Abstract
Objectives:
To assess the best temporal association between the application of a fluoride varnish on enamel and bonding procedures.
Materials and Methods:
Eighty mandibular bovine incisors were used. Teeth were divided into 4 groups (20 per group); Groups 1–3 were treated with fluoride varnish (Fluor Protector, Ivoclar Vivadent, Schaan, Liechtenstein), and Group 4 served as control with no pretreatment. Tooth were stored in deionized water (37°C) and subjected to thermal cycling for 400 (Group 1), 800 (Group 2), and 2500 (Group 3) cycles corresponding, respectively, to 15, 30, and 90 days in order to simulate the three different timing of bracket bonding. Shear bond strength (SBS) was measured using an Instron Universal Testing machine. Tooth surfaces were examined under a stereomicroscope at 10× magnification to assess the amount of adhesive remnant index (ARI). One-way analysis of variance (ANOVA) and Tukey's honestly significant difference post-hoc test were used for the comparison of SBS values between groups (P < 0.05). The Chi-square test was used to examine differences among ARI scores. (P < 0.05).
Results:
One-way ANOVA and Tukey post-hoc test showed that the SBS of different groups were significantly different and was impacted by different timing of bonding (P < 0.05). The main differences were between the control group (17.02 ± 6.38 MPa) and Group 1 (6.93 ± 4.3 MPa). The ARI scores showed that there were no significant differences between the four tested groups.
Conclusions:
The SBS of the brackets bonded 15 days after the application of the fluoride was set back to an optimal value.
Key words: Fluoride varnish, orthodontic brackets, shear bond strength, topical fluoride
BACKGROUND
An essential requirement of any orthodontic therapy is the maintenance of a meticulous oral hygiene so as to effectively control the growing of bacterial plaque over tooth surfaces. The fixed orthodontic appliances may lead to an increase in the levels of plaque and alteration of its quality.[1]
Early tooth decay around the brackets can cause white or brown marks [demineralized white lesions (DWLs)] to appear on teeth during fixed orthodontic treatment. Build-up of dental plaque around these brackets is associated with an increased risk of rapid demineralization of the teeth enamel.[2] A recent study found that the prevalence of DWLs might be 74% in patients who have undergone a fixed orthodontic treatment.[3] In another study, it has been seen that, even five years after treatment, orthodontic patients had a significantly higher incidence of DWLs than a control group of participants who did not undergo orthodontic treatment.[4]
Therefore, in clinical practice, various therapies have been involved to reduce any kind of enamel lesions as much as possible. One of the most known and used is the application of topical fluorinated substances in different stages of orthodontic treatment.[5,6,7,8] Sodium fluoride gels or varnishes at different concentrations can be used safely and effectively to treat demineralization of dental structures as well as to prevent caries.[5,6,7,8,9,10,11,12]
Because of the aqueous oral cavity, the fluoride ions have the ability to precipitate inside the enamel prisms in place of calcium and phosphate, transforming the hydroxyapatite in fluorhydroxyapatite, a more resistant phase to acid attack, promoting the re-mineralization of the tooth surface, and inhibiting the action of the bacterial enzymes that produce the acid.[9,10,11,12]
However, tooth pretreatments with such agents act on the enamel interfering with the bond strength of the brackets. Different studies have already been conducted concerning the use of fluoride and its possible action on the shear bond strength of the brackets.[13,14,15,16,17,18]
The purpose of this study, therefore, is to understand, starting from the analysis of the detachment forces from the enamel surface, the best temporal association between the application of a fluoride varnish on enamel and bonding procedures in order to avoid any negative influence of the fluoride treatment on the bond strength of the brackets.
MATERIALS AND METHODS
Eighty freshly extracted mandibular bovine incisors, obtained from the same farm in order to have the same level of fluoride concerning their feeding, were used. Teeth were cleaned of debris and then polished with nonfluoridate pumice and rubber prophylactic cups at low speed for 15 s. Tooth selection criteria included integrity of the buccal and lingual enamel surfaces under visible light at 4× magnification, absence of traumatic injuries, cavities, enamel erosions, and smooth and flat buccal surface suitable for bonding. They were then stored in distilled water for no more than 2 weeks (ISO/TR 11405).
Teeth were randomly divided into 4 groups (20 teeth each) by using a random numbers table. Three groups (Groups 1–3) were treated with fluoride varnish (Fluor Protector, Ivoclar Vivadent, Schaan, Liechtenstein) according to manufacturer's instructions, and one (Group 4) served as control with no pretreatment.
