ABSTRACT
The aim of this study was to evaluate the pupil size of normal subjects at different illumination levels with a novel pupillometer. The pupil size of healthy study participants was measured with an infrared-video PupilX pupillometer (MEye Tech GmbH, Alsdorf, Germany) at five different illumination levels (0, 0.5, 4, 32, and 250 lux). Measurements were performed by the same investigator. Ninety images were executed during a measurement period of 3 seconds. The absolute linear camera resolution was approximately 20 pixels per mm. This cross-sectional study analysed 490 eyes of 245 subjects (mean age: 51.9 ± 18.3 years, range: 6–87 years). On average, pupil diameter decreased with increasing light intensities for both eyes, with a mean pupil diameter of 5.39 ± 1.04 mm at 0 lux, 5.20 ± 1.00 mm at 0.5 lux, 4.70 ± 0.97 mm at 4 lux, 3.74 ± 0.78 mm at 32 lux, and 2.84 ± 0.50 mm at 250 lux illumination. Furthermore, it was found that anisocoria increased by 0.03 mm per life decade for all illumination levels (R2 = 0.43). Anisocoria was higher under scotopic and mesopic conditions. This study provides additional information to the current knowledge concerning age- and light-related pupil size and anisocoria as a baseline for future patient studies.
KEYWORDS: Pupil size, pupillometer, anisocoria
Introduction
Pupil size determines retinal illuminance and the quality of the retinal image via optimizing diffraction, ocular aberrations, and depth of focus.1 In clinical routine, the precise and easy measurement of pupil size is important for the planning and outcome of refractive surgery and neuro-ophthalmological investigations.2–4 Previously, pupillometric analyses were performed with variable devices and under variable test conditions. The majority of previous pupil size studies were executed under scotopic conditions in healthy eyes.5,6 Only a few studies under photopic illumination conditions were conducted.7–9 The complexity of comparable and reliable data on pupil size is still problematic, and factors such as illumination, accommodation, and attention might influence the accuracy of measurement.10,11 Due to spontaneous pupillary oscillations, it is difficult to measure pupil size during free gaze. Moreover, even differences in iris colour can complicate the identification of iris borders.4
A recently developed pupillometer PupilX (Albomed GmbH, Schwarzenbruck, Germany) makes it possible to measure bilateral pupil sizes simultaneously under constant and adjustable illumination levels, facilitating comparable measurements under scotopic, mesopic, and photopic conditions.2 The device works with a telecentric optical system with two focus-free infrared cameras (880 nm), so no adjustment of the oculars or pupil distance is required. A deflection mechanism via mirrors prevents direct illumination, allowing for measurements of pupil size under uniform light conditions.2 Schilde et al. compared the pupil size of healthy subjects measured with PupilX, ProCyon (Proscience Instruments, London, UK), and Colvard (Oasis Medical Inc., San Dimas, CA, USA) and demonstrated a disparity in the precision of the different devices. PupilX provided the most accurate bilateral measurements compared with ProCyon and unilateral measurements compared with Colvard.2
The aim of this study was to evaluate the pupil size of healthy subjects at different illumination levels in order to establish normative data for pupil size measured with PupilX.
Methods
The experimental protocol complied with the tenets of the Declaration of Helsinki and was approved by the local ethical committee (Landesärztekammer Saarland).
Subjects
The pupil diameter of healthy Caucasian study participants was measured using the PupilX pupillometer (Albomed) (Figure 1). Exclusion criteria were any history of eye disease, loss of vision, trauma, or interfering topical or systemic medication. Participants with diabetes mellitus or neurological or psychiatric diseases were also excluded. An additional slit-lamp examination and funduscopy excluded morphological abnormalities. Participants with considerably higher than the 95% upper limit of physiological anisocoria (n = 13) were re-examined and additional pharmacological testing was performed to exclude sympathetic or parasympathetic pareses. All subjects had no accounted disease and were not excluded from the study.
Figure 1.

