Abstract
Background
American workers spend 70–80% of their time at work being sedentary. Traditional approaches to increase moderate-vigorous physical activity (MVPA) may be perceived to be harmful to productivity. Approaches that target reductions in sedentary behavior and/or increases in standing or light-intensity physical activity [LPA] may not interfere with productivity and may be more feasible to achieve through small changes accumulated throughout the workday.
Methods/Design
This group randomized trial (i.e., cluster randomized trial) will test the relative efficacy of two sedentary behavior focused interventions in 24 worksites across two states (N=720 workers). The MOVE+ intervention is a multilevel individual, social, environmental, and organizational intervention targeting increases in light-intensity physical activity in the workplace. The STAND+ intervention is the MOVE+ intervention with the addition of the installation and use of sit-stand workstations to reduce sedentary behavior and enhance light-intensity physical activity opportunities. Our primary outcome will be objectively-measured changes in sedentary behavior and light-intensity physical activity over 12 months, with additional process measures at 3 months and longer-term sustainability outcomes at 24 months. Our secondary outcomes will be a clustered cardiometabolic risk score (comprised of fasting glucose, insulin, triglycerides, HDL-cholesterol, and blood pressure), workplace productivity, and job satisfaction.
Discussion
This study will determine the efficacy of a multilevel workplace intervention (including the use of a sit-stand workstation) to reduce sedentary behavior and increase LPA and concomitant impact on cardiometabolic health, workplace productivity, and satisfaction.
Keywords: sedentary behavior, workplace, cluster randomized trial, cardiometabolic health, physical activity, sit-stand workstations
1. Introduction
The health benefits of moderate-vigorous physical activity (MVPA) are well-established, and progress is being made toward the 2008 Physical Activity Guidelines for Americans.1 In addition to recommendations for MVPA, the Guidelines state the need to “avoid inactivity” and suggest any amount of physical activity will produce a health benefit. American adults spend an average of 7.5h/day sedentary.2 While the strongest benefit on health is conferred from MVPA, recent studies suggest replacing sedentary time (i.e., sitting/reclining with low energy expenditure while awake3) with standing or other non-exercise activities - even when holding MVPA constant - is associated with lower cardiometabolic risk4,5 and longevity.6,7
Sedentary behavior has been identified as important health target for workplaces.8 American workers, especially those with primarily desk-based jobs, can spend up to 70–80% of their time at work being sedentary.9 Traditional approaches to increase MVPA may be unsustainable in workplace settings as they require time away from work, and may be perceived as harmful to productivity.10 Sedentary behavior interventions (i.e., approaches targeting reductions in sitting and/or increases in standing or light-intensity physical activity [LPA]) may not interfere with productivity,11,12 and may be more feasible to achieve through small changes accumulated throughout the workday. Additionally, intervention strategies that incorporate environmental and policy-level changes - which are likely necessary for sustained behavior change - may be more feasible to implement in workplaces than other contexts.
Sedentary behavior interventions in the workplace have shown promising effects.13 Multi-level approaches targeting individual, social, and environmental factors have been most effective.14,15 The most robust environmental support has been the use of sit-stand workstations, providing opportunities for workers to reduce sitting while maintaining productivity.13 However, a recent Cochrane review rated sit-stand workstation interventions to be “of very low methodological quality” due to small sample sizes, short follow-up (≤ 4 months), and quasi-experimental designs. Notably, there are feasibility problems for trials randomizing individuals within a single worksite to different environmental conditions (i.e., dependency among observations).16
Two recent group randomized trials17,18 have addressed this by selecting worksites as the unit of randomization. Both studies delivered programs that targeted individual, social, environmental, and policy factors, alongside the installation of sit-stand workstations, to reduce sedentary time. Danquah et al.17, in a 3-month intervention among Danish public and private health workers (n worksites = 19; n subjects = 317), observed 48 min/8-hr workday reductions relative to a usual practice control. Healy et al.18, in a 12-month intervention of Australian public health workers (n worksites = 14; n subjects = 231), observed 45 min/8-hr workday reductions relative to a usual practice control.
While the results of these studies address critical issues raised in the Cochrane Review,16 three important limitations warrant further study. First, effects on sedentary time were smaller at the most distal time point compared to interim time points, suggesting “novelty” effects may exist. Longer-term follow-up of sustained impacts needs to be examined. Second, a relatively homogenous set of worksites within a single workplace sector were included. More diversity in worksite type is necessary to demonstrate generalizability. Finally, the interventions were compared to a usual practice control. Given the ongoing presence of alternative health promotion activities, it is important to compare sedentary behavior interventions to more robust comparison conditions. The purpose of this paper is to describe the development and design of a multi-level group randomized controlled worksite intervention aimed at reducing employee’s sedentary time.
2. Methods
2.1 Study aims
Our primary aim is to evaluate the efficacy of a workplace-delivered, multicomponent intervention and the provision of a sit-stand workstation, relative to a multicomponent comparison without a workstation, for reducing sitting and increasing LPA in the workplace over 12 months. Additional process outcomes at 3 months and maintenance outcomes at 24 months will be collected. Our secondary aim is to evaluate relative changes between intervention arms in cardiometabolic risk (composite measure of fasting glucose, insulin, triglycerides, HDL-cholesterol, and blood pressure), workplace productivity, and workplace satisfaction outcomes over 12 months.
2.2 Study design
Our design is a two-arm group-randomized trial. Worksites (N=24) of small to moderate size (20–50 employees enrolled; N=720 employees across the 24 sites) will be randomized to one of two interventions: (a) MOVE+, a multi-level behavioral intervention targeting increases in LPA at the worksite; or (b) STAND+, the multi-level MOVE+ intervention along with the installation of sit-stand workstations to allow workers to stand at their desks while working. Both worksite interventions are expected to reduce sitting and increase LPA over 12 months and improve cardiometabolic risk and work performance outcomes. We hypothesize the effects to favor the STAND+ study arm because the additional sit-stand workstation enhancement will provide a robust environmental stimulus to reduce sitting and provide a unique catalyst for LPA in the workplace. The MOVE+ arm will receive sit-stand workstations at 12 months and both arms will be assessed for follow-up at 24 months.
2.3 Study setting
Worksites will be enrolled in the greater Phoenix, AZ, USA and Minneapolis, MN, USA metropolitan regions. Twelve worksites will be randomized in each region. Selected worksites will be drawn from three distinct work sectors: higher education, industry/healthcare (e.g., law firms, health insurance providers), and government (e.g., state departments). Worksites will be equally selected in each sector across each region (n=4/sector/region worksites).
2.4 Study eligibility
2.4.1 Worksite eligibility criteria
Worksites will be screened for eligibility by study questionnaires completed by worksite leadership and followed up with interviews by study personnel to verify eligibility. Worksite eligibility criteria will be as follows: (a) small to moderate in size (i.e., 20–50 employees); (b) >80% of employees working full time in the office (30+ hours/week); (c) predominant worksite occupation being seated office work with little movement or walking (i.e., computer or telephone-based work); (d) not currently undergoing a wellness program aimed at reducing sitting or increasing LPA at work; (e) <10% of employees currently using a sit-stand workstation at work; (f) willing to have sit-stand workstations installed at the workplace; and (g) worksite leadership willing to be randomized to either study arm. To minimize the potential for contamination across worksites, we plan to recruit relatively isolated units, with minimal physical interaction with other worksites.
2.4.2 Participant eligibility criteria
Upon enrollment of the worksite, all employees within the worksite will be invited to complete participant-level screening via a self-administered questionnaire. Participant eligibility criteria will be as follows: (a) 18 years or older; (b) generally good health and able to safely reduce sitting and increase LPA; (c) working full-time on-site (i.e. 30+ hours and at least 4 days in the office per week); (d) not currently pregnant; (e) predominant worksite occupation being seated office work; (f) not currently using a sit-stand workstation at their primary desk location at work; (g) willing to have a sit-stand workstation installed at their desk; and (h) willing to be randomized to either study arm.
