Abstract
Background
Stigma is associated with many negative health outcomes. Research has examined perceived and internalized stigma in individuals with irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD), but less has been done to evaluate levels of enacted stigma associated with these conditions. The aim of this study was to evaluate the presence of enacted stigma toward IBS and IBD in the general population compared to an adult-onset asthma (AOA) control group.
Methods
Participants were recruited via social media and a research-dedicated website and completed all measures online. Participants were randomized to one of six clinical vignettes: (i) IBD male, (ii) IBD female, (iii) IBS male, (iv) IBS female, (v) AOA male, or (vi) AOA female. Participants read the assigned vignette and then completed measures of emotional empathy, level of familiarity, and enacted stigma.
Key Results
Participants reported higher levels of enacted stigma toward IBS compared to both IBD and AOA. No differences in stigma were found between IBD and AOA. Higher levels of familiarity were most strongly correlated with reduced IBD-related stigma, with weaker but still significant correlations between level of familiarity and IBS and AOA. Higher levels of emotional empathy were associated with reduced stigma for IBD, IBS, and AOA.
Conclusions & Inferences
Individuals with IBS experience greater levels of enacted stigma compared to IBD and AOA. This finding is consistent with previous research that has shown greater levels of perceived and internalized stigma in IBS compared to IBD.
Keywords: discriminatory behavior, enacted stigma, inflammatory bowel disease, irritable bowel syndrome, patient outcomes
1 | INTRODUCTION
Many individuals with chronic medical conditions experience stigma, or the labeling of a person as different or defective because of a perceived trait.1,2 Research on stigma has focused primarily on mental health3,4 and other chronic illnesses such as HIV/AIDS,5,6 cancers,7,8 epilepsy,9,10 and obesity.11,12 Stigma is associated with a multitude of negative health outcomes, including increased illness symptoms, psychological distress, and treatment non-adherence, and decreased self-esteem, self-efficacy, and access to medical care.13–16 Stigma is frequently conceptualized into three domains: perceived, internalized, and enacted.17 Perceived stigma refers to how an individual senses that others hold negative attitudes or beliefs toward oneself or one’s condition. When an individual accepts negative beliefs regarding his/her illness and incorporates those beliefs into his/her own identity, this is known as internalized stigma. Enacted stigma refers to discriminatory acts or negative attitudes that one may experience as a result of his or her illness.
Irritable bowel syndrome (IBS) is a functional gastrointestinal disorder that is characterized by symptoms of pain, bloating, gas, and diarrhea or constipation, which are not associated with any known structural or tissue abnormalities. Inflammatory bowel diseases (IBD; Crohn’s disease, ulcerative colitis) are chronic digestive diseases that present with symptoms similar to those found in IBS, but are associated with inflammation to all or some of the digestive tract. Due to societal taboos around discussions of bowel functioning, and historically viewing these disorders as psychosomatic, individuals with IBS and IBD may each experience stigma.
Research in IBS and IBD has previously been conducted for perceived and internalized stigma but is lacking in the area of enacted stigma.18–20 One recent study of young adults with IBD found that the experience of perceived and enacted stigma frequently leads to patients choosing not to disclose or to attempt to conceal these conditions.21 Research on perceived stigma in IBS and IBD showed that perceived stigma negatively impacts clinical outcomes, including increased depression and anxiety, lower quality of life, and reduced self-esteem and self-efficacy.20 However, perceived stigma impacts these groups differently, as IBS patients were shown to perceive more stigma from their health care providers than patients with IBD. Internalized stigma in both conditions is associated with an increase in health care utilization and reductions in health-related quality of life, psychological functioning, and perception of health competence.18,22
In this study, we sought to evaluate stigmatizing attitudes (i.e., enacted stigma) toward patients with IBS and IBD in the general population, utilizing a validated experimental design in the HIV/AIDS literature.23,24 This design features vignettes depicting individuals with IBS, IBD, and adult-onset asthma (AOA). As AOA historically has not been associated with high levels of stigmatization, it was chosen as a patient control group.25 We hypothesize that participants will display greater stigma toward individuals with bowel disorders (IBS and IBD) than AOA. Based on previous research in perceived stigma toward functional disorders, we also hypothesize that participants will display greater stigma toward IBS than IBD.20,26
2 | METHODS
Potential participants were recruited via social media (Facebook, Twitter) and a research-dedicated website (researchmatch.org) between June and October 2014. Study questionnaires were administered online via the third party survey site www.surveymonkey.com. After obtaining informed consent, participants completed the following information:
2.1 | Demographic
Gender, race, ethnicity, education level, marital status, sexual orientation, employment status, geographic location, household income, and chronic illness status.
