Abstract
Little is known about implications of temperament for children who receive nitrous oxide inhalation sedation (N2O/O2) for dental care. The aim of this study was to investigate whether child temperament is associated with success in N2O/O2. Child-caregiver dyads were enrolled from patients aged 36–95 months receiving dental care with N2O/O2 at a university-based pediatric dental clinic. To assess child temperament, 48 caregivers completed the Children's Behavior Questionnaire Short Form. Patient behavior was abstracted from Frankl scores recorded in the patient's chart. The overall behavioral failure rate was 15% (n = 7/48). There was no significant difference in sedation outcome associated with sex, health, insurance status, or complexity of treatment provided. Sedation outcome was significantly associated with the broad temperament domain of Effortful Control and its subscales Attentional Focusing and Inhibitory Control. The Negative Affectivity subscales of Frustration, Sadness, and Soothability and the Extraversion/Surgency subscales Activity and Impulsivity were also significantly associated with sedation outcome. The results of this study suggest that Effortful Control is associated with behavior during dental treatment with N2O/O2. The subscales of Attention Focusing, Inhibitory Control, Frustration, Fear, Sadness, Soothability, Activity, and Impulsivity may also be important determinants of child behavior during dental treatment.
Key Words: Sedation, Temperament, Psychology, Child
Nitrous oxide inhalation sedation (N2O/O2) is commonly employed to improve cooperation for pediatric dental procedures. The clinical efficacy of nitrous oxide is sufficient and predictable in most cases. However, there are children for whom nitrous oxide fails to provide adequate levels of sedation. For example, Burnweit et al found that N2O/O2 effectively facilitated minor surgical procedures for greater than 95% of their pediatric patients, and Soldani et al reported similar results for pediatric patients receiving orthodontic extractions.1–4 While N2O/O2 is effective for many children, inconsistency in efficacy may result in an aborted, traumatic, or even harmful dental experience for the child. In turn, early traumatic dental visits can contribute to lifelong dental fear and avoidance.5,6 Therefore, a dentist's ability to accurately predict a child's capacity and willingness to cooperate during a procedure becomes a major determining factor in the decision to use nitrous oxide to facilitate a positive dental experience.7
A number of studies have attempted to determine factors associated with positive behavior during dental treatment. Most of this research has explored how child temperament affects sedation outcome.8–12 Temperament was defined by Rothbart et al13 as “individual differences in reactivity and self-regulation assumed to have a constitutional basis.” Rothbart et al developed the Children's Behavior Questionnaire (CBQ) and its derivative, the Children's Behavior Questionnaire Short Form (CBQ-SF), which have emerged as the most frequently used mechanisms in contemporary research of evaluating child temperament.14 These instruments evaluate a wide variety of temperament characteristics, including an individual's ability to maintain attention, self-regulation, baseline activity level, and impulsivity. The CBQ-SF temperament instrument is validated for children aged 36–95 months. Recently, Lane et al15 used the CBQ-SF and showed that children with impulsive behavior were more likely to demonstrate lack of cooperation during oral sedation. To our knowledge, there are no published studies investigating child temperament during dental treatment when employing only N2O/O2. The purpose of this study was to determine associations between child temperament, as determined by the CBQ-SF, and N2O/O2 outcomes.
METHODS
Experimental Subjects
The study was approved by the ethics committee of the University of Washington (UW; issue date June 9, 2014, registration 47262). On the day of the treatment visit, informed consent to participate in the study was obtained from the caregiver of each child-caregiver dyad by one of the investigators. For children aged 7 years and older, the child's assent was also obtained. Forty-eight child-caregiver dyads were enrolled to the study. The CBQ-SF temperament instrument is validated for children aged 36–95 months, so the study enrollment was limited to this age range. Children with minimal health concerns (American Society of Anesthesiologists Physical Status Classification I or II) who were scheduled to undergo a restorative dental visit requiring administration of local anesthetic and tooth preparation or extraction were eligible for inclusion. To avoid selecting patients with a known history of successful N2O/O2 inhalation sedation, only patients who had never received N2O/O2 at the pediatric dental clinic at the UW were enrolled. Children with non–English-reading caregivers, those with caregivers younger than 18 years, children who had previously been treated with nitrous oxide at the pediatric dental clinic at the UW, and children who had previously enrolled in the study were excluded.