2.5 Procedure
2.5.1 Recruitment
Worksites within each sector will be contacted by email and telephone and invited to participate in the Stand & Move at Work study. Brief informational handouts directed toward worksite managers will be prepared detailing study goals and expectations. If a worksite is deemed eligible, informational sessions will be conducted by study personnel at the worksite to outline the study requirements and expectations at the worksite and individual level. A memorandum of understanding will be developed and signed by the worksite manager and study principal investigators to facilitate adherence to the intervention.
An online eligibility survey will be distributed to each worksite employee following the informational sessions. All eligible participants will be invited to schedule a 30-minute slot during an assessment morning held at the worksite. Randomization will not occur until all four worksites in the recruitment wave (2 per region) have completed their baseline assessments. Therefore, a participant will be considered enrolled in the active intervention once they have consented, completed baseline assessments, and paired worksites have been randomized to study arm. Prior work by our research team has suggested that we should expect 40%-75% participation within the identified worksite, which based upon worksite size will approximate our target recruitment of N=720 participants.
2.5.2 Randomization
Randomization to either the STAND+ or MOVE+ intervention arms of the trial will be at the level of the worksite. Randomization will be stratified on the three sectors nested within each of the two regions (Phoenix, AZ and Minneapolis/St. Paul, MN). Within each region, eligible worksites will be enrolled in pairs matched on sector, and each matched pair will be randomized so that one is randomized to receive the STAND+ intervention with the other receiving the MOVE+ intervention. This scheme will ensure a balanced design by both region and sector. We will also rotate the enrollment of sector pairs over the seasons of the full calendar year to help avoid seasonal effects, beginning with the first two pairs enrolled in January and the final two pairs enrolled in November. Enrolling two pairs every other month will also alleviate logistical and labor burdens for recruitment, data collection, and intervention implementation.
2.5.3 Interventions
The ‘Stand & Move at Work’ interventions will be delivered over 12 months. The intervention development team is comprised of behavioral scientists, exercise scientists, ergonomists, and worksite wellness coordinators. The primary behavioral target of the MOVE+ intervention is to accumulate 30 minutes or more additional LPA each day. This target was selected as an achievable goal with evidence for modest cardiometabolic benefit.19 The primary behavioral target of the STAND+ intervention is, in addition to the MOVE+ target, to increase time spent standing to 50% of desk-based time during the workday (e.g. standing for 3 hours out of 6 total desk-hours per day). This target was selected based upon preliminary work by our research team where this target was selected and was deemed feasible to achieve and produced significant cardiometabolic benefit.20
All intervention materials will be manualized into the Stand & Move at Work “Toolkit.” The toolkit will be distributed to each worksite prior to the intervention start date. It is expected that each worksite and/or sector may differ in the time, resources, space, and personnel available to dedicate to the implementation of the intervention. The Toolkit will therefore be comprised of both “required” strategies (i.e., strategies that are required to be implemented by worksite staff during the intervention period) and “optional” strategies (i.e., strategies that worksite staff are encouraged to implement as are appropriate given the worksite context). Additional strategies generated by the worksite staff will also be encouraged. This approach ensures uniformity of the delivered interventions across worksites and allows flexibility and autonomy among worksites. Actual implementation of intervention strategies will be closely monitored through quarterly worksite audits and worksite leader interviews.
2.5.3.1. Intervention framework
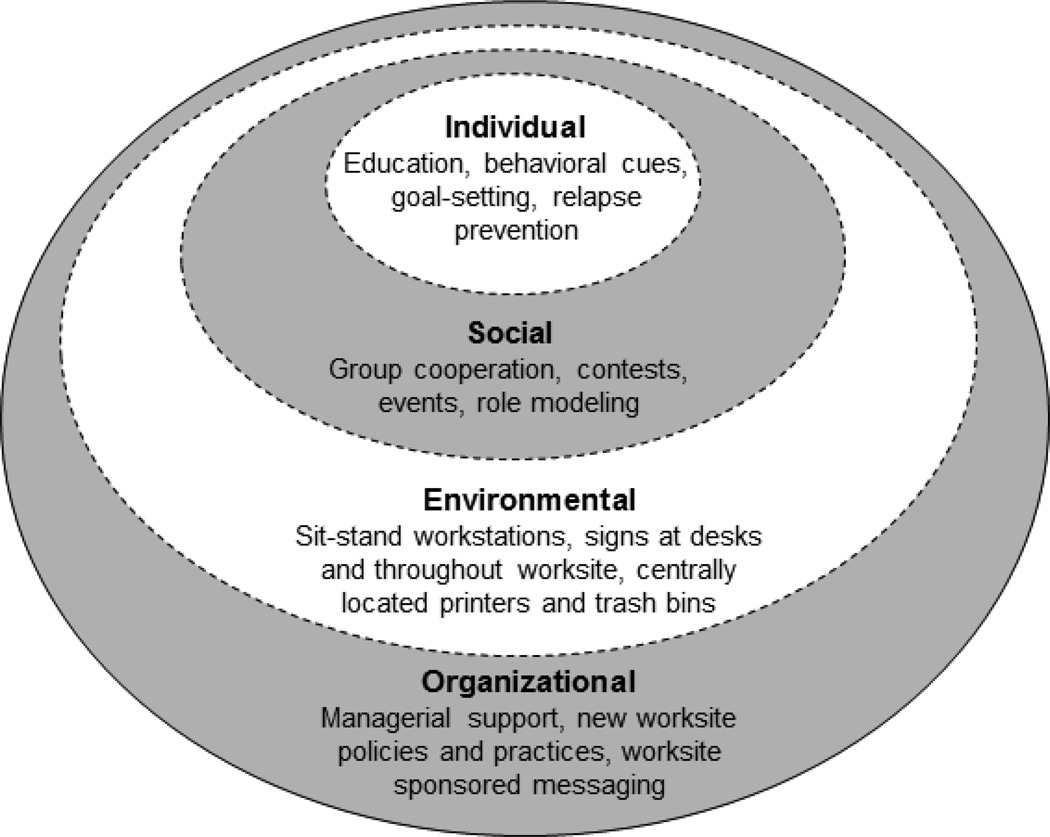
Stand & Move at Work interventions are based upon the social ecological framework, which posits behavior is influenced at multiple levels.21 Interventions that are scalable and create sustainable public health impact require “real-world” approaches that include strategies across numerous levels of the social ecological spectrum.22,23 This framework is widely used in the physical activity behavioral intervention field24 and has more recently become common in sedentary behavior focused interventions.25 Our approach will target intervention strategies at the individual, social, environmental, and organizational levels (Figure 1). Intervention strategies are also heavily based on social cognitive theory principles that seek to enhance sources of self-efficacy, improve outcome expectations, and leverage person-environment-behavior interactions (i.e., reciprocal determinism).26 To ensure that behavior change techniques are incorporated at each level, the behavior change taxonomy outlined by Michie et al.27, was translated into a workplace specific multi-level model that is outlined in Table 1 and summarized below.
Figure 1.
Social ecological approach to reducing sitting and increasing light-intensity physical activity in the workplace.
Table 1.
