Abstract
Objectives
To assess the association between job strain (JS) and the incidence of coronary heart disease (CHD) in North Italian employed men, adopting a stratified analysis by occupational class (OC).
Methods
The study was conducted on 4103 working men, CHD-free at baseline, enrolled in population-based and factory-based cohorts. Risk factor measurements and follow-up procedures were carried out adopting the WHO MONICA standardised procedures. OCs were derived from the Erikson-Goldthorpe-Portocarero classification. JS categories were defined based on overall sample medians of psychological job demand (PJD) and decision latitude (DL) derived from items of the Job Content Questionnaire, satisfying construct validity criteria. Age-adjusted and risk factors-adjusted CHD HRs were estimated from Cox models, contrasting high-strain (high PJD and low DL) versus non-high-strain categories.
Results
In a median follow-up of 14.6 years, 172 CHD events occurred, corresponding to a CHD incidence rate of 2.78/1000 person-years. In the overall sample, high-strain compared with non-high-strain workers evidenced a 39% excess CHD risk, not statistically significant. No association was found among managers and proprietors. Conversely, the HR of high strain versus non-high strain was 1.78 (95% CI 1.20 to 2.66) among non-manual and manual workers, with no substantial differences between them. The exclusion of the events occurring in the first 3 years of follow-up did not change the results. Adopting the quadrant-term JS groupings, among manual and non-manual workers, high-strain and active (high PJD and high DL) categories in comparison to the low strain one (low PJD and high DL) showed HRs of 2.92 and 2.47, respectively.
Conclusions
Our findings support the association of JS and CHD incidence among manual and non-manual workers. The non-high strain may not be the best reference category, when assessing the contribution of JS in determining CHD incidence.
Keywords: coronary heart disease, job strain, occupational class
Strengths and limitations of this study.
A recently published meta-analysis and subsequent papers have drastically reduced the role of job strain (JS), measured by the Job Content Questionnaire (JCQ), as a primary risk factor for coronary heart disease (CHD), but some methodological shortcomings have been highlighted.
In our pooled analysis with population-based and factory-based cohorts and a wide range of job titles, we assessed the association between JS and CHD adopting some methodological refinements: we selected relevant JCQ items which showed satisfactory construct validity, and we performed a stratified analysis by occupational classes, motivated by the knowledge that stressors in salaried workers and other professional categories may have different contents.
We explored the association using as the reference category low JS, instead that the wider non-high JS category, which nullifies the separate effects of control and demands at work, focusing merely on the joint effect.
Our findings showed that the CHD risks were higher among high JS manual and non-manual workers only, suggesting that JCQ better grasps JS in low-wage working categories; and the CHD risk increased substantially in high JS when compared with low-strain only.
The study did not include women due to the low incidence rate, and the small sample size anyhow deserves replications in different contexts to enhance confidence in results.
Organisational stressors at the work place and sedentary activities are the two most common work-related cardiovascular disease (CVD) risk factors in postindustrialised societies.1 The job demand–control model,2 developed by Karasek in the late 1970s is a widely used questionnaire to assess perceived work stress conditions. It is based on two major constructs: psychological job demand (PJD) and decision latitude (DL), defining high-strain, active, passive and low-strain categories.
Belkic et al3 reviewing 17 prospective cohort, 9 case–control and 8 cross-sectional studies, concluded in favour of a positive association between job strain (JS) and CVD in men. Kivimaki et al4 in a meta-analysis of cohort studies estimated an overall age-adjusted 43% excess risk for high JS, assessed with the demand–control model. This report combined HRs published by studies using different end points, some reporting combining estimates for men and women, and some adopting the approximate job title-imputed method to estimate exposures. This paper reported higher relative risks for the effort–reward imbalance model5 and injustice at work too. A recent paper, based on a collaborative pooled analysis including mainly unpublished (10 out of 13) and published cohort studies, found an overall gender-adjusted and age-adjusted HR for high versus non-high JS of 1.23 (95% CI 1.10 to 1.37). The non-high JS reference group combines active, passive and low-strain original categories. Based on this low excess risk and an arguable estimate of the high JS prevalence, the authors calculated a small population-attributable risk of 3–4%.6
This publication stimulated an intense debate in the scientific community,7–13 and many scientists argued that some shortcomings had contributed to bias the results to the null association. Among them, it is noteworthy to mention the low participation rates and the predominance of white collars in comparison to blue collars. Both these selection biases may have produced a reduced recruitment of more stressed workers, which is a frequently reported problem in these studies. Another potential bias may be due to the misclassification of exposure as JS may change overtime, due to the predominance of different stressors in the work organisations in different time periods. A recent letter14 highlighted some methodological and conceptual limitations related to the evaluation of JS. Some of them are arguable and some can only be addressed in future studies, as available data from most recent studies in psychosocial CHD epidemiology were not designed and did not collect the required information.14
The aim of the present paper is to assess the association between JS and the incidence of CHD in pooled analysis of population-based and factory-based North Italian cohorts of employed men, in particular focusing on a stratified analysis based on occupational classes. In a previous paper,15 we found that JS contributes to explain the excess CHD risk in manual compared with non-manual workers, but not the one observed in managers and self-employers. This finding may imply that the JCQ model better describes strain conditions among salaried manual and non-manual workers only. We reported HRs for the entire follow-up period and after exclusion of the events occurred in the first 3 years, to investigate reverse causation.
