Abstract
Background:
Use of MRI with diffusion-weighted imaging (DWI) can identify infarcts in 30%–50% of patients with TIA. Previous guidelines have indicated that MRI-DWI is the preferred imaging modality for patients with TIA. We assessed the frequency of MRI utilization and predictors of MRI performance.
Methods:
A review of TIA and minor stroke patients evaluated at Veterans Affairs hospitals was conducted with regard to medical history, use of diagnostic imaging within 2 days of presentation, and in-hospital care variables. Chart abstraction was performed in a subset of hospitals to assess clinical variables not available in the administrative data.
Results:
A total of 7,889 patients with TIA/minor stroke were included. Overall, 6,694 patients (84.9%) had CT or MRI, with 3,396/6,694 (50.7%) having MRI. Variables that were associated with increased odds of CT performance were age >80 years, prior stroke, history of atrial fibrillation, heart failure, coronary artery disease, anxiety, and low hospital complexity, while blood pressure >140/90 mm Hg and high hospital complexity were associated with increased likelihood of MRI. Diplopia (87% had MRI, p = 0.03), neurologic consultation on the day of presentation (73% had MRI, p < 0.0001), and symptom duration of >6 hours (74% had MRI, p = 0.0009) were associated with MRI performance.
Conclusions:
Within a national health system, about 40% of patients with TIA/minor stroke had MRI performed within 2 days. Performance of MRI appeared to be influenced by several patient and facility-level variables, suggesting that there has been partial acceptance of the previous guideline that endorsed MRI for patients with TIA.
In recent years, it has been recognized that some patients with transient neurologic symptoms will have ischemic brain lesions demonstrated with sophisticated imaging methods.1,2 Therefore, due to the presence of tissue damage, it has been proposed that patients with imaging evidence of infarction, despite transient symptoms, should be classified as having had a stroke instead of TIA.3 A committee of the American Stroke Association also proposed that for patients with symptoms suggestive of a TIA, MRI with diffusion-weighted imaging (DWI) is the preferred imaging modality due to increased sensitivity for detection of acute ischemic brain lesions.3
Detection of ischemic lesions in patients with transient symptoms can be useful in the identification of patients at increased short-term risk of stroke.4–7 In addition, visualization of the ischemic lesion can clarify the anatomical location of the patient's symptoms and may help elucidate the mechanism of the ischemic process (e.g., atherothrombotic, embolic).8
Performance of brain MRI for patients with stroke has increased by over 200% in relative terms during 1999–2008.9 Brain MRI has drawbacks, including anxiety for some patients, increased health care costs,9 and potential discovery of incidental abnormalities.10,11 Widespread adoption of MRI for TIA/minor stroke could require reconfiguration of neuroimaging services.
We sought to assess how frequently MRI was performed for patients with TIA and minor stroke and whether there were patient- or hospital-level predictors of MRI performance. We evaluated utilization patterns with the Veterans Affairs (VA) system, where there are no predefined radiology protocols for brain imaging and clinicians can select their preferred test with no cost constraints.
METHODS
Patients with TIA or minor stroke who were cared for in either the emergency department (ED) or inpatient setting during fiscal year 2011 were identified (n = 8,427) using ICD-9 primary discharge codes for TIA (435.0, 435.1, 435.3, 435.8, 435.9) or stroke (433.X1, 434.00, 434.X1, and 436). As described elsewhere, because electronic health record data did not include a measure of stroke severity, a validated approach to identify major stroke patients was employed. Patients with stroke were classified as having major stroke if any of the following were present: length of stay >6 days, ventilator use, feeding tube use, coma, intensive care unit stay, inpatient rehabilitation stay prior to discharge, or receipt of thrombolysis. Because our goal was to create a cohort of patients with TIA and minor stroke, patients with major stroke were excluded. We further excluded patients who were admitted from a non-VA hospital (n = 84), who left against medical advice (n = 100), who were discharged to hospice (n = 2), who were transferred to another facility within 2 days (n = 336), or who died within 2 days (n = 18). Among the 7,889 patients eligible for inclusion, an additional 1,195 patients were excluded from the predictive models because they had a pacemaker (n = 523) or did not receive imaging within 2 days of presentation (n = 1,072), leaving an analytic cohort of 6,694.
Data collected from this study are described more fully elsewhere.12 In brief, the VA Medical SAS datasets were used to obtain information on demographics, medical history, and health care utilization, including data on cranial imaging. Data from the VA Corporate Data Warehouse provided information on blood pressure (BP) and other patient risk factors, such as smoking history. Facility-specific data were obtained from VA internal program offices regarding emergency medicine and neurology staffing and hospital complexity, which classifies facilities into 3 levels based on a combination of patient characteristics, clinical services offered, educational and research missions, and administrative complexity. Information on services offered in the ED (e.g., CT availability) were obtained from a national VA-wide survey of ED medical directors.12
A separate, detailed electronic medical chart review of patients at select high-volume VA hospitals (a 35% random sample of facilities with at least 50 TIA or minor stroke patients in fiscal year 2011) was performed by trained abstractors to obtain clinical factors (e.g., symptom duration) that were not available from the administrative data. Patients were included in this medical record review if they had a diagnosis of either TIA or ischemic stroke. Patients with ischemic stroke who had a NIH Stroke Scale of ≤2 at the time of presentation were considered to have minor stroke and were therefore included.
