset), sleep quality (scale from 0 – 100, with higher values indicating higher quality), and ease of waking (scale from 0 – 100, with 100 indicating more ease). From this information, total sleep time (total minutes of sleep) and sleep efficiency (total sleep time / total time in bed × 100) each night were also calculated. The youth also wore an actigraph during the EMA protocol. Actigraphs are wristwatch-like devices that provide an estimate of the sleep/wake cycle via movement. They summarize the frequency of motions into epochs of specified time duration and store the summary in memory. These data are then downloaded and analyzed to generate various sleep parameters, including objective estimates of sleep midpoint, sleep latency, sleep efficiency, wake after sleep onset, and total sleep time. While actigraphs are similar to the more widely used “fitbit” wearable technology, fitbits have not yet been validated for sleep (Evenson et al., 2015).
Five nights of actigraphy data were captured from 78.9% (N=90) of the 114 youth, 1 – 4 nights were captured for 15.8% (N=18) of youth, and zero nights were captured for 5.3% (N=6) of youth. Five nights of sleep diary data were captured from 81.6% (N=93) of the 114 youth, 1–4 nights were captured for 14.9% (N=17) of youth, and zero nights were captured for 3.5% (N=4) of youth.
Potential Predictors and Moderators
In this exploratory study, we selected 80 potential predictors and moderators related to (1) EMA emotions, events, and social interactions, (2) diary and actigraphy sleep, and (3) clinical and demographic characteristics. These groups, and the variables within each group, were selected based on conceptual models, empirical findings on psychosocial treatment in youth with anxiety, available data, and examination of correlations and principal component analyses to reduce collinearity. Details and descriptive statistics of all potential predictors and moderators are included in Supplemental Table 1.
EMA emotions
Variables related to EMA emotions included: (1) means of current positive affect (PA), distress, and nervous emotions across EMA calls; (2) instabilities of current PA, distress, and nervous emotions across EMA calls; (3) means of peak distress and nervous emotions across EMA calls where negative events were reported; and (4) means of current PA, distress, and nervous emotions across EMA calls when with one’s mother and when alone. We focused on PA (mean of interested, happy, excited, and cheerful emotions), distress (mean of sad, upset, and angry emotions), and nervous emotions to reduce high collinearity among individual emotions and based on principal component analysis results suggesting these three factors. We only considered emotions when youth were with one’s mother and alone because: (1) emotions with other individuals (e.g., father, peer, sibling) were very highly correlated with emotions with mother, and (2) there was the least amount of missing data when considering emotions with their mother, as this variable could only be calculated for a youth if they were called while with the indicated person, and youth reported the most calls with their mother.
EMA events and social interactions
At each EMA call, youth were asked to indicate who they were currently interacting with, the most positive and negative event that occurred in the past hour (even if they were minor), and how the youth responded to the event. Variables related to these prompts included: (1) proportion of calls with various individuals (mother, father, sibling, peer, alone); (2) responses to negative events (e.g., use of coping strategies, talking about the event, feeling control over the event); (3) reporting one or more negative events within a given category (worry, interpersonal, motivation, loss, achievement); and (4) reporting one or more positive events within a given category (academic, peer, screen, leisure, family). Positive and negative event categories were selected because they contained the events types most frequently endorsed by youth.
Sleep characteristics
Our analyses included the means of both actigraphy and sleep diary sleep latency, sleep efficiency, wake after sleep onset, and total sleep time, as well as the mean sleep quality and ease of waking from sleep diary. Because adolescence is a time known for disparate sleep across weekdays and weekends, we considered using weekend- or weekday-specific means or other estimates that capture variability. However, we ultimately chose to use just the means across all nights for multiple reasons. First, prior research in indicates that 5 nights of actigraphy is required for adequate reliability in our sample of youth (Acebo et al., 1999). As such, including all available weekday and weekend data increased reliability. Second, some data were collected during summer months when some youth have schedule mornings and others do not. Therefore, a simple weekday/weekend split would not necessarily have captured schedule changes perfectly. For this reason, we considered including estimates of night-to-night within-subject variability across the measurement period. These estimates of variability were very highly correlated with the means. Thus, in an effort to reduce the number of baseline characteristics evaluated – as well as to prioritize interpretability—we ultimately decided to use only the mean characteristics. Additional characterization of the youth’s sleep (means and variability across all days, weekend- and weekday-specific means) is provided in Supplemental Table 2.
Clinical measures and other self-report questionnaires
Questionnaires considered were: the PARS (RUPP Study Group, 2002), Family Assessment Device subscales and total score (FAD; Epstein, Baldwin, & Bishop, 1983), parental- and child-rated depression (Mood and Feelings Questionnaire, MFQ; Angold, Erkanli, Silberg, Eaves, & Costello, 2002), Quick Inventory of Depressive Symptomology (QIDS; Rush et al., 2003), parental trait anxiety (State-Trait Anxiety Inventory; Spielberger et al., 1983), and the Children’s Sleep Habits questionnaire subscales and total score (CSH; Owens, Spirito, & McGuinn, 2000). Parental diagnostic characteristics were indicators for mother’s lifetime anxiety and depression. Child diagnostic characteristics were indicators for the presence of GAD, SAD, SocAD, and externalizing disorders (presence of ODD and/or ADHD), as well as total number of DSM-IV anxiety diagnosis. The total number of DSM-IV anxiety diagnoses ranged from 1 – 4 and included GAD, SAD, SocAD, Specific Phobia, and Panic Disorder.
Demographic characteristics
Age in years, race, gender, total household income, parental marital status, and parental college education were each considered as potential predictors and moderators.
Treatment Outcome
Independent evaluators (IEs) blind to treatment assignment used the PARS to rate anxiety severity pre- and post-treatment (after session 16). A total score was computed by summing six items (anxiety severity, frequency, distress, avoidance, and interference) as experienced by the youth during the previous week. We used the percent change in PARS from pre- to post-treatment as our primary outcome, as the combined moderator method requires a single continuous measure of treatment response. Scores greater than zero reflect a reduction in anxiety.