All the teeth were stored in deionized water (37°C) and subjected to thermal cycling for 400 (Group 1), 800 (Group 2), and 2500 (Group 3) cycles corresponding, respectively, to 15, 30, and 90 days in order to simulate the three different timing of bracket bonding after the application of the fluoride varnish.
Brackets (Edgewise Standard, 4.4 mm × 3.2 mm, Leone S.p.A., Florence, Italy) were all bonded using the same standard technique; enamel surfaces were treated with 37% phosphoric acid (Etching gel 3M, Unitek, Monrovia, CA) for 60 s, rinsed with a water spray for 20 s, and air dried. All brackets were bonded with transbond XT (3M Unitek, Monrovia, CA) and light-cured with the same LED lamp (Bluephase Polywave, Ivoclar Vivadent, Schaan, Liechtenstein) for 40 s. Excessive sealant and adhesive were removed from the periphery of the bracket base to keep each bonding area uniform. The exposure was performed from both the mesial and distal sides for 20 s.
For shear bond strength (SBS) tests, each tooth was mounted on self-cured acrylic resin blocks with a mounting jig used to align its buccal surface so that it was perpendicular to the bottom of the mold. Specimens were then mounted in the jig and the SBS was measured with an Instron Universal Testing machine (Model 3343, Instron Corp., Canton, MA). Continuous shear force was applied at a crosshead speed of 1 mm per minute until bracket failure. All the brackets were bonded by a single operator.
The force required to detach the bracket was recorded in Newtons (N) and converted to megapascals (MPa) using the following formula: Bond strength (MPa) = debonding force (N)/[w × l] (mm2), where w = width of the bracket base, l = height of the bracket base and, 1 MPa = 1 N/mm2. After the detachment, each tooth surface was examined under a stereomicroscope at 10 × magnification to assess the amount of adhesive remnant using adhesive remnant index (ARI).[19]
The ARI index was ranked from 0 to 3 as follows: 0 = no adhesive on the enamel; 1 = less than 50% adhesive on the enamel; 2 = more than 50% adhesive on the enamel; 3 = 100% adhesive on the enamel.
Statistical Analysis
Description and inferential statistical analyses were performed using MedCalc statistical software (MedCalc Software, Ostend, Belgium).[20]
Normal distribution of the data was verified with the Kolmogorov–Smirnov test. The data were found to be normally distributed, and there was homogeneity of variance among the groups. Thus, the statistical evaluation was performed using parametric tests. One-way analysis of variance (ANOVA) and Tukey's honestly significant difference post-hoc test were used for the comparison of SBS values between groups (P < 0.05). The Chi-square test was used to examine whether there were differences among the groups in the ARI scores. P value was considered statistically significant if P < 0.05.
RESULTS
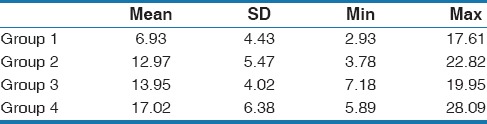
Descriptive statistics, including the mean, standard deviation (SD), and minimum and maximum values of the SBS for each of the four groups are presented in Table 1. One-way ANOVA and Tukey post-hoc test showed that the SBS of different groups were significantly different and was impacted by the different timing of bonding (P < 0.05). The main differences were between the control group (17.02 ± 6.38 MPa) and the Group 1 (6.93 ± 4.3 MPa).
Table 1.
Mean, standard deviation (SD), and minimum and maximum values of the shear bond strength for each of the four groups
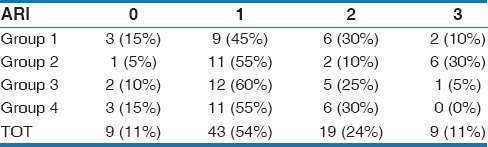
There were no statistical differences between the Group 2 and Group 3. The residual adhesive on the enamel surfaces, as indicated by the ARI scores, are presented in Table 2. The results of the Chi-square comparisons showed that there were no significant differences between the four groups tested. All groups showed a higher percentage of ARI scores of 0 and 1, which indicated that debonding distribution failures were mainly at the adhesive–enamel interface.
Table 2.
The residual adhesive index (ARI) scores
DISCUSSION
Orthodontic patients are often at high risk of developing dental lesions during orthodontic treatment, especially when their compliance to oral hygiene instructions is poor. Enamel demineralization is an undesirable but common complication of orthodontic fixed appliance therapy. Controlling dental plaque before and during fixed orthodontic treatment, without compromising the SBS of brackets, has always been an area of research in orthodontics.
