Abstract
Background:
Although majority of neurotrauma patients require long term ventilatory support but the timing of tracheostomy in such patients is controversial.
Method:
This retrospective study was conducted at a Tertiary Care Hospital, Pune, India. Patients >18 years of age, who underwent percutaneous tracheostomy (PCT) from June 2010 to November 2014 at neurotrauma unit (NTU) of hospital, were included. Patients were divided in two groups according to the timing of tracheostomy, early tracheostomy (ET) group (≤5 days; N=100) and late tracheostomy (LT) group (>5 days; N=64). The nonparametric Mann-Whitney test, and Chi-square tests were used to compare these groups.
Result:
There were no significant differences between the groups in terms of age, sex, APACHE II and GCS Score. Patients in the ET group had a significantly shorter stay in the NTU compared to patients in the LT group (mean, 18 vs. 21.2 days, p=0.005), fewer mechanical ventilation days (mean, 8.1 vs. 11.7 days, P=0.000) and shorter length of stay in hospital (mean, 28.8 vs. 34.37 days, P=0.019). There was no difference between ET and LT groups in post PCT ventilator free days (mean, 8.2 vs. 9.4 days; P=0.094). Mortality rates in ET vs. LT groups were also comparable (35% vs. 29.7%; P=0.480).
Conclusion:
Results suggest that ET in neurotrauma patients might be associated with shorter length of stay in NTU and hospital, and shorter duration of mechanical ventilation however there was no mortality difference.
Keywords: Early tracheostomy, neurotrauma, traumatic brain injury
Introduction
Long-term mechanical ventilation is the most common situation for which tracheostomy is indicated for patients in Intensive Care Units (ICUs).[1] The procedure is performed in about 24% of critically ill patients in ICU;[2] and as many as 10% of patients requiring at least 3 days of mechanical ventilation eventually receive a tracheostomy for prolonged mechanical ventilation or airway support.[3] There are several advantages associated with tracheotomy over prolonged translaryngeal endotracheal intubation, which include efficient suctioning of secretions, easier nursing care, greater comfort, less sedation, smaller dead space, lower airway resistance, reduced trauma to the oropharynx and larynx, less incidence of nosocomial pneumonia, decreased periods of mechanical ventilation and consequently length of ICU and hospital stay.[4,5,6]
More recently, it has been suggested that tracheostomy is considered within 2–10 days of intubation and that a projected need for 14 days of intubation is used as the criterion for the procedure.[3] Trauma and neurologic damage from stroke, head injury, and spinal cord injury represent a subset of patients, who may benefit from early tracheostomy (ET).[7] In patients with severe multi-trauma and/or head injury with low Glasgow Coma Score (GCS), tracheostomy at the earliest convenient time, often within 3–4 days of intubation, appears to afford some benefits.[3] As these patients often require prolonged intubation, primarily for airway protection after initial few days, and often struggled with endotracheal tubes requiring frequent use of sedatives.[8]
Studies have shown that ET in patients with traumatic brain injury is associated with lower incidences of nosocomial pneumonia, shorter duration of mechanical ventilation, ICU and hospital stay.[9,10,11,12,13] Gessler et al. also showed tracheostomy within 7 days of critical care admission for patients with poor-grade subarachnoid hemorrhage was associated with fewer respiratory adverse events.[14] However, ET had no impact on in-hospital mortality.[9,11,12] It has been suggested that ET should be recommended in traumatic brain injury patients who have a chance of survival.[15,16]
Although ET is part of the standard process in the management of patients with traumatic brain injury or neurological damage, search of medical literature showed that there is relatively little data available on impact and importance of ET in neurotrauma patients. This retrospective study was designed with a hypothesis that patients with traumatic brain injury or neurological damage requiring mechanical ventilation, ET (<5 days) in comparison to late tracheostomy (LT) (>5 days) would be associated with reduced duration of mechanical ventilation, ICU, and hospital stay. Here, we present results from this retrospective study.