Statistical Analysis
For interpretability, continuous baseline measures were standardized and dichotomous baseline measures were coded as .5 and −.5. Similarly, treatment was coded as .5 for CBT and −.5 for CCT (Kraemer & Blasey, 2004). Given the exploratory nature of our work, we followed recommendations by the American Statistical Association and focused on effect sizes (ESs) rather than p-values (Wasserstein & Lazar, 2016). Therefore, for each baseline characteristic, we used non-parametric Spearman correlations to calculate ESs for predictors and moderators (denoted rp and rm, respectively) using methods described by Kraemer (2013). Non-parametric Spearman correlation effect sizes allow for non-continuous and non-normal predictors and moderators and reduce the influence of extreme observations. After considering the range of observed moderator and predictor ESs generated by the baseline variables, we chose an ES cutoff of |.15| to define moderators and predictors. That is, we considered a baseline variable to be a moderator if rm > |.15|, and considered it to be a non-specific predictor if rp > |.15| and it was also not identified as a moderator. This cutoff is similar to cutoffs in previously published applications of the combined moderator method (e.g., see Frank et al., 2015; Smagula et al., 2016; Wallace et al., 2013). We also calculated 95% bootstrap simultaneous confidence intervals (SCIs) based on 10,000 replications for the predictor and moderator effect sizes of the characteristics meeting the minimum ES threshold of |.15|. These 95% SCIs control the Type-I error rate in the context of multiple comparisons (Mandel & Betensky, 2008).
We followed previously published methods (Kraemer, 2013; Smagula et al., 2016; Wallace et al, 2013) to develop an optimal combined moderator of the treatment effect on percent reduction in anxiety. This approach uses multivariable regression to estimate weights for each moderator, with the weights representing the extent to which each moderator distinguishes individual outcome differences between those in CBT versus CCT in context of the other moderators. After the weights are estimated, they are extracted and subsequently used to calculate a single optimal combined moderator, M*, for each individual. Similar to Smagula et al. (2016), we used LASSO regression (Least Absolute Shrinkage and Selection Optimizer; Tibshirani, 1996) to estimate weights in M*. LASSO regression allows for a large number of potentially correlated individual variables to be included in a model without overfitting. This is operationalized by automatically shrinking the weights of the least useful variables (e.g., those that are more highly correlated with other individual variables and/or not predictive), thereby optimizing predictive accuracy. After calculating M* using the estimated LASSO weights, we calculated its moderator ES (rm) and 95% bootstrap confidence interval based on 10,000 replications. We identified the value of M* at which the predicted outcomes for CBT and CCT groups crossed one another, indicating a different preferred treatment for those above or below the cross point. Within the subgroups above and below this cross point, we calculated Cohen’s d treatment effect sizes with 95% bootstrap confidence intervals.
We used stratified threefold cross-validation, repeated ten times, to estimate the potetnial predictive abilities of the combined moderator in an independent sample. Within each of the ten repititions, threefold cross-validation randomly divides the sample into 3 training/testing sets that each have a 2:1 ratio of CBT to CCT as in the original data. One-third of the data is removed (the “testing set”), and the remaining 2/3 of the data (the “training set”) is used to identify moderators with rm > |.15|, obtain weights for M*, and determine the cross point at which the predicted lines cross. This model is then used to predict M* for each individual in the testing set and, subsequently, classify them as having CBT preferable to CCT (CBT>CCT) or vice versa (CCT>CBT) depending on whether their M* value is above or below the identified cross point. The moderator ES and the treatment ESs within the subgroups above and below the identified cross point are then calculated for the testing set. This procedure is followed three times within a single repitition (leaving a different 1/3 of the data out each time), with ten total repititions, resulting in a total of thirty sets of moderator and treamtment ES estimates. To ensure sufficient sample size within each testing data set, we only considered variables with < 5% missing data.
Results
In our exploratory search, ten variables were identified as predictors (Table 1), all with small correlation ESs (rp magnitudes ranging from 0.15 to 0.28). EMA-derived measures indicated that greater positive affect when interacting with one’s mother, a greater percentage of calls in which the youth was alone, and not reporting a worry-related negative concern at any of the calls were all associated with a greater percent reduction in anxiety. Longer sleep (reported by parents retrospectively and captured objectively through actigraphy) also predicted a greater percent reduction in anxiety. Other measures indicated that a lower parent-reported depression score, a higher baseline anxiety score, not having a mother with a lifetime history of depression, being younger, and being male were associated with a greater percent reduction in anxiety.
Table 1.
Predictors of treatment outcome. Positive effect sizes (ESs) indicate greater reduction in anxiety as the predictor increases. Negative ESs indicate greater reduction in anxiety as the predictor decreases. SCI = simultaneous confidence interval adjusted for 16 moderators and predictors.
| Predictors | Correlation ES (95% SCI) | N |
|---|---|---|
| PA when with mother (EMA) | 0.28 (−0.03, 0.54) | 101 |
| Problems with Sleep Duration (CSH) | −0.24 (−0.49, 0.05) | 109 |
| Female | −0.23 (−0.48, 0.05) | 114 |
| Anxiety (PARS) | 0.23 (−0.04, 0.47) | 114 |
| Total sleep time in minutes (actigraphy) | 0.22 (−0.06, 0.47) | 108 |
| Proportion of calls interacting with no one (EMA) | 0.19 (−0.08, 0.45) | 113 |
| Maternal lifetime depression diagnosis | −0.17 (−0.44, 0.10) | 112 |
| At least 1 worry-related negative concern (EMA) | −0.17 (−0.43, 0.12) | 113 |
| Parent-rated child depressive symptoms (MFQ) | −0.17 (−0.43, 0.13) | 111 |
| Child age | −.15 (−.41, 0.12) | 114 |
Abbreviations: PA = positive affect, EMA = ecological momentary assessment, CSH = childhood sleep habits questionnaire; PARS = pediatric anxiety rating scale; MFQ = moods and feelings questionnaire.
Six variables were identified as potential moderators (Table 2), all with small correlation ESs (rm magnitudes ranging from 0.16 to 0.24). These individual moderators were: total number of anxiety DSM-IV diagnoses, sleep quality (daily sleep diary), ease of waking (daily sleep diary), sleep efficiency (daily sleep diary), parental college education, and reporting an interpersonal negative concern (i.e., related to peers, family, and/or loneliness) through EMA. 109 youth had complete data on all six moderators. The six moderators and ten predictors were relatively independent of one another, with a median (Q1, Q3) magnitude correlation of 0.08 (0.04, 0.14) and a maximum magnitude correlation of 0.49 (from diary sleep quality and diary sleep efficiency). The estimated weights for the combined moderator M* are provided in Table 2. The correlation ES (95% CI) for M* was rm = 0.41 (0.23, 0.57). In comparison, the ES of the largest individual moderator ES (total number of DSM-IV anxiety diagnoses) was rm = 0.24, 95% SCI = (−0.09, 0.53) and the ES from a combined moderator based on only clinical and sociodemographic characteristics (total number of DSM-IV anxiety diagnoses and parental education) was rm=0.28, 95% CI = (0.08, 0.48).
