Abstract
Introduction
The ability to better prognosticate burn injury outcome is challenging and historically, most center use the Baux or revised Baux score to help prognosticate burn outcome, however, the weighted contribution of comorbidity on burn mortality has traditionally not been accounted for nor adequately studied. We therefore sought to determine the effect of comorbidities, using the Charlson comorbidity index (CCI) on burn mortality.
Methods
The purpose of this study was to determine the effect of comorbidities on burn injury mortality as determined by the LA50 (lethal TBSA burn at which 50% of the cohort will succumb from the burn injury) in a retrospective analysis of patients admitted to a regional burn center from 2002–2012. Independent variables analyzed included basic demographics, burn mechanism, presence of inhalation injury, TBSA (total body surface area), length of hospital stay, and pre-existing comorbidities. Bivariate analysis was performed and logistic regression modeling using significant variables was utilized to estimate odds of death.
Results
7640 patients were included in this study. Overall survival rate was 96%. 40% of our burn cohort had at least one comorbidity. There was a linear increase in the likelihood of death with an increase in CCI. The logistic regression model for mortality outcomes identified four statistically significant variables: age, TBSA, inhalational injury and the presence of comorbidities (OR = 1.59 for each 1 point increase in CCI; 95% CI 1.44–1.77). The unadjusted LA50 was 53% for the entire cohort. Partial adjustment multivariate regression controlling for burn mechanism and inhalation injury only, produced a slight reduction in LA50 for the 0–18 and 19–64 age categories to 76% and 48%, respectively, but a significant decrease occurred in the ≥ 65 years age group with a reduced LA50 to 20% (p<0.001). After full adjustment for all significant covariates, including comorbidities, the independent magnitude of effect of comorbidities on the LA50 was evident in the <65 cohort. The full adjustment showed a LA50 decreased by 15 and 5%, respectively in the 0–18 and >18–65 age groups respectively (p<0.001), however, in the >65 years age cohort there was no change in the LA50.
Conclusion
Preexisting comorbidities have a significant effect on burn injury mortality in all age groups, particularly the younger burn population. The measured effect of comorbidities in the >65yr age cohort was mitigated by the co-linearity between age and comorbidities. The inclusion of CCI is imperative so as to better prognosticate burn outcome and help guide expectations and resource utilization, particularly in the younger burn cohort..
Introduction
Burn injuries are among the most devastating of all injuries and a major global public health crisis.[1,2] Burns are the fourth most common type of trauma worldwide, following traffic accidents, falls, and interpersonal violence.[3] Survival following burn injury has increased in the United States over the past 50 years. This can be attributed the advances in our understanding of burn injury, early nutrition, improved critical care, infection control and early excision and grafting of burn wounds within a multidisciplinary burn care team model.
Objective estimates of the probability of death from burn injuries are difficult. The most widely used formulas for the prediction of mortality from burns are based on a minimal set of easily obtained variables. A classic example based on the Baux Score[4,5] calculated the percent likelihood of mortality as the patient’s age in years plus the percentage of the total body-surface area (TBSA) that was burned. This formula has become obsolete.[6] The ability to better prognosticate burn outcome is challenging and most burn centers use the Baux score or its revision (probability of mortality = Age + Percent TBSA + Presence of Inhalation Injury), to help prognosticate of burn injury outcome upon presentation, but the weighted contribution of comorbidity on burn mortality has not been adequately studied.
In 1987, Charlson et al. developed the Charlson comorbidity Index (CCI) to predict the ten-year mortality of patients with a range of medical conditions.[7] Each condition is given a score from one to six. A higher score predicted the increased likelihood of mortality. Older adults also tend to be at increased risk for other adverse outcomes including longer lengths of stay and higher hospital costs following burn injury as compared with younger patients with similar injuries.[8] There are several potential reasons for worse burn outcome in older adults. Preexisting medical problems—including cardiovascular, pulmonary, and renal disease—can complicate fluid resuscitation, a cornerstone of the early post-burn management period. Surgical management can also be more complicated in older patients because blood loss, intubation, and anesthesia may be poorly tolerated.[9] However, the relative impact of pre-existing medical comorbidities on survival following burn injury remains poorly understood.