Methods
Study cohorts
As a part of the WHO-MONICA Project, three surveys of the Brianza population (located North of Milan) took place over a 10-year period (1986–1987, 1989–1990 and 1993–1994) to estimate coronary risk factor changes over time.15 In each survey a 10-year age-stratified and gender-stratified random sample was drawn from municipality roles from 25 to 64 years old residents in five area-representative towns. The participation rates were 70.1%, 67.2% and 70.8% respectively. The PAMELA (Pressioni Arteriose Monitorate E Loro Associazioni) study was another population survey, conducted in 1991–1992,16 with the sampling procedure applied to the 25–74 years old residents of the city of Monza, the largest town in Brianza. The participation rate was 66.9% among people up to 65 years of age. The overall sample size of individuals who were free of CHD and employed at the time of recruitment was 2350 men and 1334 women.
The SEMM (Surveillance of Employees of the Municipality of Milan) study recruited employees of six departments of the Milan Municipality, screened for CVD risk factors between May 1991 and March 1996. The cohort contributed to the JACE Study.17 The participation rates were 75.3% for men and 76.2% for women, respectively; and the overall sample size of the SEMM cohort, free of CHD at baseline, was of 2569 men and 5254 women. Women were not included in the analysis due to low number of CHD events (46 events in all the cohorts). The study approvals were obtained from the Ethical Committee of the University Hospital of Monza.
Occupational classes
As reported in a previous paper,15 we derived Erikson-Goldthorpe-Portocarero (EGP) classes. To achieve sufficient statistical power, EGP classes were aggregated in three occupational classes, as follows: professionals, administrators, managers, proprietors and self-employers (EGP classes I, II and IV, called here briefly managers and proprietors), non-manual (EGP classes III and V) and manual (skilled and unskilled, EGP classes VI and VII) workers.
JS scales and scores
The Job Content Questionnaire (JCQ) was administered to all employed workers, using two different versions sharing the same core items. In the MONICA Brianza and PAMELA studies as well as for employees of the two first recruited departments of the SEMM study, the short MONICA-MOPSY version18 was used. The extended version of JCQ was instead adopted for the remaining four SEMM departments, when the study was included into the JACE Project.16 In the online supplementary table S1 the original items for demand and control are reported for both questionnaires. The common items assessing PJD and DL, each on a four-point scale ranging from completely agree to completely disagree, were used. A comparability analysis19 20 showed that equivalent PJD and DL scores and subscores can be calculated from both questionnaires.
bmjopen-2016-014119supp001.pdf (88.6KB, pdf)
We derived the conventional four JCQ categories based on the quadrant approach, with high strain defined as PJD values higher than the overall sample median and DL values lower than or equal to the median. The remaining three JS categories, that is, active, passive and low strain were also defined according to the standard criteria.2 These three last strain categories were collapsed in a unique category, called non-high JS, to allow direct comparisons with the results reported by the recent pooled-cohort meta-analysis.6
Measurements of other risk factors at baseline
In MONICA surveys, cardiovascular risk factors were collected at baseline strictly adhering to the standardised procedures and quality standards of the WHO-MONICA Project (http://www.ktl.fi/publications/monica/manual/index.htm). In the PAMELA and in the SEMM studies, risk factors were measured based on MONICA-like procedures. In brief, blood pressure was measured on sitting participants at rest for at least 10 min, using a standard mercury sphygmomanometer equipped with larger cuff bladders if needed. The study variable for systolic blood pressure is the average of two measurements taken 5 min apart. Venous blood specimens were taken from the antecubital vein in fasting participants (12 hours or more). Serum total cholesterol and high-density lipoprotein (HDL) cholesterol were measured by an enzymatic method. Blood glucose was determined on the same samples by an enzymatic method.
From standardised interview information on cigarette smoking habits was available and dichotomised as current versus past smokers/never-smokers in this analysis. Diabetes mellitus was defined using self-reported diagnoses and information on insulin and oral hypoglycaemic treatments or based on a fasting blood glucose exceeding 126 mg/dL. Self-reported information on hospitalisation for myocardial infarction, unstable angina pectoris and coronary revascularisation was used to define a positive history of coronary event at baseline. Items on educational attainment were part of the standardised questionnaire, and it was dichotomised as ‘low’ (less than high school) and ‘high’ (high school or more).