Table 2.
Moderators of treatment outcome and weights for the combined moderator, M*. Positive moderator effect sizes indicate that CBT becomes more preferable to CCT as the value of the moderator increases. Negative effect sizes indicate that CCT becomes more preferable to CBT as the value of the moderator increases. SCI = simultaneous confidence interval adjusted for 16 moderators and predictors.
| Moderators | Correlation ES (95% SCI) | N | Weight in M* |
|---|---|---|---|
| Total number of anxiety DSM-IV diagnoses | .24 (−.09, .53) | 114 | 25.13 |
| Mean sleep quality (Daily Sleep Diary) | −.19 (−.45, .11) | 110 | −.78 |
| At least 1 parent with college degree | .18 (−.11, .46) | 114 | 9.26 |
| Mean SE (Daily Sleep Diary) | .18 (−.14, .47) | 110 | 9.15 |
| At least 1 interpersonal negative event (EMA) | .18 (−.09, .47) | 113 | 9.57 |
| Mean ease of waking (Daily Sleep Diary) | −.16 (−.40, .11) | 110 | −13.9 |
Abbreviations: EMA = ecological momentary assessment; SE = sleep efficiency, transformed as log(100 – SE + 1) for normality, such that higher values of the transformed variable indicate worse SE and lower values indicate higher SE.
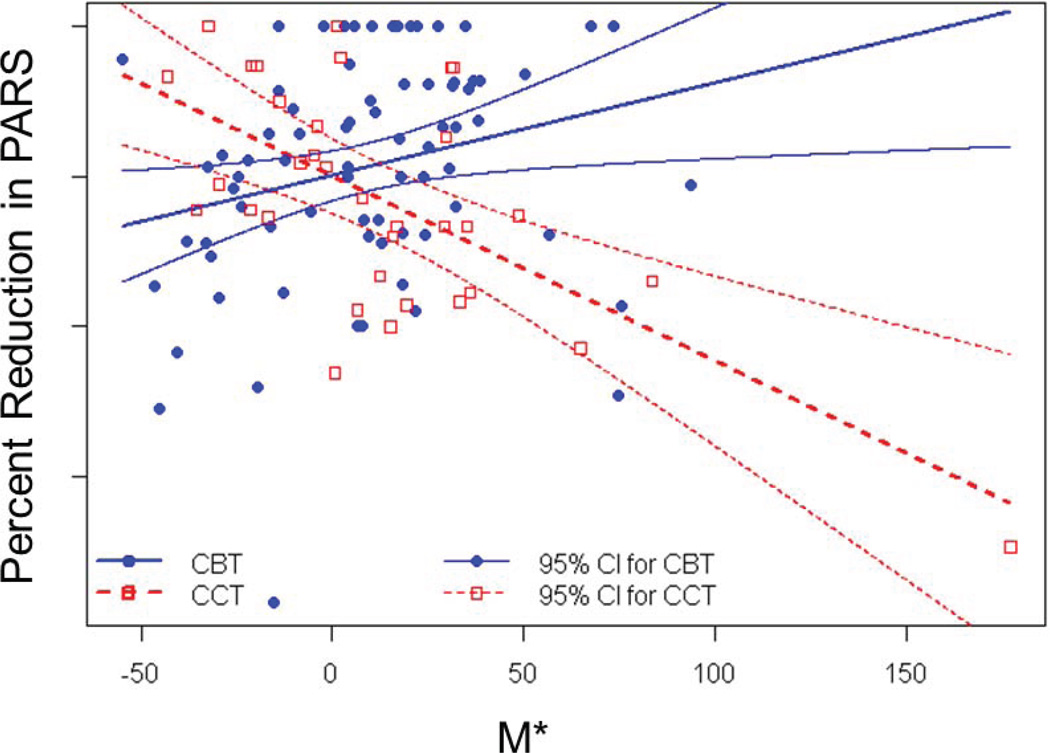
Figure 1 illustrates the predicted outcomes for CBT and CCT across the observed range of M* as well as the point at which the two predicted lines cross (M* = −0.21). Above the cross-point, CBT was strongly preferable to CCT [d (95% CI) = 0.93 (0.37, 1.63), N=70]. Below the cross-point, CCT was strongly preferable to CBT [d (95%CI) = −0.71 (−1.33, −0.25), N=39]. In contrast, the treatment ES in the overall sample was small, leaning in favor of CBT [d (95% CI) = 0.32 (−0.04, 0.73)]. There was one influential yet valid outlier in the combined moderator model. However, similar inference was made after removing this observation [M* rm (95% CI) =0.36 (0.17, 0.52); CBT>CCT subgroup d (95% CI)=0.86 (0.31, 1.55), N=69; CCT>CBT subgroup d (95% CI) = −0.80 (−1.37, −0.28), N=39].
Figure 1.
Predicted outcomes (with 95% confidence intervals) for cognitive behavioral therapy (CBT) and child-centered therapy (CCT) across the range of the combined moderator, M*
Table 3 compares the CBT>CCT and CCT>CBT subgroups as defined by M*. The 39 youth for whom CCT>CBT tended to have only one DSM-IV anxiety diagnosis (the minimum requirement for the study), higher mean sleep quality, more ease of waking, higher sleep efficiency, were less likely to have had a parent with a college degree, and were less likely to have had negative event related to an interpersonal concern. Conversely, the 70 youth for whom CBT > CCT tended to have more DSM-IV anxiety diagnoses, lower sleep quality, less ease of waking, lower sleep efficiency, were more likely to have a parent with a college degree, and were more likely to have a negative event related to an interpersonal concern. Cohen’s d ESs indicated that the CBT>CCT and CCT>CBT groups differed on each of these measures with at least a small ES (|d| range = 0.25 to 0.90).
Table 3.
