Abstract
This report describes endovascular approaches for occlusion of vertebro-vertebral arteriovenous fistula (W-AVF) in a series of three cases and a review of the literature. Complete neuroimaging assessment, including CT, MR and DSA was performed in three patients (two female, one male) with W-AVF. Based on DSA findings, the W-AVF were occluded by endovascular positioning of detachable balloons (case 1), coils (case 2), or a combination of both (case 3) with parent artery patency in two out of three cases. In this small series, endovascular techniques for occlusion of W-AVF were safe and effective methods of treatment. To date, there are no guidelines on the best treatment for W-AVF. Detachable balloons, endovascular coiling, combined embolization procedures could all be considered well-tolerated treatments.
Keywords: arteriovenous fistula, vertebral artery, embolization, detachable coils, detachable balloon
Introduction
A direct communication between the extracranial vertebral artery or its muscular/radicu-lar branches and epidural venous intervertebral plexus, without intervening capillaries, is termed vertebro-vertebral arteriovenous fistula (VV-AVF)1,2.
We describe the endovascular approaches used for occlusion of VV-AVF in three patients and the selection criteria, and compare our experience with literature reports of VV-AVF treatments.
The clinical and neuroradiological records of all patients referred to our Institute for the diagnostic and therapeutic work-up of a craniospinal vascular malformation in the decade 2000-2010 were retrospectively reviewed. All patients underwent a complete neuroimaging assessment, including computed tomography angiography (CTA) or magnetic resonance angiography (MRA) of the supraortic vessels and digital subtraction angiography (DSA) to evaluate the best treatment options for fistula occlusion. The clinical and radiological characteristics of our series are summarized in Table 1.
Table 1.
Clinical and radiological characteristics of patients.
| Age /Sex | Location | Etiology | Symtoms | |
|---|---|---|---|---|
| 1 | 61/M | Right VA C2-C3 | Previous multiple fractures at C2-C6 level. | Rigor nucahs and inferior limbs weakness |
| 2 | 56/F | Right VA C3-C4 | Spontaneous; chiropractic manipulation | Cervical pain radiating down to the right arm |
| 3 | 34/F | Right VA C2-C3 | Secondary (NF1) | Bilateral tinnitus, objective vertigo, right arm paresthesia |
Case 1
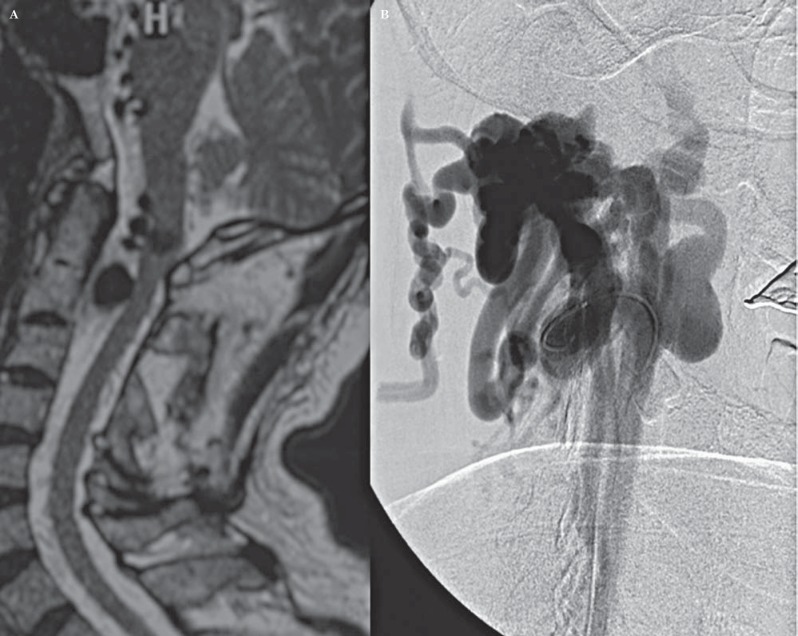
A 61-year-old man, with previous multiple fractures at C2-C6 level and epidural hematoma at C1-C4 after a recent cervical trauma, presented rigor nucalis and inferior limbs weakness. MRA showed a right ectasic vertebral artery (VA) at the anterior epidural level (Figure 1A). DSA showed a direct VV-AVF between the right VA at C2 level and periradicular venous plexus (Figure 1B).