Administration of Temperament-Rating Instrument
During the child's appointment, caregivers completed the CBQ-SF. The CBQ-SF is a 94-item survey in which caregivers rate their child on a 7-point Likert-type scale. The CBQ-SF was developed for use in situations in which the full questionnaire, composed of 195 questions, is not practical. It has been validated and is nearly as reliable as the standard-length CBQ. The CBQ-SF evaluates 15 temperament subscales. A subset of questions within the CBQ-SF comprise the CBQ-Very Short Form (CBQ-VSF). The CBQ-VSF is used to evaluate the overall temperament domains of Effortful Control, Negative Affectivity, and Extraversion/Surgency. Temperament scores were calculated using the methods included with the CBQ-SF and CBQ-VSF instruments.
N2O/O2 and the Dental Procedure
At the beginning of the dental procedure, an appropriately sized double-mask scavenger breathing circuit (Parker Hannifin Corporation, Mayfield Heights, Ohio) was selected and placed, the flow rate was set between 5 and 6 L/min, and 100% oxygen was used for the first 1 to 2 minutes followed by titration of nitrous oxide in 10% intervals up to a maximum total of 50% nitrous oxide and 50% oxygen. Patients had the option of watching Internet-streaming video during the dental procedure. All procedures were performed by pediatric dental residents of the UW. A total of 17 different dentists participated in delivery of patient care. At the end of the appointment, nitrous oxide flow was terminated, and 100% oxygen was delivered for 3 to 5 minutes. Patients were determined to have returned to their pretreatment responsiveness prior to discharge.
Rating Behavior
At the completion of the dental procedure, the treating dentist rated overall behavior displayed during the course of the dental appointment according to the Frankl Behavior Scale. The child's overall Frankl score was defined as his or her lowest Frankl score for any segment of treatment. Scores ranged from definitely negative (Frankl −/−; refusal of treatment, forceful crying, fearfulness, or any other overt evidence of extreme negativism), negative (Frankl −; reluctance to accept treatment, uncooperative, some evidence of negative attitude but not pronounced), positive (Frankl +; acceptance of treatment, cautious behavior at times, willingness to comply with the dentist, at times with reservation, but patient follows the dentist's directions cooperatively), to definitely positive (Frankl +/+; definitely positive, good rapport with the dentist, interest in the dental procedures, laughter and enjoyment). The treating dentists were blinded to the child's CBQ-SF score.