Methods
This retrospective study was conducted at a Tertiary Care Hospital, Pune, India. The medical records of all patients who underwent tracheostomy at Neurotrauma Unit (NTU) of the hospital from June 2010 to November 2014 were reviewed. The institutional review board approvals were taken for the retrospective review of patient data sets, with the requirement to obtain informed consent waived by the board.
Patients > 18 years of age, who underwent percutaneous tracheostomy (PCT) were included in this retrospective analysis. Patients coming from outside hospital with tracheostomy in situ were excluded. Patients were divided into two groups, ET group (patients who underwent tracheostomy in ≤5 days after endotracheal Intubation during NTU stay) and LT group (patients who underwent tracheostomy >5 days of endotracheal intubation, during NTU stay). Acute Physiology and Chronic Health Evaluation and GCS score were used to define the severity of illness. Patients were followed till discharge from hospital or death due to any cause during hospital stay [Figure 1].
Figure 1.
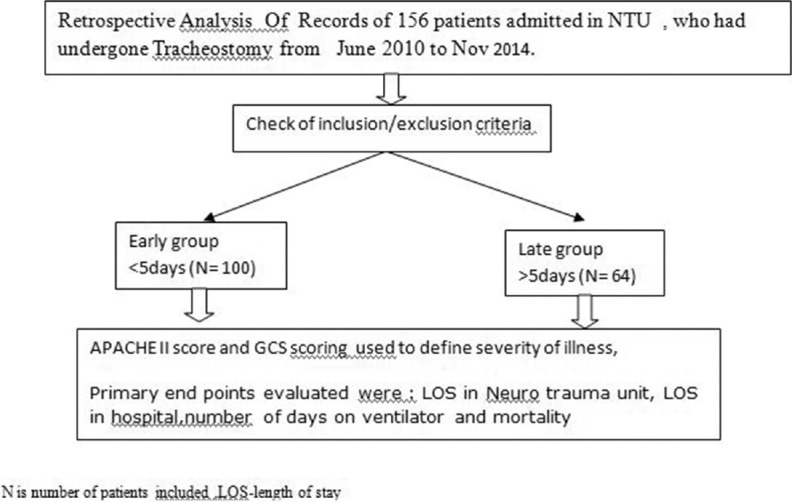
Flowchart of our study.
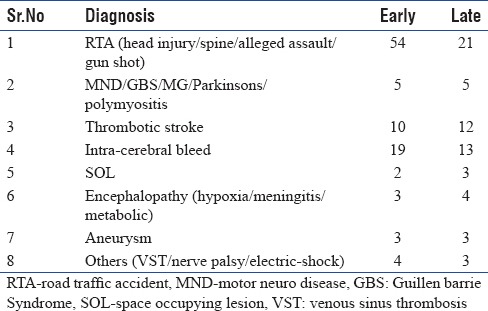
The primary endpoints in the study were to evaluate benefits of ET (≤5 days) as compared to LT (>5 days) from the time of endotracheal intubation vis-à-vis, length of stay (LOS) in ICU, hospital, number of days on ventilator and mortality. Case-mix of tracheostomized patients included our study is depicted in Table 1.
Table 1.
Dermographic distribution of Tracheostomy patients included our study
Data were analyzed using Statistical Package of Social Sciences v20.0 (IBM, USA). Continuous variables were summarized with standard descriptive statistics. Since data did not follow a normal distribution, the data between two groups were compared using nonparametric Mann–Whitney U-test. Categorical variables presented in frequency n (%) and compared using Chi-square test. P < 0.05 was considered statistically significant.
Results
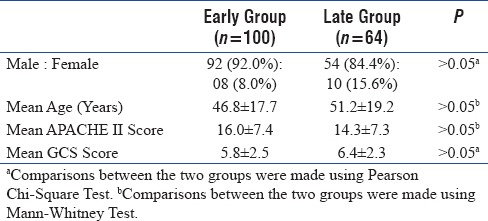
A total of 164 patients (early 100 [61%], late 64 [39%]) were included in this study. Baseline characteristics were comparable between two study groups, and are presented in Table 2.
Table 2.
