Abstract
Background: We sought to assess the association between age and the prevalence of obesity among children with and without autism spectrum disorder (ASD) in the 2011–2012 National Survey of Children's Health.
Methods: Analyses were restricted to 43,777 children, ages 10–17, with valid measures of parent-reported weight, height, and ASD status. Exploratory analyses describe the impact of sex, race/ethnicity, and household income on the relationship between age and obesity in ASD.
Results: Although the overall prevalence of obesity among children with ASD was significantly (p < 0.001) higher than among children without ASD (23.1% vs. 14.1%, 95% confidence interval for difference 3.6 to 14.4), child age significantly (p = 0.035) modified this difference. In a multivariable logistic regression analysis, adjusted for sex, race/ethnicity, and household income, the odds of obesity among children with ASD compared with children without ASD increased monotonically from ages 10 to 17 years. This pattern arose due to a consistently high prevalence of obesity among children with ASD and a decline in prevalence with advancing age among children without ASD. These findings were replicated using a propensity score analysis. Exploratory analyses suggested that the age-related change in obesity disparity between children with and without ASD may be further modified by sex, race/ethnicity, and household income.
Conclusions: The patterns of prevalence observed with increasing age among children with and without ASD were unexpected. A better understanding of the etiological and maintenance factors for obesity in youth with ASD is needed to develop interventions tailored to the specific needs of these children.
Keywords: : obesity, disability, racial/ethnic disparities, health disparities, epidemiology
Background
Childhood obesity has been called a pandemic because its prevalence has increased across all child demographic subgroups.1 Since 1980, obesity rates in the United States have tripled among children, ages 6–11, and quadrupled among adolescents2; 2012 estimates indicate that more than one-third of children and adolescents are overweight or obese. Although the problem is ubiquitous, groups at high risk for obesity have been identified based on race/ethnicity, income, and disability status.3,4 African American and Hispanic and low-income children have higher obesity prevalence than their counterparts without these characteristics.5,6 Children with developmental disabilities (DD), including those with autism spectrum disorder (ASD), also appear to be at elevated risk for obesity.7–10
ASD is a developmental disorder that is characterized by persistent social impairments, verbal and nonverbal communication difficulties, and restrictive and repetitive patterns of behaviors, activities, and/or interests11 that frequently become evident by 3 years of age and are typically diagnosed by 5 years of age.12 In the most recent CDC survey, 1 in 68 (1.47%) 8-year-old US children have been diagnosed with ASD.13
The etiology of obesity is complex and multifactorial, but at the most basic level, obesity arises from positive energy imbalance, where calories consumed exceed those expended to support basal metabolism, activity, and growth. Children with ASD often exhibit selective eating, frequently resulting in low intakes of fruits and vegetables with ASD and high intakes of calorically dense foods.14–17 As youth age, they are more likely to have access to more energy-dense snacks and less engagement in physical activity compared with the peers without ASD,18 and their physical activity levels decline with age.19,20
Parents of children with ASD report using television for its calming effect,21 which may contribute to high levels of sedentary behavior. Our own work has demonstrated that screen time is greater in children with ASD than their typically developing peers.22 Finally, the proportion of youth with ASD who are treated with atypical antipsychotics and other psychotropic medications associated with weight gain increases with age. To the extent that these pathways may contribute to positive energy balance for children with ASD, it might be expected that these children would experience increases in adiposity over time, resulting in the prevalence of obesity increasing with age.
Estimates of the prevalence of overweight and obesity in children with ASD based on national samples are limited and have only examined the impact of age in broad categories. In the United States, obesity in children is defined as BMI-for-age ≥95th percentile, using reference data from the Centers for Disease Control's National Center for Health Statistics.23 The large National Survey of Children's Health (NSCH) is one of the few nationally representative surveys of adequate size to estimate the prevalence of obesity in children with developmental disabilities. Using data from the 2003 NSCH, Curtin et al. found that 30% of children with ASD, ages 3–17, were obese compared with 24% of children without ASD, reflecting an unadjusted 40% elevation in risk.10 Several research groups have reported elevated obesity prevalence using data from the more recent 2011–2012 NSCH. Youth with ASD, ages 10–17 years, were found to have significantly elevated risks of obesity (24% in ASD vs. 16% non-ASD) in unadjusted analyses.24 Using the same dataset, but a slightly different approach, McCoy et al. found obesity prevalence of 22.2% in children with ASD compared with 14.1% in children without ASD.25 In addition, using NSCH 2011–2012, but including a broader age range of children 6–17 years, Corvey et al. reported that the observed elevation in obesity prevalence disappeared after accounting for comorbid disorders and medication use.18
The prevalence of obesity has also been estimated from clinical samples. Using their common registry protocol and measured heights and weights, the Autism Speaks Autism Treatment Network (ATN) estimated obesity prevalence in children aged 2–17 years from 19 sites in the United States and Canada between 2008 and 2013. They reported an obesity prevalence of 18% in children with ASD compared with nationally representative estimates of 16.7% in the population overall; this difference was not statistically significant. However, child age strata revealed significant elevations in obesity prevalence for children aged 2–5 and 12–17 years compared with those age groups in the overall population based on the US National Health and Nutrition Examination Survey (NHANES).26 The large Partners HealthCare System Research Patient Database Repository (RPDR) provides data from 2075 patients with ASD (2008–2011), with estimated obesity prevalence in children aged 2–20 years of 23.2%.8 Compared with children aged 6–11 years, odds of obesity were higher and similar in children aged 12–15 and 16–20 years.8 Smaller retrospective clinical chart reviews arrive at similar obesity prevalence estimates of 21.9%27 and 19% in children with ASD.28
Despite the well-established and striking differences in obesity prevalence among children in the general population by race/ethnicity and socioeconomic status, scant data are available for race/ethnic or sociodemographic subgroups with ASD. Clinical data from the ATN indicate that compared with white children with ASD, Hispanic children with ASD have twice the prevalence of overweight/obesity.29 In black children, odds were elevated by 50% compared with whites, but only in unadjusted analyses. Elevated obesity risk in Hispanic youth was also noted in the RPDR patient database where, in unadjusted analyses, Hispanic children with ASD had almost twice the odds of both overweight and obesity compared with children without ASD.8 This latter study also identified increased odds of overweight/obesity associated with public rather than private insurance, even after adjustment for race/ethnicity. Given the co-occurrence of racial minority status with poverty in the United States, such adjustment may mask important population phenomena.
