Abstract
Endometrioid carcinoma with a prominent squamous component has the ability to mimic pilomatrixoma. One previous case is documented of cutaneous metastasis in the upper limb derived from ovarian endometrioid carcinoma mimicking pilomatrixoma. Here, we describe a case of metastasis of endometrial endometrioid carcinoma in the distal vagina, treated with radiotherapy and later resected. The histology of the lesion was thought initially to represent pilomatrixoma; this has not previously been described in the vagina, where no hair matrix cells are normally present. We hypothesise that radiotherapy may have effectively ‘sterilised’ the glandular component, blinding the malignant features. Further management was significantly altered by the reinterpretation of this result as metastatic disease. We emphasise that in the context of known endometrioid carcinoma, the diagnosis of pilomatrixoma should be made with caution, particularly where radiotherapy has been used.
Background
The ability of endometrioid carcinoma to mimic pilomatrixoma (a benign tumour derived from hair follicles) was first described in 1996.1 This phenomenon was originally described in a case of ovarian endometrioid carcinoma, which showed areas of terminally differentiated squamous cells with ghost cells, typical of pilomatrixoma of the skin. The interpretation of this result was initially debated: a case of pilomatrixoma-like tissue in the ovary, found incidentally alongside primary endometrial endometrioid carcinoma, was reported as an atypical differentiation of mature teratoma.2 A report in 1998 noted the ability of visceral carcinomas having squamous metaplasia to exhibit pilomatrixoma-like features; specifically, 6% of endometrioid carcinomas were noted to show ghost cells.3 The authors therefore suggested that the diagnosis of pilomatrixoma should be made with caution where there is a history of endometrioid carcinoma.3 In 2010, the first case of cutaneous metastasis of endometrioid carcinoma mimicking skin pilomatrixoma was reported in the upper limb.4 Here, we report the second case of metastasis: in this case to the distal vagina, a site where primary pilomatrixoma is not known to occur. Differentiation between a benign pilomatrixoma and an endometrioid carcinoma makes an important clinical difference and this case should be considered as a note of caution.
Case presentation
We present the case of a woman aged 55 years with a history of endometrial endometrioid carcinoma, FIGO5 stage 1A grade 2, treated with total laparoscopic hysterectomy and bilateral salpingo-oopherectomy in 2012. No adjuvant treatment was given. At the routine 3-year follow-up, the patient reported occasional vaginal and rectal bleeding. On examination, a lesion was noted involving the distal posterior wall of the vagina and introitus. A biopsy was taken, which subsequently identified metastatic disease strongly ER and PR-positive. Subsequent MRI showed a 29 mm lesion in the perineum involving the posterior wall of the vagina, adjacent to, but not invading, the anterior rectum. CT at this time also showed multiple metastases within the lungs. Palliative radiotherapy was performed: 27.5 Gy in 10 fractions over 12 days in August 2015, with subsequent hormonal treatment (megestrol acetate 160 mg daily).
Response to therapy was significant with reduction in lung disease and the vaginal lesion. Following interdisciplinary discussion (involving the patient), a decision was made to resect the remaining vaginal lesion with further subsequent radiotherapy to achieve local control. Resection was performed in December 2015. The lesion in the left posterior vaginal wall had separated into several smaller lesions within an area measuring 2 cm in diameter with one small 2 mm necrotic appearing deposit (preoperative image, figure 1). Excision was performed, with the deep margin appearing to extend to the fascia directly adjacent to the rectal mucosa.
Figure 1.

Preoperative image showing left posterior vaginal wall lesions involving the introitus after initial radiotherapy.
Histology of the excised lesion showed vaginal tissue with a nodular mass of calcified material in the corium associated with ghost cells and an accompanying foreign body giant cell reaction around the calcification. The appearances were thought typical of a pilomatrixoma (figure 2A).
Figure 2.