Figure 1.
A) Sagittal T2-w MRI shows a right ectasic vertebral artery at the anterior epidural level; B) Preoperative right vertebral artery DSA shows a direct VV-AVF between the right VA at C2 level and the periradicular venous plexus.
An endovascular approach was chosen. Systemic heparinization was given seven days before the procedure. Before sacrificing the vessel an occlusion test was performed. Due to a good collateral circulation, a right VA occlusion was planned. An 8 Fr introducer sheath (Cordis) was placed in the right common femoral artery route and the right VA was catheterized with a 8 Fr. The site of the fistula was less evident, the large size of the single arterial communication and the high flow prompted an endovascular balloon occlusion of the VV-AVF. A BAL1XRAY (Balt, Extrusion, Montmorency, France) mounted on a MABDTE (Balt Extrusion, Montmorency, France) microcatheter was maneuvred into the right VA and positioned in the fistulous tract under fluoroscopic control. The balloon was inflated with 50% of 300 mg I/ml iohexol and 50% of saline, and after satisfactory occlusion of the AVF, was detached at this site. Postembolization angiograms showed immediate occlusion of the fistula with no early filling of the epidural veins (Figure 2A-C).
Figure 2.
Operative DSA (A-C): the balloon is detached at the fistula point with preservation of parent vertebral artery patency.
Case 2
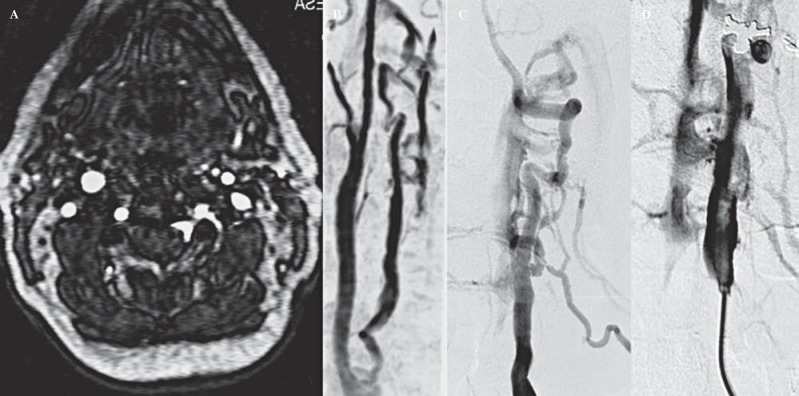
A 56-year old woman presented with cervical pain radiating down to the right arm. She also reported a pulsatile bruit on the right side of the neck which, in auscultation, was spreading over the chest. Physical and neurological examinations were otherwise unremarkable and medical history was negative for surgical or endovascular procedures. A history of chiropractic manipulation to alleviate the pain was referred. MRA revealed an extradural fistula of the vertebral artery at the C3-C4 level (Figure 3A, B). DSA showed a dilated extracranial segment of the right VA and a high flow communication between the muscular branches of the VA and the periradicular venous plexus (Figure 3C, D). The intervention was performed under general anesthesia and the systemic heparization protocol was the same as adopted in the first patient. A 6 Fr introducer sheath (Cordis) was placed in the right common femoral artery route and the right vertebral artery was catheterized with a 6 Fr. A microcatheter (Cordis, Prowler plus 0.14) was placed proximal to the arterial edge of the fistula and coiling was attempted with two electrodetachable coils (Micrus, 4×15 and 6×25, respectively). Immediate occlusion of the fistula was reported. Angiographic post-procedural evaluation confirmed complete occlusion of the fistula with preservation of right vertebral artery patency. The patient experienced no complications and had a total regression of symptoms (Figure 4A-C).
Figure 3.
Axial MRA TOF 3D (A) and MIP reconstruction (B) showing an extradural fistula of the vertebral artery involving the perivertebral venous plexus at C3-C4 level. Vertebral artery DSA (C, D) shows a dilated extracranial segment of the right vertebral artery between the muscular branches of the vertebral artery and a dilated periradicular venous plexus.
Figure 4.
Vertebral artery operative DSA (A-C) shows complete occlusion of the fistula with coils and preservation of right vertebral artery patency.