The release of the 2011–2012 wave of the NSCH provided an opportunity to examine the prevalence of obesity relative to age and to explore whether sociodemographic factors influenced any age-related findings using the most recent nationally representative US data available. We hypothesized that disparities in the prevalence of obesity between 10- to 17-year-old children with and without ASD would increase with age due to increases in obesity prevalence with age among children with ASD. We also conducted exploratory analyses to identify sociodemographic factors that might contribute to any age-related increase in obesity. We also expected that age-related obesity disparities might be greater in boys and in nonwhite and lower income groups.
Methods
For the present study, we analyzed data from the 2011–2012 NSCH, a nationally representative survey conducted by the CDC National Center for Health Statistics.30 The survey screened households for the presence of children aged 0–17 years, and one child was randomly selected to be the subject of the telephone survey. The questions were answered by a parent or guardian in the household who indicated that they had knowledge of the child's health. The overall response rate for 2011–2012 was 23.0%. A total of 95,677 parent interviews were completed from February 2011 through June 2012. Additional information about NSCH, including its sample design, data collection procedures, and questionnaire content, is available at www.cdc.gov/nchs/slaits/nsch.htm. This public-use data set is available through the Data Resources Center for Child and Adolescent Health (www.childhealthdata.org).30 The IRB at Tufts University confirmed that these publicly available deidentified data constituted nonhuman subject research and thus the study was deemed exempt.
Assessment of ASD Status
Parent confirmation that their child was currently diagnosed with ASD was based on responses to two separate survey questions. Parents were first asked if they had ever been told by a doctor or other healthcare provider that their child had autism, Asperger's disorder, pervasive developmental disorder, or other autism spectrum disorder. Parents who answered yes to this question were given a follow-up question: “Does the child currently have autism or autism spectrum disorder?” In this analysis, only children whose parents answered yes to both questions are included in the current ASD category. Parents who answered yes to the first question, but indicated that their child does not currently have ASD (n = 190) were combined with parents who answered no. Reasons for the change in diagnosis included changes in behaviors or symptoms, the condition improved on its own or with treatment, or the healthcare provider changed the diagnosis.
Assessment of Weight Status
The public-use data file for NSCH 2011–2012 includes a BMI classification variable, with children identified as underweight (<5th percentile BMI-for-age), healthy weight (5th to <85th percentile BMI-for-age), overweight (85th to <95th percentile BMI-for-age), or obese (≥95th percentile BMI-for-age) using the CDC 2000 growth reference.31 BMI-for-age was calculated using parent-reported height, weight, and age (calculated from date of birth and interview date). The child's age in months was used to calculate BMI-for-age. However, because the NSCH reports the age in years only, all children were assumed (by NSCH) to be at the midpoint of their age-year for this calculation. BMI classifications for children under 10 years of age were not provided by NSCH in the public-use data set because parent-reported data at ages less than 10 are not sufficiently accurate to estimate obesity prevalence.32 The primary binary outcome used in the present study is obesity, which was created by comparing those children identified as obese using BMI-for-age (≥95 percentile) with all other children, the nonobese (underweight, normal weight, overweight).
Assessment of Sociodemographic Characteristics
As indicated above, age is reported in integer years. The race/ethnicity variable provided in the public-use data set classifies children as follows: Hispanic; non-Hispanic white; non-Hispanic black; and other non-Hispanic. Because of small sample sizes in many states, non-Hispanic children reporting only one race category of Asian, American Indian, Alaska Native, Native Hawaiian, or Pacific Islander or who are more than one race (multiracial) are aggregated as other non-Hispanic. Non-Hispanic children who reported more than one race are categorized as other non-Hispanic. Children who were missing information on race (∼2% weighted percentage) were grouped with other non-Hispanic.
Socioeconomic status was based on an index of income relative to the Department of Health and Human Services Federal Poverty Guidelines [federal poverty level (FPL)], with missing values imputed using single imputation.33 Percentage (%) of FPL is then classified as 0%–99% FPL; 100%–199% FPL; 200%–399% FPL; and 400% FPL or more.
Statistical Analyses
All statistical analyses were carried out using the survey procedures in SAS 9.3 software (SAS Institute, Inc., Cary, NC), which are capable of handling complex sample design structures. Sampling weights that adjusted for survey nonresponse, noncoverage, and nontelephone households were provided in the NSCH public-use data set. As the focus of the primary analysis was on assessing the association between obesity and ASD in relation to age, individual standardized weights were calculated to correct erroneous weighted estimates that arose from analyzing strata with small sample sizes using the NSCH sampling weights. Individual standardized weights were calculated by multiplying the NSCH sampling weight variable by the ratio of the overall mean weight of the entire survey to the corresponding stratum-specific mean weight defined by age (eight categories), ASD status (two categories), and obesity status (two categories). Using this approach, the effects of extreme-valued NSCH sampling weights on the estimates in the smaller strata were lessened by shifting the extreme values toward the center of the overall distribution of sampling weights.
Chi-square tests were used to compare the prevalence of sociodemographic characteristics between children with and without ASD. Multivariable logistic regression was used to examine the relationships between obesity and participant characteristics. A cross-product term was included in the regression models to characterize the relationship between obesity and ASD by age, and a test for interaction was used to assess its significance. To examine the influence of other factors on the cross-product term, age, sex, racial/ethnic group, and household income were added to the model and their influence on the age coefficients was examined. Model accuracy was quantified using the c-statistic. Results are reported in terms of regression coefficients, adjusted prevalence, and adjusted odds ratios with corresponding 95% confidence intervals (CIs).
Given the observational nature of the study, the relationship between obesity and ASD by age was further assessed using a propensity score analysis to verify the results of the primary multivariable-adjusted analysis. The propensity of being a child with ASD was estimated using logistic regression analysis by including age, sex, racial/ethnic group, and household income as covariates in the model. The propensity score was then used to perform a nine-digit match of one child with ASD to three children without ASD using a greedy matching algorithm.34 The resulting propensity-matched sample consisted of 3700 children, 925 with ASD and 2775 without ASD.
In exploratory analyses, we sought to elucidate the role of sex, race/ethnicity, and household income on the pattern of age-related prevalence using likelihood ratio tests. Sample size limitations dictated further aggregation to dichotomized categories consisting of white non-Hispanic vs. nonwhite/Hispanic and household income of <200% FPL vs. 200% or more FPL.
