Abstract
Embolization is very effective in preventing bleeding of unruptured aneurysms with lower rates of mortality and morbidity than surgical treatment. Neurosurgery remains, however, a good alternative. This retrospective analysis examined data stored the digital database of Bellaria Hospital Radiology Department, evaluating patients, treatments and devices used as well as outcomes and complications. Therapy should be tailored to each individual case to offer each patient the best treatment. Out of 265 unruptured intracranial aneurysms detected, 182 were treated by embolization. 16 cases presented complications (12 only radiologically found); severe clinical consequences occurred in 3%: one ischaemia and five haemorrhages. Conservative treatment was adopted in 21 patients. Long-term follow-up is mandatory as aneurysms could increase their size and develop an irregular morphology in ten years' time. Endovascular embolization is a very effective treatment with positive outcomes in the majority of cases and a percentage of retreatments of 8%. In order to increase the number of successful cases, a multidisciplinary cooperation with neurosurgeons is strongly recommended.
Keywords: unruptured brain aneurysms, endovascular treatment, embolization
Introduction
In recent years, advances in computed tomography (CT) and magnetic resonance (MR) have increased the number of incidentally found unruptured intracranial aneurysms. This is a cause of concern for neuroradiologists and neurosurgeons because of the difficulty in managing these patients.
Embolization is very effective in preventing bleeding of unruptured aneurysms with lower rates of mortality and morbidity than surgical treatment3, especially in highly specialised centres treating large numbers of aneurysms. In addition, embolization is better tolerated than surgery9-11. Moreover, major developments of endovascular devices and the experience gained after years of international research have improved the number of positive outcomes9,12,13 and decreased the risk of complications7.
Complications rates vary, but in our experience at Bellaria Hospital it is around 2%8. Neurosurgery, however, remains the basic reference. This retrospective analysis of the Bellaria Hospital database sought to define the following points: which lesions need treatment? If so, which kind of treatment? Instead, which aneurysms can be subjected to conservative treatment? Therapy should be tailored to each individual case to offer each patient the best treatment. It is very important to intervene considering the particular features of each case, in order to offer each patient the best treatment for himself. So a multidisciplinary cooperation with neurosurgeons is strongly recommended.
Materials and Methods
The data were collected from the digital database of Bellaria Hospital Radiology Department that provided details on procedures and follow-ups.
Patients
Between 2000 and 2011, 265 unruptured intracranial aneurysms were treated at Bellaria Hospital. Patients comprised 194 women and 53 men. The following parameters were evaluated to optimize individual treatment: aneurysm morphology (saccular, sacciform, giant, small, multilobed, narrow or wide neck, weak wall, presence of blebs…) and location, morphology of the arterial cerebral tree (compatible or not with safe catheterization) and patients' clinical conditions.
Treatment
One hundred and eighty-two patients underwent embolization, 62 were moved to the Neurosurgical Department and 21 were subjected to conservative treatment. The devices used for embolization were: coils (98 patients), stent and coils (42 patients), stent (37 patients), glue (3 patients), artery occlusion (2 patients).
Subsequently, patients were followed up with MR and MR angiography1,11, CT and CT angiography for one, three and six months and when possible for one or more years to evaluate the effectiveness of embolization, stability of treatment and any procedure-related complications.
Results
Sixty-two patients (Table 1) were treated in the Neurosurgery Department. The criteria taken into consideration for surgical referral were the aneurysm characteristics (location, morphology, dimensions) in 50 cases. The decision was made in accordance with vessel characteristics in eight cases because of excessive tortuosity or vasospasm. Conservative treatment, despite, was adopted in 21 patients: in 19 cases because of the small size of the sac and in 2 cases due to the patient's clinical conditions (Table 2).
Table 1.
Neurosurgical criteria. At Bellaria Hospital, the morphologic characteristics of aneurysms are major criteria used to decide the most appropriate treatment for each patient. Neurosurgery was preferred in 50 cases out of 62 because of large irregular aneurysms, or if associated vessels were involved. In eight cases, vessel tortuosity or vasospasm did not allow safe catheterization.
| Criteria | No. of aneurysms |
|---|---|
| Aneurysm characteristics (location, morphology, dimensions, associated vessels) | 50 |
| Vessel characteristics (tortuosity, vasospasm) | 8 |
| Patient preference | 1 |
| Unknown (information not found in data base) | 2 |
| Total | 62 |
Table 2.