Characteristics of subgroups revealed by the optimal combined moderator, M*, and Cohen’s d effect size comparisons with 95% simultaneous confidence intervals (SCIs) across the six comparisons. SCIs are based on 10,000 bootstrap samples.
| Moderator | M* < −.21 (CCT > CBT) N=39 |
M* > −.21 (CBT > CCT) N=70 |
Cohen’s d (95% SCI) comparing subgroups |
|---|---|---|---|
| Total number of DSM-IV Anxiety Diagnoses, mean (SD) | 1.03 (0.16) | 1.47 (0.61) | 0.90 (0.55, 1.34) |
| Mean sleep quality (Daily Sleep Diary) , mean (SD) | 74.25 (18.11) | 62.29 (16.96) | −0.69 (−1.34, −0.14) |
| At least 1 parent with college degree, %(n) | 35.9 (14) | 61.4 (43) | 0.52 (0.00, 1.08) |
| Mean SE (Daily Sleep Diary), mean(SD) | 1.35 (0.45) | 1.67 (0.53) | 0.62 (0.13, 1.18) |
| At least 1 interpersonal negative event (EMA), %(n) | 48.7 (19) | 90.0 (63) | 0.95 (0.45, 1.52) |
| Mean ease of waking (Daily Sleep Diary), mean (SD) | 73.35(18.79) | 57.9(19.94) | −0.79 (−1.40, −0.26) |
Abbreviations: EMA = ecological momentary assessment; SE = sleep efficiency, transformed as log(100 – SE + 1) for normality, such that higher values of the transformed variable indicate worse SE and lower values indicate higher SE
Based on the 30 internal cross-validation samples, the combined moderator correlation ES was small [mean (SD) rm =0.16 (0.12)]. The mean (SD) treatment ES above the cut point was moderate [d = 0.50 (0.37)] and in favor of CBT versus CCT. However, the mean (SD) treatment ES below the cut point was negligible [d =0.10 (0.54)] indicating no difference in CBT versus CCT. Thus, as is often the case, there was an attenuation of the ESs when the model was used for prediction. In an independent sample similar to the one used herein, a youth with M*>-0.21 may be expected to have a greater percent reduction in anxiety on CBT than CCT, whereas a youth with M*<-0.21 may be expected to have a similar outcome on either CCT or CBT.
Discussion
This study used a recently developed statistical approach to explore how measures of day-to-day sleep and emotional/social functioning predict or moderate treatment outcome in anxious youth. Novel EMA predictors of a better outcome regardless of treatment included higher PA when with one’s mother and fewer worry-related negative events. Both are suggestive of better day-to-day functioning. Moreover, having higher PA when with one’s mother could be an asset for both CBT and CCT because it allows the youth to benefit from feeling supported while experiencing anxiety and may also buffer emotional reactivity to negative peer events (Oppenheimer et al., 2016). Total sleep time, captured through both a self-report questionnaire and actigraphy, is also a notable predictor in the context of literature suggesting that shorter sleep leads to poor attention, emotion regulation, and memory consolidation; these features may exacerbate symptoms and interfere with treatment engagement and learning (Shochat, Cohen-Zion, & Tzischinsky, 2014). Our findings that greater baseline depression severity, presence of maternal lifetime depression, and older age are related to worse treatment outcome mirror some previous findings (Curry et al., 2006; Lundkvist-Houndoumani et al., 2014).
Some predictor findings were unexpected. Higher baseline anxiety predicted better outcome; however, this is likely explained by the fact that our outcome was percent reduction in anxiety (as opposed to total reduction in anxiety or post-treatment anxiety), and as such, greater anxiety at baseline allows for a larger percent reduction in anxiety. The finding that a greater proportion of EMA calls where the youth was alone was related to greater anxiety reduction was also unexpected. This may be an indication of a youth having more independence and perhaps experiencing fewer anxiety-reinforcing interactions with family and friends (e.g., co-rumination, accommodation, amplifying of distress), although further investigation is warranted. Finally, some characteristics found to be important in previous studies (e.g., social anxiety disorder, parental anxiety disorder, externalizing disorders) were not shown to be important in the present study. Given the exploratory nature of our study and relatively large SCIs that contained zero, we emphasize the importance of replicating these findings in an independent sample.
The novel combined moderator analyses suggested that youth for whom CBT>CCT (M* > −0.21) tended to have more DSM-IV anxiety diagnoses, worse daily self-reported sleep (quantified through sleep quality, ease of waking, and sleep efficiency), interpersonal negative events reported through EMA, and college-educated parents. Structured CBT provides youth with specific cognitive restructuring strategies that may apply not only to daytime worries and ruminations, but also to worries and ruminations at bedtime, which are very common in anxious youth and are associated with problems with sleep (Caporino et al., 2015; Hiller, Lovato, Gradisar, Oliver, & Slater, 2014; Peterman et al., 2016; Peterman, Carper, & Kendall, 2015). However, CBT does require advanced cognitive and verbal skills on behalf of the youth, and asks parents to help youth practice the use of coping strategies. Thus, the youth with college educated parents may have an advantage in CBT treatment. Our internal cross-validation upheld the finding that youth with greater values of M* may have a preferable outcome on CBT relative to CCT.
Youth in our sample for whom CCT>CBT (M* < −0.21) tended to have only one DSM-IV anxiety diagnosis, better sleep, no interpersonal negative events reported through EMA, and non-college educated parents. These youth were generally less severe clinically and had fewer problems with day-to-day functioning (e.g., “worried well”). Because they were less likely to have college educated parents, a psychotherapy that does not require as much parental involvement or cognitive/verbal skills (such as CCT) may be beneficial. However, in our internal cross-validation, the youth with lower values of M* had similar outcomes on CBT and CCT.
Our results indicate that both day-to-day functioning and clinical measures play an important role in understanding which youth will respond to CBT and/or CCT. Four of ten predictors were day-to-day measures, and the strongest predictor was mean day-to-day positive affect when with ones’ mother, as measured through EMA. The strongest individual moderator was a traditional clinical interview measure (total number of DSM-IV anxiety diagnoses); however, four of the six individual moderators we identified were measures of day-to-day functioning. The combined moderator ES including both day-to-day and traditional clinical/sociodemographic measures was rm= 0.41 (0.23, 0.57). This ES dropped to rm=0.28 (0.08, 0.48) when the day-to-day measures were excluded. Thus, these data support the utility of including day-to-day measures of functioning along with more traditional measures in future analyses.
Our findings provide a platform for generating hypotheses for new and enhanced treatment strategies. Sleep characteristics were among the strongest predictors and moderators. Because past research has indicated that sleep is actually modifiable in adults with a brief targeted intervention (Troxel, Germain, & Buysse, 2012), and recent trials with adolescents also show promise (Gradisar et al., 2011, Bei et al., 2013), it may prove to be a prime target for enhancing and personalizing treatment. Surprisingly, given its level of influence in our findings and its longstanding association with affective psychopathology (Gregory & Sadeh, 2012), sleep is rarely considered as a predictor or moderator of anxiety treatment response. Therefore, sleep deserves greater attention and can provide important treatment information. For example, our findings suggest that it will be important to assess and address problems with total sleep time prior to beginning either CBT or CCT. If a youth has other sleep problems related to quality and efficiency and CBT is not available, a possible treatment strategy may be to treat their sleep first and then begin a different available psychotherapy (similar to CCT), or use a multi-pronged approach to target sleep simultaneous to other anxiety symptoms.