Study end points and follow-up procedures
All participants were followed from the baseline examination until first cardiovascular event, emigration, death, 80th birthday or 31 December 2008, whichever came first, based on locally adapted procedures, developed within the MORGAM Project (http://www.thl.fi/publications/morgam/manual/followup/fumethod.htm). Vital status was actively investigated for all participants, including those who moved to different towns in Italy, and death certificates were obtained from local health districts. Suspected fatal events were identified on the basis of selected underlying causes of death, International Classification of Diseases (ICD)-9 codes 410-414. Suspected non-fatal events were identified based on ICD-9 hospital discharge codes: 410-411 for acute coronary events, and 36.0-9 for coronary revascularisation. Acute events were further investigated and adjudicated according to the MONICA diagnostic criteria. The study end point is the occurrence of a first major acute coronary event (myocardial infarction, acute coronary syndrome), fatal or non-fatal, or coronary revascularisation. The follow-up was completed for 98.9% of them, with no differences across cohorts and occupational classes.
Statistical analysis
Of the 4827 male workers in the age range 25–64 years, we excluded 724 participants with missing values of JCQ items or CHD risk factors, and hence the final sample size was 4103. We calculated the age-adjusted mean (prevalence) of major CHD risk factors by occupational class and strain categories from generalised linear models, and tested differences among groups using Wald χ2 tests.
Factor analysis with varimax rotation and Cronbach's α coefficients were used to assess the construct validity and internal consistency of JCQ items, respectively. These analyses were carried out on the population-based cohorts, characterised by wide job title variability.
Cox proportional hazards model with lifespan (attained age) on the time scale was adopted to study the associations between the risk of CHD event and JS, dichotomised for most analyses in high strain versus non-high strain (reference category comprising passive, active and low strain), adjusting for major risk factors and a dummy variable to indicate the study type (population-based vs factory-based). Stratified analyses were carried out adding a JS×occupational class interaction term in the models; the p value for the interaction term represented the formal test for the hypothesis of no change in the association between JS and CHD in different occupational classes (Wald χ2 test). We also performed a separate analysis, using the four JCQ categories (with low strain as reference group). The analyses were performed using the Statistical Analysis System (V.9.4, SAS Institute, Cary, North Carolina, USA). The figure was drawn using the R software (R Foundation for Statistical Computing, Wien, Austria. http://www.R-project.org/).
Results
In a median follow-up time of 14.6 years (IQR 13.2–17.6 years), 172 incident major coronary events occurred in our study sample, corresponding to a cumulative incidence rate of 2.78/1000 person-years. Age-adjusted rates among managers and proprietors and non-manual and manual workers were 3.1 (95% CI 2.32 to 4.14) and 1.97 (1.60 to 2.41), respectively. The exclusion of individuals with missing data did not alter the excess risk in managers and proprietors with respect to the non-manual and manual workers (see online supplementary table S5).
As shown in online supplementary table S2, the results of the factor analysis carried out on the populations-based MONICA-PAMELA samples, evidenced a satisfactory construct validity of JCQ items, with the notable exception of one item of skill discretion (SD), ‘do not repeat things over and over’, and two items of PJD, ‘work very fast’ and ‘work very hard’. Since these items did not contribute to the definition of the expected constructs, they were excluded and the scores calculated with the residual available items. Cronbach's α coefficients were 0.70 and 0.75 for DL and 0.53 and 0.58 for PJD among managers and proprietors and non-manual and manual workers, respectively.
Table 1 shows the distributions of main sociodemographic variables, JS categories and cardiovascular risk factors in the entire sample and in the two OCs. Non-manual and manual workers were younger and less educated than managers and proprietors. In the entire sample, 26% were classified at high strain, as expected due to the quadrant-term approach based on medians and the orthogonality between the constructs (Pearson correlation coefficient between PJD and DL was −0.09). The highest prevalence of high strain was found among non-manual and manual workers, while active and low-strain categories were prevalent among managers and proprietors. Managers and proprietors showed higher age-adjusted mean values of total cholesterol, but were less likely to smoke than non-manual and manual workers (all p<0.05). Conversely, the EGP-aggregated occupational class did not differ for mean systolic blood pressure and HDL cholesterol, nor for prevalence of diabetes (all p>0.2). As shown in online supplementary table S3, none of the considered risk factors showed statistically significant differences between the four JCQ categories.
Table 1.
