Abstract
Although rare in the oral cavity, oral non-Hodgkin lymphoma frequently mimics odontogenic and other oral pathologies. The purpose of this report is to discuss the diagnostic difficulty in a case of a 75-year-old man with diffuse large B-cell lymphoma presenting initially as a toothache.
Background
Lymphoma is a heterogeneous malignancy of the lymphatic system. Characterised by proliferation of lymphocytes or their precursors, lymphomas are broadly categorised into Hodgkin (HL) and non-Hodgkin lymphoma (NHL), respectively, depending on the presence or absence of the so-called Reed-Sternberg cells.1 NHL is by far more common than HL, and includes more than 20 subtypes of lymphoid neoplasms.1
As opposed to HL, NHL often (10–50%) presents outside lymph nodes at sites such as the gastrointestinal tract, skin, testes, central nervous system, orbit, kidney and salivary glands.2 3 Although rare, NHL can present in the oral cavity; accounting for ∼3.5% of all intraoral malignancies.3 4 Oral lymphoma is often a component of disseminated disease process that may also involve regional lymph nodes. However, lymphoma may present primary extranodal disease confined to the oral cavity.4–6 The palate, gingivae and the base of the tongue are the most frequently reported sites.7–10 A recent systematic review concluded that overall, diffuse large B-cell lymphoma (DLBCL) is the most common subtype affecting the oral cavity followed by small lymphocytic lymphoma and Burkitt's lymphoma; DLBCL is more common among adults and HIV patients, and Burkitt's lymphoma is more common in children.11
The clinical presentation of NHL in the oral cavity is often non-specific, and might resemble other disorders including other malignant diseases. Frequently reported presentations include persistent pain, swelling, or ulcerated mass, labial parasthesia or other sensory changes, facial asymmetry, and tooth loosening.4–10 Occasionally, NHL might mimic an odontogenic infection or periapical/periodontal disease.
In this report we discuss the diagnostic difficulty in a case of DLBCL presenting as chronic apical periodontitis.
Case presentation
A 75-year-old man initially presented with a dull and throbbing pain in the lower left quadrant for the past 2 weeks. His medical history was significant for prostate cancer successfully treated with chemotherapy 3 years previously. He was non-smoker and occasional drinker of alcohol. Extraoral examination revealed no fever, cervical lymphadenopathy or facial swelling. Intraoral examination revealed that the lower teeth were endodontically treated and restored with full coverage crowns. The lower left first and second premolar teeth were tender to percussion, but showed no mobility or periodontal pocketing. The lower left buccal vestibule was tender to palpation, but there was no erythema or swelling; a clinical diagnosis of chronic apical periodontitis was made, and the patient was prescribed an analgesic (400 mg ibuprofen per needed) and referred for an endodontic care where root canal retreatment of the lower left first and second premolars was performed. One week following root canal therapy, the patient returned with the same symptom of dull pain in the lower left quadrant. Intraoral examination at this point revealed a localised fluctuant swelling in the lower left buccal vestibule opposite to the lower left first and second premolar teeth. A diagnosis of apical abscess was made; incision and drainage was performed and revealed thick yellowish purulent discharge. The patient was prescribed an antibiotic (500 mg amoxicillin three times per day for 5 days) and scheduled for re-evaluation of the root canal treatment. Two weeks later, he presented at the re-evaluation appointment with the symptom of vestibular swelling and dull pain accompanied with an intermittent numbness of the lower lip.
Investigations
Given the patient's poor response to root canal therapy and antibiotics, and the development of lip hypoesthesia with no obvious cause, a panoramic X-ray was requested, which revealed a prominent but ill-defined radiolucency within the body of the left mandible (figure 1). A CT scan revealed the presence of an osteolytic lesion involving the left body of the mandible and causing partial erosion of the lingual cortical plate (figure 2). A bone biopsy was performed under local anaesthesia and revealed the presence of a jelly-like tissue occupying the left mandibular body in the premolars and molars area; the tissue was soft and easily fragmented (figure 3). Histopathological examination showed multiple fragments of necrotic tissues and chronic inflammatory cell infiltrate with proliferation of large cells with moderate cytoplasm, large vesicular nuclei and prominent nucleoli. The cells were positive for CD-20, PAX5, BCL-2, and negative for BCL-6, cyclin-D1, CD-3 and CD-5. Ki67 immunostaining showed a proliferation index of 70% (figure 4). The pathological features were consistent with the diagnosis of DLBCL. Complete blood count indices were within normal limits, and HIV serology proved negative.
Figure 1.