Given the increasing number of older adults in the population and their persistent injury risk factors, there will likely be a greater number of older adults sustaining burn injury. We therefore sought to examine the impact of pre-existing medical co-morbidities on in-hospital mortality. The primary objective of the study was to determine the measured effect comorbidities, using the updated Charlson comorbidity index, on burn injury mortality based on LA50 (lethal TBSA burn at which 50% of the cohort will succumb from the burn injury). We hypothesize that preexisting comorbidities will have a significantly measureable effect on burn injury mortality.
Methods
This is a retrospective study of all burn patients admitted to the University of North Carolina Jaycee Burn Center from 2001 to 2012. This study was conducted following approval from our Institutional Review Board. The North Carolina Jaycee Burn Center at UNC was established in 1981 and averages more than 1200 acute admissions per year. The burn center is a single unit, 36-bed facility that has been verified by the American Burn Association for pediatric and adult care.
The medical records of subjects identified by the UNC Burn database query were reviewed to verify baseline demographic data, injury characteristics, and provide detailed information on medical comorbidities. Injury characteristics of interest included burn etiology, TBSA burned, presence of inhalation injury, and intubation status on admission to the burn center. Inhalation injury diagnosis was based on history, physical examination, and/or bronchoscopic examination.
To examine the effect of baseline medical comorbidities on outcome, a modified Charlson Comorbidity Index score was calculated for each patient. The standardized Charlson Index has been reported to accurately predict the probability of mortality within 1 year for a number of medical conditions. [7,10] The score is the weighted sum of comorbid conditions. There are 17 comorbid conditions included in the score and each is assigned a weight from 1 to 6 points. The weighted sum of all comorbid conditions is the patient’s Charlson score. (Table 1)
Table 1.
Charlson Comorbidity Index score System
| Comorbidity | Score |
|---|---|
| Myocardial infarction | 1 |
| Congestive heart failure | 1 |
| Peripheral vascular disease | 1 |
| Cerebrovascular disease | 1 |
| Dementia | 1 |
| Chronic pulmonary disease | 1 |
| Rheumatologic disease | 1 |
| Peptic ulcer disease | 1 |
| Mild liver disease | 1 |
| Diabetes without chronic complications | 1 |
|
| |
| Diabetes with chronic complications | 2 |
| Hemiplegia or paraplegia | 2 |
| Renal disease | 2 |
| Solid tumor | 2 |
| Leukema | 2 |
| Lymphoma | 2 |
|
| |
| Moderate or severe liver disease | 3 |
|
| |
| AIDS/HIV | 6 |
| Metastatic solid tumor | 6 |
|
| |
| Maximum comorbidity score | 37 |
The outcomes of interest in this study included in-hospital mortality. Baseline patient and injury characteristics were compared between groups (Lived/Died) using Analysis of Variance for continuous variables and chi-squared for discrete variables. We employed both univariate and multivariate models in order to determine the relative influence of comorbidities when controlling for other variables. To determine LA 50 TBSA, we used a multivariate logistic regression model controlling for pertinent confounders (age, inhalation injury, mechanism of injury and comorbidities). We categorized our burn cohort into 3 age groups (0–18, 19–64, and ≥65) and determined the LA50 for each patient population. We used linear regression to examine hospital length of stay and logistic regression to examine mortality. A comparison of Area Under the Receiver Operating Characteristic (AUROC) curve between regression models was done with and without CCI to determine accuracy of including CCI in predicting burn mortality. Assessment of co-linearity between variables in the logistic regression model was performed using the Variance Inflation Factor (VIF) Stata/MP (Version 12) (Statacorp, College Station, TX) was used for all data management and statistical analysis.
Results
A total of 7,640 patients were admitted and treated during the study period with a mean age of 32 ± 22 years. Of these patients, 68% were males. The age category cohort of 0–18, 19–64, and ≥65 years accounted for 30%, 62% and 8%, respectively. Caucasians made up 51% of the population. The most common mechanism of burn injury was scald (49%) followed by flame injury (45%). The overall mean TBSA for this population was 8.6± 12%. (Table 2) There was no significant difference in TBSA based on race or sex but a difference in noted within the age categories. The mean %TBSA for each age the category cohort of 0–18, 19–64, and ≥65 years was 6.8 ± 7.7 %, 9 ± 13.1%, and 11.6 ± 15.3%, respectively (p < 0.001). The mean length of hospital and ICU stay was 12.7 ± 24.7 days and 5.1 ± 20.2 days respectively (p < 0.001). Burn patients with at least one comorbidity represented 40% of the population (n=3,057).
Table 2.
