Abstract
Purpose: For Black women who have sex with women (BWSW), obtaining routine healthcare can be obstructed by a number of psychosocial barriers, including experiences of stigma, related to both sexual orientation and race, and medical mistrust, both race-based and global. Previous research demonstrates that sexual orientation and race-based stigma, as well as global and race-based medical mistrust, each have a negative impact on health outcomes and engagement in care (EIC) independently. This study addresses gaps in the literature by examining the impact of these psychosocial barriers and their interactions among BWSW, an understudied population.
Methods: Participants (256 BWSW) were surveyed at a Black Gay Pride festival. Separate generalized linear models assessed the independent and multiplicative effects of participants' self-reported sexual orientation stigma, race-based stigma, race-based medical mistrust, and global medical mistrust related to their engagement in routine physical exams and blood pressure screenings.
Results: Prevalence rates of both stigma measures were low, but prevalence rates of global and race-based medical mistrust were high. The results show that experiencing sexual orientation stigma or having race-based medical mistrust predicts significantly lower EIC. Furthermore, the frequencies of obtaining recent physical examinations and blood pressure screenings were significantly related to three- and two-way interactions between stigma and medical mistrust, respectively.
Conclusion: There is an urgent need to address the intersectionality of these psychosocial barriers in an effort to increase BWSW's EIC.
Keywords: : barriers to care, lesbian, race/ethnicity/culture, women who have sex with women (WSW)
Introduction
Engagement in healthcare is an imperative first step toward maintaining well-being and treating illness.1 Policy-driven attention has increasingly been drawn to preventive efforts for an array of health conditions. Yet, sexual and racial/ethnic minority populations, such as Black women who have sex with women (BWSW), within the United States still experience a myriad of health disparities at elevated rates. It is a well-established and persistent trend that Black adults are uninsured or underinsured at higher rates, have less access to healthcare, and receive lower quality healthcare than their peers from other ethnic or racial backgrounds.2 Thus, given the race- and sexual orientation-related disparities in engagement in care (EIC) in the United States, understanding the barriers to EIC is vital. Accomplishing this feat could help eliminate disparities in access to and engagement in care, and could concurrently improve the health and well-being of BWSW.3
This study examines the psychosocial factors of race- and sexual orientation-related stigma, as well as race-based and global medical mistrust, in relation to EIC within a BWSW sample. For BWSW, both race and sexual orientation can be sources of stigma, and each of these types of stigma has yielded significant negative consequences for physical and mental health.4–7 The social sciences field has established a long history of race-based stigma that affects Black people in the United States.8 This stigma is strongly related to disparities in physical health,9 as well as in seeking and receiving quality healthcare.10 Sexual orientation stigma differs from race-based stigma, in that, it is a potentially concealable identity and includes additional stressors related to stigmatized identity disclosure.11 When women who have sex with women (WSW) do disclose their sexual identities and behaviors to care providers, they are more likely to receive higher quality treatment, have higher rates of engagement in primary and preventive care, and report being more satisfied with the services they receive.12 Perceiving that sexual orientation stigma exists in the healthcare setting, however, often precludes disclosure of this nature.12,13 Still, there is minimal research on the effects of sexual orientation stigma on Black women. Sexual orientation and race-based stigma independently yield negative consequences, yet the additive effects of experiencing both of these types of stigma have received limited research attention and warrants examination. This study is the first that we know of to assess the interaction of these two distinct types of stigma in relation to EIC among BWSW.
In addition to stigma, medical mistrust is also a potential barrier to EIC. When patients have a global sense of medical mistrust (i.e., when they distrust the healthcare system as a whole), they have poorer EIC, which can lead to worse health outcomes.14,15 While a number of studies have examined the role of mistrust in healthcare services,16–20 insufficient research on the role of medical mistrust and the subsequent relationship with EIC has been conducted, particularly with BWSW. Two studies on this topic found that higher rates of medical mistrust are associated with lower levels of engagement in preventive medicine, such as routine wellness appointments,21 and are a barrier to routine care among Black men who have sex with men.4 Moreover, race-based medical mistrust (i.e., the belief that a specific racial group will not receive equal and adequate care from the healthcare system) is a well-established barrier to care for Black people19; White adults are, generally, more likely to engage in preventive health services than their non-White counterparts.22 However, the role of race-based medical mistrust has yet to be examined among BWSW.
