Abstract
A significant proportion of patients discharged from the emergency department (ED) with asthma exacerbations will relapse within 4 weeks. This systematic review summarises the evidence regarding relapses and factors associated with relapse in adult patients discharged from EDs after being treated for acute asthma. Following a registered protocol, comprehensive literature searches were conducted. Studies tracking outcomes for adults after ED management and discharge were included if they involved adjusted analyses. Methodological quality was assessed using the Newcastle–Ottawa Scale (NOS) and the Risk of Bias (RoB) Tool. Results were summarised using medians and IQRs or mean and SD, as appropriate. 178 articles underwent full-text review and 10 studies, of various methodologies, involving 32 923 patients were included. The majority of the studies were of high quality according to NOS and RoB Tool. Relapse proportions were 8±3%, 12±4% and 14±6% at 1, 2 and 4 weeks, respectively. Female sex was the most commonly reported and statistically significant factor associated with an increased risk of relapse within 4 weeks of ED discharge for acute asthma. Other factors significantly associated with relapse were past healthcare usage and previous inhaled corticosteroids (ICS) usage. A median of 17% of patients who are discharged from the ED will relapse within the first 4 weeks. Factors such as female sex, past healthcare usage and ICS use at presentation were commonly and significantly associated with relapse occurrence. Identifying patients with these features could provide clinicians with guidance during their ED discharge decision-making.
Keywords: Asthma
Introduction
Asthma affects over 17.5 million adults in North America and its prevalence continues to rise, as evidenced by the 12.3% relative increase from 2001 (7.3%) to 2009 (8.2%).1 Worldwide, asthma prevalence ranges from low (underdeveloped countries) to high (developed countries).2 Asthma is predominantly a chronic disease that can be controlled with appropriate pharmacological and non-pharmacological interventions;3 however, exacerbations do not always respond to standard or additional treatment options, leading to urgent visits to health providers, admissions to hospital and, in severe and rare cases, death.4 In the USA, patients with exacerbations had significantly higher asthma-related healthcare costs: $1740 over 1 year compared with $847 for asthmatics without exacerbations.5 While patients with acute asthma often seek care in the emergency department (ED),6–8 most are successfully treated and subsequently discharged;7 8 only 6–12% of adult patients presenting to the ED with an exacerbation of asthma will be admitted.8 9
The understanding and management of acute asthma have advanced considerably in recent years. Current evidence-based guidelines (National Asthma Education and Prevention Plan (NAEPP),10 Global Initiative for Asthma (GINA),11 and Canadian Thoracic Society (CTS)12) suggest that early treatment with short-acting β2-agonists, inhaled short-acting anticholinergic agents and systemic corticosteroids (SCS) will reduce hospitalisations. On ED discharge, SCS are recommended,13 14 and further studies suggest that prescribing inhaled corticosteroids (ICS) at discharge can reduce relapse following discharge at least in adult patients.15–17 ICS in combination with long-acting β-agonists (ICS/LABA) are more effective than ICS monotherapy in patients with persistent asthma, with the number needed to treat of 19 to prevent one exacerbation.18 On the other hand, the impact of non-pharmacological interventions (ie, ED-based educational strategies) on relapses remains unclear.19 20
While considerable improvement in the management of acute asthma should lead to better outcomes over time, practice variation does exist and many patients presenting to EDs do not always receive evidence-based treatment.13 Moreover, what works in certain settings may not be applicable to others. Despite the dissemination of effective interventions for the prevention of relapses after asthma exacerbations, these outcomes still occur, affect the quality of life21 of patients with asthma and represent significant costs to the healthcare system.5
A number of studies have examined factors associated with relapse outcomes in adults after ED discharge.22–26 Notwithstanding this research, there remains a relative paucity of literature attempting to compile the existing information to influence management. The objective of this study was to summarise the evidence regarding relapses and factors associated with increased relapse in patients discharged from EDs after being treated for asthma exacerbations.
Methods
Protocol
A study protocol was developed a priori to define the objectives, search strategy, eligibility criteria, outcomes of interest, the process for abstracting and synthesising information from eligible studies, and the methods for data analysis. The systematic review conforms to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and was registered with International prospective register of systematic reviews (PROSPERO) (CRD42015023844). No ethics approval was required.
Literature search
Comprehensive searches of seven electronic databases (Medline, EMBASE, Cochrane Library, CINAHL, SCOPUS, LILAC, and ProQuest Dissertations and Theses) were conducted from their inception to June 2015. The search strategy was designed by a health sciences librarian (LD) and comprised controlled vocabulary and keywords. The search used a slightly modified version of an ‘emergency room’ search filter27 (see online supplementary appendix A; complete search strategy is available on request).
bmjresp-2016-000169supp_appendix.pdf (131.3KB, pdf)
References were manually selected from the first 10 pages of Google Scholar. In addition, proceedings from important Canadian Association of Emergency Physicians (CAEP) and US Society for Academic Emergency Medicine (SAEM) conferences held between 2005 and 2015 that involved research presentations were hand-searched. No limits were applied on the basis of date, study design, language or publication status.
