Abstract
Aims and Objectives:
Evaluation of neonatal hypernatremia and hypernatremic dehydration in neonates receiving exclusive breastfeeding.
Introduction:
Neonatal hypernatremia is a serious condition in the newborn period. We present infants with hypernatremic dehydration due to breast milk (BM) hypernatremia. Hypernatremic dehydration in breast-fed newborns is usually secondary to insufficient lactation. We present the neonatal hypernatremia and hypernatremic dehydration encountered between January and December, 2012, its causes and treatment.
Methodology:
This was a retrospective study. We analyzed records of babies admitted to the Neonatal Intensive Care Unit who were investigated and found to have hypernatremia and whose mother's BM sodium (BM Na) was done.
Inclusion Criteria:
(1) Babies with serum Na >145 meq/l, (2) euglycemia, (3) normocalcemic, (4) no clinical and lab evidence of sepsis, (5) exclusive breast feeds.
Exclusion Criteria:
Neonates not satisfying any mentioned criterion.
Results:
BM Na correlated strongly with neonatal hypernatremia in exclusively breast-fed babies who did not otherwise have any risk factor.
Conclusion:
Elevated BM Na is an important etiological factor in neonatal hypernatremia.
Keywords: Breast milk sodium, exclusive breastfeeding, neonatal hypernatremia
Introduction
Neonatal hypernatremia is a potentially lethal condition and is associated with cerebral edema, intracranial hemorrhage, hydrocephalus, and gangrene.[1] Hypernatremia was previously thought to be unusual in breast-fed babies. Nevertheless, from 1979 to 1989, there were sporadic reports of hypernatremia dehydration occurring in breast-fed babies.[2,3,4,5,6] Since 1990s, there has been an increase in the number of breastfed infants reported to have hypernatremia and hypernatremic dehydration. The condition carries an acute morbidity and mortality.
Normal neonatal feeding is advocated on demand every 2 h, with a minimum intake of 30 ml of breast milk (BM)/feed. Adequate BM intake depends on several interrelated stages such as normal mammary development (mammogenesis), unimpeded initiation of lactation (lactogenesis), sustained ongoing milk synthesis (galactopoiesis), and effective milk removal. Milk removal depends on effective maternal and infant breastfeeding techniques, combined with an intact milk-ejection reflex, and total daily milk intake depends on the frequency and duration of feeds.[7] It is normal over the 1st week of life for the neonate to lose as much as 7% of its birth weight through normal diuresis. Neonates should start to gain weight thereafter and regain their birth weight by the 10th day of life. Rapid weight loss or weight loss >7% of birth weight is a cause for concern. The first signs of neonatal dehydration include the failure to have bowel movements or the presence of urate crystals, combined with weight loss.[8]
Methodology
We analyzed records of babies admitted to the Neonatal Intensive Care Unit (NICU) who were investigated and found to have hypernatremia. BM sodium (BM Na) of mothers of such infants was also done when neonatal hypernatremia was detected. Eight such cases are reported here. The symptoms and signs of hypernatremia in neonates that we encountered were lethargy, irritability reduce urinary frequency, weight loss, fever, doughy skin. These neonates were referred from the postnatal care wards to the NICU for lethargy and poor feeding. Their births were uneventful and were placed with the mothers for routine care postdelivery. They were thoroughly evaluated for sepsis, hypoglycemia, hypocalcemia, and serum electrolytes. These babies were on exclusive breastfeeding. Babies were euglycemic, normocalcemic, and with septic screen negative but increased serum Na were included in this study. BM Na of the mother's milk was also done. Mothers whose BM Na was not done at the time of neonatal hypernatremia were excluded.
Normal levels of breast milk sodium
In 1949, Macy established mean (standard deviation [SD]) Na content of colostrums in first 5 days is 22 mmol/l and transitional milk from day 5 to day 10 is 13 mmol/l and of mature milk after 15 days is 7 mmol/l.[7,9] Furthermore, after the first few days of lactations, the BM Na does not seem to show a significant diurnal change and does not appear to differ between either breast.[9] The results showed that on the 3rd day postpartum, BM Na+ concentration was 23.05 (SD 1.10) mmol/l, mean direct BM intake (DBMI) was 202 (SD 68.9) g/day, and mean Na+ intake was 4.36 (SD 0.22) mmol/day and 1.36 (SD 0.07) mmol/kg/day. BM Na+ concentration was inversely related to infant DBMI, and Na+ intake was directly related to infant DBMI and not to BM Na+ concentration. These levels were taken for the present study.