Objectives of this study
The purpose of this study is to determine the prevalence and effects of psychosocial barriers to routine EIC in BWSW, specifically in terms of sexual orientation and race-based stigma, and race-based and global medical mistrust. We hypothesize that increased rates of all four psychosocial barriers, as well as the interaction between sexual orientation, race-based stigma, and race-based medical mistrust will relate to lower EIC.
Methods
Participants and setting
All measures and procedures were approved by the University of Connecticut Institutional Review Board. Pencil and paper surveys were administered using venue intercept procedures23,24 at a Black Gay Pride community festival in Atlanta, Georgia. Potential participants were invited to take the survey and were told that the survey asked about health-related beliefs and behaviors, contained personal questions, was anonymous, and would take 15 minutes to complete. Verbal consent was obtained from all participants. Of 279 women who initially participated, 24 women were excluded—10 reported not previously having sex with women, 13 did not identify as Black/African American, and 1 was missing data for both variables. Analyses were conducted on the remaining 255 BWSW with cases excluded pairwise. Participants' names were not collected at any time. In addition, participants were offered $7 compensation for their participation and were given the option of donating their incentive payment to a local community-based organization.
Measures
In addition to collecting demographic information (i.e., age, highest level of education, annual income, current employment status, and self-identified sexual orientation), the surveys assessed the following: healthcare access; engagement in routine healthcare (Table 1); perceived sexual orientation and race-based stigma; and global and race-based medical mistrust.
Table 1.
Response Frequencies and Percentages of Reported Healthcare Access and Engagement in Care
| BWSW (N = 255), n (%) | |
|---|---|
| Was there any time in the past 2 years when you were completely without any health plan or insurance coverage? | |
| Yes | 110 (43.1) |
| No | 145 (56.9) |
| Do you have a regular doctor or other health professional, such as a nurse or physician's assistant, you usually go to when you are sick or need healthcare? | |
| Yes | 188 (73.7) |
| No | 67 (26.3) |
| Do you have a doctor or nurse you can talk with about sexual health? | |
| Yes | 200 (78.1) |
| No | 55 (21.5) |
| Are you comfortable talking about sexual health with a doctor or nurse? | |
| Yes | 234 (91.8) |
| No | 21 (8.2) |
| When was the last time you had a physical examination by a doctor or other health professional?a | |
| Past 6 months | 127 (51.2) |
| Past year | 86 (34.7) |
| Past 2 years | 18 (7.3) |
| Past 5 years | 7 (2.8) |
| More than 5 years | 10 (4.0) |
| When was the last time you had your blood pressure checked?b | |
| Past 6 months | 183 (74.1) |
| Past year | 53 (21.5) |
| Past 2 years | 7 (2.8) |
| Past 5 years | 1 (0.4) |
| More than 5 years | 3 (1.2) |
n = 248 due to 3.1% missing data.
n = 247 due to 3.5% missing data.
BWSW, Black women who have sex with women.
Healthcare access
Participants were asked to answer a series of questions about their access to healthcare, including whether they went without health insurance at some point in the past 2 years, currently have a regular doctor or healthcare professional to whom they can go for medical care, and are comfortable talking about sexual health with their provider. Responses were dichotomized Yes/No.
Engagement in routine care
EIC was assessed by asking participants when they last had a physical examination and their blood pressure checked by a doctor or other health professional. Given that engagement in care can be measured in multiple ways, we chose a “Gaps in Care” approach25 that is based on assessing time intervals between clinic visits or time since most recent appointment. Furthermore, the Centers for Disease Control and Prevention26 indicates that having a routine checkup by a medical practitioner within the last 12 months is an effective indicator of engagement in care. Similarly, frequent blood pressure checks are also important indicators of engagement in care for BWSW, particularly because Black people tend to have poorer blood pressure control than people from other racial groups.27 The response scale for these items ranged from “1—in the past six months,” to “5—more than five years ago.”
