Abstract
Background
During upper extremity (UE) stroke rehabilitation it is critical to match patient-ability to task-difficulty to promote neural reorganization and UE skill re-learning. However, there are few methods to do so. A Fugl-Meyer Upper Extremity Assessment (FMA-UE) “keyform,” derived from Rasch Analysis informed and progressed an UE rehabilitation program.
Objective
Test the feasibility of the keyform method for systematically planning and progressing rehabilitation. We hypothesized that optimally-challenging task-practice will maximize UE motor skill reacquisition.
Methods
Inclusion criteria: ischemic stroke >3 mo., voluntarily shoulder flexion ≥30° and simultaneous elbow extension ≥20°. The keyform method defined initial targets (goals) and progressed therapy after every 3rd session. Therapy targets were practiced within the context of client-selected functional tasks not in isolation. Feasibility was defined by subject pain/fatigue, UE motor function (Wolf Motor Function Test, WMFT) and movement patterns (kinematics). Assessments were administered pre- and post-treatment and compared with paired t-tests. Task-difficulty and patient-ability measures were calculated with Rasch analysis and compared with paired t-tests (p<0.05).
Results
Ten subjects (59.70±9.96 yrs., 24.1±30.54 mo. post-stroke) participated in 9 sessions, 200 movement repetitions/session in <2 hrs without pain or fatigue. Subjects gained UE motor function (WMFT: Pre 22.23±24.26 seconds, Post 15.46±22.12 seconds, p=0.01), improved shoulder-elbow coordination (index of curvature: Pre 1.30±0.15, Post 1.21±0.11, p=0.01) and exhibited reduced trunk compensatory movement (trunk displacement: Pre 133.97±74.15 mm, Post 108.08±64.73 mm, p=0.02). Task-difficulty and patient-ability measures were not statistically different throughout the program (Person-ability measures of 1.01±0.05, 1.64±0.45 and 2.22±0.65 logits and item difficulty measures of 0.93±0.37, 1.70±0.20, and 2.06±0.24 logits at the 3 testing time points respectively, p>0.05).
Conclusion
The FMA-UE keyform is a feasible method to assure that the difficulty of tasks practiced were well matched to initial and evolving levels of UE motor ability.
Recovery of movement skills after stroke is viewed as a motor (re)leaning process which means that a patient requires extensive practice of movement tasks.1,2 The content of practice sessions, what is practiced, matters. Repetitive practice of very easy movement tasks with continual success has no advantage for learning.3,4 Repetitive practice of very difficult movement tasks with little success also has no advantage for learning5 and, in stroke, may elicit altered, compensatory movements6 which may interfere with long term recovery.7 Repetitive practice of movement tasks at the “just right” level of challenge, neither too easy nor too difficult, optimizes the sensorimotor feedback available for learning by offering opportunity for implicit error detection and motor strategizing.3,8–11 However, there is no objective method for matching the difficulty of movement tasks to levels of patient ability in order to achieve the just right challenge level.
The Rasch mathematical model,12 derived from item response measurement theory,13 offers a method to quantify task-difficulty relative to patient-ability. Rasch analysis arranges measures of item-difficulty and person-ability along the same linear continuum. In doing so, the analysis indicates what items are easy enough for the individual with “poor” arm motor skills and what items are challenging enough the individual with “good” arm motor skills.14,15 The Rasch model was previously applied to the Fugl-Meyer Upper Extremity Assessment (FMA-UE),16 a widely used assessment of post-stroke arm movement ability.17 The analysis produced a FMA-UE “keyform.”17–19
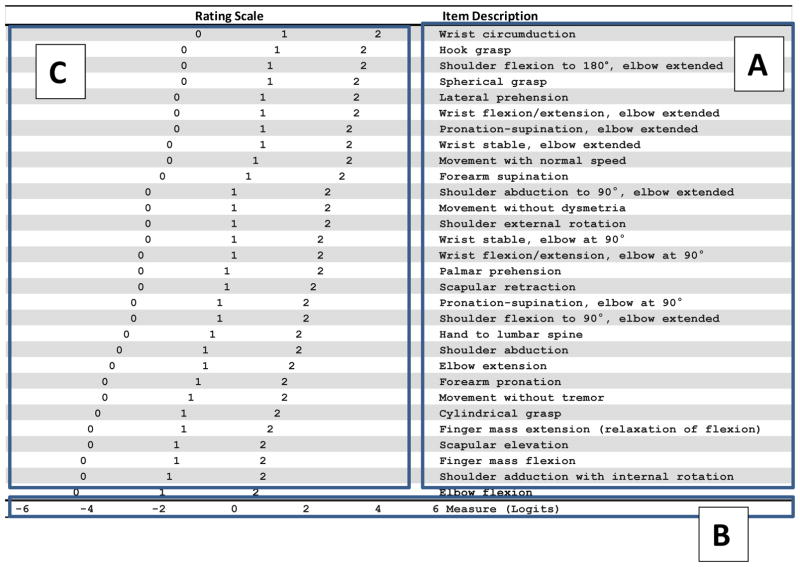
The keyform is a way to locate an individual’s level of ability relative to the item-difficulty hierarchy without the need for software or specialized statistical training.20,21 The FMA-UE keyform is shown in Figure 1. It consists of 3 regions established with Rasch analysis. Region A contains the items arranged in an item-difficulty hierarchy, where easy items are at the bottom and hard items are at the top. Region B is the measurement metric, or “ruler”, calibrated in log odds ratio units (logits, the Rasch model unit of measurement) from −6 to +6 which places FMA-UE items and client scores on the same scale. Region C is where the rater circles clients’ ratings for each item: 0, unable; 1, partial; and 2, near normal ability to perform. The rating scale stairsteps from the bottom left corner to the top right corner. The location of each rating relative to the “ruler” was plotted by the Rasch analysis to indicate the amount of upper extremity (UE) motor ability required to achieve that specific rating for the corresponding item. For example, a rating of 1 on the easiest item, elbow flexion, requires approximately −2 logits of UE motor ability and a rating of 2 on the most difficult item, wrist circumduction, requires approximately 4 logits of UE motor ability.