Demographic and Baseline Characteristics
Primary endpoints
Comparative assessment of primary endpoints is presented in Table 3. The mean LOS in NTU was significantly lower (U = 2322, Z =−2.825, P = 0.005) in ET group, compared to LT group. The ventilator days were also significantly lower (U = 1919, Z = −4.333, P = 0.000) in early group, compared to LT group. Likewise, compared to LT group mean LOS in hospital was significantly lower (U = 2460.5, Z = −2.351, P = 0.019) in ET group. However, time of tracheostomy had no impact on post-PCT ventilator-free days (U = 2650, Z = −1.674, P = 0.094), and data were comparable between two groups. Results are illustrated in Figure 2.
Table 3.
Comparative Assessment - Early Vs. Late Tracheostomy Group
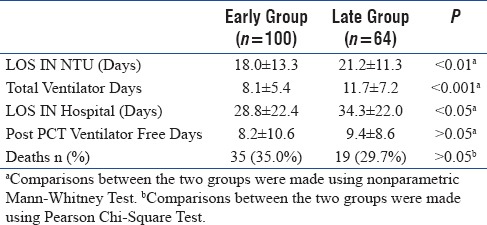
Figure 2.
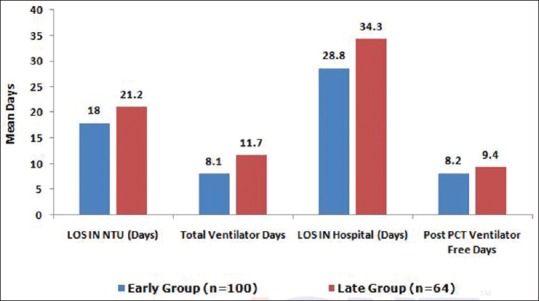
Comparative assessment of primary end points.
Although incidence of death were higher in ET group 35 (35.0%), compared to LT group 19 (29.7%), results showed no significant relationship between time of PCT (ET vs. LT) and mortality, and mortality rate were comparable (χ2 = 0.499, P = 0.480), between two groups. A Pearson product-moment correlation coefficient was computed to assess the relationship between the time of PCT and mortality. There was a negative correlation between the two variables, r = −0.055, n = 164, P = 0.483. A scatterplot summarizes the results [Figure 3]. Overall, there was a negative but statistically insignificant correlation between time of PCT and mortality, and ET does not correlate with patients’ survival.
Figure 3.
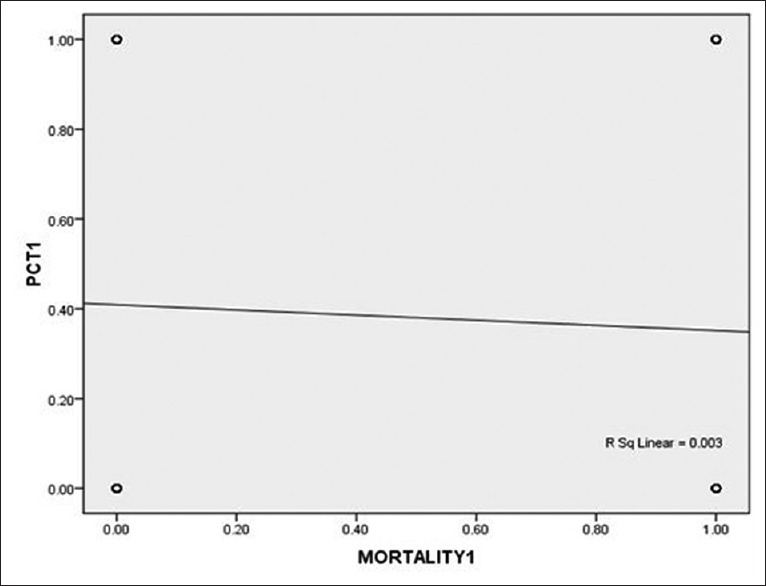
Correlation between time of percutaneous tracheostomy and mortality.