Patient characteristics.
| Patient characteristics (n=7,640) | n | Mean (± SD) or % |
|---|---|---|
| Sex | ||
| Male | 5,244 | 69% |
| Female | 2,396 | 31% |
| Age | ||
| Overall | 32.0 (± 22.4) | |
| 0–18 years | 2,298 | 30% |
| 19–64 years | 4,744 | 62% |
| ≥ 65 years | 598 | 8% |
| Type of Burn | ||
| Flame | 3,426 | 45% |
| Scald | 3,678 | 49% |
| Other | 480 | 6% |
| Inhalation | ||
| Inhalation injury | 562 | 7% |
| No inhalation injury | 7,078 | 93% |
| Charlson Comorbidity Index (CCI) | ||
| Overall mean | 7,640 | 0.906864 (± 1.4) |
| 40% | ||
| TBSA | ||
| Overall mean | 7,640 | 8.6 (± 12.0) |
| By sex | ||
| Male | 5,244 | 9.0 (± 12.6) |
| Female | 2,396 | 7.7 (± 10.7) |
| By age | ||
| 0–18 years | 2,298 | 6.8 (± 7.7) |
| 19–64 years | 4,744 | 9.0 (± 13.1) |
| ≥ 65 years | 598 | 11.6 (± 15.3) |
| Survival | ||
| Overall | 7,274 | 96% |
| By sex | ||
| Male | 5,017 | 96% |
| Female | 2,257 | 94% |
| By age | ||
| 0–18 years | 2,272 | 99% |
| 19–64 years | 4,444 | 95% |
| ≥ 65 years | 422 | 77% |
| ICU stay | ||
| Overall mean | 5.1 (± 20.2) | |
| Hospital stay | ||
| Overall mean | 12.7 (± 24.7) | |
TBSA=total burn surface area
During the study period, the overall mortality was 4%. The mean age of survivors vs. non-survivors was 31 ± 21.9 years and 58 ± 20.5 years, respectively. (Table 3) TBSA was significantly associated with mortality (p<0.001). The average TBSA for patients who died was 39.9 ± 29.2%. Although patients with an inhalation injury represented a small portion (7%) of the cohort, 23% of these patients in the burn cohort died. Patients who died presented to the hospital with an average of 2.6 ± 1.9 comorbidities. Flame burns were associated with significantly higher mortality rate (7%) than scald (1%) and other types of burns (4%, p<0.001). Race and gender had no significant impact on mortality.
Table 3.
Bivariate analysis of patient demographics and clinical characteristics
| Live | Dead | p- Value (p) | |
|---|---|---|---|
| Age | 30.9 (± 21.9) | 58.3 (± 20.5) | < 0.001 |
| TBSA | 7.3 (± 8.7) | 39.9 (± 29.2) | < 0.001 |
| Inhalation | < 0.001 | ||
| Inhalation injury | 77% | 23% | |
| No inhalation injury | 97% | 3% | |
| CCI | < 0.001 | ||
| Mean | 0.8 (± 1.4) | 2.6 (± 1.9) | |
| 0 | 98% | 2% | |
| 1+ | 91% | 9% | |
| Race | 0.005 | ||
| White (51%) | 94% | 4% | |
| Other (49%) | 96% | 4% | |
| Sex | 0.082 | ||
| Male (69%) | 96% | 4% | |
| Female (31%) | 94% | 4% | |
| ICU stay | 4.1 (± 15.8) | 28.6 (± 47.2) | |
| LOS | 11.9 (± 22.9) | 30.6 (± 47.6) | |
| Mechanism | < 0.001 | ||
| Flame (45%) | 93% | 7% | |
| Scald (48%) | 99% | 1% | |
| Other (6%) | 96% | 4% |
TBSA= total body surface area
CCI=Charlson comorbidity Index
LOS= length of hospital Stay
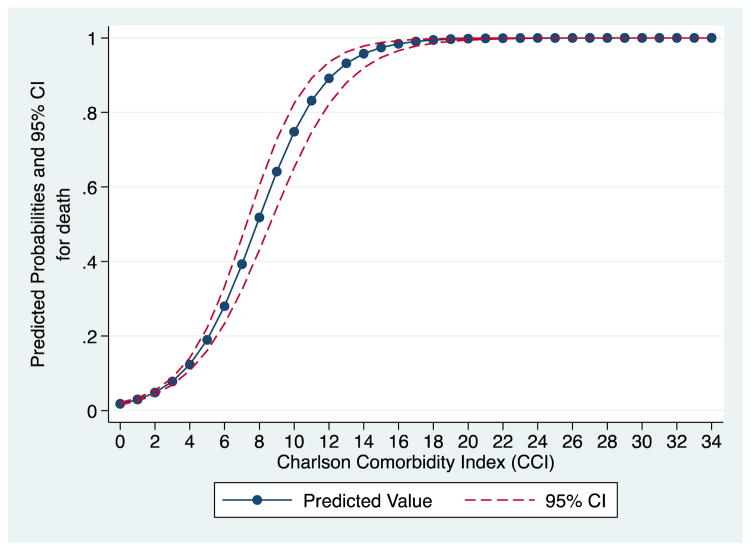
A multivariate logistic regression was then performed on patient demographics and clinical characteristics in a model for mortality outcomes identifying five variables as statistically significant: age, TBSA, mechanism of injury, presence of inhalation injury (odds ratio [OR] = 2.85; 95% confidence interval [CI] 1.99–4.08), and presence of comorbidities. (Table 4) The patient groups older than 18 years of age, 19 to 64 (OR = 2.92; 95% CI 1.31–6.52) and older than 65 years old (OR = 8.32; 95% CI 3.347–20.793), had higher odds of mortality compared to their younger counterparts. The odds of mortality increased 1.59 times (95% confidence interval 1.44–1.77) for each point increase in CCI after controlling for patient demographics and burn characteristics. There is a linear increase in the likelihood of death with an increase in CCI. (Figure 1) Comparison of AUROC was done on logistic regression models with and without CCI to determine accuracy of this variable in predicting mortality. There was a significant difference between the two models (p< 0.01).