Study selection
The review included studies assessing the proportion of adult patients (or adults and children with ≥80% of the study population being ≥17 years of age) relapsing after receiving treatment in the ED for an asthma exacerbation. Relapse and variables significantly associated with relapse after multivariable modelling were the primary outcomes presented in this review. To be included as factors associated with relapse, studies must have conducted adjusted analyses. Relapse was defined as an urgent visit to any ED, clinic or physician office for worsening asthma symptoms within 4 weeks of the initial ED visit. Secondary outcomes included time between ED discharge and relapse, and medical management received in the ED.
Two reviewers (JH, NA) independently screened the titles and abstracts of studies identified by the literature search. Articles initially deemed relevant and those whose abstracts and titles provided insufficient information were retrieved and independently reviewed (JH, NA) to determine study eligibility. Disagreements were discussed and resolved with a third party (CVR).
Data extraction and quality assessment
Information on patients, methods, interventions and outcomes was extracted from the original reports onto standardised data collection forms independently by two authors (JH, NA). Information was cross-referenced to ensure accuracy. If necessary, authors were contacted to clarify information or provide unpublished data.
Assessment of study quality
Two reviewers (JH, NA) independently evaluated each of the included studies using the Newcastle–Ottawa Scale (NOS) for observational studies and the Cochrane Risk of Bias Tool (RoB), a quality assessment tool used to assess controlled clinical trials (CCT) for risk of bias. Any discrepancies were discussed with a third party (CVR). Information on study quality will help authors evaluate the validity of the findings.
Data synthesis and statistical analysis
Characteristics of the included studies were summarised using descriptive statistics (eg, numbers with proportions for dichotomous variables and means with standard deviations (±SD) or medians with interquartile ranges (IQR) for continuous variables). An evidence table was constructed to report information on each article's source, year of publication, country of origin, study design, sample size and outcomes. Analyses were focused on the proportion of relapses; a subgroup analysis by the end of data collection (year) was completed. Inter-rater agreement between the two reviewers evaluating study quality using the NOS was measured using the κ statistic. Effect estimates from individual studies were presented as adjusted ORs (aORs) with 95% CIs when possible. Owing to the variations in models used to generate aORs and in the factors reported, results were not pooled in a traditional meta-analysis. Finally, factors associated with relapse at a statistically significant level (p<0.05) were summarised in a table. Figures were generated using GraphPad Prism V.6.07 for Windows (GraphPad Software, La Jolla, California, USA).
Results
Search results
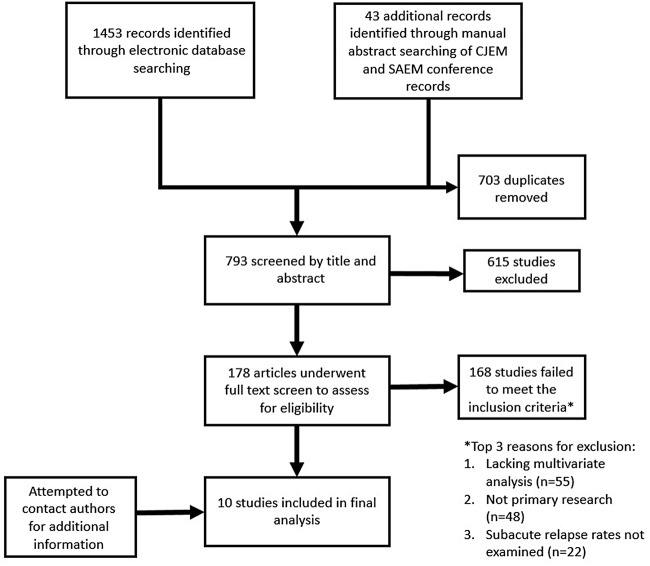
After combining the results of the electronic search strategy with the grey literature, removing duplicates, screening for titles and abstracts, and reviewing full-text articles, 10 studies were included in the review (figure 1). The most common reason for exclusion was a lack of multivariate analysis (n=55; including 19 randomised controlled trials (RCTs)), followed by studies that were not primary research (n=48). Studies which did not examine relapse (n=22) and those which had a partially or wholly inpatient population (n=20) were also excluded. A minority of studies (n=23) were excluded for various other reasons, such as the involvement of paediatric populations, or patient presentation to the ED was not due to acute asthma. A full list of excluded studies is available on request.
Figure 1.
PRISMA flow diagram illustrating the overview of the systematic literature search.
Study characteristics
Five prospective cohort studies,22–24 26 28 two retrospective cohort studies,29 30 two administrative data analyses31 32 and one RCT33 were included (table 1). Apart from one study,30 all included studies were conducted in North America.22–24 26 28 29 31–33 Similarly, aside from one abstract, all other included studies were published peer-reviewed articles.29 One study performed its multivariate analysis based on 8-week relapse proportions.24 Demographic characteristics of included studies are displayed in table 2. Note that ED management was left to the discretion of the treating physician in all studies but one,24 which outlined a specific protocol. The definition of relapse was commonly given as some variant of ‘any urgent medical treatment for asthma, regardless of location of care’, except for two studies30 32 that restricted their relapses to those presenting back to the ED.