Behavior change techniques delivered in ‘Stand and Move at Work’ interventions.
| Behavioral Taxonomy | Organizational | Environmental | Social | Individual |
|---|---|---|---|---|
| 1. Information about behavior | Quarterly meetings* PI calls |
Signage* | PI calls | E-newsletter* |
| 2. Information about consequences/benefits |
Quarterly meetings* PI calls |
Signage* Ideaboard |
PI calls | E-newsletter* |
| 3. Information about others’ approval |
Quarterly support emails* Ideaboard PI calls |
PI calls | E-newsletter* | |
| 4. Prompt intention formation | 5-min breaks* PI calls Standing/w alking meetings |
Signage* Footrest* Desk** Ideaboard |
Walking/ Stretching groups |
E-newsletter* Goal-setting sheet* |
| 5. Prompt barrier identification | Quarterly meetings* PI calls |
E-newsletter* 1 on 1 coaching* |
||
| 6. Encouragement | Quarterly support emails* 5-min breaks* PI calls |
Signage* Ideaboard Contests |
E-newsletter quiz Contests |
E-newsletter* 1 on 1 coaching* |
| 7. Graded tasks | Contests | Contests | E-newsletter* | |
| 8. Provide instruction | Quarterly meetings* PI calls |
Signage* Walking routes* Ideaboard |
Ideaboard | E-newsletter* |
| 9. Model behavior | Leader and advocate* | E-newsletter* | ||
| 10. Goal setting | Quarterly support emails* | E-newsletter* Goal-setting sheet* 1 on 1 coaching* |
||
| 11. Review goals | Quarterly support emails* | E-newsletter* Goal-setting sheet* |
||
| 12. Prompt self-monitoring | E-newsletter* Goal-setting sheet* 1 on 1 coaching* |
|||
| 13. Provide feedback | Quarterly support emails* Quarterly meetings* |
E-newsletter* | ||
| 14. Provide rewards | Quarterly support emails* | Footrests* | E-newsletter quiz Contests |
|
| 15. Teach to use cues | Signage* Walking routes* Footrests* Desk* Ideaboard |
E-newsletter* Signage* |
||
| 16. Agree behavioral contract | Leader and advocate* Quarterly meetings* 5-min breaks* PI calls |
E-newsletter* 1 on 1 coaching* Goal setting sheet* |
||
| 17. Prompt practice | 5-min breaks* | Footrests* Desk** Contests |
Contests | E-newsletter* |
| 18. Follow up prompts | Quarterly meetings* PI calls |
E-newsletter* | ||
| 19. Opportunity for social comparison |
Quarterly support emails* PI Calls |
E-newsletter* | ||
| 20. Social support | Quarterly support emails* PI calls Ideaboard Standing/w alking meetings |
Ideaboard | Ideaboard Walking/ Stretching groups |
E-newsletter* |
| 21. Identification of a role model |
Quarterly support emails* Ideaboard |
Ideaboard | Ideaboard | E-newsletter* |
| 22. Prompt self talk | E-newsletter* | |||
| 23. Relapse prevention | Signage* | E-newsletter* | ||
| 24. Stress management | E-newsletter* | |||
| 25. Motivational interviewing | 1 on 1 coaching* | |||
| 26. Time management | E-newsletter* |
Required toolkit item for both study arms;
Required toolkit item for STAND+ only
2.5.3.2. Intervention elements
2.5.3.2.1 Policy-level components
The intervention framework is highly dependent on the identification and engagement of worksite administrators and managers to enact policy-level workplace modifications, implement robust environmental changes (e.g., sit-stand workstations), and to model and promote behavior change. Therefore, a required item will be to identify a worksite leader and advocate(s). A leader is defined as a person holding a higher-level management position to which the department, division, or unit employees report. The primary role of this individual will be to provide higher-level support for intervention strategies to be implemented. Primary responsibilities will be to determine appropriate Toolkit items, encourage participation in worksite initiatives, and approve potential policy changes. An advocate is defined as a person who plays an active role with study participants and will work closely with the Stand & Move at Work study team to implement the selected changes. Advocates will be considered the primary contact to link worksite employees, management, and the study team. Primary responsibilities will include aiding the implementation of strategies agreed upon by higher-level management.
Organizational changes will be reinforced by the distribution of four quarterly support emails sent by the leader to employees in the workgroup. Templates will be provided to minimally include: (a) support for the program and employee participation; (b) a brief review of the previous quarter progress; (c) commendation of individuals who have shown high levels of engagement; and (d) an outline of new intervention initiatives for the upcoming quarter. Leaders will also formally agree to allow employees up to 5 minute breaks every hour.
Shared leader and advocate responsibilities will include quarterly meetings with an experienced behavioral science research team member who will be the designated worksite coordinator throughout the study to review past progress and plan for the coming quarter using the Toolkit as a guide. The aim of the research team member is to facilitate the intervention by ensuring all materials and concepts are explained fully explained, it is not to actively lead the intervention. As such, all team members will have extensive knowledge of the Stand and Move Toolkit to provide the leaders and advocates with support. Successes and challenges from the previous quarter will be discussed and each worksite will be encouraged to implement a new strategy to maintain or potentially increase employee interest in the program. Similarly, all worksite leaders and advocates will be invited to join a monthly STAND+ and MOVE+ conference call with the study principal investigators. These will serve several purposes: (a) to provide opportunities for other worksites to share and learn from other worksites within the same randomized study arm; (b) to document worksite participation, progress, and new strategies; and (c) to provide insight into the breadth and scale of the study to reinforce participation from a scientific and health-based perspective.
2.5.3.2.2 Environment-level components
The primary environmental difference between the STAND+ and MOVE+ study arms will be the installation of a sit-stand workstation for the STAND+ arm only. The workstations will be installed by our trained research staff, as well as worksite-specific ergonomic and wellness professionals. The Ergotron sit-stand workstation Workfit-TL model (Ergotron, Inc., St. Paul, MN) has been selected because it is able to be retro-fitted for use with almost all workspaces, requires little or no installation as it is simply placed on the existing desk surface, is affordable relative to many alternatives, has more desk surface area then many alternatives on the market, it can be easily raised and lowered to a broad range of positions, and can accommodate one or two large computer monitors. The Workfit-TL transitions from seated to standing positions by holding two levers and providing minimal force. Prior to installation a workspace inventory will be conducted for each participant to identify any potential barriers to use such as overhead shelving, insufficient computer cabling, or fixed keyboard trays. To eliminate these barriers, overhead shelving will be moved by worksite facilities management, cable extenders added (if needed), and additional wireless keyboards will be provided to those with keyboard trays so that participants are not required to move their existing keyboards with each sit-stand transition. The same Ergotron Workfit-TL will be installed at the 12-month time point for all MOVE+ arm participants. All participants will receive ergonomic instructions for both sitting and standing postures via the e-newsletter and will undergo a coaching session at the time of installation.
Other required environmental changes will include a signage starter pack that is designed to (a) provide information about the behavior; (b) provide information on benefits of action (e.g., benefit of taking the stairs); (c) encourage goal setting (e.g., “make this a standing meeting”; (d) provide general encouragement (e.g., “we stand for health”); (e) provide instruction (e.g., walking routes around the office space); and (f) serve as visual cues. Signage will also demonstrate organizational support for the program and intent to change the cultural norm. Walking routes will be created for each worksite to reinforce the behavioral targets listed above. Typical routes will include alternative restrooms, centralized printing and trash can areas, and indoor and outdoor (if possible) perimeter routes. The distance per route and estimated number of steps will be provided on the signage. Advocates will be encouraged to place walking routes in communal and prominent areas throughout the worksite.
All participants regardless of randomization will be provided with a footrest. The footrests will serve the following three purposes: (a) as a resting position for either foot while both seated and standing; (b) as a stretching aid (gastrocnemius and soleus); and (c) as a visual reminder regarding participation in the program. Leaders and advocates may also wish to implement additional optional environmental changes throughout the program via combined environmental, individual, and social strategies. For example, a prominent and interactive communal board to promote the Stand & Move at Work program (termed an “Ideaboard”) or implementing environmentally based worksite challenges (e.g., centralized printing only challenges). Ideaboard templates and example challenges will be provided in the Toolkit.
