Short abstract
The DOTS (“directly observed treatment, short course”) strategy has been successfully used in developing countries to provide effective control of tuberculosis. Field workers in Malawi are promoting the same approach for HIV infection through the expansion of highly active antiretroviral therapy
Highly active antiretroviral therapy (HAART) must be expanded in sub-Saharan Africa, where the HIV/AIDS epidemic is taking an appalling toll. Malawi, a small, poor African country, is expanding HAART nationally. The “directly observed treatment, short course” (DOTS) strategy has been successfully used for years to provide effective national control of tuberculosis, and the same concepts are being applied for delivering HAART. We describe how the principles of standardised case finding, standardised treatment regimens, regular monitoring and evaluation, and uninterrupted supplies of drugs can be used to deliver HAART. If implemented well, these principles should ensure a controlled delivery system, which would reduce the risks of inconsistent prescribing practices and the development of drug resistance.
Response to Malawi's HIV/AIDS epidemic
In 2003 sub-Saharan Africa had an estimated 3.4 million new cases of HIV infection and up to 2.4 million deaths.1 Malawi has one of the highest HIV/AIDS prevalence rates in sub-Saharan Africa, with 14% of those aged 15-49 years infected.2 In 2003 an estimated 900 000 people had HIV/AIDS and about 86 000 died from AIDS related illnesses. AIDS is killing young adults in their most productive years, retarding development, producing a huge orphan population, and creating the foundations for political instability.
HAART has dramatically improved the survival of patients with HIV/AIDS in developed countries,3,4 where AIDS is now regarded as a potentially treatable and chronic condition rather than a fatal disease. In Malawi 170 000 people are estimated to need HAART.2 A countrywide survey by the Ministry of Health, however, found that just over 4000 people had started on HAART in the public and private sectors in 2003 and about 5000 were taking the medications at the start of 2004.5 A fast track approach to expanding treatment is urgently needed.
Fast countrywide expansion of HAART
The World Health Organization in September 2003 declared the lack of access to HAART a global health emergency.6 The organisation called for ambitious and unprecedented action to ensure that by the end of 2005 at least three million people needing HAART in developing countries would have access to it—the so called “3 by 5” initiative. Malawi has developed a two year (2004-5) antiretroviral expansion plan, with the goal of delivering HAART to 80 000 eligible patients in the country by the end of 2005. The plan wants antiretroviral drugs to be supplied free to as many eligible patients as possible. It provides a detailed outline of how antiretrovirals will be made available in a total of 54 central, district, and mission hospitals in the country by December 2004.
Learning from tuberculosis control
The delivery of antiretrovirals, according to standards practised in developed countries, requires high levels of expertise and technology. Malawi is one of the world's poorest countries, with a huge human resources deficit and about $12 (£7; €10) per head of population spent annually on health.7 The country does not have the human or technological resources to offer many different HAART regimens to patients or the means to assess and monitor patients by measuring viral load and CD4 lymphocyte counts.
Through the efforts of organisations such as WHO and the International Union Against Tuberculosis and Lung Disease, DOTS (similarly demanding of expertise and technology in developed countries) has been administered to millions of patients with tuberculosis in poor countries.8 Malawi has run an effective DOTS tuberculosis control programme for 20 years, providing diagnosis by a simple algorithm based on sputum smear microscopy and treatment regimens recommended by WHO. A rigorous system of monitoring and evaluation enables information to be collected nationally on case finding and treatment outcome. Every year up to 27 000 patients access the treatment, with acceptable success rates.9
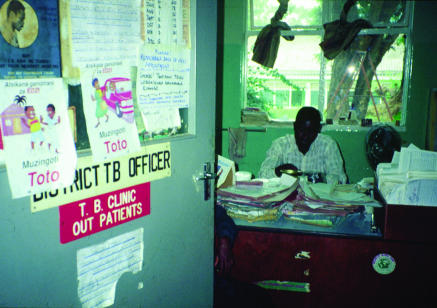
The Malawi tuberculosis control programme is run by paramedical staff; health assistants working as district tuberculosis officers and clinical officers working as regional tuberculosis officers provide supervisory and monitoring roles (figure). The key to success is standardisation. Every treatment facility operates in the same way, and all regional officers conduct supervision using the same tools and procedures. Tuberculosis treatment and HAART are both taken for a long time (eight months for tuberculosis, for life for HAART). The delivery of HAART has much to learn from the tuberculosis services,10 and we have developed a national plan to expand delivery of antiretrovirals.