Sexual orientation and race-based stigma
Participants answered six questions about their experiences with perceived stigma from healthcare providers. Three questions focused specifically on sexual orientation stigma (Cronbach's α = 0.83), and the same three questions were asked again, but targeting race-based stigma (Cronbach's α = 0.90). For example, “I have been mistreated by healthcare providers because of my sexual orientation” and “I have been ignored by healthcare providers because of my race.” The response scale ranged from “1—strongly disagree,” to “4—strongly agree.”
Medical mistrust
Medical mistrust is a subjective assessment that “measures [a participant's] suspicion of mainstream healthcare systems and healthcare professionals, and the treatment provided to individuals of the respondent's ethnic or racial group” (p. 211).28 Participants answered eight items derived from the Group-Based Medical Mistrust Scale28 concerning race-based medical mistrust (Cronbach's α = 0.73). Participants answered three items concerning global medical mistrust drawn from the Medical Mistrust Index (LaVeist T: Measuring trust in healthcare: Medical Mistrust Index 2.1, 2013; Cronbach's α = 0.80). Responses to both scales ranged from “1—strongly disagree,” to “4—strongly agree.”
Data analysis
First, descriptive analyses were provided as counts and percentages for all variables. For interpretation purposes, response sets were collapsed to “agree” and “disagree,” however, variables with this response set were treated as continuous in generalized linear models (GLMs). Second, two GLMs were conducted with the psychosocial barriers to separately predict each EIC item. There were less than 10% missing data for any given variable. For all analyses, P < 0.05 was used to define statistical significance. Predictive Analytics SoftWare (PASW) Statistics version 18.0 (SPSS, Inc., Chicago, IL) was utilized for all analyses.
Results
Descriptives
Participants' average age was 32.80 (SD = 9.66) years old. Their average level of education was 14.24 (SD = 2.07), which corresponds to 2 years of college-level education. A majority of participants, 76%, were employed and 46% reported earning more than $30,000 annually. Participants self-identified as “Lesbian/Same gender loving” or “Bisexual.” While many participants reported being without health insurance at some point in the past 2 years, most (74%) reported having a regular doctor or healthcare professional at the time of the survey. An overwhelming percentage of participants had a physical examination (86%) or blood pressure check (95%) in the past year. Almost all participants felt comfortable talking about sexual health with a care provider, but only 78% of participants reported actually having a provider they felt they could talk with about sexual health (Table 1).
Rates of sexual orientation stigma ranged from 4% to 7%, while race-based stigma ranged from 6% to 9% on all items, including participants' reported beliefs that their healthcare was not as good as others', and of being mistreated or ignored by providers due to their sexual orientation or race, respectively. Participants reported experiencing both sexual orientation and race-based stigma at rates of 1.6–2.4%. More than half (54%–60%) of participants felt that people of their race are not treated the same by and do not receive the same level of care from doctors and healthcare workers as people of other races. Approximately 20% of participants felt that healthcare workers do not take medical complaints from people of their race seriously and people of their race should be suspicious of medicine. Rates of global medical mistrust were higher. A majority of participants (62%) agreed that healthcare providers, at times, have done harmful things to patients without their knowledge. Fifty-six percent of participants agreed that patients have been deceived or misled by healthcare providers, and 55% of participants agreed that healthcare providers cover up mistakes that they make.