People often wear braces for more than 1 year, and there is a risk that tooth decay will damage the teeth, requiring restorations and fillings. Fluoride is effective in reducing tooth decay in such patients. Individuals receiving orthodontic treatment may be prescribed various forms of fluoride treatment. Topically applied sodium fluoride solution causes remineralization, mainly by reducing apatite dissolution by forming less soluble fluorapatite. The effects of fluoride on the prevention of tooth decay and re-mineralization of decalcified enamel have been elaborately described.[21,22,23,24]
However, in previous studies, the effect of fluoride application on SBS has been reported with different and controversial results. In general, fluoride pretreatment induces lower SBS values resulting in reduced bond strength of the brackets; topical application of fluoride interferes with the etching effect of phosphoric acid on enamel surfaces, resulting in reduced bond strength of orthodontic brackets.[13,14,15,25,26,27,28]
In order to simulate the aging of the tooth after the fluoride treatment, we used the thermocycling technique that is widely used as an artificial aging methodology.[29] A literature review concluded that 10000 cycles corresponds approximately to 1 year of in-vivo functioning.[30] In the current study, 400, 800, and 2500 cycles were used in order to simulate the aging period of 15, 30, and 90 days, respectively.
In our results, the SBS of orthodontic bracket was significantly and highly decreased by the application of the fluoride varnish. The minimal value recommended as adequate for orthodontic purposes is 6 MPa.[31,32] Group 1 showed the lowest values with a mean SBS of 6.93 MPa that could be considered a satisfactory result even if it is really close to the minimum value. However, in this group, many measurements were lower than 6 MPa with the lowest value of 2.93 MPa, which is really an undesirable clinical situation due to the high possibility of detachment of the bracket.
However, fluorides are one of the most favored remineralizing agent and their positive role in prophylaxis treatments should not be limited due to the possible negative effect on the SBS.
That is why we tested the hypothesis of bonding brackets in a delayed time expecting that the negative effect on the SBS could be reduced after 15 or 30 days.
The results of the test groups, after 30 and 90 days of aging, showed higher values of SBS, with a mean over 12 MPa that could be considered a “safety” condition confirming the hypothesis of the study. The ARI results indicated that more than 85% samples were included between scores 0 and 1. The most desired clinical condition is a low ARI score with less composite remaining on the tooth surface in order to reduce enamel damage during debonding procedures. The worst score to be considered is an ARI of 3; in our tests, the samples included in this score were mainly from the groups 1 and 2. None of the control group 4 were included in the ARI 3. However, considering our results, we can confirm that all the test groups showed a good ARI index, between score 0 and 1, suggesting that the bond between bracket and resin was stronger than that between the resin and enamel.
The use of bovine tooth is considered a limitation of this study, owing to the difficulties in obtaining human teeth. However, bovine enamel has already been used in several other studies as a substitute model without statistically significant differences in SBS comparing bovine and human enamel.[33,34,35]
It is acknowledged that the in vitro bond strength testing is not truly representative of the highly demanding intraoral conditions and at best gives only an indication of the possible clinical performance of the material tested. In spite of these limitations, the results can still assist in suggesting the ideal timing of bonding procedure after the use of fluoride varnishes.
Difference in the application time, variation in the fluoride concentrations used, the properties of the bonding agents, and/or bracket retention mechanism should always be considered when comparing such results.