Case 3
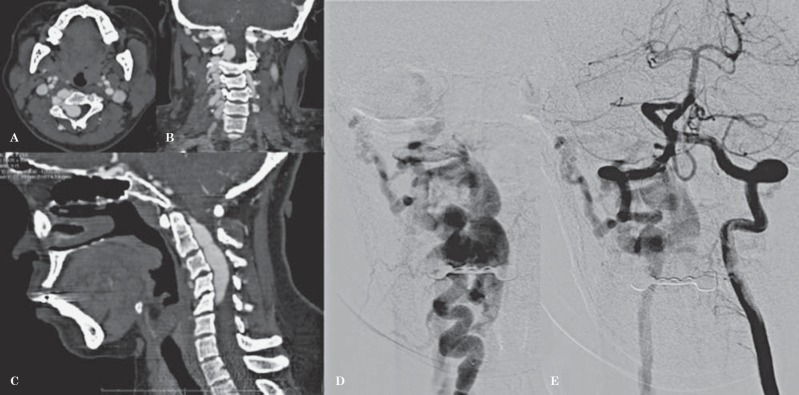
A 34-year-old woman with neurofibromatosis type 1 (NF1) presented with a four-month history of bilateral tinnitus, objective vertigo and right arm paresthesia. No history of trauma was referred. A supraaortic vessels color Doppler examination was negative. An arterial puff was discovered on the jugular vein. CTA showed an extradural fistula of the right VA with multiple arteriovenous high flow shunts at C2-C5 level (Figure 5A-C). DSA confirmed the diagnosis (Figure 5D, E).
Figure 5.
Contrast-enhanced CT angiography, MPR reconstruction (A) axial (B) coronal (C) sagittal, shows an extradural fistula of the right VA with multiple arteriovenous high-flow shunts at C2-C5 level. Pre-operative DSA right (D) and left (E) VA injection: large VVAF in NF1 with flow steal.
An endovascular approach was performed. An 8 Fr introducer sheath (Cordis) was placed in the right common femoral artery route and the right vertebral artery was catheterized with a 8 Fr A BAL1XRAY detachable latex balloon (Balt Extrusion, Montmorency, France) mounted on a MABDTE (Balt Extrusion, Montmorency, France) microcatheter maneuvered into the right VA and positioned at the fistulous tract under fluoroscopic control. The VA was sacrificed due to a good collateral circulation (Figure 6A). DSA control after two months showed partial reperfusion of the VV-AVF so endovascular VA occlusion was undertaken with coils (Figure 6B). Control angiograms from the controlateral VA showed complete occlusion of the fistula and opacification of the right posterior inferior cerebellar artery (PICA) from the left VA (Figure 6C). The peri and postprocedural periods were uneventful and the patient experienced no complications and had a total regression of symptoms.
Figure 6.
Operative DSA: partial occlusion with detachable balloon (A). Complete VA and fistula occlusion with further coiling (B). C) Post-embolization DSA by controlateral VA injection shows patency of the right PICA.
Discussion
VV-AVF is uncommon and consists of an abnormal communication between the extracranial vertebral artery or its branches and the deep venous plexus1. The most common cause of VV-AVF is penetrating neck injury, blunt cervical trauma, iatrogenic forms of trauma including direct percutaneous puncture of a carotid or vertebral artery for diagnostic angiography, or vertebral artery injury during insertion of central venous catheters2,3. Dys-plastic conditions of the vascular wall such as NF1, fibromuscular dysplasia or Ehlers-Danlos should be considered predisposing factors4-11. Whatever the pathogenesis, VV-AVF may be asymptomatic or become symptomatic due to compression on the spinal cord or roots, bleeding, or vascular steal.
A surgical approach to VV-AVF is no longer warranted in most circumstances. The classic surgical procedure is based on direct surgical ligature of punctiform fistulas and the use of bypass venous graft from the subclavian to the distal vertebral artery for large, complex fistulas with several arterial feeders. Steal flow symptoms, massive hemorrhages and injuries to surrounding structures have been associated with surgical treatment2.