Table 4.
Multivariate logistic regression model of mortality in burn cohort
| Variable | Adjusted odds ratio, 95% Confidence interval (CI) | p-Value |
|---|---|---|
| TBSA | 1.09 (1.08–1.10) | < 0.001 |
| Age | ||
| 0–18 years (reference group) | ||
| 19–64 years | 2.92 (1.31–6.52) | 0.009 |
| ≥ 65 years | 8.34 (3.35–20.79) | < 0.001 |
| Inhalation injury | 2.85 (1.99–4.08) | < 0.001 |
| Mechanism of injury | ||
| Scald (reference group) | ||
| Flame | 1.60 (1.03–2.50) | 0.037 |
| Other | 2.99 (1.57–5.74) | 0.001 |
| Charlson Comorbidity index (CCI) | 1.59 (1.441–1.77) | < 0.001 |
TBSA= total body surface area
Figure 1.
The predicted probability for death based on Charlson co-morbidity index
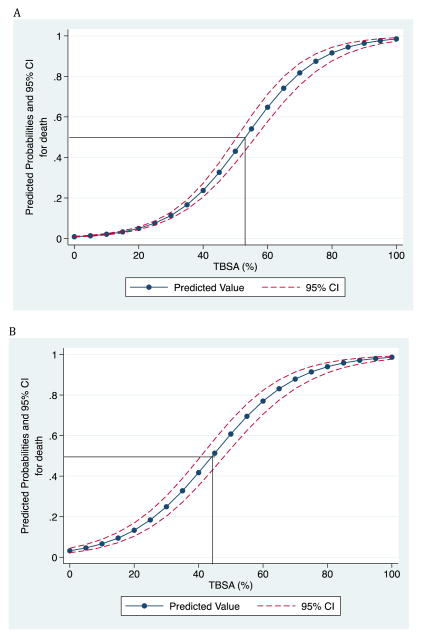
LA50 determination was based on a logistic regression of burn outcome by TBSA that increased by a geometric progression. (Table 5) The unadjusted LA50 for the entire study population was 53%. A partial adjustment for inhalation injury and mechanism of burn led to a reduction in LA50 of 8%. (Figures 2A & B). A multivariate logistic regression was then repeated using significant variables from the bivariate analysis, adjusting for age, mechanism of burn, presence of inhalation injury, and comorbidities. The unadjusted regression model for each age group showed a LA50 for age groups 0–18, 19–64, and ≥65 years of 81%, 55%, and 30% TBSA, respectively. As expected, there was a decrease in LA50 for TBSA as mechanism of burn and inhalation injury were factored into the model. Partial adjustment multivariate regression controlling for burn mechanism and inhalation injury only, produced a slight reduction in LA50 for the 0–18 and 19–64 age categories to 76% and 48%, respectively (Fig. 3A &4A), but a significant decrease occurred in the ≥ 65 years age group with a reduced LA50 to 20% (p<0.001).(Fig 5A) After full adjustment for all significant covariates, including comorbidities, the independent magnitude of effect of comorbidities on the LA50 was evident in the <65 cohort. When compared to the partially adjusted model, the full adjustment showed LA50 decreased further from 76 to 61% and 48 to 43% TBSA, respectively in the 0–18 and >18–65 age groups respectively (p<0.001), however in the >65 years age group, there was no change in the LA50. (Fig 5B) These results suggest that the presence of documented pre-existing comorbidities has a significant effect on the predicted probability of mortality, particularly in burn patients ≤ 65 years. Investigation of co-linearity in the logistic regression model was performed using Variance Inflation Factor. Independent variables TBSA, Inhalation injury and mechanism of burn had VIF less than 4. Age and comorbidities each had a VIF of 21 and 146 respectively. An interaction term for produced a VIF of 193 and tolerance of 0.005
Table 5.