Results
A total of 45,217 children between the ages of 10–17 years had information on ASD status and 43,864 had parent-reported weight status, resulting in 43,777 children with information on both ASD and weight status available for analysis. Overall, the prevalence of ASD among children aged 10–17 years was 2.11% (95% CI: 1.82 to 2.41) or about 1 in 47. As expected, a greater proportion of children with ASD were male (83.7% of children with ASD vs. 50.5% non-ASD, p < 0.001, Table 1). Children with ASD were significantly less likely to reside in a household with incomes <100% FPL (11.7% vs. 18.3%, p < 0.01). Children with ASD were slightly younger than those without ASD (mean age 13.3 vs. 13.7 years, respectively, p = 0.04). Differences in the race/ethnicity distribution of children with and without ASD were of borderline significance (p = 0.07), with children with ASD more likely to be white (63.2% vs. 55.5%).
Table 1.
Participant Characteristics by Group
| Full sample (n = 43,777) | Propensity score-matched sample (n = 3700) | |||||||
|---|---|---|---|---|---|---|---|---|
| With ASD n = 925 | Without ASD n = 42,852 | Difference (95% CI) | p-value | With ASD n = 925 | Without ASD n = 2775 | Difference (95% CI) | p-value | |
| Obese weight status (%) | 23.1 | 14.1 | 9.0 (3.6 to 14.4) | <0.001 | 23.1 | 15.6 | 7.5 (1.4 to 13.6) | 0.01 |
| Age, mean (standard error) | 13.3 (0.17) | 13.7 (0.03) | −0.4 (−0.7 to −0.02) | 0.04 | 13.3 (0.17) | 13.4 (0.11) | −0.1 (−0.5 to 0.3) | 0.76 |
| Male sex (%) | 83.7 | 50.5 | 33.2 (28.7 to 37.8) | <0.001 | 83.7 | 80.5 | 3.2 (−2.3 to 8.8) | 0.27 |
| Racial/ethnic group (%) | ||||||||
| White, non-Hispanic | 63.2 | 55.5 | 7.7 (0.0 to 15.5) | 0.07 | 63.2 | 68.6 | −5.4 (−14.0 to 3.3) | 0.22 |
| Black, non-Hispanic | 9.2 | 14.3 | −5.1 (−9.3 to −1.0) | 9.2 | 7.7 | 1.5 (−3.2 to 6.1) | ||
| Hispanic | 20.1 | 18.7 | 1.4 (−6.6 to 9.4) | 20.1 | 14.1 | 6.0 (−2.5 to 14.6) | ||
| Multiracial/other, non-Hispanic/missing | 7.5 | 11.5 | −4.0 (−7.0 to −1.1) | 7.5 | 9.6 | −2.1 (−6.1 to 1.8) | ||
| Household income (%) | ||||||||
| <100% FPL | 11.7 | 18.3 | −6.6 (−10.0 to −3.1) | 0.01 | 11.7 | 20.3 | −8.6 (−13.5 to −3.7) | 0.01 |
| 100%–199% FPL | 19.7 | 21.0 | −1.3 (−6.5 to 3.9) | 19.7 | 22.2 | −2.5 (−8.8 to 3.8) | ||
| 200%–399% FPL | 37.7 | 29.4 | 8.3 (0.8 to 15.8) | 37.7 | 33.1 | 4.6 (−3.7 to 12.9) | ||
| 400% or more FPL | 30.9 | 31.3 | −0.4 (−6.8 to 5.9) | 30.9 | 24.4 | 6.5 (−0.7 to 13.6) | ||
| Racial/ethnic group (%) | ||||||||
| White, non-Hispanic | 63.2 | 55.5 | 7.7 (0.0 to 15.5) | 0.06 | 63.2 | 68.6 | −5.4 (−14.2 to 3.4) | 0.22 |
| Nonwhite/Hispanic | 36.8 | 44.5 | −7.7 (−15.5 to 0.0) | 36.8 | 31.4 | 5.4 (−3.4 to 14.2) | ||
| Household income (%) | ||||||||
| <200% FPL | 31.4 | 39.2 | −7.8 (−13.9 to −1.8) | 0.01 | 31.4 | 42.5 | −11.1 (−18.3 to −3.8) | 0.003 |
| 200% or more FPL | 68.6 | 60.8 | 7.8 (1.8 to 13.9) | 68.6 | 57.5 | 11.1 (3.8 to 18.3) | ||
ASD, autism spectrum disorder; CI, confidence interval; FPL, federal poverty level.
The prevalence of obesity among children with ASD aged 10–17 years was 23.1% compared with 14.1% in children without ASD (Table 1). In both groups of children, prevalence differed by sex. Among children with ASD, the prevalence of obesity for boys was 25.3% and for girls 12.2% (p = 0.056). Among children without ASD, the prevalence of obesity was 16.6% and 11.7% (p < 0.001), respectively.
Table 2 displays the results from the unadjusted multivariable logistic regression model, which included only a cross-product term between ASD and age, and an adjusted model that included age, sex, racial/ethnic group, and household income as additional covariates. The c-statistic suggests that the adjusted model is more accurate than the unadjusted model. Moreover, including sex, racial/ethnic group, and household income not only changed the values of the regression coefficients markedly but also the test for interaction became statistically significant (p = 0.035).
Table 2.
Regression Coefficients Relating Autism Spectrum Disorder and Age to Obesity Status from Three Models
| Unadjusted modela | Adjusted modelb | Propensity score-matched model | |
|---|---|---|---|
| Intercept | −1.3312 | −2.2975 | −1.1762 |
| ASD | 0.1618 | 0.0601 | 0.0069 |
| Age | −0.1389 | −0.1371 | −0.1672 |
| Interaction: ASD × age | 0.1294 | 0.1552 | 0.1576 |
| p-value for interaction | 0.062 | 0.035 | 0.061 |
| c-statistic | 0.59 | 0.68 | 0.59 |
No other factors in model.
Adjusted for sex, racial/ethnic group, and household income.