Following completion of dental care, demographic (age, sex, American Society of Anesthesiologist status, insurance type) and treatment complexity (simple = intracoronal restorations or complex = stainless steel crown, pulp therapy, extraction) variables were abstracted from the patient chart, and appointment success or failure was recorded. Success was defined as the ability to complete treatment with a Frankl score of positive or definitely positive.
Statistical Analyses
Study data were collected and managed using REDCap (Research Electronic Data Capture, Vanderbilt University, Nashville, Tenn). Descriptive statistics and analytics were completed using Stata 13 (StataCorp LP, College Station, Tex). Demographic and treatment variables were tested for association with sedation success/failure using Fisher exact test. Temperament scales were assessed for association with sedation success/failure and separately with demographic variables using a Wilcoxon rank sum test.
RESULTS
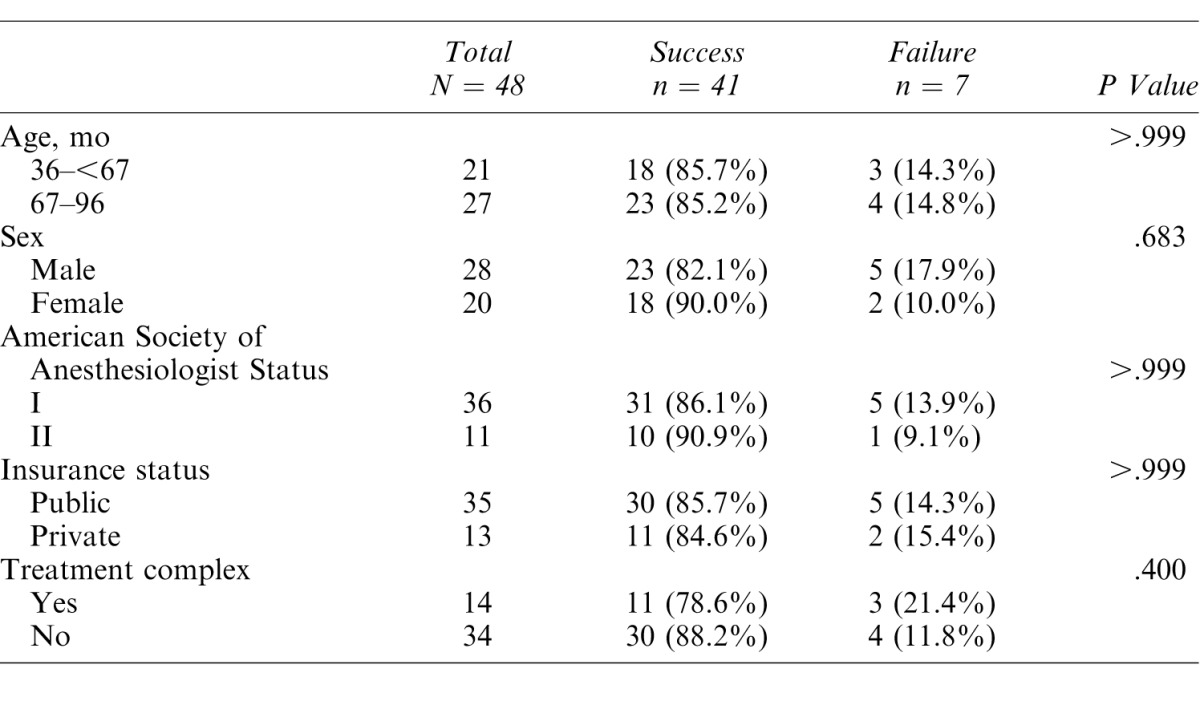
Forty-eight children between the ages of 36 and 95 months were enrolled in the study; 58% were male. Demographic characteristics of study participants are detailed in Table 1. There was no significant association found between demographic variables (age, sex, American Society of Anesthesiologist status, and insurance) or treatment complexity (defined as stainless steel crowns, pulp therapy, and/or extraction) and sedation failure.
Table 1. .
Demographic Variables and Association With Overall Sedation Outcome
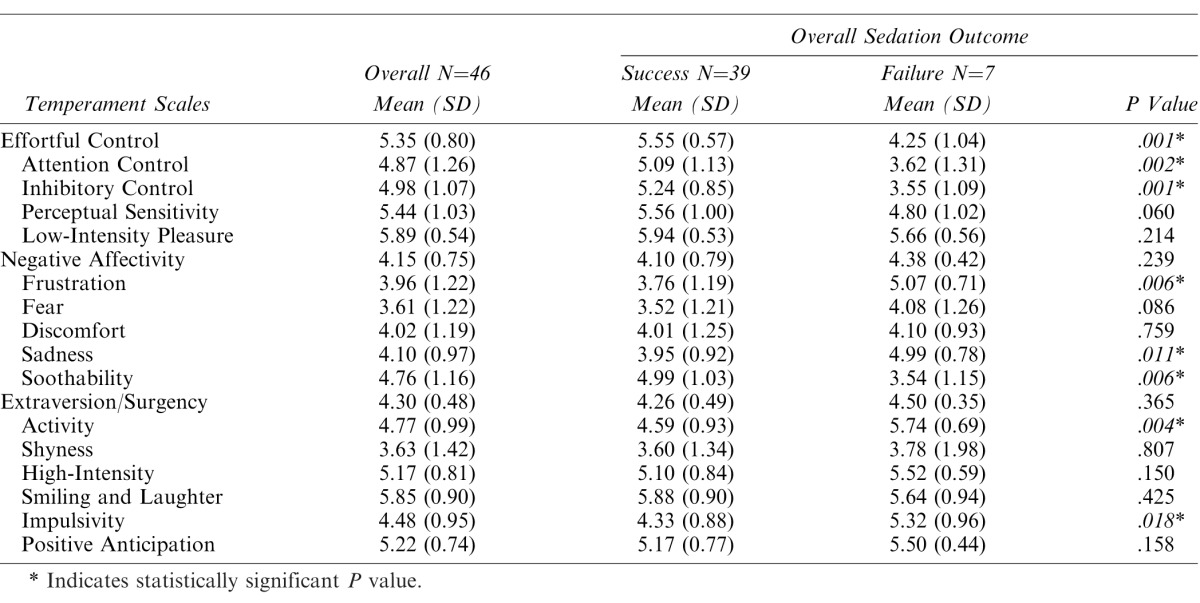
The overall behavioral failure rate was 15.6% (n = 7/48). The domain of Effortful Control (P = .001) and its subscales Attention Control (P = .002) and Inhibitory Control (P = .001) were significantly associated with treatment success. The Negative Affectivity subscales of Frustration (P = .006), Sadness (P = .011), and Soothability (P = .006), and the Extraversion/Surgency subscales Activity (P = .004) and Impulsivity (P = .018) were also significantly associated with overall sedation failure (Table 2).