Picture of the device, PupilX. The participant needs to look into the black light-tight rubber eyecups. The investigator could monitor all data at the screen sinistral at this picture.© Albomed. Reproduced with permission from Albomed. Permission to reuse must be obtained from the rightsholder.
Technical procedure
A participant’s pupil diameter was measured at five successive illumination levels with 0, 0.5, 4, 32, and 250 lux. The protocol order proceeded from the dimmest to the brightest condition. No subject was exposed to bright light directly before the measurement. Furthermore, all patients underwent a 2-minute retinal adaptation phase in the same room under low mesopic conditions (darkened room where the only light was from the device). This was monitored by the same investigator. By using light-tight rubber eyecups, the PupilX pupillometer allows for measurements under scotopic conditions without the need to completely darken the examination room. The subjects were requested to look straight ahead and keep their eyes open for the whole measurement period. The participants saw a white uniform LED (light-emitting diode) field (Cree XP-G2 [cool white]; continuous distribution with peaks at approximately 440 and 550 nm, colour temperature of ~6500 K) with adjustable brightness, which could be switched off for scotopic conditions. The patient’s eyes were measured at five illumination levels, starting at 0 lux. At each continuous level of illumination, 90 images were acquired with two focus-free infrared cameras (880 nm), 30 images per second over a measurement period of 3 seconds. After each illuminance level, the recording was paused for 5–10 seconds to allow the pupil diameter to return to baseline and to provide a short break for the participant. The subject was requested to stay in position at the device. At that time they did not see any light (light-tight rubber eye cups). We proceeded the measurements at 0.5, 4, 32, and 250 lux, providing a short break of 5–10 seconds after each illumination level. Each participant just had one run, including all five illumination levels. All measurements were performed and observed via display by the same investigator.
Data analysis
Proprietary algorithms of the device detect the pupils and measure the diameters in real time. The cameras operate at 30 frames per second, giving a temporal resolution of 33 ms. The spatial resolution of the system is 45 microns per pixel in both horizontal and vertical directions. The absolute linear camera resolution was approximately 20 pixels per mm. Pupil tracking circles were automatically fitted to image data indicating the pupil borders. The pupil diameter was measured using a proprietary algorithm that matches a best-fit circle to the pupil outline. In the case of non-circular pupils, this reports an average diameter. The resolution of measurements of the entire system is ±0.1 mm for pupils <3.3 mm and ±3% for pupils >3.3 mm. All measurements could be observed on the monitor. Recordings with blink artefacts were automatically discarded and repeated. Both eyes were recorded simultaneously. The software of the device analysed automatically the average pupil size of all 90 images with standard deviation (i.e., short-term variability within the measurement period) and anisocoria over the measurement period of 3 seconds. Data could also be selected for all 90 single measurements taken during the measurement period. A post hoc quality analysis was performed for every subject by the same investigator.
The accepted thresholds for the CIE (International Commission on Illumination) curve for vision are scotopic = illuminance levels below 0.05 lux, photopic = illuminance levels above 50 lux (National Physical Laboratory, London, UK).
Statistical analysis was performed with MATLAB R2014b (version 8.4.0; The MathWorks, Natick, MA, USA). p < 0.05 was defined as statistically significant. In order to investigate possible correlation between pupil size and illumination intensity or age, we used regression analysis and calculated R2 and p values for each analysis.
Results
This cross-sectional study analysed 490 eyes of 245 participants, 122 male and 123 female. The mean age was 51.9 ± 18.3 years; participants ranged in age from 6 to 87 years. All participating subjects were Caucasian. Number of cases per age group were as follows: ages 6–19, n = 5; 20–29, n = 27; 30–39, n = 41; 40–49, n = 40; 50–59, n = 41; 60–69, n = 36; 70–79, n = 42; and 80–87, n = 12. On average, pupil diameter decreased with increasing light intensities for both eyes, with a mean pupil diameter of 5.39 ± 1.04 mm at 0 lux, 5.20 ± 1.00 mm at 0.5 lux, 4.70 ± 0.97 mm at 4 lux, 3.74 ± 0.78 mm at 32 lux, and 2.84 ± 0.50 mm at 250 lux illumination. There was a statistically significant decrease in pupil size at higher illumination levels (p < 0.0001, Friedman rank-sum test) (Figure 1). Pairwise post hoc comparisons revealed statistically significant differences for all 10 possible combinations of five different illumination levels (p < 0.0001 throughout all 10 Wilcoxon tests). There was no statistically significant difference between the pupil size of female and male participants (p = 0.47, Wilcoxon test).