Distribution of sociodemographic characteristics and age-adjusted mean and prevalence of major CVD risk factors at baseline, in the entire sample and by aggregated Erikson-Goldthorpe-Portocarero occupational classes
| Occupational class |
||||
|---|---|---|---|---|
| Entire sample | Managers and proprietors | Non-manual and manual workers | p Value | |
| Subjects CHD-free at baseline, n | 4103 | 819 | 3284 | – |
| Age, years | 40.9 (9.3) | 44.0 (10.3) | 40.1 (8.8) | <0.0001* |
| High school diploma or higher (%) | 39.4 | 45.8 | 37.8 | <0.0001† |
| High Job Strain (%) | 26.0 | 12.9 | 29.2 | <0.0001† |
| Active (%) | 14.8 | 23.6 | 12.6 | |
| Passive (%) | 35.6 | 24.2 | 38.5 | |
| Low job strain (%) | 23.7 | 39.3 | 19.8 | |
| Systolic blood pressure, mm Hg | 127.2 (16.2) | 126.7 | 127.5 | 0.22‡ |
| Total cholesterol, mg/dL | 211.4 (41.3) | 215.5 | 210.7 | 0.002‡ |
| HDL cholesterol, mg/dL | 49.5 (12.9) | 49.4 | 49.6 | 0.79‡ |
| Current cigarette smokers (%) | 39.2 | 35.8 | 40.0 | 0.03‡ |
| Diabetes mellitus (%) | 2.6 | 2.8 | 2.3 | 0.3‡ |
| Median follow-up, years | 14.6 | 17.2 | 14.0 | – |
| CHD first fatal or non-fatal events, n | 172 | 64 | 108 | – |
Men were 25–64 years old and employed at time of recruitment.
Unless, otherwise indicated, the numbers reported in the table are means and SDs.
*ANOVA F-test.
†χ2 Test.
‡Wald χ2 test (2df) from generalised linear model adjusted for age. Mean and prevalence of risk factors estimated at the sample age mean of 41 years.
ANOVA, analysis of variance; CHD, coronary heart disease; HDL, high-density lipoprotein.
Table 2 shows the results of the analysis assessing the association between JS and CHD incidence, for the entire sample and by occupational classes. In the entire sample, high-strain participants evidenced an overall higher HR of 1.39 (95% CI 0.99 to 1.97) in comparison with non-high strain, which was confirmed even after the exclusion of the first 3 years of follow-up (HR=1.39, 0.96 to 2.03). No increased hazard of events for high versus non-high strain was found among managers and proprietors, with HRs ranging from 0.71 to 0.61, both not statistically significant. Conversely, the HR for high versus non-high JS was 1.78 (1.20 to 2.66) among non-manual and manual workers, which again did not substantially change when events in the first 3 years were excluded (HR=1.80; 1.17 to 2.76). The JS×occupational class interaction term was statistically significant (p=0.04), suggesting the presence of heterogeneity by occupational class in the association between JS and CHD. Finally, these findings were confirmed when population-based and factory-based cohorts were analysed separately (see online supplementary table S4). When manual and non-manual workers were analysed separately, as table 3 shows, the HRs for the high-strain versus non-high-strain workers were 1.94 (95% CI 1.13 to 3.32) and 1.70 (95% CI 0.94 to 3.08) for manual and non-manual workers, respectively. There was no evidence of occupation×JS interaction (p=0.7). To maximise the available number of events, this analysis was carried out including the entire follow-up period, but nevertheless, wide CIs acknowledge the poor statistical power.
Table 2.
Multivariate-adjusted HRs and 95% CIs of first CHD event, for HS versus no HS, as reference category
| Entire sample |
Occupational class |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Managers and proprietors |
Manual and non-manual workers |
||||||||||||
| N | #CHD | HR | 95% CI | N | #CHD | HR | 95% CI | N | #CHD | HR | 95% CI | p Value* | |
| Job strain categories | |||||||||||||
| All events in the entire follow-up period included | |||||||||||||
| No HS | 3038 | 126 | REF | 713 | 57 | REF | 2325 | 69 | REF | 0.04 | |||
| HS | 1065 | 46 | 1.39 | 0.99 to 1.97 | 106 | 7 | 0.71 | 0.32 to 1.56 | 959 | 39 | 1.78 | 1.20 to 2.66 | |
| Events occurred after the first 3 years of follow-up | |||||||||||||
| No HS | 3002 | 108 | REF | 697 | 47 | REF | 2305 | 61 | REF | 0.04 | |||
| HS | 1049 | 39 | 1.39 | 0.96 to 2.03 | 102 | 5 | 0.61 | 0.24 to 1.55 | 947 | 34 | 1.80 | 1.17 to 2.76 | |
MONICA Brianza, PAMELA and SEMM cohorts. Men were 25–64 years old and employed at time of recruitment.