Participants were then randomized to one of six clinical vignettes: (i) IBD Male, (ii) IBD Female, (iii) IBS Male, (iv) IBS Female, (v) AOA Male, or (vi) AOA Female. The first paragraph of the vignette provided a brief description of each medical condition, followed by a description of a 28-year-old with that specific diagnosis (Appendix S1). After being presented with the clinical vignette, participants were asked to verify the name of the illness they just read about (IBS, IBD, or AOA).The following questionnaires were then administered:
2.1.1 | Level of Familiarity Scale (Disease Specific; LOF)
The LOF is an 11-item questionnaire that assesses a person’s degree of contact with people living with a specific illness.27 Participants are asked to check each item that applies (e.g., “I live with a person with Crohn’s Disease,” “A friend of the family has IBS.”). Each item is scored for the level of intimacy (11=most intimate contact, 7=medium intimacy, 1=little intimacy.). If more than one item is endorsed, the highest level of intimacy item is recorded (Maximum score=11).
2.1.2 | Enacted Stigma Scale (Disease Specific, ESS)
The ESS is a 30-item, study-specific questionnaire adapted from three stigma scales: Explanatory Model Interview Catalogue (EMIC) stigma scale for the community, the Perceived Stigma Scale for IBS (PSS-IBS), and the Internalized Stigma of Mental Illness (ISMI) stereotype endorsement subscale.28 The EMIC is a standard measure of illness stigma that has been modified for studies across multiple conditions.29 The PSS-IBS is a measure of GI-specific illness perceptions; items were modified to capture enacted stigma (e.g., “My IBS is believed to be more “in my head” than physical” to “Most symptoms people with IBS/IBD/Asthma experience are more in their head than physical”).30 Items are rated on a 5-point Likert scale (Strongly Disagree to Strongly Agree); higher scores denote greater enacted stigma (Maximum score=150). The ISMI is a measure of internalized stigma with five subscales; the stereotype endorsement scale measures how much a person agrees with stigmatizing attitudes (e.g., “Negative stereotypes about IBS/IBD keep me isolated from the “normal” world.”). The ESS demonstrated excellent reliability (Cronbach α: IBS=0.90, IBD=0.88, AOA=0.81).
2.1.3. | Attributions Questionnaire (Disease Specific, AQ-9)
The AQ-9 is 9-item measure of stereotype endorsement for a specific illness.31 Each item corresponds with a stereotype factor from the long version of the questionnaire (AQ-27): Blame, Anger, Pity, Help, Dangerousness, Fear, Segregation, and Coercion. Items are rated on a 1 (none at all) to 9 (very much) point scale. Higher scores denote greater stereotype endorsement. The AQ-9 is used to confirm construct validity of the ESS only.
2.1.4 | Interpersonal Reactivity Index (IRI)
The IRI is a 28-item measure of an individual’s degree of empathic capacity, or the ability to understand and share the feelings of another.32 Items are rated on a 5-Point Likert Scale (Does Not Describe Me Well to Describes Me Very Well). Higher scores denote greater empathy.
2.2 | Statistical analyses
All responses from the online system were exported into SPSS v. 22 for analyses. Total scores and means for each questionnaire were computed. Data were evaluated for normal distribution and completeness, with incomplete subjects removed from the study sample. Descriptive statistics (percentages, mean [Standard Deviation]) evaluated the demographic characteristics of the participants. Reliability statistics (Cronbach alpha, Guttman statistic) evaluated the internal consistency and split-half reliability of the ESS (reported in Methods section above) and Pearson’s correlation with the AQ-9 evaluated the construct validity of the ESS.
Participants’ response to item 5 of the LOF indicated whether he or she had a diagnosis of IBS, IBD, or AOA; participants were dichotomously categorized (Yes/No) if their diagnosis matched the diagnosis of the patient they were rating (e.g., participant with IBD randomized to IBD patient group=Yes, participant with IBS randomized to AOA=No). These groups were compared prior to additional analyses to determine if significant differences exist that may influence enacted stigma. Pearson’s correlations evaluated relationships between continuous demographic variables and study measures.
A series of independent samples t-tests and one-way Analysis of Variance (ANOVA) determined significant differences in mean scores for enacted stigma, level of familiarity, and emotional empathy for each demographic variable. Cohen’s d evaluated estimates of effect size for enacted stigma between IBS and IBD, IBS and AOA, and IBD and AOA. Additional Pearson’s correlations assessed relationships between stigma, level of familiarity, and emotional empathy. Stepwise linear regression evaluated the percentage variance in enacted stigma accounted for by diagnosis, level of familiarity, and emotional empathy (all variables entered in Step 1). Analysis of covariance (ANCOVA) measured the relationships between stigma, familiarity, and emotional empathy while controlling for any demographic variables with significant group differences. Finally, to evaluate differences by gender of the patient vignette IBS and IBD participants were matched to AOA gender controls for comparison. Based on Bonferroni correction, statistical significance was set to P≤.01 for t-tests and ANOVA to control for type 1 error due to multiple comparisons.