Also important in the context of developing and testing new treatment strategies is the finding that higher positive affect with one’s mother was the strongest predictor of treatment outcome on either CBT or CCT. This finding is particularly interesting given conflicting data on the added value of incorporating a family component into CBT (Barmish & Kendall, 2005; Drake & Ginsburg, 2012; Manassis et al., 2014). Our finding suggests that continuing to investigate treatment strategies for improving interpersonal relationships with mothers (and potentially other family members) in the context of anxiety treatment is a worthwhile endeavor.
Beyond generating hypotheses for developing and enhancing treatments, the optimal combined moderator we present also has potential for informing personalized treatment decisions in practice because it provides clinicians with a stronger and more consistent treatment indication than if individual moderators were used. Internal cross-validation indicated that the weights we estimated could be used to calculate M* for a new youth from a similar sample as the one used herein. If M* > −0.21, the youth may require CBT. If M* <-0.21, the youth may have a similar outcome on CCT or CBT. In the latter case, availability or preference may be used to guide the treatment decision between CBT and CCT. However, we emphasize that a number of additional steps are required before this type of predictive model could actually be widely used in community practice. It will be important to: (a) develop ways to modify EMA and diary measures so that they can be more easily obtained in a clinical setting; (b) perform similar analyses that include other common pediatric anxiety treatment options such as SSRIs and/or combination therapies, and (c) externally validate the estimated weights and cut-point in a new, independent sample. If these steps were completed, a clinician could capture a youth’s relevant baseline information and then use a handheld computer to apply the weights derived herein to calculate the youth’s M* value and determine whether they were likely to have a preferable outcome on CBT or CCT.
Our findings should be considered in the context of limitations. An inherent limitation is the hypothesis-generating and exploratory nature of the study. However, we took a number of steps to ensure proper communication and utility of this approach. First, we focus on effect sizes rather than p-values, as suggested by the American Statistical Association (Wasserstein & Lazar, 2016) and Kraemer (2013). While we do provide 95% simultaneous confidence intervals (SCIs) for ESs to keep the type-I error rate at 0.05 across multiple confidence intervals, these SCIs are meant to provide a degree of variability surrounding the ES rather than a definitive indication of which characteristics are or are not “important” in this sample. Second, we focus on results from an optimal combined moderator rather than multiple individual moderators. To this end, we note that we don’t overly emphasize which specific variables have higher or lower weights in the combined moderator, but rather assert that we are unlikely to be overfitting too much given our use of the LASSO. Third, we internally validate our exploratory findings using cross-validation. Our cross-validation results suggest that continued application and validation of the optimal combined moderator method has the potential to lead the field towards personalized treatment decisions for anxiety. However, we emphasize that the weights and cut-point presented herein must be rigorously externally validated outside this specific sample in order to assess its generalizability and usefulness in an applied setting of personalized treatment in the community.
There are limitations in the outcome variable, percent change in PARS from pre- to post-treatment. We chose to use continuous percent change in PARS as our outcome, rather than a dichotomous variable such as remission, because: (1) percent change in PARS was the a priori outcome selected for the CATS project broadly; (2) continuous outcomes contain the most heterogeneity to be explained through moderators, and thus tend to allow for the greatest moderator effect sizes (Kraemer, 2013), and (3) the optimal combined moderator approach requires a continuous outcome (Kraemer, 2013), although we are currently developing methods to extend this approach to other outcomes. We also note that the CATS study observed PARS at post-treatment as well as at 1-year follow-up. However, as is the case for most clinical trials, there was some attrition at year 1 follow-up such that the complete data sample size would have become too low to confidently apply the optimal combined moderator method. Therefore, we focused on percent change in PARS from pre- to post- treatment so that we could best demonstrate the feasibility and utility of the optimal combined moderator approach. Further analyses should be performed to determine whether the predictors and moderators of post-treatment outcome are reflective of the outcome at one-year follow-up as well as other outcomes such as change in parent- and child-reported symptoms.
Finally, the optimal combined moderator presented herein is novel in that it was developed based on self-reported and behavioral characteristics of day-to-day functioning as well as clinical and sociodemographic measures. These characteristics were chosen for several reasons, including the fact that measurement of these characteristics in order to inform treatment personalization is feasible. However, the consideration of other biological and physiological characteristics (e.g., genetics, electroencephalography, functional magnetic resonance imaging) that are more challenging to measure in a clinical setting could also inform our understanding of which factors predispose youth to have a stronger response to either treatment (i.e., predictors), or a stronger response to CBT versus supportive therapies (i.e., moderators).