Discussion
Even though tracheostomy is one of the most commonly performed procedures in the ICU but the timing of the procedure still remains a matter of debate, and the recommendations are still based on the experience of specialists rather than on scientific evidence.[3,7,13] A number of observational studies have attempted to define the appropriate timing of tracheostomy, but have shown considerable variability.[7,13] The studies have defined ET as within 3–10 days of mechanical ventilation, while LT as within 7–14, 14–28, or >28 days after initiation of mechanical ventilation.[7] In this study, the decision of tracheostomy was done by primary consultant or neurosurgeon/neurophysician.
The inclusion of patients with different diagnoses and diverse indications for ventilatory support has been a major limitation of these studies in estimating the right timing of tracheostomy.[13] Since the advantages of tracheostomy are not uniform across the different diagnoses, and patients with certain conditions will obviously gain more benefit from ET.[7,13] Neurotrauma patients represent a subgroup, in whom studies have shown a relatively consistent cutoff time of 7–8 days, to define ET versus LT.[7]
Patient included in our study were mainly neuro: Road traffic accident, group results of our study also show benefits of ET in neurotrauma patients with severely impaired consciousness. In our study, mean LOS in NTU was significantly lower in ET group compared to LT group (mean, 18 vs. 21.2 days, P = 0.005). A prospective study by Alali et al.[11] also showed shorter LOS in ICU (median, 13 vs. 19 days) in ET (≤8 days) compared LT (>8 days). The LOS in ICU was also significantly shorter in the ET group, in a retrospective study by Wang et al.[10] (P < 0.001), Ahmed and Kuo,[12] (P < 0.001), and Siddiqui et al.[17] (P < 0.05). In contrast, a study by Pinheiro et al.[13] showed no difference between the groups (ET vs. LT) regarding the number of ICU-free days.
Compared to LT, ET was linked with fewer mechanical ventilation days (mean, 8.1 vs. 11.7 days, P = 0.000), in our study. Likewise, ET was also associated with fewer mechanical ventilation days (median, 10 vs. 16 days) in study by Alali et al.,[11] and Siddiqui et al.[17] (mean, 10.0 vs. 13.0 days; P < 0.05). However, there was no difference between the ET and LT group, with regard to ventilator days in a retrospective study by Ahmed and Kuo,[12] (mean, 15.7 vs. 20.0 days; P = 0.57).
Furthermore, ET was associated with shorter LOS in hospital compared to LT (mean, 28.8 vs. 34.37 days, P = 0.019), in our study. These findings were similar to finding by Alali et al.,[11] (median, 20 days vs. 27 days) and Rizk et al.,[9] (P < 0.0001), showing shorter LOS in hospital in ET compared to LT group. However, retrospective study by Ahmed and Kuo[12] revealed that LOS in hospital was comparable between ET and LT groups (median, 24 days vs. 28 days; P = 0.42). McCredie et al. study showed ET with acute brain injury reduced duration of mechanical ventilation (mean difference [MD] - 2.72 days, 95% confidence interval [CI], −1.29–−4.15; P = 0.0002; n = 412) and ICU LOS (MD - 2.55 days, 95% CI, −0.50–−4.59; P = 0.01; n = 326).[16]
Although ventilator-associated pneumonia (VAP) rates were not documented for two groups and is a limitation of this study, but it can be postulated that ET might have associated with lower VAP rate, resulting in shorter LOS in NTU and hospital, and shorter duration of mechanical ventilation.
However, ET had no impact on post-PCT ventilator-free days and duration was comparable between ET and LT groups (mean, 8.2 vs. 9.4 days; P = 0.094); retrospective study by Pinheiro Bdo et al.[13] also demonstrated that ventilator-free days were comparable between ET versus LT groups (median, 4 vs. 0 days; P = 0.23).