Figure 1.
District tuberculosis officers in Malawi help to implement the country's tuberculosis control programme
Framework for delivering antiretrovirals
As for DOTS, we have developed a framework for delivering antiretrovirals that consists of a goal, specific objectives, a strategy, a policy package, key operations, and indicators (box 1) to measure progress with antiretroviral therapy. National guidelines for such treatment are available, and progress has already been made. At the moment there are 23 antiretroviral clinics in the public health sector delivering HAART, with the number scheduled to increase to 54 by the end of the year. So far, 375 healthcare workers in the public sector have been trained to use HAART, with the number expected to increase by an additional 100 by the end of 2004.
Eligibility criteria for treatments when resources are limited
The commonest type of tuberculosis in Malawi is pulmonary disease. The diagnostic algorithm stipulates that all people suspected of having pulmonary disease (defined as having a cough for three or more weeks) have sputum smears examined for the presence of acid-fast bacilli. Patients with acid-fast bacilli in their sputum are registered as smear positive for pulmonary disease, whereas those without are registered as smear negative pulmonary disease if they fulfil certain other criteria.11
Box 1: Indicators to measure progress with delivery of antiretroviral drugs
Input indicators
A guidelines manual for delivering antiretroviral therapy
Number of HIV clinics administering such therapy
Number of staff trained and accredited in use of antiretroviral drugs
Antiretroviral drugs and HIV test kits always available in hospital pharmacies, and uninterrupted supplies of the drugs to patients
Output indicators
Number of patients who start on standardised antiretroviral therapy
Number of patients who are still alive—and still taking the therapy—at a given time
Percentage of patients who show 95% adherence to the therapy
Percentage of patients having antiretroviral therapy who have returned to work
Number of new orphans registered each year in a district in which antiretroviral therapy is available
This simple approach recognises the fact that mycobacterial culture is not feasible in peripheral units but that light microscopes and trained microscopy staff are available. In a similar vein, simple criteria have been developed for assessing eligibility for HAART. An essential criterion is a documented positive HIV serology test, ascertained by whole blood rapid tests for HIV-1 and HIV-2. Adult patients known to be HIV seropositive and who have understood the implications of antiretroviral therapy are eligible for HAART if they are assessed as being in clinical stages III or IV as classified by WHO,12 in clinical stage II with total lymphocyte count < 1200x106/l or have a CD4 count < 200x106/l. Most antiretroviral clinics will have no access to CD4 counts and will therefore start patients on therapy on the basis of clinical criteria. In staff training, the diagnosis of opportunistic infections and correct staging of disease are strongly emphasised.
Standardised antiretroviral therapy
Malawi has stipulated its first line, alternative first line, and second line HAART regimens (box 2). For rapid countrywide expansion, the country has adopted the first line regimen only, except in the few centres where expertise already exists in using HAART regimens.
This new approach simplifies the management of patients, the whole system of recording and reporting, and drug procurement and drug security. It is based on observational experience in three sites that 85-90% of patients do well on this regimen. Patients who develop side effects will either stop treatment or be referred to the centres with more experienced staff who can use alternative first line therapy. Once antiretroviral clinics have shown they are competent to deliver the first line regimen, they will be assessed for their readiness to deliver alternative first line and second line regimens according to the national treatment guidelines.