Conservative treatment criteria used. Aneurysms smaller than 7 mm in diameter; smaller sacs of patients with multiple aneurysms. Clinical conditions precluded treatment in two patients: a non-compliant oldest old patient and a young woman with severe cardiovascular disease.
| Criteria | No. of aneurysms |
|---|---|
| Dimensions (< 7 mm, 8 patients with multiple aneurysms) | 19 |
| Clinical conditions | 2 |
| Total | 21 |
Intraprocedural difficulties arose in seven out of 182 embolization procedures. In three cases the procedure was interrupted due to anatomic characteristics such as vascular tortuosity, risk for a safe catheterisation. Thromboembolism occurred in another three cases and haemorrhage in one case, all resolved during the same intervention without complications. According to specific procedures, patients were administered anticoagulants (heparin and other similar drugs), antiplatelets (aspirin and Clopidogel), fibrinolytics (rTPA, urokinase) or thrombolytics (GPIIIAIIb, Tirofibam, Abciximab). The case of procedural haemorrhage was treated by immediate embolization, without any complication.
Sixteen cases out of 182 presented complications: one small dissection, nine cases of is-chaemia and six haemorrhages. Severe clinical consequences occurred in one ischemia and in five haemorrhages (3% out of total). The aneurysms involved were eleven giant aneurysms, four medium aneurysms and only two small aneurysms. Moreover, fifteen of them had a wide neck, six of them presented bleb and five had an irregular wall or calcifications.
In terms of efficacy of endovascular treatment, only fourteen patients presented a re-canalization: eight of these patients were subjected to coils embolization, five had stent and coil embolization, and one underwent stent embolization. Thirteen of the 14 patients were retreated and presented excellent results. Only one aneurysm presented another recanalization that required a second treatment that proved successful after a long-term follow-up (MR angiography for four years)1,14.
Discussion
Thanks to the experience gained during the last ten years, individual treatments are now preferred. Focusing on the diagnostic phase, neuroradiologists and neurosurgeons cooperate to determine the most appropriate treatment for each patient. Moreover, thanks to the development of modern devices, diagnostic techniques and treatment modalities have significantly improved. Each aneurysm is now subjected to 3D high-resolution analysis, assessing its location and size, neck and sac and identifying potential spasm and the patency of its arterial tree. Therefore, it is possible to determine whether an aneurysm requires treatment or long-term observation, and when embolization rather than surgery is preferred.
The morphologic characteristics of aneurysms have been major criteria used to decide the most appropriate treatment for each patient: in fact, Neurosurgery is preferred for giant, irregular aneurysms, or if associated vessels are involved (Figure 1). Small and regular sacs, despite, underwent a conservative treatment, but a long-term follow-up had been crucial as aneurysms could increase their size and develop an irregular morphology in ten years' time15,17-20. This was demonstrated in a case of an 80-year-old woman with multiple aneurysms: a small aneurysm located in the perical-losal-callosal marginal bifurcation, diagnosed in 2003, proved stable at MR angiographic controls until 2010. Then, its size had grown and its lining proved irregular both to at MR angiography and angiography (Figure 2). Subsequently, after an accurate evaluation with Neurosurgeons, the patient was treated in the neurosurgery department. This diagnosis and clinical procedure helped avoid a subarachnoid haemorrhage in a high-risk patient.
Figure 1.
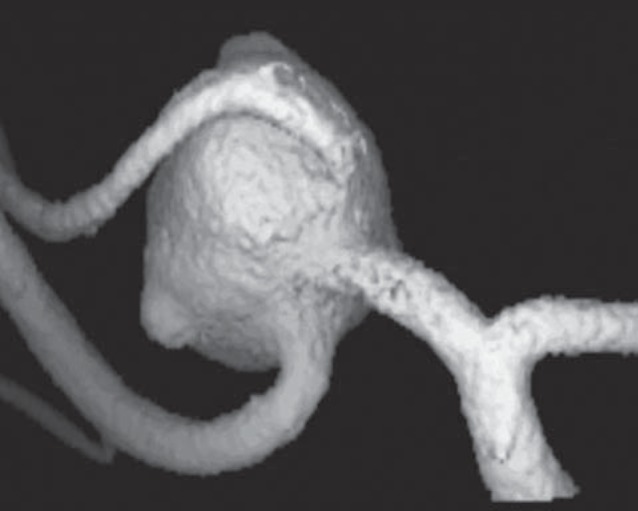
Irregular wide-necked aneurysm of the medium cerebral artery with bleb and involvement of the origin of M2 vessels. These morphologic characteristics were criteria for neurosurgery rather than endovascular treatment.
Figure 2.