Generalized linear models
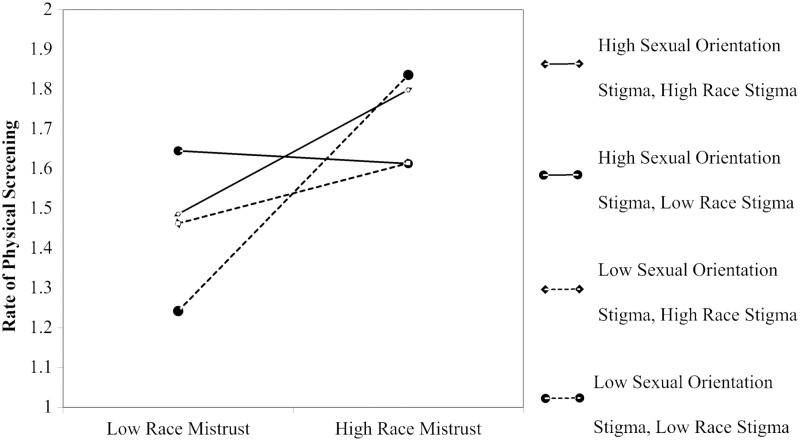
Results for engagement in physical examinations indicate that higher rates of race-based medical mistrust independently predicted significantly lower rates of engagement in physical examinations (RR: 3.964, 95% CI: 1.224–12.839; see Table 2 for complete GLM results). However, this main effect of race-based medical mistrust was qualified by significant two-way interactions with sexual orientation stigma (RR: 0.401, 95% CI: 0.161–1.000) and race-based stigma (RR: 0.486, 95% CI 0.254–0.929), in addition to a significant two-way interaction between race-based and sexual orientation stigma (RR: 0.364, 95% CI: 0.146–0.911). The race-based medical mistrust by race-based stigma and the sexual orientation stigma by race-based stigma interactions followed the same pattern; when both predictors were high, participants were multiplicatively significantly less likely to report recent engagement in physical examinations. The interaction between race-based medical mistrust and sexual orientation stigma shows that when participants reported higher rates of race-based medical mistrust, they were less likely to have engaged in recent physical examinations regardless of their level of sexual orientation stigma. Perceiving higher rates of sexual orientation stigma in the absence of race-based medical mistrust, however, was still associated with less recent engagement in physical examinations.
Table 2.
Generalized Linear Model Relative Rate and 95% Confidence Interval Results for Medical Mistrust, Stigma, and Engagement in Care Behaviors Among Black Women Who Have Sex with Women
| Parameter | Last time had a physical examination, RR (95% CI) | Last time had blood pressure checked, RR (95% CI) |
|---|---|---|
| Global mistrust | 1.053 (0.899–1.234) | 0.909 (0.821–1.007) |
| Race-based medical mistrust | 3.964 (1.224–12.839)* | 1.651 (0.771–3.534) |
| Sexual orientation stigma | 5.611 (0.842–37.370) | 3.441 (1.008–11.751)* |
| Race-based stigma | 3.626 (0.878–14.983) | 1.851 (0.739–4.641) |
| Race-based medical mistrust × sexual orientation stigma | 0.401 (0.161–1.000)* | 0.624 (0.345–1.128) |
| Sexual orientation stigma × race-based stigma | 0.364 (0.146–0.911)* | 0.532 (0.294–0.964)* |
| Race-based medical mistrust × race-based stigma | 0.486 (0.254–0.929)* | 0.788 (0.518–1.198) |
| Race-based medical mistrust × sexual orientation stigma × race-based stigma | 1.765 (1.116–2.791)* | 1.342 (0.997–1.806) |
P < 0.05; **P < 0.01; ***P < 0.001.
CI, confidence interval; RR, relative rate.
These significant two-way interactions were all qualified by a significant three-way interaction between race-based medical mistrust, sexual orientation stigma, and race-based stigma (RR: 1.765, 95% CI 1.116–2.791). Overall, high race-based medical mistrust remained significantly related to less recent physical examinations. BWSW who reported high race-based medical mistrust, even in the absence of sexual orientation and race-based stigma, were less likely to have engaged in recent physical examinations at rates comparable to those reported by participants who were high on all three variables (i.e., race-based medical mistrust, sexual orientation stigma, and race-based stigma). High race-based medical mistrust with high race-based stigma (with or without high sexual orientation stigma) was also related to less recent engagement in physical examinations. Conversely, individuals who were low on all three measures (race-based medical mistrust, race-based stigma, and sexual orientation stigma), as expected, had engaged in physical examinations more recently (Fig. 1).
FIG. 1.
Three-way interaction between race-based medical mistrust, race-based stigma, and sexual orientation stigma predicting engagement in physical examinations. Note: Engagement in care—physical examination response scale: 1 = in the past 6 months; 5 = more than 5 years ago.