Table 1.
Descriptive characteristics of studies selected for inclusion in the review
| Author | Year of publication | Country | Study design | Study period | Sample size | Relapse proportion (at 2 weeks) |
|---|---|---|---|---|---|---|
| Rowe33 | 2007 | Canada | Randomised controlled trial | – | 137 | 12.40% |
| McCarren24 | 1998 | USA | Prospective cohort | 1992–1995 | 284 | 10% |
| Emerman26 | 1999 | USA | Prospective cohort | 1996–1997 | 641 | 17% |
| Singh28 | 1999 | USA | Prospective cohort | 1996–1997 | 1228 | 15.80% |
| Rowe22 | 2008 | Canada | Prospective cohort | 2004–2005 | 695 | 13.90% |
| Rowe23 | 2015 | Canada | Prospective cohort | 2003–2007 | 807 | 14% |
| Lin29 | 2009 | Canada | Retrospective cohort | 2006–2007 | 257 | – |
| Prabhakaran30 | 2013 | Singapore | Retrospective cohort | 2008–2009 | 1303 | 7.4% (4 week) |
| Baibergenova31 | 2006 | Canada | Administrative database | 2003–2004 | 23 253 | – |
| Withy32 | 2008 | USA | Administrative database | 1999–2004 | 4318 | 4% |
Table 2.
Select demographic characteristics of studies included in the review
| Age (mean) | Female (%) | COPD status | Discharge medication | Race (largest proportion) | Current smoking (%) | Insurance (public/private) | Hospitalisation | Previous intubation (%) | ICS usage (%) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Rowe33 (2007) | 30±10 | 59 | NA | Prednisone, β-agonist, ICS ± LABA | NA | 39 | NA | 68% ever | 7 | 47 |
| McCarren24 | 35±10 | 40 | Excluded | 9–11 days of prednisone, theophylline, steroid inhaler | 87% black | 37 | NA | 46% in past year | NA | NA |
| Emerman26 | 34±10 | 69 | Excluded | 5–7 days of prednisone + EP discretion | 49% black | 30 | 74% | 26% in past year | 13 | 41 |
| Singh28 | 36±10 | 64 | 3% | 67% received steroids | 54% black | 35 | 70% | 62% ever | 17 | 43 |
| Rowe22 (2008) | 29±10 | 64 | Excluded | 5–7 days of prednisone + EP discretion | 87% white | 39 | 72% | 20% in past 2 years | 8 | 52 |
| Rowe23 (2015) | 30 (24–39)* | 58 | Excluded | 5–7 days of prednisone + EP discretion | 85% white | 33 | 50% (medication coverage) | 24% in past 2 years | 7 | 68 |
| Lin29 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Prabhakaran30 | 36±16 | 48 | Excluded | ± prednisolone (79%), ICS | 37% Chinese | NA | NA | NA | NA | NA |
| Baibergenova31 | NA | 62 | NA | NA | NA | NA | NA | NA | NA | NA |
| Withy32 | NA | 54 | NA | NA | NA | NA | 100% | NA | NA | NA |
*Median (IQR).
COPD, chronic obstructive pulmonary disease; EP, emergency physician; ICS, inhaled corticosteroids; LABA, long-acting β-agonists; NA, not available.
Quality assessment
All included observational studies had a relatively low risk of bias according to the NOS. Two studies26 28 scored seven out of eight possible points because their loss to follow-up was >20%. All the remaining studies scored the full eight points (k=0.73). The included RCT had low risk of bias according to the RoB Tool.
Primary outcomes
Relapse proportions
One RCT33 and seven observational studies22–24 26 28 30 32 33 reported the proportion of patients experiencing relapse after management and discharge for acute asthma. The authors of the two29 31 studies that failed to report their relapse proportions were contacted; however, in both cases, additional information was not obtained. Relapse proportions were recorded at 1 week,22–24 26 32 33 2 weeks22–24 26 28 32 33 and 4 weeks.23 24 30 The relapse proportion at 2 weeks ranged from 4%31 to 17%.26 When 2-week and 4-week relapse proportions were examined based on the studies' last year of data collection, there were slightly lower relapse rates in recent years (figure 2). Six studies tracked relapse proportions at multiple postdischarge durations.22–24 26 32 33 All six studies had the greatest proportion of relapses occurring within the first week, with a median of 61% (IQR: 50–68) of all relapses occurring during week one. After this early peak, relapse proportions appear to increase at a relatively linear rate between weeks 1 and 4 (figure 3). Median relapses were 8% at 1 week, 14% at 2 weeks, and 17% at 4 weeks (figure 3).
Figure 2.