Supplementary Material
Day-to-day PA with one’s mother and sleep duration were among predictors
CBT was indicated for youth with >1 DSM anxiety diagnoses and poor sleep quality
CBT was also indicated for youth with college-educated parents
Sleep may be an important modifiable factor for personalizing treatment
Acknowledgments
This research was supported by the following National Institute of Mental Health grants: MH063747, MH086438, HD080097 (Kendall, PI), K01 MH096944 (Wallace, PI), P50 MH080215 (Ryan, PI), K23 MH092400 (McMakin, PI). Support for research participant recruitment was also provided by the Clinical and Translational Science Institute at the University of Pittsburgh (NIH/NCRR/CTSA Grant UL1 RR024153).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Acebo C, Sadeh A, Seifer R, Tzischinsky O, Wolfson AR, Hafer A, Carskadon MA. Estimating sleep patterns with activity monitoring in children and adolescents: how many nights are necessary for reliable measures? Sleep. 1999;22(1):95–103. doi: 10.1093/sleep/22.1.95. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV. 4th. Washington, D.C: American Psychiatric Association; 1994. [Google Scholar]
- Alfano CA, Patriquin MA, De Los Reves A. Subjective-objective sleep comparisons and discrepancies among clinically-anxious and healthy children. Journal of Abnormal Child Psychology. 2015;43(7):1343–1353. doi: 10.1007/s10802-015-0018-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfano CA, Pina AA, Zerr AA, Villalta IK. Pre-sleep arousal and sleep problems of anxiety-disordered youth. Child Psychiatry & Human Development. 2010;41(2):156–167. doi: 10.1007/s10578-009-0158-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angold A, Erkanli A, Silberg J, Eaves L, Costello EJ. Depression scale scores in 8–17 year olds: Effects of age and gender. Journal of Child Psychology and Psychiatry. 2002;43(8):1052–1063. doi: 10.1111/1469-7610.00232. [DOI] [PubMed] [Google Scholar]
- Barmish AJ, Kendall PC. Should parents be co-clients in cognitive-behavioral therapy for anxious youth? Journal of Clinical Child and Adolescent Psychology. 2005;34(3):569–581. doi: 10.1207/s15374424jccp3403_12. [DOI] [PubMed] [Google Scholar]
- Bei B, Byrne ML, Ivens C, Waloszek J, Woods MJ, Dudgeon P, Allen NB. Pilot study of a mindfulness-based, multi-component, in-school group sleep intervention in adolescent girls. Early intervention in psychiatry. 2013;7(2):213–220. doi: 10.1111/j.1751-7893.2012.00382.x. [DOI] [PubMed] [Google Scholar]
- Beidel DC, Turner SM, Morris TL. Psychopathology of childhood social phobia. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38(6):643–650. doi: 10.1097/00004583-199906000-00010. [DOI] [PubMed] [Google Scholar]
- Bennett K, Manassis K, Walter SD, Cheung A, Wilansky Traynor P, Diaz Granados N, Barrett P. Cognitive behavioral therapy age effects in child and adolescent anxiety: An individual patient data metaanalysis. Depression and Anxiety. 2013;30(9):829–841. doi: 10.1002/da.22099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berman SL, Weems CF, Silverman WK, Kurtines WM. Predictors of outcome in exposure-based cognitive and behavioral treatments for phobic and anxiety disorders in children. Behavior Therapy. 2000;31(4):713–731. [Google Scholar]
- Bodden DH, Dirksen CD, Bögels SM. Societal burden of clinically anxious youth referred for treatment: A cost-of-illness study. Journal of Abnormal Child Psychology. 2008;36(4):487–497. doi: 10.1007/s10802-007-9194-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent D, Emslie G, Clarke G, Wagner KD, Asarnow JR, Keller M, Abebe K. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: The TORDIA randomized controlled trial. JAMA. 2008;299(8):901–913. doi: 10.1001/jama.299.8.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caporino NE, Read KL, Shiffrin N, Settipani C, Kendall PC, Compton SN, Keeton C. Sleep-related problems and the effects of anxiety treatment in children and adolescents. Journal of Clinical Child & Adolescent Psychology. 2015:1–11. doi: 10.1080/15374416.2015.1063429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JA, Deblinger E, Mannarino AP, Steer RA. A multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(4):393–402. doi: 10.1097/00004583-200404000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP, Iyengar S. Community treatment of posttraumatic stress disorder for children exposed to intimate partner violence: A randomized controlled trial. Archives of Pediatrics & Adolescent Medicine. 2011;165(1):16–21. doi: 10.1001/archpediatrics.2010.247. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP, Knudsen K. Treating sexually abused children: 1 year follow-up of a randomized controlled trial. Child Abuse & Neglect. 2005;29(2):135–145. doi: 10.1016/j.chiabu.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Compton SN, Peris TS, Almirall D, Birmaher B, Sherrill J, Kendall PC, Rynn MA. Predictors and moderators of treatment response in childhood anxiety disorders: Results from the CAMS trial. Journal of Consulting and Cinical Psychology. 2014;82(2):212. doi: 10.1037/a0035458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cousins JC, Whalen DJ, Dahl RE, Forbes EE, Olino TM, Ryan ND, Silk JS. The bidirectional association between daytime affect and nighttime sleep in youth with anxiety and depression. Journal of Pediatric Psychology. 2011;36(9):969–979. doi: 10.1093/jpepsy/jsr036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawley SA, Beidas RS, Benjamin CL, Martin E, Kendall PC. Treating socially phobic youth with CBT: Differential outcomes and treatment considerations. Behavioural and Cognitive Psychotherapy. 2008;36(04):379–389. [Google Scholar]
- Curry J, Rohde P, Simons A, Silva S, Vitiello B, Kratochvil C, Pathak S. Predictors and moderators of acute outcome in the Treatment for Adolescents with Depression Study (TADS) Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45(12):1427–1439. doi: 10.1097/01.chi.0000240838.78984.e2. [DOI] [PubMed] [Google Scholar]
- Drake KL, Ginsburg GS. Family factors in the development, treatment, and prevention of childhood anxiety disorders. Clinical Child and Family Psychology Review. 2012;15(2):144–162. doi: 10.1007/s10567-011-0109-0. [DOI] [PubMed] [Google Scholar]
- Epstein NB, Baldwin LM, Bishop DS. The McMaster family assessment device. Journal of Marital and Family Therapy. 1983;9(2):171–180. [Google Scholar]