Figure 1.
FMA-UE Keyform
Abbreviations: Fugl-Meyer Upper Extremity Assessment (FMA-UE)
According to the Rasch model, a patient will successfully accomplish easy items and have less success with difficult items. The model also predicts that a patient will have a 50% probability of success at the point where his/her level of ability (i.e., patient-ability measure) is similar to the difficulty of an item (i.e., item-difficulty measure). An individual’s item response pattern, i.e., the pattern of circled ratings on the keyform, will be consistent with this expectation. For example, a patient will have a consistent pattern of “2”s on easy items at the bottom of the keyform, a consistent pattern of “0”s on difficult items at the top of the keyform, and a fluctuation of item responses (between one rating and the next lowest rating) in the middle of the keyform. The area of item response fluctuations is called the transition zone.18
Conceptually, the keyform’s transition zone represents the idea of evolution from one ability level to another. Said differently, it identifies items for which the patient has some, but not quite enough ability to accomplish. FMA-UE items test the ability to perform arm movements, thus items within the transition zone indicate arm movements that are optimally challenging (i.e., neither too difficult nor too easy) for the client to practice in therapy sessions. Therefore, the FMA-UE keyform may meet the need for an objective method to match the difficulty of arm movements to an individual’s ability level in order to plan optimally challenging practice sessions.
The purpose of this proof-of-concept study was to test the feasibility of using the keyform to design arm movement task practice sessions that match person-ability and task-difficulty at the beginning of, and throughout a stroke rehabilitation program. We hypothesized that repetitive practice at the just right challenge level would maximize arm motor skill reacquisition.
METHODS
Study procedures were IRB approved and participants provided informed consent. Ten subjects, recruited from local clinics, were included if they 1) experienced stroke ≥3 months prior; 2) exhibited voluntary paretic shoulder flexion ≥30° with simultaneous elbow extension ≥20° to enable engagement in treatment-related reaching tasks; 3) demonstrated passive range of motion throughout the paretic UE within 20° of normal values; and 4) were 21–90 years of age. Subjects were excluded if they exhibited 1) brainstem or cerebellar lesion, 2) other neurological injury/disease; 3) self-reported pain or orthopedic condition interfering with UE movement; or 4) were unable to understand 3-step directions during initial communication with the study therapist.
Protocol
Subjects completed 9 rehabilitation sessions; 3 times/week for 3 weeks. Subjects completed 200 movement repetitions (see explanation below) per session which was expected to require a maximum of 2 hours.22 The FMA-UE was administered at enrollment (PRE, i.e., prior to treatment week 1), after every 3rd treatment session (prior to treatment weeks 2 and 3), and immediately following (POST) the rehabilitation program. The 3 reflex items were not administered because they threaten construct validity.17
Keyform transition zone and optimally difficult therapy targets
The procedure for using the keyform to plan treatment is illustrated in Figure 2. The FMA-UE16 was administered in a standardized manner and videotaped. Following the procedure outlined by Velozo et al,18 a trained rater scored the FMA-UE by circling item ratings on the keyform. The rater was neither the evaluator nor the study therapist, and in effort to elicit unbiased keyform use, the rater was not familiar with the study’s purpose. Following the procedure described by Velozo and Woodbury23 the rater identified the transition zone by following the consistent pattern of ratings at the bottom of the keyform upwards until it deviated to the next lower adjacent rating (e.g., from a rating of 2 to 1, or from a rating of 1 to 0). This marked the lower boundary of the transition zone which was defined as the first 5 consecutive items for which 3 of these items received the next lowest rating. We reasoned that these 5 items represented the expected next steps in the subject’s transition from a current skill level to a greater skill level.18 For this study, these 5 items specified the optimally challenging arm movements that were targeted in the therapy program.