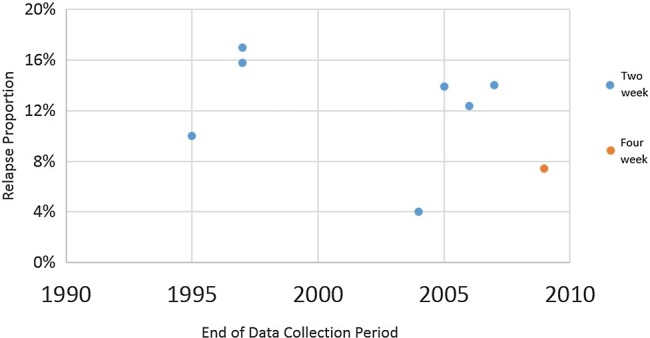
Proportion of patients experiencing relapse relative to the year when the data were collected.
Figure 3.
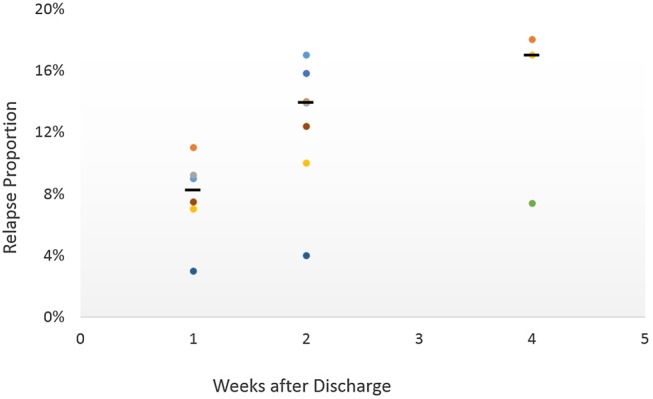
Reported relapse rates at varying time periods after discharge from ED. Medians displayed with lines. Distinct studies represented by different colours. ED, emergency department.
Factors significantly associated with relapse
Although 19 RCT studies underwent a full-text review, only one paper was included.33 There were two studies which reported performing multivariate analyses, but the results were not presented.34 35 In the included RCT, there were three factors identified as significant on multivariate analysis: ICS use prior to ED presentation, prior intubation and female sex. The strongest association identified in the RCT was female sex (HR=7.2; 95% CI 2.3 to 23.1).
Factors commonly and significantly associated with relapse occurrence within 4 weeks of ED discharge in observational studies included: patient sex, previous healthcare usage, symptom duration and ICS usage at ED presentation (table 3). The most commonly investigated variable was female sex; from models reported in six studies,22 23 28 31–33 five reported a significant finding with aOR ranging from 1.17 (95% CI 1.03 to 1.34) to 7.2 (95% CI 2.3 to 23.1) (figure 4).
Table 3.
Factors significantly (p<0.05) associated, on multivariate analysis, with asthma relapse within 4 weeks of ED treatment (✓), factors studied but not found to be significant (ø) and factors not assessed (NA)
| Rowe 2007 | Emerman 1999 | Singh 1999 | Rowe 2008 | Rowe 2015 | Lin 2009 | Prabhakaran 2013 | Baibergenova 2006 | Withy 2008 | |
|---|---|---|---|---|---|---|---|---|---|
| Female sex | ✓ (7.2, 2.3 to 23.1) | NA | ø | ✓ (1.57, 1.14 to 2.09) | ✓ (1.9, 1.2 to 3.0) | NA | NA | ✓ (1.23, 1.10 to 1.37) | ✓ (1.17, 1.03 to 1.34) |
| Older age | ø | NA | NA | ø | ø | NA | ✓ (0.98, 0.97 to 1.0) | ✓ (0.81, 0.69 to 0.94) | Ø |
| Past healthcare usage | NA | ✓ (1.3, 1.1 to 1.5) | NA | ✓ (1.47, 1.18 to 1.80) | ø | ø | NA | NA | NA |
| Severity | NA | NA | NA | ø | ø | ø | NA | ✓ (2.51, 1.12 to 5.62) | NA |
| Symptom duration | NA | ✓ (2.5, 1.2 to 5.2) | NA | ø | ✓ (1.7, 1.3 to 2.3) | NA | NA | NA | NA |
| ICS at presentation | ✓ (3.1, 1.0 to 9.8) | NA | NA | ✓ (1.39, 1.07 to 1.78) | ✓ (1.9, 1.1 to 3.2) | NA | NA | NA | NA |
| Cost/insurance | NA | NA | NA | ø | ø | NA | NA | NA | ✓ (1.15, 1.0 to 1.32) |
ED, emergency department; ICS, inhaled corticosteroids.
Figure 4.