The approach is borrowed from the tuberculosis treatment model, where five essential first line tuberculosis drugs are used in slightly different combinations to treat different forms of the disease. No investment has been made in expensive, toxic, and difficult to manage second line drugs for treating multidrug resistant tuberculosis, which is rare in Malawi owing mainly to good management with first line therapy.13
Good drug adherence and compliance with the treatment regimen are two essential components for successful treatment with either DOTS or HAART. In Malawi, guardians (spouses, members of the extended family, or sometimes children) have been used for several years to help patients with adherence and compliance with DOTS.14,15 The same principles are being applied to HAART. While evidence is growing that this may be a useful approach,16 not everyone is enthusiastic about its applicability.17
Registration, recording, and reporting
One of the important elements in preventing multidrug resistant tuberculosis is an uninterrupted supply of drugs. The number of cases registered nationally for treatment in the previous two quarters allows for realistic, six monthly procurement orders. (The number of cases is obtained from tuberculosis registers into which district tuberculosis officers enter the details of every patient registered for treatment.) The data in these registers are collated into quarterly reports on case finding, which in turn are put together into national reports. Standardised treatment outcomes of patients in these quarterly cohorts are also regularly evaluated using patient treatment cards, with reports on cure, death, default, and transfer-out being provided at treatment facilities and also nationally. The system is well tried, with no drug interruptions for years in Malawi and with regular reports on treatment outcome.
Malawi has adopted a similar system for monitoring antiretroviral therapy. Antiretroviral registers, patient master cards and forms for quarterly cohort analysis have already been used successfully in certain districts. The routinely collected data should allow regular, up to date information to be collected nationally on variables such as the number of patients ever started on HAART, the number alive, and the percentage of patients back in employment.
Box 2: Antiretroviral therapy regimens in Malawi
First line regimen
Stavudine plus lamivudine plus nevirapine
Alternative first line regimens in cases of adverse side effects
With severe peripheral neuropathy due to stavudine—use zidovudine plus lamivudine plus nevirapine
With hepatitis due to nevirapine—use stavudine plus lamivudine plus efavirenz
Severe skin reactions due to nevirapine—use stavudine plus lamivudine plus efavirenz
Second line regimen in the event of failure of first line regimen
Zidovudine plus didanosine plus nelfinavir
Summary points
The DOTS (“directly observed treatment, short course”) strategy for tuberculosis control is of proved effectiveness in resource poor countries
Expanding highly active antiretroviral therapy (HAART) in countries such as Malawi may be achieved using the same principles as for tuberculosis control programmes
These include the adoption of standard criteria for starting treatment and a reliable system for registering and monitoring cases and evaluating treatment outcomes
Conclusion
Expanding HAART in resource poor countries will be a major challenge. Even if the technical difficulties of delivering treatment can be solved, there is the additional problem of scarcity of skilled human resources, particularly in sub-Saharan Africa. In May 2004 Malawi launched a national in-service antiretroviral training programme, and five months later it had trained 375 medical officers, clinical officers, and nurses in antiretroviral management at a total cost of $85 000. With funds from WHO and the Global Fund against AIDS, Tuberculosis and Malaria, it plans to continue regular in-service training on HAART as well as integrating this topic into the undergraduate curriculum at the schools of medicine, health sciences, and nursing. Parallel to these attempts to increase the number of health workers able to manage HAART is an urgent need to tackle the national crisis in human resources, by producing more clinicians and nurses from training institutions and to retain those entering the service. The number of patients on HAART will after a few years far exceed those receiving tuberculosis treatment, and the human resource equation will be vital in determining success or failure of this intervention.
Some argue that rapid expansion in such an environment is fraught with danger and that HAART should rather be introduced in controlled settings through research programmes and improved infrastructure.18 This view ignores, however, the scale of the problem and the urgent need to provide lifesaving drugs to thousands of people. DOTS has a good track record for tuberculosis control in poor areas of the world, and if the same model for the delivery of antiretroviral drugs can be made to work at a national level, many lives can be saved and the risk of drug resistance kept low.
Supplementary Material
 A box of the five components of the DOTS strategy and a patient record chart for monitoring antiretroviral therapy are on bmj.com
A box of the five components of the DOTS strategy and a patient record chart for monitoring antiretroviral therapy are on bmj.com
Contributors and sources: All the authors have worked with several other partners on producing the national antiretroviral treatment guidelines and the national antiretroviral expansion plan, which they are now implementing. This article is based on the authors' collective country based experience and is supplemented by published, peer reviewed research on tuberculosis and antiretroviral therapy. Simon Makombe is an antiretroviral therapy officer in Malawi who has contributed considerably to the implemenation of the expansion programme.