In addition to this, there were no significant differences between the ET vs. LT groups regarding overall hospital mortality (35% vs. 29.7%; P = 0.480). These results were in line with hospital mortality rate shown by Alali et al.,[11] (8.4% vs. 6.8%; odds ratio [OR], 1.25; 95% CI, 0.80–1.96) and by Ahmed and Kuo[12] (15% vs. 4%; P = 0.19). A meta-analysis of five studies by Dunham et al.[18] also indicated increased hospital mortality with ET compared to LT (OR, 1.97; P < 0.0001). McCredie et al. also showed ET did not reduce short-term mortality (relative risk, 1.25; 95% CI, 0.68–2.30; P = 0.47 n = 301).[16] In contrast, mortality rate was lower in the ET group in retrospective analysis by Pinheiro Bdo et al.,[13] (9% vs. 47%; P = 0.049) and Siddiqui et al.[17] (8.2% vs. 17.6%).
Siempos et al. in his systemic review and meta-analysis of early versus late or no tracheostomy, in post hoc analyses showed duration of sedation in ET patient (MD - 7.09 days [−14.64–0.450] P = 0.07), length of ICU stay (MD - 9.14 days [−15.53–−2.75]), length of hospital stay (MD - 3.61 days [−11.63–2.08] P = 0.17), and duration of mechanical ventilation (MD - 3.61 days [−7.00–−0.22] P = 0.04).[19]
Retrospective design, small number of patients and not measuring ventilator-associated VAP rates are the main limitations of our study. In this study, we could access very limited data so we could not comment on use and length of sedation, information about intracranial pressure, patient-centered endpoints such as comfort, communication, mobilization, and quality of life.[19] Nevertheless, findings of our retrospective study demonstrate a significant association between ET and shorter LOS in NTU, hospital and duration of mechanical ventilation and are in agreement with finding of previous studies in neurotrauma patients. A meta-analysis by Dunham et al.[18] also demonstrated an aggregate benefit for ET (P = 0.02) vis-à-vis ventilator/ICU days, compared to LT. Results of our study also showed low mortality rate in LT patients. This can be attributed to fact that more critical cases will eventually undergo tracheostomy procedure earlier. Nonetheless, mortality findings might have been different in our study with a larger cohort of patients.
Conclusion
ET offers advantages in the management of neurotrauma patients with impaired consciousness. However, large-scale, controlled prospective studies will be required to further evaluate its role in neurotrauma patients requiring prolonged ventilatory support.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would also like to acknowledge MIS team at medONE Pharma Solutions, New Delhi, India, for assistance in the preparation of this manuscript.
References
- 1.Andriolo BN, Andriolo RB, Saconato H, Atallah ÁN, Valente O. Early versus late tracheostomy for critically ill patients. Cochrane Database Syst Rev. 2015;1:CD007271. doi: 10.1002/14651858.CD007271.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Esteban A, Anzueto A, Alía I, Gordo F, Apezteguía C, Pálizas F, et al. How is mechanical ventilation employed in the intensive care unit? An international utilization review. Am J Respir Crit Care Med. 2000;161:1450–8. doi: 10.1164/ajrccm.161.5.9902018. [DOI] [PubMed] [Google Scholar]
- 3.Durbin CG., Jr Tracheostomy: Why, when, and how? Respir Care. 2010;55:1056–68. [PubMed] [Google Scholar]
- 4.Shan L, Hao P, Xu F, Chen YG. Benefits of early tracheotomy: A meta-analysis based on 6 observational studies. Respir Care. 2013;58:1856–62. doi: 10.4187/respcare.02413. [DOI] [PubMed] [Google Scholar]