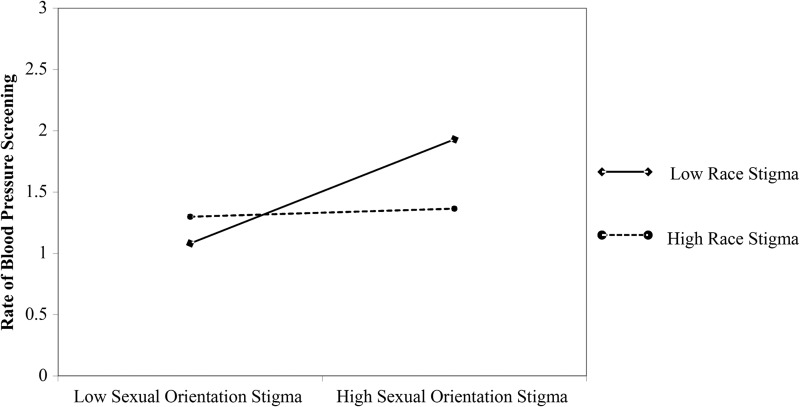
The results of our second model suggest a significant relationship between sexual orientation stigma and less recent engagement in blood pressure screenings (RR: 3.441, 95% CI 1.008–11.751). No significant main effects emerged for global medical mistrust, race-based medical mistrust, or race-based stigma with engagement in these screenings. However, a significant interaction between race-based stigma and sexual orientation stigma (RR: 0.532, 95% CI 0.294–0.964) demonstrated that in the absence of race-based stigma, participants who perceived higher levels of sexual orientation stigma reported significantly less recent engagement in blood pressure screenings (Fig. 2).
FIG. 2.
Two-way interaction between race-based stigma and sexual orientation stigma predicting engagement in blood pressure screening. Note: Engagement in care—blood pressure screening response scale: 1 = in the past 6 months; 5 = more than 5 years ago.
Discussion
These novel findings build on the existing literature not only by detailing recent trends in BWSW's EIC but also by providing the first empirical assessment of how experiencing these forms of stigma and medical mistrust independently and interactively relate to the frequency with which BWSW obtain routine healthcare. The findings contribute to the literature by documenting relatively high rates of EIC and low rates of experienced stigma, while also warning about the significant and multiplicative effects of stigma and medical mistrust on EIC.
A majority of participants reported having a physical examination or blood pressure check during the past year. This exceeds the reported average rates at which the general U.S. population received an annual preventive examination between 2002 and 2010.29 These unexpected rates of EIC may be an indicator of successful health policy, or potentially an artifact of our measures or sample (discussed below). However, despite overall frequent EIC, psychosocial barriers were still evident and significantly deterred participants' likelihood of undergoing routine care in the past year.
Of note, race-based medical mistrust was markedly prevalent among our sample. High levels of race-based medical mistrust were significantly associated with less EIC. Notably, even in the absence of race-based stigma, race-based medical mistrust related to less recent EIC. This finding underscores the critical need for novel approaches to patient care in which care providers and institutions work to repair the well-established and long-lasting damaged relationship between Black people and the healthcare system. Increasing the multicultural competency of healthcare providers through mandated coursework that addresses these topics and encouraging these individuals to gain exposure to diverse populations through direct patient interactions, could decrease the prevalence of race-based medical mistrust. Individual providers may also increase the frequency with which racial minorities interact with the healthcare industry by offering community-level services to provide opportunities for patient–provider interactions. Direct contact of this nature could increase the trust of racial minority patients in the healthcare system at large.