HRs estimated from Cox regression models with age as the time scale, adjusted for study type (population-based vs factory-based), systolic blood pressure, total cholesterol, HDL cholesterol, diabetes and current smokers. Job strain categories are based on items of Psychological Job Demand and Decision Latitude.
*p Value for interaction test between occupational class and high-strain (1 df Wald χ2 test).
CHD, coronary heart disease; HDL, high-density lipoprotein; HS, high job strain; no HS, non-high job strain; PAMELA, Pressioni Arteriose Monitorate E Loro Associazioni; SEMM, Surveillance of Employees of the Municipality of Milan.
Table 3.
Multivariate-adjusted HRs and 95% CIs of first CHD event, for HS versus no HS (reference category), among non-manual and manual workers only
| Non-manual workers |
Manual workers |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| N | #CHD | HR | 95% CI | N | #CHD | HR | 95% CI | p Value* | |
| Job strain categories | |||||||||
| All events in the entire follow-up period | |||||||||
| No HS | 1067 | 32 | REF | 1258 | 37 | REF | 0.7 | ||
| HS | 399 | 17 | 1.70 | 0.94 to 3.08 | 560 | 22 | 1.94 | 1.13 to 3.32 | |
| Events occurred after the first 3 years of follow-up | |||||||||
| No HS | 1058 | 27 | REF | 1247 | 34 | REF | 0.7 | ||
| HS | 394 | 14 | 1.68 | 0.88 to 3.23 | 553 | 20 | 1.95 | 1.11 to 3.43 | |
MONICA Brianza, PAMELA and SEMM cohorts. Men were 25–64 years old and employed at time of recruitment.
HRs estimated from Cox regression models with age as the time scale, adjusted for study type (population-based vs factory-based), systolic blood pressure, total cholesterol, HDL cholesterol, diabetes and current smokers. Job strain categories are based on items of Psychological Job Demand and Decision Latitude.
*p Value for interaction test between occupational class and high strain (1 df Wald χ2 test).
CHD, coronary heart disease; HDL, high-density lipoprotein; HS, high job strain; no HS, non-high job strain; PAMELA, Pressioni Arteriose Monitorate E Loro Associazioni; SEMM, Surveillance of Employees of the Municipality of Milan.
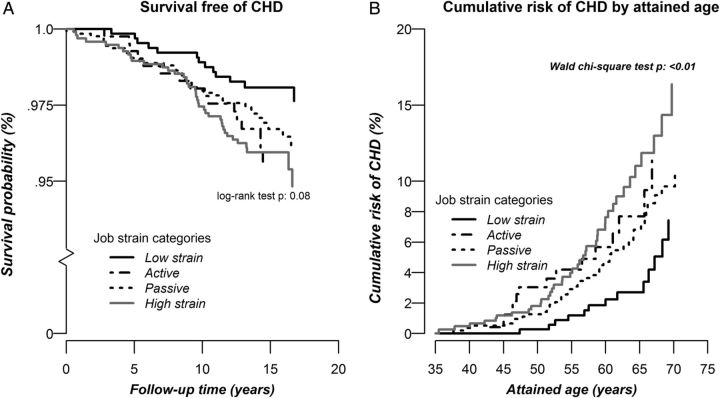
Table 4 shows the results of the association analysis between JS and CHD when the four JCQ quadrant-term categories are kept separated, including all events that occurred in the entire follow-up period, to maximise the available statistical power. Compared with the low-strain group, the high strain non-manual and manual workers evidenced HR of 2.92 (95% CI 1.54 to 5.51), higher than when using the non-high-strain group as the reference category. In addition, a risk excess was also found for active workers (2.47; 1.17 to 5.23), indicating that the demand dimension of JCQ in these workers is playing a major role in increasing the CHD risks. As shown in figure 1, the survival curve of low strain in comparison with all the other JS categories diverged already in the first years of follow-up, and persisted later on (panel A). This observation is in support of the detected small effect of reverse causation assessed with the exclusion of the events that occurred during the first 3 years of follow-up. Moreover, the increase in cumulative risk over attained age (figure 1, panel B) indicates that high strain men at the age of 50 years have the same cumulative risk of low strain men a decade older (figure 1, panel B).
Table 4.
Multivariate-adjusted HRs and 95% CIs of first CHD event, according to job strain category
| Entire sample |
Managers and proprietors |
Manual and non-manual workers |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Job strain categories | N | #CHD | HR | 95% CI | N | #CHD | HR | 95% CI | N | #CHD | HR | 95% CI |
| High strain | 1065 | 46 | 1.57 | 1.01 to 2.44 | 106 | 7 | 0.60 | 0.25 to 1.47 | 959 | 39 | 2.92 | 1.54 to 5.51 |
| Active | 605 | 26 | 1.28 | 0.77 to 2.12 | 193 | 11 | 0.64 | 0.31 to 1.32 | 412 | 15 | 2.47 | 1.17 to 5.23 |
| Passive | 1462 | 63 | 1.14 | 0.76 to 1.72 | 198 | 22 | 1.16 | 0.64 to 2.1 | 1264 | 41 | 1.67 | 0.89 to 3.12 |
| Low strain | 971 | 37 | 1.00 | REF | 322 | 24 | 1.00 | REF | 649 | 13 | 1.00 | REF |
Low strain as reference category. MONICA Brianza, PAMELA and SEMM cohorts. Men were 25–64 years old and employed at time of recruitment.