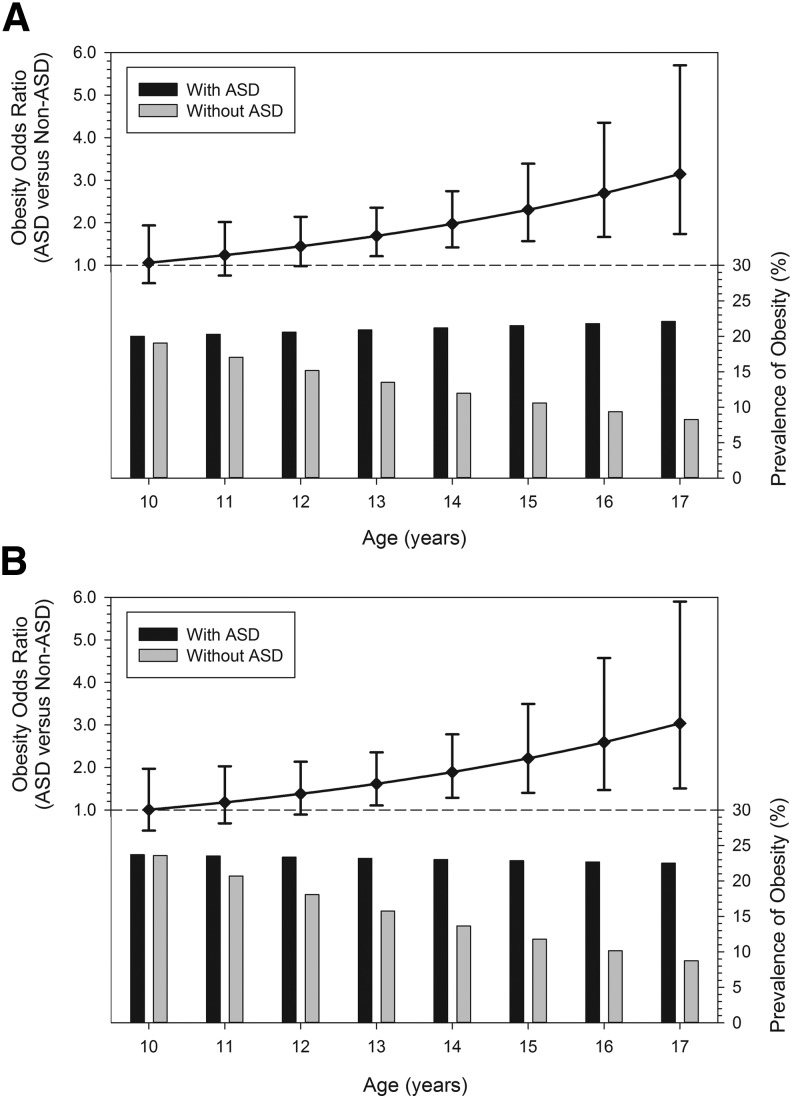
The results from the adjusted model are illustrated in Figure 1A in terms of odds ratios and prevalence of obesity. Although the prevalence of obesity remained relatively constant across the ages among children with ASD, the prevalence of obesity in children without ASD decreased with age. At age 10, there was relatively little difference in obesity prevalence between the two groups (20.0% vs. 19.1%), whereas at age 17, the prevalence in the ASD group was almost three times as high as in the non-ASD group (22.1% vs. 8.3%) (Table 3, Overall row). As a result of the contrasting patterns of prevalence, the odds ratio for obesity among children with ASD from age 10 to age 17 increased monotonically and significantly, relative to children without ASD, from 1.06 to 3.15 (Table 3, Overall row, and Figure 1A, p = 0.035 test for interaction).
Figure 1.
Relationship between ASD, obesity status, and age from (A) an adjusted multivariable logistic regression model and (B) a propensity score-matched model. The top portion shows the odds of obesity for children with ASD relative to those without ASD at each age between 10 and 17 years, with corresponding 95% confidence intervals. The bottom portion shows the prevalence of obesity for children with and without ASD for each age between 10 and 17 years. The test of interaction between ASD and age was statistically significant for the adjusted multivariable logistic regression model (p = 0.035), but not for the propensity score-matched model (p = 0.062). The adjusted multivariable logistic regression model results correspond to the model shown in Table 2 and the Overall row shown in Table 3. ASD, autism spectrum disorder.
Table 3.
Odds Ratios, Prevalence, and Differences in Prevalence of Obesity of Children with Autism Spectrum Disorder Vs. Children without Autism Spectrum Disorder by Child Age, According to Categories of Sex, Race/Ethnicity, and Household Income
| Age of child (years) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Odds ratio ASD vs. non-ASD (%) Difference (%) |
10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 |
| Overall | 1.06 | 1.24 | 1.45 | 1.69 | 1.98 | 2.31 | 2.69 | 3.15 |
| 20.0 vs. 19.1 | 20.3 vs. 17.0 | 20.6 vs. 15.2 | 20.9 vs. 13.5 | 21.2 vs. 12.0 | 21.5 vs. 10.6 | 21.8 vs. 9.4 | 22.1 vs. 8.3 | |
| 0.9 | 3.3 | 5.4 | 7.4 | 9.2 | 10.9 | 12.4 | 13.8 | |
| Male | 1.16 | 1.34 | 1.55 | 1.80 | 2.08 | 2.41 | 2.79 | 3.23 |
| 23.8 vs. 21.2 | 24.5 vs. 19.5 | 25.2 vs. 17.8 | 25.8 vs. 16.2 | 26.6 vs. 14.8 | 27.3 vs. 13.5 | 28.0 vs. 12.2 | 28.8 vs. 11.1 | |
| 2.6 | 5.0 | 7.4 | 9.6 | 11.8 | 13.8 | 15.8 | 17.7 | |
| Female | 1.22 | 1.18 | 1.14 | 1.10 | 1.06 | 1.03 | 0.99 | 0.96 |
| 21.0 vs. 17.9 | 17.7 vs. 15.4 | 14.9 vs. 13.3 | 12.4 vs. 11.4 | 10.3 vs. 9.8 | 8.6 vs. 8.4 | 7.1 vs. 7.1 | 5.8 vs. 6.0 | |
| 3.1 | 2.3 | 1.6 | 1.0 | 0.6 | 0.2 | 0.0 | −0.2 | |
| White, non-Hispanic | 1.25 | 1.44 | 1.65 | 1.90 | 2.18 | 2.51 | 2.89 | 3.31 |
| 17.9 vs. 14.8 | 18.6 vs. 13.7 | 19.3 vs. 12.6 | 20.0 vs. 11.6 | 20.7 vs. 10.7 | 21.5 vs. 9.8 | 22.3 vs. 9.1 | 23.1 vs. 8.3 | |
| 3.1 | 4.9 | 6.7 | 8.4 | 10.0 | 11.7 | 13.3 | 14.8 | |
| Nonwhite/Hispanic | 1.01 | 1.13 | 1.27 | 1.42 | 1.60 | 1.80 | 2.02 | 2.27 |
| 25.3 vs. 25.2 | 24.2 vs. 22.0 | 23.2 vs. 19.2 | 22.2 vs. 16.6 | 21.2 vs. 14.4 | 20.2 vs. 12.3 | 19.3 vs. 10.6 | 18.5 vs. 9.1 | |
| 0.1 | 2.2 | 4.0 | 5.5 | 6.8 | 7.9 | 8.7 | 9.4 | |
| <200% FPL | 0.99 | 1.20 | 1.45 | 1.74 | 2.11 | 2.55 | 3.08 | 3.73 |
| 27.9 vs. 28.1 | 28.7 vs. 25.2 | 29.4 vs. 22.4 | 30.2 vs. 19.9 | 30.9 vs. 17.5 | 31.7 vs. 15.4 | 32.5 vs. 13.5 | 33.3 vs. 11.8 | |
| −0.2 | 3.5 | 7.0 | 10.3 | 13.4 | 16.3 | 19.0 | 21.5 | |
| 200% or more FPL | 1.17 | 1.32 | 1.49 | 1.68 | 1.91 | 2.15 | 2.43 | 2.75 |
| 16.7 vs. 14.6 | 16.7 vs. 13.2 | 16.8 vs. 11.9 | 16.8 vs. 10.7 | 16.8 vs. 9.6 | 16.9 vs. 8.6 | 16.9 vs. 7.7 | 17.0 vs. 6.9 | |
| 2.1 | 3.5 | 4.9 | 6.1 | 7.2 | 8.3 | 9.2 | 10.1 | |
The greedy matching algorithm using propensity scores yielded similar distributions of sociodemographic characteristics between children with and without ASD. The prevalence of obesity among children with ASD remained significantly higher compared with children without ASD (Table 1). The propensity score-matched sample confirmed the significance of the adjusted logistic regression results as the coefficients characterizing the relationship between obesity and ASD by age were similar (Table 2) and the odds ratios and prevalence of obesity mirrored those of the adjusted logistic regression model (Fig. 1B).