As symptoms are usually progressive, prompt treatment is needed: the endovascular occlusion of the VV-AVF is considered the first therapeutic option, with a variety of devices developed to achieve fistula occlusion while possibly preserving the parent VA patency2,9. As with surgery, periprocedural and postprocedural ischemic or thromboembolic complications and vessel injuries can also occur2,12. Detachable balloons3,13-14, stent grafts15-20, and detachable coils21-27 are the embolic materials that have been used to treat VV-AVF. Particulate embolic agents and cyanoacrylate glue are avoided in the treatment of high-flow fistulas, as they are likely to be swept away by rapid flow without occlusion of the fistula. Endovascular treatment with a detachable balloon to occlude the fistula is preferred over microsurgical ligation, coil embolization, or stent-grafting. Detachable balloons are most suitable for occlusion of fistulas because they can be repeatedly inflated and deflated prior to their detachment so that precise placement and optimal occlusion of the fistula can be achieved3,13-14. However the balloon could deflate with a recurrence of the fistula. When the fistula is not well seen or masked by ectasic vessels, detachable coils, used in our case 2, show advantages such as electrically induced thrombosis with no recanalization and retrievability when the position is not satisfactory. These advantages help to reduce the risk of embolic complications, especially in high-flow fistulas, preserving the patency of the adjacent artery21,28. Experience with endovascular stent-graft repair is limited15-20. These devices are feasible and offer a therapeutic alternative in the treatment of VV-AVF, particularly for preserving vessel patency. However, these devices are currently very rigid and not suitable if vessels are tortuous15-20. This minimally invasive treatment may become of the choice management of this kind of lesions, but at the moment should be considered experimental18,29-33.
In particular situations, endovascular treatment can be very difficult and a complex approach is required. Gao et al.9 reported two cases of VV-AVF in two patients with NF1, successfully treated with a combined complex approach. In one of these patients, both right and left VAs were catheterized, respectively: a detachable balloon was placed in the VV-AVF varix to provide flow control, which allowed to three coils to be deployed together for obliteration; an appropriate mixture of glue was then used to avoid coil migration.
Reviewing the recent literature (Table 2), endovascular treatment with detachable balloons, alone or with other devices, was used in 12/29 patients (41%): all VAs, except one3, were sacrificed with no clinical outcome. In all cases this approach was therapeutic, except for one which required surgery10. Endovascular coiling alone or with other devices was performed in 16/29 patients (55%): all VAs were sacrificed except for three21,27 with no neurological symptoms. Endovascular stenting was performed in 2/29 (6%) patients: both VAs were patent after the procedure15,16. Detachable balloons, endovascular coiling, or combined embolization treatment should be chosen by evaluating the fistula and parent vessel anatomy, hemodynamics and flow (high or low)29,30,34-37. According to our experience if the AVF flow is low and the point of fistula is evident at DSA, as in our case 2, progressive coil occlusion is recommended. For high flow VV-AVF, when the VA sacrifice is possible and well-tolerated and the point of fistula is less evident, as in our cases 1 or 3, balloon occlusion or combined treatment (coil and glue; coil and balloon) are advised.
Table 2.
Review of the literature.
| Author | Patients | Device | Flow/size | Level | Cause | Parent VA |