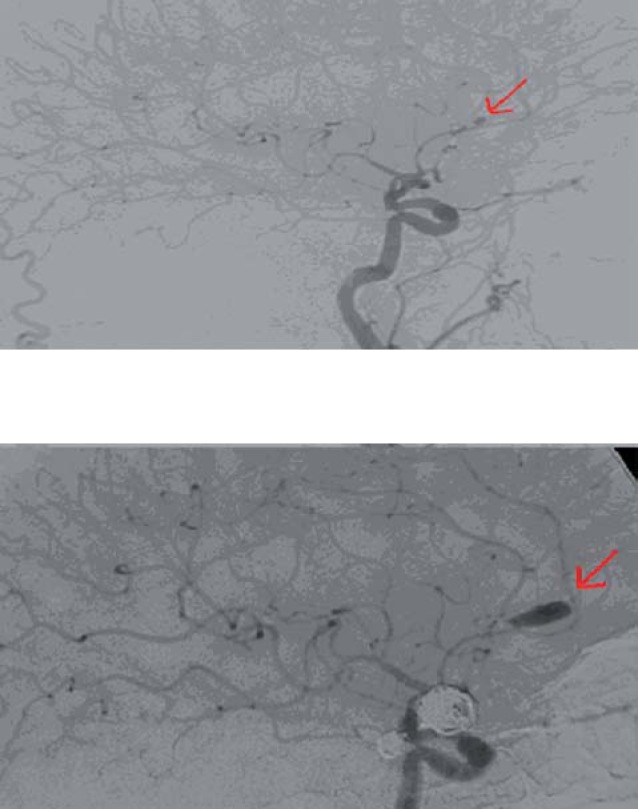
Angiogram of an 80-year-old woman with → multiple aneurysms: small aneurysm of the pericallosal-callos-al marginal bifurcation at diagnosis in 2003. After seven years of follow-up, the same aneurysm in 2010 has enlarged. The patient was treated in the neurosurgery department to avoid subarachnoid haemorrhage.
In our retrospective analysis, we found that morphologic characteristics of aneurysms were involved in complications: giant irregular and wide-necked aneurysms tend to have a higher percentage. The severity of these complications varies from absence of symptoms to death, and the main complications have been ischaemic and haemorrhagic events. Regarding haemorrhages, one patient out of six presented serious neurologic deficits and four of these patients died. Among this four, one of them was treated with a Neuroform stent, but it's difficult to understand the real cause of the death, because the temporal correlation between embolization and haemorrhage is not certain as the incident occurred more than 20 days after stent placement. Instead, three out of these four patients had been treated with Flow Diverter stents. This kind of stent offers great potential in terms of treatment efficacy, especially with giant unruptured partially thrombosed aneurysms. However, flow diverter gives rise to concern as there are no precise indications for its usage and because in medicine literature it is sometimes associated with post-procedural bleeding that can lead to death16. Another major problem in using this kind of device is the post-treatment antiplatelet therapy. This therapy is necessary to avoid serious cases of intra-stent thromboembolism but identifying the correct antiplatelet dosage and avoiding the risk of complications is highly complex. So our 4 cases of death have been discussed in a dedicated article on complications in the treatment of intracranial aneurysms with flow diverter stents4.
In our experience, endovascular treatment is very effective, as it emerges from the Results. Two negative factors affect the efficacy of endovascular treatment: incomplete occlusion of the aneurysm after the first treatment and possible refilling of the aneurysm sac. So we decided to evaluate the aneurysms involved in recanalization. According to the data collected at Bellaria Hospital, the percentage of patients with this complication is 8%, percentage lower than that reported in the literature (14-15%)5,9. Retreatments were effective and did not result in complications, presenting as events not so worrying as in the past.
Conclusions
Endovascular embolization is a very effective treatment that leads to positive results in the majority of cases. Its low rate of serious complications widely justifies its usage and now retreatment is not so worrying as in the past.
In order to increase the number of successful cases, a multidisciplinary cooperation with neurosurgeons is strongly recommended. This collaboration is necessary to analyse the clinical characteristics of each patient and the morphological characteristics of each aneurysm to identify the most appropriate treatment, and to evaluate those patients which could present complications, in order to offer the best result in terms of safeness and efficacy.