Effect of prognostic factors on LA50 %TBSAa
| Unadjusted | Partially Adjusted for inhalation injury and mechanism | Fully Adjustedb | |
|---|---|---|---|
| Overall LA50 %TBSA | 53% | 45% | 35% |
| Age | |||
| ≤ 18 years | 81% | 76% | 61% |
| 19–64 years | 55% | 48% | 43% |
| ≥ 65 years | 30% | 20% | 19% |
Lethal TBSA burn at which 50% of the cohort will succumb from the burn injury.
Adjusted for inhalation injury, burn mechanism, and preexisting comorbidities.
Figure 2.
Unadjusted (A) and Adjusted (B) LA50 %TBSA for entire burn cohort
* Adjusted for Burn Mechanism, Age and Inhalational injury
Discussion
In this study, we show the weighted contribution of the addition of comorbidities, using the CCI to the predictive probability of death following burn injury. Previous studies examining mortality from burns have identified three major risk factors associated with increased mortality: age > 60 years old, TBSA > 40%, and presence of inhalation injury.[11–13] Presence of all three risk factors is associated with mortality of 90%. [11,12] Smoke inhalation injury is generally considered to be the strongest predictor of burn mortality. [13] In our burn population, however, we found that the presence of preexisting medical comorbidities had significant impact on mortality as evident by significant reduction in LA50 in those aged ≤ 65 years. In addition, we found the measured effect of comorbidities to be most pronounced in patients ≤ 18, suggesting that younger patients with medical comorbidities are more susceptible to worse outcomes. In the ≥65 age group the fully adjusted model showed only a 1% TBSA decrease in LA50 from the partially adjusted model due to co-linearity between age and the presence of comorbidities. Co-linearity was confirmed with VIF greater than 10 and tolerance close to 0.
Outcomes in trauma patients have been known to be effected by fraility.*** Frailty has been defined in older adults as the increase vulnerability to stressors due to age-related physiologic declines across multiple organ systems and risk of adverse outcomes.** However, frailty isn’t related to just aging alone and can affect those that are chronically ill at younger ages.** There is no current gold standard for diagnosing frailty. There are many screening tools such as FRAIL (Fatigue, Resistance, Ambulation, Illness, Loss of Weight) and Frailty Index (FI), that can be utilized for early assessment and identification of vulnerable patients.*** Once assessment has been completed, physicians and family must weigh the risk and benefits of interventions as well as make decisions regarding aggressiveness of care.
Historically, several models have been created to help guide prognostication of burn outcome. The Baux score described in 1961 was used to predict mortality based on age and percent TBSA alone. [4]This model did not account for inhalation injury. The Abbreviated Burn Severity Index (ABSI) created in 1982 subsequently accounted for the presence of inhalation injury but excluded comorbidities. [14]Since 2007, other prediction models that have been utilized are the Belgian Outcome in Burn Injury (BOBI) model and revised Baux score to predict burn outcomes. However, these latest models do not take into account the effects preexisting medical conditions[15,16]and may result in overestimation or underestimation of burn severity.