- Evenson KR, Goto MM, Furberg RD. Systematic review of the validity and reliability of consumer-wearable activity trackers. International Journal of Behavioral Nutrition and Physical Activity. 2015;12:159. doi: 10.1186/s12966-015-0314-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes EE, Stepp SD, Dahl RE, Ryan ND, Whalen D, Axelson DA, Silk JS. Real-world affect and social context as predictors of treatment response in child and adolescent depression and anxiety: An ecological momentary assessment study. Journal of Child and Adolescent Psychopharmacology. 2012;22(1):37–47. doi: 10.1089/cap.2011.0085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank E, Wallace ML, Hall M, Hasler B, Levenson JC, Janney CA, Ritchey FC. An Integrated Risk Reduction Intervention can reduce body mass index in individuals being treated for bipolar I disorder: Results from a randomized trial. Bipolar Disorders. 2015;17(4):424–437. doi: 10.1111/bdi.12283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gradisar M, Dohnt H, Gardner G, Paine S, Starkey K, Menne A, Trenowden S. A randomized controlled trial of cognitive-behavior therapy plus bright light therapy for adolescent delayed sleep phase disorder. Sleep. 2011;34(12):1671–1680. doi: 10.5665/sleep.1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg PE, Sisitsky T, Kessler RC, Finkelstein SN, Berndt ER, Davidson JR, Fyer AJ. The economic burden of anxiety disorders in the 1990s. Journal of Clinical Psychiatry. 1999 doi: 10.4088/jcp.v60n0702. [DOI] [PubMed] [Google Scholar]
- Gregory AM, Sadeh A. Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Medicine Reviews. 2012;16(2):129–136. doi: 10.1016/j.smrv.2011.03.007. [DOI] [PubMed] [Google Scholar]
- Guyer AE, Lau JY, McClure-Tone EB, Parrish J, Shiffrin ND, Reynolds RC, et al. Amygdala and ventrolateral prefrontal cortex function during anticipated peer evaluation in pediatric social anxiety. Archives of General Psychiatry. 2008;65(11):1303–1312. doi: 10.1001/archpsyc.65.11.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herres J, Cummings CM, Swan A, Makover H, Kendall PC. Moderators and mediators of treatments for youth with anxiety. In: Maric M, Prins PJM, Ollendick TH, editors. Moderators and mediators of youth treatment outcomes. New York: Oxford University Press; 2015. [Google Scholar]
- Hiller RM, Lovato N, Gradisar M, Oliver M, Slater A. Trying to fall asleep while catastrophising: What sleep-disordered adolescents think and feel. Sleep Medicine. 2014;15(1):96–103. doi: 10.1016/j.sleep.2013.09.014. [DOI] [PubMed] [Google Scholar]
- Hudson JL, Kendall PC, Coles ME, Robin JA, Webb A. The other side of the coin: Using intervention research in child anxiety disorders to inform developmental psychopathology. Development and Psychopathology. 2002;14(04):819–841. doi: 10.1017/s095457940200408x. [DOI] [PubMed] [Google Scholar]
- Hudson JL, Rapee RM, Lyneham HJ, McLellan LF, Wuthrich VM, Schniering CA. Comparing outcomes for children with different anxiety disorders following cognitive behavioural therapy. Behaviour Research and Therapy. 2015;72:30–37. doi: 10.1016/j.brat.2015.06.007. [DOI] [PubMed] [Google Scholar]
- James AA, Soler A, Weatherall RR. Cognitive behavioural therapy for anxiety disorders in children and adolescents. The Cochrane Library. 2005 doi: 10.1002/14651858.CD004690.pub2. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Compton SN, Walkup JT, Birmaher B, Albano AM, Sherrill J, Gosch E. Clinical characteristics of anxiety disordered youth. Journal of Anxiety Disorders. 2010;24(3):360–365. doi: 10.1016/j.janxdis.2010.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall PC, Hudson JL, Gosch E, Flannery-Schroeder E, Suveg C. Cognitive-behavioral therapy for anxiety disordered youth: A randomized clinical trial evaluating child and family modalities. Journal of Consulting and Clinical Psychology. 2008;76(2):282. doi: 10.1037/0022-006X.76.2.282. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Peterman JS. CBT for adolescents with anxiety: Mature yet still developing. American Journal of Psychiatry. 2015;172(6):519–530. doi: 10.1176/appi.ajp.2015.14081061. [DOI] [PubMed] [Google Scholar]
- Kerns CM, Read KL, Klugman J, Kendall PC. Cognitive behavioral therapy for youth with social anxiety: Differential short and long-term treatment outcomes. Journal of Anxiety Disorders. 2013;27(2):210–215. doi: 10.1016/j.janxdis.2013.01.009. [DOI] [PubMed] [Google Scholar]
- Knight A, McLellan L, Jones M, Hudson J. Pre-treatment predictors of outcome in childhood anxiety disorders: A systematic review. Psychopathology Review. 2014;1(1):77–129. [Google Scholar]
- Kovacs M, Devlin B. Internalizing disorders in childhood. Journal of Child Psychology and Psychiatry. 1998;39(1):47–63. [PubMed] [Google Scholar]
- Kraemer HC. Discovering, comparing, and combining moderators of treatment on outcome after randomized clinical trials: A parametric approach. Statistics in Medicine. 2013;32(11):1964–1973. doi: 10.1002/sim.5734. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Blasey CM. Centring in regression analyses: A strategy to prevent errors in statistical inference. International Journal of Methods in Psychiatric Research. 2004;13(3):141–151. doi: 10.1002/mpr.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langley AK, Bergman RL, McCracken J, Piacentini JC. Impairment in childhood anxiety disorders: Preliminary examination of the child anxiety impact scale-parent version. Journal of Child and Adolescent Psychopharmacology. 2004;14(1):105–114. doi: 10.1089/104454604773840544. [DOI] [PubMed] [Google Scholar]
- Laurent J, Catanzaro SJ, Joiner TE, Jr, Rudolph KD, Potter KI, Lambert S, Gathright T. A measure of positive and negative affect for children: scale development and preliminary validation. Psychological Assessment. 1999;11(3):326. [Google Scholar]
- Lundkvist-Houndoumadi I, Hougaard E, Thastum M. Pre-treatment child and family characteristics as predictors of outcome in cognitive behavioural therapy for youth anxiety disorders. Nordic Journal of Psychiatry. 2014;68(8):524–535. doi: 10.3109/08039488.2014.903295. [DOI] [PubMed] [Google Scholar]
- Manassis K, Lee TC, Bennett K, Zhao XY, Mendlowitz S, Duda S, Barrett P. Types of parental involvement in CBT with anxious youth: A preliminary meta-analysis. Journal of Consulting and Clinical Psychology. 2014;82(6):1163. doi: 10.1037/a0036969. [DOI] [PubMed] [Google Scholar]
- Mandel M, Betensky RA. Simultaneous confidence intervals based on the percentile bootstrap approach. Computational Statistics & Data Analysis. 2008;52(4):2158–2165. doi: 10.1016/j.csda.2007.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMakin DL, Alfano CA. Sleep and anxiety in late childhood and early adolescence. Current Opinion in Psychiatry. 2015;28(6):483–489. doi: 10.1097/YCO.0000000000000204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMakin DL, Dahl RE, Buysse DJ, Cousins JC, Forbes EE, Silk JS, Franzen PL. The impact of experimental sleep restriction on affective functioning in social and nonsocial contexts among adolescents. Journal of Child Psychology and Psychiatry. 2016 doi: 10.1111/jcpp.12568. [DOI] [PubMed] [Google Scholar]
- Mor N, Doane LD, Adam EK, Mineka S, Zinbarg RE, Griffith JW, Nazarian M. Within-person variations in self-focused attention and negative affect in depression and anxiety: A diary study. Cognition and Emotion. 2010;24(1):48–62. [Google Scholar]