We subdivided the patients into age groups per decade. Figure 2 illustrates the pupil size for all subgroups at all illumination levels, showing a clear trend of decreasing pupil size with either age or illumination intensity. The differences in the pupil diameter in the subgroups were higher at scotopic and mesopic conditions (0, 0.5, 4 lux) than under photopic conditions (250 lux). The linear regression analysis illustrates the pupil size for all subgroups at all illumination levels, indicating a statistically significant decrease in the pupil size with increasing illumination and age. A decrease in pupil size was mainly found after the fourth decade of life (Figure 3). The results of the linear regression analysis indicate a linear correlation between pupil size and age, except at 250 lux (Figure 3). The pupil size decreased the most at 0 lux with 0.30 mm per life decade. Under mesopic light conditions, the pupil size decreased 0.28 mm per life decade at 0.5 lux, 0.29 mm at 4 lux, and 0.15 mm at 32 lux. The decrease in pupil size per life decade was lowest under photopic conditions, with a decrease of 0.11 mm at 250 lux.
Figure 2.
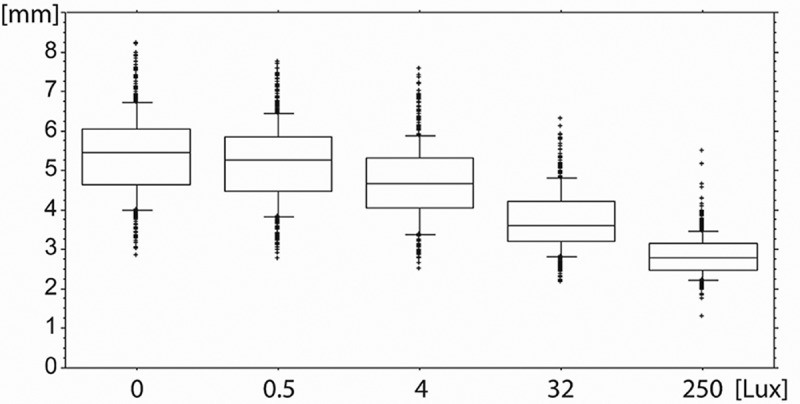
Box plot showing cumulated data with all outliers of pupil size (mm) at five illumination levels (0, 0.5, 4, 32, 250 lux) in normal subjects. The whiskers indicate 10% and 90% of data.
Figure 3.
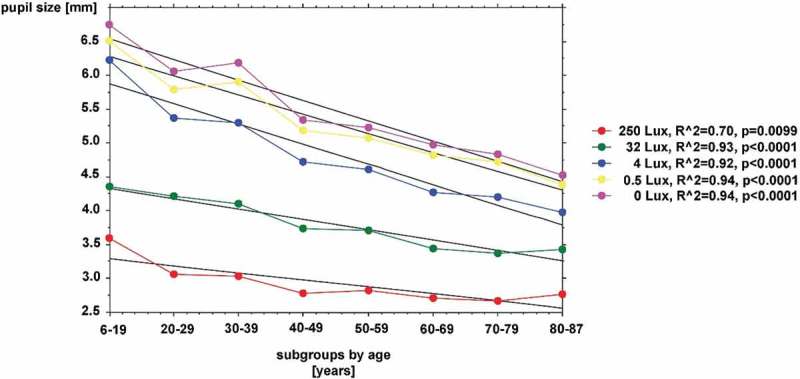
Line plot showing linear regression analysis of mean pupil size and age for five different illumination levels. The colour-coded caption indicates the different illumination levels of 0, 0.5, 4, 32, and 250 lux. The ordinate shows pupil size in mm, the abscissa shows eight different subgroups for age decades in years. The black line indicates the linear regression line for each illumination level; R2 and p values are described in the caption. Note that R2 and p values indicate a linear correlation at all illumination levels, except 250 lux. The mean pupil size decreases with increasing age and illumination intensity. The results of the linear regression analysis indicate a linear correlation between pupil size and age. Number of cases per age group: ages 6–19, n = 5; 20–29, n = 27; 30–39, n = 41; 40–49, n = 40; 50–59, n = 41; 60–69, n = 36; 70–79, n = 42; and 80–87, n = 12.