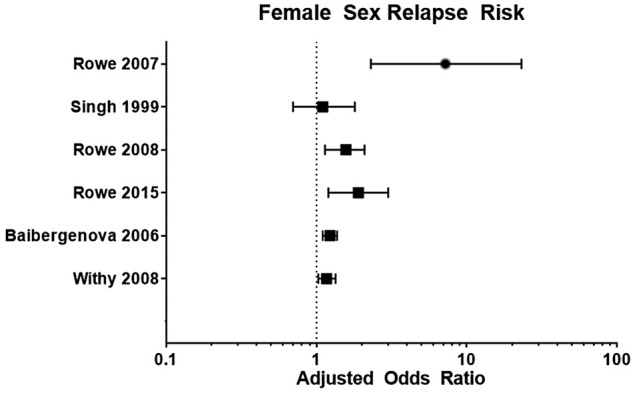
Adjusted ORs for female sex acting as a predictor for acute asthma relapse after ED treatment and discharge. ED, emergency department.
Healthcare usage included subcategories (table 3) for ED asthma visits such as: visits that occurred in the past 6 months,24 1 year,26 and 2 years,22 past urgent clinic visits for asthma26 and prior hospitalisations for asthma.22 Severity at ED presentation was assessed using the Canadian Triage and Acuity Scale (CTAS) score of one.30 Symptom duration was assessed either directly by asking patients to report the length of their symptoms,23 26 or indirectly by asking how long they had been experiencing difficulty with activities or work.24 Symptoms present for over 24 hours had a relatively strong association with relapse, and had an aOR consistently above 1.5 (range: aOR: 1.7 (95% CI: 1.3 to 2.3) to aOR: 2.5 (95% CI: 1.2 to 5.2)). ICS usage (including ICS/LABA combination) at presentation had consistently positive associations with relapse (range: aOR: 1.39 (95% CI: 1.07 to 1.78) to aOR: 3.1 (95% CI: 1.0 to 9.8)).22 23 Increasing age, either by unit increase (aOR=0.98; 95% CI 0.97 to 1.0) or by age categories (eg, ages 46–55; aOR=0.81; 95% CI 0.69 to 0.94), was the only factor associated with a lower likelihood of relapse in more than one study.30 31
Secondary outcomes
Time between ED discharge and relapse
One study reported that the median time to relapse was 9 days (IQR: 3–19);30 however, no other studies reported this outcome.
Medical management
Four studies22–25 reported that the proportion of patients arriving with a recent history of SCS use ranged from 2% to 23%. Similarly, five studies tracked those patients receiving SCS after ED discharge22 23 26 30 33 as ranging from 63% to 100%. Proportions of patients using ICS at ED presentation22 23 26 28 33 and those prescribed ICS at discharge22 23 30 33 varied widely among studies with ranges of 35–82% and 29–100%, respectively. ICS/LABA usage at presentation was reported by three studies22 23 33 and was relatively consistent with a range from 32–33%. Short-acting β2-agonist use before presentation was much more uniform (82–87%).22 23 26 28 33
Discussion
This comprehensive systematic review identified 10 studies involving 32 923 patients that performed multivariate analysis to investigate factors associated with relapse after treatment for adult patients seen with acute asthma in the ED setting. Quality assessment showed that all included studies were of high methodological quality, which strengthens the validity of these results. Given the variations in models used to generate aORs and in the factors reported, results were not pooled in a traditional meta-analysis. Overall, there is strong evidence that women and patients on pre-existing ICS therapy are more likely to relapse, and perhaps should be managed more aggressively.
Relapse proportions were notably high within the first week in most of the studies which reinforces the need for primary care providers to see patients early after discharge to reassess response to therapy, adjust management and provide additional recommendations.11 Apart from two studies, relapses were relatively consistent across the included studies: one that reported relapse proportions of 4% at 2 weeks32 and another that reported 7.4% at 4 weeks.30 These two studies restricted their outcomes to patients relapsing to EDs and that may have influenced the estimates; all other studies provided patient-reported relapse outcomes involving multiple potential treatment location. In both studies,30 32 a large number (44.8% and 46.0%, respectively) of patients had outpatient follow-up arranged prior to discharge to address asthma symptoms, and this is a possible contributor to the significantly reduced proportion of patients relapsing. The author of the second study30 (based in Singapore and the only study included in this review that originated outside North America) acknowledged that the reported relapse proportions were lower than expected potentially due to differences in healthcare delivery relative to North America. One such difference is a higher availability of after-hours, or 24-hour, primary care.36 Given the relative recency of these two studies, they are potentially overstating the recent relapse reduction shown in figure 2; despite this, there is some evidence that the number of patients receiving guideline-recommended care in EDs has been increasing over recent years, leading to improved outcomes.13
It is important to highlight the large number of relapses occurring within the first few days after ED discharge. Nearly two-thirds of patients experiencing relapse do so within the first week and this appears to be an area where improved ED management, and perhaps strategies to prompt primary care follow-up, could improve outcomes.35
Many of the factors significantly associated with relapse risk on multivariate analysis make intuitive sense. Female sex is a predisposing factor for severe asthma37 and women have been shown to perceive symptoms differently, so it is perhaps not surprising that this review finds that female sex was also associated with more frequent relapses following ED visits for acute asthma. Logic predicts that patients with past tendencies to use the ED will not hesitate to return; likewise, patients who are experiencing unrelenting symptoms over a longer duration may be struggling with self-management of their asthma, or have more severe baseline disease, and may need urgent care. Indeed, lack of symptom improvement has been identified as a common cause for patients with asthma to seek urgent care.7 Although infrequently examined by these studies, medication cost and patient insurance certainly impact treatment efficacy, especially when we consider that up to 37% of patients will not fill their prescriptions after an asthma exacerbation.38 It was encouraging that results were directionally concurrent; in other words, there were no factors associated with relapse that were found to reduce relapse among the included studies.