Figure 2.
Process of using the FMA-UE keyform to plan treatment sessions
Functional activities to address therapy targets
Assuring the functional relevance of the rehabilitation program was high priority, thus the 5 arm movements identified in the transition zone were practiced within the context of functional activities so that they were not disconnected from their functional application. We developed a detailed study-specific Treatment Activity Menu which linked each of the 30 FMA-UE voluntary movement items to functional tasks that primarily require the item’s arm movement. The therapist and subject collaborated to identify 2 functional activities from the menu for each of the 5 target movements (total of 10 functional activities). An example of this menu is provided in Table 1. As shown in the Table, the menu links the FMA-UE item “shoulder flexion with elbow extension” to the functional tasks “setting the table” and “household cleaning” because the tasks naturally require repetition of the targeted movement. The process of scoring the keyform, locating the transition zone, identifying targets and choosing functional activities required ~15 minutes. Subjects performed 20 repetitions of each target within each functional activity for a total of 200 repetitions/session. The number of repetitions is based on work indicating its feasibility, safety and effectiveness.24 The functional tasks practiced in a session were at the just-right level of difficulty because their selection was derived from the client’s keyform, thus linked to his/her UE motor ability measure.
Table 1.
Example of the Treatment Activty Menu
| Movement Target (from the FMA-UE Keyform transition zone): Shoulder Flexion with Elbow Extension | ||
|---|---|---|
| Functional Category and Task | Task set up to assure repetitive practice of targeted movement | Task modifications |
| Self and Home Care | ||
| • Set the table | Therapist locates cups, plates, bowls, utensils on surface to require repeated shoulder flexion with elbow extension as subject sets the table. | To assure repetition of targeted motion and avoid other movement patterns: alter size and weight of cups, plates, bowls, utensils; alter surface height; have subject sit vs. stand; alter distance of cups etc. relative to subject (near vs. far). Note: If subject does not have prehension skills therapist should alter task so that subject pushes cups etc.. into place with a closed fist rather than picks up. |
| • Household cleaning | Subject wipes various surfaces in the kitchen area. Therapist structures task to elicit repeated shoulder flexion with elbow extension for each each swiping motion. | Use mitt vs. a cloth if subject does not have grasp or prehension skills. Alter subject’s posture relative to surface to targeted motion rather than trunk rotation. |
Task-practice sessions were conducted by a licensed occupational therapist. Heart rate and blood pressure were recorded before, during and after each session and the study therapist closely monitored the subject for possible pain or fatigue. The tasks practiced within a session were at the just-right difficulty and not expected to elicit movement compensations. However, aspects of each task such as object weight, speed of performance or surface heights were manipulated to assure this. For example, see Table 1, if the subject was practicing “shoulder flexion with elbow extension” in the context of setting the table, the therapist graded the task by altering the weight of the cups/plates or table height. Additionally, because functional tasks often incorporate multiple movement patterns, the therapist manipulated task set-up or instructions to assure a primary focus on the therapy target and to avoid repetition of too-easy or too-difficult motions (i.e., motions that were outside the keyform transition zone). For example, the therapist placed cups/plates on the table away from the body, rather than close to the body, to focus on shoulder flexion with elbow extension. Similarly, the therapist instructed the subject to push a cup/plate along the surface rather than pick it up thereby avoiding repetition of too-difficult prehension motions.
Systematic progression of difficulty throughout the rehabilitation program
To assure systematic task difficulty progression throughout the program, patients were reassessed with the FMA-UE keyform after every 3rd treatment session. The process of identifying therapy targets and selecting functional activities was repeated. The expectation was that as a patient gained UE motor ability the keyform transition zone will shift upwards to identify 5 new, slightly more difficult therapy targets.
Was the just-right challenge level obtained?