In addition, we found a statistically significant increase in anisocoria with increasing age (p < 0.05 for all multivariate statistics (both Kruskal-Wallis test and analysis of variance [ANOVA]) under scotopic and low mesopic conditions (0 and 0.5 lux illuminance levels). Each difference between right and left eyes was defined as anisocoria at this study. Figure 4 shows anisocoria in mm at all decades of age. We used linear regression as an interpolation method to estimate the progression of anisocoria for the sum of all illuminations levels and found an increase of 0.03 mm per life decade for all illumination levels (R2 = 0.43). Figure 5 shows higher anisocoria under scotopic and mesospic than photopic illuminance condition, thereby confirming our finding of a statistically significant increase in anisocoria with increasing age at 0 and 0.5 lux.
Figure 4.
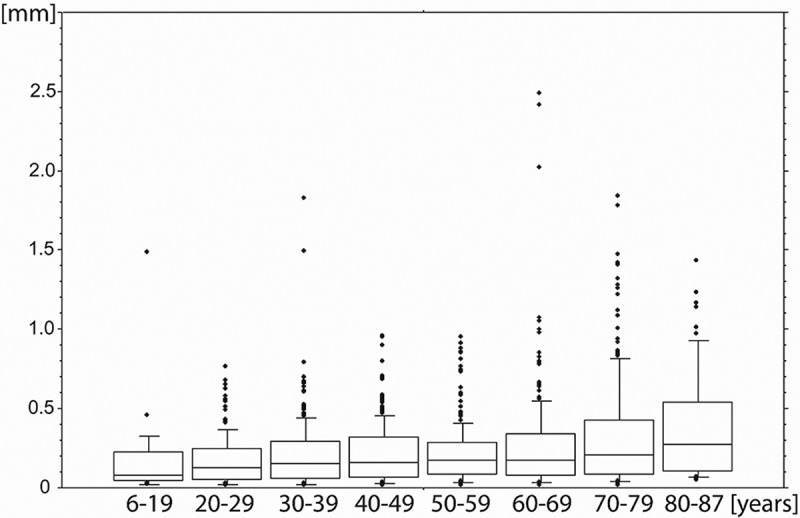
Box plot showing anisocoria in relation to age with all outliers for all illumination levels. The ordinate shows anisocoria in mm, the abscissa shows eight different subgroups for age decades in years. The whiskers indicate 10% and 90% of data.
Figure 5.
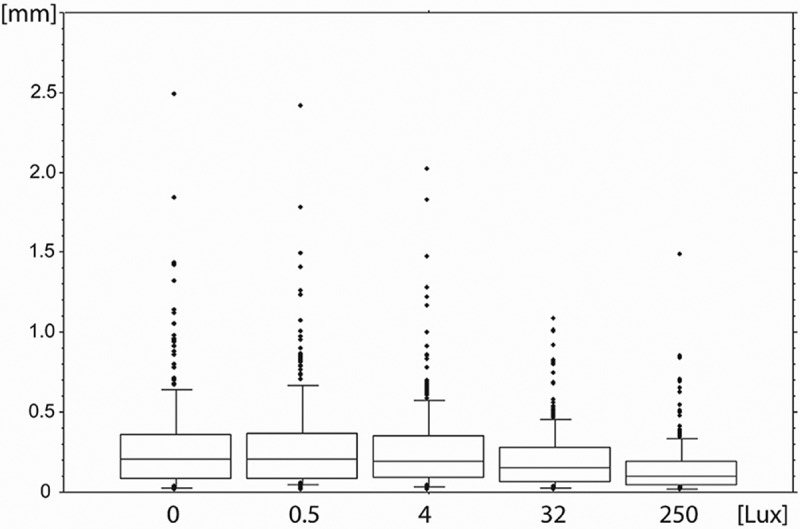
Box plot showing anisocoria in relation to illumination level with all outliers. The ordinate shows anisocoria in mm for all subjects and the abscissa shows five different illumination levels (0, 0.5, 4, 32, and 250 lux). The whiskers indicate 10% and 90% of data.