Funding: ADH is supported by Family Health International, and EJS is supported by Management Sciences for Health. The national expansion of HAART will be funded mainly through the Global Fund to fight AIDS, Tuberculosis and Malaria.
Competing interests: None declared.
References
- 1.UNAIDS, World Health Organization. AIDS epidemic update. Geneva: UNAIDS/WHO, 2003. (UNAIDS/03.39E.)
- 2.National AIDS Commission. National estimate of HIV/AIDS in Malawi in 2003. Lilongwe, Malawi: National AIDS Commission Malawi, 2003.
- 3.Palella FJ, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. N Engl J Med 1998;338: 853-60. [DOI] [PubMed] [Google Scholar]
- 4.Mocroft A, Ledergerber B, Katlama C, Kirk O, Reiss P, d'Arminio Monforte A, et al. Decline in the AIDS and death rates in the EuroSIDA study: an observational study. Lancet 2003;362: 22-9. [DOI] [PubMed] [Google Scholar]
- 5.Chimzizi R, Harries A, Libamba E. Report of a country-wide survey of HIV/AIDS services in Malawi (for the year 2003). Lilongwe, Malawi: National Tuberculosis Control Programme and HIV/AIDS Unit, Ministry of Health, and National AIDS commission, 2004.
- 6.Jong-wook L. Global health improvement and WHO: shaping the future. Lancet 2003;362: 2083-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ministry of Health and Population. Malawi national health accounts: a broader perspective of the Malawian health sector. Lilongwe, Malawi: Ministry of Health, 2001.
- 8.World Health Organization. Treatment of tuberculosis. Guidelines for national programmes. Geneva: WHO, 2003. (WHO/CDS/TB/2003.313.)
- 9.World Health Organization. WHO report 2004. Global tuberculosis control surveillance, planning and financing. Geneva: WHO, 2004. (WHO/HTM/TB/2004.331.)
- 10.Harries AD, Nyangulu DS, Hargreaves NJ, Kaluwa O, Salaniponi FM. Preventing antiretroviral anarchy in sub-Saharan Africa. Lancet 2001;358: 410-4. [DOI] [PubMed] [Google Scholar]
- 11.Ministry of Health and Population. Manual of the national tuberculosis control programme of Malawi. 5th ed. Lilongwe, Malawi: Ministry of Health and Population, 2002.
- 12.World Health Organization. Scaling up antiretroviral therapy in resource-limited settings: treatment guidelines for a public health approach. Geneva: WHO, 2003. (Revision.)
- 13.Warndorff DK, Yates M, Ngwira B, Chagaluka S, Jenkins PA, Drobniewski F et al. Trends in antituberculosis drug resistance in Karonga district, Malawi, 1986-1998. Int J Tuberc Lung Dis 2000;4: 752-7. [PubMed] [Google Scholar]
- 14.Manders AJE, Banerjee A, van den Borne HW, Harries AD, Kok GJ, Salaniponi FML. Can guardians supervise TB treatment as well as health workers? A study on adherence during the intensive phase. Int J Tuberc Lung Dis 2001;5: 838-42. [PubMed] [Google Scholar]
- 15.Banerjee A, Harries AD, Mphasa N, Nyirenda TE, Veen J, Ringdal T, et al. Evaluation of a unified regimen for all new cases of tuberculosis using guardian-based supervision. Int J Tuberc Lung Dis 2000;4: 333-9. [PubMed] [Google Scholar]
- 16.Mitty JA, Stone VE, Sands M, Macalino G, Flanigan T. Directly observed therapy for the treatment of people with human immunodeficiency virus infection: a work in progress. Clin Infec Dis 2002;34: 984-90. [DOI] [PubMed] [Google Scholar]
- 17.Liechty CA, Bangsberg DR. Doubts about DOT: antiretroviral therapy for resource-poor countries. AIDS 2003;17: 1383-7. [DOI] [PubMed] [Google Scholar]
- 18.Stevens W, Kaye S, Corrah T. Antiretroviral therapy in Africa. BMJ 2004;328: 280-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.