Studies discussing asthma relapse are common in the medical literature; however, no similar systematic reviews were identified in our searches. In addition, while most guidelines do make mention of factors associated with relapse, the vast majority are not evidence-based and nor do they provide recommendations on how to use these factors in practice. For example, the most recent guideline from the GINA11 focused on medical management to prevent asthma relapse, provided no summary of factors associated with relapse, and failed to guide clinicians regarding which high-risk patients to target. In a similar vein, the National Review on Asthma Deaths (NRAD) in 2015 identified that 10% of asthma deaths in the UK occur within 28 days of discharge from the ED.39 The authors state that there is a need for health professionals to ‘be aware of the factors that increase the risk of asthma attacks’, without explicitly stating what those factors are.
Factors which could practically be screened to provide the most benefit would include female sex, previous ICS usage and healthcare resource usage. Identifying patients with these traits and targeting them for more explicit discharge planning and rigorous outpatient follow-up might mitigate the severity and frequency of relapses. Options might include the identification of care gaps that may be influencing their asthma attacks (ie, improper inhaler techniques, non-adherence to medication, lack of education), stepping up their preventer medication (ie, adding ICS to those ICS naïve at presentation15 or switching from ICS to ICS/LABA33), providing the medications in the ED rather than the prescriptions or directing strategies from the ED to ensure that patients have close follow-up with a primary care provider for monitoring of symptoms, adjustment on medication and consideration of referrals.
Strengths and limitations
There are several potential limitations to this review that require discussion. First, high-quality evidence in this field is limited and this review included a variety of prospective designs (eg, RCTs and cohorts), which was an important a priori decision. To be reported in the factors associated with relapses, all prospective studies needed to report an adjusted analysis. Second, data collected from patient interviews may be subject to recall bias. With a few exceptions,22 23 data were collected using slightly different interview questions, necessitating some grouping based on author discretion. In addition, differential loss to follow-up or incomplete outcome data in the included studies may have introduced attrition bias. Third, owing to the relatively small number of included studies and overall small sample size, we were unable to formally assess the potential for publication bias; however, comprehensive searches of grey and published literature were performed without restrictions on language, dates or publication status, so it is unlikely that many studies were missed. Fourth, the ORs of non-significant factors from multivariable analyses were not reported in most papers, which may over-represent the influence of some factors. Finally, selection bias is always a concern in systematic reviews; however, two independent reviewers with a separate third-party adjudicator were used throughout all stages of the review in order to minimise selection bias and ensure consistency.
Conclusion
Reducing relapses after treatment for acute asthma represents a potential improvement in the quality of life for patients with asthma and a reducible strain on crowded EDs. Moreover, they present an opportunity to improve outcomes for patients while reducing direct healthcare costs. Practical factors associated with relapse occurrence within 4 weeks of ED discharge have been identified, which may help to stratify patients based on their risks and potentially influence disposition decisions. Further research should focus on strategies to decrease relapses using validated clinical decision rules in order to identify patients at high risk for relapse after discharge, optimise their management and improve outcomes.
Acknowledgments
The authors would like to thank the Emergency Medicine Research Group in the Department of Emergency Medicine at the University of Alberta, especially Scott Kirkland and Leeor Eliyahu for their collaboration throughout the project.
Footnotes
Contributors: JH is the guarantor of the study. JH, NA, CV-R, LD and BHR contributed to the design and execution of the study and the drafting and revision of the manuscript.
Funding: JH was funded by an Alberta Innovates Health Solutions Summer Studentship. NA was funded by the Respiratory Health Strategic Clinical Network (RHSCN) of Alberta Health Services. CV-R was supported by the Canadian Institutes of Health Research (CIHR) in partnership with the Knowledge Translation Branch (Ottawa, Ontario). BHR's research is supported by CIHR through a Tier I Canada Research Chair in Evidence-based Emergency Medicine (Ottawa, Ontario). BHR is the Scientific Director of the Emergency SCN at AHS and the Institute of Circulatory and Respiratory Health (ICRH) at CIHR, and a member of the RHSCN.
Disclaimer: The funding agencies had no input on the conduct of the review and take no responsibility for the content and conclusions presented.