2.5.3.2.3 Individual- and social-level components
An e-newsletter (The Insider) will provide a regular and direct medium for delivering individual-and social-level intervention content. The Insider will incorporate both individual (e.g., goal-setting) and social elements (e.g., quizzes and worksite social announcements). The Insider will be sent weekly during the first month of the intervention to facilitate transition and encourage early engagement. During months 2–12, the Insider will be sent bi-weekly, and a total of 26 newsletters will be sent. See Table 2 for a list of Insider topics. The content has been developed and designed by behavioral scientists and worksite wellness professionals to target 25 out of the 26 components of the behavioral taxonomy wheel. Motivational interviewing will be the only component not targeted, given the need for face-to-face interaction. The Insider will be coordinated with and reinforced by additional complementary organizational, environmental, and social components.
Table 2.
E-newsletter topics.
|
Other individual level strategies will include a 1-on-1 coaching session to identify specific goals and behavior change strategies relating to the key intervention messages. Using a goal setting sheet, participants will be encouraged to record and display their goals within daily eyesight. Participants will also receive instructions regarding the desk-based ergonomic set up (both MOVE+ and STAND+). The STAND+ arm will receive specific instructions (guided by an experienced ergonomist) regarding their new sit-stand workstation set up. Key messages will include switching position regularly and gradually increasing standing or LPA time. Social strategies (i.e., formation of walking or stretching groups) may be endorsed by leaders via support emails, actively led by advocates, or promoted via additional signage and Ideaboard content.
Due to the variation in worksite culture, job demands and environmental challenges, it is expected that new ideas and variations of the suggested Toolkit items will emerge. This will be discussed and documented during the quarterly meetings and quarterly audits. The required multi-level tactics show reinforcement of behavior change across the social-ecological spectrum, utilizing all aspects of the behavior change taxonomy wheel. This integrated approach shows promise for shifting the cultural norm within a workplace from reinforcing highly sedentary, seated behavior patterns to one where standing and moving is expected, rewarded, and celebrated. This cultural shift is necessary to produce sustainable, long lasting changes that are likely to impact health and well-being on a large scale.
2.5.3.3. Primary differences between study arms
The primary study arm differences will be implemented at the environmental level with the provision of a sit-stand desk at the start of the intervention for the STAND+ group only. This primary difference will require small adaptations to other intervention strategies. First, participant goals will differ per arm to reflect the different arm intervention goals (i.e., increasing standing and LPA time for STAND+ vs. increasing LPA only for MOVE+). All participants will be encouraged to adhere to a ‘30-minute rule’, however, the meaning of this target rule will differ per arm. For the STAND+ group this will be communicated as achieving a 30:30-minute sit to stand ratio to ultimately replace half their sit time with a combination of standing and moving at work. For the MOVE+ group this will be communicated as replacing 30 minutes of sit time with an equal accumulation of moving more throughout the work day. The 1-on-1 sessions held at the start of the program will facilitate specific goalsetting at the individual level to help achieve the ‘30-minute rule’ per arm. Consequently, the strategies communicated during the 1-on-1 session and throughout the study duration will differ slightly per arm (see Table 3). Second, although the STAND+ and MOVE+ arms will be provided with an identical Stand & Move Toolkit and the same level of support to implement socio-ecological changes, it is likely that the application of the Toolkit will differ per arm to target the specific target intervention arm goals. Finally, in some instances, the e-newsletter topics will remain the same across arms but the content will be adjusted per arm to reduce contamination and ensure that information is specific to the intervention arm. For example, the ergonomically themed e-newsletter will include sit-stand desk information for the STAND+ group, however, the MOVE+ content will only include seated desk information. Stand & Move intervention support for STAND+ will cease following the 12-month assessment period. However, MOVE+ participants will receive a sit-stand desk and ergonomic advice at the 12-month time point, and after which no additional intervention support will continue post-installation. Both arms will still have access to the Toolkit during this follow-up period (12–24 months).
Table 3.
Intervention strategies per study arm
| STAND+ | MOVE+ | |
|---|---|---|
| Individual strategies | ||
| Take 15 × 2-min, 10 × 3-min or 6 × 5-min move breaks throughout your workday | X | X |
| Progress from 5 to 30 minute standing breaks every hour | X | |
| Use a restroom further away | X | X |
| Use the stairs only | X | X |
| Remove the trash can from your desk | X | X |
| Remove the recycling can from your desk | X | X |
| Use a walking route once a day | X | X |
| Stretch for 5 minutes per day | X | X |
| Use face to face interaction rather than email | X | X |
| Use centralized printing areas | X | X |
| Get away from your desk for lunch | X | X |
| Use a smaller water bottle to fill it more frequently | X | X |
| Stand during phonecalls | X | X |
| Check your emails while standing | X | |
| Set reminders to stand every 30-min on your calendar | X | |
| Leave your sit-stand desk in the standing position at the end of the workday to encourage standing the next day |
X | |
| Set reminders to move every 30-min on your calendar | X | X |
| Workplace strategies | ||
| Implement a short break (to stand or move) during meetings > 60-min in duration | X | X |
| Implement walking meetings | X | X |
| Implement standing meetings | X | X |
| Implement standing challenges (e.g one person standing at all times, group standing periods) |
X | |
| Implement moving challenges (e.g stair/walking route challenges, not using restrooms on the same floor, passing an item around the office throughout the day) |
X | X |
| Promote standing and moving at the organizational level vi a quarterly support emails | ||
| X | X | |
2.6 Measures
All measurements will be taken at baseline and 12 months, with additional interim measurement at 3 months and follow-up at 24 months. Table 4 shows the measures taken at each assessment visit. Demographic and health history variables will be assessed at all time points. All questionnaires will be administered via Qualtrics (Salt Lake City, UT) and participants will be allowed to complete the measures at their convenience during the week of each measurement time point.
Table 4.
Measurement schedule.
| Measurement Month |
Baseline 0 |
Process 3 |
Primary 12 |
Maintenance 24 |
|---|---|---|---|---|
| Demographics, health history | ◊ | |||
| Primary Aim | ||||
| Sitting (at work) | • | • | • | • |
| Light-intensity physical activity (at work) | ||||
| Secondary Aim | ||||
| Blood pressure | • | • | • | • |
| Blood draws (glucose, insulin, HDL, triglycerides) | • | • | • | • |
| Workplace productivity | ◊ | ◊ | ◊ | ◊ |
| Work engagement | ◊ | ◊ | ◊ | ◊ |
| Workplace satisfaction | ◊ | ◊ | ◊ | ◊ |
| Additional outcomes | ||||
| Workplace sedentary behavior | ◊ | ◊ | ◊ | ◊ |
| Physical activity | ◊ | ◊ | ◊ | ◊ |
| Diet | ◊ | ◊ | ◊ | ◊ |
| Functional health and well-being | ◊ | ◊ | ◊ | ◊ |
| Musculoskeletal problems | ◊ | ◊ | ◊ | ◊ |
Objectively monitored;
Online survey-administered.
2.6.1 Primary outcomes
Our primary outcomes, time spent sitting and LPA at work, will be assessed with the activPAL3 micro accelerometer (PAL Technologies, Glasgow, United Kingdom) for seven consecutive days at each measurement time point. The activPAL provides a valid and reliable measure of posture (sitting vs. standing) for free-living settings28,29 and uses a transducer suitable for detecting lower intensity movements.30 The activPAL will be waterproofed using medical grade adhesive covering and attached to the midline of the thigh using a breathable, hypoallergenic tape. This method allows for the monitor to be worn continuously for seven consecutive days without removing for bathing or other water-based activities (a valuable feature that reduces missing data). Additional adhesive dressing will be given to all participants for re-application as necessary. The primary outputs of the activPAL are time spent sitting, time spent upright, and time spent “stepping.” Participants concurrently will complete an online daily log where they will report their sleep/wake schedule and time arriving and departing their workplace. The daily logs will be used to filter time spent sitting and LPA during work hours. In addition, any uninterrupted sedentary bouts of more than six hours that occur within reported wake times will be considered non-wear times and treated as missing data. Days with <10h of monitor wear data or <80% of reported work time as monitor wear data will be excluded from analyses. Outcomes will be reported as a standardized 8h workday to account for differences in total work time.