Statistical methods.
Demographic, medical history, Charlson Comorbidity Index, and ED/hospitalization descriptors were compared between those who received MRI and those who received CT without MRI by using χ2, Fisher exact test, or Wilcoxon rank-sum test. Differences in facility characteristics were also compared using these same tests.
A predictive model using administrative data was built for performance of MRI (present or absent). For the development group, two-thirds of the sample was randomly chosen and the remaining third was used for validation. Bivariate logistic regression models were used to assess associations between patient and facility characteristics and the log odds ratio of receiving MRI in 2 days. The logistic model included a random intercept for facility, which was incorporated into the model for the correlation of patients from the same hospital. Clinically important variables were selected for inclusion in a multivariable logistic model regardless of statistical significance in bivariate models. These were age, race, history of stroke, myocardial infarction (MI), atrial fibrillation (AF), congestive heart failure (CHF), and dementia. Other covariates were chosen based on a variable selection method; if they were significant at the 0.25 level in bivariate models, they were eligible for inclusion into the multivariable regression model. Backwards variable selection was used with staying criteria of 0.05 to eliminate variables. The C-statistic for the resulting model was calculated. The resulting model was fit to the validation sample and the C-statistic was reported as a measure of model performance. Analyses were generated using SAS/STAT software, version 9.2, of the SAS System for Windows (SAS Institute, Cary, NC). Institutional review board approval was obtained.
RESULTS
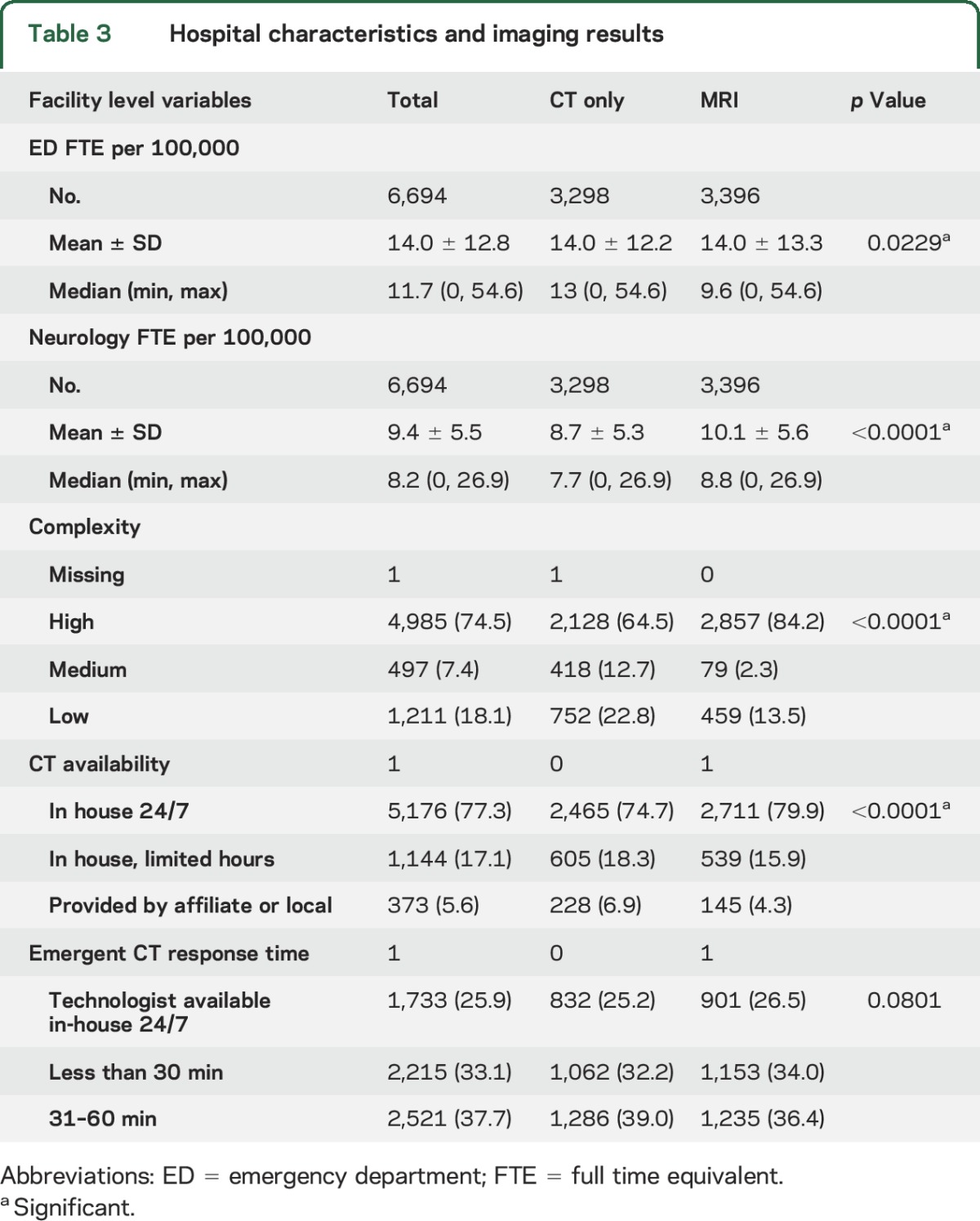
A total of 8,427 patients with TIA or minor stroke were cared for in a VA ED or inpatient setting in fiscal year 2011. We examined imaging among the 7,889 patients eligible for analysis. A total of 6,694 (84.9%) had cranial imaging (either CT or MRI) performed within 2 days of presentation (table 1), with 3,298 (49.3%) having CT without MRI and 3,396 (50.7%) having MRI. Using the administrative data, we saw in bivariate analyses that the clinically important variables that were selected a priori were significantly associated with CT performance rather than MRI: age >80 years (58.6% with CT only, 41.4% MRI), prior stroke (54.5% CT, 45.5% MRI), prior MI (56.7% vs 43.3%), AF (60.5% CT, 39.5% MRI), dementia (62.6% CT, 37.4% MRI), and CHF (58.3% CT, 41.7% MRI) (p < 0.0001 for each; table 1). Among hospital characteristics, greater availability of CT on a 24/7 basis, higher hospital complexity, and greater neurology staffing levels were associated with increased MRI performance (tables 2 and 3). Between fiscal year 2011 and fiscal year 2014, the use of MRI without CT increased from 9.7% in 2011 to 12.0% in 2014 (p < 0.0001). The use of brain or carotid imaging was slightly higher for TIA patients compared to minor stroke (93.0% vs 86.3%, p < 0.0001).