HRs from Cox regression models with age as the time scale, adjusted for study type (population-based vs factory-based), systolic blood pressure, total cholesterol, HDL cholesterol, diabetes and current smokers. CHD occurred during the entire follow-up period. Job strain categories are based on items of Psychological Job Demand and Decision Latitude.
CHD, coronary heart disease; HDL, high-density lipoprotein; PAMELA, Pressioni Arteriose Monitorate E Loro Associazioni; SEMM, Surveillance of Employees of the Municipality of Milan.
Figure 1.
Survival curves (panel A, left) and cumulative risk of coronary heart disease by attained age (panel B, right) in the four JCQ quadrant-term categories, among the occupational class of non-manual and manual workers. Men were 25–64 years old and employed at time of recruitment. JCQ, Job Content Questionnaire; CHD, coronary heart disease.
Discussion
In summary, in the investigated North Italian employed male pooled cohort we found a small increase in risk of CHD events in high JS when compared with non-high JS workers of 39%, not statistically significant. This estimate replicates the findings of recent meta-analyses, extending their results to a Southern European country with low CHD incidence rates.6 11 The novelty of our paper relates to results of the stratified analysis, which showed an excess risk of 78% (HR=1.78; 95% CI 1.20 to 2.66) among high-strain non-manual and manual workers. In this occupational class, when the four JCQ categories were separately analysed, the relative risk of CHD events of high-strain versus low-strain participants increased to 2.92 (95% CI 1.54 to 5.51). It is noteworthy mentioning that the HR for active versus low-strain workers was also elevated (HR=2.47; 1.17 to 5.23), indicating that the association can be biased towards the null hypothesis when active, low-strain and passive men are grouped in a unique non-high-strain class.
The use of JCQ constructs based on the results of factor validity assessment has evidenced satisfactory internal consistency and reliability of the scores. The SD item ‘do not repeat things over and over’ may have different meanings in a variety of job profiles, working environments and countries; and it may not always connote monotony.21 Two items of demand ‘work very fast’ and ‘work very hard’ assume minor importance in postindustrial work forces, while items describing pressure for having the work done or conflicting demands are stressors that still continue to characterise present day working conditions, as also reported by other authors.22 This observation requires further investigations, as it points to the conclusion that the established JCQ may be well suited to grasp the working conditions of salaried workers, in the low levels of organisation only. The stressful aspects of job characteristics among people ranking at the higher level of organisations are probably related to prolonged working hours and excessive competitiveness, which are not adequately investigated by the actual formulation of the JCQ.23
We did not find relevant differences in the distribution of traditional cardiovascular risk factors, including systolic blood pressure, cholesterol as well as the prevalence of diabetes and cigarette smoking, among JCQ categories. In the population-based sample we did find differences among JS categories in the 24-hour systolic blood pressure means, but not when using clinical blood pressure measurements in the same age range.24 This observation is in line with previous findings supporting the major importance of a direct, rather than an indirect, effect of JS on the cardiovascular system.21 This direct effect is assumed to be attributable to the effect on psychobiological processes, as documented by studies which have found a reduced heart rate variability25 and alterations of the hormonal or immune systems.26
Among the strengths of the present study are the long follow-up period, the standardisation of the methods to collect risk factors at baseline and to validate events, as they have been carried out adhering to the procedures of the MONICA and MORGAM studies. Among the limitations, we acknowledge that our findings are on men only. We did not include women, due to the low number of events, which did not allow us to further stratify the analyses by occupational classes. We did not explore a dose–response relationship, but our findings support the major role of PJD in determining the increased CHD risk, as both high-strain and active workers showed the higher risks when compared with low-strain participants. We also did not explore the interaction effects with other work-related risk factors like social support and physical inactivity, as well as with behavioural risk factors.27 28 As we do have these baseline data for some of the cohorts, we will investigate these interactions in future reports, hoping to contribute to the current interest of the scientific community on these topics.29–33 Finally, we did not collect data at baseline on other complementary theoretical models of stressful work, in particular the effort–reward imbalance model, which has shown remarkable associations with CVD and CHD outcomes.4 5
In conclusion, our findings support the association between JS and CHD incidence in manual and non-manual workers, not among managers and proprietors. This can be attributable to the better chances of the present formulation of the JCQ to grasp job stressors in the low-wage working categories. Moreover, to assess the effect of high strain on CHD, it is more accurate to use the low strain instead of the wider non-high strain as the reference category, since the adoption of the latter may contribute to bias the association to the null. Our results require replications on larger and diversified samples.