3 | RESULTS
Four hundred and twenty-four potential participants visited the study website and 420 consented. Of those, 392 completed all study questionnaires (93% completion rate). Participants were equally randomized across illness vignettes. Demographic characteristics are listed in Table 1. The majority of the sample was female, Caucasian, non-Hispanic, college educated, heterosexual, and employed at least part-time. All geographic regions of the United States were represented. One-third of participants had a chronic medical illness diagnosis.
TABLE 1.
Demographic characteristics of study sample
| Variable | N=392 |
|---|---|
| Gender | |
| Male | 31.4% (123) |
| Female | 68.4% (268) |
| Age (mean ± SD) | 34.5 ± 12.1 |
| Race | |
| Caucasian | 85.3% (326) |
| African American | 2.9% (11) |
| Other | 14.7% (45) |
| Ethnicity | |
| Hispanic | 18.5% (71) |
| Non-Hispanic | 81.5% (313) |
| Married/Co-Habitating | 50.5% (196) |
| Heterosexual | 94% (358) |
| College Educated | 71.5% (278) |
| Employed (at least part-time) | 72.6% (283) |
| Geographic Location | |
| New England | 6.6% (26) |
| Mid Atlantic | 9.0% (35) |
| East North Central | 23.0% (90) |
| West North Central | 5.6% (22) |
| South Atlantic | 12.5% (49) |
| East South Central | 8.7% (34) |
| West South Central | 5.6% (22) |
| Mountain | 17.1% (67) |
| Pacific | 6.4% (25) |
| Outside of USA | 5.4% (21) |
| Household income >50 000 USD per year | 54.8% (213) |
| Chronic illness diagnosis | 32.4% (127) |
| Illness randomization | |
| IBD male | 14% (55) |
| IBD female | 18.1% (71) |
| IBS male | 18.6% (73) |
| IBS female | 15.6% (61) |
| AOA male | 20.9% (82) |
| AOA female | 12.8% (50) |
| Positive diagnosisa | |
| IBD | 7.1% (28) |
| IBS | 4.1% (16) |
| AOA | 5.4% (21) |
Participant diagnosed with same illness assigned to rate via randomization as identified by Level of Familiarity Scale.
The ESS was a reliable and valid measure of enacted stigma; reliability statistics for the ESS are reported above. The AQ-9 was strongly correlated with the ESS (r=.61, P<.001), supporting construct validity. Participants who were randomized to either the IBD or IBS vignette and self-disclosed having the same diagnosis they were rating (positive group) demonstrated significantly less enacted stigma than those who did not have the illness (IBD P<.001; IBS P<.01). No differences in enacted stigma were found for the AOA group and as such, diagnosis positive participants were excluded from enacted stigma analyses for IBS and IBD only. No differences existed between positive and negative diagnosis groups for emotional empathy for IBD, IBS, or AOA.
3.1 | Levels of enacted stigma by illness
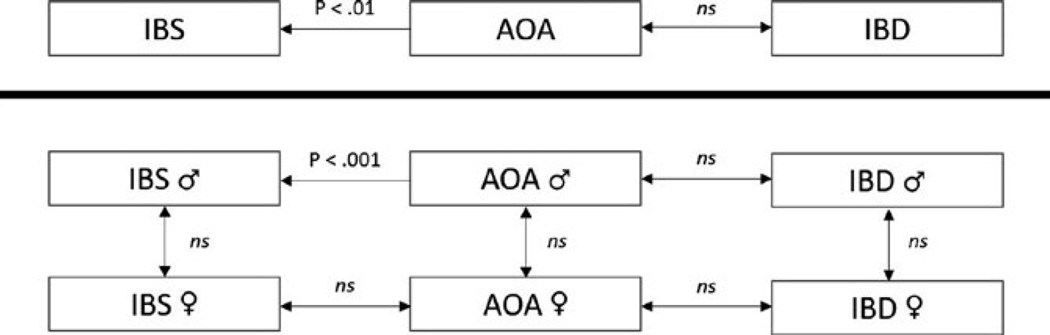
As a whole, participants reported significantly higher levels of enacted stigma toward IBS than IBD or AOA (Table 2). No differences existed for stigma between IBD and AOA (P>.05). Effect sizes when comparing the three groups were small for IBD compared to AOA (d=0.26), medium for IBS compared to IBD (d=0.52), and large for IBS compared to AOA (d=0.79). Only one difference in stigma level existed when comparing IBS and IBD patients to gender-matched AOA controls in that males with IBS were significantly more stigmatized than males with AOA (P<.001). This comparison did not yield significant differences in females with IBS or males or females with IBD when compared to gender-matched AOA controls. Differences in enacted stigma did not exist between male and female patients for each illness group (e.g., IBS males vs IBS females) (Fig. 1).
TABLE 2.