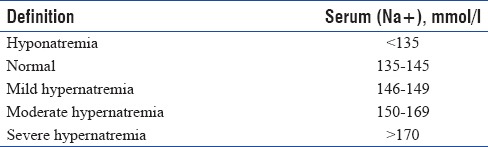
For definition of hypernatremia, Table 1 is to be referred.
Table 1.
Hypernatremia may be associated with:
Decreased fluid intake
Excessive fluid loss or excessive Na intake.
Results
The results are depicted in Table 2. BM Na correlated strongly with neonatal hypernatremia in exclusive breast-fed babies who did not otherwise have any risk factor.
Table 2.
Characteristics of cases of hypernatremia in breast-fed neonates admitted in the Neonatal Intensive Care Unit

Management
Babies who were active and accepting feeds were continued on oral feeds and monitored. Those who were lethargic or showed signs of severe dehydration were managed according to the algorithm in Figure 1.
Discussion
Hypernatremia due to high BM Na is an established entity.[11] This has been attributed to dehydration and malnutrition due to low BM production although high BM Na may also play a role.[3,5]
BM of mothers of neonates with increased serum Na who were exclusively breast-fed and no risk factor for hypernatremia indicates that BM was the source of Na load.
Hypernatremic dehydration has always been a problem in breast-fed infants and has had inadequate exposure in medical literature for several reasons. First, when dealing with sick neonate galactopoiesis failure can occur due to infrequent breast stimulation and drainage. This is related to inadequate prolactin surges and a buildup of local inhibitory factors in the milk. Ineffective milk removal was primarily associated with poor breastfeeding techniques (i.e., incorrect position and latch). There can be compounding factors, including maternal and infant anatomical abnormalities that interfere with suckling dynamics.
Some researchers have found that babies were at risk of breastfeeding failure from the beginning because of the following factors: Low birth weight, early breastfeeding difficulties.[1,12]
In our study, four of the eight infants showed signs of severe dehydration, which was successfully treated as per protocol, is shown in Table 3. Four babies did not show any sign of dehydration but were having hypernatremia biochemically. None had convulsion at the time of presentation. In none of the babies was BM with-held. They were monitored while breastfeeding was continued. The level of Na in the serum of babies as well as in the BM returned to normal. Serum Na was elevated in otherwise healthy newborns, and BM Na was significantly and persistently elevated in all four cases. Elevated BM Na thus appears to be the etiological factor in these cases.
Recent studies have identified breastfeeding malnutrition as a key factor in its pathophysiology but have failed to classify the causes of insufficient milk intake.[1,8,12]
Studies show that there were progressive changes in the Na content of BM in the postpartum period when they compared two group of mothers; preterm and term. Although there may be differences in various components of BM at the beginning and end of feed, the result showed this is not the case with respect to Na content of BM in the absence of unusual dietary habits or systemic or local disease processes affecting the breast. Na content of BM at birth is very high and declines rapidly over the subsequent days.
Macy (1949) has studied the breast milk Na values on various days.[9] In 1998, Kaplan's paper outlined the course of two infants who died.[1] The first newborn died on day 12 of life after presenting on day 9 with seizures and massive intraventricular, periventricular, and cortical hemorrhages on CT scan with plasma Na concentration of 180 mmol/l. While hypernatremia itself can cause seizure, seizures can itself occur during treatment, especially during fluid resuscitation. Hence, hypernatremic dehydration should be rehydrated slowly. Rapid correction of increased serum Na concentration predisposes to osmotic changes in the brain which can exacerbate the existing cerebral edema. Hence, oral rehydration with expressed BM or direct breastfeed or a fluid rehydration at a rate of 100 ml/kg/day can be done. There are very few protocols for intravenous rehydration. In our hospital, none of the babies had seizures either before or during the treatment.
Another study from Italy reported that during the 1st day of life, 7.7% of exclusively breast-fed healthy, term, newborn infants present a weight loss exceeding 10%, and in 35% of these, hypernatremia was detected mean for BM Na+ concentrations in their study was 23.05, standard deviation was 1.10, and 95% confidence interval was 20.87 and 25.24. They reported an inverse relation between BM Na+ concentration and infants DBMI. Their study concluded that a high concentration of BM Na+ may be predictive of impending lactation failure, but it is not an indication to interrupt breastfeeding.