Table 2. .
Temperament Associations With Overall Sedation Outcome and Frankl Scores
DISCUSSION
The purpose of this study was to determine associations between child temperament and nitrous oxide sedation outcomes. In this study, the overall N2O/O2 success rate was 85.4%. There was no association between variables such as age, sex, and treatment complexity, indicating that we did not detect a difference in treatment success over a relatively wide age range (3–8 years). Likewise, there was no statistically significant behavioral difference in children who received a variety of different dental procedures (eg, composite restoration vs pulpotomy, extraction, etc). Others have reported similar success rates for dental and medical treatment provided with nitrous oxide.1,2,4 With such high rates of success, it can be assumed that there is wide variation in the temperament of children who are able to successfully undergo treatment. Perhaps it is therefore more useful clinically to attempt to identify how children who fail treatment differ from the majority.
In the present study, we used the CBQ-SF to evaluate child temperament. The CBQ-SF is used to evaluate temperament domains of Effortful Control, Negative Affectivity, and Extraversion/Surgency. These categories are further divided into 15 subscales. Our results showed that children who failed restorative treatment had significantly different scores in the overall domain of Effortful Control. Similarly, Lane et al15 identified low Effortful Control as a factor in pediatric dental sedation failure. Others have not clearly identified specific dimensions associated with treatment failure; however, Aminabadi et al16 showed that children with higher overall temperament scores were less likely to complete treatment, and Su et al17 also showed that this type of “difficult temperament” was associated with uncooperative behavior. In this study, we also found that children with treatment failures differed from successful peers in 2 of 5 Negative Affectivity subscales and 2 of 6 Extraversion/Surgency subscales. These findings suggest that a wide variety of individual characteristics affect a child's ability to receive treatment.
In this study, many temperament characteristics were associated with treatment success. These characteristics were generally descriptive of children with a constellation of high Effortful Control, high Soothability, and low Frustration, Activity, and Impulsivity. Such attributes are typical of children considered to have “easy temperament.” An experienced practitioner may be able to identify such children intuitively, but few studies have attempted to quantify the role of temperament in a child's ability to cope with dental treatment. Although analysis of child temperament is a complicated matter, the growing body of clinical temperament research suggests that practitioners should be aware of a constellation of factors that identify a child with difficult temperament. While it is not possible to easily identify difficult temperament using a psychological instrument, a review of selected questions from the CBQ-SF reveals examples of characteristics that might factor in to a child's ability to receive care.
Effortful control:
Sometimes becomes absorbed in a picture book and looks at it for a long time
Can easily stop an activity when she or he is told “no”
Frustration:
Gets angry when told she or he has to go to bed
Sadness:
Cries sadly when a favorite toy gets lost or broken
Soothability:
Is very difficult to soothe when she or he has become upset
Activity Level:
Seems always in a big hurry to get from one place to another
Impulsivity:
Usually rushes into an activity without thinking about it.
The specific factors identified in this study are consistent with previous work on child temperament and dental care. Perhaps the most significant finding relates to the temperament category of Effortful Control. This is consistent with predictive factors that have been identified elsewhere. Over the course of a dental procedure, children who are able to successfully receive care must inhibit negative reactions. This corresponds to the innate ability to focus on a task and persist even though it is difficult. Because effortful control appears to be particularly important in predicting treatment success, future studies should investigate how an assessment of this domain could be practically implemented in clinical scenarios to help guide treatment decisions. By determining which children fail to receive dental care with nitrous oxide sedation, practitioners may reduce negative patient experiences and improve case selection for pharmacologic behavior guidance techniques such as oral sedation and general anesthesia.
Study Limitations
A major limitation of this study was the number of providers involved in patient care. The study was conducted at a university-based pediatric dental clinic where 17 different dental residents performed treatments with nitrous oxide inhalation and rated patient behavior. The number of providers introduced variability from the standpoint of provider experience, skill level, and nitrous oxide administration technique. In addition, children were allowed to self-select streaming video programming, which may have affected the treatment experience and individual behavior. The low number of patients enrolled in this pilot study also limits the interpretation of the results. In future studies, larger sample sizes, a more focused age range, and more detailed behavioral data may enable researchers to draw more definitive conclusions regarding specific dimensions of temperament and child cooperation. Lastly, video recording of each patient encounter would allow more consistent evaluation of treatment response.