Critical to this study was the expectation that the keyform method specified optimally difficult therapy targets. This expectation was investigated at the conclusion of the study by comparing the sample’s mean FMA-UE ability-measure to the mean FMA-UE transition zone item-difficulty measures at each testing time point (prior to week 1, prior to week 2 and prior to week 3). More specifically, at each time point, individual FMA-UE scores were converted into person-measures (logits) with Rasch analysis (Winsteps software25), then an average person-ability measure was calculated for the sample. Also, for each individual, the difficulty of the items within his/her transition zone was calculated (logits), then an average item-difficulty measure was calculated for the sample. The difficulty of transition zone items was defined as the average “step threshold” values calculated by the Rasch analysis. A step threshold is a boundary between each rating scale step (e.g., between “0” and “1” or between “1” and “2”) and reflects an amount of UE motor ability at which point it is equally probable that the patient would receive one or the other rating for the corresponding item.14 The sample’s mean person-ability measure was compared to the mean item-difficulty measure at each time point with paired samples t-tests (SPSS v.20, p<0.05). Similar values, i.e., insignificant results, supported our expectation that task-difficulty matched person-ability indicating the just-right challenge was obtained.
Measures of treatment effect
Treatment effect was evaluated with the Wolf Motor Function Test (WMFT)26 and kinematic analyses of a functional reaching task administered at enrollment (PRE) and immediately following (POST) intervention. PRE and POST data were compared with paired t-tests (SPSS v. 20, p<0.05).
WMFT
The WMFT is a 15-item assessment of UE function, defined as the ability to use the paretic arm to quickly accomplish tasks such as place the hand on a table, lift a soda can or stack checkers. It was administered according to standardized procedures, videotaped, and scored. The time to perform each task was recorded (seconds) and reported as an average so that lower scores indicated greater functional performance.
Kinematic analysis
Subjects were seated in a standardized posture on a backless bench with 3/4ths of the thigh on the seat, knees 90° flexed, feet flat, no trunk restraint and closely guarded by a therapist. Subjects were instructed to, first with the non-paretic UE then with the paretic UE, “reach as fast as you can” to a soda can located at 80% of arm’s length at midline, a location affording maximum shoulder flexion and elbow extension.27 Kinematic data were recorded with an 8-camera PhaseSpace system (240 Hz) using a custom marker set consistent with current models.28 Data were filtered (4th-order Butterworth low-pass, 10 Hz cutoff) and processed through a custom UE model (OBSIS software, Mt. Pleasant SC). Three trials for each arm were performed. Here we report data from the paretic UE only.
Kinematic Variables
We anticipated that some subjects would not be able to grasp the soda can. We therefore structured the kinematic analysis to capture all subjects’ performance by examining only the reach-to-touch phase of the task. The start/end of this phase was marked when the velocity of a medial wrist marker exceeded/fell below 10% of its maximal linear velocity. As the purpose of this proof-of-concept pilot study was to gain initial information about the feasibility of using the keyform to direct treatment, we selected 2 kinematic variables (from the many kinematic variables that could have been calculated) to provide information about the strategy utilized to execute the movement.
Index of curvature (IOC) is a surrogate spatial measure of shoulder-elbow interjoint coordination.29 We calculated IOC of a marker placed on the first metacarpal as the actual path distance divided by the straight-line distance between the hand starting position and target. A straight-line trajectory has an IOC=1.
Trunk displacement (TD) indicates a compensatory strategy as excessive trunk movement substitutes for reduced elbow extension.27 We calculated the resultant distance traveled by a marker placed at T10 so that reduced TD signified less movement compensation.
RESULTS
Demographic data for the 10 participants is shown in Table 2. Subjects were an average of 59.70±9.96 years of age, and 24.1±30.54 months post-stroke. All subjects were able to complete 200 movement repetitions per session in an average of 1.5–2 hours without adverse event, pain or fatigue.
Table 2.
Sample Demographics
| Code | Gender | Age | Ethnicity | Handed | Affected Side | Type | Lesion location | Months post stroke | PRE FMA-UE (out of 60) | POST FMA-UE | PRE WMFT | POST WMFT |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| S01 | M | 61 | AA | R | L | I | M1 | 29 | 40 | 56 | 6.83 | 5.00 |
| S02 | M | 72 | C | R | L | H | M1 | 60 | 29 | 34 | 25.32 | 14.28 |
| S03 | M | 60 | AA | L | L | I | FP | 5 | 22 | 27 | 84.27 | 76.42 |
| S04 | M | 64 | C | R | R | I | TP | 96 | 27 | 37 | 29.53 | 8.79 |
| S05 | M | 47 | C | R | L | I | M1 | 6 | 44 | 56 | 5.20 | 3.16 |
| S06 | M | 62 | C | L | R | I | M1 | 7 | 39 | 53 | 15.58 | 12.91 |
| S07 | M | 67 | C | L | R | I | M1 | 7 | 33 | 47 | 25.83 | 17.76 |
| S08 | M | 53 | AA | L | R | I | M1 | 4 | 57 | 59 | 2.03 | 2.03 |
| S09 | M | 70 | C | R | R | I | M1 | 12 | 56 | 57 | 2.66 | 2.06 |
| S10 | F | 41 | A | L | R | I | M1 | 15 | 32 | 48 | 25.05 | 12.20 |
Abbreviations: Male (M), Female (F), African-American (AA), Caucasian (C), Left (L), Right (R), Ischemic (I), Hemorrhagic (H), Primary Motor Cortex (M1), Fronto-parietal cortices (FP), Tempo-parietal cortices (TP), Fugl Meyer Upper Extremity Assessment (FMA-UE), Wolf Motor Function Test (WMFT).