|---|---|---|---|---|---|---|
| Modi et al.4 | 1 | Balloon | High/Large | C3 | Spontaneous | Patent |
| Reddy et al.5 | 1 | Cods (failed); Surgery | - | C2-C3 | Traumatic | Sacrificed due to coiling |
| Shirikawa et al.7 | 1 | Coils | High/Large | C6 | Traumatic | Sacrificed |
| Sadato et al.8 | 1 | Stent | High/Large | C4-C5 | Spontaneous | Patent |
| Gonzalez et al.9 | 1 | Stent | High/Small | C7 | Iatrogenic | Patent |
| Benndorf et al.15 | 1 | Cods (failed); Coils (transvenous) | High/Giant | Low | NF1 | Sacrificed |
| Kahara et al.16 | 1 | Coils | High/Large | C3-C4 | NF1 | Sacrificed |
| Siddharta et al.17 | 2 | Coils (1); Balloon (1) | High/Large (both) | C5 (both) | NF1 | Sacrificed (both) |
| Hauck et al.18 | 1 | Cods (failed); Coils and surgery. | –/Large | C3-C4 | NF1 | Sacrificed |
| Gao et al.19 | 2 | Balloon, coils and glue; | High/Large (Both) | C2-C3 C5 | NF1 | Sacrificed |
| Paolini et al.20 | 1 | Balloon (failed); Surgery | High/Large | C2-C3 | NF1 | Sacrificed |
| Patro et al.21 | 1 | Surgery (failed); Coils | High/Large | C5-C6 | NF1 | Sacrificed |
| Briganti et al.22 and Present Report | 3 |
|
|
|
|
Sacrificed Patent Sacrificed |
| Taylor et al.24 | 2 |
|
|
|
|
Sacrificed (both) |
| De Keukeleire et al.25 | 1 | Coils | High/Large | C2 | Spontaneous | Sacrificed |
| Wang et al.26 | 1 | Coils and glue | High/Large | C3 | Spontaneous | Sacrificed |
| Mortimer et al.27 | 1 | Coils | – | Low | Traumatic | Sacrificed |
| Kai et al.28 | 2 | Coils (venous) | Low/ Small | C6 C1 | Iatrogenic | Patent (Both) |
| Herrera et al.29 | 4 | Balloon | Low/Small | Various | Traumatic (all) | Sacrificed (All) |
| Heuer et al.30 | 1 | Coils | High/NA | C2 | Traumatic | Sacrificed |
| 29 |
Conclusion
In this small series, endovascular techniques for occlusion of VV-AVF were safe and effective methods of treatment. In expert hands, even the sacrifice of the parent VA can be accomplished without complications. To date, there are no guidelines on the best treatment of VV-AVF, and detachable balloons, endovascular coiling, and combined embolization procedures can all be considered well-tolerated treatments. No rules for flow diverter devices are currently available.
References
- 1.Deans WR Block S Leibrock L et al. Arteriovenous fistula in a patient with neurofibromatosis. Radiology. 1982; 144: 103–107. [DOI] [PubMed] [Google Scholar]
- 2.Beaujeux RL Reizine DC Casasco DC et al. Endovascular treatment of vertebral arteriovenous fistula. Radiology; 1992; 183: 361–367. [DOI] [PubMed] [Google Scholar]
- 3.Modi M Bapuraj JR Lal A et al. Vertebral arteriovenous fistula presenting as cervical myelopathy: a rapid recovery with balloon embolization. Cardiovasc Intervent Radiol. 2010; 33 (6): 1253–1256. doi: 10.1007/s00270-009-9708-2. Epub 2009 Sep 19. [DOI] [PubMed] [Google Scholar]
- 4.Hori Y Goto K Ogata N et al. Diagnosis and endovascular treatment of vertebral arteriovenous fistulas in Neurofibromatosis Type 1. Interv Neuroradiol. 2000; 6 (3): 239–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benndorf G Assmann U Bender A et al. Vertebral arteriovenous fistula associated with neurofibromatosis type I misdiagnosed as a giant aneurysm. Interv Neuroradiol. 2000. 6 (1): 67–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kahara V Lehto U Ryymin P et al. Vertebral epidural arteriovenous fistula and radicular pain in neurofibromatosis type 1. Acta Neurochir (Wien). 2002, 144 (5): 493–496. [DOI] [PubMed] [Google Scholar]
- 7.Siddharta W Chavhan G Shrivastava M et al. Endovascular treatment for bilateral vertebral arteriovenous fistulas in neurofibromatosis 1. Australas Radiol. 2003, 47 (4): 457–461. [DOI] [PubMed] [Google Scholar]
- 8.Hauck EF Nauta HJV. Spontaneous spinal epidural arteriovenous fistulae in neurofibromatosis type-1. Surg Neurol. 2006; 66 (2): 215–221. [DOI] [PubMed] [Google Scholar]