Competing interests: BHR was the principal investigator of three included studies, and C-VR was an investigator in two included studies; however, BHR was excluded from the selection of potentially eligible manuscripts and final inclusion/exclusion decisions and C-VR was not asked to adjudicate on either study. CV-R, JH, NA and LD have reported no potential conflicts of interest that exist with any companies/organisations whose products or services may be discussed in this article.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Croisant S. Epidemiology of asthma: prevalence and burden of disease. Adv Exp Med Biol 2014;795:17–29. doi:10.1007/978-1-4614-8603-9_2 [DOI] [PubMed] [Google Scholar]
- 2.Masoli M, Fabian D, Holt S et al. for the Global Initiative for Asthma (GINA) Program. The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy 2004;59:469–78. doi:10.1111/j.1398-9995.2004.00526.x [DOI] [PubMed] [Google Scholar]
- 3.Loymans RJ, Gemperli A, Cohen J et al. Comparative effectiveness of long term drug treatment strategies to prevent asthma exacerbations: network meta-analysis. BMJ 2014;348:g3009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stableforth D. Death from asthma. Thorax 1983;38: 801–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ivanova JI, Bergman R, Birnbaum HG et al. Effect of asthma exacerbations on health care costs among asthmatic patients with moderate and severe persistent asthma. J Allergy Clin Immunol 2012;129:1229–35. doi:10.1016/j.jaci.2012.01.039 [DOI] [PubMed] [Google Scholar]
- 6.Hasegawa K, Tsugawa Y, Brown DF et al. A population-based study of adults who frequently visit the emergency department for acute asthma. California and Florida, 2009–2010. Ann Am Thorac Soc 2014;11:158–66. doi:10.1513/AnnalsATS.201306-166OC [DOI] [PubMed] [Google Scholar]
- 7.Lawson CC, Carroll K, Gonzalez R et al. “No other choice": reasons for emergency department utilization among urban adults with acute asthma. Acad Emerg Med 2014;21:1–8. doi:10.1111/acem.12285 [DOI] [PubMed] [Google Scholar]
- 8.Rowe BH, Bota GW, Clark S et al. Multicenter Airway Research Collaboration. Comparison of Canadian versus American emergency department visits for acute asthma. Can Respir J 2007;14:331–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lougheed MD, Garvey N, Chapman KR et al. The Ontario Asthma Regional Variation Study: emergency department visit rates and the relation to hospitalization rates. Chest 2006;129:909–17. doi:10.1378/chest.129.4.909 [DOI] [PubMed] [Google Scholar]
- 10.National Asthma Education Prevention Program. Guidelines for the Diagnosis and Management of Asthma. 3rd edn https://www.nhlbi.nih.gov/about/org/naepp (accessed 3 Jan 2016). [Google Scholar]
- 11.Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention 2015. http://www.ginasthma.org (accessed 3 Jan 2016).
- 12.Lougheed MD, Lemiere C, Ducharme FM et al. Canadian Thoracic Society 2012 guideline update: diagnosis and management of asthma in preschoolers, children and adults. Can Respir J 2012;19:127–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hasegawa K, Sullivan AF, Tsugawa Y et al. Comparison of US emergency department acute asthma care quality: 1997–2001 and 2011–2012. J Allergy Clin Immunol 2015;135:73–80. doi:10.1016/j.jaci.2014.08.028 [DOI] [PubMed] [Google Scholar]
- 14.Edmonds ML, Milan SJ, Camargo CA Jr et al. Early use of inhaled corticosteroids in the emergency department treatment of acute asthma. Cochrane Database Syst Rev 2012;(12):CD002308 doi:10.1002/14651858.CD002308.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rowe BH, Bota GW, Fabris L et al. Inhaled budesonide in addition to oral corticosteroids to prevent asthma relapse following discharge from the emergency department: a randomized controlled trial. JAMA 1999;281:2119–26. [DOI] [PubMed] [Google Scholar]
- 16.Rowe BH, Spooner CH, Ducharme FM et al. Corticosteroids for preventing relapse following acute exacerbations of asthma. Cochrane Database Syst Rev 2001;(1):CD000195 doi:10.1002/14651858.CD000195 [DOI] [PubMed] [Google Scholar]
- 17.Edmonds ML, Milan SJ, Brenner BE et al. Inhaled steroids for acute asthma following emergency department discharge. Cochrane Database Syst Rev 2012;(12):CD002316 doi:10.1002/14651858.CD002316.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Canadian Agency for Drugs and Technologies in Health. Long-acting beta(2)-agonist and inhaled corticosteroid combination therapy for adult persistent asthma: systematic review of clinical outcomes and economic evaluation. CADTH Technol Overv 2010;1:e0120. [PMC free article] [PubMed] [Google Scholar]