Discussion
This study provides additional information to the current knowledge for bilateral pupil size and anisocoria in healthy subjects under scotopic, mesopic, and photopic conditions as measured with PupilX (Albomed). The results of this study are consistent with previous reports about decreasing pupil size with increasing age and illumination levels.5,8,9,12,13 Furthermore, we could demonstrate that the amount of anisocoria increased with age. We found no significant relationship between gender and pupil size.
Many comparison studies have demonstrated that the size of the pupil measured with various devices differs.2,14,15 However, precise measurement of pupil size is important for the clinical outcome of refractive surgery.3,4 Schilde et al. reported that the PupilX digital pupillometer provides repeatable, comparable, and precise bilateral measurements under indirect infrared illuminance conditions with easy and automated handling.2
A possible limitation of this study is the variable length of time needed for full dark adaptation of the retina in different individuals. In this study, 2 minutes were allowed for each participant. We have chosen this retinal adaptation phase because it is practicable in clinical routine and is also assimilable to daily life illuminance conditions. Furthermore, the rapid-phase pupil constriction following the onset of light stimuli represents the rod/cone-driven extrinsic photo activity and a brief 2- to 3-second pause allows the pupil to dilate briefly.16 The pupil reaction is the fast part of retinal adaptation and takes only few seconds to a minute.17,18 Therefore, possible differences caused by the short recovery intervals between the illuminance levels might be acceptable. Factors influencing pupil size, including fatigue or emotional stress, can hardly be excluded.19 In addition, accommodation cannot be completely excluded and could lead to smaller pupil sizes.20 However, it is unlikely that accommodation plays a major role, as the device uses a telecentric system and does not offer a near target.
In our experience, the advantages of PupilX were easy handling and good measurements even for participants with dark irises and darkened eyelashes. However, this study analysed Caucasian subjects only. Recordings with blink artefacts were automatically discarded. In addition, based on our experience, even children could easily be measured with PupilX due to its quick measurement. However, eye movements cause artefacts. In cases of obvious artefacts, individual measurement data could be excluded for experimental setups. However, the whole measurement should be observed via display to minimise artefacts caused by inobservance, pendant eyelids, or long darkened eyelashes.