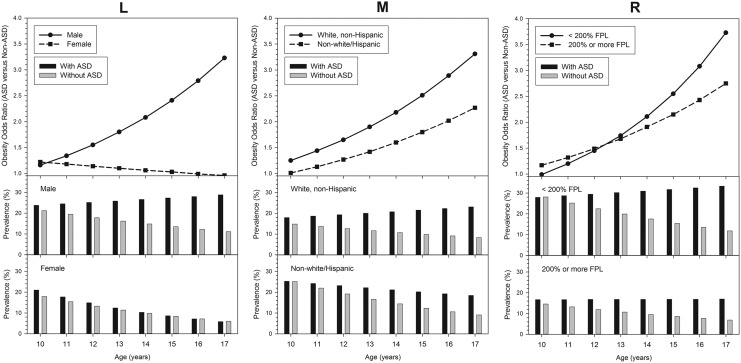
Exploratory analyses were conducted to determine whether the ASD status and age relationship varied as a function of sex, race/ethnicity, and household income relative to poverty (Fig. 2 and Table 3). The odds of obesity among children with ASD relative to children without ASD increased more dramatically across the age range for male children than it did for female children (p < 0.001). While the prevalence of obesity increased slightly with age among male children with ASD (from 23.8% at age 10 to 28.8% at age 17), it declined among the female children with ASD (from 21.0% at age 10 to 5.8% at age 17). For children without ASD, the prevalence of obesity declined with age for both sexes. The odds of obesity among children with ASD relative to children without ASD increased significantly across the age range for both racial/ethnic groups (p < 0.001). However, the prevalence of obesity increased with age among the white non-Hispanic children with ASD (from 17.9% to 23.1%), in contrast to a decline among the non-white/Hispanic children with ASD (from 25.3% to 18.5%). For children without ASD, the prevalence of obesity declined with age for both racial/ethnic groups. With regard to household income, the odds of obesity among children with ASD relative to children without ASD increased more steeply across the age range for children from households with lower income (<200% FPL) than for households with higher incomes (200% or more FPL), but did not reach statistical significance (p = 0.25). This is a reflection of the increase in obesity prevalence among children with ASD from lower household incomes (from 27.9% to 33.3%) relative to declines among lower income children without ASD (from 28.1% to 11.8%). In contrast, the prevalence of obesity was flat across the age range for higher income children with ASD, while it declined with age among children without ASD.
Figure 2.
Relationship between ASD, obesity status, and age stratified by sex (left panel, L), racial/ethnic Group (middle panel, M), and household income (right panel, R). The top portions show the odds of obesity for children with ASD relative to those without ASD at each age between 10 and 17 years by demographic category. The bottom portions show the prevalence of obesity for children with and without ASD for each age between 10 and 17 years by demographic category. The analyses were adjusted for sex, racial/ethnic group, and household income accordingly. The figures correspond to the rows of summary data shown in Table 3. The odds ratios across the age categories varied significantly between male and female children (p < 0.001), significantly between racial/ethnic groups (p < 0.001), but not significantly between household income categories (p = 0.25).
Discussion
In our analysis of the nationally representative data gathered as part of the NSCH 2011–2012, we found a significantly elevated prevalence of obesity among children with ASD aged 10–17 years (23.1%) compared with same-age peers without ASD (14.1%). The elevated obesity prevalence based on nationally representative samples in children with ASD compared with those without the condition has been previously reported by our group10 and others9,18,24,25,35 as well as in school-based and clinical samples.8,26–28,36 Chen et al. reported an obesity prevalence of 21.1% among 10–17-year-olds in the 2003 round of NSCH, similar to our estimates, and consistent with a leveling off in prevalence trends over time seen in other nationally representative samples of US children.2
We observed that the disparity in obesity between children with and without ASD increased with age. However, contrary to our hypothesis of increasing prevalence with age in children with ASD, the prevalence of obesity was quite consistent between ages 10 and 17 years. In contrast, obesity prevalence declined with advancing age from 10 to 17 years among children without ASD. Thus, the obesity disparity based on ASD status rose over adolescence due to decreasing obesity prevalence in those without ASD.