Keyform
A sequence of FMA-UE keyforms for a representative subject (S01) is shown in Figure 3. PRE treatment in Panel A, the end of weeks 1 and 2 in panels B and C respectively, and POST treatment in panel D. The subject’s actual ratings for each FMA-UE item were circled on the keyform. The subject’s summed FMA-UE scores were 40, 45, 50 and 56/60 which correspond to Rasch ability measures of 1.04±0.33, 1.62±0.35, 2.31±0.39 and 3.55±0.55± logits at the pre, week 1, week 2 and post assessment time periods respectively. Observing the subject’s pattern of item ratings provides information about the evolution of his movement skills across the program. At each assessment the subject had a consistent pattern of “2”s on the easy items at the bottom of the keyform and a consistent pattern of “1”s on the more difficult items at the top of the keyform. The keyform also shows a fluctuation of item responses (between one rating and the next lowest rating) in the middle of each keyform indicating motions for which the subject had some, but not full ability to accomplish. The transition zones on each keyform are indicated by a rectangle. Using the study’s activity menu, the therapist linked each transition zone item to functional tasks that primarily require the item’s arm movement. These tasks were then repetitively practiced. For example, in week 1 (panel A) this subject practiced functional tasks that included those specified in Table 1 to target “shoulder flexion with elbow extension”. In week 2 (panel B) the subject practiced functional tasks that included turning a doorknob and using a socket wrench to target “forearm supination.” In week 3 (panel C) the subject practiced tasks that included painting and polishing shoes to target “wrist flexion/extension with elbow extension.” Note how the transition zone shifted higher at each testing point thereby illustrating an increase in his skill level over time.
Figure 3.
Sequence of Keyforms
Abbreviations: Fugl-Meyer Upper Extremity Assessment (FMA-UE)
Was the just-right challenge level obtained?
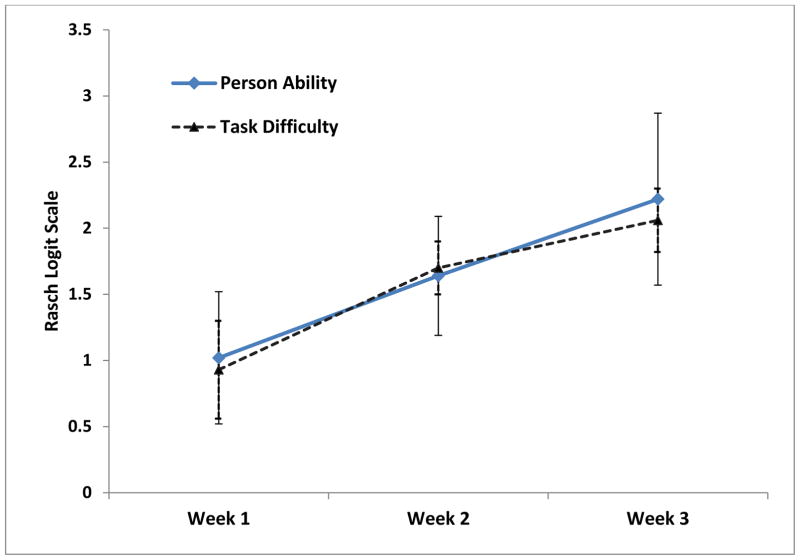
The sample’s mean Rasch person-ability and item-difficulty values were similar for each treatment week (Figure 4). The sample’s mean person-ability measures were 1.01±0.05, 1.64±0.45 and 2.22±0.65 logits and item difficulty measures were 0.93±0.37, 1.70±0.20, and 2.06±0.24 logits at the 3 testing time points. Comparison of person to item measures yielded no statistically significant differences (p>0.05 for each comparison).
Figure 4.
Person Ability and Item Difficulty match
WMFT
Subjects were able to complete the WMFT items at PRE in an average of 22.23±24.26 seconds and at POST in average of 15.46±22.12 seconds; a statistically significant change (t=3.21, df = 9, p=0.01, CI= 2.00–11.54).