- 9.Gao P Chen Y Zhang H et al. Vertebral arteriovenous fistulae (AVF) in neurofibromatosis type 1: a report of two cases. Turk Neurosurg. 2013; 23 (2): 289–293. [DOI] [PubMed] [Google Scholar]
- 10.Paolini S Colonnese C Galasso V et al. Extradural arteriovenous fistulas involving the vertebral artery in neurofibromatosis type 1. J Neurosurg Spine. 2008; 8 (2): 181–185. [DOI] [PubMed] [Google Scholar]
- 11.Patro SN Gupta AK Arvinda HR et al. Combined transarterial and percutaneous coiling of a spontaneous vertebrovertebral fistula associated with neurofibromatosis Type 1. Case report. J Neurosurg. 2009: 111 (1): 37–40. [DOI] [PubMed] [Google Scholar]
- 12.Higashida RT Halbach W Tsai FY et al. Interventional neurovascular treatment of traumatic carotid and vertebral artery lesions: results in 234 cases. Am J Roentgenol. 1989; 153 (3): 577–582. [DOI] [PubMed] [Google Scholar]
- 13.Reddy M Schoggl A Saringer W et al. Traumatic arteriovenous fistula of the vertebral artery. Case report. Neurol Med Chir (Tokyo). 2002; 42 (7): 289–292. [DOI] [PubMed] [Google Scholar]
- 14.Yoshida S Nakazawa K Oda Y. Spontaneous vertebral arteriovenous fistula: Case Report. Neurol Med Chir (Tokyo). 2000; 40 (4): 211–215. [DOI] [PubMed] [Google Scholar]
- 15.Sadato A Satow T Ishii A et al. Large vertebral arteriovenous fistula treated with stent-grafts. Case report. Neurol Med Chir (Tokyo). 2003; 43 (5): 250–254. [DOI] [PubMed] [Google Scholar]
- 16.Gonzalez A Mayol A Gil Peralta A et al. Endovascular stent-graft treatment of an iatrogenic vertebral arteriovenous fistula. Neuroradiology. 2001; 43 (9): 784–786. [DOI] [PubMed] [Google Scholar]
- 17.Surber R Werner GS Conhert T et al. Recurrent vertebral arteriovenous fistula after surgical repair: treatment with self-expanding stent-graft. J Endovasc Ther. 2003; 10 (1): 49–53. [DOI] [PubMed] [Google Scholar]
- 18.Alaraj A Wallace A Amin-Hanjani S et al. Endovascular implantation of covered stents in the extracranial carotid and vertebral arteries: case series and review of the literature. Surg Neurol Int. 2011; 2: 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Briganti F Tortora F Marseglia M et al. Covered stent implantation for the treatment of direct carotid-cavernous fistula and its mid-term follow-up. Interv Neuroradiol. 2009. 15 (2): 185–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Priestley R Bray P Bray A et al. Iatrogenic vertebral arteriovenous fistula treated with a hemobahn stent-graft. J Endovasc Ther. 2003; 10 (3): 657–663. [DOI] [PubMed] [Google Scholar]
- 21.Briganti F Tortora F Elefante A et al. An unusual case of vertebral arteriovenous fistulas with electrodetachable coil embolization. Minim Invasive Neurosurg. 2004; 47 (6): 386–388. [DOI] [PubMed] [Google Scholar]
- 22.Taylor CG Husami Y Colquhoun IR et al. Direct cervical vertebro-venous fistula with radiculopathy and MRI changes resolving after successful endovascular embolisation: a report of two cases. Neuroradiology. 2001; 43 (12): 1118–1122. [DOI] [PubMed] [Google Scholar]
- 23.Asai J Hayashi T Suzuki R et al. Spontaneous resolution of an idiopathic cervical direct vertebral arteriovenous fistula after partial coil embolization in a patient presenting with myeloradiculopathy. Clin Neurol Neurosurg. 2002; 104 (2): 146–151. [DOI] [PubMed] [Google Scholar]
- 24.De Keukeleire K Defreyne L Vanlangenhove P et al. Asymptomatic congenital extradural vertebral arteriovenous fistula: treatment with electrolytically detachable coils. Cardiovasc Intervent Radiol. 2006, 29 (2): 311–314. [DOI] [PubMed] [Google Scholar]
- 25.Wang Q Song D Chen G. Endovascular treatment of high-flow cervical direct vertebro-vertebral arteriovenous fistula with detachable coils and onyx liquid embolic agent. Acta Neurochir (Wien). 2011; 153 (2): 347–352. [DOI] [PubMed] [Google Scholar]