The limited number of pediatric studies that include height and weight data and have sample sizes large enough to examine prevalence of obesity by age is congruent with our finding of decreasing obesity with increasing age in typically developing adolescents. Specifically, analysis of the 2007 NSCH reported an obesity prevalence of 23% in 10–11-year-olds, monotonically decreasing to 13% in 16–17-year-olds.3 Analysis of data on Mexican American adolescents aged 12–19 years studied in the NHANES, 1999–2002, also indicated declining prevalence by age37; comparable data for other groups in NHANES have not been published. A large 2004–2005 study of almost 37,000 Brazilian school children with measured heights and weights also reported decreasing obesity prevalence across adolescence.38 In this latter study, using obesity definitions promulgated by the International Obesity Task Force,39 prevalence fell at each subsequent adolescent age studied, from 4.8% at age 10 to 1.2% at age 15.38 A second smaller cross-sectional study of ∼1500 Brazilian adolescents showed a similar pattern.40 The reasons for the age-related decline in obesity prevalence in typically developing adolescents are unclear. Identification of factors promoting healthy weight in teens without ASD might inform design of interventions for those with ASD.
Similarly, the factors contributing to the maintenance of high rates of obesity among children with ASD over the ages 10–17 are not established, but must reflect energy intake, energy expenditure, or both. Restricted dietary preferences may reflect core features of ASD and lead to energy-dense and nutrient-poor diets. In addition, as children with autism become adolescents, they are likely to have more access to energy-dense snacks and more autonomy in what they eat. On the energy intake side, atypical dietary intake patterns seen in autistic children may reflect core features of ASD, including sensory sensitivity and/or need for sameness, and behavioral rigidity. The use of food as a reward is a common practice with children with ASD and may contribute to excess energy intake.41,42 Several studies have documented nutrient inadequacy associated in children with ASD14,17,43 as well as lower intakes of fruits and vegetables.15,16,27 Mealtime stress represents an additional potential risk factor for the excess caloric intake associated with poor quality diets.44 Qualitative studies document high levels of parent stress related to the restricted diet and feeding behaviors of children with ASD.45 As autistic children become adolescents, parents may give in or give up on promoting healthful diets for their children.46 These mechanisms should be explored for their potential role in the maintenance of obesity in this population.
With respect to energy expenditure, it is likely that opportunities to engage in physical activity may decline as youth with ASD age. It may be easier to accommodate younger children with ASD in physical activities than it is to accommodate older youth. Typically, during the first decade of life, there are many occasional opportunities for physical play that do not have a competitive focus or require specific motor skills. In addition, there is often considerable adult emphasis on including everyone. In contrast, during the second decade, there is greater focus on competitive sports, which require consistent and extended practice, greater motor and social communication skills, and strong emotional regulation. Several studies document the individual/family-, social-, and community-level barriers to participation in physical activity faced by children with ASD.47–49 In our own work, poor motor skills, difficulty with social skills, limited friendships, and limited knowledge and training of service providers to accommodate the needs of children with ASD were highly cited as physical activity barriers.47 Lack of a peer exercise partner, parental time constraints, and transportation are cited as barriers as well.50 In addition, older children with ASD often are very fixated on electronics, which may reflect a specific restrictive interest, social isolation, a calming technique, or be used as a reward. As children with ASD get older and larger, parents may have more difficulty forcing them to engage in physical activities as well as preventing them from engaging in sedentary activities. Low total energy expenditure would be expected to result from lower levels of physical activity and high amounts of screen time. In our cross-sectional study of children with ASD, ages 3–11 years, BMI z-score was related both to total screen time and to total sedentary time on weekends.47
Our exploratory analyses of the impact of sex, race/ethnicity, and household income on the age-related obesity differences between children with and without ASD, while based on small numbers of children with ASD, also yielded some unanticipated findings. The obesity prevalence for boys with ASD increased slightly over the ages studied, while it decreased sharply in boys without ASD, resulting in a markedly increasing obesity disparity by autism status with age for boys. In contrast, in the limited number of girls included in our sample, there was a marked decline in obesity prevalence with age so that by age 17 there was no difference in obesity rates compared with girls without ASD. It will be important to determine if this finding can be replicated in future studies. If it is, a better understanding of the differences in eating, physical activity, and attitudes toward obesity in adolescent boys and girls with ASD may inform future interventions.
The preliminary observation that white non-Hispanic children with ASD experienced increases in obesity prevalence, while minority children with ASD and children without ASD in both race/ethnic groups experienced declines, was also unexpected and should be replicated in a larger sample and explored further.
The suggestion that the age-related obesity disparity among youth with ASD may be greater among lower income youth was surprising and also needs to be validated in a larger sample. One could speculate that low physical activity and high levels of sedentary behavior could reflect greater limitation of financial resources, with effects of lower energy expenditure that accumulate over time. It is also possible that with the increasing autonomy over food intake that occurs over adolescence together with the lower cost of energy-dense snack foods, lower household income could translate into calorie intakes that exceed energy expenditure. Qualitative approaches, such as key informant interviews or focus groups directly with youth and/or with their caregivers, could be used to advance understanding of the influence of these sex, race/ethnicity, and socioeconomic status factors and formulate specific hypotheses for further study and evaluation in programs and interventions.
Our study findings should be considered in the context of some limitations in our analyses. A cross-sectional design is not ideal to study age-related changes. Obesity status relied on parent-reported height and weight, which are subject to error. We restricted our analysis to children age 10 and greater, given a National Center for Health Statistics report that indicated parent report at these ages was fairly similar to measured values, whereas for children less than 10 years, parent-reported rates of obesity are often three- to fourfold higher than measured rates. However, even among the older age group, there appear to be smaller but systematic discrepancies. Specifically, parent report for youth aged 10–11 years overestimated obesity by ∼6%, whereas for youth aged 16–17 years, parent report underestimated obesity prevalence by ∼6%.32 It is possible that parents of children without ASD and parents of children with ASD differ in their accuracy in reporting their child's height and weight, which could bias our comparisons. In addition, because age is reported in integer years, some additional error arises due to the application of a mid-year age for determination of BMI-for-age percentiles for categorization of obesity status; this error would be expected to be random and have little effect on prevalence estimation. Our decision to examine obesity rather than overweight was made due to its lower false-positive rate and stronger associations with physical and psychosocial health consequences and persistence into adulthood.51,52
We lacked detailed information to explore the role of medication use, which is fairly common in children with ASD; some medications used to treat ASD are associated with weight gain.53 In addition, the overall response rate for 2011–2012 was 23.0%, which was substantially lower than the prior NSCH survey conducted in 2007 (46.7%). This decline in response rate is primarily due to the inclusion of cell phone interviews in 2011–2012.54 Finally, despite the seemingly large sample size of the NSCH, only 925 children, including 175 girls, were diagnosed as having ASD, which limited power and conclusions that can be drawn from our exploratory analyses of the impact of sex, race/ethnicity, and household income on the age-related obesity disparity in ASD. Nevertheless, the findings are provocative and presented to prompt further inquiry.