Supplementary Material
Acknowledgments
The authors thank all collaborators who helped in assessing baseline risk factors and collecting follow-up data. The authors also deeply recognise and thank the advices who reviewed the preliminary versions of this paper, and helped to improve it.
Footnotes
Contributors: MMF conceived the research question, drafted the manuscript and is the principal investigator (PI) of the MONICA-Brianza and the SEMM study cohorts. GV and LB were responsible of the statistical analyses, contributed to interpretation of the data and revised the manuscript. GG and GC are the PIs of the PAMELA study and of the MONICA-Brianza cohorts, respectively; they both helped with data interpretation and contributed critically to the Introduction and Discussion sections. All authors read and approved the final version of the paper, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding: This work and the latest activities of the MONICA Brianza Study were mainly supported by the Health Administration of Regione Lombardia (grant numbers 17155/2004 and 10800/2009). The follow-up was partially supported with grants from the Italian Ministry of Health (grant 2012/597) and it was carried out in collaboration with the Centro di Epidemiologia, Sorveglianza e Promozione della Salute of the Istituto Superiore di Sanità in Roma.
Competing interests: None declared.
Ethics approval: San Gerardo Hospital, Monza, Italy.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Statistical details are available on request to the corresponding author.
References
- 1.Olsen O, Kristensen TS. Impact of work environment on cardiovascular diseases in Denmark. J Epidemiol Community Health 1991;45:4–10. 10.1136/jech.45.1.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Karasek RA. Job demands, job decision latitude, and mental strain: implications for job Redesign. Adm Sci Q 1979, 24:285–308. 10.2307/2392498 [DOI] [Google Scholar]
- 3.Belkic KL, Landsbergis PA, Schnall P, et al. Is job strain a major source of cardiovascular disease risk? J Work Environ Health 2004;30:85–128. 10.5271/sjweh.769 [DOI] [PubMed] [Google Scholar]
- 4.Kivimaki M, Virtanen M, Elovainen M, et al. Work stress in the etiology of coronary heart disease–a meta-analysis. J Work Environ Health 2006;32:431–42. 10.5271/sjweh.1049 [DOI] [PubMed] [Google Scholar]
- 5.Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol 1996;1:27–41. 10.1037/1076-8998.1.1.27 [DOI] [PubMed] [Google Scholar]
- 6.Kivimäki M, Nyberg ST, Batty GD, et al. Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data. Lancet 2012;380:1491–7. 10.1016/S0140-6736(12)60994-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Netterstrøm B. Job strain as a measure of exposure to psychological strain. Lancet 2012;380:1455–6. 10.1016/S0140-6736(12)61512-8 [DOI] [PubMed] [Google Scholar]
- 8.Choi B, Schnall P, Ko S, et al. Job strain and coronary heart disease. Lancet 2013;381:448. 10.1016/S0140-6736(13)60243-3. [DOI] [PubMed] [Google Scholar]
- 9.Landsbergis P, Schnall P. Job strain and coronary heart disease. Lancet 2013;381:448 10.1016/S0140-6736(13)60242-1 [DOI] [PubMed] [Google Scholar]
- 10.Theorell T. Commentary triggered by the Individual Participant Data Meta-Analysis Consortium study of job strain and myocardial infarction risk. Scand J Work Environ Health 2014;40:89–95. 10.5271/sjweh.3406 [DOI] [PubMed] [Google Scholar]
- 11.Kivimäki M, Kawachi I. Need for more individual-level meta-analyses in social epidemiology: example of job strain and coronary heart disease. Am J Epidemiol 2013;177:1–2. 10.1093/aje/kws407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choi B, Dobson M, Landsbergis P, et al. RE: “Need for more individual-level meta-analyses in social epidemiology: example of job strain and coronary heart disease”. Am J Epidemiol 2013;178:1007–8. 10.1093/aje/kwt192 [DOI] [PubMed] [Google Scholar]
- 13.Landsbergis PA, Dobson M, Schnall P. RE: “Need for more individual-level meta-analyses in social epidemiology: example of job strain and coronary heart disease”. Am J Epidemiol 2013;178:1008–9. 10.1093/aje/kwt193 [DOI] [PubMed] [Google Scholar]
- 14.Burr H, Formazin M, Pohrt A. Methodological and conceptual issues regarding occupational psychosocial coronary heart disease epidemiology. Scand J Work Environ Health 2016;42:251–5. 10.5271/sjweh.3557 [DOI] [PubMed] [Google Scholar]