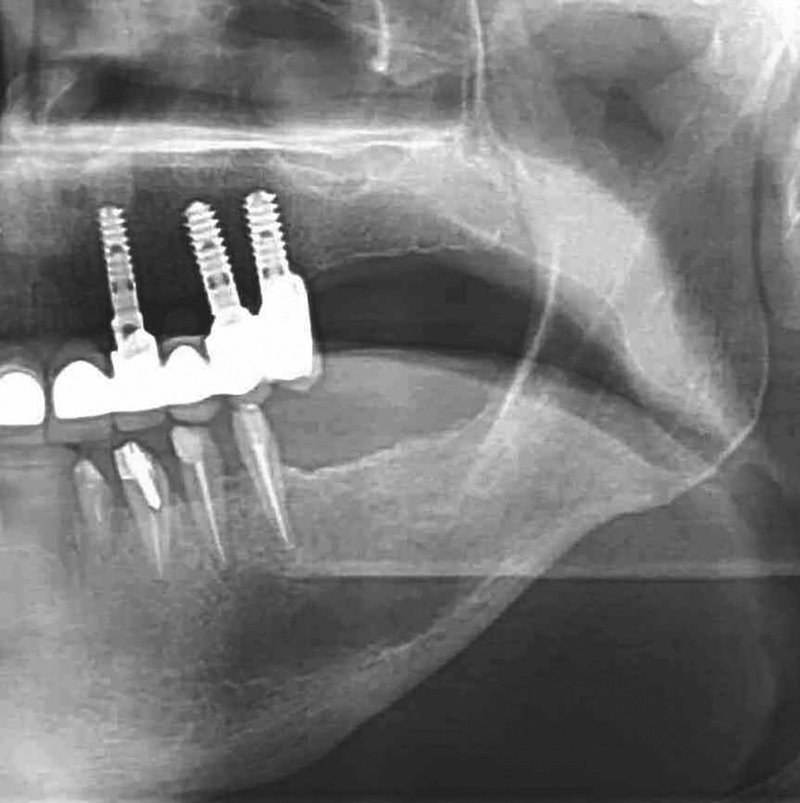
An orthopantogram showing widening of the apical periodontal ligament in the lower left premolars, and a prominent, but ill-defined radiolucency within the body of the left mandible.
Figure 2.

Axial CT showing a lytic lesion in the left mandibular body with partial erosion of the lingual cortical plate.
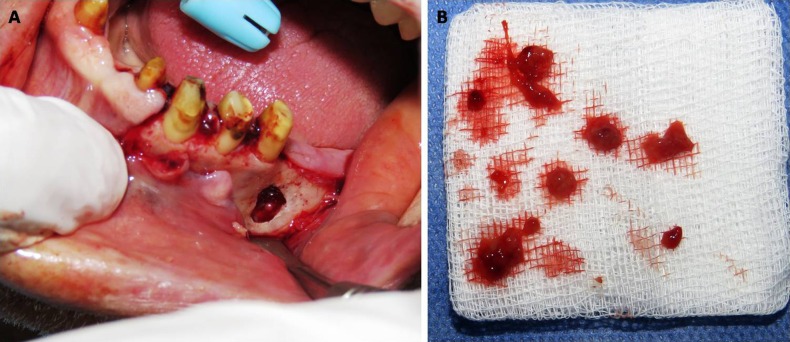
Figure 3.
Bone biopsy revealed jelly-like tissue occupying the left mandibular body. The tissue was soft and fragmented easily.
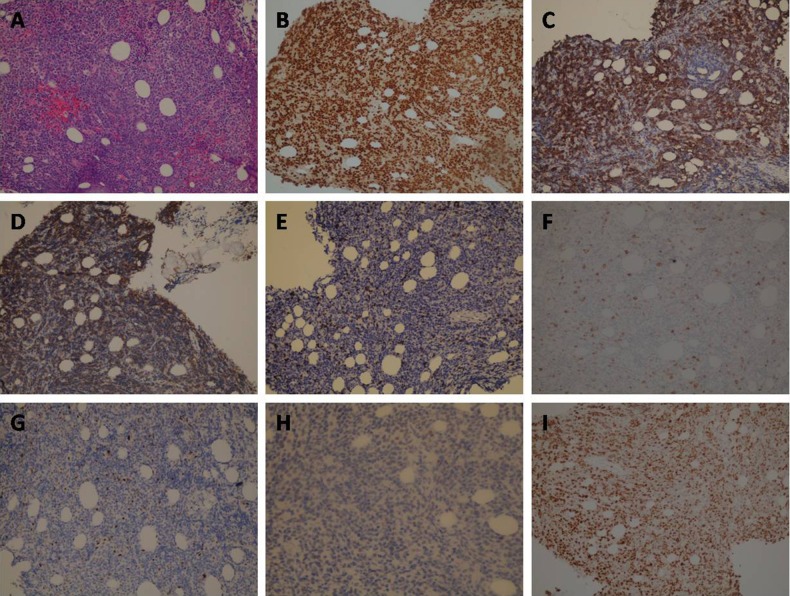
Figure 4.