There are a few studies that examined the impact of comorbidities on burn injuries. However, those studies were done on a smaller population and didn’t adequately weigh the contribution of comorbidities on burn mortality. [17–22] A larger 2007 study was done by Thombs et al [23] looked at the effect of various comorbidities on burn injury mortality based on the National Burn Repository (NBR) report on 31,338 burn records from 1995–2005. They found that various pre-existing medical conditions, using the Charlson Comorbidity index and Elixhauser method of comorbidity measurement, affected burn mortality. Medical conditions such as HIV/Aids, metastatic cancer, liver disease, and renal disease had a poor prognostic outcome in acute burn injury.
The limitations of this study are those inherent to any study with a retrospective. Though we have a great sample size, this is a single center study, which may affect generalizability of our findings. Utilizing a large administrative dataset with pertinent comorbidity data would help overcome this limitation or indeed a prospective multicenter study. Also, the contribution of frailty and its effect on to outcome was not evaluated. Furthermore, the Charlson comorbidity index was originally based on the predictive power to estimate mortality in medicine patients and was never intended to generalizations to surgical or burn cohort. It has undergone several modifications and has been utilized and validated in other surgical patient cohort.[23–29]
Conclusion
Patient mortality remains the primary outcome measure for burn care. Scoring systems aim to use the most predictive premorbid and injury factors to yield an expected likelihood of death for a given patient. Age, burn surface area and inhalational injury remain the mainstays of burn prognostication, but their fidelity is imprecise without accounting for pre-existing comorbidity data. Our study has elucidated the measured effect of comorbidities on the LA 50 TBSA. With increasing health care cost, the inclusion of CCI is imperative to better prognosticate burn outcome and help guide expectations and resource utilization.
References
- 1.Forjuoh SN. Burns in low- and middle-income countries: a review of available literature on descriptive epidemiology, risk factors, treatment, and prevention. Burns. 2006;32:529–537. doi: 10.1016/j.burns.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 2.Peck MD, Kruger GE, van der Merwe AE, et al. Burns and fires from non-electric domestic appliances in low and middle income countries Part I. The scope of the problem Burns. 2008;34:303. doi: 10.1016/j.burns.2007.08.014. [DOI] [PubMed] [Google Scholar]
- 3.Mathers C, Boerma T, Fat DM. The Global Burden of Disease: 2004 Update. World Health Organization; Geneva: 2008. [Google Scholar]
- 4.Baux S. Contribution a l’Etude du traitement local des brulures thermigues etendues. Paris: These; 1961. [Google Scholar]
- 5.Zawacki BE, Azen SP, Imbus SH, Chang YT. Multifactorial probit analysis of mortality in burned patients. Ann Surg. 1979;189:1–5. doi: 10.1097/00000658-197901000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ryan CM, Schoenfeld DA, Thorpe WP, Sheridan RL, Cassem EH, Tompkins RG. Objective estimates of the probability of death from burn injuries. N Engl J Med. 1998 Feb 5;338(6):362–6. doi: 10.1056/NEJM199802053380604. [DOI] [PubMed] [Google Scholar]
- 7.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 8.Li BG, Hsu WS, Shih TS. Causes of death in aged burn patients: analysis of 36 cases. Burns. 1990;16:207–10. doi: 10.1016/0305-4179(90)90041-t. [DOI] [PubMed] [Google Scholar]
- 9.Wibbenmeyer LA, Amelon MJ, Morgan LJ, Robinson BK, Chang PX, Lewis R, 2nd, et al. Predicting survival in an elderly burn patient population. Burns. 2001;27:583–90. doi: 10.1016/s0305-4179(01)00009-2. [DOI] [PubMed] [Google Scholar]
- 10.Needham DM, Scales DC, Laupacis A, Pronovost PJ. A systematic review of the Charlson Comorbidity Index using Canadian administrative databases: a perspective on risk adjustment in critical care research. J Crit Care. 2005;20:12–9. doi: 10.1016/j.jcrc.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 11.Brusselaiers N, Hoste EAJ, Monstrey S, Colpaert KE, De Waele JJ, Vandewoude KH, Blot SI. Outcome and changes over time in survival following severe burns from 1985 to 2004. Intensive Care Med. 2005;31:1648–53. doi: 10.1007/s00134-005-2819-6. [DOI] [PubMed] [Google Scholar]