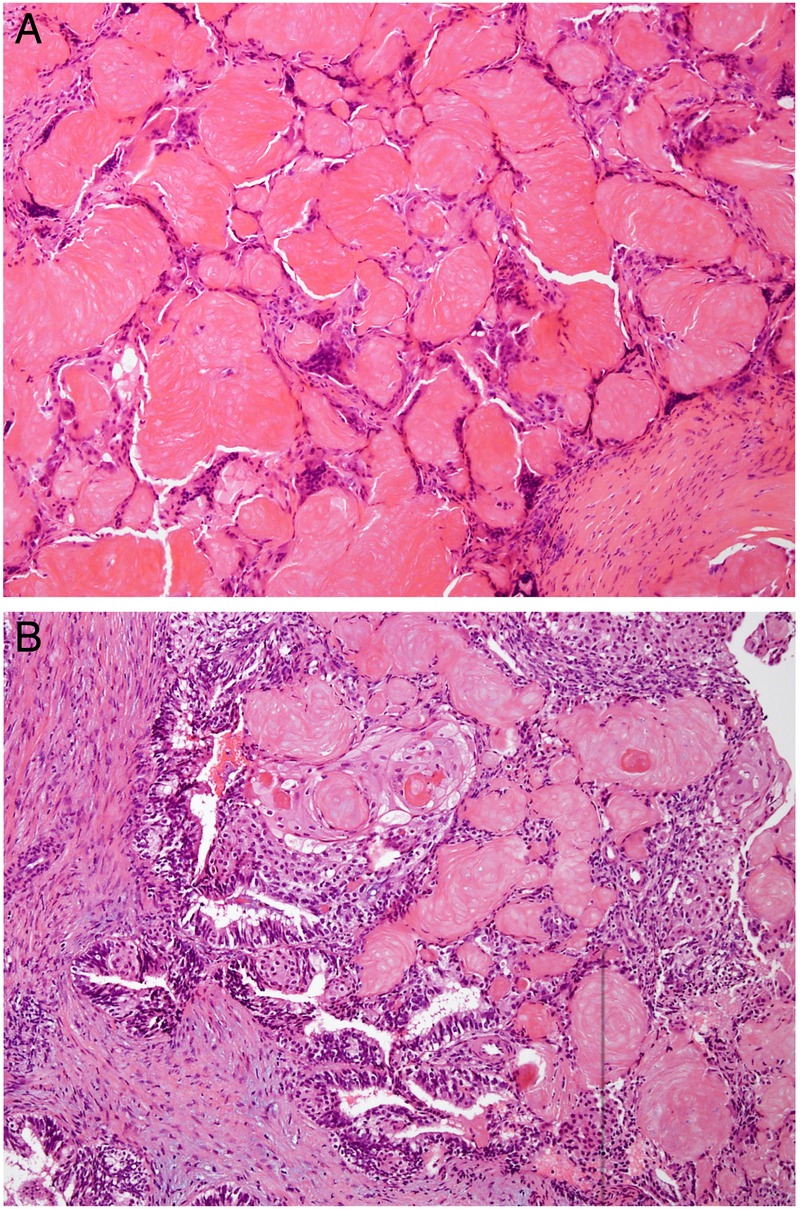
(A) H&E-stained section of the postradiotherapy vaginal lesion with nests of eosinophilic ‘ghost cells’ showing outlines of necrotic cells without retained nuclei surrounded by foreign body type giant cells mimicking a pilomatrixoma. (B) H&E-stained section of the first vaginal recurrence showing a central focus of endometrioid adenocarcinoma with squamous metaplasia and adjacent foci of acellular ghosts of squamous epithelium identical to those in the second lesion.
This result was discussed in detail at a multidisciplinary meeting. Given that this lesion is not recognised to occur in this anatomic location, where there is normally an absence of hair matrix cells, a literature search was performed to identify any published cases of vaginal pilomatrixoma. Several large pilomatrixoma case series were identified, none of which reported any genital pilomatrixomas.6–9 One case was identified, however, describing metastatic endometrioid ovarian adenocarcinoma mimicking pilomatrixoma.4 This occurred in a patient who had widespread metastatic disease. The identified lesions involved the upper limb and axilla, initially interpreted as pilomatrixoma, however, after further review were reclassified as metastases.
In light of this, the original pathology from this case was reviewed. The presenting endometrial tumour showed striking squamous metaplasia and review of the initial vaginal recurrence from 2015 showed recurrent carcinoma and a background of necrotic squamous epithelium resembling ghost cells of a pilomatrixoma (figure 2B). The second recurrence showed only the ghost cell component, closely mimicking a pilomatrixoma, possibly due to ‘sterilisation’ of the glandular component following radiotherapy.
Outcome and follow-up
Further radiotherapy was applied (40 Gy in 20 fractions) with no further local recurrence to date and no further vaginal or rectal bleeding. Radiotherapy was well tolerated with no further vaginal symptoms.