Table 1.
Comparison of baseline characteristics between those who received MRI vs CT without MRI (within 2 days of event) for TIA/minor stroke using administrative data
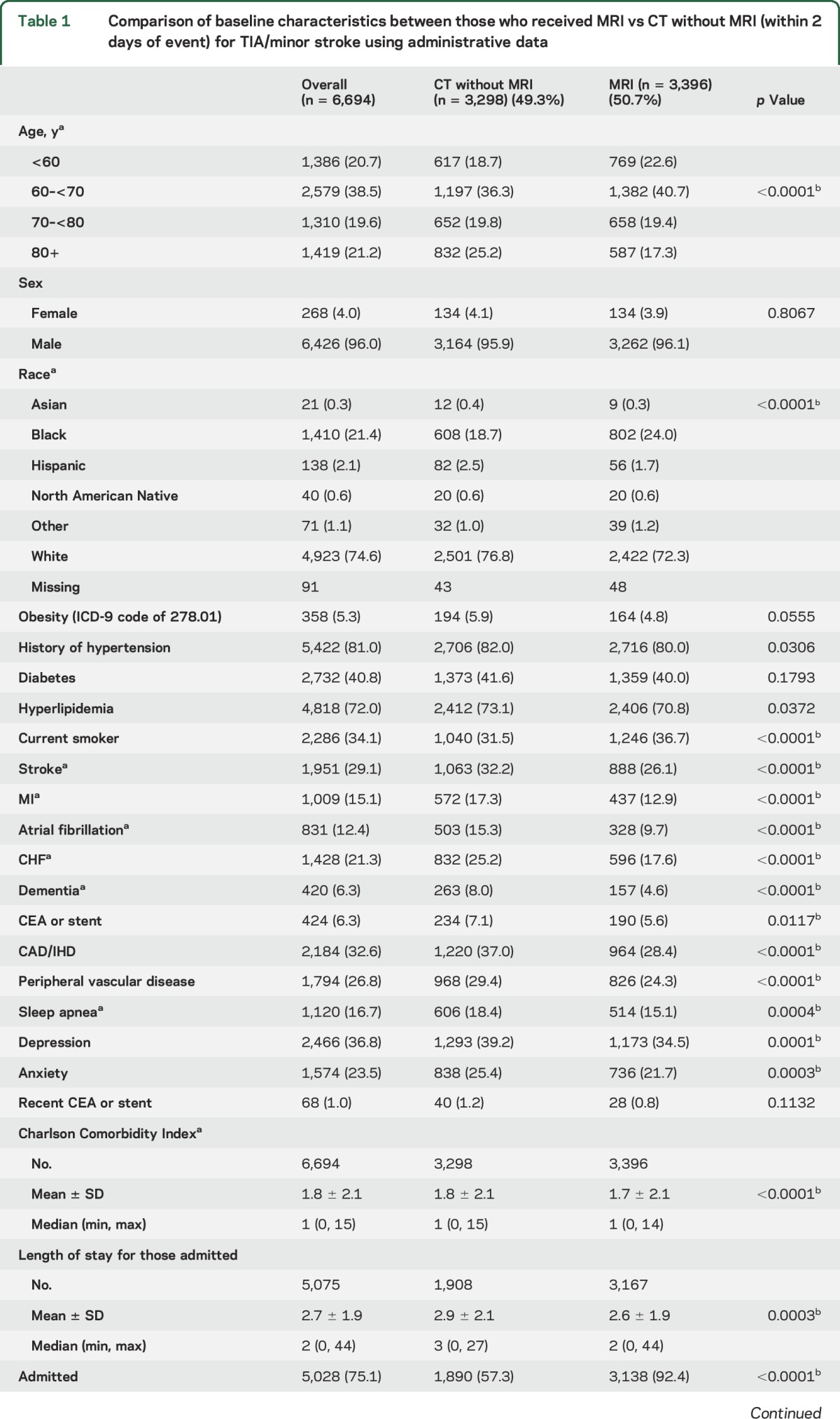
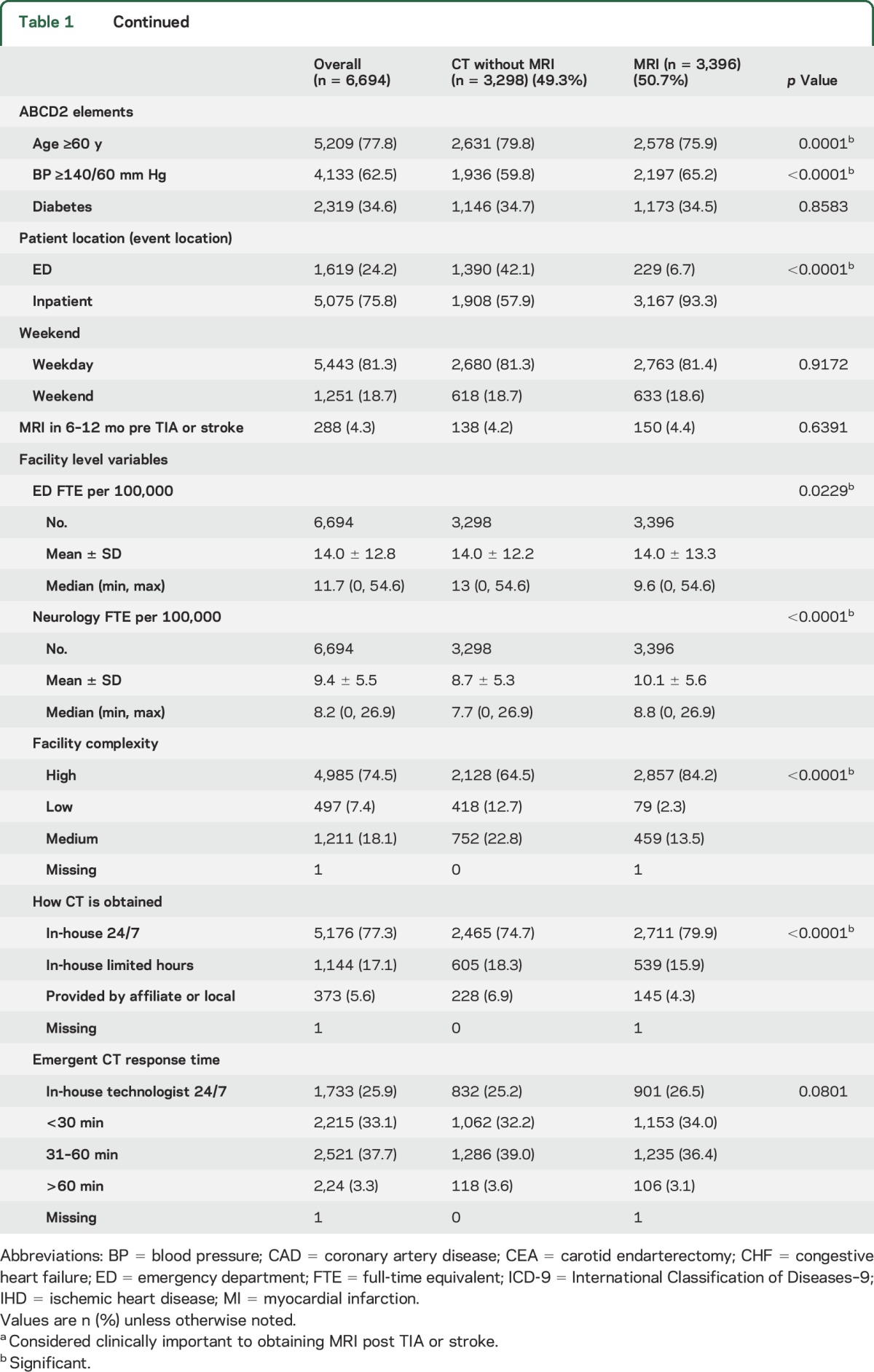
Table 2.