- 26.Mortimer A Stubbs E Cookson D et al. Delayed presentation of a vertebral arterio-venous fistula secondary to penetrating cervical trauma: endovascular management using coil embolisation - A case report. J Radiol Case Rep. 2009; 3 (6): 9–15. doi: 10.3941/jrcr.v3i6.81. Epub 2009 Jun 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kai Y Hamada JI Mizuno T et al. Transvenous embolization for vertebral arteriovenous fistula: report of two cases and technical notes. Acta Neurochir (Wien). 2001; 143 (2): 125–128. [DOI] [PubMed] [Google Scholar]
- 28.Miralbes S Catlin F Andrea I et al. Vertebral arteriovenous fistula: endovascular treatment with electrodetachable coils. Neuradiology. 1998; 40 (11): 761–762. [DOI] [PubMed] [Google Scholar]
- 29.De Divitiis O Elefante A De Divitiis E. Historic background of spinal disorders. World Neurosurg. 2013; 79 (1): 91–94. [DOI] [PubMed] [Google Scholar]
- 30.De Divitis O Elefante A. Cervical spinal brucellosis: A diagnostic and surgical challenge. World Neurosurg. 2012; 78 (3–4): 257–259. [DOI] [PubMed] [Google Scholar]
- 31.Elefante A Peca C Del Basso De Caro ML et al. Symptomatic spinal cord metastasis from cerebral oligodendroglioma. Neurol Sci. 2012; 33 (3); 609–613. [DOI] [PubMed] [Google Scholar]
- 32.Capalbo D Elefante A Spagnuolo MI et al. Posterior reversible encephalopathy syndrome in a child during an accelerated phase of a severe APECED phenotype due to an uncommon mutation of AIRE. Clin Endocrinol (Oxf). 2008; 69 (3): 511–513. [DOI] [PubMed] [Google Scholar]
- 33.Caranci F Napoli M Cirillo M et al. Basilar artery hypoplasia. Neuroradiol J. 2012; 25 (6): 739–743. [DOI] [PubMed] [Google Scholar]
- 34.Caranci F Briganti F Cirillo L et al. Epidemiology and genetics of intracranial aneurysms. Eur J Radiol. 2013. pii: S0720-048X(13)00011-9. doi: 10.1016/j.ejrad.2012.12.026. [Epub ahead of print]. [DOI] [PubMed]
- 35.Briganti F Cicala D Tortora F et al. Endovascular treatment of a giant dissecting aneurysm of the posterior cerebral artery: A case report and literature review. Neuroradiol J. 2012; 25 (6): 695–701. [DOI] [PubMed] [Google Scholar]
- 36.Briganti F. Reply to comment of Dr. W-J van Rooij on: Italian multicenter experience with flow diverter devices for intracranial unruptured aneurysm treatment with periprocedural complications a retrospective data analysis. Neuroradiology. 2012; 54 (10): 1181–1182. [DOI] [PubMed] [Google Scholar]
- 37.Briganti F Napoli M Tortora F et al. Italian multicenter experience with flow-diverter devices for intracranial unruptured aneurysm treatment with periprocedural complications - A retrospective data analysis. Neuroradiology. 2012; 54: 1145–52. doi: 10.1007/s00234-012-1047-3. Epub 2012 May 9. [DOI] [PubMed] [Google Scholar]
- 38.Briganti F Cirillo S Caranci F et al. Development of “de novo” aneurysms following endovascular procedures. Neuroradiology. 2002; 44 (7): 604–609. [DOI] [PubMed] [Google Scholar]
- 39.Spetzler RF Detwiler PW Riina HA et al. Modified classification of spinal cord vascular lesions. J Neurosurg. 2002; 96 (2 Suppl): 145–156. [DOI] [PubMed] [Google Scholar]
- 40.Shirakawa M Nishioka T Yamashita K et al. Traumatic vertebro-vertebral arteriovenous fistula manifesting as radiculopathy. Neurol Med Chir (Tokyo). 2008, 48 (4): 167–170. [DOI] [PubMed] [Google Scholar]
- 41.Herrera DA Vargas SA Dublin AB. Endovascular treatment of traumatic injuries of vertebral artery. Am J Neuroradiol. 2008; 29 (8): 1585–1589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Heuer GG Brandon BC Bhowmick DA et al. Symptomatic high-flow arteriovenous fistula after a C-2 fracture. Case report. J Neurosurg Spine. 2008, 8 (4): 381–384. [DOI] [PubMed] [Google Scholar]