Discussion
This case demonstrates the second documented report of metastatic endometrioid carcinoma being initially interpreted as benign pilomatrixoma. Our case differs from the previous case report in several ways. The time from initial diagnosis to metastasis was 3 years (1 month in the previous case). The primary site of malignancy was the endometrium (ovary in the previous case). Finally, the site of recurrence was the vaginal mucosa (skin of the upper limb and axilla in the previous case). There are no previous reports of pilomatrixoma presenting in the vaginal mucosa where there is an absence of hair matrix cells. Additionally, ∼60% of pilomatrixomas are diagnosed in the first two decades of life, with <25% presenting over the age of 50.6–8 The diagnosis of pilomatrixoma should be made with caution in postmenopausal women, particularly in sites where pilomatrixoma is uncommon or not known to occur. In both cases discussed, metastatic disease was evident prior to the diagnosis, and in both cases, radiotherapy was used, raising the possibility of a ‘sterilisation’ phenomenon of the glandular component of the tissue resulting in the pilomatrixoma-like appearance.
Learning points.
In patients with a history of endometrioid carcinoma, the diagnosis of pilomatrixoma should be made with caution, particularly where radiotherapy has been used; metastatic disease must be considered.
Where unexpected results are obtained, documented case reports may change interpretation of results and therefore considerably influence patient management.
Where radiation therapy has been applied, histological lesions may show unexpected features (or lack thereof), and should be interpreted with caution.
Footnotes
Contributors: SMS drafted the manuscript and collated contributions from other authors. PB made the pathological diagnosis, and provided comments and images related to histology. CJ was the radiation oncologist involved in the case and provided discussion, input and patient communication (including written consent). OM was the gynaecology oncologist involved in the case, performed the surgery (with images included in the report) and provided input and comments around the case.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Fang J, Keh P, Katz L et al. Pilomatricoma-like endometrioid adenosquamous carcinoma of the ovary with neuroendocrine differentiation. Gynecol Oncol 1996;61:291–3. 10.1006/gyno.1996.0142 [DOI] [PubMed] [Google Scholar]
- 2.Alfsen GC, Strom EH. Pilomatrixoma of the ovary: a rare variant of mature teratoma. Histopathology 1998;32:182–3. 10.1046/j.1365-2559.1998.0285c.x [DOI] [PubMed] [Google Scholar]
- 3.Zámecník M, Michal M, Mukensnábl P. Pilomatrixoma-like visceral carcinomas. Histopathology 1998;33:395 10.1046/j.1365-2559.1998.00125.x [DOI] [PubMed] [Google Scholar]
- 4.Lalich D, Tawfik O, Chapman J et al. Cutaneous metastasis of ovarian carcinoma with shadow cells mimicking a primary pilomatrical neoplasm. Am J Dermatopathol 2010;32:500–5. 10.1097/DAD.0b013e3181c6dfc1 [DOI] [PubMed] [Google Scholar]
- 5.Amant F, Mirza MR, Koskas M et al. Cancer of the corpus uteri. Int J Gynaecol Obstet 2015;131(Suppl 2):S96–S104. 10.1016/j.ijgo.2015.06.005 [DOI] [PubMed] [Google Scholar]
- 6.Moehlenbeck FW. Pilomatrixoma (calcifying epithelioma). A statistical study. Arch Dermatol 1973;108:532–4. 10.1001/archderm.1973.01620250020004 [DOI] [PubMed] [Google Scholar]
- 7.Wang J, Cobb CJ, Martin SE et al. Pilomatrixoma: clinicopathologic study of 51 cases with emphasis on cytologic features. Diagn Cytopathol 2002;27:167–72. 10.1002/dc.10161 [DOI] [PubMed] [Google Scholar]
- 8.Guinot-Moya R, Valmaseda-Castellon E, Berini-Aytes L et al. Pilomatrixoma. Review of 205 cases. Med Oral Patol Oral Cir Bucal 2011;16:e552–5. 10.4317/medoral.16.e552 [DOI] [PubMed] [Google Scholar]
- 9.Hernandez-Núñez A, Nájera Botello L, Romero Maté A et al. Retrospective study of pilomatricoma: 261 tumors in 239 patients. Actas Dermosifiliogr 2014;105:699–705. 10.1016/j.ad.2014.01.003 [DOI] [PubMed] [Google Scholar]