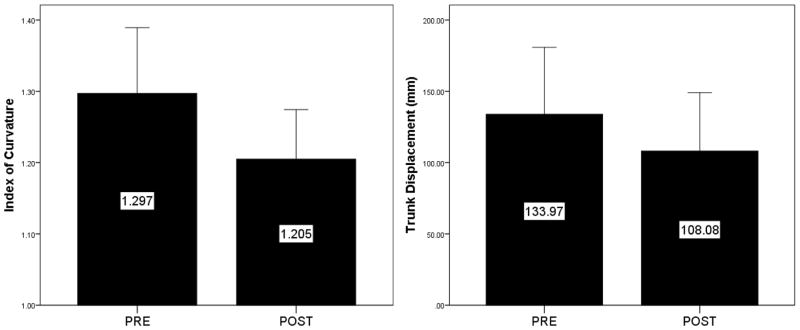
Kinematic Results
Figure 5 presents the kinematic results. Subjects demonstrated improved shoulder-elbow interjoint coordination evident as a reduction of the average IOC value from 1.30±0.15 at PRE to 1.21±0.11 at POST, a statistically significant change (t=3.07, df=9, p=0.01). Subjects demonstrated less compensatory trunk motions evident as a reduced average TD from 133.97±74.15 mm at PRE to 108.08±64.73 mm at POST, a statistically significant change (t=2.80, df=9, p=0.02).
Figure 5.
Kinematic Analysis Results
DISCUSSION
Results from this proof-of-concept study suggest that the FMA-UE keyform enabled design of task practice sessions in which the difficulty of tasks practiced were well matched to initial and evolving levels of patient-ability. By continually matching task-difficulty to patient-ability the sessions maintained optimal challenge3 and assured repetition of novel movements.8 Subjects’ gained UE motor function (WMFT) and shoulder-elbow coordination (IOC) while also demonstrating less trunk displacement (TD). To our knowledge, this is the first study examining use of the FMA-UE keyform to inform day-to-day rehabilitation.
The FMA-UE keyform transition zone defined optimally difficult arm movements as therapy targets by indicating the items for which the patient had partial success as evidenced by the fluctuating item response pattern within the transition zone. The transition zone is the manifestation of the Rasch model prediction that a person has a 50% probability of successful item performance when item-difficulty calibrations match patient-ability measures. In this way the Rasch model was used to identify arm movements at an individual’s just-right challenge level. This is important because practicing tasks for which a person has partial success optimizes feedback about the success/failure of the learner’s chosen movement strategy3 whereas motor learning is delayed if task-difficulty is too high or low.3,5 The similarity between the sample’s person-ability and transition zone item-difficulty measures suggests that the just-right challenge level was achieved. Furthermore, the WMFT and kinematic data indicate that the program improved motor function and reduced movement compensations, suggesting that the keyform method informs the design of a rehabilitation program with benefits similar to other intensive task-practice programs.
An important tenet of current post-stroke rehabilitation theory is that therapy should focus on functional activity rather than impairment.30 A reasonable concern was that our program would lack functionality because therapy targets were inspired by FMA-UE items which do not measure functional skills such as dressing or bathing. To address this concern we carefully designed procedures to assure movement practice within the context of functional activities rather than in isolation. The study menu (see Table 1) identified standardized functional activities for which each target was a critical and salient movement component. Subjects collaborated with the study therapist to choose motivating functional activities which elicited repetition of the movement targets in order to assure the targets were connected to their functional expression. In this way our program is consistent with modern theoretical frameworks which view stroke recovery as a skill (re)learning process.1
Limitations
The functional tasks practiced in a session were at the just-right level of difficulty because their selection was derived from the client’s keyform, thus linked to his/her UE motor ability measure. Various aspects of the task (object size, object location relative to the subject, surface height) were manipulated to assure that the focus of the practice session remained on the targeted motions identified in the keyform’s transition zone. However, it is possible that the therapist’s task manipulations altered the task difficulty level so that they, rather than the keyform, provided the just-right challenge. Two limitations of this study are the small sample size and lack of a control group although its purpose was to test the feasibility of the keyform method and obtain early evidence of a treatment effect. Data from this study informed the design of a large RCT ongoing in our laboratory.
Conclusions/Implications
The use of the keyform, based on the Rasch model, is a novel way to use a standardized assessment to systematically choose tasks that are appropriately matched to individual levels of motor ability throughout a rehabilitation program. The concept behind the method was to keep task-difficulty equal to participants’ skill-level throughout the program thereby optimizing sensorimotor feedback available for learning. Results provide early support that the keyform fills the critical need for a user-friendly method to relate the difficulty of tasks practiced to the ability level of the patient during UE rehabilitation.