Bivariate and multivariable model for MRI from development sample (n = 4,418)
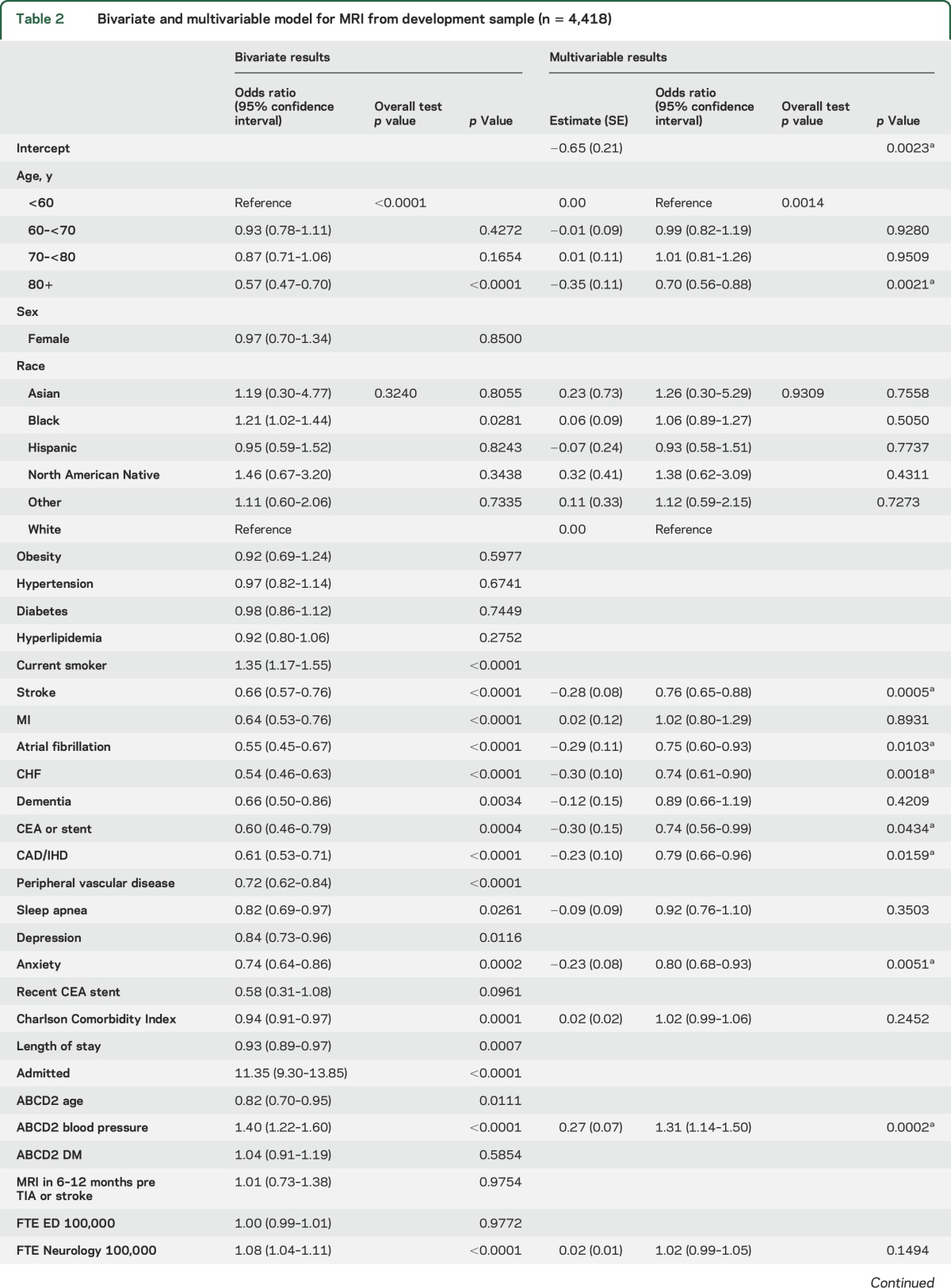
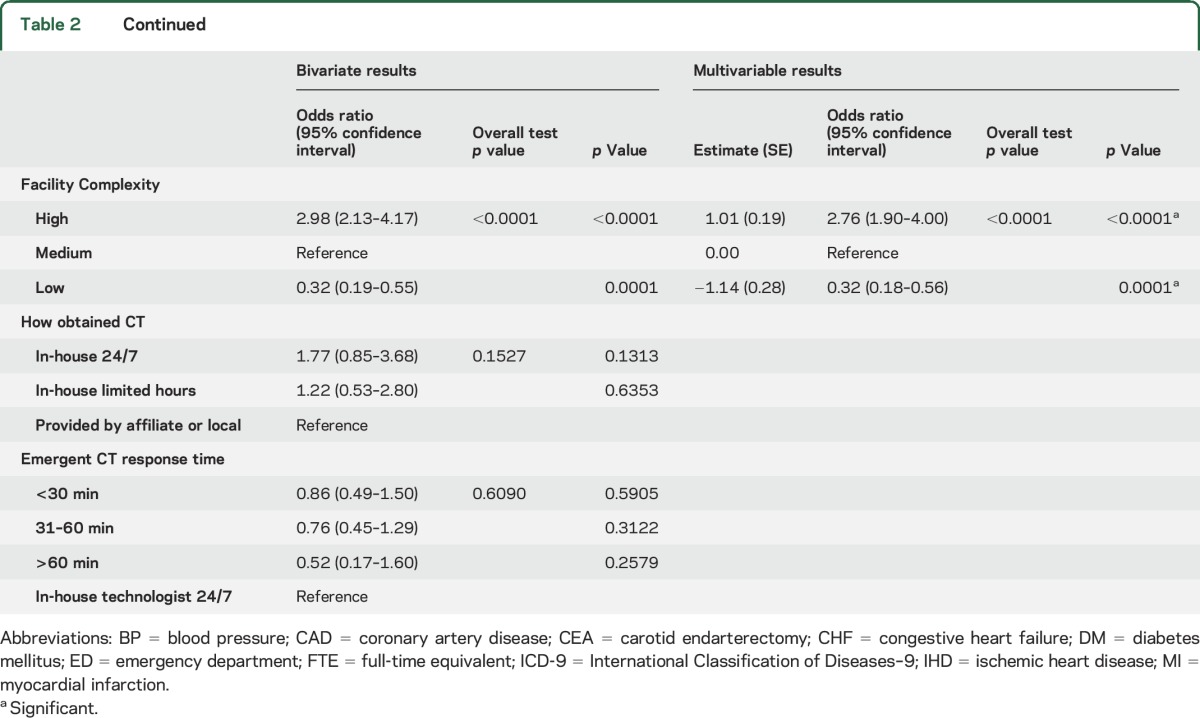
Table 3.