2.6.2 Secondary outcomes
The secondary outcomes of the intervention are cardiometabolic risk, workplace productivity, work engagement, and workplace satisfaction. We will measure resting blood pressure and fasting levels of glucose, insulin, triglycerides, and HDL-cholesterol at each assessment period. Blood pressure will be measured with the Omron BP742 automated machine and the Omron HEM-RML30 cuff (Omron Healthcare Inc., Lake Forest, IL) three times following five minutes of quiet sitting, with 30 seconds in between each measurement. The lowest two measures of diastolic and systolic blood pressures will be averaged for final blood pressure values. Participants will be instructed to fast for nine consecutive hours prior to each blood draw. Blood will be drawn from the antecubital vein into EDTA vacutainers, and plasma will be stored at −80C until analysis in batch. Samples from the Phoenix site will be shipped to UMN on dry ice periodically for batch-processing. Biomarker analyses will be conducted by the Advanced Research and Diagnostic Laboratory at the University of Minnesota, Minneapolis, MN, using a Roche COBAS 6000 chemistry analyzer (Roche Diagnostics, Indianapolis, IN). Plasma glucose will be measured in by the hexokinase method (interassay CV = 1.3% at 97.2 mg/dL, 1.8% at 223.3 mg/dL). Plasma HDL-C will be measured by the modified direct enzymatic approach (interassay CV = 3.2% at 27.0 mg/dL, 1.9% at 51.7 mg/dL). Plasma triglycerides will be measured with the GPO-Trinder kit (Roche Diagnostics, Indianapolis, IN; interasssay CV = 2.0% at 112.4 mg/dL, 2.3% at 195.8 mg/dL). Plasma insulin will be measured with a sandwich immunoassay using electrochemilumincescence (Roche Diagnostics, Indianapolis, IN; interassay CV = 3.1% at 121.2 pmol/L, 3.1% at 377.9 pmol/L).
Risk factors for diabetes and cardiovascular disease are fundamental to the concept of metabolic syndrome and will be studied on a continuous spectrum rather than using clinical cutpoints. The literature has clearly demonstrated that these components operate on a continuous linear spectrum in predicting future disease occurrence31–35 and optimal statistical power can be retained using a composite continuous score. The Z-scores for each component based on the baseline mean and standard deviation of the entire group will be computed and summed for each participant (HDL z-score is subtracted rather than added). The sum of these z-scores - which we refer to as the metabolic risk score - will be a secondary outcome measure. This metabolic risk score has become common in epidemiologic and more recently experimental and clinical studies.34,36–39
Workplace productivity will be measured using the validated Work Productivity and Activity Impairment Questionnaire – General Health (WPAI-GH).40 This six-item questionnaire asks about the total hours missed from work and total hours that the respondent worked during the past 14 days, and the degree to which they feel that a health problem has affected both their productivity at work and their ability to do daily activities. WPAI-GH outcomes will be expressed as (1) the percentage of work time missed due to ill-health (absenteeism), (2) the percentage impairment while working due to ill-health (presenteeism), (3) the percentage of overall work impairment due to health, and (4) the percent of activity impairment due to health using the same methods by Zhang et al.41 The questionnaire had been shown to have moderate-strong correlations with health outcomes (Spearman r= 0.34 – 0.77) among patients with rheumatoid arthritis. In addition, WPAI-GH had been validated to quantify work impairments associated with other diseases.42 The Utrecht Work Engagement Scale (UWES-9) will be used to determine work engagement. The 9-item questionnaire assesses three dimensions of work engagement: vigor, dedication, and absorption, using a 7-point Likert-type frequency scale ranging from 0 (never) to 6 (always).43,44 The internal consistencies (Cronbach’s alpha) of the three-factor structure of UWES-9 ranges from 0.81 – 0.85 for vigor, from 0.83 – 0.87 for dedication, and from 0.75 to 0.83 for absorption. Moreover, the questionnaire had been shown to be a stable indicator of occupational well-being.45 Workplace satisfaction will be measured using a single-item question that pertains to overall job satisfaction of respondents on their main job using a 7-point scale that ranges from 1 (extremely dissatisfied) to 7 (extremely satisfied).46 The questionnaire is a reliable (α= 0.73) and valid measure of overall job satisfaction (r= 0.82 vs the 15-item Job Satisfaction Scale).47 Adverse events that may potentially be related to participation in either intervention arm will be assessed at each measurement timepoint or more often if reported by participants.
2.6.3. Exploratory outcomes
Additional exploratory outcomes will be assessed at each assessment period. The 24-Hour Physical Activity Recall will be administered on a single random day during each assessment period to assess overall physical activity and physical activity type.48 The questionnaire classifies each 15-minute epoch of the participant’s past 24 hours into lying down or sleeping, seated, standing, moving about, moderate, heavy, or very heavy activity. The total time spent on each of these categories will be summed and an energy expenditure estimate will be calculated using established MET codes from the compendium of physical activities. The Workforce Sitting Questionnaire (WSQ)49 will be used to assess total and domain-specific forms of sitting. The questionnaire evaluates total sitting time related to (1) transportation, (2) work, (3) television watching, (4) using a computer at home, and (5) doing leisure activities on work and non-workdays. Dietary consumption will be assessed on a single random day during each assessment period using the Automated Self-Administered 24-Hour (ASA24) Dietary Assessment Tool. The ASA24 is a web-based tool that allows users to recall their diet in the past 24 hours.50,51 Musculoskeletal complaints will be assessed with the Nordic Musculoskeletal Questionnaire,52 a validated measure of pain, discomfort, and physical limitations in nine bodily regions during the last month and year. This measure will be used to examine any unique musculoskeletal complaints that may arise as a result of additional standing or LPA. Finally, focus groups will be conducted at the 12-month timepoint at each worksite to collect feedback regarding the barriers and facilitators to the intervention implementation. These will be conducted by an experienced qualitative scientist who is not a member of the research team to avoid potential bias.
2.7 Data analysis
2.7.1 Statistical analysis plan
Threats to internal validity (e.g. contamination, envy)53 preclude randomization of individuals within the same worksite; hence, a group-randomized trial is being conducted.54 Such a trial involves randomization of worksites with members within a worksite being assigned to the same experimental condition. Hierarchical linear (or generalized linear) models will be used to provide valid estimates of the intervention effect and its variance (for generating the test of statistical significance). Because the number of sites is limited by feasibility, the asymptotic balance of all measured and unmeasured confounders is not applicable, and hence it is important to randomize worksites within small blocks (or pairs) of matched worksites with similar characteristics likely to affect the outcome measure. Because our goal is to enroll 12 worksites in the Phoenix area and 12 in the Minneapolis area, we will stratify the randomization scheme on geographical location so that we will not have any confounding by geographical location (AZ vs. MN). We will identify six pairs of sites in AZ and six pairs in MN, with the pair members having the same sector (academia, government, or healthcare/industry). Each pair will be randomized so that one worksite in each pair is assigned to the MOVE+ intervention and the other in that pair assigned to the STAND+ intervention. One of the site PIs and a Biostatistician at the University of Minnesota will be responsible for the randomization. Randomization will occur immediately following the baseline data collection for both sites. The PI will notify the biostatistician when there are two matched worksites ready for randomization. The two worksites will be ordered as “First” and “Second” depending on the calendar dates of the baseline data collection. The statistician, with no knowledge of the worksites, will use a coin flip to assign the two worksites to the Stand+ or Move+ interventions.