- 19.Tapp S, Lasserson TJ, Rowe BH. Education interventions for adults who attend the emergency room for acute asthma. Cochrane Database Syst Rev 2007;(3):CD003000 doi:10.1002/14651858.CD003000.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Villa-Roel C, Nikel T, Ospina M et al. Effectiveness of educational interventions to increase primary care follow-up for adults seen in the Emergency Department for Acute Asthma: a systematic review and meta-analysis. Acad Emerg Med 2016;23:5–13. doi:10.1111/acem.12837 [DOI] [PubMed] [Google Scholar]
- 21.Fitzgerald JM, Hargreave FE. Acute asthma: emergency department management and prospective evaluation of outcome. CMAJ 1990;142:591–5. [PMC free article] [PubMed] [Google Scholar]
- 22.Rowe BH, Villa-Roel C, Sivilotti ML et al. Relapse after emergency department discharge for acute asthma. Acad Emerg Med 2008;15:709–17. doi:10.1111/j.1553-2712.2008.00176.x [DOI] [PubMed] [Google Scholar]
- 23.Rowe BH, Villa-Roel C, Majumdar SR et al. Rates and correlates of relapse following ED discharge for acute asthma: a Canadian 20-site prospective cohort study. Chest 2015;147:140–9. doi:10.1378/chest.14-0843 [DOI] [PubMed] [Google Scholar]
- 24.McCarren M, McDermott MF, Zalenski RJ et al. Prediction of relapse within eight weeks after an acute asthma exacerbation in adults. J Clin Epidemiol 1998;51:107–18. [DOI] [PubMed] [Google Scholar]
- 25.Emerman CL, Cydulka RK. Factors associated with relapse after emergency department treatment for acute asthma. Ann Emerg Med 1995;26:6–11. [DOI] [PubMed] [Google Scholar]
- 26.Emerman CL, Woodruff PG, Cydulka RK et al. Prospective multicenter study of relapse following treatment for acute asthma among adults presenting to the emergency department. MARC investigators. Multicenter Asthma Research Collaboration. Chest. 1999;115:919–27. [DOI] [PubMed] [Google Scholar]
- 27.Sandy C. A filter to retrieve studies related to Emergency Departments from the OVID MEDLINE Database. John W. Scott Health Sciences Library, University of Alberta, 2015. [Google Scholar]
- 28.Singh AK, Cydulka RK, Stahmer SA et al. Sex differences among adults presenting to the emergency department with acute asthma. Multicenter Asthma Research Collaboration Investigators. Arch Intern Med 1999;159(28(11):1237–43. [DOI] [PubMed] [Google Scholar]
- 29.Lin D, Yarascavitch A, Wilmott A et al. Asthma bouncebacks at 2 urban Canadian emergency room departments [abstract]. CJEM 2009;11:299. [Google Scholar]
- 30.Prabhakaran L, Vasu A, Yian TS et al. The current care delivery practice for asthma at the Emergency Department in a tertiary Hospital in Singapore. J Asthma Allergy Educators 2013;4:15–21. [Google Scholar]
- 31.Baibergenova A, Thabane L, Akhtar-Danesh N et al. Patient characteristics associated with nocturnal emergency department visits for asthma. J Asthma 2006;43:469–75. doi:10.1080/02770900600758382 [DOI] [PubMed] [Google Scholar]
- 32.Withy K, Davis J. Follow-up after an emergency department visit for asthma: urban/rural patterns. Ethn Dis 2008;18(2 Suppl 2):S2–247–51. [PMC free article] [PubMed] [Google Scholar]
- 33.Rowe BH, Wong E, Blitz S et al. Adding long-acting ß-agonists to inhaled corticosteroids after discharge from the emergency department for acute asthma: a randomized controlled trial. Acad Emerg Med 2007;14((10):833–40. doi:10.1197/j.aem.2007.06.020 [DOI] [PubMed] [Google Scholar]
- 34.FitzGerald JM, Shragge D, Haddon J et al. A randomized, controlled trial of high dose, inhaled budesonide versus oral prednisone in patients discharged from the emergency department following an acute asthma exacerbation. Can Respir J 2000;7:61–7. [DOI] [PubMed] [Google Scholar]
- 35.Silverman RA, Nowak RM, Korenblat PE et al. Zafirlukast treatment for acute asthma: evaluation in a randomized, double-blind, multicenter trial. Chest 2004;126:1480–9. doi:10.1378/chest.126.5.1480 [DOI] [PubMed] [Google Scholar]
- 36.Khoo HS, Lim YW, Vrijhoef HJM. Primary healthcare system and practice characteristics in Singapore. Asia Pac Fam Med 2014;13:8 doi:10.1186/s12930-014-0008-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Postma DS. Gender differences in asthma development and progression. Gend Med 2007;4(Suppl(B):S133–46. [DOI] [PubMed] [Google Scholar]
- 38.Hatoun J, Bair-Merritt M, Cabral H et al. Increasing medication possession at discharge for patients with asthma: the meds-in-hand project. Pediatrics 2016;137:1–8. [DOI] [PubMed] [Google Scholar]
- 39.Royal College of Physicians. Why asthma still kills: the National Review of Asthma Deaths (NRAD) Confidential Enquiry report . London: RCP, 2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjresp-2016-000169supp_appendix.pdf (131.3KB, pdf)