Hospital characteristics and imaging results
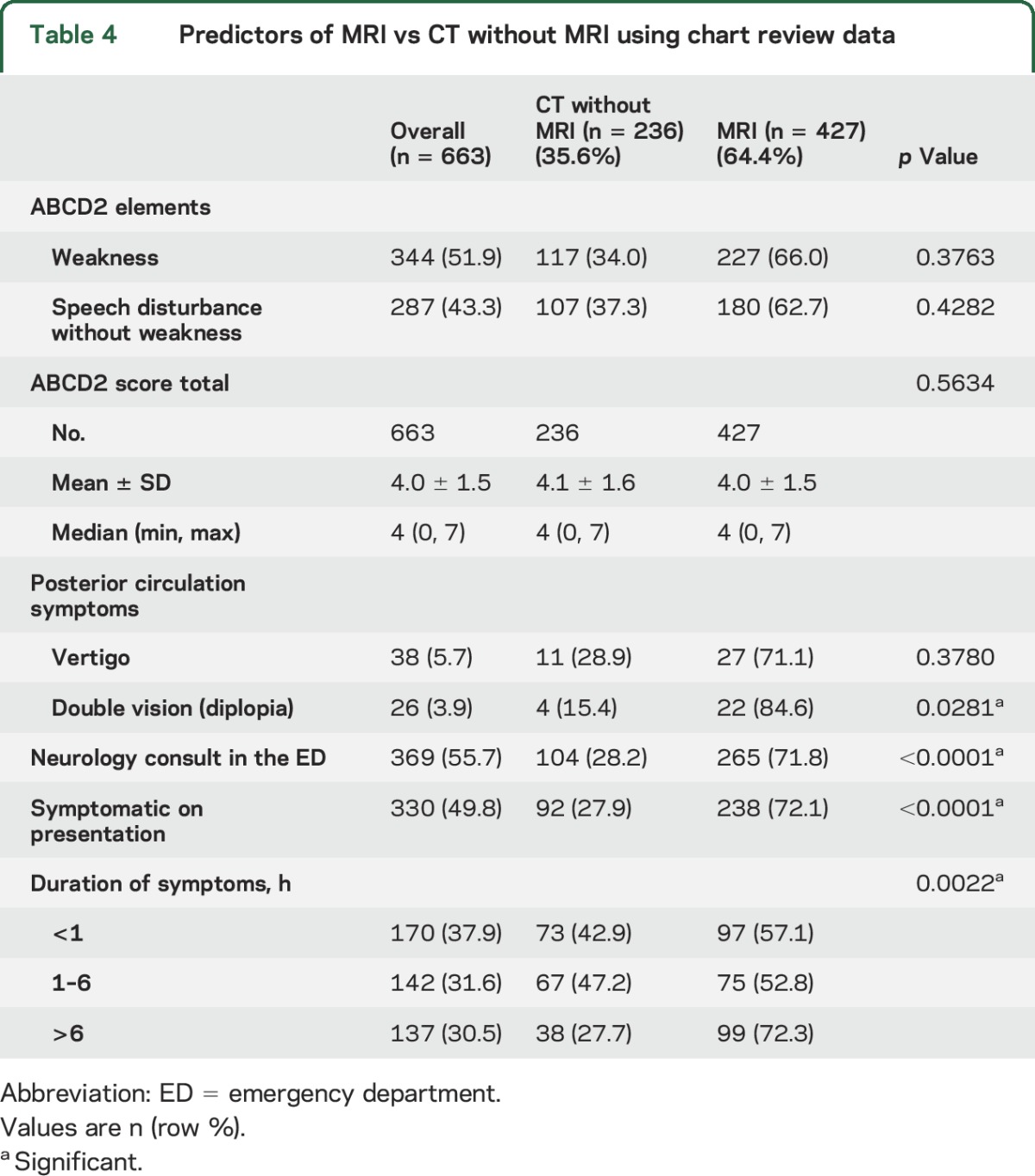
On chart review, diplopia as a complaint (87% with diplopia had MRI vs 13% CT only, p = 0.03), neurologic consultation at presentation (73% had MRI vs 27% CT only, p < 0.0001), and symptom duration of >6 hours (7% had MRI vs 26% CT only, p = 0.0009) were associated with MRI performance (table 4). Other symptoms such as weakness, speech disturbance, or vertigo were not associated with MRI performance.
Table 4.
Predictors of MRI vs CT without MRI using chart review data
The multivariable modeling fit to the development set included age, race, prior stroke, prior MI, history of AF, CHF, dementia, sleep apnea, Charlson Comorbidity Index, history of carotid endarterectomy (CEA) or stent, coronary artery disease/ischemic heart disease (CAD/IHD), anxiety, ABCD2 score for BP ≥140/90 mm Hg, neurologist availability (number of full-time equivalent employees per 100,000 patients), and hospital complexity. Explanatory variables associated with increased likelihood of MRI were BP ≥140/90 mm Hg and high hospital complexity, while age >80 years, prior stroke, AF, CHF, history of CEA or stent, CAD/IHD, anxiety, and low hospital complexity were associated with decreased likelihood of MRI. When this model was fit to the validation set, AF, dementia, sleep apnea, and low hospital complexity were associated with reduced likelihood of receiving a MRI, while neurologist availability and high hospital complexity were associated with an increased chance of MRI performance. The C-statistic for the development sample was 0.74 and for the validation set was 0.76.