Mean (SD) of enacted stigma, stereotype endorsement, level of familiarity, and emotional empathy by illness group
| IBD | IBS | AOA | F | P | |
|---|---|---|---|---|---|
| Level of familiarity | 6.5 (3.8) | 5.7 (3.8) | 7.9 (2.6) | 13.87 | .000a |
| Enacted stigma | 45.6 (10.6) | 51.9 (13.2) | 43.1 (8.5) | 18.57 | .000b |
| Stereotype endorsement | 17.8 (5.5) | 19.1 (7.6) | 18.2 (6.2) | 1.36 | .258 |
| Emotional empathy | 88.1 (11.9) | 86.3 (13.7) | 89.3 (13.0) | 1.45 | .237 |
AOA>both IBS and IBD.
IBS>both IBD and AOA.
FIGURE 1.
Differences in enacted stigma by diagnosis and gender of patient vignette
3.2 | Demographic differences in enacted stigma
Mean differences in enacted stigma by illness were compared for each categorical demographic variable shown in Table 1., with gender being the only variable demonstrating a significant difference. Specifically, male participants reported greater stigma toward IBD than women (P<.01). These gender differences exist for IBS and AOA (P<.05), however, they do not meet the level of significance set for this study. All other remaining demographic variables demonstrated no significant differences in levels of enacted stigma.
Next, we evaluated enacted stigma between male and female participants based on the gender of the patient in the vignette and found that male participants were more likely than female participants to stigmatize females with IBD and were more likely to stigmatize males with AOA (both P<.01). Male participants also stigmatized males with IBD more than female participants, however, this finding was above significance for this study (P=.05). No differences exist in stigmatizing attitudes by participant gender for females with AOA, or for males or females with IBS.
3.3 | Relationship between level of familiarity, emotional empathy, and enacted stigma
Overall, participants were significantly more familiar with AOA than IBD and IBS (P<.001), with similar levels of familiarity for IBS and IBD (Table 2). Higher levels of familiarity were most strongly correlated with reduced IBD-related stigma (r=−0.47, P<.001). Greater familiarity also correlated with less stigma in IBS (r=−0.24, P<.05) and AOA (r=−0.29, P<.05), however, the relationship was considerably weaker than that seen in the IBD group.
Levels of participant emotional empathy were consistent across illness groups. Participants who reported greater levels of emotional empathy were less likely to stigmatize each illness, with similar relationship sizes for IBD (r=−0.36, P<.01) and IBS (r=−0.33, P<.01), and a weaker yet significant relationship for AOA (r=−0.29, P<.05). Gender differences exist in levels of emotional empathy (male=82.79 ± 11.5, female=90.23 ± 12.9, P<.001), however, when controlling for gender in the relationship between emotional empathy and stigma, the relationship remained significant (P<.001).
Results from the regression model suggest level of familiarity contributes most to the variance in enacted stigma (R2adj=0.16; 16%), followed by emotional empathy (R2adj=0.08; 8%). The illness being rated was excluded from the model.
4 | DISCUSSION
In this study, we utilized a validated experimental design to evaluate enacted stigma toward individuals with IBS and IBD. We hypothesized that enacted stigma would be greater toward IBS and IBD than for the AOA control group, and that the greatest enacted stigma would be toward IBS, due to its functional nature. In line with our hypothesis, IBS received the greatest amount of enacted stigma, which is consistent with results from existing research. In a recent study by our group,18 there were greater levels of perceived stigma in individuals with IBS compared to those with IBD. Similarly, a 2004 study of functional somatic syndromes (FSS; including IBS) and matched medical controls groups (including IBD) found the FSS group perceived more stigma than the medical control group. We did not, however, find support for our prediction that there would be greater stigma toward IBD compared to AOA.
Effect sizes for IBS stigma compared to IBD and AOA demonstrate that IBS has a somewhat greater degree of stigma than a comparable condition (i.e., Crohn’s disease) and much greater stigma than asthma, a relatively non-stigmatized illness. A 1996 meta-analysis of HIV/AIDS-related stigma found a modest effect size (d=0.45) when compared to other stigmatized illnesses such as cancer, heart disease, and diabetes.33 Research on workplace stigma toward obese individuals finds moderate effect sizes (d=−0.52) compared with the non-obese.34 Based on these data, IBS is at comparable risk for stigmatization as HIV and obesity; IBD is at considerably lower risk for stigmatization than these highly stigmatized groups, but at greater risk than asthma.
Participants with greater emotional empathy were less likely to stigmatize each illness, with a similar relationship size for IBS and IBD, and a small but significant relationship in AOA. Significant differences exist by participant gender in emotional empathy, with women demonstrating more emotional empathy than men. However, we found the relationship between emotional empathy and stigma remained after controlling for this gender difference.