Initial analyses will provide descriptions of the baseline frequencies and means (SD) of characteristics by worksite and by experimental condition. Statistical testing of differences in baseline characteristics is not necessary, but will provide assurance that the randomization has not produced a grossly unbalanced assignment. If the distributions of our outcome variables are not normally distributed, we will log-transform the outcome data. Our primary hypotheses will be tested by invoking a repeated-measures hierarchical linear model of the experimental contrast between the two conditions of the 12-month measure of LPA (min/8-hr) and sitting (min/8-hr), respectively. Because total time is standardized to 8 hours, we will also express our outcomes in percent of time in LPA and sitting. A repeated measures hierarchical analysis will be conducted. The covariates expected to include are age, sex, body mass index, and the baseline values of the dependent variables (e.g., sitting time, LPA, and metabolic risk score). The resulting estimate and its standard error provide a t-statistic based on 2(g-1) degrees of freedom (df), where g represents the number of worksites per experimental condition.54 A similar analysis will examine the secondary hypothesis for the metabolic risk score. Other outcomes, including sit-stand transitions, will use hierarchical generalized linear models with a log link. The analysis approach for process (3 month) and maintenance (24 month) outcomes will be similar.
In terms of missing data, sensitivity to member-dropout is small; if on average only 85% are followed, the detectable effect sizes increase by a factor 1.05. Worksite dropout would be a major threat to validity, but that is highly unlikely to occur. Baseline characteristics of those not providing follow-up data will be examined to assess whether these are non-informative missingness. Under the assumption that dropout is not related to the measures that would have been collected, the analysis of the data excluding dropouts is unbiased.
2.7.2 Sample size calculation
We will enroll 24 worksites (N=12 per condition) evenly distributed across Arizona and Minnesota with, on average, 30 employees per worksite (Total N members = 720 employees). In a baseline-adjusted analysis, let D represent the minimal detectable intervention effect, g the number of worksites per experimental condition, m the average number of members per worksite, S2 the member variance, T2 the work-site level variance, rm and rg the member and work-site correlations over time respectively, and t(d,a/2) and t(d,p) the critical t-statistic values based on d df for a/2=Type I alpha level (2-sided) and p=power. Then the minimal detectable difference is D2 = (t(d,a/2) + t(d,p))2 (S2(1- r2m)/m+ T2(1- r2g))*2/g. Dividing by S2 yields the square of the Effect Size (ES),54,55 and T2/S2 is the variance components ratio (VCR). In the unlikely situation where the g is unequal, replacing 2/g by (1/g0+1/g1) will lead to a minimal increase in D unless the g are grossly unequal. With g=12 (worksites per condition), d=22, and N=720, m=30; a/2 is set to 0.025 and power is set 80%. The detectable effect sizes for this trial range from 0.21 to 0.26 across sedentary time, LPA, and cardiometabolic risk, which are relatively small effects, and thus we are well powered in this study. On an absolute scale we will be able to detect a difference between intervention arms as small as 12.2 min/8-hr work day of LPA and 14.6 min/8-hr work day of sitting time. Our preliminary studies clearly demonstrate our ability to achieve these effects: (a) For LPA; a cross-over study20 showed a 38.4min/8-hr workday increase (other two studies did not target LPA or did not use a monitor designed to detect LPA); (b) for sitting, both the crossover and a natural experiment showed >30min/8-hr workday reductions; and (c) for cardiometabolic risk, all three studies showed moderate to large effect sizes. This study is powered well to detect effects that are considerably smaller than what we have observed in our preliminary studies.
3. Discussion
This project stands to be one of the most definitive studies to date on the efficacy of multi-level workplace interventions to increase LPA, reduce sitting, and improve cardiometabolic health. Findings will inform the potential health benefits of sit-stand workstations, an increasingly popular environmental intervention among employers. The findings will be highly generalizable to much of the sedentary workforce, and will inform employer and insurer decisions regarding cost, investment, and potential healthcare savings.
The likelihood of dissemination has been an important design feature of our preliminary studies and this is reflected in the current proposed research strategy. First, our choice of a group-randomized trial is critical to produce the most generalizable results that employers and worksites can immediately use to enhance the health and well-being of their workplace. Second, our active interventions will be delivered in collaboration and support by the wellness professionals already employed in the worksites. We acknowledge the challenge of maintaining internal validity with this approach, but have been successful with this approach in our preliminary studies and feel that this will enhance the long-term sustainability of our approach. Third, we have partnered with Ergotron, Inc. to provide low-cost sit-stand workstations that can be retro-fitted for almost any desk configuration that is used by worksites. This approach has distinct advantages over full-desk height-adjustability or walking workstation options which are generally not feasible options for most worksites. In summary, we believe this study will result in findings with high dissemination potential.
Several characteristics of our study warrant careful consideration. First, given the design of our study (i.e. a group-randomized trial), we are not randomly assigning individuals to intervention arms. We are assigning the intervention arm condition to entire worksites, so all employees in a given worksite will receive the same intervention. The statistical power of group-randomized trials is typically much lower than the individual randomized trial, due to the clustering of members within groups (employees within worksites). Our sample size is 24 worksites rather than 720 individuals, and we have strong rationale from our preliminary studies and are using precise behavioral monitors to maximize our power. Given issues of cross-contamination and generalizability, a group-randomized trial is state-of-the-art and required to move the field forward, and we are prepared to recruit the sample and power to achieve the necessary effects. Second, we do not have an inactive control group. Both groups will receive an active intervention. While this may be viewed as a limitation by some, we believe this is necessary and favorable to achieve the most meaningful and generalizable results. Our preliminary studies have consistently suggested that the use of sit-stand workstations are a critical environmental feature for decreasing sitting and increasing LPA. Furthermore, worksites are interested in knowing whether this modest investment is worthwhile for the health and well-being of their employees. Adding an additional arm is not feasible in this large group-randomized trial. We believe comparing two active interventions is ideal for producing real-world, generalizable results that can readily be used by worksites related to the health impact of sit-stand workstations. Third, we have chosen to give the MOVE+ intervention worksites the sit-stand workstations immediately following the primary outcome at 1-year. This approach allows us to minimize resentful demoralization that may occur by withholding the sit-stand workstations for a full two years, and it also allows us to test the timing of sit-stand workstation roll-out by comparing the two arms at the 24-month time point, which is an additional question above and beyond the primary follow-up analysis at 24 months. We believe this design will provide the most scientific insight from these interventions, while also enhancing the real-world, generalizable aspect of this project.
No study is without its challenges and limitations, especially group-randomized intervention trials in worksites. Thus, we have carefully considered four challenge-areas and describe a plan for addressing them before and during the trial, as follows:
Ability to recruit and enroll 24 worksites: We have already solicited considerable interest in our trial from worksites. We started with large employers with whom we worked for our preliminary studies. These companies have many other worksites now interested in being involved in our proposed trial. We are well on our way toward having a sufficient number of interested worksites from which we can begin to formally screen for inclusion into the study.
Ability to recruit and retain the full sample: Our preliminary studies demonstrate our ability to recruit and retain worksites and participants within the worksites. Combined across our three intervention studies described earlier, we recruited 6 worksites for interventions lasting one to six months, and we had 100% retention at the worksite level. At the individual participant level, retention was ∼90%. We attribute much of our success to having managers at the worksite take a role in endorsing the studies, and often modeling the intervention behavior, when appropriate. We also worked with the respective wellness personnel at the worksites so that our efforts would be appropriately integrated in the most effective way at each site.
Cooperation among worksites for organization-level changes: Our initial efforts to garner interest from worksites for this trial have been met with great enthusiasm. These sites are genuine in embracing change for a more active and healthy employee environment. Our decision to include two active intervention arms (both of which involve organization-level changes) is critical to our success in working effectively and sustainably with worksites.