DISCUSSION
We sought to determine the extent to which MRI is being performed for patients with TIA and minor stroke within a large, national integrated health system. We found that MRI was performed within 2 days of initial presentation in about 51% of patients in whom imaging was performed. Several clinical features were more common among patients who were imaged with CT only, whereas other patient and facility characteristics were more frequent among patients receiving MRI.
In terms of patient features that were more frequent in the population with CT only, several characteristics were indicative of greater comorbidity burden. Elderly patients, those with prior stroke, those with dementia, and those with AF or CHF were all more likely to have a CT only. This may reflect the treating physician's desire to not burden a sick population with excessive testing. In addition, if the patient's functional status is limited, then the results of MRI may not influence treatment decisions.13 A previous study from a German TIA registry also found that younger patients and patients without AF were more likely to have a brain MRI performed.14
The chart review portion of the analysis found that diplopia was more frequent in patients who had an MRI. Diplopia as a manifestation of TIA or stroke suggests ischemia in the vertebrobasilar circulation, especially in the midbrain or pons. Because the areas supplied by the vertebral and basilar arteries, particularly the brainstem and cerebellum, are better visualized with MRI as opposed to CT, it makes clinical sense to prefer imaging with MRI in patients with diplopia as a presenting complaint.15 The clinical yield of imaging in patients with new-onset, isolated diplopia has been questioned, however. In a series of 93 patients over age 50 years with new onset of diplopia and no other neurologic abnormalities, only one patient had a relevant lesion on MRI.16
Involvement of neurologists was more common in patients who underwent brain MRI. In previous stroke studies, involvement of neurologists was associated with better outcomes but more extensive testing, especially ordering of brain MRI scans.17 It is possible that neurologists are more aware of clinical guidelines recommending MRI for patients with TIA-like presentations and that neurologists are more cognizant of the relationship between ischemic lesions on DWI and future stroke risk.18 In a recent multicenter study of patients with TIA or minor stroke, MRI was performed in 58.5% of patients and multiple acute infarcts were associated with a higher rate of recurrent cerebrovascular events.19
Patients with symptom duration of more than 6 hours were more likely to receive brain imaging with MRI. This could be due to the fact that longer-lasting symptoms are more likely to have an imaging correlate on brain MRI.3,8 In addition, patients with longer-lasting symptoms are more likely to be admitted to the hospital, which could in turn lead to additional diagnostic testing.
Our study has several limitations. First, the larger administrative dataset did not allow us to ascertain some clinical variables that may have influenced the imaging strategy, such as whether the symptoms were referable to the anterior or posterior circulation; these variables were available only in the smaller chart review component. Second, some facilities within the large VA system lack access to MRI on a 7-day-per-week basis, which may have affected the imaging choices. Third, the administrative database did not allow us to determine the clinical utility of having the MRI in addition to CT.13 In addition, the available data do not indicate whether DWI was routinely done as part of the MRI protocol. The study results are generalizable to medium and large community hospitals in the United States but they may not be generalizable to comprehensive stroke centers that have continuous MRI availability. Finally, there may be other confounding variables that affected choice of imaging tests that we were not able to evaluate, such as clinician views on the value of MRI in patients with TIA-like symptoms.20
We found in a national, integrated health system that MRI within 2 days of event was performed in about 51% of patients who presented with a TIA or minor stroke and had brain imaging performed. This finding suggests that there has been partial acceptance of the previous recommendation that brain MRI is the preferred imaging test for patients with TIA-like symptoms. Future studies should address the clinical utility of brain MRI in this patient population.
GLOSSARY
- AF
atrial fibrillation
- BP
blood pressure
- CAD
coronary artery disease
- CEA
carotid endarterectomy
- CHF
congestive heart failure
- DWI
diffusion-weighted imaging
- ED
emergency department
- IHD
ischemic heart disease
- MI
myocardial infarction
- VA
Veterans Affairs
AUTHOR CONTRIBUTIONS
Dr. Chaturvedi: study concept and design, analysis and interpretation of data, wrote first draft. S. Ofner, F. Baye, and Z. Yu: statistical analysis, interpretation of data. Dr. Myers: acquisition of data, analysis and interpretation of data. Drs. Phipps, Sico, Damush, Miech, Reeves, Johanning, Williams, Arling, and Cheng: analysis and interpretation of data, critical revision of manuscript. Dr. Bravata: study concept and design, analysis and interpretation of data, critical revision of manuscript, study supervision.
STUDY FUNDING
This work was supported by the Department of Veterans Affairs (VA), Health Services Research & Development Service (HSRD), Stroke Quality Enhancement Research Initiative (QUERI) Service Directed Project (SDP 12–178). Dr. Sico is supported by a VA HSRD Career Development Award (HX001388-01A1).