Historically, many studies utilizing the vignette design studied HIV/AIDS-related stigma and prejudice, and have primarily been done outside of the USA35–39 Some of these studies centered on disentangling stigma toward the HIV/AIDS diagnosis from stigma regarding its mode of transmission (e.g., men who have sex with men, injecting drug use, commercial sex, blood transfusion), particularly among health care workers.37,39,40 In one study looking at prejudice among Chinese medical students, more prejudice was directed toward individuals who were injecting drug users or involved in commercial sex, regardless of whether they had AIDS or leukemia, than those who had contracted HIV from a blood transfusion.39
Similarly, studies conducted within the United States on obesity-related stigma show an association between stigma and perceived responsibility or control over development of the condition.41,42 In a 2013 study, vignettes depicted individuals with anorexia nervosa, bulimia nervosa, binge eating disorder, major depressive disorder, and obesity.43 Obese individuals were blamed more than individuals with any other condition, and both obese individuals and those with binge eating disorder were seen as more responsible for their condition due to perceived lack of self-discipline. Findings from both HIV/AIDs and obesity-related stigma literature align with the ideas presented in Jones et al.’s seminal work that postulated that the perception of responsibility for contracting an illness leads to greater stigma and prejudicial attitudes. Patients with IBS report attitudes related to “my IBS is all in my head” and “my IBS is caused by something I have done” implying controllability in illness.30 Thus, others may perceive that IBS is caused by something people are doing, such as how they manage stress, the food they choose to eat, or other lifestyle factors that they are perceived to have control over.
Most stigma studies in the United States, have focused on mental illness. In a 2015 study, vignettes presented individuals with schizophrenia, depression, prescription pain medication addiction, and heroin addiction, and these were described as either being untreated or treated.44 Participants endorsed more enacted stigma (e.g., less willingness to work closely with them at a job) toward individuals with untreated heroin addiction, depression, and schizophrenia compared to a control group. In the current study, IBS, a condition traditionally viewed as a psychosomatic condition associated with more anxiety, depression, and neuroticism compared to IBD and AOA was the most stigmatized.45–47 This result is supported by the concept of level of peril, outlined by Jones et al.48 Peril focuses on perceived dangers associated with stigmatized individuals, such as the threat of individuals with mental disorders engaging in a verbal or physical attack. In addition, this concept relates to how encountering stigmatized individuals makes us “starkly aware of our own frailty”.48 Individuals with IBS in the current study may have been associated with a higher level of peril due to the association it has with mental health issues, such as anxiety, depression and neuroticism. Also, as IBS is a poorly understood condition, especially among the lay community, it may be associated with greater peril than IBD which has more a definitive etiology and significantly lower prevalence rate than IBS.
Another vignette study of US college students showed that both younger students and those with less familiarity with mental illness were more likely to stigmatize and maintain social distance from mentally ill individuals.49 In our study we found that higher levels of familiarity were associated with reduced stigma in individuals with IBD, and this was seen to a lesser, but significant, degree in IBS and AOA. Antistigma interventions and campaigns tend to focus on education aimed at addressing this level of familiarity.50,51 Several patient advocacy groups exist for IBS and IBD (e.g., Crohn’s & Colitis Foundation of America, International Foundation for Functional GI Disorders) and could be leveraged by clinicians to counteract IBD-and IBS-related stigma.
When comparing stigma scores for IBS and IBD to gender-matched controls, the only difference existed for males with IBS scoring higher than males with asthma. Previous research indicates that women are perceived as less responsible for their illnesses than men52 and offered more support relative to men.53 As IBS is more prevalent in women,54 males with IBS may be the most prone to disease-related stigma. When evaluating the gender of the participant, male participants demonstrated the highest stigma levels across illness groups. Data are limited for evaluating gender differences in chronic illness enacted stigma, however, a 2008 study by Mosher et al.55 found that there were no gender differences in stigma toward cancer patients, including in levels of control over their condition. Conversely, in a study of obesity, men are more likely to attribute obesity to a lack of willpower and reported greater dislike of obese individuals, and hold a greater overall weight bias.56 Additional research in this area is warranted.
4.1 | Limitations
The sample was racially homogeneous and was primarily comprised of non-Hispanic Caucasians. Additionally, the sample was highly educated. Further research with minority populations and with varying education levels is needed to determine how findings may differ in these groups. An additional limitation is due to the survey methodology of this study. As with all survey studies, there is the potential for participants to bias their answers for social desirability, but the anonymity of the online administration may have corrected for that potential. We do not know the overall rates of IBD, IBS, or AOA in our study sample. Based on those in the positive diagnosis group, IBS and AOA fell at or below national prevalence rates (IBS=6% based on Rome IV criteria, AOA=8%) while IBD was significantly higher than that found in the general population (less than 1% versus 7% of study sample). This may limit the generalizability of our findings to the broader US population.
Future studies should aim to evaluate perceived stigma in patients and enacted stigma in identified significant others, both interpersonal and health care providers, to determine the congruence of these phenomena. Evaluations of existing educational programs available via patient advocacy groups should be conducted in a more systematic way to measure stigma levels pre-and postintervention.
Key Points.
Chronic illness stigma is a salient issue in gastrointestinal disease. Enacted stigma, or discriminatory actions or attitudes, toward inflammatory bowel disease and irritable bowel syndrome (IBS) has yet to be evaluated.