Communication and coordination across two sites: The principal investigators have worked together very effectively in coordinating their preliminary studies and using their formative work toward designing a state-of-the art worksite randomized trial. We have capitalized on the many layers of the social-ecological model and have assembled a very strong multi-disciplinary approach. We have identified the key areas of strength that each worksite brings, so that there are clear roles for each investigator and staff at each of the worksites. We have developed a leadership plan that lays out the vision for effective communication and coordination. The mix of investigators from varying career stages and the presence of senior mentorship are key elements to our predicted success.
Health promotion strategies to promote moderate-vigorous physical activity are well-known; however, less is known about strategies to reduce sitting and increase light-intensity physical activity. This research will provide new evidence-based strategies for improving workers’ health using administrative and environmental tactics including the use of sit-stand workstations. This project stands to be the most definitive study to date on the efficacy and effectiveness of multi-level workplace interventions to decrease sitting and increase LPA at work, improve cardiometabolic health, and enhance workplace productivity.
Acknowledgments
Funding Sources
This work was supported by the National Institutes of Health [R01CA198971].
Abbreviations
- MVPA
moderate-vigorous physical activity
- LPA
light-intensity physical activity
- HDL
high-density lipoprotein
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Trial registration: ClinicalTrials.gov Identifier: NCT02566317 (date of registration: 10/1/2015).
Competing Interests
The authors declare that they have no competing interests.
References
- 1.Physical Activity Guidelines Advisory Committee. Physical activity guidelines advisory committee report, 2008. Washington, DC: US Department of Health and Human Services; 2008. [Google Scholar]
- 2.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008 Apr 1;167(7):875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sedentary Behaviour Research Network. Letter to the editor: standardized use of the terms “sedentary” and “sedentary behaviours”. Appl Physiol Nutr Metab. 2012;37(3):540–542. doi: 10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- 4.Buman MP, Winkler EA, Kurka JM, et al. Reallocating time to sleep, sedentary hehaviors, or active behaviors: associations with cardiovascular disease risk biomarkers, NHANES 2005–2006. Am. J. Epidemiol. 2014;179(3):323–334. doi: 10.1093/aje/kwt292. [DOI] [PubMed] [Google Scholar]
- 5.Healy GN, Winkler EAH, Owen N, Anuradha S, Dunstan DW. Replacing sitting time with standing or stepping: associations with cardio-metabolic risk biomarkers. European Heart Journal. 2015;36(39):2643–2649. doi: 10.1093/eurheartj/ehv308. 2015-10-14 00:00:00. [DOI] [PubMed] [Google Scholar]
- 6.Matthews CE, Moore SC, Sampson J, et al. Mortality benefits for replacing sitting time with different physical activities. Medicine and science in sports and exercise. 2015;47(9):1833–1840. doi: 10.1249/MSS.0000000000000621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stamatakis E, Rogers K, Ding D, et al. All-cause mortality effects of replacing sedentary time with physical activity and sleeping using an isotemporal substitution model: a prospective study of 201,129 mid-aged and older adults. International Journal of Behavioral Nutrition and Physical Activity. 2015;12(1):1–10. doi: 10.1186/s12966-015-0280-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Straker L. Sedentary work. Evidence on an emergent work health and safety issue. 2016 [Google Scholar]
- 9.McCrady SK, Levine JA. Sedentariness at work: how much do we really sit? Obesity. 2009;17(11):2103–2105. doi: 10.1038/oby.2009.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brown HE, Burton N, Gilson ND, Brown W. Measuring presenteeism: which questionnaire to use in physical activity research? J Phys Act Health. 2014;11(2):241–248. doi: 10.1123/jpah.2011-0307. [DOI] [PubMed] [Google Scholar]
- 11.Husemann B, Von Mach CY, Borsotto D, Zepf KI, Scharnbacher J. Comparisons of musculoskeletal complaints and data entry between a sitting and a sit-stand workstation paradigm. Human Factors: The Journal of the Human Factors and Ergonomics Society. 2009;51(3):310–320. doi: 10.1177/0018720809338173. [DOI] [PubMed] [Google Scholar]
- 12.Straker L, Levine J, Campbell A. The Effects of Walking and Cycling Computer Workstations on Keyboard and Mouse Performance. Human Factors: The Journal of the Human Factors and Ergonomics Society. 2009;51(6):831–844. doi: 10.1177/0018720810362079. December 1, 2009. [DOI] [PubMed] [Google Scholar]
- 13.Neuhaus M, Eakin E, Straker L, et al. Reducing occupational sedentary time: a systematic review and meta-analysis of evidence on activity-permissive workstations. Obesity Reviews. 2014;15(10):822–838. doi: 10.1111/obr.12201. [DOI] [PubMed] [Google Scholar]
- 14.Healy GN, Lawler S, Thorp A, et al. Reducing prolonged sitting in the workplace, An evidence review: full report. Creating Healthy Workplace evidence review series. 2012:88. [Google Scholar]
- 15.Pronk NP. Physical activity promotion in business and industry: evidence, context, and recommendations for a national plan. J Phys Act Health. 2009 Nov;6 Suppl 2(2):S220–S235. [PubMed] [Google Scholar]
- 16.Shrestha N, Kukkonen-Harjula KT, Verbeek JH, Ijaz S, Hermans V, Bhaumik S. Workplace interventions for reducing sitting at work. The Cochrane Library. 2016 doi: 10.1002/14651858.CD010912.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Danquah I, Kloster S, Holtermann A, et al. Take a Stand!–a multi-component intervention aimed at reducing sitting time among office workers–a cluster randomized trial. International Journal of Epidemiology. 2016:dyw009. doi: 10.1093/ije/dyw009. [DOI] [PubMed] [Google Scholar]
- 18.Healy GN, Eakin EG, Owen N, et al. A Cluster RCT to Reduce Office Workers’ Sitting Time: Impact on Activity Outcomes. Medicine and science in sports and exercise. 2016 May 17; [Google Scholar]
- 19.Buman MP, Hekler EB, Haskell WL, et al. Objective light-intensity physical activity associations with rated health in older adults. Am J Epidemiol. 2010 Nov 15;172(10):1155–1165. doi: 10.1093/aje/kwq249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dutta N, Koepp GA, Stovitz SD, Levine JA, Pereira MA. Using sit-stand workstations to decrease sedentary time in office workers: a randomized crossover trial. International journal of environmental research and public health. 2014;11(7):6653–6665. doi: 10.3390/ijerph110706653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stokols D. Establishing and maintaining healthy environments: toward a social ecology of health promotion. American Psychologist. 1992;47(1):6. doi: 10.1037//0003-066x.47.1.6. [DOI] [PubMed] [Google Scholar]
- 22.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Education Quarterly. 1988;15(4):351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 23.Heath GW, Parra DC, Sarmiento OL, et al. Evidence-based intervention in physical activity: lessons from around the world. The Lancet. 2012;380(9838):272–281. doi: 10.1016/S0140-6736(12)60816-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.King AC, Stokols D, Talen E, Brassington GS, Killingsworth R. Theoretical approaches to the promotion of physical activity: forging a transdisciplinary paradigm. American Journal of Preventive Medicine. 2002 Aug;23(2 Suppl):15–25. doi: 10.1016/s0749-3797(02)00470-1. [DOI] [PubMed] [Google Scholar]