Acknowledgments
This study is supported in part by the Ralph H. Johnson VA Medical Center and the Office of Research and Development, Rehabilitation Research and Development, Department of Veterans Affairs; Career Development-2 (B-6332W), PI: M.L. Woodbury, and VA Merit Review Awards (N0799-R), PI: M.L. Woodbury. This work was also supported by the Medical University of South Carolina COBRE for Stroke Recovery, an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health under grant number COBRE P20GM12345 (PIs: S. Kautz, R. Adams). The authors would like to thank MUSC Masters of Occupational Therapy students Patty Pierson, Emily Jeffers, Kelly Callahan, Hunter Faulk and Catie Lang for their assistance in data entry and analysis.
Footnotes
This material was presented in part as a research paper at the American Occupational Therapy Association national conference, Nashville TN, 2014
There are no conflicts of interest
References
- 1.Krakauer JW. Motor learning: its relevance to stroke recovery and neurorehabilitation. Curr Opin Neurol. 2006 Feb;19(1):84–90. doi: 10.1097/01.wco.0000200544.29915.cc. [DOI] [PubMed] [Google Scholar]
- 2.Askim T, Indredavik B, Vangberg T, Haberg A. Motor network changes associated with successful motor skill relearning after acute ischemic stroke: a longitudinal functional magnetic resonance imaging study. Neurorehabil Neural Repair. 2009 Mar-Apr;23(3):295–304. doi: 10.1177/1545968308322840. [DOI] [PubMed] [Google Scholar]
- 3.Guadagnoli MA, Lee TD. Challenge point: a framework for conceptualizing the effects of various practice conditions in motor learning. J Mot Behav. 2004 Jun;36(2):212–224. doi: 10.3200/JMBR.36.2.212-224. [DOI] [PubMed] [Google Scholar]
- 4.Adkins DL, Boychuk J, Remple MS, Kleim JA. Motor training induces experience-specific patterns of plasticity across motor cortex and spinal cord. J Appl Physiol. 2006 Dec;101(6):1776–1782. doi: 10.1152/japplphysiol.00515.2006. [DOI] [PubMed] [Google Scholar]
- 5.Sanger TD. Failure of motor learning for large initial errors. Neural computation. 2004 Sep;16(9):1873–1886. doi: 10.1162/0899766041336431. [DOI] [PubMed] [Google Scholar]
- 6.McCrea PH, Eng JJ, Hodgson AJ. Saturated muscle activation contributes to compensatory reaching strategies after stroke. J Neurophysiol. 2005 Nov;94(5):2999–3008. doi: 10.1152/jn.00732.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alaverdashvili M, Foroud A, Lim DH, Whishaw IQ. “Learned baduse” limits recovery of skilled reaching for food after forelimb motor cortex stroke in rats: a new analysis of the effect of gestures on success. Behav Brain Res. 2008 Apr 9;188(2):281–290. doi: 10.1016/j.bbr.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 8.Nudo RJ, Milliken GW, Jenkins WM, Merzenich MM. Use-dependent alterations of movement representations in primary motor cortex of adult squirrel monkeys. J Neurosci. 1996 Jan 15;16(2):785–807. doi: 10.1523/JNEUROSCI.16-02-00785.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Plautz EJ, Milliken GW, Nudo RJ. Effects of repetitive motor training on movement representations in adult squirrel monkeys: role of use versus learning. Neurobiol Learn Mem. 2000 Jul;74(1):27–55. doi: 10.1006/nlme.1999.3934. [DOI] [PubMed] [Google Scholar]
- 10.Kleim JA, Barbay S, Nudo RJ. Functional reorganization of the rat motor cortex following motor skill learning. J Neurophysiol. 1998 Dec;80(6):3321–3325. doi: 10.1152/jn.1998.80.6.3321. [DOI] [PubMed] [Google Scholar]
- 11.Boyd L, Winstein C. Explicit information interferes with implicit motor learning of both continuous and discrete movement tasks after stroke. J Neurol Phys Ther. 2006 Jun;30(2):46–57. doi: 10.1097/01.npt.0000282566.48050.9b. discussion 58–49. [DOI] [PubMed] [Google Scholar]
- 12.Wright B, Masters GN. Rating scale analysis. Chicago, IL: MESA press; 1982. [Google Scholar]
- 13.Hambleton RK, Swaminathan H, Rogers HJ. Fundamentals of Item Response Theory. Newbury Park, CA: Sage Publications; 1991. [Google Scholar]