References
- 1.Adams WM Laitt RD Jackson A. The role of MR angiography in the pretreatment assessment of intracranial aneurysms: a comparative study. Am J Neuroradiol. 2000; 21 (9): 1618–1628. [PMC free article] [PubMed] [Google Scholar]
- 2.Alshekhlee A Mehta S Edgell RC et al. Hospital mortality and complications of electively clipped or coiled unruptured intracranial aneurysm. Stroke. 2010; 41 (7): 1471–1476. [DOI] [PubMed] [Google Scholar]
- 3.Brinjikji W Rabinstein AA Lanzino G et al. Patient outcomes are better for unruptured cerebral aneurysms treated at centers that preferentially treat with endovascular coiling: a study of the national inpatient sample 2001–2007. Am J Neuroradiol. 2011; 32: 1065–1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cirillo L Leonardi M Dall'olio M et al. Complications in Treatment of intracranial aneurysms with Silk stents: an Analysis of 30 consecutive patients. Interv Neuroradiol. 2012; 18: 413–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Friedman J Nichols D Meyer F et al. Guglielmi detachable coil treatment of ruptured saccular cerebral aneurysms: retrospective review of a 10-year single-centre experience. Am J Neuroradiol. 2003; 526–533. [PMC free article] [PubMed]
- 6.Heiserman JE Dean BL et al. , Neurologic complications of cerebral angiography. Am J Neuroradiol. 1994: 15: 1408–1411. [PMC free article] [PubMed] [Google Scholar]
- 7.Lee T Baytion M Sciacca R et al. Aggregate analysis of the literature for unruptured intracranial aneurysm treatment. Am J Neuroradiol. 2005; 26 (8): 1902–1908. [PMC free article] [PubMed] [Google Scholar]
- 8.Leonardi M Cenni P Spagnoli M et al. Three-Year Retrospective Study of Complications Arising during Interventional Procedures. Interv Neuroradiol. 2003: 9: 395–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Molyneux AJ Kerr R. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomized trial. J Stroke Cerebrovasc Dis. 2002; 11 (6): 304–314. [DOI] [PubMed] [Google Scholar]
- 10.Molyneux AJ Kerr RS. International subarachnoid aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion; Lancet. 2005; 366 (9488): 809–811. [DOI] [PubMed] [Google Scholar]
- 11.Molyneux AJ Kerr RS Birks J et al. Risk of recurrent subarachnoid haemorrhage, death, or dependence and standardised mortality ratios after clipping or coiling of an intracranial aneurysm in the International Subarachnoid Aneurysm Trial (ISAT): long-term follow-up. Lancet Neurol. 2009; 8 (5): 427–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murayama Y Nien YL et al. Guglielmi detachable coil embolization of cerebral aneurysms: 11 years' experience. J Neurosurgery. 2003; 98: 959–966. [DOI] [PubMed] [Google Scholar]
- 13.Oishi H Yamamoto M Shimizu T et al. Endovascular Therapy of 500 small asymptomatic unruptured intracranial aneurysms. Am J Neuroradiol. 2012; 33: 958–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Okahara M Kiyosue H Hori Y et al. Three-dimensional time-of-flight MR angiography for evaluation of intracranial aneurysms after endosaccular packing with Guglielmi detachable coils: comparison with 3D digital subtraction angiography. Eur Radiol. 2004; 14 (7): 1162–8. Epub 2004. [DOI] [PubMed] [Google Scholar]
- 15.Tsutsumi K Ueki K Morita A et al. , Risk of rupture from incidental cerebral aneurysms. Neurosurgery. 2000; 93 (4): 550–553. [DOI] [PubMed] [Google Scholar]
- 16.Turowsky B Macht S Kulcsar Z et al. Early fatal hemorrhage after endovascular cerebral aneurysm treatment with a flow diverter (SILK-Stent). Neuroradiology. 2011; 53: 37–41. [DOI] [PubMed] [Google Scholar]
- 17.Wiebers DO Whisnant JP O'Fallon WM. The natural history of unruptured intracranial aneurysms. N Engl J Med. 1981; 304 (12): 696–698. [DOI] [PubMed] [Google Scholar]
- 18.Wiebers DO Whisnant JP Sundt TM Jr et al. The significance of unruptured intracranial saccular aneurysms. Neurosurgery. 1987; 66 (1): 23–29. [DOI] [PubMed] [Google Scholar]
- 19.Wiebers DO Whisnant JP Huston J. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003; 362 (9378): 103–110. [DOI] [PubMed] [Google Scholar]
- 20.Winn HR Almaani WS Berga SL et al. The long-term outcome in patients with multiple aneurysms. Incidence of late hemorrhage and implications for treatment of incidental aneurysms. Neurosurgery. 1983; 59 (4): 642–651. [DOI] [PubMed] [Google Scholar]