CONCLUSION
Based on the results of the present study, the following conclusions can be drawn:
The use of fluoride varnish significantly lowered the SBS values
The SBS values of bracket bonded after 15 days from the varnish application were just over the minimum value recommended (6 MPa)
The results after 30 days returned to an optimal value
The indication is to wait more than 15 days after the application of the fluoride varnish in order to obtain an optimal bond strength of the bracket to the enamel.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Naranjo AA, Triviño ML, Jaramillo A, Betancourth M, Botero JE. Changes in the subgingival microbiota and periodontal parameters before and 3 months after bracket placement. Am J Orthod Dentofacial Orthop. 2006;30:275. doi: 10.1016/j.ajodo.2005.10.022. [DOI] [PubMed] [Google Scholar]
- 2.Maxfield BJ, Hamdan AM, Tufekci E, Shroff B, Best AM, Lindauer SJ. Development of white spot lesions during orthodontic treatment: Perceptions of patients, parents, orthodontists, and general dentists. Am J Orthod Dentofacial Orthop. 2012;141:337–44. doi: 10.1016/j.ajodo.2011.08.024. [DOI] [PubMed] [Google Scholar]
- 3.Enaia M, Bock N, Ruf S. White-spot lesions during multibracket appliance treatment: A challenge for clinical excellence. Am J Orthod Dentofacial Orthop. 2011;140:e17–24. doi: 10.1016/j.ajodo.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 4.Ogaard B. Prevalence of white spot lesions in 19-year-olds: A study on untreated and orthodontically treated persons 5 years after treatment. Am J Orthod Dentofacial Orthop. 1989;96:423–7. doi: 10.1016/0889-5406(89)90327-2. [DOI] [PubMed] [Google Scholar]
- 5.Geiger AM, Gorelick L, Gwinnett AJ, Benson BJ. Reducing white spot lesions in orthodontic populations with fluoride rinsing. Am J Orthod Dentofacial Orthop. 1992;101:403–7. doi: 10.1016/0889-5406(92)70112-N. [DOI] [PubMed] [Google Scholar]
- 6.Marinho VC, Higgins JP, Logan S, Sheiham A. Topical fluoride (toothpastes, mouthrinses, gels or varnishes) for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2003;4:CD002782. doi: 10.1002/14651858.CD002782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marinho VC, Higgins JP, Sheiham A, Logan S. Combinations of topical fluoride (toothpastes, mouthrinses, gels, varnishes) versus single topical fluoride for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2009 doi: 10.1002/14651858.CD002781.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marinho VC, Worthington HV, Walsh T, Clarkson JE. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2013;7:CD002279. doi: 10.1002/14651858.CD002279.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lynch RJ, Mony U, Ten Cate JM. The effect of fluoride at plaque fluid concentrations on enamel de- and remineralisation at low pH. Caries Res. 2006;40:522–9. doi: 10.1159/000095652. [DOI] [PubMed] [Google Scholar]
- 10.ten Cate JM. Contemporary perspective on the use of fluoride products in caries prevention. Br Dent J. 2013;214:161–7. doi: 10.1038/sj.bdj.2013.162. [DOI] [PubMed] [Google Scholar]
- 11.Stecksén-Blicks C, Renfors G, Oscarson ND, Bergstrand F, Twetman S. Caries-preventive effectiveness of a fluoride varnish: A randomized controlled trial in adolescents with fixed orthodontic appliances. Caries Res. 2007;41:455–9. doi: 10.1159/000107932. [DOI] [PubMed] [Google Scholar]
- 12.Benson PE, Parkin N, Dyer F, Millett DT, Furness S, Germain P. Fluorides for the prevention of early tooth decay (demineralised white lesions) during fixed brace treatment. Cochrane Database Syst Rev. 2013;12:CD003809. doi: 10.1002/14651858.CD003809.pub3. [DOI] [PubMed] [Google Scholar]
- 13.Garcia-Godoy F, Hubbard GW, Storey AT. Effect of fluoridated etching gel on enamel morphology and shear bond strength of orthodontic brackets. Am J Orthod Dentofacial Orthop. 1991;100:163–70. doi: 10.1016/S0889-5406(05)81523-9. [DOI] [PubMed] [Google Scholar]