- 14.Bond TG, Fox CM. Applying the Rasch Model: fundamental measurement in the human sciences. Mahwah, N.J: Erlbaum; 2001. [Google Scholar]
- 15.Wright BD, Stone MH. Best test design. Chicago: Mesa Press; 1979. [Google Scholar]
- 16.Fugl-Meyer AR, Jaasko L, Leyman I, Olsson S, Steglind S. The post-stroke hemiplegic patient: a method for evaluation of physical performance. Scandanavian Journal of Rehabilitation Medicine. 1975;7(1):13–31. [PubMed] [Google Scholar]
- 17.Woodbury ML, Velozo CA, Richards LG, Duncan PW, Studenski S, Lai SM. Dimensionality and construct validity of the Fugl-Meyer Assessment of the upper extremity. Archives of Physical Medicine & Rehabilitation. 2007 Jun;88(6):715–723. doi: 10.1016/j.apmr.2007.02.036. [DOI] [PubMed] [Google Scholar]
- 18.Velozo CA, Woodbury ML. Translating measurement findings into rehabilitation practice: An example using the Fugl-Meyer Assessment of the Upper Extremity with clients following stroke. Journal of Rehabilitation Research and Development. 2011;48(10):1211–1222. doi: 10.1682/jrrd.2010.10.0203. [DOI] [PubMed] [Google Scholar]
- 19.Woodbury ML, Velozo CA, Richards LG, Duncan PW, Studenski S, Lai SM. Longitudinal stability of the Fugl-Meyer Assessment of the upper extremity. Archives of Physical Medicine & Rehabilitation. 2008 Aug;89(8):1563–1569. doi: 10.1016/j.apmr.2007.12.041. [DOI] [PubMed] [Google Scholar]
- 20.Kielhofner G. The construction of keyforms for obtaining instantaneous measures from the Occupational Performance History Interview Rating Scales. Occupational Therapy Journal of Research: Occupation, Participation and Health. 2005;25:1–10. [Google Scholar]
- 21.Linacre JM. Instantaneous measurement and diagnosis. In: Smith RM, editor. Physical Medicine and Rehabilitation State of the Art Reviews. Vol 11: Outcome Measurement. Philadelphia: Hanley & Belfus, Inc; 1997. pp. 315–324. [Google Scholar]
- 22.Waddell KJ, Birkenmeier RL, Moore JL, Hornby TG, Lang CE. Feasibility of high-repetition, task-specific training for individuals with upper-extremity paresis. Am J Occup Ther. 2014 Jul-Aug;68(4):444–453. doi: 10.5014/ajot.2014.011619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Page SJ, Boe S, Levine P. What are the “ingredients” of modified constraint-induced therapy? An evidence-based review, recipe, and recommendations. Restor Neurol Neurosci. 2013 Jan 1;31(3):299–309. doi: 10.3233/RNN-120264. [DOI] [PubMed] [Google Scholar]
- 24.Birkenmeier RL, Prager EM, Lang CE. Translating Animal Doses of Task-Specific Training to People With Chronic Stroke in 1-Hour Therapy Sessions: A Proof-of-Concept Study. Neurorehabil Neural Repair. 2010 Apr 27;24(7):620–635. doi: 10.1177/1545968310361957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Winsteps Rasch measurement computer program [computer program]. Version v. 3.70. Beaverton, Oregon: Winsteps.com; 2006. [Google Scholar]
- 26.Blanton S, Wolf SL. An application of upper-extremity constraint-induced movement therapy in a patient with subacute stroke. Phys Ther. 1999 Sep;79(9):847–853. [PubMed] [Google Scholar]
- 27.Cirstea MC, Levin MF. Compensatory strategies for reaching in stroke. Brain. 2000 May;123:940–953. doi: 10.1093/brain/123.5.940. [DOI] [PubMed] [Google Scholar]
- 28.Rettig O, Fradet L, Kasten P, Raiss P, Wolf SI. A new kinematic model of the upper extremity based on functional joint parameter determination for shoulder and elbow. Gait Posture. 2009 Nov;30(4):469–476. doi: 10.1016/j.gaitpost.2009.07.111. [DOI] [PubMed] [Google Scholar]
- 29.Michaelsen SM, Luta A, Roby-Brami A, Levin MF. Effect of trunk restraint on the recovery of reaching movements in hemiparetic patients. Stroke. 2001 Aug;32(8):1875–1883. doi: 10.1161/01.str.32.8.1875. [DOI] [PubMed] [Google Scholar]
- 30.Van Peppen RP, Kwakkel G, Wood-Dauphinee S, Hendriks HJ, Van der Wees PJ, Dekker J. The impact of physical therapy on functional outcomes after stroke: what’s the evidence? Clin Rehabil. 2004 Dec;18(8):833–862. doi: 10.1191/0269215504cr843oa. [DOI] [PubMed] [Google Scholar]