Strengths of our analysis include a nationally representative data set with a larger sample size than is available from other US data sources so that sufficient data were available to examine the prevalence of obesity by single years of age. Our estimates of prevalence and related characteristics are expected to be representative of children in the United States nationally.
Conclusions
Our study demonstrates an increasing disparity in obesity prevalence over the years of adolescence between children with ASD and without ASD. The stability of the high obesity prevalence for youth with ASD across the adolescent ages studied, in contrast to declines seen for youth without ASD, is worthy of further investigation, ideally in longitudinal studies. Exploratory analyses suggest that these age-related discrepancies are particularly pronounced in males and may also be greater in nonminority youth and in lower income households. Given the large disparities in childhood obesity by race/ethnicity observed in typically developing children, it is important to establish whether sociodemographic factors in children with ASD/DD exert similar effects.
Better understanding of these age-related changes in obesity in children with and without autism and their associations with behavioral and sociodemographic factors could identify targets for prevention and treatment of obesity in adolescents with ASD. Such information will be important to the design and tailoring of programming and interventions for older youth with ASD, as well as for the anticipatory guidance offered to parents. Finally, our finding of declining obesity rates during adolescence in US youth without ASD suggests that further examination of factors associated with a change from being obese to a more healthy weight in this population may identify characteristics that could be exploited to promote more healthy weights in adolescents with ASD and across populations during early adulthood.
Acknowledgments
The Secondary Data Analysis Core of the Healthy Weight Research Network for Children with Autism Spectrum Disorder and Developmental Disabilities (HWRN) (1 UA3MC25735-01-00) conducted this research as part of the larger research agenda on obesity and its correlates in this population. The authors thank the other members of the HWRN for their participation in the Network's efforts. This effort was also supported by the Boston Obesity Nutrition Research Center P30DK46200.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Kimm SYS, Obarzanek E. Childhood obesity: A new pandemic of the new millennium. Pediatrics 2002;110:1003–1007 [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Halfon N, Larson K, Slusser W. Associations between obesity and comorbid mental health, developmental, and physical health conditions in a nationally representative sample of us children aged 10 to 17. Acad Pediatr 2013;13:6–13 [DOI] [PubMed] [Google Scholar]
- 4.Wang Y, Beydoun MA. The obesity epidemic in the United States—Gender, age, socioeconomic, racial/ethnic, and geographic characteristics: A systematic review and meta-regression analysis. Epidemiol Rev 2007;29:6–28 [DOI] [PubMed] [Google Scholar]
- 5.Wang Y, Zhang Q. Are American children and adolescents of low socioeconomic status at increased risk of obesity? Changes in the association between overweight and family income between 1971 and 2002. Am J Clin Nutr 2006;84:707–716 [DOI] [PubMed] [Google Scholar]
- 6.Delva J, O'Malley PM, Johnston LD. Racial/ethnic and socioeconomic status differences in overweight and health-related behaviors among American students: National trends 1986–2003. J Adolesc Health 2006;39:536–545 [DOI] [PubMed] [Google Scholar]
- 7.Bandini LG, Curtin C, Hamad C, et al. Prevalence of overweight in children with developmental disorders in the continuous National Health And Nutrition Examination Survey (NHANES) 1999–2002. J Pediatr 2005;146:738–743 [DOI] [PubMed] [Google Scholar]
- 8.Broder-Fingert S, Brazauskas K, Lindgren K, et al. Prevalence of overweight and obesity in a large clinical sample of children with autism. Acad Pediatr 2014;14:408–414 [DOI] [PubMed] [Google Scholar]
- 9.Chen AY, Kim SE, Houtrow AJ, et al. Prevalence of obesity among children with chronic conditions. Obesity 2010;18:210–213 [DOI] [PubMed] [Google Scholar]
- 10.Curtin C, Anderson SE, Must A, et al. The prevalence of obesity in children with autism: A secondary data analysis using nationally representative data from the National Survey of Children's Health. BMC Pediatr 2010;10:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed (DSM-5®). American Psychiatric Association: Arlington, VA, 2013 [Google Scholar]
- 12.Christensen DL, Baio J, Van Naarden Braun K, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2012. MMWR Surveill Summ 2016;65:1–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Autism and Developmental Disabilities Monitoring (ADDM) Network. www.cdc.gov/ncbddd/autism/addm.html Last accessed September23, 2016
- 14.Bandini LG, Anderson SE, Curtin C, et al. Food selectivity in children with autism spectrum disorders and typically developing children. J Pediatr 2010;157:259–264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hubbard KL, Anderson SE, Curtin C, et al. A comparison of food refusal related to characteristics of food in children with autism spectrum disorder and typically developing children. J Acad Nutr Diet 2014;114:1981–1987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Suarez MA, Crinion KM. Food choices of children with autism spectrum disorders. Int J School Health 2015;2:e27502 [Google Scholar]
- 17.Zimmer MH, Hart LC, Manning-Courtney P, et al. Food variety as a predictor of nutritional status among children with autism. J Autism Dev Disord 2012;42:549–556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Corvey K, Menear KS, Preskitt J, et al. Obesity, physical activity and sedentary behaviors in children with an autism spectrum disorder. Matern Child Health J 2016;20:466–476 [DOI] [PubMed] [Google Scholar]
- 19.Obrusnikova I, Cavalier AR. Perceived barriers and facilitators of participation in after-school physical activity by children with autism spectrum disorders. J Dev Phys Disabil 2011;23:195–211 [Google Scholar]
- 20.Tyler K, MacDonald M, Menear K. Physical activity and physical fitness of school-aged children and youth with autism spectrum disorders. Autism Res Treat 2014:312163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nally B, Houlton B, Ralph S. The management of television and video by parents of children with autism. Autism 2000;4:331–337 [Google Scholar]
- 22.Must A, Phillips SM, Curtin C, et al. Comparison of sedentary behaviors between children with autism spectrum disorders and typically developing children. Autism 2014;18:376–384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics 2007;120 Suppl 4:S164–S192 [DOI] [PubMed] [Google Scholar]