The prevalence of stigma was low in both measured domains. These outcomes are promising; however, they may be a result of sampling from a large metropolitan area with multiple active and out Black same gender-loving communities. Participants may be better able to find healthcare providers who are open to and affirming of both racial and sexual minority communities. Even with low rates, these results emphasize that stigma remains a significant determinant to EIC. Our findings demonstrate that experiencing sexual orientation stigma relates significantly to less frequent blood pressure screenings and this effect is exaggerated when an individual also experiences race-based stigma. Race-based and sexual orientation stigma also interacted with race-based medical mistrust to predict rates of EIC. Participants who experienced none-to-low race-based medical mistrust, race-based stigma, and sexual orientation stigma, most frequently obtained physical examinations, and did so at rates significantly higher than participants who reported any combination of stigma and race-based medical mistrust. For BWSW who face generally higher rates of stigmatization due to their multiple minority statuses, these findings are particularly disconcerting, indicating that their health-related needs are less likely to be met through routine healthcare than those of majority group members who do not face these psychosocial barriers. Inasmuch, due to the lack of research conducted with this population, future work must determine how these findings manifest across populations of BWSW from varied communities and backgrounds where greater variance in reported stigma and medical mistrust exists.
One additional major novel finding concerns a discrepancy in EIC that can be attributed to both stigma and medical mistrust. Our analyses revealed a disparity between participants who reported being comfortable talking about their sexual health with a care provider (91%) and those who said they actually had a care provider with whom they could talk about their sexual health (78%). This disconnect is concerning and ought to be made known to policy makers and care providers alike. While healthcare reform has helped to reduce the financial barrier to EIC recently, psychosocial barriers persist. Moving forward, healthcare providers must work actively with their patients to reduce patient mistrust of the healthcare community and deliver stigma-free care. This will help to create a healthcare environment in which patients feel comfortable seeking help from and engaging with providers about their sexual health. One way to accomplish this is by requiring healthcare programs to train future practitioners in how to engage patients in discussions about sensitive topics so that patients do not feel judged, stigmatized, or uncomfortable because of their race or sexual orientation. Achieving these aims could increase the quality of care that patients receive. Quality bedside manner is linked to better health outcomes, patient satisfaction, and making more appropriate medical decisions.30 Consequently, by requiring medical practitioners to become knowledgeable in taking sexual health histories, patients are apt to experience better health.
Limitations
One limitation of this study is that we utilized convenience sampling at a gay pride event. Accordingly, individuals who are reluctant to disclose their sexual orientation may not be accounted for in this sample, as they may have been less likely to attend such an event. Another limitation of this study that can be addressed in future research includes the operationalization of our variables. Multiple types of stigma were examined, but not the complex breakdown of each, including internalized, enacted, and anticipated stigma.31 Finally, our measure of EIC was limited to two routine items; measures of EIC that include assessing engagement and retention in healthcare, including sexual health, would provide a more comprehensive understanding of participants' routine healthcare behaviors. Future research should address these issues.
Conclusion
It is well established that WSW and Black women report lower rates of engagement in healthcare when compared to their heterosexual and Latina or White counterparts,32–34 which is reflected in the former subgroups' comparatively worse health outcomes.35–40 These findings suggest that BWSW's unique experiences with stigma and medical mistrust are likely contributing to these disparities in seeking care, even when care is clinically necessary. The emergence of new biomedical technologies that screen for and treat life threatening diseases and conditions has led to great advances in medical care, yet they are ineffective if patients are not under the care of medical practitioners to utilize these technologies. To more comprehensively and effectively address the varied psychosocial barriers to EIC and their related health disparities in populations such as BWSW, future research should address an intervention development that targets stigma and medical mistrust as barriers to EIC. This work has yet to be examined among BWSW and is sorely needed. Furthermore, identifying additional outcome variables that more fully account for the health-related disparities of BWSW in relation to race-based medical mistrust, and race-based and sexual orientation stigma, may provide beneficial means of promoting the health and well-being of this overlooked population.
In summary, the observed rates of medical mistrust are troubling and call for interventions specifically targeting this area among BWSW. Our findings can inform interventions to more effectively target the unique psychosocial barriers that differentially affect minority groups. In turn, we can make advances to eradicate health-related disparities among minority populations in the United States and thereby promote better health statuses for populations in need.