- 5.Mahafza T, Batarseh S, Bsoul N, Massad E, Qudaisat I, Al-Layla AE. Early vs. late tracheostomy for the ICU patients: Experience in a referral hospital. Saudi J Anaesth. 2012;6:152–4. doi: 10.4103/1658-354X.97029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Young D, Harrison DA, Cuthbertson BH, Rowan K TracMan Collaborators. Effect of early vs. late tracheostomy placement on survival in patients receiving mechanical ventilation: The TracMan randomized trial. JAMA. 2013;309:2121–9. doi: 10.1001/jama.2013.5154. [DOI] [PubMed] [Google Scholar]
- 7.Cheung NH, Napolitano LM. Tracheostomy: Epidemiology, indications, timing, technique, and outcomes. Respir Care. 2014;59:895–915. doi: 10.4187/respcare.02971. [DOI] [PubMed] [Google Scholar]
- 8.Chintamani, Khanna J, Singh JP, Kulshreshtha P, Kalra P, Priyambada B, et al. Early tracheostomy in closed head injuries: Experience at a tertiary center in a developing country – A prospective study. BMC Emerg Med. 2005;5:8. doi: 10.1186/1471-227X-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rizk EB, Patel AS, Stetter CM, Chinchilli VM, Cockroft KM. Impact of tracheostomy timing on outcome after severe head injury. Neurocrit Care. 2011;15:481–9. doi: 10.1007/s12028-011-9615-7. [DOI] [PubMed] [Google Scholar]
- 10.Wang HK, Lu K, Liliang PC, Wang KW, Chen HJ, Chen TB, et al. The impact of tracheostomy timing in patients with severe head injury: An observational cohort study. Injury. 2012;43:1432–6. doi: 10.1016/j.injury.2011.03.059. [DOI] [PubMed] [Google Scholar]
- 11.Alali AS, Scales DC, Fowler RA, Mainprize TG, Ray JG, Kiss A, et al. Tracheostomy timing in traumatic brain injury: A propensity-matched cohort study. J Trauma Acute Care Surg. 2014;76:70–6. doi: 10.1097/TA.0b013e3182a8fd6a. [DOI] [PubMed] [Google Scholar]
- 12.Ahmed N, Kuo YH. Early versus late tracheostomy in patients with severe traumatic head injury. Surg Infect (Larchmt) 2007;8:343–7. doi: 10.1089/sur.2006.065. [DOI] [PubMed] [Google Scholar]
- 13.Pinheiro Bdo V, Tostes Rde O, Brum CI, Carvalho EV, Pinto SP, Oliveira JC. Early versus late tracheostomy in patients with acute severe brain injury. J Bras Pneumol. 2010;36:84–91. doi: 10.1590/s1806-37132010000100014. [DOI] [PubMed] [Google Scholar]
- 14.Gessler F, Mutlak H, Lamb S, Hartwich M, Adelmann M, Platz J, et al. The impact of tracheostomy timing on clinical outcome and adverse events in poor-grade subarachnoid hemorrhage. Crit Care Med. 2015;43:2429–38. doi: 10.1097/CCM.0000000000001195. [DOI] [PubMed] [Google Scholar]
- 15.Paydar S, Khalili H, Mousavi SM. Perfect timing of tracheostomy in patients with traumatic brain injury. Bull Emerg Trauma. 2014;2:136–7. [PMC free article] [PubMed] [Google Scholar]
- 16.Victoria AM, Aziz SA, Damon CS, Neil KJ, Adhikari, Gordon DR, Brain HC, et al. Effects of early versus late tracheostomy or prolonged intubation in critically ill patient with acute brain injury: A systematic review and meta-analysis. Neurocrit care. 2016 doi: 10.1007/s12028-016-0297-z. DOI 10.1007/s12028-016-0297-z. [DOI] [PubMed] [Google Scholar]
- 17.Siddiqui UT, Tahir MZ, Shamim MS, Enam SA. Clinical outcome and cost effectiveness of early tracheostomy in isolated severe head injury patients. Surg Neurol Int. 2015;6:65. doi: 10.4103/2152-7806.155757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dunham CM, Cutrona AF, Gruber BS, Calderon JE, Ransom KJ, Flowers LL. Early tracheostomy in severe traumatic brain injury: Evidence for decreased mechanical ventilation and increased hospital mortality. Int J Burns Trauma. 2014;4:14–24. [PMC free article] [PubMed] [Google Scholar]
- 19.Siempos II, Ntaidou TK, Filippidis FT, Choi AM. Effect of early versus late or no tracheostomy on mortality and pneumonia of critically ill patients receiving mechanical ventilation: A systematic review and meta-analysis. Lancet Respir Med. 2015;3:150–8. doi: 10.1016/S2213-2600(15)00007-7. [DOI] [PubMed] [Google Scholar]