This study finds that patients with IBS, specifically males, experience the most enacted stigma from people in the general population even though people are generally equally familiar with both conditions.
Irritable bowel syndrome patients report feeling stigmatized and this study corroborates that people without IBS hold negative attitudes toward the illness. Health care providers should be aware of the presence of stigma in IBS patients and its potential impact of patient outcomes.
Acknowledgments
FUNDING
This study was partially supported by the T32DK101363 training grant in Gastrointestinal Physiology and Psychology.
Footnotes
CONFLICTS OF INTEREST
The authors have no competing interests to disclose.
AUTHOR CONTRIBUTION
TT and JN were responsible for study design and data collection; TT performed the statistical analysis; TT and AB wrote the manuscript; JN and LK assisted with data interpretation and manuscript preparation.
SUPPORTING INFORMATION
Additional Supporting Information may be found online in the supporting information tab for this article.
REFERENCES
- 1.Link BG, Phelan JC. Stigma and its public health implications. The Lancet. 2006;367:528–529. doi: 10.1016/S0140-6736(06)68184-1. [DOI] [PubMed] [Google Scholar]
- 2.Link B, Struening E, Rahav M, Phelan J, Nuttbrock L. On stigma and its consequences: evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. J Health Soc Behav. 1997;38:177–190. [PubMed] [Google Scholar]
- 3.Parcesepe AM, Cabassa LJ. Public stigma of mental illness in the United States: a systematic literature review. Adm Policy Ment Health. 2013;40:384–399. doi: 10.1007/s10488-012-0430-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abdullah T, Brown TL. Mental illness stigma and ethnocultural beliefs, values, and norms: an integrative review. Clin Psychol Rev. 2011;31:934–948. doi: 10.1016/j.cpr.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 5.Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J Int AIDS Soc. 2013;16(suppl 2):18734. doi: 10.7448/IAS.16.3.18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smit PJ, Brady M, Carter M, et al. HIV-related stigma within communities of gay men: a literature review. AIDS care. 2012;24:405–412. doi: 10.1080/09540121.2011.613910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marlow LA, Waller J, Wardle J. Does lung cancer attract greater stigma than other cancer types? Lung Cancer. 2015;88:104–107. doi: 10.1016/j.lungcan.2015.01.024. [DOI] [PubMed] [Google Scholar]
- 8.Mutebi M, Edge J. Stigma, survivorship and solutions: addressing the challenges of living with breast cancer in low-resource areas. S Afr Med J. 2014;104:383. doi: 10.7196/samj.8253. [DOI] [PubMed] [Google Scholar]
- 9.Bautista RE, Shapovalov D, Shoraka AR. Factors associated with increased felt stigma among individuals with epilepsy. Seizure. 2015;30:106–112. doi: 10.1016/j.seizure.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 10.Leaffer EB, Hesdorffer DC, Begley C. Psychosocial and sociodemographic associates of felt stigma in epilepsy. Epilepsy Behav. 2014;37:104–109. doi: 10.1016/j.yebeh.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 11.Papadopoulos S, Brennan L. Correlates of weight stigma in adults with overweight and obesity: A systematic literature review. Obesity (Silver Spring) 2015;23:1743–1760. doi: 10.1002/oby.21187. [DOI] [PubMed] [Google Scholar]
- 12.Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16:319–326. doi: 10.1111/obr.12266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carter-Harris L. Lung cancer stigma as a barrier to medical help-seeking behavior: practice implications. J Am Assoc Nurse Pract. 2015;27:240–245. doi: 10.1002/2327-6924.12227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Drapalski AL, Lucksted A, Perrin PB, et al. A model of internalized stigma and its effects on people with mental illness. Psychiatr Serv. 2013;64:264–269. doi: 10.1176/appi.ps.001322012. [DOI] [PubMed] [Google Scholar]
- 15.Else-Quest NM, LoConte NK, Schiller JH, Hyde JS. Perceived stigma, self-blame, and adjustment among lung, breast and prostate cancer patients. Psychol Health. 2009;24:949–964. doi: 10.1080/08870440802074664. [DOI] [PubMed] [Google Scholar]