Acknowledgments
This project was supported by National Institute of Mental Health grant R01MH094230. The authors would like to thank Samantha Lawrence for her help with the preparation of this article.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Mittler JN, Martsolf GR, Telenko SJ, Scanlon DP: Making sense of “consumer engagement” initiatives to improve health and health care: A conceptual framework to guide policy and practice. Milbank Q 2013;91:37–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agency for Healthcare Research and Quality: 2014 National Healthcare Quality & Disparities Report. Rockville, MD: Agency for Healthcare Research and Quality, 2015. [AHRQ Pub. No. 15-0007] [Google Scholar]
- 3.U.S. Department of Health and Human Services: Office of Disease Prevention and Health Promotion. Healthy People 2020. Available at www.healthypeople.gov/2020/default.aspx Accessed November17, 2016
- 4.Eaton LA, Driffin DD, Kegler C, et al. : The role of stigma and medical mistrust in the routine health care engagement of black men who have sex with men. Am J Public Health 2015;105:e75–e82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Makadon HJ, Mayer KH, Garofalo R: Optimizing primary care for men who have sex with men. JAMA 2006;296:2362–2365 [DOI] [PubMed] [Google Scholar]
- 6.Paradies Y: A systematic review of empirical research on self-reported racism and health. Int J Epidemiol 2006;35:888–901 [DOI] [PubMed] [Google Scholar]
- 7.Steele LS, Tinmouth JM, Lu A: Regular health care use by lesbians: A path analysis of predictive factors. Fam Pract 2006;23:631–636 [DOI] [PubMed] [Google Scholar]
- 8.Wailoo K: Stigma, race, and disease in 20th century America. Lancet 2006;367:531–533 [DOI] [PubMed] [Google Scholar]
- 9.Williams DR, Mohammed SA: Discrimination and racial disparities in health: Evidence and needed research. J Behav Med 2009;32:20–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care; Smedley BD, Stith AY, Nelson AR, editors: Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press, 2003, p 764. [PubMed] [Google Scholar]
- 11.Pachankis JE: The psychological implications of concealing a stigma: A cognitive-affective-behavioral model. Psychol Bull 2007;133:328–345 [DOI] [PubMed] [Google Scholar]
- 12.Pierre MS: Under what conditions do lesbians disclose their sexual orientation to primary healthcare providers? A review of the literature. J Lesbian Stud 2012;16:199–219 [DOI] [PubMed] [Google Scholar]
- 13.Austin EL: Sexual orientation disclosure to health care providers among urban and non-urban southern lesbians. Women Health 2013;53:41–55 [DOI] [PubMed] [Google Scholar]
- 14.LaVeist TA, Isaac LA, Williams KP: Mistrust of health care organizations is associated with underutilization of health services. Health Serv Res 2009;44:2093–2105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Musa D, Schulz R, Harris R, et al. : Trust in the health care system and the use of preventive health services by older black and white adults. Am J Public Health 2009;99:1293–1299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Caterinicchio RP: Testing plausible path models of interpersonal trust in patient-physician treatment relationships. Soc Sci Med Med Psychol Med Sociol 1979;13A:81–99 [DOI] [PubMed] [Google Scholar]
- 17.Thorne SE, Robinson CA: Reciprocal trust in health care relationships. J Adv Nurs 1988;13:782–789 [DOI] [PubMed] [Google Scholar]
- 18.Thom DH, Campbell B: Patient-physician trust: An exploratory study. J Fam Pract 1997;44:169–177 [PubMed] [Google Scholar]
- 19.LaVeist TA, Nickerson KJ, Bowie JV: Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Med Care Res Rev 2000;57(Suppl 1):146–161 [DOI] [PubMed] [Google Scholar]