- 15.Ferrario MM, Veronesi G, Chambless LE, et al. The contribution of major risk factors and job strain to occupational class differences in coronary heart disease incidence: the MONICA Brianza and Pamela population-based cohorts. Occup Environ Med, 2011;68:717–22. 10.1136/oem.2010.060822 [DOI] [PubMed] [Google Scholar]
- 16.Cesana G, De Vito G, Ferrario M, et al. Ambulatory blood pressure normalcy: the PAMELA Study. J Hypertens Suppl 1991;9:S17–23. [PubMed] [Google Scholar]
- 17.Houtman I, Kornitzer M, de Smet P, et al. Job stress, absenteeism and coronary heart disease European cooperative study (the JACE study): design of a multicentre prospective study. Eur J Public Health 1999;9:52–7. 10.1093/eurpub/9.1.52 [DOI] [Google Scholar]
- 18.World Health Organization. MONICA Psychosocial Optional Study Manual: suggested measurement instruments. Copenhagen: WHO Regional Office for Europe, 1989. [Google Scholar]
- 19.Karasek R, Choi B, Ostergren PO, et al. Testing two methods to create comparable scale scores between the job content questionnaire (JCQ) and JCQ-like questionnaires in the European JACE Study . Int J Behav Med 2007;14:189–201. 10.1007/BF03002993 [DOI] [PubMed] [Google Scholar]
- 20.Fransson EI, Nyberg ST, Heikkilä K, et al. Comparison of alternative versions of the job demand-control scales in 17 European cohort studies: the IPD-Work consortium. BMC Public Health 2012;12:62 10.1186/1471-2458-12-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Steptoe A, Kivimaki M. Stress and cardiovascular disease: an update on current knowledge. Annu Rev Public Heath 2013;34:337–54. 10.1146/annurev-publhealth-031912-114452 [DOI] [PubMed] [Google Scholar]
- 22.Choi B, Kurowski A, Bond M, et al. Occupation-differential construct validity of the Job Content Questionnaire (JCQ) psychological job demands scale with physical job demands item: a mixed methods research. Ergonomics 2012;55:425–39. 10.1080/00140139.2011.645887 [DOI] [PubMed] [Google Scholar]
- 23.Karasek R, Theorell T. Healthy work: stress, productivity, and the reconstruction of working life. New York: Basic Books Pub, 1990. [Google Scholar]
- 24.Cesana G, Ferrario M, Sega R, et al. Job strain and ambulatory blood pressure levels in a population-based employed sample of men in northern Italy. Scand J Work Environ Health 1996;22:294–305. 10.5271/sjweh.144 [DOI] [PubMed] [Google Scholar]
- 25.Borchini R, Bertù L, Ferrario MM, et al. Prolonged job strain reduces time-domain heart rate variability on both working and resting days among cardiovascular-susceptible nurses. Int J Occup Med Environ Health 2015;28:42–51. 10.2478/s13382-014-0289-1 [DOI] [PubMed] [Google Scholar]
- 26.Emeny RT, Zierer A, Lacruz ME, et al. Job strain-associated inflammatory burden and long-term risk of coronary events: findings from the MONICA/KORA Augsburg case-cohort study. Psychosom Med 2013;75:317–25. 26 10.1097/PSY.0b013e3182860d63 [DOI] [PubMed] [Google Scholar]
- 27.Kivimäki M, Nyberg ST, Fransson EI, et al. Associations of job strain and lifestyle risk factors with risk of coronary artery disease: a meta-analysis of individual participant data. CMAJ 2013;185:763–9. 10.1503/cmaj.121735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nyberg ST, Heikkilä K, Fransson EI, et al. Job strain in relation to body mass index: pooled analysis of 160 000 adults from 13 cohort studies. J Intern Med 2012;272:65–73. 10.1111/j.1365-2796.2011.02482.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Choi B, Dobson M, Ko S, et al. Job strain and lifestyle factors. CMAJ 2014;186:63–4. 10.1503/cmaj.114-0003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Choi B, Ko SB, Landsbergis P, et al. Job strain and health-related behaviors. Am J Public Health 2014;104:e3 10.2105/AJPH.2013.301757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Choi B, Dobson M, Landsbergis P, et al. Job strain and obesity. J Intern Med 2014;275:438–40. 10.1111/joim.12173 [DOI] [PubMed] [Google Scholar]
- 32.Smith PM, Mustard CA. Job strain, health behaviours and heart disease. CMAJ 2013;185:1251 10.1503/cmaj.113-2135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smith P. Potentially misleading conclusions: job strain and health behaviors. Am J Public Health 2014;104:e4 10.2105/AJPH.2013.301758 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-014119supp001.pdf (88.6KB, pdf)