DISCLOSURE
S. Chaturvedi serves as a consultant to Merck, is Assistant Editor of Stroke, serves on the editorial boards of Neurology® and Journal of Stroke & Cerebrovascular Diseases, and receives grant funding from Boehringer-Ingelheim. S. Ofner, F. Baye, and L. Myers report no disclosures relevant to the manuscript. M. Phipps serves on a clinical advisory board for Castlight Health. J. Sico has been on an advisory board for Acorda Therapeutics. T. Damush, E. Miech, and M. Reeves report no disclosures relevant to the manuscript. J. Johanning holds intellectual property on noninvasive frailty assessment technology through FutureAssure LLC. L. Williams, G. Arling, E. Cheng, Z. Yu, and D. Bravata report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Coutts SB, Simon JE, Eliasziw M, et al. Triaging transient ischemic attack and minor stroke patients using acute magnetic resonance imaging. Ann Neurol 2005;57:848–854. [DOI] [PubMed] [Google Scholar]
- 2.Purroy F, Jiménez-Caballero PE, Mauri-Capdevila G, et al. Predictive value of brain and vascular imaging including intracranial vessels in transient ischaemic attack patients: external validation of the ABCD3-I score. Eur J Neurol 2013;20:1088–1093. [DOI] [PubMed] [Google Scholar]
- 3.Easton JD, Saver JL, Albers GW, et al. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease: The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke 2009;40:2276–2293. [DOI] [PubMed] [Google Scholar]
- 4.Coutts SB, Modi J, Patel SK, et al. . Recurrent stroke after transient ischemic attack and minor stroke: results of the prospective CATCH study. Stroke 2012;43:1013–1017. [DOI] [PubMed] [Google Scholar]
- 5.Giles MF, Albers GW, Amarenco P, et al. Early stroke risk and ABCD2 score performance in tissue- vs time-defined TIA: a multicenter study. Neurology 2011;77:1222–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Merwick Á, Albers GW, Amarenco P, et al. Addition of brain and carotid imaging to the ABCD2 score to identify patients at early risk of stroke after transient ischaemic attack: a multicentre observational study. Lancet Neurol 2010;9:1060–1069. [DOI] [PubMed] [Google Scholar]
- 7.Yaghi S, Rostanski SK, Boehme AK, et al. Imaging parameters and recurrent cerebrovascular events in patients with minor stroke or transient ischemic attack. JAMA Neurol 2016;73:572–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kidwell CS, Alger JR, Di Salle F, et al. Diffusion MRI in patients with transient ischemic attacks. Stroke 1999;30:1174–1180. [DOI] [PubMed] [Google Scholar]
- 9.Burke JF, Kerber KA, Iwashyna TJ, Morgenstern LB. Wide variation and rising utilization of stroke magnetic resonance imaging: data from 11 States. Ann Neurol 2012;71:179–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vernooij MW, Ikram MA, Tanghe HL, et al. Incidental findings on brain MRI in the general population. N Engl J Med 2007;357:1821–1828. [DOI] [PubMed] [Google Scholar]
- 11.Orme NM, Fletcher JG, Siddiki HA, et al. Incidental findings in imaging research: Evaluating incidence, benefit, and burden. Arch Intern Med 2010;170:1525–1532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bravata DM, Myers L, Cheng E, et al. Quality of care for veterans with transient ischemic attack and minor stroke. Stroke 2015;2015. Abstract at International Stroke Conference. [Google Scholar]
- 13.Burke JF, Gelb DJ, Quint DJ, Morgenstern LB, Kerber KA. The impact of MRI on stroke management and outcomes: a systematic review. J Eval Clin Pract 2013;19:987–993. [DOI] [PubMed] [Google Scholar]
- 14.Al-Khaled M, Eggers J. MRI findings and stroke risk in TIA patients with different symptom durations. Neurology 2013;80:1920–1926. [DOI] [PubMed] [Google Scholar]
- 15.Fiebach JB, Schellinger PD, Jansen O, et al. CT and diffusion-weighted MR imaging in randomized order: diffusion-weighted imaging results in higher accuracy and lower interrater variability in the diagnosis of hyperacute ischemic stroke. Stroke 2002;33:2206–2210. [DOI] [PubMed] [Google Scholar]
- 16.Murchison AP, Gilbert ME, Savino PJ. Neuroimaging and acute ocular motor mononeuropathies: a prospective study. Arch Ophthalmol 2011;129:301–305. [DOI] [PubMed] [Google Scholar]
- 17.Mitchell JB, Ballard DJ, Whisnant JP, Ammering CJ, Samsa GP, Matchar DB. What role do neurologists play in determining the costs and outcomes of stroke patients? Stroke 1996;27:1937–1943. [DOI] [PubMed] [Google Scholar]
- 18.Roquer J, Rodríguez-Campello A, Cuadrado-Godia E, et al. Acute brain MRI: DWI patterns and stroke recurrence after mild-moderate stroke. J Neurol 2010;257:947–953. [DOI] [PubMed] [Google Scholar]
- 19.Amarenco P, Lavallée PC, Labreuche J, et al. One-year risk of stroke after transient ischemic attack or minor stroke. N Engl J Med 2016;374:1533–1542. [DOI] [PubMed] [Google Scholar]
- 20.Coutts SB, Cucchiara B. Stroke risk after TIA: DWI is only part of the answer. Neurology 2013;80:1914–1915. [DOI] [PubMed] [Google Scholar]