- 24.Dreyer Gillette ML, Borner KB, Nadler CB, et al. Prevalence and health correlates of overweight and obesity in children with autism spectrum disorder. J Dev Behav Pediatr 2015;36:489–496 [DOI] [PubMed] [Google Scholar]
- 25.McCoy SM, Jakicic JM, Gibbs BB. Comparison of obesity, physical activity, and sedentary behaviors between adolescents with autism spectrum disorders and without. J Autism Dev Disord 2016;46:2317–2326 [DOI] [PubMed] [Google Scholar]
- 26.Hill AP, Zuckerman KE, Fombonne E. Obesity and autism. Pediatrics 2015;136:1051–1061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Egan AM, Dreyer ML, Odar CC, et al. Obesity in young children with autism spectrum disorders: Prevalence and associated factors. Child Obes 2013;9:125–131 [DOI] [PubMed] [Google Scholar]
- 28.Curtin C, Bandini L, Perrin EC, et al. Prevalence of overweight in children and adolescents with attention deficit hyperactivity disorder and autism spectrum disorders: A chart review. BMC Pediatr 2005;5:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Vinck-Baroody O, Shui A, Macklin EA, et al. Overweight and obesity in a sample of children with autism spectrum disorder. Acad Pediatr 2015;15:396–404 [DOI] [PubMed] [Google Scholar]
- 30.2011/12 National Survey of Children's Health. Maternal and Child Health Bureau in collaboration with the National Center for Health Statistics. 2011/12 NSCH SAS Indicator Data Set prepared by the Data Resource Center for Child and Adolescent Health, Child and Adolescent Health Measurement Initiative. www.childhealthdata.org Last accessed September23, 2016
- 31.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data 2000;314:1–27 [PubMed] [Google Scholar]
- 32.Akinbami LJ, Ogden CL. Childhood overweight prevalence in the United States: The impact of parent-reported height and weight. Obesity 2009;17:1574–1580 [DOI] [PubMed] [Google Scholar]
- 33.Blumberg SJ, Foster EB, Frasier AM, et al. Design and operation of the National Survey of Children's Health, 2007, National Center for Health Statistics. Vital Health Stat 2012;1. [PubMed] [Google Scholar]
- 34.Parsons LS. Reducing Bias in a Propensity Score Matched-Pair Sample Using Greedy Matching Techniques. SAS Institute, Inc.: Cary, NC, 2001 [Google Scholar]
- 35.Phillips KL, Schieve LA, Visser S, et al. Prevalence and impact of unhealthy weight in a national sample of US adolescents with autism and other learning and behavioral disabilities. Matern Child Health J 2014;18:1964–1975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zuckerman KE, Hill AP, Guion K, et al. Overweight and obesity: Prevalence and correlates in a large clinical sample of children with autism spectrum disorder. J Autism Dev Disord 2014;44:1708–1719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Forrest KYZ, Leeds MJ. Prevalence and associated factors of overweight among Mexican-American adolescents. J Am Diet Assoc 2007;107:1797–1800 [DOI] [PubMed] [Google Scholar]
- 38.Pelegrini A, Petroski EL, Coqueiro RDS, et al. Overweight and obesity in Brazilian schoolchildren aged 10 to 15 years: Data from a Brazilian sports project. Arch Latinoam Nutr 2008;58:343–349 [PubMed] [Google Scholar]
- 39.Cole TJ, Bellizzi MC, Flegal KM, et al. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000;320:1240–1243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Valeria da Veiga G, Dias PC, dos Anjos LA. A comparison of distribution curves of body mass index from Brazil and the United States for assessing overweight and obesity in Brazilian adolescents. Rev Panam Salud Publica 2001;10:79–85 [DOI] [PubMed] [Google Scholar]
- 41.Bandini L, Curtin C, Anderson SE, et al. Food as a reward in children with autism. Abstract presented at the joint annual meeting of the ASPET/BPS at Experimental Biology FASEB J 2013;1063.11 [Google Scholar]
- 42.Marshall J, Sheller B, Mancl L. Caries-risk assessment and caries status of children with autism. Pediatr Dent 2008;32:69–75 [PubMed] [Google Scholar]
- 43.Ma NS, Thompson C, Weston S. Brief report: Scurvy as a manifestation of food selectivity in children with autism. J Autism Dev Disord 2016;46:1464–1470 [DOI] [PubMed] [Google Scholar]
- 44.Curtin C, Hubbard K, Anderson SE, et al. Food selectivity, mealtime behavior problems, spousal stress, and family food choices in children with and without autism spectrum disorder. J Autism Dev Disord 2015;45:3308–3315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Suarez MA, Atchison BJ, Lagerwey M. Phenomenological examination of the mealtime experience for mothers of children with autism and food selectivity. Am J Occup Ther 2014;68:102–107 [DOI] [PubMed] [Google Scholar]
- 46.van Steijn DJ, Oerlemans AM, de Ruiter SW, et al. Are parental autism spectrum disorder and/or attention-deficit/Hyperactivity disorder symptoms related to parenting styles in families with ASD (+ADHD) affected children?. Eur Child Adolesc Psychiatry 2013;22:671–681 [DOI] [PubMed] [Google Scholar]
- 47.Must A, Phillips S, Curtin C, et al. Barriers to physical activity in children with autism spectrum disorders: Relationship to physical activity and screen time. J Phys Act Health 2015;12:529–534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shields N, Synnot AJ, Barr M. Perceived barriers and facilitators to physical activity for children with disability: A systematic review. Br J Sports Med 2012;46:989–997 [DOI] [PubMed] [Google Scholar]
- 49.Stanish H, Curtin C, Must A, et al. Enjoyment, barriers, and beliefs about physical activity in adolescents with and without autism spectrum disorder. Adapt Phys Activ Q 2015;32:302–317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Obrusnikova I, Miccinello DL. Parent perceptions of factors influencing after-school physical activity of children with autism spectrum disorders. Adapt Phys Activ Q 2012;29:63–80 [DOI] [PubMed] [Google Scholar]
- 51.Barlow SE, Dietz WH. Obesity evaluation and treatment: Expert committee recommendations. The Maternal and Child Health Bureau, Health Resources and Services Administration and the Department of Health and Human Services. Pediatrics 1998;102:E29. [DOI] [PubMed] [Google Scholar]
- 52.Guo SS, Roche AF, Chumlea WC, et al. The predictive value of childhood body mass index values for overweight at age 35 y. Am J Clin Nutr 1994;59:810–819 [DOI] [PubMed] [Google Scholar]
- 53.Curtin C, Jojic M, Bandini LG. Obesity in children with autism spectrum disorder. Harv Rev Psychiatry 2014;22:93–103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Blumberg SJ, Bramlett MD, Kogan MD, et al. Changes in prevalence of parent-reported autism spectrum disorder in school-aged U.S. children: 2007 to 2011–2012. National Health Statistics Reports; 2013 [PubMed] [Google Scholar]