Our results provide additional information on pupil size for normal subjects in digital pupillometry. The majority of previous pupil size studies were executed under scotopic conditions.5,6 In contrast, studies under well-defined mesopic and photopic illumination conditions are rare.7–9 These studies with different luminance levels represent the pupil in its normal working conditions. The pupil controls the retinal illuminance and therefore determines the quality of the retina image.1 Previous studies illustrated an age-dependent decrease in pupil size under scotopic conditions,6,8,12,13 particularly after the fourth decade of life.13 Furthermore, an increase in pupil size was found in the first decade of life, reaching a peak in the second decade and then decreasing again.5,21 This study confirmed an age-related significant decrease of pupil size, particularly after the fourth decade of life. The age-dependent decrease in pupil size was higher under scotopic and mesopic conditions (0, 0.5, 4 lux) than under photopic conditions (250 lux). This is in accordance with findings by Winn et al. of a significant linear relationship between pupil size and log luminance and further decreasing gradient with increasing age.9 In this study pupil size decreased by 0.3 mm per life decade under scotopic conditions and 0.11 mm per life decade under photopic conditions. This is less than reported in other studies, where pupil size decreases under low light condition were reported at 0.4 mm per life decade and 0.25 mm per life decade at 30 cd/m.2,8,9 In turn, Winn et al. showed a decreasing pupil size gradient of 0.015 mm per year at 4400 cd/m.2,9 Explanations for this age-related decreased pupil size could be atrophy of the dilatator muscle, rigidity of the iris, decreased sympathetic tone, or reduced parasympathetic inhibition.22
Furthermore, we found an increased amount of anisocoria with age at all illumination levels. However, each difference between right and left eyes was defined as anisocoria. Anisocoria was higher under scotopic and mesospic conditions. This is in accordance with Lam et al. who descriped the prevalence of simple anisocoria decreases with brighter conditions based on pupillary diameter difference.23 Silbert et al. also found an increase of anisocoria with age, even among at a younger population.23
The fact that the amount of anisocoria increases with age could be useful for future neuro-ophthalmological diagnostics. It is important to distinguish whether anisocoria is physiological or an expression of an oculosympathetic paresis that would require further diagnostics. However, anisocoria is also possible after photorefractive keratectomy,24 corneal abrasion, marginal keratitis, acute anterior uveitis, or even in the case of retinal detachment.23,24 Normative data of age-dependent pupil size at a range of luminances could have an impact on the age-related design of bifocal contact lenses or intraocular lenses.27 Furthermore, precise mesopic and scotopic pupil sizes are important for the corneal ablation zone and for multifocal intraocular lens insertion in refractive surgery.2,3 In additional, data on mesopic pupil sizes are necessary for current studies about accommodative intraocular lenses.8 Pupillometry is even applied in psychological and pharmaceutical studies.17
In conclusion, this study provided additional information to the current knowledge for pupil size and anisocoria with different illumination conditions in normal subjects measured with PupilX. This could be a baseline for future patient studies.
Acknowledgements
We would like to thank Axel von Wallfeld (MEye Tech GmbH) for material and technical support. We would like to thank all members of Eye Clinic Sulzbach for their support.
References
- [1].Campbell FW, Green DG.. Optical and retinal factors affecting visual resolution. J Physiol 1965;181:576–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Schilde T, Bende T, Matallana M, Kohlhaas M.. Messung des Pupillendurchmessers. Augenspiegel 2013;6:32–34. [Google Scholar]
- [3].Young RS. Pupil size and the ablation zone in laser refractive surgery: considerations based on geometric optics. J Cataract Refract Surg 2003;10:1924–1931. [DOI] [PubMed] [Google Scholar]
- [4].Rosen E, Gore C, Taylor D, Chitkara D, Howes F, Kowalewski E. Use of a digital infrared pupillometer to assess patient suitability for refractive surgery. J Cataract Refract Surg 2002;28:1433–1438. [DOI] [PubMed] [Google Scholar]