- 16.Bogart LM, Wagner GJ, Green HD, Mutchler MG, Klein DJ, McDavitt B. Social network characteristics moderate the association between stigmatizing attributions about HIV and non-adherence Among Black Americans living with HIV: a longitudinal assessment. Ann Behav Med. 2015;49:865–872. doi: 10.1007/s12160-015-9724-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Earnshaw V, Quinn D. The impact of stigma in healthcare on people living with chronic illnesses. J Health Psychol. 2012;17:157–168. doi: 10.1177/1359105311414952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Taft TH, Riehl ME, Dowjotas KL, Keefer L. Moving beyond perceptions: internalized stigma in the irritable bowel syndrome. Neurogastroenterol Motil. 2014;26:1026–1035. doi: 10.1111/nmo.12357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taft T, Keefer L, Leonhard C, Nealon-Woods M. Impact of perceived stigma on inflammatory bowel disease patient outcomes. Inflamm Bowel Dis. 2009;15:1224–1232. doi: 10.1002/ibd.20864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taft T, Keefer L, Artz C, Bratten J, Jones M. Perceptions of illness stigma in patients with inflammatory bowel disease and irritable bowel syndrome. Qual Life Res. 2011;20:1391–1399. doi: 10.1007/s11136-011-9883-x. [DOI] [PubMed] [Google Scholar]
- 21.Saunders B. Stigma, deviance and morality in young adults’ accounts of inflammatory bowel disease. Sociol Health Illn. 2014;36:1020–1036. doi: 10.1111/1467-9566.12148. [DOI] [PubMed] [Google Scholar]
- 22.Taft TH, Ballou S, Keefer L. A preliminary evaluation of internalized stigma and stigma resistance in inflammatory bowel disease. J Health Psychol. 2013;18:451–460. doi: 10.1177/1359105312446768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li L, Zunyou W, Yu Z, Chunqing L, Roger D, Sheng W. Using case vignettes to measure HIV-related stigma among health professionals in China. Int J Epidemiol. 2007;36:178–184. doi: 10.1093/ije/dyl256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mahmood A, Khatoon F, Ali M, Iqbal T, Rahim Irshad QM. Attitude of medical students towards AIDS and leukemia patients. Pak J Med Sci. 2012;28:187–191. [Google Scholar]
- 25.Snadden D, Brown JB. Asthma and stigma. Fam Pract. 1991;8:329–335. doi: 10.1093/fampra/8.4.329. [DOI] [PubMed] [Google Scholar]
- 26.Looper KJ, Kirmayer LJ. Perceived stigma in functional somatic syndromes and comparable medical conditions. J Psychosom Res. 2004;57:373–378. doi: 10.1016/j.jpsychores.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 27.Holmes EP, Corrigan PW, Williams P, Canar J, Kubiak MA. Changing attitudes about schizophrenia. Schizophr Bull. 1999;25:447–456. doi: 10.1093/oxfordjournals.schbul.a033392. [DOI] [PubMed] [Google Scholar]
- 28.Boyd Ritsher J, Otilingam PG, Grajales M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res. 2003;121:31–49. doi: 10.1016/j.psychres.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 29.van Brakel WH, Sihombing B, Djarir H, et al. Disability in people affected by leprosy: the role of impairment, activity, social participation, stigma and discrimination. Global Health Action. 2012;5:1–11. doi: 10.3402/gha.v5i0.18394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jones MP, Keefer L, Bratten J, et al. Development and initial validation of a measure of perceived stigma in irritable bowel syndrome. Psychol Health Med. 2009;14:367–374. doi: 10.1080/13548500902865956. [DOI] [PubMed] [Google Scholar]
- 31.Corrigan P, Markowitz FE, Watson A, Rowan D, Kubiak MA. An attribution model of public discrimination towards persons with mental illness. J Health Soc Behav. 2003;44:162–179. [PubMed] [Google Scholar]
- 32.Davis MH. Measuring individual differences in empathy: evidence for a multidimensional approach. J Pers Soc Psychol. 1983;44:113–126. [Google Scholar]
- 33.Crawford AM. Stigma associated with AIDS: a meta-analysis. J Appl Soc Psychol. 1996;26:398–416. [Google Scholar]
- 34.Rudolph CW, Wells CL, Weller MD, Baltes BB. A meta-analysis of empircal studies of weight-based bias in the workplace. J Vocat Behav. 2009;74:1–10. [Google Scholar]
- 35.Drewes J, Kleiber D. Contagiousness under antiretroviral therapy and stigmatization toward people with HIV. AIDS Care. 2014;26:1383–1386. doi: 10.1080/09540121.2014.913768. [DOI] [PubMed] [Google Scholar]
- 36.Lawson KL, Bayly M, Cey E. Judgements regarding the acceptability of childbearing and parental fitness made towards women living with HIV. AIDS Care. 2013;25:676–679. doi: 10.1080/09540121.2012.748162. [DOI] [PubMed] [Google Scholar]
- 37.Rogers SJ, Tureski K, Cushnie A, Brown A, Bailey A, Palmer Q. Layered stigma among health-care and social service providers toward key affected populations in Jamaica and The Bahamas. AIDS Care. 2014;26:538–546. doi: 10.1080/09540121.2013.844762. [DOI] [PubMed] [Google Scholar]