- Ollendick TH, Jarrett MA, Grills-Taquechel AE, Hovey LD, Wolff JC. Comorbidity as a predictor and moderator of treatment outcome in youth with anxiety, affective, attention deficit/hyperactivity disorder, and oppositional/conduct disorders. Clinical Psychology Review. 2008;28(8):1447–1471. doi: 10.1016/j.cpr.2008.09.003. [DOI] [PubMed] [Google Scholar]
- Oppenheimer CW, Ladouceur CD, Waller JM, Ryan ND, Allen KB, Sheeber L, Silk JS. Emotion socialization in anxious youth: Parenting buffers emotional reactivity to peer negative events. Journal of Abnormal Child Psychology. 2016:1–12. doi: 10.1007/s10802-015-0125-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens JA, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): Psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23(8):1043–1052. [PubMed] [Google Scholar]
- Peterman JS, Carper MM, Elkins RM, Comer JS, Pincus DB, Kendall PC. The effects of cognitive-behavioral therapy for youth anxiety on sleep problems. Journal of Anxiety Disorders. 2016;37:78–88. doi: 10.1016/j.janxdis.2015.11.006. [DOI] [PubMed] [Google Scholar]
- Peterman JS, Carper MM, Kendall PC. Anxiety disorders and comorbid sleep problems in school-aged youth: Review and future research directions. Child Psychiatry & Human Development. 2015;46(3):376–392. doi: 10.1007/s10578-014-0478-y. [DOI] [PubMed] [Google Scholar]
- Rapee R. The influence of comorbidity on treatment outcome for children and adolescents with anxiety disorders. Behaviour Research and Therapy. 2003;41(1):105–112. doi: 10.1016/s0005-7967(02)00049-9. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Lyneham HJ, Hudson JL, Kangas M, Wuthrich VM, Schniering CA. Effect of comorbidity on treatment of anxious children and adolescents: results from a large, combined sample. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52(1):47–56. doi: 10.1016/j.jaac.2012.10.002. [DOI] [PubMed] [Google Scholar]
- Research Units on Peadiatric Psychopharmacology Anxiety Study Group. The pediatric anxiety rating scale (PARS): Development and psychometric properties. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41(9):11061–1069. doi: 10.1097/00004583-200209000-00006. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, et al. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry. 2003;54(5):573–583. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- Schleider JL, Ginsburg GS, Keeton CP, Weisz JR, Birmaher B, Kendall PC, Walkup JT. Parental psychopathology and treatment outcome for anxious youth: Roles of family functioning and caregiver strain. Journal of Consulting and Clinical Psychology. 2015;83(1):213. doi: 10.1037/a0037935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shochat T, Cohen-Zion M, Tzischinsky O. Functional consequences of inadequate sleep in adolescents: a systematic review. Sleep Medicine Reviews. 2014;18(1):75–87. doi: 10.1016/j.smrv.2013.03.005. [DOI] [PubMed] [Google Scholar]
- Short MA, Gradisar M, Lack LC, Wright H, Carskadon MA. The discrepancy between actigraphic and sleep diary measures of sleep in adolescents. Sleep Medicine. 2012;13(4):378–384. doi: 10.1016/j.sleep.2011.11.005. [DOI] [PubMed] [Google Scholar]
- Shortt AL, Barrett PM, Fox TL. Evaluating the FRIENDS program: A cognitive-behavioral group treatment for anxious children and their parents. Journal of Clinical Child Psychology. 2001;30(4):525–535. doi: 10.1207/S15374424JCCP3004_09. [DOI] [PubMed] [Google Scholar]
- Silk JS, Forbes EE, Whalen DJ, Jakubcak JL, Thompson WK, Ryan ND, Dahl RE. Daily emotional dynamics in depressed youth: A cell phone ecological momentary assessment study. Journal of experimental child psychology. 2011;110(2):241–257. doi: 10.1016/j.jecp.2010.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silk JS, Tan PZ, Ladouceur CD, Meller S, Siegle GJ, McMakin DL, Mannarino A. A randomized clinical trial comparing individual cognitive behavioral therapy and child-centered therapy for child anxiety disorders. Journal of Clinical Child & Adolescent Psychology. 2016:1–13. doi: 10.1080/15374416.2016.1138408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smagula SF, Wallace ML, Anderson SJ, Karp JF, Lenze EJ, Mulsant BH, Lotrich FE. Combining moderators to identify clinical profiles of patients who will, and will not, benefit from aripiprazole augmentation for treatment resistant late-life major depressive disorder. Journal of Psychiatric Research. 2016;81:112–118. doi: 10.1016/j.jpsychires.2016.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southam-Gerow MA, Kendall PC, Weersing VR. Examining outcome variability: Correlates of treatment response in a child and adolescent anxiety clinic. Journal of Clinical Child Psychology. 2001;30(3):422–436. doi: 10.1207/S15374424JCCP3003_13. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- Swan A, Kendall PC. Fear and missing out: Youth anxiety and functional outcomes. Clinical Psychology: Science and Practice. 2016 [Google Scholar]
- Tan PZ, Forbes EE, Dahl RE, Ryan ND, Siegle GJ, Ladouceur CD, Silk JS. Emotional reactivity and regulation in anxious and nonanxious youth: a cell phone ecological momentary assessment study. Journal of Child Psychology and Psychiatry. 2012;53(2):197–206. doi: 10.1111/j.1469-7610.2011.02469.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tibshirani R. Regression shrinkage and selection via the lasso. Journal of the Royal Statistical Society. Series B (Methodological) 1996:267–288. [Google Scholar]
- Troxel WM, Germain A, Buysse DJ. Clinical management of insomnia with brief behavioral treatment (BBTI) Behavioral Sleep Medicine. 2012;10(4):266–279. doi: 10.1080/15402002.2011.607200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, Waslick B. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. New England Journal of Medicine. 2008;359(26):2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace ML, Frank E, Kraemer HC. A novel approach for developing and interpreting treatment moderator profiles in randomized clinical trials. JAMA psychiatry. 2013;70(11):1241–1247. doi: 10.1001/jamapsychiatry.2013.1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walz LC, Nauta MH, aan het Rot M. Experience sampling and ecological momentary assessment for studying the daily lives of patients with anxiety disorders: A systematic review. Journal of Anxiety Disorders. 2014;28(8):925–937. doi: 10.1016/j.janxdis.2014.09.022. [DOI] [PubMed] [Google Scholar]
- Wasserstein RL, Lazar NA. The ASA’s statement on p-values: Context, process, and purpose. The American Statistician. 2016 [Google Scholar]
- Weisz JR, Weiss B, Han SS, Granger DA, Morton T. Effects of psychotherapy with children and adolescents revisited: A meta-analysis of treatment outcome studies. Psychological Bulletin. 1995;117(3):450. doi: 10.1037/0033-2909.117.3.450. [DOI] [PubMed] [Google Scholar]
- Willis TA, Gregory AM. Anxiety disorders and sleep in children and adolescents. Sleep Medicine Clinics. 2015;10(2):125–131. doi: 10.1016/j.jsmc.2015.02.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.