Conclusion
Neonatal hypernatremia is not as rare as is commonly believed. Feeding difficulties in the babies can give rise to inadequate BM secretion. Monitoring the mother and baby in the 1st week of life for successful establishment of breastfeeding is essential. In an otherwise healthy baby, poor feeding and weight loss could be a reason to suspect hypernatremia. Neonatal hypernatremia due to BM hypernatremia is now an established entity, and BM Na should be looked for in every neonate with hypernatremia. There is no reason to stop breastfeeding even if the BM Na is high as it decreases as time progresses. Breastfeed still remains crucially beneficial to baby and should be strongly advocated.
The correction was calculated with preillness weight [Tables 3 and 4].[11]
Table 3.
Formula for correction of Hypernatremia
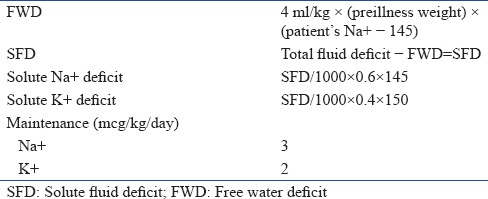
Table 4.
Fluid schedule for Hypernatremic dehydration
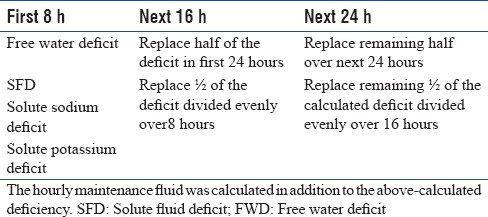
The hourly maintenance fluid was calculated in addition to the above-calculated deficiency.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kaplan JA, Siegler RW, Schmunk GA. Fatal hypernatremic dehydration in exclusively breast-fed newborn infants due to maternal lactation failure. Am J Forensic Med Pathol. 1998;19:19–22. doi: 10.1097/00000433-199803000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Clarke TA, Markarian M, Griswold W, Mendoza S. Hypernatremic dehydration resulting from inadequate breast-feeding. Pediatrics. 1979;63:931–2. [PubMed] [Google Scholar]
- 3.Rowland TW, Zori RT, Lafleur WR, Reiter EO. Malnutrition and hypernatremic dehydration in breast-fed infants. JAMA. 1982;247:1016–7. [PubMed] [Google Scholar]
- 4.Hauser GJ, Kulick AF. Electrolytes disorders in Pediatric Intensive Care Unit. In: Wheeler DS, editor. Pediatric Critical Care Medicine. 1st ed. USA: Springer; 2007. pp. 1161–3. [Google Scholar]
- 5.Roddey OF, Jr, Martin ES, Swetenburg RL. Critical weight loss and malnutrition in breast-fed infants. Am J Dis Child. 1981;135:597–9. doi: 10.1001/archpedi.1981.02130310003002. [DOI] [PubMed] [Google Scholar]
- 6.Marino R, Gourji S, Rosenfeld W. Neonatal metabolic casebook. Hypernatremia and breast feeding. J Perinatol. 1989;9:451–3. [PubMed] [Google Scholar]
- 7.Koo WW, Gupta JM. Breast milk sodium. Arch Dis Child. 1982;57:500–2. doi: 10.1136/adc.57.7.500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Livingstone VH. Problem-solving formula for failure to thrive in breast-fed infants. Can Fam Physician. 1990;36:1541–5. [PMC free article] [PubMed] [Google Scholar]
- 9.Laing IA. Hypernatremic dehydration in newborn infants. Acta Pharmacol Sin. 2002;23(Supplement):48–51. [Google Scholar]
- 10.Greenbaum LA. Electrolytes and acid base disorders. In: Kliegman RM, editor. Nelson Textbook of Pediatrics. 19th ed. Philadelphia: Elsevier; 2011. pp. 212–3. 248. [Google Scholar]
- 11.Choukair MK. Fluids and electrolytes. In: Siberry GK, editor. The Harriet Lane Handbook. 15th ed. London: Mosby Publishers; 2000. pp. 232–3. [Google Scholar]
- 12.Chilton LA. Prevention and management of hypernatremic dehydration in breast-fed infants. West J Med. 1995;163:74–6. [PMC free article] [PubMed] [Google Scholar]