- 38.Chan KY, Stoové MA, Sringernyuang L, Reidpath DD. Stigmatization of AIDS patients: disentangling Thai nursing students’ attitudes towards HIV/AIDS, drug use, and commercial sex. AIDS Behav. 2007;12:146–157. doi: 10.1007/s10461-007-9222-y. [DOI] [PubMed] [Google Scholar]
- 39.Chan KY, Yang Y, Li Z-R, Stoove MA, Reidpath DD. Interrelationships between HIV/AIDS and risk behavior prejudice among medical students in southern China. Curr HIV Res. 2009;7:606–611. doi: 10.2174/157016209789973655. [DOI] [PubMed] [Google Scholar]
- 40.Chan KY, Yang Y, Zhang K-L, Reidpath DD. Disentangling the stigma of HIV/AIDS from the stigmas of drugs use, commercial sex and commercial blood donation - a factorial survey of medical students in China. BMC Public Health. 2007;7:1–12. doi: 10.1186/1471-2458-7-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Frederick DA, Saguy AC, Gruys K. Culture, health, and bigotry: How exposure to cultural accounts of fatness shape attitudes about health risk, health policies, and weight-based prejudice. Soc Sci Med. 2015 doi: 10.1016/j.socscimed.2015.12.031. Published online. [DOI] [PubMed] [Google Scholar]
- 42.Puhl RM, Schwartz MB, Brownell KD. Impact of perceived consensus on stereotypes about obese people: a new approach for reducing bias. Health Psychol. 2005;24:517–525. doi: 10.1037/0278-6133.24.5.517. [DOI] [PubMed] [Google Scholar]
- 43.Ebneter DS, Latner JD. Stigmatizing attitudes differ across mental health disorders: a comparison of stigma across eating disorders, obesity, and major depressive disorder. J Nerv Ment Dis. 2013;201:281–285. doi: 10.1097/NMD.0b013e318288e23f. [DOI] [PubMed] [Google Scholar]
- 44.McGinty EE, Goldman HH, Pescosolido B, Barry CL. Portraying mental illness and drug addiction as treatable health conditions: effects of a randomized experiment on stigma and discrimination. Soc Sci Med. 2015;126:73–85. doi: 10.1016/j.socscimed.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 45.Hazlett-Stevens H, Craske MG, Mayer EA, Chang L, Naliboff BD. Prevalence of irritable bowel syndrome among university students: the roles of worry, neuroticism, anxiety sensitivity and visceral anxiety. J Psychosom Res. 2003;55:501–505. doi: 10.1016/s0022-3999(03)00019-9. [DOI] [PubMed] [Google Scholar]
- 46.Tayama J, Nakaya N, Hamaguchi T, et al. Effects of personality traits on the manifestations of irritable bowel syndrome. BioPsychoSoc Med. 2012;6:1–8. doi: 10.1186/1751-0759-6-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Farnam A, Somi MH, Sarami F, Farhang S, Yasrebinia S. Personality factors and profiles in variants of irritable bowel syndrome. World J Gastroenterol. 2007;13:6414–6418. doi: 10.3748/wjg.v13.i47.6414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jones E, Farina A, Hastorf A, Markus H, Miller D, Scott R. Social Stigma: The Psychology of Marked Relationships. New York: W.H. Freeman and Company; 1984. [Google Scholar]
- 49.Feeg VD, Prager LS, Moylan LB, Smith KM, Cullinan M. Predictors of mental illness stigma and attitudes among college students: using vignettes from a campus common reading program. Issues Ment Health Nurs. 2014;35:694–703. doi: 10.3109/01612840.2014.892551. [DOI] [PubMed] [Google Scholar]
- 50.Corrigan PW, Green A, Lundin R, Kubiak MA, Penn DL. Familiarity with and social distance from people who have serious mental illness. Psychiatr Serv. 2001;52:953–958. doi: 10.1176/appi.ps.52.7.953. [DOI] [PubMed] [Google Scholar]
- 51.Angermeyer MC, Matschinger H. The effect of personal experience with mental illness on the attitude towards individuals suffering from mental disorders. Soc Psychiatry Psychiatr Epidemiol. 1996;31:321–326. doi: 10.1007/BF00783420. [DOI] [PubMed] [Google Scholar]
- 52.Borchert J, Rickabaugh CA. When illness is perceived as controllable: the effects of gender and mode of transmission on AIDS-related stigma. Sex Roles. 1995;33:657. [Google Scholar]
- 53.Schulte A. Consensus versus disagreement in disease-related stigma: a comparison of reactions to AIDS and cancer patients. Sociol Perspect. 2002;45:81–104. [Google Scholar]
- 54.Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol. 2012;10:712–721. doi: 10.1016/j.cgh.2012.02.029. [DOI] [PubMed] [Google Scholar]
- 55.Mosher CE, Danoff-Burg S. An attributional analysis of gender and cancer-related stigma. Sex Roles. 2008;59:827–838. [Google Scholar]
- 56.Lieberman DL, Tybur JM, Latner JD. Disgust sensitivity, obesity stigma, and gender: contamination psychology predicts weight bias for women, not men. Obesity. 2012;20:1803–1814. doi: 10.1038/oby.2011.247. [DOI] [PubMed] [Google Scholar]