- 20.Hall MA, Dugan E, Zheng B, Mishra AK: Trust in physicians and medical institutions: What is it, can it be measured, and does it matter? Milbank Q 2001;79:613–639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sheppard VB, Mays D, LaVeist T, Tercyak KP: Medical mistrust influences black women's level of engagement in BRCA 1/2 genetic counseling and testing. J Natl Med Assoc 2013;105:17–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dryden R, Williams B, McCowan C, Themessl-Huber M: What do we know about who does and does not attend general health checks? Findings from a narrative scoping review. BMC Public Health 2012;12:723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eaton LA, Kalichman SC, Cherry C: Sexual partner selection and HIV risk reduction among black and white men who have sex with men. Am J Public Health 2010;100:503–509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eaton L, West T, Kenny D, Kalichman S: HIV transmission risk among HIV seroconcordant and serodiscordant couples: Dyadic processes of partner selection. AIDS Behav 2009;13:185–195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mugavero MJ, Davila JA, Nevin CR, Giordano TP: From access to engagement: Measuring retention in outpatient HIV clinical care. AIDS Patient Care STDS 2010;24:607–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xu F, Mawokomatanda T, Flegel D, et al. : Surveillance for certain health behaviors among states and selected local areas—Behavioral Risk Factor Surveillance System, United States, 2011. MMWR Surveill Summ 2014;63:1–149 [PubMed] [Google Scholar]
- 27.Delgado J, Jacobs EA, Lackland DT, et al. : Differences in blood pressure control in a large population-based sample of older African Americans and non-Hispanic whites. J Gerontol A Biol Sci Med Sci 2012;67:1253–1258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thompson HS, Valdimarsdottir HB, Winkel G, et al. : The group-based medical mistrust scale: Psychometric properties and association with breast cancer screening. Prev Med 2004;38:209–218 [DOI] [PubMed] [Google Scholar]
- 29.Mehrotra A, Prochazka A: Improving value in health care—Against the annual physical. N Engl J Med 2015;373:1485–1487 [DOI] [PubMed] [Google Scholar]
- 30.Zeldow PB, Makoul G: Communicating with patients. In: Behavior & Medicine. Edited by Wedding D, Stuber ML. Boston, MA: Hogrefe & Huber Publishers, 2006. pp 201–218 [Google Scholar]
- 31.Clement S, Schauman O, Graham T, et al. : What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med 2015;45:11–27 [DOI] [PubMed] [Google Scholar]
- 32.Charlton BM, Corliss HL, Missmer SA, et al. : Reproductive health screening disparities and sexual orientation in a cohort study of US adolescent and young adult females. J Adolesc Health 201;49:505–510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dahlhamer JM, Galinsky AM, Joestl SS, Ward BW: Barriers to health care among adults identifying as sexual minorities: A US national study. Am J Public Health 2016;106:1116–1122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Frost JJ: U.S. Women's Use of Sexual and Reproductive Health Services: Trends, Sources of Care and Factors Associated with Use, 1995–2010. New York: Guttmacher Institute, 2013. Available at www.guttmacher.org/pubs/sources-of-care-2013.pdf Accessed November18, 2016 [Google Scholar]
- 35.Ward BW, Dahlhamer JM, Galinsky AM, Joestl SS: Sexual orientation and health among US adults: National Health Interview Survey, 2013. Natl Health Stat Rep 2014;77:1–10 [PubMed] [Google Scholar]
- 36.Agénor M: What are the numbers? The epidemiology of cancer by sexual orientation and gender identity. In: Cancer and the LGBT Community: Unique Perspectives from Risk to Survivorship. Edited by Boehmer U, Cham Elk R., Switzerland: Springer International Publishing, 2015, pp 117–140 [Google Scholar]
- 37.Centers for Disease Control and Prevention: CDC Health Disparities and Inequalities Report—United States, 2013. MMWR Morb Mortal Wkly Rep 2013;62(Suppl 3):53–91 [PubMed] [Google Scholar]
- 38.Lick DJ, Durso LE, Johnson KL: Minority stress and physical health among sexual minorities. Perspect Psychol Sci 2015;8:521–548 [DOI] [PubMed] [Google Scholar]
- 39.Molina Y, Lehavot K, Beadnell B, Simoni J: Racial disparities in health behaviors and conditions among lesbian and bisexual women: The role of internalized stigma. LGBT Health 2014;1:131–139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Przedworski JM, McAlpine DD, Karaca-Mandic P, VanKim NA: Health and health risks among sexual minority women: An examination of 3 subgroups. Am J Public Health 2014;104:1045–1047 [DOI] [PMC free article] [PubMed] [Google Scholar]