- 14.Attin R, Stawarczyk B, Keçik D, Knösel M, Wiechmann D, Attin T. Shear bond strength of brackets to demineralize enamel after different pretreatment methods. Angle Orthod. 2012;82:56–61. doi: 10.2319/012311-48.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Al-Kawari HM, Al-Jobair AM. Effect of different preventive agents on bracket shear bond strength: In vitro study. BMC Oral Health. 2014;14:28. doi: 10.1186/1472-6831-14-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elsaka SE, Hammad SM, Ibrahim NF. Evaluation of stresses developed in different bracket-cement-enamel systems using finite element analysis with in vitro bond strength tests. Prog Orthod. 2014;15:33. doi: 10.1186/s40510-014-0033-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moosavi H, Ahrari F, Mohamadipour H. The effect of different surface treatments of demineralised enamel on microleakage under metal orthodontic brackets. Prog Orthod. 2013;14:2. doi: 10.1186/2196-1042-14-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ladhe KA, Sastri MR, Madaan JB, Vakil KK. Effect of remineralizing agents on bond strength of orthodontic brackets: An in vitro study. Prog Orthod. 2014;15:28. doi: 10.1186/s40510-014-0028-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Artun J, Bergland S. Clinical trials with crystal growth conditioning as an alternative to acid etch enamel pretreatment. Am J Orthod. 1984;85:333–40. doi: 10.1016/0002-9416(84)90190-8. [DOI] [PubMed] [Google Scholar]
- 20.Stephan C, Wesseling S, Schink T, Jung K. Comparison of eight computer programs for receiver-operatic characteristic analysis. Clin Chem. 2003;49:433–9. doi: 10.1373/49.3.433. [DOI] [PubMed] [Google Scholar]
- 21.Cardoso Cde A, Lacerda B, Mangueira DF, Charone S, Olympio KP, Magalhães AC, et al. Mechanisms of action of fluoridated acidic liquid dentifrices against dental caries. Arch Oral Biol. 2015;60:23–8. doi: 10.1016/j.archoralbio.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 22.Songsiripradubboon S, Hamba H, Trairatvorakul C, Tagami J. Sodium fluoride mouthrinse used twice daily increased incipient caries lesion remineralization in an in situ model. J Dent. 2014;42:271–8. doi: 10.1016/j.jdent.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 23.Marinho VC, Worthington HV, Walsh T, Chong LY. Fluoride gels for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2015;6:CD002280. doi: 10.1002/14651858.CD002280.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wright JT, Hanson N, Ristic H, Whall CW, Estrich CG, Zentz RR. Fluoride toothpaste efficacy and safety in children younger than 6 years: A systematic review. J Am Dent Assoc. 2014;145:182–9. doi: 10.14219/jada.2013.37. [DOI] [PubMed] [Google Scholar]
- 25.Cossellu G, Lanteri V, Butera A, Sarcina M, Farronato G. Effects of six different preventive treatments on the shear bond strength of orthodontic brackets: In vitro study Acta Biomater Odontol Scand. 2015;1:13–7. doi: 10.3109/23337931.2015.1021351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meng CL, Li CH, Wang WN. Bond strength with APF applied after acid etching. Am J Orthod Dentofacial Orthop. 1998;114:5103. doi: 10.1016/s0889-5406(98)70170-2. [DOI] [PubMed] [Google Scholar]
- 27.Cacciafesta V, Sfondrini MF, Calvi D. Scribante A Effect of fluoride application on shear bond strength of brackets bonded with a resin-modified glass-ionomer. Am J Orthod Dentofacial Orthop. 2005;127:580–3. doi: 10.1016/j.ajodo.2004.02.017. [DOI] [PubMed] [Google Scholar]
- 28.Montasser MA, Taha M. Effect of enamel protective agents on shear bond strength of orthodontic brackets. Prog Orthod. 2014;15:34. doi: 10.1186/s40510-014-0034-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.De Munck J, Van Landuyt K, Coutinho E, Poitevin A, Peumans M, Lambrechts P, et al. Micro-tensile bond strength of adhesives bonded to Class-I cavity-bottom dentin after thermo-cycling. Dent Mater. 2005;21:999–1007. doi: 10.1016/j.dental.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 30.Gale MS, Darvell BW. Thermal cycling procedures for laboratory testing of dental restorations. J Dent. 1999;27:89–99. doi: 10.1016/s0300-5712(98)00037-2. [DOI] [PubMed] [Google Scholar]
- 31.Reynolds IR. A review of direct orthodontic bonding. Br J Orthod. 1975;2:171–8. [Google Scholar]
- 32.Whitlock BOIII, Eick JD, Ackerman RJ, Jr, Glaros AG, Chappell RP. Shear strength of ceramic brackets bonded to porcelain. Am J Orthod Dentofacial Orthop. 1994;106:358–64. doi: 10.1016/S0889-5406(94)70056-7. [DOI] [PubMed] [Google Scholar]
- 33.Nakamichi I, Iwaku M, Fusayama T. Bovine teeth as possible substitutes in the adhesion test. J Dent Res. 1983;62:1076–81. doi: 10.1177/00220345830620101501. [DOI] [PubMed] [Google Scholar]
- 34.Oesterle LJ, Shellhart WC, Belanger GK. The use of bovine enamel in bonding studies. Am J Orthod Dentofacial Orthop. 1998;11:515–9. doi: 10.1016/s0889-5406(98)70171-4. [DOI] [PubMed] [Google Scholar]
- 35.Krifka S, Börzsönyi A, Koch A, Hiller KA, Schmalz G, Friedl KH. Bond strength of adhesive systems to dentin and enamel – Human vs. bovine primary teeth in vitro. Dent Mater. 2008;24:888–94. doi: 10.1016/j.dental.2007.11.003. [DOI] [PubMed] [Google Scholar]