In conclusion, child temperament has been demonstrated to be a potentially important determinant of nitrous oxide sedation success in dental treatment. These results show that treatment failure with N2O/O2 was associated with Effortful Control. The subscales of Attention Focusing, Inhibitory Control, Frustration, Fear, Sadness, Soothability, Activity, and Impulsivity were also associated with treatment failure. These factors are descriptive of difficult temperament and should be considered when evaluating pediatric treatment options.
REFERENCES
- 1. Burnweit C, Diana-Zerpa JA, Nahmad MH, et al. Nitrous oxide analgesia for minor pediatric surgical procedures: an effective alternative to conscious sedation? J Pediatr Surg. 2004; 39: 495– 499. [DOI] [PubMed] [Google Scholar]
- 2. Soldani F, Manton S, Stirrups DR, Cumming C, Foley J. . A comparison of inhalation sedation agents in the management of children receiving dental treatment: a randomized, controlled, cross-over pilot trial. Int J Paediatr Dent. 2010; 20: 65– 75. [DOI] [PubMed] [Google Scholar]
- 3. Bryan RA. . The success of inhalation sedation for comprehensive dental care within the Community Dental Service. Int J Paediatr Dent. 2002; 12: 410– 414. [DOI] [PubMed] [Google Scholar]
- 4. Foley J. . A prospective study of the use of nitrous oxide inhalation sedation for dental treatment in anxious children. Eur J Paediatr Dent. 2005; 6: 121– 128. [PubMed] [Google Scholar]
- 5. Locker D, Liddell A, Dempster L, Shapiro D. . Age of onset of dental anxiety. J Dent Res. 1999; 78: 790– 796. [DOI] [PubMed] [Google Scholar]
- 6. Gatchel RJ. . The prevalence of dental fear and avoidance: expanded adult and recent adolescent surveys. J Am Dent Assoc. 1989; 118: 591– 593. [DOI] [PubMed] [Google Scholar]
- 7. Guideline on use of nitrous oxide for pediatric dental patients. Pediatr Dent. 2013; 35: E174– E178. [PubMed] [Google Scholar]
- 8. Quinonez R, Santos RG, Boyar R, Cross H. . Temperament and trait anxiety as predictors of child behavior prior to general anesthesia for dental surgery. Pediatr Dent. 1997; 19: 427– 431. [PubMed] [Google Scholar]
- 9. Radis FG, Wilson S, Griffen AL, Coury DL. . Temperament as a predictor of behavior during initial dental examination in children. Pediatr Dent. 1994; 16: 121– 127. [PubMed] [Google Scholar]
- 10. Isik B, Baygin O, Kapci EG, Bodur H. . The effects of temperament and behaviour problems on sedation failure in anxious children after midazolam premedication. Eur J Anaesthesiol. 2010; 27: 336– 340. [DOI] [PubMed] [Google Scholar]
- 11. Lochary ME, Wilson S, Griffen AL, Coury DL. . Temperament as a predictor of behavior for conscious sedation in dentistry. Pediatr Dent. 1993; 15: 348– 352. [PubMed] [Google Scholar]
- 12. Jensen B, Stjernqvist K. . Temperament and acceptance of dental treatment under sedation in preschool children. Acta Odontol Scand. 2002; 60: 231– 236. [DOI] [PubMed] [Google Scholar]
- 13. Rothbart MK, Ahadi SA, Evans DE. . Temperament and personality: origins and outcomes. J Pers Soc Psychol. 2000; 78: 122– 135. [DOI] [PubMed] [Google Scholar]
- 14. Valeri BO, Holsti L, Linhares MB. . Neonatal pain and developmental outcomes in children born preterm: a systematic review. Clin J Pain. 2015; 31: 355– 362. [DOI] [PubMed] [Google Scholar]
- 15. Lane KJ, Nelson TM, Thikkurissy S, Scott JM. . Assessing temperament as a predictor of oral sedation success using the Children's Behavior Questionnaire Short Form. Pediatr Dent. 2015; 37: 429– 435. [PubMed] [Google Scholar]
- 16. Aminabadi NA, Puralibaba F, Erfanparast L, Najafpour E, Jamali Z, Adhami SE. . Impact of temperament on child behavior in the dental setting. J Dent Res Dent Clin Dent Prospects. 2011; 5: 119– 122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Su JM, Ye XW, Ruan WH, Wu ZF, Huang XJ. . The characteristics of uncooperative children's temperament during dental treatment [in Chinese]. Shanghai Kou Qiang Yi Xue. 2006; 15: 279– 281. [PubMed] [Google Scholar]