- 12.Ryan C, Schoenfeld DA, Thorpe WP, Sheridan RL, Cassem EH, Tompkins RG. Objective estimates of the probability of death from burn injuries. NEJM. 1998;338:362–6. doi: 10.1056/NEJM199802053380604. [DOI] [PubMed] [Google Scholar]
- 13.Meshulam-Derazon S, Nachumovsky S, Ad-El D, Sulkes J, Hauben DJ. Prediction of morbidity and mortality on admission to a burn unit. Plast Reconstr Surg. 2006;118(1):116–20. doi: 10.1097/01.prs.0000221111.89812.ad. [DOI] [PubMed] [Google Scholar]
- 14.Tobiasen J, Hiebert JM, Edlich RF. The abbreviated burn severity index. Ann Emerg Med. 1982;11(5):260–262. doi: 10.1016/s0196-0644(82)80096-6. [DOI] [PubMed] [Google Scholar]
- 15.Belgian Outcome in Burn Injury Study Group. Development and validation of a model for prediction of mortality in patients with acute burn injury. Br J Surg. 2009;96(1):111–117. doi: 10.1002/bjs.6329. [DOI] [PubMed] [Google Scholar]
- 16.Osler T, Glance LG, Hosmer DW. Simplified estimates of the probability of death after burn injuries: extending and updating the Baux score. J Trauma. 2010;68(3):690–697. doi: 10.1097/TA.0b013e3181c453b3. [DOI] [PubMed] [Google Scholar]
- 17.Germann G, Barthold U, Lefering R, Raff T, Hartmann B. The impact of risk factors and pre-existing conditions on the mortality of burn patients and the precision of predictive admission-scoring systems. Burns. 1997;23(3):195–203. doi: 10.1016/s0305-4179(96)00112-x. [DOI] [PubMed] [Google Scholar]
- 18.Germann G, Barthold U, Lefering R, Raff T, Hartmann B. The impact of risk factors and pre-existing conditions on the mortality of burn patients and the precision of predictive admission-scoring systems. Burns. 1997;23(3):195–203. doi: 10.1016/s0305-4179(96)00112-x. [DOI] [PubMed] [Google Scholar]
- 19.Covington DS, Wainwright DJ, Parks DH. Prognostic indicators in the elderly patient with burns. J Burn Care Rehabil. 1996;17:222–30. doi: 10.1097/00004630-199605000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Barret JP, Gomez P, Solano I, Gonzalez-Dorrego M, Crisol FJ. Epidemiology and mortality of adult burns in Catalonia. Burns. 1999;25:325–9. doi: 10.1016/s0305-4179(98)00190-9. [DOI] [PubMed] [Google Scholar]
- 21.Horbrand F, Schrank C, Henckel-Donnersmarck G, Mühlbauer W. Integration of preexisting diseases and risk factors in the Abbreviated Burn Severity Index (ABSI) Anasthesiol Intensivmed Notfallmed Schmerzther. 2003;38:151–7. doi: 10.1055/s-2003-37773. [DOI] [PubMed] [Google Scholar]
- 22.Raff T, Germann G, Barthold U. Factors influencing the early prediction of outcome from burns. Acta Chir Plast. 1996;38:122–7. [PubMed] [Google Scholar]
- 23.Thombs BD, Singh VA, Halonen J, Diallo A, Miner SM. The Effects of Preexisting Medical Comorbidities on Mortality and Length of Hospital Stay in Acute Burn Injury: Evidence From a National Sample of 31,338 Adult Patients. Ann Surg. 2007;245(4):629–634. doi: 10.1097/01.sla.0000250422.36168.67. PMC. Web. 28 Sept. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lundgren RS, Kramer CB, Rivara FP, Wang J, Heimbach DM, Gibran NS, Klein MB. Influence of comorbidities and age on outcome following burn injury in older adults. J Burn Care Res. 2009;30(2):307–314. doi: 10.1097/BCR.0b013e318198a416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Journal of Clinical Epidemiology. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 26.Romano PS, Roos LL, Jollis JG. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol. 1993;46(10):1075–1079. doi: 10.1016/0895-4356(93)90103-8. [DOI] [PubMed] [Google Scholar]
- 27.Halfon P, Eggli Y, van Melle G, Chevalier J, Wasserfallen JB, Burnand B. Measuring potentially avoidable hospital readmissions. J Clin Epidemiol. 2002;55(6):573–587. doi: 10.1016/s0895-4356(01)00521-2. [DOI] [PubMed] [Google Scholar]
- 28.Schneeweiss S, Wang PS, Avorn J, Glynn RJ. Improved comorbidity adjustment for predicting mortality in Medicare populations. Health Serv Res. 2003;38(4):1103–1120. doi: 10.1111/1475-6773.00165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]