- [5].Kohnen EM, Zubcov AA, Kohnen T.. Scotopic pupil size in a normal pediatric population using infrared pupillometry. Graefes Arch Clin Exp Ophthalmol 2004;242:18–23. [DOI] [PubMed] [Google Scholar]
- [6].Schnitzler EM, Baumeister M, Kohnen T.. Scotopic measurement of normal pupils: Colvard versus Video Vision Analyzer infrared pupillometer. J Cataract Refract Surg 2000;26:859–866. [DOI] [PubMed] [Google Scholar]
- [7].MacLachlan C, Howland HC.. Normal values and standard deviation for pupil diameter and interpupillary distance in subjects aged 1 month to 19 years. Ophthalmic Physiol Opt 2002;22:175–182. [DOI] [PubMed] [Google Scholar]
- [8].Heine C, Yazdani F, Wilhelm H.. Pupillary diameter in every day situations. Klin Monatsbl Augenheilkd 2013;230:1114–1118. [DOI] [PubMed] [Google Scholar]
- [9].Winn B, Whitaker D, Elliott DB, Phillips NJ. Factors affacting light-adapted pupil size in normal human subjects. Invest Ophthalmol Vis Sci. 1994;35(3):1132–7. [PubMed] [Google Scholar]
- [10].Ettinger ER, Wyatt HJ, London R.. Anisocoria, variation and clinical observation with different conditions of illuminations and accommodation. Invest Ophthalmol Vis Sci 1991;32:501–509. [PubMed] [Google Scholar]
- [11].Lüdtke H, Wilhelm B, Adler M, Schaeffel F, Wilhelm H. Mathematical procedures in data recording and processing of pupillary fatigue waves. Vision Res 1998;38:2889–2896. [DOI] [PubMed] [Google Scholar]
- [12].Loewenfeld IE. Pupillary changes related to age In: Thompson HS, Daroff R, Frisèn L, Glaser JS, Sanders MD, editors. Topics in Neuro-Ophthalmology. Baltimore, MD: Williams and Wilkins; 1972:124–150. [Google Scholar]
- [13].Borgmann H. [Basic data for clinical pupillography. II. The age-dependence of the pupil diameter in darkness]. Greafes Arch Clin Exp Ophthalmol 1972;184:300–308. [DOI] [PubMed] [Google Scholar]
- [14].Kohnen T, Terzi E, Bühren J, Kohnen EM.. Comparison of digital and handheld infrared pupillometer for determiníng scotopic pupil diameter. J Cataract Refract Surg 2003;29:112–117. [DOI] [PubMed] [Google Scholar]
- [15].Schmitz S, Krummenauer F, Henn S, Dick HB.. Comparison of three different technologies for pupil diameter measurement. Greafes Arch Clin Exp Ophthalmol 2003;241:472–477. [DOI] [PubMed] [Google Scholar]
- [16].Larson M, Behrends M.. Portable infrared pupillometry: a review. Anesth Analg 2015;120:1242–1253. [DOI] [PubMed] [Google Scholar]
- [17].Wickremasinghe S, Smith G, Stevens J.. Comparison of dynamic digital pupillometry and static measurements of pupil size in determining scotopic pupil size before refractive surgery. J Cataract Refract Surg 2005;31:1171–1176. [DOI] [PubMed] [Google Scholar]
- [18].Campbell FW, Rushton WAH.. Measurement of the scotopic pigment in the living human eye. J Physiol 1955;130:131–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Bradley MM, Miccoli L, Escrig MA, Lang PJ.. The pupil as a measure of emotional arousal and autonomic activation. Psychophysology 2008;45:602–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Hiraoka M, Moroda M, Hashimoto Y, Suganuma M.. Near triad measurement—accommodative pupillometry with horizontal eye tracking and its qualitative analysis Nihon Ganka Gakkai Zasshi 2006;110:263–270. [PubMed] [Google Scholar]
- [21].Silbert J, Matta N, Tian J, Singman E, Silbert DI.. Pupil size and anisocoria in children measured by the plusoptiX photoscreener. J AAPOS 2013;17:609–611. [DOI] [PubMed] [Google Scholar]
- [22].Kumnick LS. Aging and pupillary mechanism. J Gerontol 1956;11:160–164. [DOI] [PubMed] [Google Scholar]
- [23].Lam BL, Thompson HS, Walls RC.. Effect of light on the prevalence of simple anisocoria. Ophthalmology 1996;103:790–793. [DOI] [PubMed] [Google Scholar]
- [24].Geerling G, Neppert B, Wirbelauer C, Laqua H.. Relative mydriasis after photorefractive keratectomy. J Refract Surg 2000;16:69–74. [DOI] [PubMed] [Google Scholar]
- [25].Pearson RV, Rose GE Anisocoria in unilateral ophthalmic disease. Br J Ophthalmol 1991;75:31–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Kecik D, Kasprzak K.. Pupillometry in unilateral retinal detachment. Klin Oczna 1991;93:124–125. [PubMed] [Google Scholar]
- [27].Borish IM. Pupil dependency of bifocal contact lenses. Am J Optom Physiol Opt 1988;65:417–423. [DOI] [PubMed] [Google Scholar]