- 25.Neuhaus M, Healy GN, Fjeldsoe BS, et al. Iterative development of Stand Up Australia: a multi-component intervention to reduce workplace sitting. International Journal of Behavioral Nutrition and Physical Activity. 2014;11(1):1. doi: 10.1186/1479-5868-11-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bandura A. Self-efficacy: the exercise of control. New York: W. H. Freeman; 1997. [Google Scholar]
- 27.Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013 Aug;46(1):81–95. doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- 28.Kozey-Keadle S, Libertine A, Lyden K, Staudenmayer J, Freedson PS. Validation of wearable monitors for assessing sedentary behavior. Med. Sci. Sports Exerc. 2011 Aug;43(8):1561–1567. doi: 10.1249/MSS.0b013e31820ce174. [DOI] [PubMed] [Google Scholar]
- 29.Dowd KP, Harrington DM, Bourke AK, Nelson J, Donnelly AE. The measurement of sedentary patterns and behaviors using the activPAL™ Professional physical activity monitor. Physiol. Meas. 2012;33(11):1887. doi: 10.1088/0967-3334/33/11/1887. [DOI] [PubMed] [Google Scholar]
- 30.Chen KY, Janz KF, Zhu W, Brychta RJ. Re-defining the roles of sensors in objective physical activity monitoring. Med. Sci. Sports Exerc. 2012;44(1 Suppl 1):S13. doi: 10.1249/MSS.0b013e3182399bc8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lempiäinen P, Mykkänen L, Pyörälä K, Laakso M, Kuusisto J. Insulin resistance syndrome predicts coronary heart disease events in elderly nondiabetic men. Circulation. 1999;100(2):123–128. doi: 10.1161/01.cir.100.2.123. [DOI] [PubMed] [Google Scholar]
- 32.Kekäläinen P, Sarlund H, Pyörälä K, Laakso M. Hyperinsulinemia cluster predicts the development of type 2 diabetes independently of family history of diabetes. Diabetes Care. 1999;22(1):86–92. doi: 10.2337/diacare.22.1.86. [DOI] [PubMed] [Google Scholar]
- 33.Hanson RL, Imperatore G, Bennett PH, Knowler WC. Components of the “metabolic syndrome” and incidence of type 2 diabetes. Diabetes. 2002;51(10):3120–3127. doi: 10.2337/diabetes.51.10.3120. [DOI] [PubMed] [Google Scholar]
- 34.Hillier TA, Rousseau A, Lange C, et al. Practical way to assess metabolic syndrome using a continuous score obtained from principal components analysis. Diab tologia. 2006;49(7):1528–1535. doi: 10.1007/s00125-006-0266-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pyörälä M, Miettinen H, Halonen P, Laakso M, Pyörälä K. Insulin resistance syndrome predicts the risk of coronary heart disease and stroke in healthy middle-aged men the 22-year follow-up results of the Helsinki Policemen Study. Arterioscler. Thromb. Vasc. Biol. 2000;20(2):538–544. doi: 10.1161/01.atv.20.2.538. [DOI] [PubMed] [Google Scholar]
- 36.Batey LS, Goff DC, Tortolero SR, et al. Summary Measures of the Insulin Resistance Syndrome Are Adverse Among Mexican-American Versus Non-Hispanic White Children The Corpus Christi Child Heart Study. Circulation. 1997;96(12):4319–4325. doi: 10.1161/01.cir.96.12.4319. [DOI] [PubMed] [Google Scholar]
- 37.Brage S, Wedderkopp N, Ekelund U, et al. Features of the Metabolic Syndrome Are Associated With Objectively Measured Physical Activity and Fitness in Danish Children The European Youth Heart Study (EYHS) Diabetes Care. 2004;27(9):2141–2148. doi: 10.2337/diacare.27.9.2141. [DOI] [PubMed] [Google Scholar]
- 38.Healy GN, Wijndaele K, Dunstan DW, et al. Objectively measured sedentary time, physical activity, and metabolic risk the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Diabetes Care. 2008;31(2):369–371. doi: 10.2337/dc07-1795. [DOI] [PubMed] [Google Scholar]
- 39.Wijndaele K, Beunen G, Duvigneaud N, et al. A Continuous Metabolic Syndrome Risk Score. Diabetes Care. 2006;29(10):2329. doi: 10.2337/dc06-1341. October 2006. [DOI] [PubMed] [Google Scholar]
- 40.Tang K, Beaton DE, Boonen A, Gignac MA, Bombardier C. Measures of work disability and productivity: Rheumatoid Arthritis Specific Work Productivity Survey (WPS-RA), Workplace Activity Limitations Scale (WALS), Work Instability Scale for Rheumatoid Arthritis (RA-WIS), Work Limitations Questionnaire (WLQ), and Work Productivity and Activity Impairment Questionnaire (WPAI) Arthritis care & research. 2011;63(S11):S337–S349. doi: 10.1002/acr.20633. [DOI] [PubMed] [Google Scholar]
- 41.Zhang W, Bansback N, Boonen A, Young A, Singh A, Anis AH. Validity of the work productivity and activity impairment questionnaire-general health version in patients with rheumatoid arthritis. Arthritis research & therapy. 2010;12(5):1. doi: 10.1186/ar3141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4(5):353–365. doi: 10.2165/00019053-199304050-00006. [DOI] [PubMed] [Google Scholar]
- 43.Schaufeli WB, Salanova M, González-Romá V, Bakker AB. The measurement of engagement and burnout: A two sample confirmatory factor analytic approach. Journal of Happiness studies. 2002;3(1):71–92. [Google Scholar]
- 44.Schaufeli WB, Bakker AB. Occupational Health Psychology Unit. Utrecht: Utrecht University; 2003. Utrecht work engagement scale: Preliminary manual. [Google Scholar]
- 45.Seppälä P, Mauno S, Feldt T, et al. The construct validity of the Utrecht Work Engagement Scale: Multisample and longitudinal evidence. Journal of Happiness Studies. 2009;10(4):459–481. [Google Scholar]
- 46.Scarpello V, Campbell JP. Job satisfaction: Are all the parts there? Personnel psychology. 1983;36(3):577–600. [Google Scholar]
- 47.Dolbier CL, Webster JA, McCalister KT, Mallon MW, Steinhardt MA. Reliability and validity of a single-item measure of job satisfaction. American Journal of Health Promotion. 2005;19(3):194–198. doi: 10.4278/0890-1171-19.3.194. [DOI] [PubMed] [Google Scholar]
- 48.Peterson M, N D, SD S, A F, MA P. The Obesity Society. Boston, MA: 2014. Validation of an On-line 24-Hour Physical Activity Recall. [Google Scholar]
- 49.Chau JY, van der Ploeg HP, Dunn S, Kurko J, Bauman AE. A tool for measuring workers’ sitting time by domain: the Workforce Sitting Questionnaire. British Journal of Sports Medicine. 2011 doi: 10.1136/bjsports-2011-090214. bjsports-2011-090214. [DOI] [PubMed] [Google Scholar]
- 50.Subar AF, Kirkpatrick SI, Mittl B, et al. The Automated Self-Administered 24-hour dietary recall (ASA24): a resource for researchers, clinicians, and educators from the National Cancer Institute. J Acad Nutr Diet. 2012 Aug;112(8):1134–1137. doi: 10.1016/j.jand.2012.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kirkpatrick SI, Subar AF, Douglass D, et al. Performance of the Automated Self-Administered 24-hour Recall relative to a measure of true intakes and to an interviewer-administered 24-h recall. Am J Clin Nutr. 2014 Jul;100(1):233–240. doi: 10.3945/ajcn.114.083238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dawson AP, Steele EJ, Hodges PW, Stewart S. Development and test-retest reliability of an extended version of the Nordic Musculoskeletal Questionnaire (NMQ-E): a screening instrument for musculoskeletal pain. The Journal of Pain. 2009;10(5):517–526. doi: 10.1016/j.jpain.2008.11.008. [DOI] [PubMed] [Google Scholar]
- 53.Cook TD, Campbell DT. The causal assumptions of quasi-experimental practice. Synthese. 1986;68(1):141–180. [Google Scholar]
- 54.Murray DM. Design and analysis of group-randomized trials. Vol. 29. Oxford University Press; 1998. [Google Scholar]
- 55.Cohen J. A power primer. Psychological Bulletin. 1992;112(1):155. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]