(A) Proliferation of large cells with moderate cytoplasm, large vesicular nuclei and prominent nucleoli (×200); (B) positive staining for PAX-5 (×200); (C) positive staining for BCL-2 (×200); (D) positive staining for CD-20 (×200); (E) negative staining for CD-3 (×200); (F) negative staining for CD-5 (×200); (G) negative staining for BCL-6 (×200); (H) negative staining for cyclin-D1(×200); (I) Ki67 immunostaining showed a proliferation index of ∼70% (×200).
Differential diagnosis
The initial clinical findings of dull pain and tenderness to percussion were suggestive of the clinical diagnosis of apical periodontitis of dental origin, but the lack of response to dental treatment, the history of previous cancer treatment, and the development of lower lip numbness brought up a concern about the possibility of metastasis from the previously treated prostate cancer or a malignant process, including lymphoma, involving the mandible or skull base.
Treatment
At the time the diagnosis was reached, the patient started to have symptoms of general fatigue, intermittent fever, loss of appetite and night sweating; features consistent with the diagnosis of lymphoma. The patient was referred to oncology where full body clinical and radiological examination revealed multiorgan involvement including bone marrow; the patient was staged IV-B and scheduled for R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine and prednisolone) therapy.
Outcome and follow-up
The patient showed poor response to therapy, and died 4 months after initial presentation to the dental clinic.
Discussion
Lymphoma arising within the oral cavity accounts for about 3.5% of all intraoral malignancies; most are NHL affecting primarily the palate, gingivae and base of the tongue.2 When affecting the oral cavity, NHL frequently presents initially with indolent clinical features that mimic odontogenic inflammatory process.4–10 The initial presenting symptoms in our patient were those of chronic apical periodontitis, and similar to previous reports, our patient had no B symptoms at presentation.12–16 The presence of fever, weight loss, night sweating, fatigue or loss of appetite in a patient presenting with an odontogenic infection should alert the clinician to the possibility of a hidden lymphoma. Another alerting symptom that should be considered seriously is numbness or parasthesia in the region innervated by the mental nerve such as the lower lip, anterior gingivae or the chin. Mental nerve neuropathy, also known as numb chin syndrome, is an important clinical sign that might be caused by iatrogenic oral surgeries, trauma, systemic diseases or malignancy. Galán Gil et al17 reported that 40% of cases presenting with numb chin syndrome are due to cancer metastasis from breast or prostate, and 20% due to NHL of the mandible or skull base. The development of lower lip numbness in our patient combined with the history of previous cancer treatment brought up a concern about the possibility of metastasis from the previously treated prostate cancer or a malignant process, involving the mandible or skull base.
Data about prognosis of lymphoma presenting as an odontogenic inflammatory process are limited, but it is generally known however that the prognosis of lymphoma depends on several factors including patient's age and his performance status, the stage and type of lymphoma, and the blood level of lactate dehydrogenase. The international prognostic index (IPI) is an accepted tool for predicting outcome in patients with lymphoma. The validity of IPI for lymphoma involving the oral region is questionable because of the rarity of such presentation and the lack of large multicentre studies evaluating its usefulness.4
Learning points.
Although rare, non-Hodgkin lymphoma (NHL) might present as an odontogenic inflammatory process.
Diffuse large B-cell lymphoma is the most common type of NHL affecting the oral cavity.
A diagnosis of lymphoma should be suspected if a patient with an odontogenic infection presents with mental nerve neuropathy or systemic symptoms such as night sweating, weight loss, fatigue and loss of appetite.
Acknowledgments
The authors would like to thank Dr Omar Al karadsheh for critical reading of the manuscript.
Footnotes
Contributors: YH was involved in the diagnosis, patient management, literature search and writing the manuscript. GA and AA were involved in pathological interpretation. CS was involved in manuscript design and writing.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Swerdlow SH, Campo E, Pileri SA et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood 2016;127:2375–90. 10.1182/blood-2016-01-643569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Epstein JB, Epstein JD, Le ND et al. Characteristics of oral and paraoral malignant lymphoma: a population-based review of 361 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;92:519–25. 10.1067/moe.2001.116062 [DOI] [PubMed] [Google Scholar]
- 3.Triantafillidou K, Dimitrakopoulos J, Iordanidis F et al. Extranodal non-Hodgkin lymphomas of the oral cavity and maxillofacial region: a clinical study of 58 cases and review of the literature. J Oral Maxillofac Surg 2012;70:2776–85. 10.1016/j.joms.2012.01.018 [DOI] [PubMed] [Google Scholar]
- 4.van der Waal RI, Huijgens PC, van der Valk P et al. Characteristics of 40 primary extranodal non-Hodgkin lymphomas of the oral cavity in perspective of the new WHO classification and the International Prognostic Index. Int J Oral Maxillofac Surg 2005;34:391–5. 10.1016/j.ijom.2004.08.009 [DOI] [PubMed] [Google Scholar]
- 5.Margiotta V, Franco V, Rizzo A et al. Gastric and gingival localization of mucosa-associated lymphoid tissue (MALT) lymphoma. An immunohistochemical, virological and clinical case report. J Periodontol 1999;70:914–18. [DOI] [PubMed] [Google Scholar]
- 6.Scully C, Eveson JW, Witherow H et al. Oral presentation of lymphoma: case report of T-cell lymphoma masquerading as oral Crohn's disease, and review of the literature. Eur J Cancer B Oral Oncol 1993;29B:225–9. 10.1016/0964-1955(93)90027-C [DOI] [PubMed] [Google Scholar]
- 7.Porter SR, Diz Dios P, Kumar N et al. Oral plasmablastic lymphoma in previously undiagnosed HIV disease. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;87:730–4. 10.1016/S1079-2104(99)70170-8 [DOI] [PubMed] [Google Scholar]
- 8.Kemp S, Gallagher G, Kabani S et al. Oral non-Hodgkin's lymphoma: review of the literature and World Health Organization classification with reference to 40 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;105:194–201. 10.1016/j.tripleo.2007.02.019 [DOI] [PubMed] [Google Scholar]
- 9.Ramanathan A, Mahmoud HA, Hui LP et al. Oral extranodal non Hodgkin's lymphoma: series of forty two cases in Malaysia. Asian Pac J Cancer Prev 2014;15:1633–7. 10.7314/APJCP.2014.15.4.1633 [DOI] [PubMed] [Google Scholar]
- 10.Laskaris G, Stergiou G, Kittas C et al. Hodgkin's disease involving the gingiva in AIDS. Eur J Cancer B Oral Oncol 1992;28B:39–41. 10.1016/0964-1955(92)90010-X [DOI] [PubMed] [Google Scholar]
- 11.Silva TD, Ferreira CB, Leite GB et al. Oral manifestations of lymphoma: a systematic review. Ecancermedicalscience 2016;17:665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Richards A, Costelloe MA, Eveson JW et al. Oral mucosal non-Hodgkin's lymphoma—a dangerous mimic. Oral Oncol 2000;36:556–8. 10.1016/S1368-8375(00)00047-6 [DOI] [PubMed] [Google Scholar]
- 13.Jaradat JM, Potluri A, Bilodeau EA. B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell lymphoma and Burkitt lymphoma: report of a case in the oral cavity. Indian J Dent Res 2013;24:384–6. 10.4103/0970-9290.118016 [DOI] [PubMed] [Google Scholar]
- 14.Dhanrajani PJ, Swaify GA, Khateery SM. Malignant lymphoma presenting as pericoronitis. A case report. Int J Oral Maxillofac Surg 1992;21:295–6. 10.1016/S0901-5027(05)80741-6 [DOI] [PubMed] [Google Scholar]
- 15.Sivolella S, Rizzo G, Valente M et al. Sporadic Burkitt lymphoma mimicking osteomyelitis of the mandible revealing clinically unsuspected HIV infection. Anticancer Res 2015;35:4837–9. [PubMed] [Google Scholar]
- 16.Yamada T, Mishima K, Ota A et al. A case of ATLL (adult T-cell leukemia/lymphoma) mimicking odontogenic infection. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:e51–5. 10.1016/j.tripleo.2010.02.021 [DOI] [PubMed] [Google Scholar]
- 17.Galán Gil S, Peñarrocha Diago M, Peñarrocha Diago M. Malignant mental nerve neuropathy: systematic review. Med Oral Patol Oral Cir Bucal 2008;13:E616–21. [PubMed] [Google Scholar]